Abstract
Inequality in access to quality healthcare is a major health policy challenge in many low- and middle-income countries. This study aimed to identify the major sources of inequity in healthcare utilization using a population-based household survey from urban Nepal. A cross-sectional survey was conducted covering 9177 individuals residing in 1997 households in five municipalities of Kathmandu valley between 2011 and 2012. The concentration index was calculated and a decomposition method was used to measure inequality in healthcare utilization, along with a horizontal inequity index (HI) to estimate socioeconomic inequalities in healthcare utilization. Results showed a significant pro-rich distribution of general healthcare utilization in all service providers (Concentration Index: 0.062, P < 0.001; HI: 0.029, P < 0.05) and private service providers (Concentration Index: 0.070, P < 0.001; HI: 0.030, P < 0.05). The pro-rich distribution of probability in general healthcare utilization was attributable to inequalities in the level of household economic status (percentage contribution: 67.8%) and in the self-reported prevalence of non-communicable diseases such as hypertension (36.7%) and diabetes (14.4%). Despite the provision of free services by public healthcare providers, our analysis found no evidence of the poor making more use of public health services (Concentration Index: 0.041, P = 0.094). Interventions to reduce the household economic burden of major illnesses, coupled with improvement in the management of public health facilities, warrant further attention by policy-makers.
Keywords: : Health economics, health inequalities, health care utilization
Key Messages
This study examines the major sources of inequity in healthcare utilization using data from a cross-sectional survey from urban Nepal.
This study found a significant pro-rich distribution of healthcare use in private service providers.
The pro-rich distribution of healthcare use and treatment was due to inequalities in household economic status and in the self-reported prevalence of non-communicable diseases such as hypertension and diabetes.
Our analysis found no evidence of the poor making more use of public health services.
Introduction
Universal health coverage aims to ensure equitable use of healthcare services for thllose in need without the imposition of financial risk (World Health Organization 2005, 2010). Providing equal treatment for those who have the same needs for healthcare, regardless of their socioeconomic and cultural background (Culyer and Wagstaff 1993; Van Doorslaer et al. 2000), has become a shared goal among many policymakers who strive to improve health systems. In an attempt to ensure equitable access to healthcare services, governments have been raising their health expenditures – for instance, between 2000 and 2011, per person public spending on health increased by 93% globally and by 127% in low-income countries with adjustment of purchasing power parity (World Health Organization 2014).
In Nepal, per capita government spending on health has increased from 11 to 29 international dollars between 2000 and 2011 (World Health Organization 2014). Around 80% of government health spending is allocated to public service providers via input-based financing, by which public health facilities receive funding to cover their operational costs. As such, most free healthcare services are provided at health posts, primary healthcare centres and publicly-funded district hospitals (Torres et al. 2011).
Despite the large share of national health spending committed to the public sector, there is no evidence that the current health financing system allows equitable utilization of healthcare. Equity in health can only be attained if persons with the same level of healthcare needs receive equal treatment (Culyer and Wagstaff 1993). Therefore, it is important to assess equity in utilization rather than access to healthcare, since access simply denotes an opportunity to receive healthcare, while utilization means exercising the opportunity (Mooney 1983). In OECD countries, previous studies assessing equity in general healthcare utilization have consistently identified a pro-rich concentration in physician visits, even where government spending is intended to cover the majority of healthcare expenses (Van Doorslaer et al. 2000; Doorslaer et al. 2004; Bago d’Uva et al. 2009), and the same propensity has been reported from three developed countries in Asia (Lu et al. 2007). Reports from Africa have also shown persistent inequity in healthcare utilization (Bonfrer et al. 2014). Here, we examined the inequality and inequity in utilization of healthcare services under Nepal’s current health financing framework, using cross-sectional household survey data.
Methods
Study design and data
Data on healthcare utilization were collected in five municipalities (Kathmandu, Kirtipur, Lalitpur, Madhyapur-Thimi and Bhaktapur) in Kathmandu Valley between November 2011 and January 2012. Details of the study design and data collection method have been published elsewhere (Saito et al. 2014). In brief, a total of 2000 households were sampled by probability-based multistage random cluster sampling, a common sampling method in cross-sectional household surveys which ensures the representativeness of samples in the study area (Macro International Inc. 1996). The pre-tested and validated study questionnaire included information on household demographics, education, consumption and durable goods, and self-reported disease episodes; and for each illness episode, information on care-seeking behaviour, treatment costs and hospitalization costs. We recorded all health provider visits and all types of morbidities that occurred in the past 30 days prior to the interview. All the reported illnesses/symptoms were coded according to a list of disease codes developed based on previous studies (Ahmed et al. 2005; Ir et al. 2010) and a focus group discussion conducted with primary healthcare workers in Kathmandu. Disease codes contained both the diagnosis made by doctors, or the symptoms if the patient had not seen a certified healthcare provider. Interviewers cross validated a diagnosis with an outpatient card or hospital discharge report whenever these were available.
Variables
Table 1 shows the list of variables used in the analysis and the sample characteristics. Healthcare utilization was recorded as any visit to a public, private or traditional healthcare provider for outpatient and/or inpatient care in the 30 days prior to the interview. Private healthcare providers included both for-profit and NGO-based service providers (Hotchkiss et al. 2014), and traditional healthcare providers denoted ayurvedic, homeopathic and traditional healers.
Table 1.
Sample characteristics by type of health service provider used in the previous 30 days, Nepal, 2011–2012 (N = 9177 individuals)a
|
All individuals |
Public |
Private |
Traditionalb |
All providers |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| Total | 9177 | 100.0 | 655 | 6.9 | 1925 | 21.6 | 128 | 1.4 | 2436 | 27.1 |
| Need factors | ||||||||||
| Age | ||||||||||
| Age under 30 | 4786 | 54.9 | 166 | 29.9 | 719 | 39.2 | 29 | 22.3 | 863 | 37.8 |
| Age 30–59 | 3551 | 37.3 | 312 | 46.9 | 803 | 43.8 | 68 | 52.2 | 1046 | 44.1 |
| Age 60 and above | 840 | 7.8 | 177 | 23.2 | 403 | 17.0 | 31 | 25.5 | 527 | 18.2 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Sex | ||||||||||
| Male | 4617 | 51.0 | 320 | 49.8 | 885 | 46.2 | 58 | 44.1 | 1149 | 47.8 |
| Female | 4560 | 49.1 | 335 | 50.2 | 1040 | 53.8 | 70 | 55.9 | 1287 | 52.3 |
| P-value | 0.67 | <0.001 | <0.001 | 0.01 | ||||||
| Self-reported diseases/symptoms | ||||||||||
| Cold/cough/fever | 1131 | 12.8 | 115 | 19.0 | 792 | 41.1 | 24 | 20.8 | 887 | 36.6 |
| Peptic ulcer/gastritis | 291 | 3.6 | 65 | 10.3 | 176 | 9.6 | 35 | 32.3 | 228 | 9.9 |
| Arthritis | 245 | 2.9 | 71 | 8.7 | 159 | 8.7 | 30 | 22.4 | 205 | 8.4 |
| Asthma | 130 | 1.1 | 48 | 5.6 | 97 | 4.2 | 7 | 4.5 | 125 | 4.1 |
| Migraine/headache | 70 | 0.9 | 19 | 3.4 | 46 | 2.9 | 4 | 2.6 | 62 | 3.1 |
| Injury | 69 | 0.7 | 24 | 3.5 | 46 | 2.4 | 3 | 2.0 | 66 | 2.6 |
| Heart diseases | 71 | 0.6 | 39 | 4.8 | 50 | 2.0 | 0 | 0.0 | 70 | 2.2 |
| Eye problem | 40 | 0.3 | 21 | 2.9 | 20 | 0.7 | 2 | 2.0 | 36 | 1.1 |
| Hypertension (≥20 yrs) | 656 | 10.2 | 201 | 32.2 | 480 | 31.6 | 29 | 26.1 | 615 | 30.9 |
| Diabetes (≥20 yrs) | 248 | 3.6 | 81 | 13.3 | 185 | 11.1 | 14 | 11.2 | 237 | 11.2 |
| Non-need factors | ||||||||||
| Education level | ||||||||||
| Primary or lower | 3581 | 40.0 | 365 | 56.9 | 953 | 50.1 | 65 | 50.7 | 1232 | 50.9 |
| Secondary or higher | 5596 | 60.0 | 290 | 43.1 | 972 | 49.9 | 63 | 49.3 | 1204 | 49.1 |
| P-value | <0.001 | <0.001 | 0.008 | <0.001 | ||||||
| Marital status | ||||||||||
| Never-married | 3988 | 44.6 | 149 | 24.5 | 629 | 32.9 | 20 | 13.8 | 757 | 31.8 |
| Currently married | 4891 | 52.4 | 449 | 68.1 | 1150 | 59.6 | 99 | 82.3 | 1491 | 61.0 |
| Divorced/separated/widowed | 298 | 3.0 | 57 | 7.4 | 146 | 7.5 | 9 | 3.9 | 188 | 7.3 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Household economic status | ||||||||||
| Household consumption per capita in NRs. | 8862 (median) | |||||||||
Sample weights applied. A total of 1997 households out of 2000 sampled households responded to the interview (99.8% response rate).
aNote that there are individuals who used more than one health service provider and/or who had multiple morbidities.
bTraditional providers include ayuredic, homeopathic and traditional healers.
We grouped predictors of healthcare utilization into need factors, non-need factors and economic status. Need factors are biological determinants used as a proxy for healthcare needs, which include age, sex and morbidity (O’Donnell et al. 2008). We included the 10 most commonly-reported diseases/symptoms as morbidity variables. Non-need factors are socioeconomic-related predictors for healthcare utilization, which include the education level of the individual (primary or lower, secondary or above) (O’Donnell et al. 2008; Trani and Barbou-des-Courieres 2012) and marital status (never-married, currently married, divorced/separated/widowed). Economic status was derived from household consumption in the past 30 days, by aggregating consumption of purchased or home-produced goods (foods, non-foods, housing and durable goods) (O’Donnell et al. 2008), which was converted into the logarithm of adult-equivalent consumption (Deaton and Zaidi 2002). Adult-equivalent consumption was also used as the ranking variable for the wealth status of the individual.
Concentration index
We constructed a concentration curve to illustrate inequality in healthcare use by the type of provider used in the previous 30 days. A concentration curve lying below the line of equality means that healthcare utilization is concentrated more among the wealthier (O’Donnell et al. 2008). To calibrate the degree and statistical significance of inequality, we used a concentration index that denotes differences in healthcare utilization across wealth status (O’Donnell et al. 2008). In this study, is the concentration index for actual utilization of healthcare utilization with ranges lying between −1 and 1. The concentration index is calculated using the covariance between the healthcare utilization and the fractional rank of the individual sorted by wealth status:
| (1) |
where is the binary variable of whether the ith person had used public, provider, traditional or all types of providers in the previous 30 days, stands for the mean of actual healthcare utilization, denotes the fractional rank of the ith individual by wealth status, and is the covariance with sampling probability weights (Kakwani et al. 1997; Doorslaer et al. 2004). The 95% confidence intervals for the concentration index and the associated P-values were obtained by the delta method (Kakwani et al. 1997; Koolman and Van Doorslaer 2004; Rao 2009). If the concentration index is significantly smaller than 0, poor individuals are more likely to use healthcare, while a larger than 0 indicates that utilization is biased towards wealthier individuals (Kakwani et al. 1997; Van Doorslaer and Masseria 2004)
Decomposition of inequality
We conducted a decomposition analysis to assess the extent to which each of needs, non-needs and consumption factors contributes to the inequality in healthcare utilization. We used the linear approximation of a probit model with the partial effects evaluated at means (Doorslaer et al. 2004), which is expressed as:
| (2) |
where i denotes the ith individual, refers to the jth need factor of the ith individual, is the kth non-need and consumption factor, and is the intercept; and are the marginal effects, dy/d and dy/d, of each need (x) and non-need/consumption (z) factor evaluated at sample means; and is the error term, which includes approximation errors (Doorslaer et al. 2004). Plugging in the estimated coefficients from Equation (2), the concentration index for y can thus be expressed as:
| (3) |
where is the mean of y; and are the concentration index of and , respectively, and calculated similarly to Equation (1); and is the generalized concentration index of the error term (Doorslaer et al. 2004; O’Donnell et al. 2008). The products ( and are the contribution of a need factor j and a non-need and consumption factor k to the actual concentration index, respectively. A concentration index was estimated for each of the factors, along with absolute and percentage contributions to the inequality in actual healthcare utilization (CM). A positive (negative) contribution indicates that the given variable operates towards pro-rich (pro-poor) distribution of healthcare visits.
Horizontal inequity
To measure the inequity in healthcare utilization, we estimated the horizontal inequity index (HI), which denotes socioeconomic differences in healthcare utilization with control for the effects of biological needs (Van Doorslaer et al. 2000). Subtracting the absolute contributions made by need factors from the concentration index for actual healthcare utilization ( yields the HI (O’Donnell et al. 2008). The HI ranges between −2 and 2, with a significantly positive (negative) HI standing for pro-rich (pro-poor) inequity (Van Doorslaer et al. 2000). We obtained P-values for the HI using a probit model which standardized the need factors (Wagstaff and Van Doorslaer 2000). Stata version 12.1 (StataCorp, College Station, TX) was used for all analyses.
Results
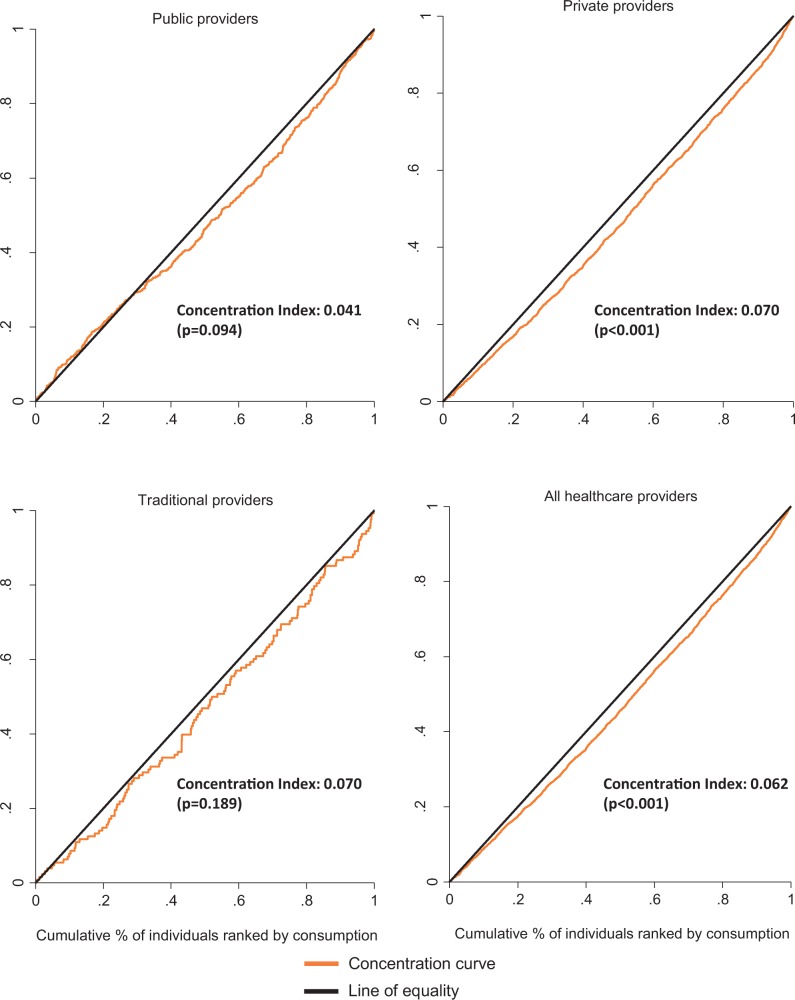
Table 1 shows the characteristics of individuals in the sampled households. In total, 1997 households responded to the interview (99.8% response rate). Overall, private service providers were used more frequently (21.6%) than public (6.9%) and traditional providers (1.4%) irrespective of the individual’s background characteristics. Figure 1 plots the concentration curves for probability of healthcare utilization by type of provider in the previous 30 days. A significant pro-rich distribution of healthcare utilization was observed for all providers (Concentration index: 0.062, P < 0.001) and for private service providers (Concentration index: 0.070, P < 0.001).
Figure 1.
Concentration curves for probability of healthcare use by type of providers, Nepal, 2011-2012.
Figure 2 depicts the inequality in healthcare utilization decomposed by need, non-need, consumption factors and a residual term. Need factors and household economic status accounted for the pro-rich concentration of healthcare utilization in both public and private providers, while non-need factors operated to reduce the pro-rich concentration in the utilization of both public and private providers.
Figure 2.
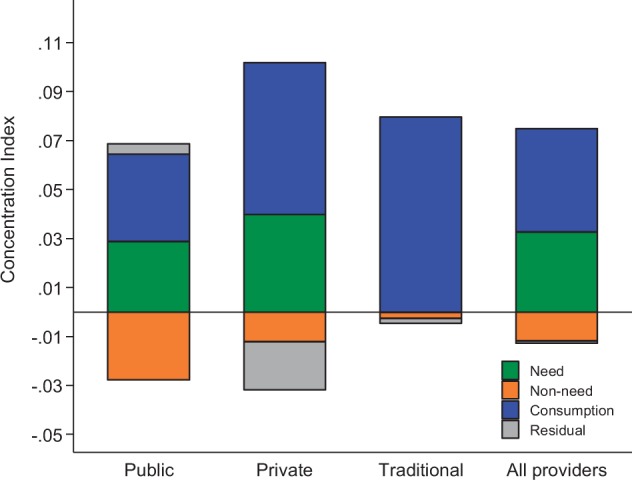
Contributions of need, non-need and consumption factors to concentration index for probability of healthcare use, by types of healthcare providers used, Nepal, 2011–2012.
Table 2 shows detailed contribution of need, non-need and consumption factors to inequality in healthcare utilization probability. Household economic status was by far the most influential factor for pro-rich utilization in all providers (67.8%), public providers (88.0%), private providers (88.5%) and traditional providers (116.4%). Self-reports of illnesses, including hypertension and diabetes, showed strong contributions in favour of the rich across all types of service provider, which cancelled out the pro-poor distribution in self-reports of other illnesses. In contrast, being educated to the secondary level or higher contributed to pro-poor healthcare utilization, which was most pronounced in public service utilization (−68.3%). Horizontal inequity—after deducting the inequality induced by need factors—was significantly pro-rich in the utilization of private (0.030, P < 0.001) and all service providers (0.029, P < 0.001).
Table 2.
Detailed contributions to inequality in probability of healthcare utilization by need, non-need and consumption factors, Nepal, 2011–2012
| Public | Private | Traditional | All providers | |||||
|---|---|---|---|---|---|---|---|---|
| Contributions to CM | Percentage contributions | Contributions to CM | Percentage contributions | Contributions to CM | Percentage contributions | Contributions to CM | Percentage contributions | |
| CI for actual healthcare use (CM) | 0.041 | 100.0 | 0.070 | 100.0 | 0.070 | 100.0 | 0.062 | 100.0 |
| Horizontal Inequity (HI) index | 0.012 | 0.030 | 0.071 | 0.029 | ||||
| Residual | 0.004 | 10.2 | −0.020 | −28.0 | −0.002 | −2.9 | −0.001 | −1.4 |
| Need factors | ||||||||
| Age | ||||||||
| Under 30 years | Ref. | |||||||
| 30–59 years | 0.003 | 8.5 | 0.003 | 4.8 | 0.003 | 3.8 | 0.003 | 4.3 |
| 60 and above | 0.001 | 3.4 | 0.000 | 0.6 | 0.002 | 2.7 | 0.001 | 1.6 |
| Sex | ||||||||
| Male | Ref. | |||||||
| Female | 0.000 | −0.6 | 0.000 | 0.2 | 0.000 | 0.0 | 0.000 | 0.0 |
| Self-reported disease | ||||||||
| Hypertension | 0.017 | 42.7 | 0.028 | 40.1 | 0.006 | 8.1 | 0.023 | 36.7 |
| Diabetes | 0.009 | 22.7 | 0.012 | 16.5 | 0.006 | 8.4 | 0.009 | 14.4 |
| Heart diseases | 0.003 | 7.2 | 0.001 | 1.5 | n.a. | n.a. | 0.001 | 1.7 |
| Cold/cough/fever | 0.001 | 3.3 | 0.004 | 6.3 | 0.001 | 1.9 | 0.003 | 5.4 |
| Injury | 0.000 | 1.0 | 0.000 | 0.5 | 0.000 | 0.0 | 0.000 | 0.5 |
| Eye problem | 0.000 | −0.8 | 0.000 | −0.1 | 0.000 | −0.2 | 0.000 | −0.2 |
| Asthma | 0.000 | −0.8 | 0.000 | −0.5 | 0.000 | −0.2 | 0.000 | −0.5 |
| Peptic ulcer/gastritis | −0.003 | −8.1 | −0.005 | −6.6 | −0.014 | −19.8 | −0.004 | −6.0 |
| Arthritis | −0.001 | −2.7 | −0.002 | −3.5 | −0.004 | −5.9 | −0.002 | −2.7 |
| Migraine/headache | −0.002 | −4.9 | −0.002 | −2.9 | −0.001 | −0.8 | −0.002 | −2.9 |
| Non-need factors | ||||||||
| Education level | ||||||||
| Primary or lower | Ref. | |||||||
| Secondary or higher | −0.028 | −68.3 | −0.012 | −16.9 | −0.008 | −12.1 | −0.012 | −19.0 |
| Marital status | ||||||||
| Never-married | Ref. | |||||||
| Currently married | 0.000 | −0.3 | 0.000 | 0.0 | 0.000 | −0.3 | 0.000 | 0.0 |
| Divorced/separated/widowed | 0.000 | 0.4 | 0.000 | −0.5 | 0.001 | 0.9 | 0.000 | −0.2 |
| Household consumption (log of consumption per capita) | 0.036 | 88.0 | 0.062 | 88.5 | 0.081 | 116.4 | 0.042 | 67.8 |
Decomposition based on probit model results. Sample weights applied. Statistically significant CM and HI are in bold type (P < 0.05).
Discussion
This study found a pro-rich concentration of private healthcare utilization in urban Nepal. Our results are consistent with previous studies on general healthcare utilization in Hong Kong, China (Leung et al. 2009; Elwell-Sutton et al. 2013), and on the provision of institutional deliveries at private facilities in Bangladesh and Nepal (Hotchkiss et al. 2014). Decomposition of need and non-need factors in previous studies has consistently shown that need factors such as age, sex and self-reported health status operate in a pro-poor direction (Doorslaer et al. 2004; Elwell-Sutton et al. 2013; Bonfrer et al. 2014). However, our analyses showed that self-reports of diabetes or hypertension, which are need factors, operate largely towards a pro-rich distribution of healthcare utilization, while the effects of other self-reported illnesses/symptoms were either pro-poor or only marginally pro-rich. This may be because the self-reported prevalence of diabetes and hypertension are concentrated in wealthier individuals in the case of urban Nepal, although we cannot exclude the possibility of undiagnosed cases (Saito et al. 2014). Among the non-need factors, having secondary or higher education has a pro-poor effect on healthcare utilization in our study. This contradicts the findings of some previous studies which found that higher education makes a pro-rich contribution to healthcare utilization (Liu et al. 2002; Van Doorslaer and Masseria 2004). However, our results are consistent with those from other low-income settings, such as Anglophone countries in Africa (Bonfrer et al. 2014). The role of secondary or higher education in pro-poor utilization might be that people with education may be able to identify, make decisions about and use affordable healthcare services (Navaneetham and Dharmalingam 2002).
Similar to previous reports, our results showed that household consumption makes by far the greatest pro-rich contribution in healthcare utilization (Doorslaer et al. 2004; Lu et al. 2007; Bago d’Uva et al. 2009; Leung et al. 2009; Elwell-Sutton et al. 2013; Bonfrer et al. 2014). Such an income gradient is plausible for utilization of the private sector, as private providers operate on a fee-for-service basis in Nepal, and patients need to bear the full cost of treatment (Saito et al. 2014). Unexpectedly, our analysis found no evidence that the poor made more use of public health services, and showed that they had even less probability of healthcare utilization after adjusting for inequality in need factors, despite the provision of free consultation services at public facilities. This contradicts with findings in Hong Kong, where public services are used predominantly by the less well-off, and Hong Kong also maintains tax-based health financing to cover public services (Leung et al. 2009). Past studies have found dissatisfaction with factors such as long waiting times, drug shortages and medical equipment reduce the utilization rates (Basu et al. 2012). Improving the management of public service providers may encourage the utilization of public facilities amongst the poorest, and provide a relatively low-cost mechanism for providing financial protection for some illnesses.
One important reason for the underutilization of public facilities can be a heavy burden of out-of-pocket payments. First issue is limited coverage of financial protection. In Nepal’s case, public health services are financed from general government revenues, and healthcare is delivered by salaried doctors and staff (Deutsche Gesellschaft fur Internationale Zusammenarbeit (GIZ) GmbH and Ministry of Health and Population 2010). Although the Government of Nepal endorsed a National Health Insurance policy in 2013 which aimed at universal coverage of health services and financial protection (Central Bureau of Statistics and The United Nations Children’s Fund 2011), this scheme has not been implemented to date, and the coverage of financial protection remains sporadic given the country’s limited fiscal space (Belay and Tandon 2011). Notwithstanding the availability of some subsidiary schemes, inconsistency exists between healthcare needs and the patient’s ability to pay. Although free essential drugs are provided at public health facilities, other medicines for treatment of non-communicable diseases and medical examinations are paid for by patients in the current health financing framework (Ministry of Health and Population 2009; Torres et al. 2011). To ensure equitable access to necessary treatment, the majority of the population would benefit from alternative financing, such as starting from a small-scale health insurance programme covering major non-communicable diseases, with the central government consolidating the risk-pooling across insurances groups, to incrementally broaden its coverage (World Health Organization 2010; Spaan et al. 2012). For instance, urban health insurance reform in China significantly improved equity in the utilization of outpatient care services between 1994 and 1996 (Liu et al. 2002).
This study has several limitations. First, data collection was conducted between November 2011 and January 2012, which was the winter season. Change in the prevalence of infectious diseases such as common cold or diarrhoea might have altered healthcare needs. For instance, diarrhoea occurs primarily in the rainy season (Strand et al. 2012). However, the Nepal Living Standard Survey 2010/2011, which took place in four different seasons, confirmed that cold/cough/fever was the most prevalent disease throughout the year (Central Bureau of Statistics 2011). Chronic illnesses showed consistent prevalence when we validated the history of illness in the past 30 days and past 12 months.
Second, the study is based on self-reported illnesses. Healthcare needs for non-communicable diseases are better estimated by physical measurements and blood tests, but logistical constraints of the study allowed only the face-to-face interviews. For this reason, there might have been potential health needs that were not calibrated in our study. Despite the limitations, this is the first study in low-income settings to assess inequalities in healthcare utilization with validated disease types from a population-based household survey with a high response rate, following an established method that is commonly used in other cross-sectional surveys with a reliable sampling frame built from the latest census data.
Conclusion
This study observed a pro-rich distribution of healthcare utilization in all providers and private service providers. Socioeconomic inequity in healthcare visits widened for private provider visits. The pro-rich distribution of healthcare utilization was largely attributable to household economic status and self-reports of diabetes or hypertension, which outweighed the pro-poor contribution of other need and non-need factors. Our analysis found no evidence of the poor making more use of public health services, and even less so after adjusting for inequality in need factors. Financial barriers due to high out-of-pocket payments may explain the limited access to both private and public facilities. Interventions to reduce the household economic burden of major illnesses, coupled with improvements in the management of public health facilities, warrant further attention by policymakers.
Ethical approval
Ethical approval for the survey was obtained from the Research Ethics Committee of the University of Tokyo (approval number 3447) and from the Nepal Health Research Council (NHRC registration number 49/2011) in August 2011. Survey respondents received a full explanation of the content of the study, as well as the risks, benefits, freedom to participate and confidentiality before signing the informed consent sheet for the interview.
Acknowledgements
We thank SOLID Nepal staff for their contributions in field data collection; and Khem Bahadur Karki, Arjun Subedi and Franziska Fuerst for their contributions during the various phases of this project.
Funding
This research was funded in part by the Japan Society for the Promotion of Science and the Japanese Ministry of Health, Labour and Welfare – via grants 22390130, 25253051, 24030401 and 25253051.
Conflict of interest statement. None declared.
References
- Ahmed SM, Tomson G, Petzold M, Kabir ZN. 2005. Socioeconomic status overrides age and gender in determining health-seeking behaviour in rural Bangladesh. Bulletin of the World Health Organization 83: 109–117. [PMC free article] [PubMed] [Google Scholar]
- Bago d’Uva T, Jones AM, Van Doorslaer E. 2009. Measurement of horizontal inequity in health care utilisation using European panel data. Journal of Health Economics 28: 280–289. [DOI] [PubMed] [Google Scholar]
- Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D. 2012. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Medicine 9: e1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belay T, Tandon A. 2011. Assessing fiscal space for health in Nepal. Heath, nutrition and population discussion paper. Washington, DC: World Bank; http://documents.worldbank.org/curated/en/2011/07/16240700/assessing-fiscal-space-health-nepal, accessed 25 July 2012. [Google Scholar]
- Bonfrer I, Van De Poel E, Grimm M, Van Doorslaer E. 2014. Does the distribution of healthcare utilization match needs in Africa? Health Policy and Planning 29: 921–937. [DOI] [PubMed] [Google Scholar]
- Central Bureau of Statistics & the United Nations Children's Fund 2011. Findings from the Multiple Indicator Cluster Survey 2010 in the Mid-and Far-Western Regions, Kathmandu: Central Bureau of Statistics, National Planning Commission Secretariat, Government of Nepal. [Google Scholar]
- Central Bureau of Statistics, N. P. C. S., Government of Nepal 2011. Nepal living standards survey 2010/2011. Kathmandu: Central Bureau of Statistics, National Planning Commission Secretariat, Goverment of Nepal. [Google Scholar]
- Culyer AJ, Wagstaff A. 1993. Equity and equality in health and health care. Journal of Health Economics 12: 431–457. [DOI] [PubMed] [Google Scholar]
- Deaton A, Zaidi S. 2002. Guidelines for Constructing Consumption Aggregates for Welfare Analysis. Washington, DC: World Bank. [Google Scholar]
- Deutsche Gesellschaft fur Internationale Zusammenarbeit (GIZ) GMBH & Ministry of Health and Population 2010. Nepal at the Crossroards: Setting the Stage for Improved Social Health Protection. Kathmandu: Deutsche Gesellschaft fur Internationale Zusammenarbeit (GIZ) GmbH. [Google Scholar]
- Doorslaer EV, Koolman X, Jones AM. 2004. Explaining income-related inequalities in doctor utilisation in Europe. Health Economics 13: 629–647. [DOI] [PubMed] [Google Scholar]
- Elwell-Sutton TM, Jiang CQ, Zhang WS, et al. 2013. Inequality and inequity in access to health care and treatment for chronic conditions in China: the Guangzhou Biobank Cohort Study. Health Policy and Planning 28: 467–479. [DOI] [PubMed] [Google Scholar]
- Hotchkiss DR, Godha D, Do M. 2014. Expansion in the private sector provision of institutional delivery services and horizontal equity: evidence from Nepal and Bangladesh. Health Policy Planning 29(Suppl 1): i12–i19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ir P, Men C, Lucas H, Meessen B, Decoster K, Bloom G, Van Damme W. 2010. Self-reported serious illnesses in rural Cambodia: a cross-sectional survey. Plos One 5: e10930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakwani N, Wagstaff A, Van Doorslaer E. 1997. Socioeconomic inequalities in health: measurement, computation, and statistical inference. Journal of Econometrics 77: 87–103. [Google Scholar]
- Koolman X, Van Doorslaer E. 2004. On the interpretation of a concentration index of inequality. Health Economics 13: 649–656. [DOI] [PubMed] [Google Scholar]
- Leung GM, Tin KY, O’Donnell O. 2009. Redistribution or horizontal equity in Hong Kong's mixed public–private health system: a policy conundrum. Health Economics 18: 37–54. [DOI] [PubMed] [Google Scholar]
- Liu GG, Zhao Z, Cai R., Yamada T, Yamada T. 2002. Equity in health care access to: assessing the urban health insurance reform in China. Social Science & Medicine 55: 1779–1794. [DOI] [PubMed] [Google Scholar]
- Lu JR, Leung GM, Kwon S, Tin KYK, Van Doorslaer E, O’Donnell O. 2007. Horizontal equity in health care utilization evidence from three high-income Asian economies. Social Science & Medicine 64: 199–212. [DOI] [PubMed] [Google Scholar]
- Macro International Inc. 1996. Sampling Manual. Calverton, MD: Macro International Inc. [Google Scholar]
- Ministry of Health and Population. 2009. National List of Essential Medicines Nepal [Online]. Kathmandu: http://www.unfpa.org/sowmy/resources/docs/library/R085_MOHNEPAL_2009_EssentialDrugs_Medicines.pdf, accessed 27 July 2012. [Google Scholar]
- Mooney GH. 1983. Equity in health care: confronting the confusion. Effective Health Care 1: 179–185. [PubMed] [Google Scholar]
- Navaneetham K, Dharmalingam A. 2002. Utilization of maternal health care services in Southern India. Social Science & Medicine 55: 1849–1869. [DOI] [PubMed] [Google Scholar]
- O’Donnell O, Van Doorsslaer E, Wagstaff A, Lindelow M. 2008. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation. World Bank Publications. [Google Scholar]
- Rao CR. 2009. Linear Statistical Inference and Its Applications, New York: Wiley. [Google Scholar]
- Saito E, Gilmour S, Rahman MM, Gautam GS, Shrestha PK, Shibuya K. 2014. Catastrophic household expenditure on health in Nepal: a cross-sectional survey. Bulletin World Health Organisation 92: 760–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaan E, Mathijssen J, Tromp N, McBain F, Ten Have A, Baltussen R. 2012. The impact of health insurance in Africa and Asia: a systematic review. Bulletin World Health Organisation 90: 685–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strand TA, Sharma PR, Gjessing HK, et al. 2012. Risk factors for extended duration of acute diarrhea in young children. Plos One 7: e36436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres LV, Gautam GS, Fuerst F, Adhikari CR. 2011. Assessment of the Government Health Financing System in Nepal: Suggestions for Reform. Kathmandu: Deutsche Gesellschaft fur Internationale Zusammenarbeit (GIZ) GmbH. [Google Scholar]
- Trani JF, Barbou-des-Courieres C. 2012. Measuring equity in disability and healthcare utilization in Afghanistan. Medicine, Conflict and Survival 28: 219–246. [DOI] [PubMed] [Google Scholar]
- Van Doorslaer E, Masseria C. 2004. Income-Related Inequality in the Use of Medical Care in 21 OECD Countries. OECD. [Google Scholar]
- Van Doorslaer E, Wagstaff A, Van Der Burg H, et al. 2000. Equity in the delivery of health care in Europe and the US. Journal of Health Economics 19: 553. [DOI] [PubMed] [Google Scholar]
- Wagstaff A, Van Doorslaer E. 2000. Measuring and testing for inequity in the delivery of health care. Journal of Human Resources 35: 716–733. [Google Scholar]
- World Health Organization 2005. Achieving Universal Health Coverage: Developing the Health Financing System. Technical Briefs for Policy-Makers Series No. 1. Geneva: World Health Organization. [Google Scholar]
- World Health Organization 2010. The World Health Report: Health Systems Financing: The Path to Universal Coverage . Geneva: World Health Organization. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. 2014. World Health Statistics 2014. (In IRIS). Geneva: World Health Organization. [Google Scholar]