Abstract
The thermoneutral zone is defined as the range of ambient temperatures where the body can maintain its core temperature solely through regulating dry heat loss, i.e., skin blood flow. A living body can only maintain its core temperature when heat production and heat loss are balanced. That means that heat transport from body core to skin must equal heat transport from skin to the environment. This study focuses on what combinations of core and skin temperature satisfy the biophysical requirements of being in the thermoneutral zone for humans. Moreover, consequences are considered of changes in insulation and adding restrictions such as thermal comfort (i.e. driver for thermal behavior). A biophysical model was developed that calculates heat transport within a body, taking into account metabolic heat production, tissue insulation, and heat distribution by blood flow and equates that to heat loss to the environment, considering skin temperature, ambient temperature and other physical parameters. The biophysical analysis shows that the steady-state ambient temperature range associated with the thermoneutral zone does not guarantee that the body is in thermal balance at basal metabolic rate per se. Instead, depending on the combination of core temperature, mean skin temperature and ambient temperature, the body may require significant increases in heat production or heat loss to maintain stable core temperature. Therefore, the definition of the thermoneutral zone might need to be reformulated. Furthermore, after adding restrictions on skin temperature for thermal comfort, the ambient temperature range associated with thermal comfort is smaller than the thermoneutral zone. This, assuming animals seek thermal comfort, suggests that thermal behavior may be initiated already before the boundaries of the thermoneutral zone are reached.
Keywords: mathematical model, metabolism, theoretical biology, thermal behaviour, thermoregulation
Introduction
The thermoneutral zone (TNZ) is defined as: ‘the range of ambient temperature at which temperature regulation is achieved only by control of sensible (dry) heat loss, i.e. without regulatory changes in metabolic heat production or evaporative heat loss.’1 One remarkable feature of the classical TNZ definition is that it only considers autonomic thermoregulatory mechanisms, and omits the influence of thermal behavior. Nevertheless, thermal behavior is considered as the major influencing factor of body temperature homeostasis,2 and is driven by thermal comfort.3 The thermal comfort zone (TCZ) is defined in terms of perception and qualifies as the state of mind that expresses satisfaction with the thermal environment.4 Furthermore the TCZ is suggested to relate to positive anticipations of the current thermal environment. In other words, thermal discomfort (i.e., negative anticipation) drives a human being to counteract the thermal environment accordingly.
According to their definitions the TNZ and the TCZ are not directly related to each other. However, physiologically, both zones share a common source of information, namely skin and core temperature.5 Furthermore, functionally, they may share a common goal, that is to preserve body temperature.6 A living body can only maintain a stable core temperature when heat production and heat loss are balanced. That means that heat transport from body core to the skin must equal heat transport from skin to the environment.
This study investigates what combinations of body core, skin and ambient temperature satisfy the biophysical requirements of being in the TNZ for humans. Nevertheless concepts apply to other animals as well. Moreover, we study the consequence of changes in insulation and adding restrictions such as thermal comfort (i.e., derive TCZ). By comparing the ambient temperature ranges associated with the TNZ and the TCZ, the aim is to better understand the link between the two, and discuss practical implications with respect to metabolic research and the built environment.
Methods
This section describes the biophysical model that is used to analyze what combinations of body core temperature (Tc), mean skin temperature (Ts) and ambient temperature (Ta) satisfy the requirements of thermal balance. The section is structured as follows: first the effect size of autonomic and behavioral thermoregulatory mechanisms are described, second the biophysical model is introduced, third the ranges of biological and physical model parameters for 2 scenarios are given, fourthly the equations for Ts and Tc are given. Fifthly, 4 categories are defined that indicate what thermoregulatory action is required to maintain thermal balance. Sixthly, the derivation of Ta ranges associated with the TNZ and TCZ is described.
Thermoregulation within the TNZ: effect size
With respect to mechanisms of thermoregulation within the TNZ, we only consider mechanisms that influence insulation, and do not result in changes in metabolic heat production. With this restriction, the body is able to change total body tissue insulation by changes in blood flow from 0.124 m2°C/W (i.e., maximal vasoconstriction) to 0.031 m2°C/W (i.e., maximal vasodilation) respectively.7 Together, through behavioral regulation clothing insulation can be changed from 0 m2°C/W (i.e., nude, 0 Clo) to 0.92 m2°C/W (i.e., arctic clothing, 6 Clo), the airflow and thereby also insulation provided by air can be modified (e.g., draft or breeze) or Ta can be adjusted (e.g., thermostat in building), see Figure 1 for a schematic overview.
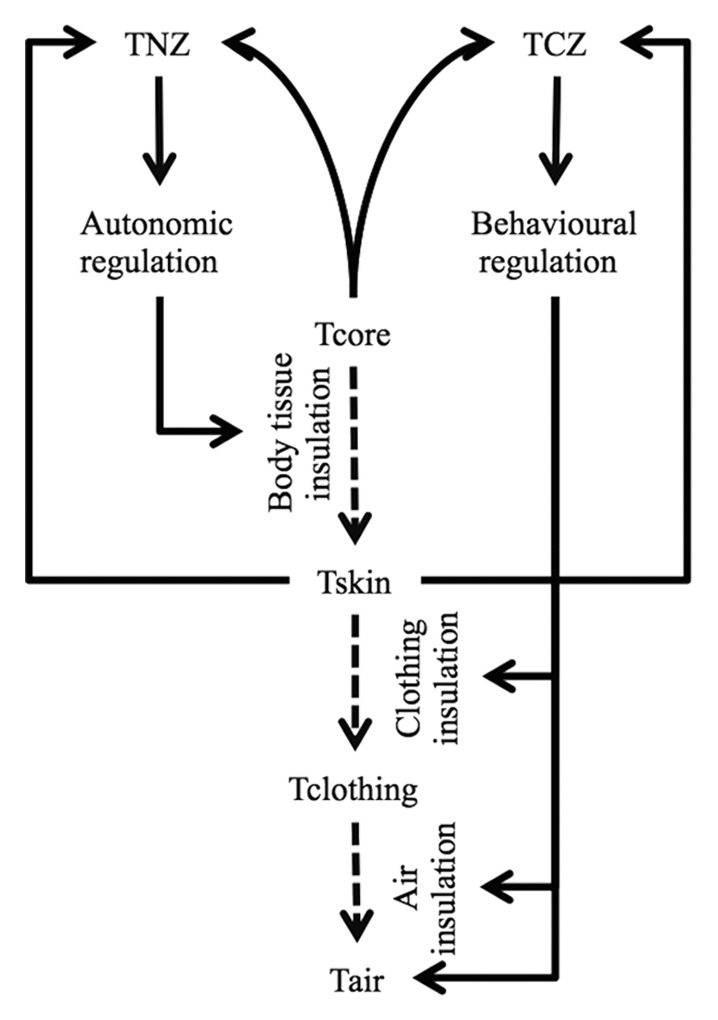
Figure 1. schematic overview of autonomic and behavioral control of thermal insulation. Solid arrows denote relation and/or control and dashed arrows denote heat flow.
Biophysical thermal network model
A biophysical thermal network model was used to calculate Tc and Ts, taking into account metabolic heat production (M), dynamic body tissue insulation (Ibody), static clothing insulation (Icl), static air insulation (Iair) and evaporative heat loss, see Figure 2.
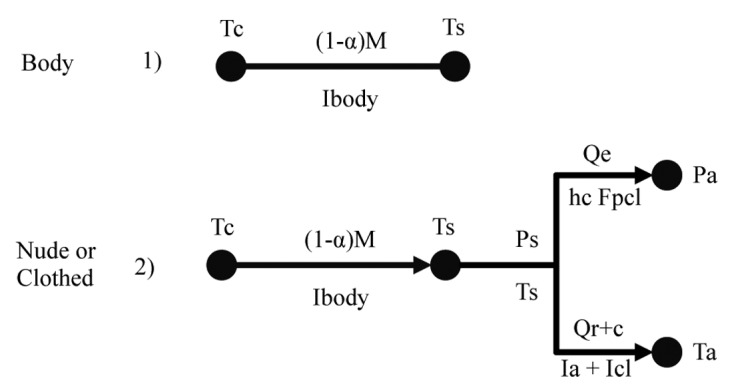
Figure 2. Thermal network to describe heat balance in the thermoneutral zone. Tc: core temperature, Ts: mean skin temperature, Ta: ambient temperature, (1−α)M: metabolic rate corrected for respiratory heat loss, Qr+c: combined radiative and convective heat loss, Ps: saturated vapor pressure at skin surface, Pa: vapor pressure of the air, Qe: evaporative heat loss, hc: convective heat loss coefficient, Fpcl: clothing evaporative permeability coefficient, Ibody: body insulation, Icl: clothing insulation, Ia: air insulation.
1. With the first model (Fig. 2. Body) the range of Ts that satisfy a steady-state thermoneutral condition is calculated for a range of Tc around Tc = 37 °C, a range of M corrected for respiratory heat loss (see Supplemental Material, A2), and a range of (Ibody) associated with maximal vasoconstriction and maximal vasodilation. Specific ranges are defined below.
2. With the second model (Fig. 2. Nude or Clothed) steady-state Tc is calculated over a range of ambient temperatures 10°C ≤ Ta ≤ 40 °C and skin temperatures 20 °C ≤ Ts ≤ 40 °C, given low wind speed (air velocity = 0.1 m/s) air insulation, in nude and in clothed condition. Ibody is calculated as a function of Ts.
Physiological insulation, anthropometry and metabolic rate
Total body insulation is defined by a passive part: tissue insulation, and an active part: regulation of skin blood flow. In case of total skin vasoconstriction, tissue insulation provided by muscle and fat is about Ibody,min = 0.124 m2°C/W for a man with 4 mm subcutaneous fat.8 In case of full skin vasodilation, passive tissue insulation is by-passed and reduces Ibody to about Ibody,min = 0.031 m2°C/W .7 Thus, Ibody is inversely related to blood flow. Several experiments show a linear relation between Ts, skin blood flow and Ibody for a resting man.7,9 Therefore, we calculate body insulation as a linear function of skin temperature (see E1). The modeled Ts of Ibody,max results from the minimal skin temperature (Ts,min) that satisfies steady-state thermoneutral condition with Tc = 36 °C. Likewise, modeled Ts of Ibody,min results from the maximal skin temperature Ts,max that satisfies steady-state thermoneutral condition with Tc = 38 °C. Thus the equation for Ibody is given by:
(E1)
Where Ts,min ≤ Ts ≤ Ts,max.
Heat loss from skin to environment scales linearly with body surface area (A). For this study, body surface area is set to correspond to an average man A = 1.86 m2.10
The minimum amount of heat production to sustain life is referred to as the basal metabolic rate (BMR). In literature, BMR for an average man is reported as BMR ≈ 86 W or BMR ≈ 46 W/m2.4 BMR is significantly related to age, gender, length and height.11 To account for these influences, we consider a 5% range 82 W ≤ BMR ≤ 90 W in this paper. BMR is often measured in physiological laboratory experiments. During such experiments, volunteers are quasi-nude and in supine position. Nevertheless, under daily living conditions, e.g., in office conditions, humans operate seldom in this state. Changes in posture, arousal and activity increase M significantly. For a sitting male, performing office work M ≈ 112W or M ≈ 60 W/m2. Similar to the BMR, a range of M is considered in this paper 106 W ≤ M ≤ 118 W.
To model both laboratory and office conditions, 2 scenarios are considered:
1) Classical TNZ: a nude person in supine position at BMR and
2) Functional TNZ: a clothed person in sitting condition at M associated with office work. The insulation provided by clothing is Icl = 1Clo = 0.155 W/m2°C.
Here, the classical scenario refers to the TNZ as defined in the glossary of terms for thermal physiology;1 the functional scenario is analogous to the definition of ‘TNZ classical’ with the difference that clothing is worn and M > BMR.
Equations for minimum and maximum Ts as a function of Tc, M, Ibody and A
Heat balance between M and heat transport from core to skin minus respiratory heat loss is satisfied when . Here, α = 0.08 is the fraction of M that is accounted for respiratory heat loss (see Supplemental Material, A2 for more details).12
Minimum Ts for which M and body heat transport is balanced corresponds to the state where Tc is minimal and M and Ibody are maximal and vice versa for maximal Ts. Hence the feasible steady-state Ts range is defined as: (E2).
Equation of Tc as a function of Ts and other heat transfer parameters
The equation for Tc below follows the scheme where M corrected for respiratory heat loss equals heat loss by radiation and convection (Qr+c) plus evaporative heat loss (Qe). For brevity, only the final equation for Tc is given in this section, see Supplemental Material for full derivation,
(E3).
Here Ta is ambient temperature in °C, Iair, is air insulation in m2°C/W, Ibody refers to body insulation in m2°C/W, Icl, is clothing insulation in m2°C/W and Qe/A is evaporative heat loss in W/m2.
Heat balance categories
Solutions for which Tc and Ts remain in steady-state are calculated for 10 °C ≤ Ta ≤ 40 °C, and skin temperature 20 °C ≤ Ts ≤ 40 °C. Constellations of Ta and Ts (solutions) that do not satisfy (36 °C ≤ Tc ≤ 38 °C) are filtered out. Until now, no restrictions on heat flow, other than (1−α)M = Qr+c + Qe, are defined; only temperatures are calculated that satisfy heat flow balance with the environment. Categories of body heat deficit, body heat surplus or body heat balance are defined by calculating the actual heat flow for each of the solutions and comparing that to the metabolic rate corrected for respiratory heat loss. The 4 categories are defined as follows:
1) TNZ body: heat loss is balanced relative to metabolic rate:
(1−α)Mmin ≤ Qr+c + Qe ≤ (1−α)Mmax ,
2) SWEAT: there is a heat surplus and evaporation is required to maintain thermal balance: Qr+c + Qe ≤ (1−α)Mmin,
3) NST: there is a heat deficit and cold induced thermogenesis by non-shivering (Mnst = 0.12M) is sufficient to maintain thermal balance: (1−α)Mmax ≤ Qr+c + Qe ≤ (1−α)(Mmax + Mnst),13
4) SH+NST: there is a heat deficit and cold induced thermogenesis by shivering and non-shivering is required to maintain thermal balance: (1−α)(Mmax + Mnst) ≤ Qr+c + Qe ≤ (Msh + Mnst),
here maximal heat production through shivering and non-shivering is capped at Msh + Mnst = 372W, which is the empirical maximum cold-induced heat production in humans.14
Finding Ta associated with TNZ and TCZ
This section describes how the set of solutions described above (i.e., combinations of Ta and Ts) are further filtered to define the Ta range for the TNZ and the TCZ.
For the TNZ, the Ta range is defined by the subset of solutions for which corresponding Ts satisfy that body heat transport equals M, i.e., Ts,min ≤ Ts ≤ Ts,max.
To find the TCZ the same method is applied, however, the values for Ts,min and Ts,max are different. In this study the main comfortable skin temperature range used is 31.5 °C ≤ Ts ≤ 35.5 °C as reported by Gagge et al.15 Moreover, a more conservative range 32.8 °C ≤ Ts ≤ 33.8 °C as reported for man in supine position by Weiwei et al. is also considered.16
Results
The results section is structured as follows: first the TNZ is presented for the classical condition (i.e., not clothed and at basal metabolic rate) and the functional condition (i.e., clothed in business suit and at office work metabolic rate), second the TCZ is presented for both conditions.
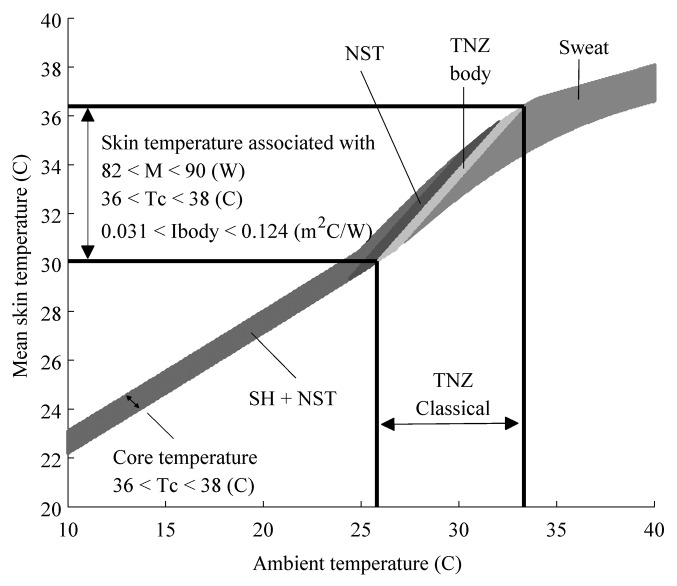
Classical TNZ: nude and basal metabolic rate
The steady-state Ta range for the TNZ for a person in a nude condition and heat production at BMR as calculated by the model are shown in Figure 3. Each band in Figure 3 depicts for a given Ta the range of Ts in which the equation constraints are satisfied for each category, e.g., ‘TNZ body’, ‘SWEAT’, ‘NST’, ‘SH+NST’. The band labeled ‘TNZ body’ depicts that thermal balance is satisfied and heat loss equals BMR. Thus, ‘TNZ body’ indicates for which Ts the ‘TNZ classical’ is supported from the perspective of human body internal heat transport.
Figure 3. The classical thermoneutral zone (denoted by ‘classical TNZ’), is defined as the range of ambient temperature at which temperature regulation is achieved only by control of sensible (dry) heat loss, i.e., without regulatory changes in metabolic heat production or evaporative heat loss. Each band depicts for a given ambient temperature the range of mean skin temperature in which the equation constraints are satisfied for each category, e.g., ‘TNZ body’, ‘SWEAT’, ‘NST’, ‘SH+NST’. The light gray area labeled TNZ body depicts solutions that satisfy that internal body heat transport equals external heat loss and core temperature ranges between 36 °C ≤ Tc ≤ 38 °C. In other words, TNZ body indicates where the classical thermoneutral zone is supported from the perspective of the human body. NST: solutions for which steady-state heat loss is between 83 W ≤ Q ≤ 88 W. The body can achieve thermal balance by non-shivering thermogenesis. Shiver+NST: solutions for which steady-state heat loss is between 88 W ≤ Q ≤ 372 W. The body can achieve thermal balance by shivering thermogenesis. SWEAT: solutions for which steady-state heat loss is Q ≤ 83 W. The body can achieve thermal balance by increased evaporation.
Steady-state skin temperature ranges between 30.5 °C ≤ Ts ≤ 36.8 °C. Where Ts = 30.5 °C corresponds to Tc = 36 °C and Ibody,max = 0.124 m2°C/W and Mmin = 82 W. Vice versa Ts = 36.8 °C corresponds to Tc = 38 °C, Ibody,min = 0.031 m2°C/W and Mmax = 90 W. Consequently, the slope of body insulation vs. skin temperature is −0.015 m2/W (used in Equation 1).
The area labeled ‘SH+NST’ is narrower than the area labeled ‘SWEAT.’ This is explained by body insulation. In case of ‘SH+NST’ the body is at maximal insulation. This means the body can vary internal heat transport up to 30W, whereas in case of ‘SWEAT’ the body is at maximal conduction, in this case the body internal heat transport can vary up to 120 W. In between maximal vasoconstriction and maximal vasodilation the body gradually changes from an insulator to a conductor, and consequently, for each ambient temperature there is a wider range of skin temperatures that satisfy the steady-state solutions.
It is important to note that the steady-state ambient temperature range associated with the classical TNZ does not guarantee that the body is in thermal balance at basal metabolic rate per se. Instead, depending on the combination of Ts and Ta, the body may require significant increases in heat production or heat loss to maintain core temperature stable within the range 36 °C ≤ Tc ≤ 38 °C (see ‘Sweat’, ‘NST’ and ‘SH+NST’ areas within the ‘TNZ classical’ range in Fig. 3) or even will not be able to keep the body in thermal balance (see white region inside ‘TNZ classical’ range in Fig. 3). For example, if skin temperature is Ts = 32°C, the body can remain in thermal balance when 26.8 °C ≤ Ta ≤ 28.9 °C, shivering is required for 26.8 °C ≤ Ta ≤ 27.3 °C, NST is sufficient for 27.3 °C ≤ Ta ≤ 27.9 °C and sweating is required for 28.5 °C ≤ Ta ≤ 28.9 °C. Only if the ambient temperatures range 27.9 °C ≤ Ta ≤ 28.5 °C the body can be in thermoneutral balance for 36 °C ≤ Tc ≤ 38 °C.
Functional TNZ: clothed and performing office work
Relative to the nude case, clothing insulation and increased M shift the TNZ to lower Ta and cause the solution areas to be wider. That is, for each Ta in ‘TNZ functional’ there is a wider range of Ts for which the body can support required heat transport than in ‘TNZ classical’.
The TNZ for a clothed person is (14.8 °C ≤ Ta ≤ 24.5 °C), see Figure 4. The skin temperature ranges between (28.8 °C ≤ Ts ≤ 36.4 °C). The slope of body insulation vs. skin temperature is −0.012 m2/W (used in Equation 1). Core temperature and body insulation ranges are the same as in the laboratory case, however Mmin = 106 W and Mmax = 118 W and corresponds to the metabolic rate of a sedentary man performing office work.
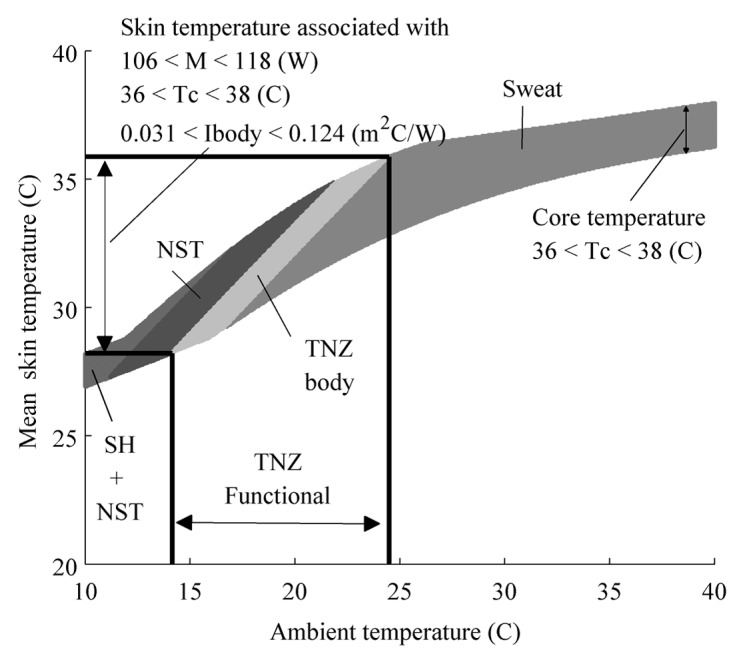
Figure 4. The functional thermoneutral zone is denoted by ‘functional TNZ’ for a person dressed in a business suit and heat production associated with light office work. The definition of ‘TNZ functional’ is analogous to the definition of ‘TNZ classical’ with the difference that the metabolic heat production is greater than the basal metabolic rate. Each band depicts for a given ambient temperature the range of mean skin temperature in which the equation constraints are satisfied for each category, e.g., ‘TNZ body’, ‘SWEAT’, ‘NST’, ‘SH+NST’. The light gray area labeled TNZ body depicts solutions that satisfy that internal body heat transport equals external heat loss and core temperature ranges between 36 °C ≤ Tc ≤ 38 °C. In other words, TNZ body indicates where the functional TNZ is supported from the perspective of the human body. NST: solutions for which steady-state heat loss is between 107 W ≤ Q ≤ 118 W. The body can achieve thermal balance by non-shivering thermogenesis. Shiver + NST: solutions for which steady-state heat loss is between 118 W ≤ Q ≤ 372 W. The body can achieve thermal balance by shivering thermogenesis. SWEAT: solutions for which steady-state heat loss is Q ≤ 98 W. The body can achieve thermal balance by increased evaporation.
TCZ: nude and basal metabolic rate
Next we narrow the band of thermoneutral skin temperatures from 30.5°C ≤ Ts ≤ 36.8 °C to the comfortable skin temperature range as reported by Gagge et al. (31.5 °C ≤ Ts ≤ 35.5 °C). This narrows the ambient temperature range of the TNZ: 25.9 °C ≤ Ta ≤ 33.3 °C to the TCZ: 27.5 °C ≤ Ta ≤ 32.3 °C, see Figure 5. Hence the laboratory steady-state TCZ is narrower than the steady-state thermoneutral zone (∆Ta,tnz = 6.9 °C vs. ∆Ta,tcz = 4.8°C). Constraining the comfortable skin temperature range even further to a conservative 32.8 °C ≤ Ts ≤ 33.8 °C as reported by WeiWei et al., the conservative comfortable ambient temperature range is restricted to 29.0 °C ≤ Ta ≤ 30.4 °C.
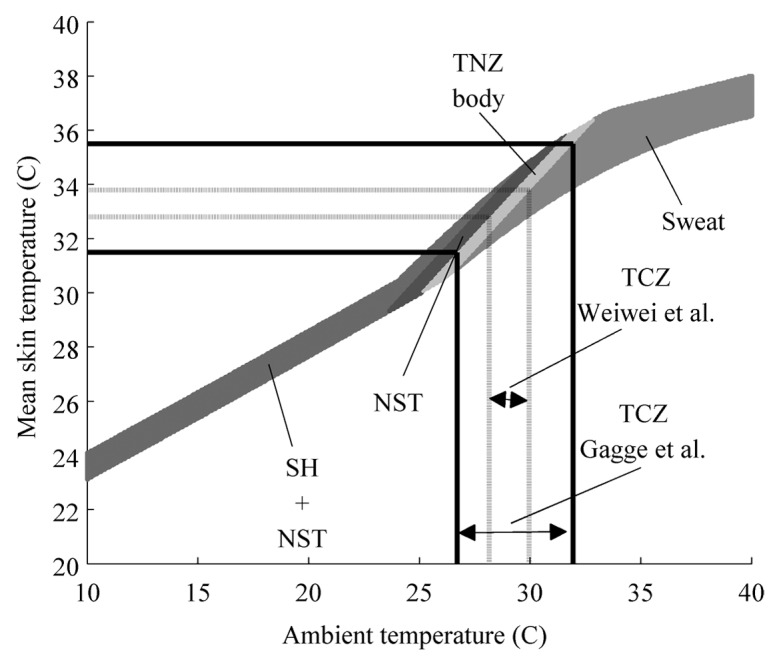
Figure 5. Steady-state ambient temperature ranges of the thermal comfort zone for a nude person. Each band depicts for a given ambient temperature the range of mean skin temperature in which the equation constraints are satisfied for each category, e.g., ‘TNZ body’, ‘SWEAT’, ‘NST’, ‘SH+NST’. The light gray area labeled ‘TNZ body’ depicts solutions that satisfy that internal body heat transport equals external heat loss and core temperature ranges between 36 °C ≤ Tc ≤ 38 °C. The Solid lines indicate comfortable mean skin temperature is as reported by Gagge et al.15 The dashed lines indicate a more conservative range of comfortable mean skin temperature range as reported by Weiwei et al.16
Interestingly, even the conservative ambient thermal comfort range includes solutions where the body would need to either produce or lose more heat to maintain thermal balance, see Figure 5 areas ‘NST’ and ‘Sweat’ within the dashed lines.
TCZ: clothed and at resting metabolic rate
As with the laboratory case, the comfortable mean skin temperature range 31.5 °C ≤ Ts ≤ 35.5 °C narrows the ambient temperature range from TNZclothed: 14.5 °C ≤ Ta ≤ 24.5°C to TCZclothed: 17.5 °C ≤ Ta ≤ 24.0 °C, see Figure 6. Hence the laboratory steady-state thermal comfort zone is narrower than the steady-state thermoneutral zone (∆Ta,tnz = 9.7 °C vs. ∆Ta,tcz = 6.5 °C). For the conservative comfortable mean skin temperature range (32.8 °C ≤ Ts ≤ 33.8 °C), the conservative comfortable ambient temperature range is narrowed down to 19.5 °C ≤ Ta ≤ 21.9 °C.
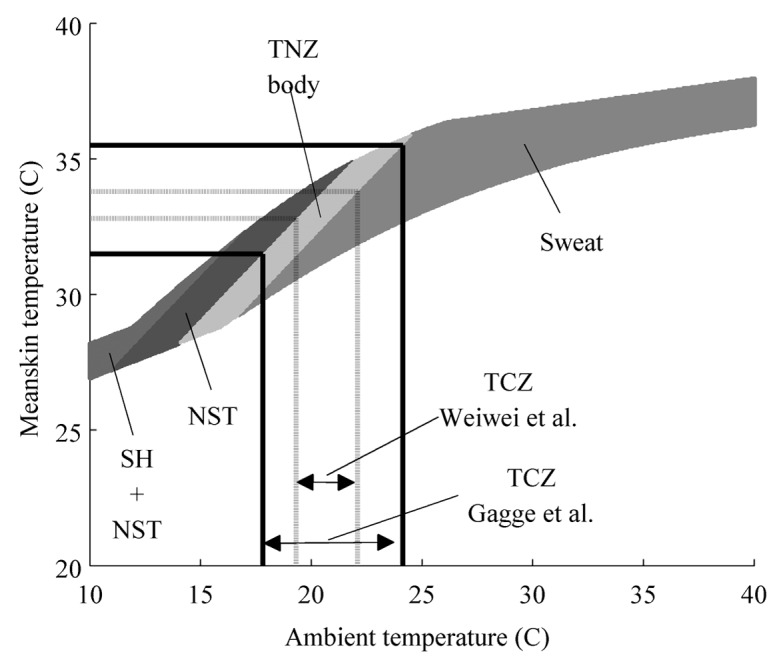
Figure 6. Steady-state ambient temperature range of the thermal comfort zone for a person dressed in a business suit and heat production at resting metabolic rate. Each band depicts for a given ambient temperature the range of mean skin temperature in which the equation constraints are satisfied for each category, e.g., ‘TNZ body’, ‘SWEAT’, ‘NST’, ‘SH+NST’. The light gray area labeled TNZ body depicts solutions that satisfy that internal body heat transport equals external heat loss and core temperature ranges between 36 °C ≤ Tc ≤ 38 °C. Comfortable mean skin temperature is as reported by Gagge et al.15 The dashed lines indicate a more conservative range of comfortable mean skin temperature range as reported by Weiwei et al.16
Discussion
This study describes what constellations of Tc, Ts, Ta satisfy the biophysical requirements of being in the thermoneutral zone for steady-state conditions. Furthermore, by constraining Ts to a temperature range associated with thermal comfort the thermal comfort zone is derived.
Toward a more accurate definition of the TNZ
The biophysical analysis in this study shows that depending on Ts, the classical definition of the TNZ does not guarantee at all that the body is indeed in a thermoneutral state. As can be seen in Figure 3, only the light gray area denoted as ‘TNZ body’ supports a thermoneutral state. For instance, in the nude condition, when ambient temperature is Ta = 30 °C, thermoneutral mean skin temperature is bound to 33.4 °C ≤ Ts ≤ 33.8 °C. However, body processes other than temperature regulation (e.g., blood pressure regulation, circadian rhythm or disease) may influence skin temperature as well.17 If Ts exceeds the predefined bounds, increased heat production (in case of higher Ts) or evaporation (in case of lower Ts) is required to maintain heat loss balanced relative to the metabolic rate. In determining the thermoneutral temperature ranges for rats the importance of skin temperature is already taken into account.18 Therefore, the current definition of the TNZ might require a revision. According to the authors a more accurate definition of the thermoneutral zone would be: ‘the combinations of ambient temperature and mean skin temperature for a given core temperature at which temperature regulation is achieved only by control of sensible (dry) heat loss, i.e. without regulatory changes in metabolic heat production or evaporative heat loss’. This subtle difference has a significant impact on the design of metabolic studies that require a thermoneutral condition, since controlling Ta alone is not sufficient.
The TNZ and experiments
The first study that describes the TNZ in air and in humans is by Hardy and Dubois.19 They report a lower critical ambient temperature Ta,H&D ≈ 28.5 °C and corresponding skin temperature TS,H&D = 33.5 °C. At first glance, these values are considerably different than reported in this study (Ta = 26.4 °C and Ts = 30.5 °C). However, Hardy and Dubois did not define where they measured skin temperature and their volunteers also had a lower M ≈ 75W and lower Ibody,max ≈ 0.093 m2°C/W. Using these averaged parameters the biophysical model finds for the lower bound Ta = 29.2 °C and Ts = 32.5 °C, which is more in line with the experimental findings. The example above stresses the importance of the M and the capacity of the body to change Ibody in relation to the TNZ. Notably, if M increases due to normal behavioral activity, the neutral ambient temperature range is considerably lowered compared with the resting state. This is especially relevant in housing of mice and small rodents for which the housing temperature is crucial to mimic the thermal conditions of humans.20
Thermal comfort and indoor environments
The relation between the TNZ and TCZ is based on mean skin temperature ranges associated with thermal comfort. Two ranges are considered: a relatively wide range as reported by Gagge et al.,15 and a more conservative, relatively narrow range as reported by WeiWei et al.16 Both skin temperature ranges associated with thermal comfort are narrower than the skin temperature range associated with the TNZ. Consequently, the derived Ta range of the TCZ is narrower than the thermoneutral zone (compare Figs. 3 and 5). In this study mean skin temperature was considered in relation to thermal comfort in a uniform and steady-state environment. However, several studies show the importance of distal skin temperatures in relation to thermal comfort in non-uniform and transient environments.21,22 Analysis of non-uniform and transient environments is outside the scope of this study, however, this may require attention in a future study. Likewise, Tc is known to affect thermal comfort as well.5,23 For instance, relatively low core temperature (Tc = 36 °C), is shown to require relatively high mean skin temperature (Ts ≈ 35 °C) to maintain thermal comfort. The model in this paper does not impose that extra restriction. Adding the restriction could possibly lead to further narrowing of the TCZ.
As thermal comfort is considered as the major driver for thermal behavior,3 results of this study suggest that thermal behavior is likely to be initiated before the bounds of the TNZ are reached. Putting this in perspective of thermal discomfort being the negative anticipation of the thermal environment there is a benefit to preserve the individual being by counteracting a potentially hazardous environment before any harm is done. Nevertheless, as a result of acclimatization (e.g., regular exposure to a thermal challenge), the body may learn that it is able to cope with that environment without harm, and as such, recognize the respective thermal environment as relatively comfortable. Indeed, an acclimation study from our laboratory shows that already after 10 d of regular exposure to a discomfortable cold environment and outside the thermoneutral zone, thermal comfort increases from ‘uncomfortable’ to ‘just comfortable’.24 Thus, the TCZ may be more flexible than the TNZ and, after acclimation, may be extended outside the TNZ.25
Current indoor thermal environment design for thermal comfort is primarily based on PMV (Predicted Mean Vote) criteria, calculated by the PMV/PPD model developed by Fanger.26 The PMV is expressed on a 7-point Thermal Sensation Scale ranging from cold (−3) to hot (+3). This vote can be linked to thermal comfort through the PPD, i.e., the percentage of people who will be dissatisfied with the thermal environment. The PMV/PPD model incorporates clothing, metabolic heat production and heat loss for a person at comfortable skin temperature. This is comparable to the current study approach, except that this study includes the variable thermal insulation of the body itself. For clothed man (1Clo) performing office work (112 W), as in the functional case covered in this study, Fanger assumes as mean skin temperature TS,F = 34.7 °C and predicts the comfortable ambient temperature range (vair = 0.1 m/s) between 21.5 °C ≤ Ta,F ≤ 25.1 °C, where ǀPMVǀ ≤ 0.5 . Using the same value for mean skin temperature the biophysical model returns 21.7 °C ≤ Ta ≤ 23.1 °C, which is comparable for the lower part, yet the upper limit of the PMV model is 2 °C higher than the upper limit of our biophysical model. This suggests that humans remain in thermal comfort even while limited increases in evaporation through sweating are required to maintain a stable body temperature.
Although the PMV/PPD model is designed for static thermal environments only, experiments show that the PMV/PPD model can also be applied during small thermal transients.4 This can be explained with the physiological aspect of the model described in this paper, that is during a small thermal transient the body may adjust body insulation or skin temperature and remain in the ‘TNZ body’ area (see Fig. 6), and thus does not require increased evaporation, metabolic heat production or any form of thermal behavior in order to preserve body temperature. However, perhaps more interesting, even within the Ta and Ts ranges associated with thermal comfort areas marked as ‘NST’ and ‘SWEAT’ are found. This suggests that a significant increase in metabolic heat production may be possible without losing thermal comfort, which in turn may be beneficial to prevent or counteract metabolic diseases such as obesity and diabetes.
Considerations and limitations
Several model parameters in this biophysical model study were chosen to reflect a human in a resting condition. In this section consequences and limitations of these model choices are considered. Furthermore, it should be noted that although the model parameter values are retrieved from empirical studies, the exercise performed in this manuscript is not an in vivo experiment and thus requires an independent study to validate the finds, both for the TNZ and the TCZ.
First, on physiological parameters, the M was chosen as BMR and that during daily office work, which is slightly higher than the BMR. Increased activity would significantly increase M. As a result the TNZ would become wider (see equation E2) and shift to cooler Ta. Furthermore, values for Ibody were obtained from studies on healthy lean male subjects; in case of obesity it is reasonable to assume higher body tissue insulation. Besides M and Ibody, body core temperature range used (36 °C ≤ Tc ≤ 38 °C) might not be sufficient to justify the entire range of body tissue insulation in resting man, i.e., there is evidence that maximal vasodilation and minimal tissue insulation are expected at body core temperature above 38 °C.27 Second, on physical and boundary parameters, skin wetness was considered 6% of total skin surface area as proposed for resting man by Gagge et al.28 In case of greater skin wetness, evaporative heat loss would be greater and consequently shift the TNZ to warmer Ta. In contrast, higher relative humidity (ϕ > 50%) would make it harder to evaporate sweat and shift the thermoneutral zone to lower Ta. Furthermore, air velocity was set relatively low (vair = 0.1 m/s). In case of draft or a breeze convective heat loss would increase and shift the TNZ to lower ambient temperatures.
Conclusion
This study describes what constellations of body core, skin and ambient temperature satisfy the biophysical requirements of being in the thermoneutral zone for steady-state conditions. Furthermore, by constraining mean skin temperature to a temperature range associated with thermal comfort the thermal comfort zone is derived. The biophysical analysis shows that the steady-state ambient temperature range associated with the thermoneutral zone does not guarantee that the body is in thermal balance at basal metabolic rate per se. Instead, depending on the constellation of core temperature, mean skin temperature and ambient temperature, the body may require significant increases in heat production or heat loss to maintain stable core temperature. Therefore, the definition of the thermoneutral zone requires a revision to include core and skin temperature as well. Furthermore, after adding restrictions on skin temperature for thermal comfort, the ambient temperature range associated with thermal comfort is smaller than the thermoneutral zone. This, assuming animals seek thermal comfort, suggests that thermal behavior may be initiated already before the boundaries of the thermoneutral zone are reached.
Glossary
Abbreviations:
- BMR
basal metabolic rate
- PMV
predicted mean vote
- PPD
percentage people dissatisfied
- NST
category label indicating body heat deficit relative to basal metabolic rate cold induced thermogenesis by non-shivering is sufficient to maintain thermal balance
- SH+NST
category label indicating body heat deficit relative to basal metabolic rate cold induced thermogenesis by shivering and non-shivering is required to maintain thermal balance
- SWEAT
category label indicating a body heat surplus increased evaporation is required to maintain thermal balance
- TCZ
thermal comfort zone
- TNZ
thermoneutral zone
- TNZ body
category label indicating body heat loss is balanced relative to metabolic rate this definition of the thermoneutral zone incorporates the combination of mean skin temperature and ambient temperature
- TNZ classical
TNZ referring to the classic definition of the thermoneutral zone which only defines the ambient temperature range
- TNZ functional
TNZ referring to the classic definition of the thermoneutral zone taking into account clothing insulation and metabolic heat production associated with light office work
- a
ambient
- air
air
- body
referring to the human body
- c
body core
- cl
clothing
- clothed
clothed
- con
convective
- e
evaporative
- H&D
referring to Hardy & Dubois
- F
referring to Fanger
- max
maximal
- min
minimal
- r
radiative
- r+c
radiative + convective
- rsp
respiratory
- s
skin or mean skin
- α
fraction of metabolic heat production that is accounted for by respiratory heat loss
- A (m2)
body surface area
- ϕ
relative humidity
- Fpcl
permeation efficiency factor for water vapor evaporated from the skin surface through clothing to the ambient air
- γ (mmHg Pa-1)
conversion factor from Pascal to mmHg
- h (W m-2 °C-1)
heat transfer coefficient
- I (m2°CW-1)
insulation
- λ (°C mmHg-1)
Lewis relation
- M (W)
Metabolic rate
- P (mmHg)
saturated vapor pressure
- T (°C)
Temperature
- Q (W)
heat loss
- v (m s-1)
velocity
- w
skin wetness fraction
- ∆T (°C )
Indicating a temperature range
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest are disclosed
Acknowledgments
This work was supported by grants from AgentschapNL (INTEWON: EOSLT10033), TKI Energo and TKI Solar Energy (TEGB|13023).
Supplemental Materials
Supplemental Materials may be found here: www.landesbioscience.com/journals/temnperature/article/29702
References
- 1.IUPS TC. Glossary of terms for thermal physiology. Third edition. Revised by The Commission for Thermal Physiology of the International Union of Physiological Sciences (IUPS Thermal Commission). The Japanese Journal of Physiology 2001; 51:245-80. [PubMed] [Google Scholar]
- 2.Romanovsky AA. . Thermoregulation: some concepts have changed. Functional architecture of the thermoregulatory system. Am J Physiol Regul Integr Comp Physiol 2007; 292:R37 - 46; http://dx.doi.org/ 10.1152/ajpregu.00668.2006; PMID: 17008453 [DOI] [PubMed] [Google Scholar]
- 3.Schlader ZJ, Simmons SE, Stannard SR, Mündel T. . The independent roles of temperature and thermal perception in the control of human thermoregulatory behavior. Physiol Behav 2011; 103:217 - 24; http://dx.doi.org/ 10.1016/j.physbeh.2011.02.002; PMID: 21315099 [DOI] [PubMed] [Google Scholar]
- 4.ASHRAE. Thermal Environmental Conditions for Human Occupancy. ASHRAE standard 55-2004 2004. [Google Scholar]
- 5.Frank SM, Raja SN, Bulcao CF, Goldstein DS. . Relative contribution of core and cutaneous temperatures to thermal comfort and autonomic responses in humans. J Appl Physiol (1985) 1999; 86:1588 - 93; PMID: 10233122 [DOI] [PubMed] [Google Scholar]
- 6.Schlader ZJ. . The relative overlooking of human behavioral temperature regulation. Temperature 2014; 1:1 - 2; http://dx.doi.org/ 10.4161/temp.29235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burton AC, Edholm OG. Man in a cold environment. London: Edward Arnold (Publishers) LTD., 1955. [Google Scholar]
- 8.Veicsteinas A, Ferretti G, Rennie DW. . Superficial shell insulation in resting and exercising men in cold water. J Appl Physiol Respir Environ Exerc Physiol 1982; 52:1557 - 64; PMID: 7107465 [DOI] [PubMed] [Google Scholar]
- 9.Ducharme MB, Tikuisis P. . In vivo thermal conductivity of the human forearm tissues. J Appl Physiol (1985) 1991; 70:2682 - 90; PMID: 1885465 [DOI] [PubMed] [Google Scholar]
- 10.Fiala D, Lomas KJ, Stohrer M. . A computer model of human thermoregulation for a wide range of environmental conditions: the passive system. J Appl Physiol (1985) 1999; 87:1957 - 72; PMID: 10562642 [DOI] [PubMed] [Google Scholar]
- 11.Harris JA, Benedict FG. . A Biometric Study of Human Basal Metabolism. Proc Natl Acad Sci U S A 1918; 4:370 - 3; http://dx.doi.org/ 10.1073/pnas.4.12.370; PMID: 16576330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Degroot DW, Kenney WL. . Impaired defense of core temperature in aged humans during mild cold stress. Am J Physiol Regul Integr Comp Physiol 2007; 292:R103 - 8; http://dx.doi.org/ 10.1152/ajpregu.00074.2006; PMID: 17197640 [DOI] [PubMed] [Google Scholar]
- 13.van Ooijen AM, van Marken Lichtenbelt WD, van Steenhoven AA, Westerterp KR. . Cold-induced heat production preceding shivering. Br J Nutr 2005; 93:387 - 91; http://dx.doi.org/ 10.1079/BJN20041362; PMID: 15877879 [DOI] [PubMed] [Google Scholar]
- 14.Tikuisis P. . Predicting survival time for cold exposure. Int J Biometeorol 1995; 39:94 - 102; http://dx.doi.org/ 10.1007/BF01212587; PMID: 8530210 [DOI] [PubMed] [Google Scholar]
- 15.Gagge AP, Stolwijk JA, Hardy JD. . Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res 1967; 1:1 - 20; http://dx.doi.org/ 10.1016/0013-9351(67)90002-3; PMID: 5614624 [DOI] [PubMed] [Google Scholar]
- 16.Weiwei L, Zhiwei L, Qihong D. . Use of mean skin temperature in evaluation of individual thermal comfort for a person in a sleeping posture under steady thermal environment. Indoor Built Environ 2014; 0:1 - 11 [Google Scholar]
- 17.Johnson JM, Brengelmann GL, Hales JR, Vanhoutte PM, Wenger CB. . Regulation of the cutaneous circulation. Fed Proc 1986; 45:2841 - 50; PMID: 3780992 [PubMed] [Google Scholar]
- 18.Romanovsky AA, Ivanov AI, Shimansky YP. . Selected contribution: ambient temperature for experiments in rats: a new method for determining the zone of thermal neutrality. J Appl Physiol (1985) 2002; 92:2667 - 79; PMID: 12015388 [DOI] [PubMed] [Google Scholar]
- 19.Hardy JD, Dubois EF. . Regulation of Heat Loss from the Human Body. Proc Natl Acad Sci U S A 1937; 23:624 - 31; http://dx.doi.org/ 10.1073/pnas.23.12.624; PMID: 16577831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Speakman JR, Keijer J. . Not so hot: Optimal housing temperatures for mice to mimic the thermal environment of humans. Mol Metab 2012; 2:5 - 9; http://dx.doi.org/ 10.1016/j.molmet.2012.10.002; PMID: 24024125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang H, Arens E, Huizenga C, Han T. . Thermal sensation and comfort models for non-uniform and transient environments, part III: Whole-body sensation and comfort. Build Environ 2010; 45:399 - 410; http://dx.doi.org/ 10.1016/j.buildenv.2009.06.020 [DOI] [Google Scholar]
- 22.Schellen L, Loomans MG, de Wit MH, Olesen BW, van Marken Lichtenbelt WD. . The influence of local effects on thermal sensation under non-uniform environmental conditions--gender differences in thermophysiology, thermal comfort and productivity during convective and radiant cooling. Physiol Behav 2012; 107:252 - 61; http://dx.doi.org/ 10.1016/j.physbeh.2012.07.008; PMID: 22877870 [DOI] [PubMed] [Google Scholar]
- 23.Attia M. . Thermal pleasantness and temperature regulation in man. Neurosci Biobehav Rev 1984; 8:335 - 42; http://dx.doi.org/ 10.1016/0149-7634(84)90056-3; PMID: 6504416 [DOI] [PubMed] [Google Scholar]
- 24.van der Lans AA, Hoeks J, Brans B, Vijgen GH, Visser MG, Vosselman MJ, Hansen J, Jörgensen JA, Wu J, Mottaghy FM, et al. . Cold acclimation recruits human brown fat and increases nonshivering thermogenesis. J Clin Invest 2013; 123:3395 - 403; http://dx.doi.org/ 10.1172/JCI68993; PMID: 23867626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lichtenbelt W, Kingma B, van der Lans A, Schellen L. . Cold exposure–an approach to increasing energy expenditure in humans. . Trends Endocrinol Metab . 2014; 25:165 - 7; http://dx.doi.org/ 10.1016/j.tem.2014.01.001; PMID: 24462079 [DOI] [PubMed] [Google Scholar]
- 26.Fanger PO. . Assessment of man’s thermal comfort in practice. Br J Ind Med 1973; 30:313 - 24; PMID: 4584998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.González-Alonso J, Crandall CG, Johnson JM. . The cardiovascular challenge of exercising in the heat. J Physiol 2008; 586:45 - 53; http://dx.doi.org/ 10.1113/jphysiol.2007.142158; PMID: 17855754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gagge AP. . Rational temperature indices of man’s thermal environment and their use with a 2-node model of his temperature regulation. Fed Proc 1973; 32:1572 - 82; PMID: 4705203 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.