Abstract
Children who begin but do not fully complete the recommended series of childhood vaccines by 2 y of age are a much larger group than those who receive no vaccines. While parents who refuse all vaccines typically express concern about vaccine safety, it is critical to determine what influences parents of ‘partially’ immunized children. This case-control study examined whether parental concern about vaccine safety was responsible for partial immunization, and whether other personal or system-level factors played an important role. A random sample of parents of partially and completely immunized 2 y old children were selected from a Canadian regional immunization registry and completed a postal survey assessing various personal and system-level factors. Unadjusted odds ratios (OR) and adjusted ORs (aOR) were calculated with logistic regression. While vaccine safety concern was associated with partial immunization (OR 7.338, 95% CI 4.138– 13.012), other variables were more strongly associated and reduced the strength of the relationship between concern and partial immunization in multivariable analysis (aOR 2.829, 95% CI 1.151 – 6.957). Other important factors included perceived disease susceptibility and severity (aOR 4.629, 95% CI 2.017 – 10.625), residential mobility (aOR 3.908, 95% CI 2.075 – 7.358), daycare use (aOR 0.310, 95% CI 0.144 - 0.671), number of needles administered at each visit (aOR 7.734, 95% CI 2.598 – 23.025) and access to a regular physician (aOR 0.219, 95% CI 0.057 – 0.846). While concern about vaccine safety may be addressed through educational strategies, this study suggests that additional program and policy-level strategies may positively impact immunization uptake.
Keywords: barriers, immunization, multivariable model, vaccination, vaccine safety, vaccine uptake
Abbreviations
- CI
Confidence interval
- OR
Unadjusted odds ratio
- aOR
Adjusted odds ratio
Introduction
Although children who receive no vaccines are a cause for concern, children who are only partially immunized by the age of 2 y are a larger and arguably more important group to understand. ‘Partially immunized’ children, who have received some but not all recommended vaccine doses, comprise the vast majority of children under/unprotected from vaccine-preventable disease. In Canada, where immunizations are not mandatory in most jurisdictions, it is estimated that 28–40% of children are partially immunized at 2 y of age, compared to less than 2% who have received no vaccines.1,2 Understanding what influences parents who only partially immunize their children is essential. While it is difficult to change the behavior of ‘committed refusers’, there is the potential to improve vaccine uptake among “children whose parents either are open to immunization but encounter barriers to obtaining vaccines or hesitate because of fears and concerns about safety." 3(p. 392) Understanding the role of vaccine safety concern and the influence of other factors (including systemic obstacles) in mediating such concern is critical in addressing the large number of partially immunized children,4 and in turn, promoting public health and population protection from vaccine-preventable diseases.
This study addressed this gap in knowledge by exploring the factors influencing parents whose children are partially immunized by 2 y of age (missing ≥1 vaccine dose, but not refusing all). We used a postal survey to examine whether concern about vaccine safety was the primary reason for failure to complete the vaccine series by 2 years, or if other attitudes and beliefs or personal and systemic factors were equally or more important.
Results
Response rate
Of the 1342 subjects in the sample (671 completely immunized children and 671 incompletely immunized children), 274 were ineligible due to invalid addresses, 18 withdrew from the study, 589 did not respond, and 461 questionnaires were completed and returned (see Fig. 1). The final response rate was 43% (461/1068); there was a statically significant difference (P < 0.001) in response rate between parents of completely immunized (51.7%, 331/640) and incompletely immunized children (30.4%, 130/428). The sample of incompletely immunized children included those who were partially immunized (n = 113) and those who had received no vaccines (n = 17); the latter group were excluded from this analysis. The partially immunized children represent a heterogeneous group who were missing any number of the 13 vaccines recommended before the age of 2 y.
Figure 1.
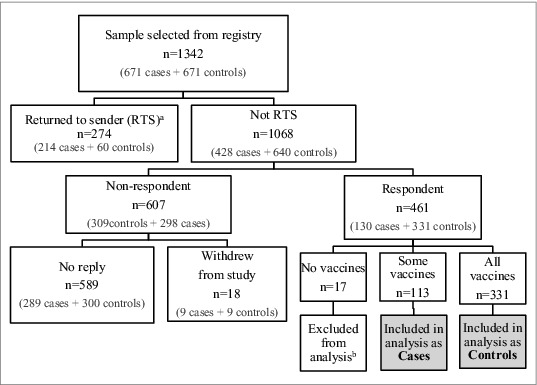
Sample selection.
a‘Returned to sender’ by the post office with no forwarding address.
bThe original sample included 17 children who had received no vaccines. These children were excluded from this analysis because (1) Children who receive no vaccines are a group distinct from those who start but do not complete immunizations4,14 and (2) Survey questions regarding experiences with immunization services were not applicable to this group.
Survey results
Table 1 presents the characteristics of respondents according to children's immunization status. There was no statistically significant difference between parents of children who were completely and partially immunized in regards to parents’ age, place of birth, marital status, level of education, Aboriginal status, or household income. Table 2 shows the unadjusted odds ratios (OR) for the associations between each exposure variable and the outcome variable (the child's immunization status). It also presents the adjusted ORs (aOR) from the multivariable logistic regression model that included all other variables in Table 2, as well as the covariates in Table 1. The aOR allows us to assess the independent association between each exposure and the outcome variable, after controlling for all other exposure variables in the model. This enables us to determine if the association between one exposure variable and the outcome variable is being altered by other exposure variables.
Table 1.
Characteristics of respondents according to child's immunization statusa
| Immunization Status b |
||
|---|---|---|
| Variable | Partially Immunized (N = 113)c | Completely Immunized (N = 331)c |
| Mother's age (mean in years) | 32.81 | 32.85 |
| Father's age (mean in years) | 34.75 | 35.16 |
| Mother's place of birth, % (n) | ||
| In Canada | 81.4% (92) | 80.1% (265) |
| Not in Canada | 16.8% (19) | 19.3% (64) |
| Father's place of birth, % (n) | ||
| In Canada | 75.2% (85) | 80.1% (265) |
| Not in Canada | 22.1% (25) | 19.0% (63) |
| Mother's level of education, % (n) | ||
| Less than high school diploma | 6.2% (7) | 4.5% (15) |
| High school graduate | 11.5% (13) | 12.4% (41) |
| Some college/university | 17.7% (20) | 14.5% (48) |
| College or Trade certificate/diploma | 20.4% (23) | 26.6% (88) |
| University undergraduate degree | 30.1% (34) | 30.2% (100) |
| Graduate/Post-graduate degree | 12.4% (14) | 10.6% (35) |
| Father's level of education, % (n) | ||
| Less than high school diploma | 4.4% (5) | 6.6% (22) |
| High school graduate | 12.4% (14) | 13.6% (45) |
| Some college/university | 10.6% (12) | 9.1% (30) |
| College or Trade certificate/diploma | 28.3% (32) | 39.3% (130) |
| University undergraduate degree | 19.5% (22) | 16.9% (56) |
| Graduate/Post-graduate degree | 20.4% (23) | 11.8% (39) |
| Primary caregiver Aboriginal, % (n) | ||
| No | 92.9% (105) | 93.1% (308) |
| Yes | 4.4% (5) | 3.0% (10) |
| Primary caregiver a single parentd, % (n) | ||
| No | 87.6% (99) | 91.8% (303) |
| Yes | 12.4% (14) | 8.2% (27) |
| Household income, % (n) | ||
| Less than $40,000 | 9.7% (11) | 7.5% (25) |
| $40,000–59,999 | 9.7% (11) | 10.3% (34) |
| $60,000–79,999 | 10.6% (12) | 14.8% (49) |
| $80,000–99,000 | 15.9% (18) | 16.9% (56) |
| $100,000–119,999 | 12.4% (14) | 14.8% (49) |
| $120,000–139,999 | 6.2% (7) | 9.4% (31) |
| More than $140,000 | 19.5% (22) | 13.3% (44) |
aChildren with no vaccines (N = 17) were excluded from this analysis.
bThere were no statistically significant differences between the groups for any of the variables.
cFrequencies may not add up to total due to item non-response.
dSelf-identified single status, may include divorced, widowed, never married, or common-law.
Table 2.
Unadjusted and adjusted/multivariable odds ratios (OR) and confidence intervals (CI) for association with partial immunization, as compared to complete immunizationa
| Variable | Unadjusted OR (95% CI) | Adjusted ORb (95% CI) |
|---|---|---|
| Knowledge, attitudes, and beliefs | ||
| Concerned about vaccine safety c | ||
| No | Reference | Reference |
| Yes | 7.338 (4.138–13.012) | 2.829 (1.151–6.957) |
| Lack of belief in disease susceptibility and severity, and vaccine effectiveness d | ||
| No | Reference | Reference |
| Yes | 6.001 (3.717–9.690) | 4.629 (2.017–10.625) |
| Distrust in medical professionals e | 1.317 (1.131–1.533) | 0.973 (0.750–1.262) |
| Distrust in government f | 1.116 (1.046–1.306) | 0.972 (0.813–1.162) |
| Personal variables | ||
| Number of children in household | ||
| <3 | Reference | Reference |
| ≥3 children | 1.643 (1.032–2.618) | 1.919 (0.927–3.973) |
| Need more social support g | 1.044 (0.945–1.153) | 1.099 (0.950–1.271) |
| Member of household with serious health issue | ||
| No | Reference | Reference |
| Yes | 1.264 (0.674–2.371) | 1.615 (0.682–3.828) |
| Moved in past 2 years | ||
| No | Reference | Reference |
| Yes | 2.471 (1.564–3.904) | 3.908 (2.075–7.358) |
| Worked & Used childcare in first 2 years? | ||
| Did not work | Reference | Reference |
| Worked, but no childcare outside home | 0.706 (0.417–1.195) | 0.525 (0.247–1.116) |
| Worked and used childcare outside home | 0.488 (0.290–0.819) | 0.310 (0.144 - 0.671) |
| Systemic variables, including experience with immunizations and the immunization delivery system | ||
| Bad immunization experience with older child | ||
| No | Reference | Reference |
| Yes | 1.532 (0.806–2.915) | 0.732 (0.285–1.881) |
| Experience with side effect(s) | ||
| No | Reference | Reference |
| Yes | 2.688 (1.714–4.216) | 1.657 (0.869–3.160) |
| Knew someone with a vaccine-preventable disease | ||
| No | Reference | Reference |
| Yes | 0.810 (0.496–1.324) | 0.813 (0.408–1.619) |
| Positive experience with immunization provider h | 0.849 (0.789–0.912) | 0.993 (0.882–1.117) |
| Received adequate information on immunizations | ||
| No | Reference | Reference |
| Yes | 0.320 (0.196–0.520) | 1.220 (0.535–2.780) |
| Heard negative views about immunizations in the media | ||
| No | Reference | Reference |
| Yes | 1.789 (1.020–3.135) | 1.768 (0.783–3.996) |
| Ever delayed immunizations because too many needles at once | ||
| No | Reference | Reference |
| Yes | 15.100 (6.391–35.675) | 7.734 (2.598–23.025) |
| Considered not getting immunizations because of needle pain | ||
| No | Reference | Reference |
| Yes | 2.632 (1.399–4.953) | 0.818 (0.293–2.248) |
| Child has a regular family doctor/pediatrician | ||
| No | Reference | Reference |
| Yes | 0.182 (0.070–0.474) | 0.219 (0.057–0.846) |
| Getting immunizations was a hassle/difficult i,j | ||
| Not difficult | Reference | Reference |
| Slightly difficult | 0.506 (0.061–4.191) | 1.389 (0.676 - 2.852) |
| Somewhat difficult | 1.372 (0.830–2.268) | 1.089 (0.373 - 3.177) |
| Quite or Very difficult | 1.983 (0.972–4.047) | 14.470 (2.206- 34.922) |
| Specific hassles: | ||
| Difficult to travel to clinic? k | ||
| No | Reference | Reference |
| Yes | 1.087 (0.637–1.854) | 0.581 (0.242–1.396) |
| Clinic far from home? l | ||
| No | Reference | Reference |
| Yes | 1.243 (0.731–2.115) | 1.089 (0.517–2.294) |
| Wait time in clinic unreasonable | ||
| No | Reference | Reference |
| Yes | 1.163 (0.627–2.158) | 0.653 (0.256–1.667) |
| Had to bring other children or get childcare | ||
| No | Reference | Reference |
| Yes | 1.111 (0.714–1.730) | 1.047 (0.533–2.056) |
| Had to take time off/rearrange work schedule | ||
| No | Reference | Reference |
| Yes | 1.278 (0.827–1.975) | 1.559 (0.808–3.007) |
| Clinic hours/appointment convenient m | 0.882 (0.777–1.001) | 0.945 (0.774–1.153) |
aDetails of coding of variables and handling of missing values are described in the online supplement.
cMeasured on a scale from 5–25; Composite score of 5 variables (each on 5-point Likert scale) measuring vaccine safety, determined by factor analysis. Dichotomized at natural breakpoint; No = scored ≤12; Yes = scored >12.
dMeasured on a scale from 9–45; Composite score of 9 variables (each on 5-point Likert scale) measuring belief in susceptibility to and severity of disease, and effectiveness of vaccines, determined by factor analysis. Dichotomized at natural breakpoint; No = scored ≤ 33; Yes = scored >33.
eMeasured on a scale from 2 to 10; Composite score of 2 variables (each on 5-point Likert scale) measuring distrust in nurses and physicians.
fMeasured on a scale from 2 to 10; Composite score of 2 variables (each on 5-point Likert scale) measuring distrust in provincial and federal governments.
gMeasured on a scale from 2 to10, based on previously validated measure (Seeman & Berkman, 1988).
hMeasured on a scale from 5–25; Composite score of 5 variables (each on 5-point Likert scale) measuring quality of previous experience (trust and positive interactions) with immunization providers (nurses and clinic staff).
iVariable non-significant overall in multivariate analysis.
jCategories for Don't know and/or Missing not statistically significant and not shown.
kMeasured on 5-point Likert scale. Dichotomized: No = Not difficult at all, Yes = Slightly difficult to very difficult.
lMeasured on 5-point Likert scale. Dichotomized: No = Very or quite close, Yes = Quite or very far.
mMeasured on a scale from 2 to 10; Composite score of 2 variables (each on 5-point Likert scale) measuring convenience of clinic hours and appointment time.
Vaccine safety concern
Concern about vaccine safety was strongly associated with being partially immunized in unadjusted analysis (OR 7.338, 95% CI 4.138 – 13.012), but the effect was substantially reduced when all other variables were added to the model (aOR 2.829, 95% CI 1.151 – 6.957). Lack of belief in disease susceptibility and severity was highly associated with partial immunization (aOR 4.629, 95% CI 2.017–10.625), and played a role in mediating the influence of vaccine safety concern. Distrust in medical professionals and the government were only associated with partial immunization in unadjusted analysis.
Personal characteristics
Having ≥ 3 children under the age of 18 y in the household was associated with being partially immunized in unadjusted analysis, but did not remain statistically significant in the multivariable model. No confounding or interaction was found between the number of children and the ‘hassles of immunization’. Residential mobility (having moved in the 2 y since the child was born) was strongly associated with partial immunization (aOR 3.908, 95% CI 2.075–7.358). In contrast, a strong predictor of complete immunization was having a primary caregiver who worked outside the home in the first 2 y after birth, if the child attended daycare (aOR 0.310, 95% CI 0.144–0.671); the association was not significant if the child did not attend daycare.
System-level variables
Parents who had delayed their child's immunizations because there were ‘too many needles given at one visit’ were much more likely to only partially immunize (OR 15.100, 95% CI 6.391 – 35.675), regardless of other variables being added to the model (aOR 7.734, 95% CI 2.598 – 23.025). Parents’ perception that getting immunizations was a ‘big hassle’ (measured as being ‘quite or very difficult’) was associated with partial immunization in multivariable analysis (aOR 14.470, 95% CI 2.206 - 34.922), while the lower categories of difficulty were not. However, none of the specific ‘hassles’ of getting a child immunized (e.g. distance to clinic, wait time in clinic) were associated with immunization status. Children with a regular family doctor/pediatrician were more likely to be completely immunized, even when all other variables were controlled for (aOR 0.219, 95% CI 0.057 – 0.846). There were a number of other systemic factors that were associated with immunization status in the unadjusted analysis that did not remain significant in the multivariable model (such as needle pain and exposure to negative views about immunizations in the media).
Discussion
Previous research has found that parents who refuse all vaccines have significant concerns about vaccine safety.5-7 Our study found that concern about vaccine safety was also a significant barrier to vaccine completion among parents of children who had started the vaccine series. It is uncertain whether these parents started immunizing despite an existing concern, or whether their concern arose after the start of the immunization series. It is known that even parents of fully immunized children often have concerns about vaccine safety,8-12 so it is conceivable that these parents had pre-existing concerns, but chose to begin immunizing, only to stop part way through the series. It is also possible that these parents had concerns about only specific vaccines and were selectively refusing some vaccines, while accepting of others.13 Unfortunately, our data does not allow us to distinguish between selective immunizers and those who received some doses but never finish the vaccine series. Future work is planned to distinguish these subsets of partial immunizers. A unique contribution of our work is that it builds on previous studies of parental beliefs that did not assess system level factors14,15, and it assesses the attitudes of parents who only partially immunize their children, addressing an identified gap in knowledge.5 Our findings indicate that, irrespective of health care system factors that may impede access, immunization uptake is strongly influenced by concern about vaccine safety and lack of belief in vaccine effectiveness or disease susceptibility and severity.
Children who moved residence since birth were more likely to be partially immunized, confirming findings of previous studies.7,16-20 It is likely that residential mobility results in practical barriers, such as not knowing where to go for immunizations or not receiving appointment reminders.5 In addition to its impact on vaccine completion, residential mobility also poses a challenge for the maintenance of accurate immunization records. The vast majority of undeliverable surveys in our sample (214 of 274) were for ‘partially immunized’ children according to the registry, when in fact these ‘unreachable’ children may have been complete for immunizations, but lost to follow up. Improvements in immunization registry systems that make it easier to access and link information could enable more efficient tracking and follow-up of families who move.18
Vaccine uptake was strongly associated with the child attending daycare when the primary caregiver worked outside the home in the first 2 y after birth. This finding was somewhat surprising, as we had anticipated that the mother's return to work would be a barrier to immunization completion, due to conflicts between immunization appointments and employment commitments.21 Our finding to the contrary suggests that, in fact, attendance at daycare promoted immunization completion. This may be due to parents’ altered perception of risk once their child leaves the ‘safe haven’ of home, a hypothesis that is consistent with our finding that belief in disease susceptibility is an important factor influencing immunization completion. Daycare immunization policies themselves were not responsible for this finding, as there is no legislated daycare immunization policy in the region and the majority of parents in our study reported that their child's daycare did not require documentation of immunization. Previous studies have assessed the impact of employment, with mixed findings,21-26 but not the influence of childcare outside the home.
Parental concern about the number of needles administered at a single visit was the strongest influence on partial immunization. It is noteworthy that children in our study setting received a total of 13 injections by age 2, with up to 4 needles at a single visit. The statistical and clinical significance of this factor in the multivariable model suggests that, regardless of concern about vaccine safety, parents who felt that too many needles were given at one visit were more likely to not complete their children's immunizations by age 2. This finding is consistent with other studies which found that parents object to the number of injections27-32 and that fewer injections at each visit might improve uptake.30,33,34 This suggests that measures to reduce the number of needles (either overall number in the schedule or number per visit) might have a meaningful impact on parents’ decision to complete immunizations. Unfortunately, decreasing the total number of needles in the schedule through introduction of combination vaccines may antagonize parents who object to combining multiple antigens in a vaccine;35 and even more of a concern is the fact that decreasing the number of needles per visit increases the number of necessary visits, which has been shown to decrease the likelihood of completing immunizations.29,34
The association between having a regular family doctor or pediatrician and completion of immunizations is supported by previous studies which show that a relationship with a trusted health care provider increases immunization uptake.36-39 However, studies that have found this association in a context where physicians provide the immunizations might have difficulty drawing conclusions about the relationship between having a physician and getting immunized, since one is a necessary prerequisite for the other. This study is unique in that it completely removes that factor, given that vaccines are provided by public health nurses in our setting. This finding could be explained by physicians promoting immunizations to their patients, even though they are not the ones providing them, or it may be that parents who have a regular physician for their child are also more likely to engage in health prevention behavior, or have greater trust in health care system recommendations, including childhood immunizations.15 In either case, the value of this trusting relationship cannot be understated. Physicians ‘dismissing’ patients from their practice for refusing to vaccinate their children40,41 jeopardizes one of the best opportunities available to positively influence parents’ vaccine attitudes and practices.
Strengths and limitations
This study included systemic factors related to the immunization delivery process in a multivariable model along with vaccine safety concern and other variables, which enabled us to determine whether system level variables moderated parental safety concerns, or were strong predictors of vaccine uptake over and above parental concern. It is important to consider whether these study results are generalizable to jurisdictions, such as the USA, where mandatory immunization school entry policies exist. It is likely that the findings are applicable to the pre-school population in such jurisdictions, which have comparable immunization coverage rates at age 2 y (30% of 19–35 month old American children are partially immunized and 1% have received no vaccine doses).42 However, vaccine uptake in school-aged children in the presence of mandatory policies would conceivably be less influenced by system-level barriers and more by parental objection to vaccines, since parental filing of an approved exemption is required for vaccine refusal. Non-coverage error in our study was minimized by using a sampling frame that was largely inclusive of the cohort of interest. However, we were not able to assess urban-rural differences because we did not have proportional sampling from rural and urban communities and our sample only included the semi-rural communities surrounding Edmonton and not remote rural residents.
Our considerable efforts to minimize survey non-response enabled us to achieve a response rate of 43%, close to our anticipated rate of 50%. However, this modest response rate and the statistically significant differential response rate between complete and partial immunizers does leave the possibility for non-response bias if the associations determined in the sample differed between respondents and non-respondents (as described in the online supplement). It is possible that survey non-response is due to overwhelming time demands on some parents, which might also be associated with being partially immunized. Thus, the lower response rate from partial immunizers in our study may result in an under-estimate of the influence of system-level factors (e.g., inconvenient clinic hours, distance to clinic) on immunization uptake.
In the absence of a previously validated questionnaire we followed a rigorous questionnaire development process (see online supplement) and used validated questions whenever possible. However the excessive length of our questionnaire likely contributed to survey non-response.
Although a number of systemic variables were significant in unadjusted analysis, many did not maintain significance in the multivariable model. It is possible that our sample size limited the ability to detect differences in multivariable analysis. Some of these variables are potentially important in the context of emerging vaccines. For instance, the negative association between vaccine uptake and parents’ experience with vaccine side effects is worthy of further exploration given the development of newer vaccines with increased risk of side effects (e.g., febrile seizure after MMR-Varicella vaccine43). Clearly, further research with larger samples that allow modeling of direct and indirect effects would be valuable, as would studies that tease apart the heterogeneity of the group of ‘partial’ immunizers.
Conclusion
While concern about vaccine safety has previously been found to be associated with refusal of vaccines, the relationship is not straightforward. Our study shows that many parents who initially started immunizing their child also had concerns about vaccine safety. Other parental attitudes and beliefs, as well as personal and systemic factors, were also found to influence immunization status, either through a direct effect or by mediating the influence of parental safety concern. Our study identified variables that can be influenced through policy and/or program strategies and are not dependent on public or parent health education. This provides an important opportunity, given the challenge of changing individuals’ attitudes and beliefs.44
System level strategies that health care providers and program and policy administrators might take to improve immunization coverage include: (a) improved tracking and follow-up of families following residential moves, including use of computerized immunization information systems and appointment reminders that provide the location of the nearest immunization clinic; (b) strategies to promote immunization of children that do not attend daycare; (c) development and use of more combination vaccines, while still allowing parents the choice of separate vaccines; and (d) improved access to regular family physicians or pediatricians, and promotion of immunization by such physicians, regardless of whether they are the designated immunization provider.
Methods
Study population and setting
The target population was parents or primary care-givers of a cohort of children who turned 2 y old between May 2008 - April 2009. The study was conducted in the city of Edmonton and surrounding rural communities (population ∼1.1. million45) in the province of Alberta, Canada. There is no mandatory immunization school entry policy in the province, so parents can choose not to immunize without any penalty or need to file an exemption. All routine childhood immunizations in Alberta are publicly-funded and administered free of charge by public health nurses in community-based clinics. In the Edmonton region, immunization records are entered into a computerized immunization registry, the details of which have been reported elsewhere.46
Study design
A sample of 1342 parents were recruited to participate in a postal survey to assess the immunization views, experiences, and characteristics of parents of children whose immunizations were complete at 2 y of age (controls, n = 671) compared to those who were incompletely immunized (cases, n = 671). ‘Completely immunized’ children had received all doses of the recommended immunization schedule: 4 doses of Diphtheria, Tetanus, acellular Pertussis, Polio and Haemophilus influenzae type b; 1 dose of Measles, Mumps, and Rubella; 1 dose of Varicella, or history of disease; 3 doses of Meningococcal C conjugate; and 4 doses of Pneumococcal 7-valent conjugate. For the purposes of this analysis, ‘incompletely immunized’ children were further subcategorized as either ‘received no vaccines’ or were ‘partially immunized’ (received ≥1 dose of any of the vaccines, but had not completed the schedule by the age of 24 months). Subjects were selected from the immunization registry using random number generation and an algorithm to account for variation in the number of doses required for children who were older at initiation of the series or due to individual clinical conditions. The sample size for the study was calculated using an effect size and response rate from a previous study,47 a 95% Confidence Interval, 80% Power (β = 0.20), and a 1:1 ratio of cases to controls.
Data Collection
A questionnaire was developed to assess (a) socioeconomic characteristics; (b) concern about vaccine safety; (c) other attitudes and beliefs about immunizations and vaccine-preventable disease; (d) personal factors; and (e) systemic factors. The details of the questionnaire design and validation process are presented in the online supplementary document. Validated postal survey procedures 48 were followed to promote a high response rate and minimize the potential for non-response bias. Study parents were mailed an advance notification letter, followed by the questionnaire and a postage-paid return envelope one week later. Participants who did not respond within 3 weeks were sent a reminder postcard, followed by a replacement survey 3 weeks later, and a final reminder another 3 weeks later. Parents could confidentially opt out of the survey at any time using their assigned tracking number. Return of the completed questionnaire implied consent to participate in the study. Ethical approval was obtained from the Health Research Ethics Board at the University of Alberta.
Data entry and analysis
Survey responses were entered into SPSS version 20.049 using the REDCap data management system.50 Double data entry of 10% of the sample found a sufficiently low level of error (0.13%) to confirm the accuracy of data entry. The outcome variable for this analysis was the child's immunization status; 1 = Partially immunized (cases) and 0 = Completely immunized (controls). Children with no vaccines (n = 17) were excluded from this analysis. Unadjusted/crude ORs of the association between each exposure variable and the outcome variable were calculated using bivariate logistic regression. A multivariable logistic regression was then performed to determine the adjusted OR (aOR) for each variable. Variables were included in the multivariable model based on their clinical significance (i.e., if evidence from the literature suggested that they were relevant or there was a scientifically plausible association with the outcome or another exposure variables), and were maintained in the model regardless of statistical significance in bivariate analysis, in case they exerted an effect in the multivariable model. Potential confounders and theoretically plausible interaction effects were also tested in the model and maintained if significant. The coding of variables for analysis can be found in the online supplement.
Supplementary Material
Disclosure of Potential Conflicts of Interest
There were no potential conflicts of interest.
Acknowledgments
This work would not have been possible without the guidance and support of Christine Newburn-Cook, PhD, RN, who passed away in August 2011.
Funding
During completion of this study, Shannon MacDonald received stipend funding from the Canadian Child Health Clinician Scientist Program, a Canadian Institutes of Health Research (CIHR) Strategic Training Initiative; Women's and Children's Health Research Institute; University of Alberta Faculty of Nursing; Alberta Innovates Health Solutions; and the Izaak Walton Killam Memorial Trust.
References
- 1. Dummer TJB, Yunsong C, Strang R, Parker L. Immunization completeness of children under two years of age in Nova Scotia, Canada. Can J Public Health 2012; 103:363-7; PMID:23617989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McWha L, MacArthur A, Badiani T, Schouten H, Tam T, King A. Measuring up: results from the national immunization coverage survey, 2002. Can Commun Dis Rep 2004; 30:37-50; PMID:15035404 [PubMed] [Google Scholar]
- 3. Diekema DS. Improving childhood vaccination rates. N Engl J Med 2012; 366:391-3; PMID:22296072;http://dx.doi.org/ 10.1056/NEJMp1113008 [DOI] [PubMed] [Google Scholar]
- 4. Opel DJ, Marcuse EK. Window or mirror: social networks’ role in immunization decisions. Pediatrics 2013; 131:e1619-20; PMID:23589807; http://dx.doi.org/ 10.1542/peds.2013-0531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Samad L, Butler N, Peckham C, Bedford H, Millennium Cohort Study Child Health Group . Incomplete immunisation uptake in infancy: maternal reasons. Vaccine 2006; 24:6823-9; PMID:17050048; http://dx.doi.org/ 10.1016/j.vaccine.2006.06.039 [DOI] [PubMed] [Google Scholar]
- 6. Samad L, Tate AR, Dezateux C, Peckham C, Butler N, Bedford H. Differences in risk factors for partial and no immunisation in the first year of life: prospective cohort study. BMJ 2006; 332:1312-3; PMID:16740559; http://dx.doi.org/ 10.1136/bmj.332.7553.1312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith PJ, Chu SY, Barker LE. Children who have received no vaccines: who are they and where do they live? Pediatrics 2004; 114:187-95; PMID:15231927; http://dx.doi.org/ 10.1542/peds.114.1.187 [DOI] [PubMed] [Google Scholar]
- 8. Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff (Millwood) 2011; 30:1151-9; PMID:21653969; http://dx.doi.org/ 10.1377/hlthaff.2011.0396 [DOI] [PubMed] [Google Scholar]
- 9. Burton-Jeangros C, Golay M, Sudre P. Compliance and resistance to child vaccination: a study among swiss mothers. Rev Épidémiol Santé 2005; 53:341-50; PMID:16353509 [DOI] [PubMed] [Google Scholar]
- 10. Wu AC, WislerSher DJ, Griswold K, Colson E, Shapiro ED, Holmboe ES, Benin AL. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Matern Child Health J 2008; 12:766-73; PMID:17987370; http://dx.doi.org/ 10.1007/s10995-007-0302-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Casiday R, Cresswell T, Wilson D, Panter-Brick C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine 2006; 24:177-84; PMID:16157422; http://dx.doi.org/ 10.1016/j.vaccine.2005.07.063 [DOI] [PubMed] [Google Scholar]
- 12. EKOS Research Associates Inc Survey of parents on key issues related to immunization: final report. Ottawa: Public Health Agency of Canada; 2011. Available from: http://resources.cpha.ca/immunize.ca/data/1792e.pdf [Google Scholar]
- 13. Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy: an overview. Hum Vaccin Immunother 2013; 9:1763-73; PMID:23584253; http://dx.doi.org/ 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bardenheier B, Yusuf H, Schwartz B, Gust D, Barker L, Rodewald L. Are parental vaccine safety concerns associated with receipt of measles-mumps-rubella, diphtheria and tetanus toxoids with acellular pertussis, or hepatitis B vaccines by children? Arch Pediatr Adolesc Med 2004; 158:569-75; PMID:15184221; http://dx.doi.org/ 10.1001/archpedi.158.6.569 [DOI] [PubMed] [Google Scholar]
- 15. Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch Pediatr Adolesc Med 2005; 159:470-6; PMID:15867122; http://dx.doi.org/ 10.1001/archpedi.159.5.470 [DOI] [PubMed] [Google Scholar]
- 16. Li J, Taylor B. Factors affecting uptake of measles, mumps, and rubella immunisation. BMJ 1993; 307:168-71; PMID:8343745; http://dx.doi.org/ 10.1136/bmj.307.6897.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miller LA, Hoffman RE, Baron AE, Marine WM, Melinkovich P. Risk factors for delayed immunization against measles, mumps, and rubella in Colorado two-year-olds. Pediatrics 1994; 94:213-9; PMID:8036076 [PubMed] [Google Scholar]
- 18. Pearce A, Elliman D, Bedford H, Law C. Residential mobility and uptake of childhood immunisations: findings from the UK millennium cohort study. Vaccine 2008; 26:1675-80; PMID:18294744; http://dx.doi.org/ 10.1016/j.vaccine.2008.01.031 [DOI] [PubMed] [Google Scholar]
- 19. Baker D, Garrow A, Shiels C. Inequalities in immunisation and breast feeding in an ethnically diverse urban area: cross-sectional study in Manchester, UK. J Epidemiol Community Health 2011; 65:346; PMID:20466709; http://dx.doi.org/ 10.1136/jech.2008.085142 [DOI] [PubMed] [Google Scholar]
- 20. Williams N, Woodward H, Majeed A, Saxena S. Primary care strategies to improve childhood immunisation uptake in developed countries: systematic review. JRSM Short Rep 2011; 2:8; PMID:21369526; http://dx.doi.org/ 10.1258/shorts.2010.010063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mindlin M, Jenkins R, Law C. Maternal employment and indicators of child health: a systematic review in pre-school children in OECD countries. J Epidemiol Commun Health 2009; 63:340-50; PMID:19193668; http://dx.doi.org/ 10.1136/jech.2008.077073 [DOI] [PubMed] [Google Scholar]
- 22. Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood diseases: maternal factors related to immunization status of preschool children in Italy. Prev Med 2000; 31:49-55; PMID:10896843; http://dx.doi.org/ 10.1006/pmed.2000.0677 [DOI] [PubMed] [Google Scholar]
- 23. Matsumura T, Nakayama T, Okamoto S, Ito H. Measles vaccine coverage and factors related to uncompleted vaccination among 18-month-old and 36-month-old children in Kyoto, Japan. BMC Public Health 2005; 5:5; PMID:15647120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brenner RA, Simons-Morton B, Bhaskar B, Das A, Clemens JD. Prevalence and predictors of immunization among inner-city infants: a birth cohort study. Pediatrics 2001; 108:661-70; PMID:11533333 [DOI] [PubMed] [Google Scholar]
- 25. Theeten H, Hens N, Vandermeulen C, Depoorter AM, Roelants M, Aerts M, Hoppenbrouwers K, Van Damme P. Infant vaccination coverage in 2005 and predictive factors for complete or valid vaccination in Flanders, Belgium: An EPI-Survey Vaccine 2007; 25:4940-8; PMID:17524528 [DOI] [PubMed] [Google Scholar]
- 26. Iordanou P, Gessouli E, Kaba E, Kroustalli E. Vaccination coverage among schoolchildren: DTP, DT, T and Sabin-polio. ICUS NURS WEB J 2006; 25:1108-7366. [Google Scholar]
- 27. Happe LE, Lunacsek OE, Marshall GS, Lewis T, Spencer S. Combination vaccine use and vaccination quality in a managed care population. Am J Manag Care 2007; 13:506-12; PMID:17803364 [PubMed] [Google Scholar]
- 28. Madlon-Kay DJ, Harper PG. Too many shots? Parent, nurse, and physician attitudes toward multiple simultaneous childhood vaccinations. Arch Fam Med 1994; 3:610-3; PMID:7921297; http://dx.doi.org/ 10.1001/archfami.3.7.610 [DOI] [PubMed] [Google Scholar]
- 29. Meyerhoff AS, Jacobs RJ. Do too many shots due lead to missed vaccination opportunities? does it matter?. Prev Med 2005; 41:540-4; PMID:15917050; http://dx.doi.org/ 10.1016/j.ypmed.2004.12.001 [DOI] [PubMed] [Google Scholar]
- 30. Woodin KA, Rodewald LE, Humiston SG, Carges MS, Schaffer SJ, Szilagyi PG. Physician and parent opinions. Are children becoming pincushions from immunizations? Arch Pediatr Adolesc Med 1995; 149:845-9; PMID:7633536; http://dx.doi.org/ 10.1001/archpedi.1995.02170210019003 [DOI] [PubMed] [Google Scholar]
- 31. Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics. 2011; 127:S92-9; PMID:21502253; http://dx.doi.org/ 10.1542/peds.2010-1722N [DOI] [PubMed] [Google Scholar]
- 32. Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, Battaglia M, Wright R, Schwartz B. Underimmunization among children: Effects of vaccine safety concerns on immunization status. Pediatrics 2004; 114:e16-22; PMID:15231968; http://dx.doi.org/ 10.1542/peds.114.1.e16 [DOI] [PubMed] [Google Scholar]
- 33. Marshall GS. One for all: newer combination vaccines in practice. Pediatr Ann 2004; 33:501-11; PMID:15354602; http://dx.doi.org/ 10.3928/0090-4481-20040801-08 [DOI] [PubMed] [Google Scholar]
- 34. Marshall GS, Happe LE, Lunacsek OE, Szymanski MD, Woods CR, Zahn M, Russell A. Use of combination vaccines is associated with improved coverage rates. Pediatr Infect Dis J 2007; 26:496-500; PMID:17529866; http://dx.doi.org/ 10.1097/INF.0b013e31805d7f17 [DOI] [PubMed] [Google Scholar]
- 35. Gidengil C, Lieu TA, Payne K, Rusinak D, Messonnier M, Prosser LA. Parental and societal values for the risks and benefits of childhood combination vaccines. Vaccine 2012; 30:3445-52; PMID:22449423; http://dx.doi.org/ 10.1016/j.vaccine.2012.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bigham M, Remple VP, Pielak K, McIntyre C, White R, Wu W. Uptake and behavioural and attitudinal determinants of immunization in an expanded routine infant hepatitis B vaccination program in British Columbia. Can J Public Health 2006; 97:90-5; PMID:16619992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics 2008; 122:718-25; PMID:18829793; http://dx.doi.org/ 10.1542/peds.2007-0538 [DOI] [PubMed] [Google Scholar]
- 38. Omer SB, Salmon DA, Orenstein WA, DeHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. New Engl J Med 2009; 360:1981-8; http://dx.doi.org/ 10.1056/NEJMsa0806477 [DOI] [PubMed] [Google Scholar]
- 39. Healy CM, Montesinos DP, Middleman AB. Parent and provider perspectives on immunization: Are providers overestimating parental concerns? Vaccine 2014; 32:579-84; PMID:24315883; http://dx.doi.org/ 10.1016/j.vaccine.2013.11.076 [DOI] [PubMed] [Google Scholar]
- 40. Flanagan-Klygis EA, Sharp L, Frader JE. Dismissing the family who refuses vaccines: a study of pediatrician attitudes. Arch Pediatr Adolesc Med 2005; 159:929-34; PMID:16203937; http://dx.doi.org/ 10.1001/archpedi.159.10.929 [DOI] [PubMed] [Google Scholar]
- 41. Leib S, Liberatos P, Edwards K. Pediatricians’ experience with and response to parental vaccine safety concerns and vaccine refusals: a survey of connecticut pediatricians. Public Health Rep 2011; 126:13-23; PMID:21812165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Centers for Disease Control and Prevention (CDC) . National, state, and local area vaccination coverage among children aged 19–35 months — United States, 2012. Morbidity and Mortality Weekly Rep (MMWR) 2013; 62(36):733-40; PMID:24025754 Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6236a1.htm [PMC free article] [PubMed] [Google Scholar]
- 43. Marin M. Broder KR. Temte JL. Snider DE. Seward JF, Centers for Disease Control and Prevention (CDC) . Use of combination measles, mumps, rubella, and varicella vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2010; 59:1-12; PMID:20448530 [PubMed] [Google Scholar]
- 44. Rosenstock IM, Strecher VJB,M.H. Social learning theory and the health belief model. Health Educ Quart 1988; 15:175-83; http://dx.doi.org/ 10.1177/109019818801500203 [DOI] [PubMed] [Google Scholar]
- 45.Alberta Interactive Health Data Application. Population Estimates-Adjusted. Available from: http://www.ahw.gov.ab.ca/IHDA_Retrieval/selectSubCategoryParameters.do [Google Scholar]
- 46. MacDonald SE, Schopflocher DP, Golonka RP. The pot calling the kettle black: the extent and type of errors in a computerized immunization registry and by parent report. BMC Pediat 2014; 14:1; PMID:24387002; http://dx.doi.org/ 10.1186/1471-2431-14-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Boulianne N, Deceuninck G, Duval B, Lavoie F, Dionne M, Carsley J, Valiquette L, Rochette L, De Serres G. Why are some children incompletely vaccinated at the age of 2? Can J Public Health 2003; 94:218-23; PMID:12790498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd, 2007. update ed. Hoboken, NJ: John Wiley & Sons; 2007. [Google Scholar]
- 49. IBM Corp IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp; 2011. [Google Scholar]
- 50. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Info 2009; 42:377-81; http://dx.doi.org/ 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


