Abstract
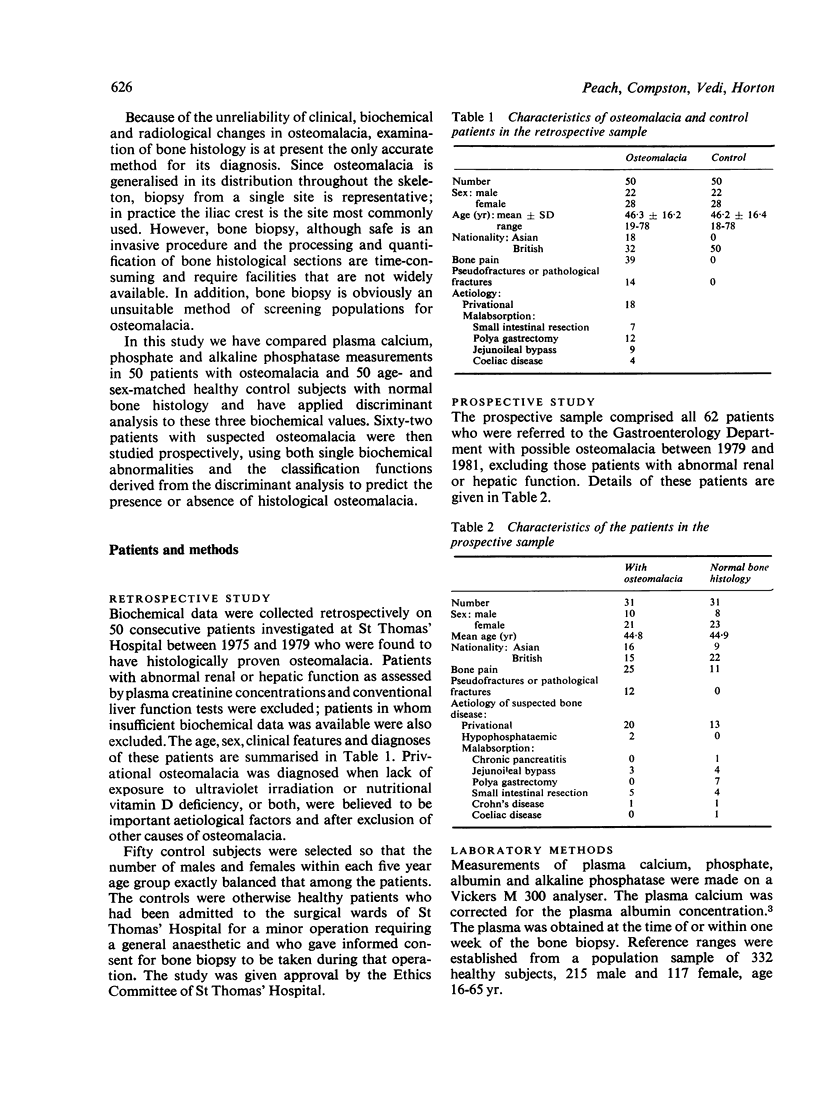
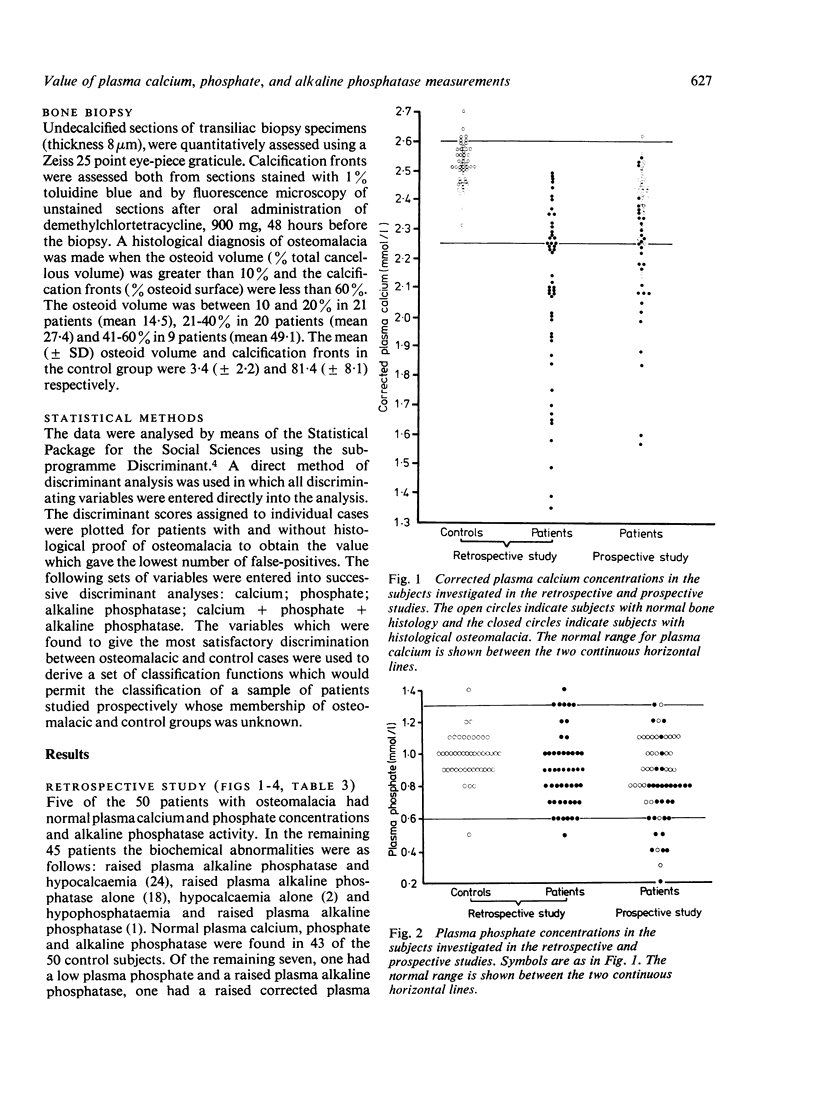
Plasma calcium and phosphate concentrations and alkaline phosphatase activities were examined retrospectively in 50 patients with histologically proven osteomalacia and 50 age- and sex-matched control subjects with normal bone histology. An abnormal plasma alkaline phosphatase activity was more useful than an abnormal plasma calcium or phosphate concentration in distinguishing between normal and osteomalacic subjects, producing a false-negative rate of 14% and a false-positive rate of 8%. False-negative and false-positive rates of 10% and 8% respectively were obtained when the presence of an abnormality in any one of the three biochemical measurements was used as a predictor of histological osteomalacia. When discriminant analysis was applied to plasma calcium, phosphate and alkaline phosphatase together a false-negative rate of 12% and a false-positive rate of 0% was obtained.
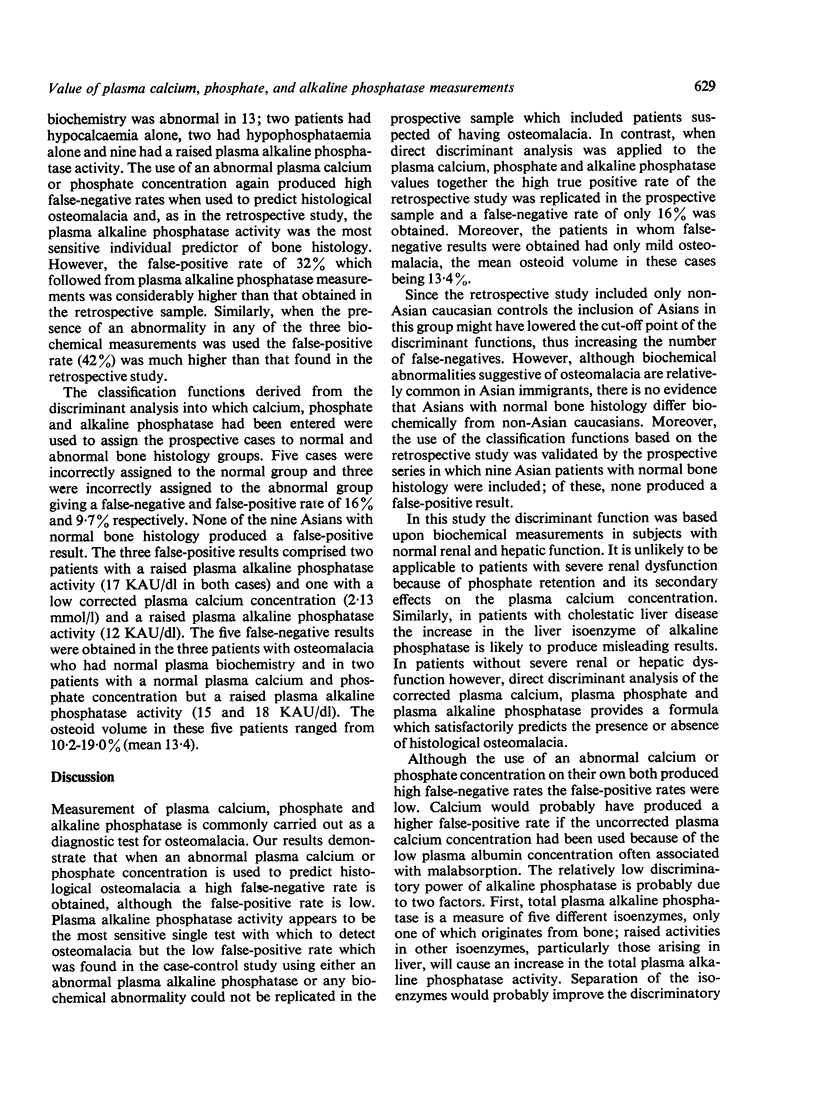
Sixty-two patients in whom a diagnosis of osteomalacia was suspected were investigated prospectively, using both single biochemical abnormalities and the classification functions derived from the discriminant analysis of all three biochemical measurements to predict the presence or absence of histological osteomalacia. Plasma alkaline phosphatase activity gave false-negative and false-positive rates of 10% and 32% respectively but was a more reliable predictor of abnormal bone histology than were plasma calcium or plasma phosphate concentrations or the presence of an abnormality in any one of the three measurements. Discriminant analysis using plasma calcium, phosphate and alkaline phosphatase together produced a false-negative rate of 16% and a false-positive rate of 10%.
We conclude that plasma alkaline phosphatase activity is the best single routine biochemical screening test for osteomalacia, although a high false-positive rate may occur. Direct discriminant analysis of plasma calcium, phosphate and alkaline phosphatase together provides a more sensitive method of detecting histological osteomalacia which should be useful in determining the prevalence of osteomalacia within high-risk populations.
Full text
PDF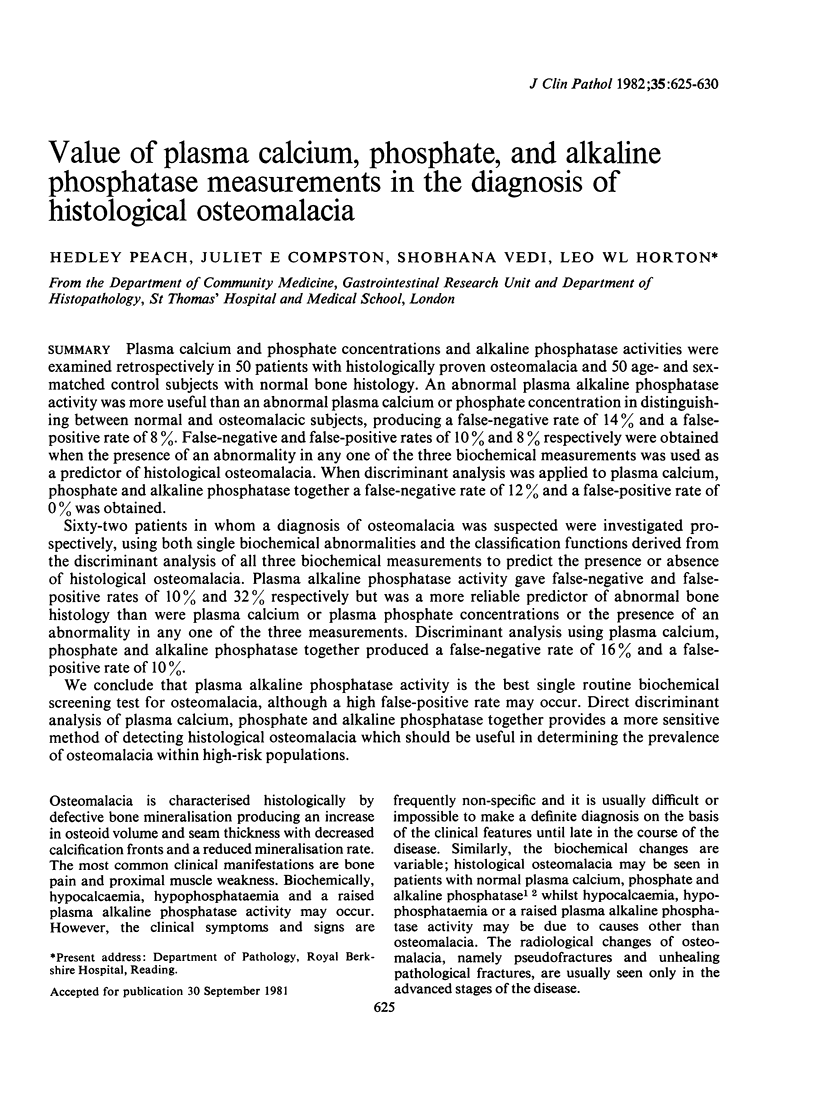


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chalmers J., Conacher W. D., Gardner D. L., Scott P. J. Osteomalacia--a common disease in elderly women. J Bone Joint Surg Br. 1967 Aug;49(3):403–423. [PubMed] [Google Scholar]
- Compston J. E., Horton L. W., Laker M. F., Ayers A. B., Woodhead J. S., Bull H. J., Gazet J. C., Pilkington T. R. Bone disease after jejuno-ileal bypass for obesity. Lancet. 1978 Jul 1;2(8079):1–4. doi: 10.1016/s0140-6736(78)91318-1. [DOI] [PubMed] [Google Scholar]
- Ellis G., Woodhead J. S., Cooke W. T. Serum-25-hydroxyvitamin-D concentrations in adolescent boys. Lancet. 1977 Apr 16;1(8016):825–828. doi: 10.1016/s0140-6736(77)92776-3. [DOI] [PubMed] [Google Scholar]
- Exton-Smith A. N., Hodkinson H. M., Stanton B. R. Nutrition and metabolic bone disease in old age. Lancet. 1966 Nov 5;2(7471):999–1001. doi: 10.1016/s0140-6736(66)92927-8. [DOI] [PubMed] [Google Scholar]
- Goel K. M., Sweet E. M., Logan R. W., Warren J. M., Arneil G. C., Shanks R. A. Florid and subclinical rickets among immigrant children in Glasgow. Lancet. 1976 May 29;1(7970):1141–1145. doi: 10.1016/s0140-6736(76)91538-5. [DOI] [PubMed] [Google Scholar]
- Heckmatt J. Z., Peacock M., Davies A. E., McMurray J., Isherwood D. M. Plasma 25-hydroxyvitamin D in pregnant Asian women and their babies. Lancet. 1979 Sep 15;2(8142):546–548. doi: 10.1016/s0140-6736(79)91612-x. [DOI] [PubMed] [Google Scholar]
- Holmes AM ENOCH B. A., Taylor J. L., Jones M. E. Occult rickets and osteomalacia amongst the Asian immigrant population. Q J Med. 1973 Jan;42(165):125–149. [PubMed] [Google Scholar]
- Jenkins D. H., Roberts J. G., Webster D., Williams E. O. Osteomalacia in elderly patients with fracture of the femoral neck. A clinico-pathological study. J Bone Joint Surg Br. 1973 Aug;55(3):575–580. [PubMed] [Google Scholar]
- Payne R. B., Little A. J., Williams R. B., Milner J. R. Interpretation of serum calcium in patients with abnormal serum proteins. Br Med J. 1973 Dec 15;4(5893):643–646. doi: 10.1136/bmj.4.5893.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vir S. C., Love A. H. Nutritional status of institutionalized and noninstitutionalized aged in Belfast, Northern Ireland. Am J Clin Nutr. 1979 Sep;32(9):1934–1947. doi: 10.1093/ajcn/32.9.1934. [DOI] [PubMed] [Google Scholar]


