Abstract
Introduction:
Chronic pain results in significant personal, societal and economic burden. Doctors and nurses have a pivotal role in patient pain management. In order to determine the effectiveness of current pain education on knowledge, attitudes and perceptions of medical and nursing students, there needs to be a valid measure to assess and quantify these domains. We reviewed the literature to identify approaches for assessing knowledge, perceptions and attitudes to pain management among nursing and medical students.
Methods:
Databases of peer-reviewed literature including CINAHL, EMBASE, ERIC, PsycInfo, Medline and PubMed were searched for articles published between 1993 and December 2014 using the following search terms: student, graduate, intern, junior, pain, pain management, analgesia, analgesic, pharmacology, pharmacological, knowledge, competence, attitude, preparedness, practice, nursing, medical, doctor, nurse.
Results:
The search revealed over 3500 articles, and on application of the inclusion criteria, 26 articles were included in the review. A total of 14 instruments were used in these studies with the Knowledge and Attitudes Survey Regarding Pain (KASRP) as the main instrument in 9 out of the 26 articles. The various instruments used different question formats such as multiple-choice questions (MCQs), true/false statements and Likert scales that went from 3 points to 7 points. Clinical skills examinations were also used in four studies to assess pain management.
Conclusion:
There is no gold standard instrument currently used to assess knowledge, perceptions and attitudes to pain management. The results of this review showed, despite the diversity of standardised instruments that have been used to assess knowledge, perceptions and attitude to pain management, the literature has consistently reported that knowledge about pain management among nursing and medical students was generally poor among both groups.
Keywords: Pain management, medical students, nursing students, assessment, knowledge
Introduction
Pain is the most common reason why people visit a healthcare professional.1 As reported by Brennan et al.,2 inadequate pain management is the source of major economic and human costs for patients, their families and society. In the United States, according to the Institute of Medicine, chronic pain affects approximately 100 million Americans.3 This number is higher than the number of diabetes, heart disease and cancer sufferers combined. The cost to the US economy of chronic pain, including healthcare and lost productivity costs, was estimated to be between US $560 and US $635 billion annually. It is important to note that these estimates do not include cancer-related pain.3 In Europe, a cross-sectional survey reported that 19% of adults suffered from chronic pain of moderate-to-severe intensity and nearly half received inadequate pain management.4 In Australia, it is expected that one in five Australians will suffer chronic pain in their lifetime, and it is estimated to cost the economy AUD 34 billion per annum.5 Blyth et al.6 have reported that chronic pain impacts a large proportion of the adult Australian population, including the working age population. A study by Mäntyselkä et al.7 also reported that pain is the most common reason why Finish patients visit a doctor. This highlights the significant burden of chronic pain on the healthcare system.8
Despite the physiological, psychological and economic impact of inadequate pain management and its ramifications for patients, their families and society, evidence indicates there is still a gap in the understanding of the pain pathophysiology, by healthcare professionals, which is likely to have contributed to the widespread inadequacy of pain treatment.2 One reason could be a lack of national guidelines regarding the management of pain as a health problem, although a lack of an integrated approach in the pre-service nursing and medical programmes is likely to have compounded the problem.9 It is also important to recognise that the approach to pain management is not simply a biological one as noted by Gatchel et al.10 Pain results from a dynamic and complex interaction among physiologic, psychological and social factors.
Graduates in medicine and nursing are the key players in prescribing and administering medication and have a pivotal role in patient pain management. However, despite the International Association for the Study of Pain (IASP) undergraduate curricula for health professionals having being recommended for over three decades, and the recognition of the importance of undergraduate education in pain and its management, pain has been found to be inadequately addressed in undergraduate curricula.3,5,11,12 A major goal of pre-service education besides promoting knowledge and skills acquisition is to facilitate the development of positive attitudes and conduct in order to deliver quality care in pain management.13–15 Nevertheless, a literature search on educational research conducted by Briggs et al.16 as a background to their survey study revealed a small number of studies exploring existing pain curricula in various disciplines with most concluding that pain education is fragmented, inadequately assessed and inconsistent between universities.
In order to determine the effectiveness of current pain education on knowledge, attitudes and perceptions of medical and nursing students, there needs to be a valid measure to assess and quantify these domains. The aim of this study was to conduct a review of the literature to identify approaches for assessing pain management knowledge among nursing and medical students. In particular, the study has addressed the following questions: (1) What instruments have been used to assess knowledge, perceptions and attitudes to pain management among medical and nursing students? (2) What are the characteristics of the studies and the instruments used?
Methods
Identification of studies
A search was performed to identify studies and reports published between January 1993 and December 2014. Databases of peer-reviewed literature including CINAHL, EMBASE, ERIC, PsycInfo, Medline and PubMed were searched. The reference lists of all selected publications were then hand-searched for any relevant references missing in the database searches. Web-based searches, using the Internet search engines ‘Google’ and ‘Google Scholar’, were conducted to identify national and international reports.
Search strategy
Search terms used included the following: student, graduate, intern, junior, pain, pain management, analgesia, analgesic, pharmacology, pharmacological, knowledge, competence, attitude, preparedness, practice, nursing, medical, doctor, nurse. These search terms were also used in Google Scholar to corroborate our primary search strategy.
Inclusion and selection criteria
The following criteria were used for the review and selection of the studies:
Published 1993–2014;
Available in English;
Specifically focused on strategies used to assess knowledge, perceptions and attitudes regarding pain management of nursing and medical students;
Relevance to the topic after review of abstracts;
Hand searching of reference lists of selected articles and reports;
Relevant reports/publications known to the researchers.
Data extraction
Data were extracted from the articles according to the headings listed in Table 1: name of first author, date of publication, country of study, study population, type of study, instrument used and a brief summary of the primary findings. Papers in which instrument scores were mentioned were reported as mean scores (±standard deviation (SD)) where possible.
Table 1.
Summary of the papers included in this study.
| Author (year of publication) | Country | Study population | Research design | Instrument | Primary finding |
|---|---|---|---|---|---|
| Weiner et al. (2014)17 | United States | Third-year medical students: Intervention group (n = 27); Control group (n = 28) | Intervention: E-learning module on chronic lower back pain (CLBP) with Objective Structured Clinical Examination (OSCE) | OSCE – one CLBP station out of nine stations | Students exposed to CLBP module. Mean scores: 79.5 (SD: 10.4)Students not exposed to CLBP module. Mean scores: 62.0 (SD: 8.6)No significant group differences were detected |
| Owens et al. (2014)18 | United Kingdom | Paediatric nursing students: Intervention group (n = 45); Control group (n = 37) | Intervention: structure pain management programme; pre-/post-intervention questionnaire | Knowledge and Attitudes Survey Regarding Pain (KASRP) – modified | Intervention group showed greater improvement in knowledge. However, results suggest lack of knowledge in relation to pathophysiology, assessment and pharmacology of pain |
| Al-Khawaldeh et al. (2013)19 | Jordan | Final-year nursing students (n = 240) | Cross-sectional study | KASRP – modified. 38-item questionnaire containing true/false and multiple-choice questions (MCQ) that examine knowledge and attitudes regarding pain management | Lack of knowledge and training regarding pain management. Mean score: 34.1% (SD: 9.90) |
| Al Khalaileh et al. (2013)20 | Jordan | Fourth-year nursing students (n = 144) | Cross-sectional study | KASRP | Low knowledge levels of pain management. Mean score: 40% (SD: 12.75) |
| Briggs et al. (2013)21 | Australia | Final-year students: medicine (n = 176), chiropractic (n = 46), occupational therapy (n = 71), pharmacy (n = 138), physiotherapy (n = 171) | Cross-sectional study | Modified Health Care Providers Pain and Impact Relationship Scale (HC-PAIRS) – 13-item questionnaire that measures attitudes of clinicians towards patients with CLBP. Back Pain Beliefs Questionnaire (BBQ) – 14-item questionnaire that measures beliefs about consequences of future life with low back problems. Clinical vignette and questionnaire to assess likely practice behaviour | Physiotherapy and chiropractic students demonstrated more ‘helpful beliefs’ about low back pain. HC-PAIRS and BBQ scores were strongly associated with clinical recommendation scores |
| Duke et al. (2013)22 | United States | Junior and senior nursing students (n = 162) and faculty (n = 16) | Cross-sectional study | KASRP – modified | Most frequently missed items were related to knowledge about pain medications and administration. KASRP score increased with increased education, but faculty and final-year students were still below the threshold competent score of 80%. Mean score: 63% (SD: 8.78) |
| Hirsh et al. (2013)23 | United States | Medical students (n = 35) and physicians (n = 50) | Cross-sectional study | Medical Condition Regard Scale (MCRS) – 11-item measure of clinicians’ attitudes towards treating a given medical condition (chronic pain). Clinical vignettes with participants indicating likelihood to recommend 10 common pain treatments | Physicians gave higher ratings for physical therapy and lifestyle activities as treatment options compared to medical students |
| Morris et al. (2012)24 | United Kingdom | First-year (n = 202) and final-year (n = 146) medical students, and first-year (n = 62) and final-year (n = 61) business students (control group) | Cross-sectional study | Original HC-PAIRS –15 items | Improved overall attitudes towards patients with CLBP for both courses as they progressed. There was a greater change in medical students compared to business students |
| Kaki (2011)25 | Saudi Arabia | Sixth-year medical students (n = 325) | Cross-sectional study | Own instrument: 10 Qs from Weissman and Dahl,26 author wrote 8 Qs | Medical students had inadequate knowledge and a negative attitude towards cancer pain management |
| Murinson et al. (2011)27 | United States | First-year medical students (n = 118) | Intervention – 4-day pain course MCQ completed after the course only | MCQ test of pain knowledge, assessment portfolio, paired work assignment, attendance | Mean score for MCQ: 75 (SD: 11.00). Mean score for paired work: 87 (SD: 12.20). Median grade for portfolios was very good (qualitative scale: fair, good, very good and excellent). Students reported a high degree of satisfaction with the course |
| Rahimi-Madiseh et al. (2010)28 | Iran | Nursing students (n = 146) | Cross-sectional study | KASRP | No students answered >60% of the items correctly. Iranian nursing students had poor knowledge of pain management. Mean score: 37% |
| Ali and Thomson (2009)12 | United Kingdom | Final-year physiotherapy (n = 62) and medical (n = 126) students | Cross-sectional study | Own instrument: 16-item questionnaire that consulted the following: HC-PAIRS/Pain Attitudes and Beliefs Scale for Physiotherapists (PABS-PT)/Pain Knowledge Questionnaire29 | Medical students had higher scores for questions relating to chronic pain management compared to physiotherapy students. Physiotherapy students had higher overall knowledge compared to medical students |
| Stevens et al. (2009)30 | United States | Control group: 2006 second-year medical students (n = 174). Intervention group: 2007 second-year medical students (n = 159) | Cohort study – Pain Assessment and Management (PAM) Curriculum implemented during Year 2. Testing conducted at the end of Year 3 | Comprehensive Clinical Skills Examination (CCSE) – three out of the eight stations were related to pain | The intervention cohort assessed acute pain and managed terminal pain more effectively than the control cohort. PAM curriculum may have made an impact on the ability to apply a systematic approach to patients with terminal pain |
| Hunter et al. (2008)31 | Canada | Final-year medical, dentistry, pharmacy, nursing, physical therapy and occupational therapy students (n = 817 in 2007) | Intervention: Interprofessional Pain Curriculum (IPC).Pre- and post-tests of the Pain Knowledge and Beliefs Questionnaire (PKBQ) | PKBQ, Daily Content and Process Questionnaire (DCPQ), Comprehensive Pain Management Plan (CPMP) | Statistically significant improvement in PKBQ scores from 2002 to 2006. DCPQ responses indicated students highly rated the patient panel and small interprofessional group sessions |
| Manalo (2008)32 | Philippines | Fifth-year medical students (n = 50) | Cross-sectional study | Questionnaire developed by Gallagher et al.33 to assess knowledge and confidence regarding cancer pain management | Poor knowledge of cancer pain management among all the students. Mean knowledge score: 6.6/13 (SD: 2.9) |
| Niemi-Murola et al. (2007)34 | Finland | Medical students from all-year levels (n = 430) | Cross-sectional study | Own instrument: 28-item questionnaire using 6-point Likert scale. Focused on attitudes and beliefs towards pain and assessment, use of opioids for cancer pain, anxiety about seeing a pain patient and attitudes concerning treatment of chronic pain | Intervention was associated with an increased empathy towards elderly patients’ pain, increased willingness to prescribe opioids and less anxiety towards seeing a patient suffering from chronic pain |
| Chiang et al. (2006)35 | Taiwan | Nursing students (n = 181) | Intervention: Paediatric Pain Education Programme (PPEP) with pre-/post-test questionnaire | Own instrument: 35 Qs adapted from KASRP and 13 MCQs adapted from Manworren.36 Measured student nurses’ paediatric pain knowledge, attitudes and self-efficacy in managing pain | Knowledge and attitudes – pre-test scores: 20/35 and post-test scores: 32/35. Self-efficacy – Pre-test mean score: 73.37% (indicating nurses were fairly confident in assessing and managing children’s pain) and post-test mean score: 87.07% |
| Goodrich (2006)37 | United States | Nursing students and faculty (n = 10). No numbers reported for nursing students | Survey administered at beginning and end of each academic semester for 2 consecutive years. Unknown if the same sample was tested | KASRP + Open-ended questionnaire on curriculum pain content (for faculty members only) | Seniors outperformed juniors, who outperformed sophomores. There were still deficiencies in many areas of knowledge and attitudes regarding pain management. Faculty tested satisfactorily on the KASRP and perceived themselves as competent in pain management |
| Greenberger et al. (2006)38 | Israel | First-year and fourth-year nursing students, and nurses beginning or completing a certification programme (n = 1149) | Cross-sectional study | Own instrument: 20 items from KASRP with 7 items from Patient Pain Questionnaire (PPQ). Items were modified to use a 7-point Likert scale instead of T/F and MCQ to examine knowledge and attitudes to pain | Knowledge and attitude levels were positively correlated with frequency of pain care delivery. However, the more participants knew about pain and the more positive their attitudes, the less they perceived themselves able to give good pain care |
| Niemi-Murola et al. (2006)39 | Finland | Fifth-year medical students (n = 97) | Two parts:(1) Questionnaire on status of pain education with regard to the International Association for the Study of Pain (IASP) curriculum administered pre-OSCE (3 weeks) and post-OSCE (3 months);(2) OSCE | OSCE – 10 stations | Communication skills were positively correlated with self-reported clinical experience. No correlation between self-reported content knowledge of IASP curriculum and OSCE results |
| Plaisance and Logan (2006)40 | United States | Nursing students (n = 313) | Cross-sectional study | KASRP | Only 3.8% of students answered >80% correctly. Poor knowledge reflected in the low KASRP scores. Mean score: 64% |
| Sloan et al. (2004)41 | United States | Third-year medical students (n = 96), 32 students in each of the four groups | Randomised Control Trial – Group 1: control, Group 2: Self-instruction module, Group 3: self-instruction module + Cancer Pain Structured Clinical Instruction Module (SCIM), Group 4: self-instruction module + SCIM + Hospice Patient Home Visit | OSCE – four stations to assess cancer pain management skills of pain history taking, physical examination, analgesic management and communication of opioid myths (used in Sloan et al.42) | Students who received all the components of the intervention did better than those in Group 1 or 2. All three treatment groups performed better than the control group in the pain management component of the Cancer Pain OSCE |
| Watt-Watson et al. (2004)11 | Canada | Final-year medical, dentistry, pharmacy, nursing, physical therapy and occupational therapy students (n = 540) | Intervention: Interprofessional Pain Curriculum (IPC) with pre- and post-tests of PKBQ | PKBQ, DCPQ, CPMP | Statistically significant change from 66% to 83% for pain knowledge and beliefs about pain. Overall student evaluations of content and format on DCPQ were positive |
| Chiu et al. (2003)43 | Australia/Philippines | Final-year nursing students: Australia (n = 81), Philippines 1 (n = 45), Philippines 2 (n = 24) | Cross-sectional study. Results from the two universities sampled in the Philippines were amalgamated and treated as one | 30-item questionnaire – 23 factual questions aim to measure knowledge of physical signs, neurobiological mechanisms, terminology and basic management principles,29 and 7 questions related to demographic data and perceptions of pain management education | No significant group difference in overall mean scores. Common questions answered poorly included those related to complex regional pain syndrome, pharmacology and central sensitisation |
| Sloan et al. (2001)42 | United States | Third-year medical students (n = 34) | Cross-sectional study | OSCE – four stations to evaluate clinical competence in cancer pain assessment and management | Students did best on the cancer pain history taking station. Physical examination station performance was poor |
| Sloan et al. (1998)44 | United States | Final-year medical students (n = 96) | Intervention: 4-week course with lectures, small-group sessions, clinical sessions with a multidisciplinary chronic pain and acute pain service. Pre-/post-test questionnaires | Own instrument: 22-item questionnaire of attitudinal statements regarding appropriate use of morphine for cancer pain | Overall improvement in knowledge scores following course completion |
SD: standard deviation.
Results
Search results
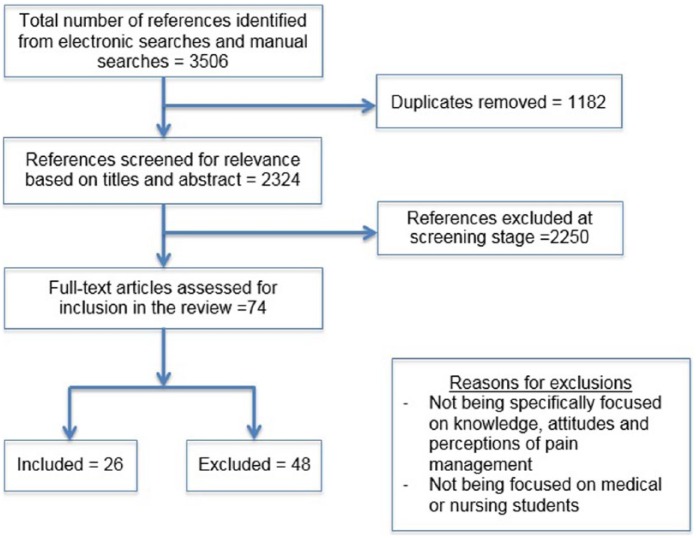
A total of 3506 citations were retrieved from the database searches. Following review of the title, abstract and full text to apply the inclusion criteria, 26 articles were selected for inclusion in the review (see Figure 1). The research was undertaken in Jordan, United States, United Kingdom, Saudi Arabia, Iran, Canada, Philippines, Finland, Taiwan, Israel and Australia. Earlier studies were conducted mainly in English-speaking countries; however, more recent studies were conducted in non-English-speaking countries (see Table 1).
Figure 1.
Flow chart showing identification of individual studies for inclusion.
Instruments
The main instrument used to assess the knowledge and attitudes was the ‘Knowledge and Attitudes Survey Regarding Pain’ (KASRP) developed by Ferrell and McCaffery in 1987.45 This tool has been used in nursing and by other health professionals and revised over the years to reflect changes in pain management practice. This instrument contains 37 close-ended questions in three different formats: (Qs 1–21) are true/false statement, (Qs 22–35) are multiple-choice options and the last two questions (Qs 36–37) are based on case studies. It examines knowledge and attitudes regarding pain management and includes aspects of pain assessment, pharmacological and non-pharmacological interventions. Of the 26 articles found, 9 articles used the KASRP or a modified version of the instrument.18–20,22,28,35,37,38,40 The instrument has internal consistency (Cronbach’s alpha = 0.70) and reliability (r = 0.80).45
Other instruments used include the Objective Structured Clinical Examination (OSCE), used in four studies.17,39,41,42 The OSCE involves stations where a student is given a scenario and asked to perform a clinical skill, for example, performing an examination or taking a pain history. The student is then marked against a set of criteria as either having achieved or not achieved the particular criterion. The Health Care Providers Pain and Impact Relationship Scale (HC-PAIRS) is another instrument used by three studies.12,21,24 HC-PAIRS is a 15-item questionnaire that measures the attitudes of clinicians towards patients with chronic lower back pain. The instrument has internal consistency (Cronbach’s alpha = 0.84), and its validity has been described as high.46
The Back Pain Beliefs Questionnaire (BBQ) was used by one of the studies.21 BBQ is a 14-item questionnaire with 5-point Likert scale statements which examines beliefs about back pain and its consequences. It has good internal consistency (Cronbach’s alpha = 0.7) and test–retest reliability (intraclass correlation coefficient (ICC): 0.87). Higher scores represent a more ‘helpful’ belief about consequences of pain.47
Different question formats like multiple-choice questions (MCQ), true/false statements and Likert scales were used among the different instruments to assess the knowledge, attitudes and perceptions regarding pain management. For example, as previously noted, the KASRP used true/false statements with MCQ, while Likert scales were used for some of the other instruments and ranged from a 3-point Likert scale32 to a 4-point,44 5-point,12 6-point23,34 and 7-point Likert scale.21,24,38
There were 10 studies that involved only nursing students,18–20,22,28,35,37,38,40,43 10 studies that involved only medical students;17,25,27,30,32,34,39,41,42,44 3 studies that compared medical students with another cohort, such as physicians,23 business students24 or physiotherapy students;12 3 studies that involved medical and nursing students with other health science disciplines;11,21,31 and 1 that included several disciplines (chiropractic, medicine, occupational therapy, pharmacy and physiotherapy students).21
The main findings from the included papers are summarised in Table 1. Despite the use of different or modified versions of the same instrument, a common finding is the poor knowledge levels among nursing and medical students, although this has improved with educational interventions or curriculum change. For example, the authors of the KASRP instrument state that an 80% score on the instrument should be the minimum acceptable level for the test45 but none of the studies reported in this review achieved this score. It is interesting to note that when full-time nursing faculty members (n = 10) were surveyed, they only achieved 71% on the KASRP.22
In view of the different instruments that were used to assess knowledge, attitudes and perceptions of pain management among medical and nursing students, comparison of results between studies is not possible. Within given studies, only two studies compared both professions along with dentistry, pharmacy, physiotherapy and occupational therapy students. Both studies were conducted in a Canadian university as part of an interprofessional pain curriculum involving the six health science faculties. Hunter et al.31 and Watt-Watson et al.11 used the Pain Knowledge and Beliefs Questionnaire (PKBQ), a 40-item instrument assessing knowledge and beliefs about pain by administering the instrument before and after an interprofessional integrated pain curriculum. The responses included true/false/don’t know, and the results were not split according to faculties but were considered together. There was a statistically significant change in correct responses from 69% to 83% in 2006 following implementation of the curriculum. From 2002 to 2006, there was a statistically significant average change of correct responses ranging from 14% to 17% following the Pain Curriculum. The authors, however, highlighted that the PKBQ needed further testing to assess its validity and reliability.
Studies that explore attitudes report them as positive versus negative. The authors of the KASRP recommend not separating items into either knowledge- or attitude-only questions, and thus, the scores are meant to reflect both knowledge and attitudes together. In the study on nursing students by Greenberger et al.,38 they found a positive association between knowledge and attitude levels, as well as an increased willingness to provide care to patients who are in pain. However, it is interesting to note that those with more positive attitudes about pain management were also less likely to perceive themselves to give good pain care.
Some studies reviewed focused on ‘pain’ generically such as chronic pain, while others focused on pain associated with certain disease process such as cancer pain. Some studies, for example, those using KASRP, focused on pain in general and did not distinguish between acute and chronic pain20,38 and used predominantly nursing students as their study participants. Other studies are more specific in the types of pain that were being assessed. For example, cancer pain,25,32,41,42,44 chronic pain23,30,34 and chronic lower back pain17,21,24 were examples of studies that focused on the management of pain in these settings, and they all involved medical students but not nursing students. The majority of studies only assessed knowledge by itself or both knowledge and attitudes. Only four studies tried to assess beliefs towards pain and its management.21,31,34,43 Contrary to the accepted biopsychosocial model for dealing with chronic pain, the focus is on therapeutics, and only a limited number of studies consider all the domains involved in pain management.
Knowledge and attitudes post-education
Eight studies included assessment and an educational intervention of various lengths and types. Two of these were related to the interprofessional Pain Curriculum, a 3.5- to 5-day programme consisting of large-group and small-group sessions with students from six health science faculties.31,43 The PKBQ scores improved after the curriculum over the 5 years it was run from 2002 until 2006, and students rated highly these small interprofessional group sessions27,31,43 that assessed pain knowledge of first-year medical students using a MCQ test following a 4-day pain course consisting of lectures, team-based learning exercises and small-group sessions. The mean score for the MCQ test was 75 (SD: 11.00, range: not reported), but there were no pre-test results to compare with as the test was only completed after the course was completed. Students did, however, report a high degree of satisfaction with the course, particularly the small-group sessions.
In the study by Stevens et al.30 conducted with medical students, a Comprehensive Clinical Skills Examination (CCSE) was used to assess pain and pain management skills following an implementation of the Pain Assessment and Management (PAM) curriculum through lectures and small-group seminars. This study found that the intervention cohort (82.8% ±3.1%) was more effective in assessing acute pain than the control cohort (66.5% ±2.9%; p < 0.001).
The study by Chiang et al.35 specifically examined paediatric pain management. Following a 4-hour Paediatric Pain Education Programme (PPEP) that involved a didactic presentation followed by interactive case-study discussions, nursing students were assessed on their knowledge and attitudes regarding paediatric pain and their self-efficacy in managing pain. Both knowledge and attitudes, and self-efficacy scores improved following this intervention.
Sloan et al.41 used OSCE to assess the effectiveness of three different educational interventions in teaching cancer pain management skills to medical students. The educational interventions included a self-instruction module, a Structured Clinical Instruction Module (SCIM) and a Hospice Patient home visit. Performance in the OSCE on cancer pain was proportionally related to the levels of student engagement with the self-instruction module. A positive relationship between knowledge and student engagement was also shown in an earlier study conducted by Sloan et al.44 with medical students. In this study, participants completed a 4-week course with lectures, small-group sessions and clinical sessions with chronic and acute pain services. Knowledge scores were tested using a 22-item questionnaire with a 4-point Likert scale and improvements were found in 10 items related to 10 aspects of pain and pain management.
Discussion
This review highlights the challenge in evaluating the literature related to pain management among medical and nursing students due to the methodical heterogeneity across these studies as reported by Carr and Watt-Watson.48 The majority of studies that involved medical students focused on a subset of pain rather than on pain in general. For example, cancer pain,28,34,35,43,44 chronic pain12,23,30,34 or chronic lower back pain17,21,24 were studied. Most of the studies were only conducted among students from one particular institution. Only one study compared students from two different countries43 and one study involved nursing students from multiple institutions from the same country.38 As noted by Briggs et al.21 cross-discipline and institutional curricula which are not aligned make it difficult to compare across disciplines or institutions, especially in the absence of an agreed national or international syllabus. Challenges with coordination, time and resources are also barriers.49
Language was described as a limitation in some of the studies where the survey instrument was translated into another language.28,35 Validity and reliability of the instrument might not have been investigated. It is unknown whether the survey instruments were adapted to cultural circumstances. The use of English instruments among participants where English is a second language may also be an influencing factor as there may be variability in participant’s understanding of the questions.19,20,25
The reporting of end-points may not always have a practical or clinical significance as it might not indicate a significant change in knowledge. For example, Sloan et al.44 reported a statistically significant improvement in knowledge scores for 10 out of 22 items. However, this was done on a 4-point Likert scale with the greatest improvement from 2.93 to 3.36. It is unclear what the implication of this change in knowledge scores is.
Despite the issues described above, some firm conclusions can be made. Overall, the studies included in this literature review show that nursing and medical students lacked satisfactory knowledge of pain management, as the majority of the students’ scores were below the acceptable level (i.e. 80% or higher KASRP scores).50 It appears that since inception in the 1990s, KASRP scores have not shown any improvement with the recommended minimum of 80% not being met in the majority of studies that have used this instrument. Effective pain management relies on good knowledge about pharmacology, a good understanding of the psychology and physiotherapy as well as pharmacology and physiology, and the ability to apply this knowledge to meeting individual patient’s needs. Despite evolving changes over the years in pain management, the studies meeting the inclusion criteria for this review (over a 20-year span) found that students’ knowledge in this area is insufficient to achieve reliable pain management for patients. Other reviews within this area have not focused on assessment tools for undergraduate students regarding pain management. For example, in the background to their survey, Briggs et al.16 conducted a review of undergraduate pain curricula in the United Kingdom. Although this review did not include assessment tools, it did find that there are limited opportunities for pain-related interprofessional learning. Gillan et al.51 looked at assessment tools for interprofessional education, but this was not related to pain. A review by Chow and Chan52 focused on pain knowledge and attitudes of nursing students found similar results.
One explanation for the low scores of the students on surveys that measure knowledge of pain management may be related to the time and the mode of delivery of the topic of pain management in nursing and medical curricula. For example, in medical education, pain management is typically taught by different disciplines. Pain management does not ‘belong’ to any one discipline and is covered in anaesthetics, palliative care, pharmacology, quality and safety and clinical skills curricula. In nursing studies, pain and pain management are often addressed across different nursing subjects, often, only as a component of the particular nursing subject, for example, in a pathophysiology or nursing therapeutics subject. This fragmentation and multidisciplinary format not only makes a literature search more complex but may lead to gaps in student knowledge as students have to integrate knowledge across different modules. Briggs et al.16 commented that the lack of a formal pain curriculum inhibits planned stepwise examination of topic through comprehensive assessment strategies. Another issue with evaluating pain education is that clinical placements account for a large proportion of learning for certain courses with the experience differing for each student. As previously mentioned, although the benefits of interprofessional learning are well recognised,10,49 its implementation in practice requires time and resources. Carr and Watt-Watson48 suggested that since pain management frequently requires healthcare professionals to work together as part of a team, educational preparation and teaching should afford them the opportunity to work and learn together. Interprofessional education may help to build effective professional relationships and, improve health outcomes and patient care.53,54
Delivered within a biopsychosocial framework well integrated and coordinated, interdisciplinary management of pain has been shown to be effective.10,55 Nevertheless, achieving success and long-term sustainability of embedding interprofessional education in health professional curricula remains elusive, as it requires commitment and acceptance from the students, faculty, institutions, accreditation agencies, government and professional bodies.56
Healthcare professionals need to be able to work together to manage pain effectively. Pain management is complex and goes beyond analgesic prescribing and administration for medical and nursing personnel. While pharmacological knowledge and prescribing preparedness are important, it is important to have a thorough knowledge of pain and be able to establish pre-emptive pain management strategies to ensure patients are not being undertreated.
A recent review of interprofessional education studies by Gillan et al.51 compared evaluation outcome measures against a modified version of the Kirkpatrick model (Table 2). The authors found that most of the articles only tested the first two levels of the Kirkpatrick model, Reaction (satisfaction) and Learning (impact on knowledge and attitudes). No articles found in that paper attempted to evaluate the outcome or benefit towards patients, the highest level in the Kirkpatrick model.51 Future studies should focus on evaluating the outcomes and benefits to patients that may come from educational interventions.
Table 2.
Kirkpatrick model.a
| Level 1 | Reaction – the degree to which participants react favourably to the education (satisfaction). |
| Level 2 | Learning – the degree to which participants acquire the intended knowledge, skills, attitudes, confidence and commitment based on their participation. |
| Level 3 | Behaviour – the degree to which participants apply what they learned during the education when they are back on the job. |
| Level 4 | Results – the degree to which specific outcomes occur as a result of the education event and subsequent reinforcement. |
Source: Adapted from Watt-Watson et al.11
One of a number of models that can be used to guide the evaluation of education for healthcare professionals.
The studies identified in this review were all quantitative studies. Qualitative studies can provide more in-depth understanding of the perceptions and attitudes towards pain management. Also, this methodology could help identify what factors and why and how these factors influence the knowledge, perceptions and attitudes of medical and nursing students towards pain management.
It is important to focus on education to improve knowledge, but ultimately a broader change is needed in the clinical culture including changing attitudes to high-quality pain management.48 There needs to be interest not only from pain specialists but also from all healthcare professionals including general practitioners, nurses, pharmacists and physiotherapists. High-quality pain management should be viewed by healthcare professionals as being important, expected and attainable. As noted by Ellis et al.,57 this should lead to a climate where healthcare professionals, patients and policy makers are able to ‘campaign for the policy and social environment where knowledge becomes practice, skills become habit and excellence becomes the norm’.
Limitations
This review only included articles that were published in English with search terms and the scope also being limitations. This review only included medical and nursing professions, and future work should consider the inclusion of other allied health professionals as they are involved in pain management. Notwithstanding, to our knowledge, this is the first review of its kind in this area and thus provides a useful base for future research.
Conclusion
There is no gold standard instrument currently used to assess knowledge, perceptions and attitudes to pain management. The results of this review showed, despite the diversity of standardised instruments that have been used to assess knowledge, perceptions and attitude to pain management, the literature has consistently reported that knowledge about pain management among nursing and medical students was generally poor among both groups. It is only through an appropriate evaluation strategy that we can be certain that pain education has really made a difference to healthcare professionals and, most importantly, to the patients. Future research should focus on how improved pain management level translates into better patient outcomes, making the transition of knowledge acquired during training and the application of this knowledge in practice.
Acknowledgments
The authors would like to thank Professor Christopher Fowler for his helpful comments on an earlier version of the manuscript.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Andrew Ung was supported by a University of Western Sydney Summer Scholarship.
References
- 1. Goldberg D, McGee S. Pain as a global public health priority. BMC Public Health 2011; 11: 770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brennan F, Carr DB, Cousins M. Pain management: a fundamental human right. Anesth Analg 2007; 105: 205–221. [DOI] [PubMed] [Google Scholar]
- 3. Institute of Medicine Report from the Committee on Advancing Pain Research, Care, and Education. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: The National Academies Press, 2011. [PubMed] [Google Scholar]
- 4. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006; 10: 287–333. [DOI] [PubMed] [Google Scholar]
- 5. Pain Australia. National pain strategy: pain management for all Australians. Tamarama, NSW: Pain Australia, 2010, 96 pp. [Google Scholar]
- 6. Blyth FM, March LM, Brnabic AJM, et al. Chronic pain in Australia: a prevalence study. Pain 2001; 89: 127–134. [DOI] [PubMed] [Google Scholar]
- 7. Mäntyselkä P, Kumpusalo E, Ahonen R, et al. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain 2001; 89: 175–180. [DOI] [PubMed] [Google Scholar]
- 8. Ospina MB, Taenzer P, Rashiq S, et al. A systematic review of the effectiveness of knowledge translation interventions for chronic noncancer pain management. Pain Res Manag 2013; 18: e129–e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. International Pain Summit of the International Association for the Study of Pain. Declaration of Montréal: declaration that access to pain management is a fundamental human right. J Pain Palliat Care Pharmacother 2011; 25: 29–31. [DOI] [PubMed] [Google Scholar]
- 10. Gatchel RJ, McGeary DD, McGeary CA, et al. Interdisciplinary chronic pain management: past, present, and future. Am Psychol 2014; 69: 119–130. [DOI] [PubMed] [Google Scholar]
- 11. Watt-Watson J, Hunter J, Pennefather P, et al. An integrated undergraduate pain curriculum, based on IASP curricula, for six health science faculties. Pain 2004; 110: 140–148. [DOI] [PubMed] [Google Scholar]
- 12. Ali N, Thomson D. A comparison of the knowledge of chronic pain and its management between final year physiotherapy and medical students. Eur J Pain 2009; 13: 38–50. [DOI] [PubMed] [Google Scholar]
- 13. Schreiner U, Haefner A, Gologan R, et al. Effective teaching modifies medical student attitudes toward pain symptoms. Eur J Trauma Emerg Surg 2011; 37: 655–659. [DOI] [PubMed] [Google Scholar]
- 14. Murinson BB, Gordin V, Flynn S, et al. Medical Student Education Sub-committee of the American Academy of Pain Medicine. Recommendations for a new curriculum in pain medicine for medical students: toward a career distinguished by competence and compassion. Pain Med 2013; 14: 345–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brunier G, Carson G, Harrison DE. What do nurses know and believe about patients with pain? Results of a hospital survey. J Pain Symptom Manage 1995; 10: 436–445. [DOI] [PubMed] [Google Scholar]
- 16. Briggs EV, Carr EC, Whittaker MS. Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom. Eur J Pain 2011; 15: 789–795. [DOI] [PubMed] [Google Scholar]
- 17. Weiner DK, Morone NE, Spallek H, et al. University of Pittsburgh Center of Excellence in Pain Education. E-learning module on chronic low back pain in older adults: evidence of effect on medical student objective structured clinical examination performance. J Am Geriatr Soc 2014; 62: 1161–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Owens D, Smith J, Jonas D. Evaluating students’ knowledge of child pain and its management after attending a bespoke course. Nurs Child Young People 2014; 26: 34–40. [DOI] [PubMed] [Google Scholar]
- 19. Al-Khawaldeh OA, Al-Hussami M, Darawad M. Knowledge and attitudes regarding pain management among Jordanian nursing students. Nurse Educ Today 2013; 33: 339–345. [DOI] [PubMed] [Google Scholar]
- 20. Al Khalaileh M, Al Qadire M. Pain management in Jordan: nursing students’ knowledge and attitude. Br J Nurs 2013; 22: 1234–1240. [DOI] [PubMed] [Google Scholar]
- 21. Briggs AM, Slater H, Smith AJ, et al. Low back pain-related beliefs and likely practice behaviours among final-year cross-discipline health students. Eur J Pain 2013; 17: 766–775. [DOI] [PubMed] [Google Scholar]
- 22. Duke G, Haas BK, Yarbrough S, et al. Pain management knowledge and attitudes of baccalaureate nursing students and faculty. Pain Manag Nurs 2013; 14: 11–19. [DOI] [PubMed] [Google Scholar]
- 23. Hirsh AT, Hollingshead NA, Bair MJ, et al. Preferences, experience, and attitudes in the management of chronic pain and depression: a comparison of physicians and medical students. Clin J Pain 2014; 30: 766–774. [DOI] [PubMed] [Google Scholar]
- 24. Morris H, Ryan C, Lauchlan D, et al. Do medical student attitudes towards patients with chronic low back pain improve during training? A cross-sectional study. BMC Med Educ 2012; 12: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kaki AM. Medical students’ knowledge and attitude toward cancer pain management in Saudi Arabia. Saudi Med J 2011; 32: 628–632. [PubMed] [Google Scholar]
- 26. Weissman DE, Dahl JL. Attitudes about cancer pain: a survey of Wisconsin’s first-year medical students. J Pain Symptom Manage 1990; 5: 345–349. [DOI] [PubMed] [Google Scholar]
- 27. Murinson BB, Nenortas E, Mayer RS, et al. A new program in pain medicine for medical students: integrating core curriculum knowledge with emotional and reflective development. Pain Med 2011; 12: 186–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rahimi-Madiseh M, Tavakol M, Dennick R. A quantitative study of Iranian nursing students’ knowledge and attitudes towards pain: implication for education. Int J Nurs Pract 2010; 16: 478–483. [DOI] [PubMed] [Google Scholar]
- 29. Trinca J. Knowledge of pain mechanisms and management in recent medical graduates. Sydney, NSW, Australia: University of Sydney, 1998. [Google Scholar]
- 30. Stevens DL, King D, Laponis R, et al. Medical students retain pain assessment and management skills long after an experiential curriculum: a controlled study. Pain 2009; 145: 319–324. [DOI] [PubMed] [Google Scholar]
- 31. Hunter J, Watt-Watson J, McGillion M, et al. An interfaculty pain curriculum: lessons learned from six years experience. Pain 2008; 140: 74–86. [DOI] [PubMed] [Google Scholar]
- 32. Manalo MFC. Knowledge toward cancer pain and the use of opioid analgesics among medical students in their integrated clinical clerkship. Palliat Care 2008; 2: 9. [Google Scholar]
- 33. Gallagher R, Hawley P, Yeomans W. A survey of cancer pain management knowledge and attitudes of British Columbian physicians. Pain Res Manag 2004; 9: 188–194. [DOI] [PubMed] [Google Scholar]
- 34. Niemi-Murola L, Nieminen JT, Kalso E, et al. Medical undergraduate students’ beliefs and attitudes toward pain: how do they mature? Eur J Pain 2007; 11: 700–706. [DOI] [PubMed] [Google Scholar]
- 35. Chiang L-C, Chen H-J, Huang L. Student nurses’ knowledge, attitudes, and self-efficacy of children’s pain management: evaluation of an education program in Taiwan. J Pain Symptom Manage 2006; 32: 82–89. [DOI] [PubMed] [Google Scholar]
- 36. Manworren RC. Pediatric nurses’ knowledge and attitudes survey regarding pain. Pediatr Nurs 2000; 26: 610–614. [PubMed] [Google Scholar]
- 37. Goodrich C. Students’ and faculty members’ knowledge and attitudes regarding pain management: a descriptive survey. J Nurs Educ 2006; 45: 140–142. [DOI] [PubMed] [Google Scholar]
- 38. Greenberger C, Reches H, Riba S. Levels and predictors of knowledge and attitudes regarding pain among Israeli baccalaureate nursing students and nurses pursuing specialty certification. Int J Nurs Educ Scholarsh 2006; 3: Article 8. [DOI] [PubMed] [Google Scholar]
- 39. Niemi-Murola L, Pirkko H, Eeva P, et al. Training medical students to manage a chronic pain patient: both knowledge and communication skills are needed. Eur J Pain 2006; 10: 167–170. [DOI] [PubMed] [Google Scholar]
- 40. Plaisance L, Logan C. Nursing students’ knowledge and attitudes regarding pain. Pain Manag Nurs 2006; 7: 167–175. [DOI] [PubMed] [Google Scholar]
- 41. Sloan PA, Plymale M, LaFountain P, et al. Equipping medical students to manage cancer pain: a comparison of three educational methods. J Pain Symptom Manage 2004; 27: 333–342. [DOI] [PubMed] [Google Scholar]
- 42. Sloan PA, Plymale MA, Johnson M, et al. Cancer pain management skills among medical students: the development of a cancer pain objective structured clinical examination. J Pain Symptom Manage 2001; 21: 298–306. [DOI] [PubMed] [Google Scholar]
- 43. Chiu LH, Trinca J, Lim LM, et al. A study to evaluate the pain knowledge of two sub-populations of final year nursing students: Australia and Philippines. J Adv Nurs 2003; 41: 99–108. [DOI] [PubMed] [Google Scholar]
- 44. Sloan PA, Montgomery C, Musick D. Medical student knowledge of morphine for the management of cancer pain. J Pain Symptom Manage 1998; 15: 359–364. [DOI] [PubMed] [Google Scholar]
- 45. Ferrell B, McCaffery M. Knowledge and attitudes survey regarding pain, http://prc.coh.org/ (accessed 7 December 2013).
- 46. Houben RM, Gijsen A, Peterson J, et al. Do health care providers’ attitudes towards back pain predict their treatment recommendations? Differential predictive validity of implicit and explicit attitude measures. Pain 2005; 114: 491–498. [DOI] [PubMed] [Google Scholar]
- 47. Symonds TL, Burton AK, Tillotson KM, et al. Absence resulting from low back trouble can be reduced by psychosocial intervention at the work place. Spine 1995; 20: 2738–2745. [DOI] [PubMed] [Google Scholar]
- 48. Carr E and Watt-Watson J. Interprofessional pain education: definitions, exemplars and future directions. Br J Pain 2012; 6: 59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hadjistavropoulos HD, Juckes K, Dirkse D, et al. Student evaluations of an interprofessional education experience in pain management. J Interprof Care 2015; 29: 73–75. [DOI] [PubMed] [Google Scholar]
- 50. Brown ST, Bowman JM, Eason FR. Assessment of nurses’ attitudes and knowledge regarding pain management. J Contin Educ Nurs 1999; 30: 132–139. [DOI] [PubMed] [Google Scholar]
- 51. Gillan C, Lovrics E, Halpern E, et al. The evaluation of learner outcomes in interprofessional continuing education: a literature review and an analysis of survey instruments. Med Teach 2011; 33: e461. [DOI] [PubMed] [Google Scholar]
- 52. Chow KM, Chan JC. Pain knowledge and attitudes of nursing students: a literature review. Nurse Educ Today 2015; 35: 366–372. [DOI] [PubMed] [Google Scholar]
- 53. Gallagher RM, Gallagher HC. Improving the working relationship between doctors and pharmacists: is inter-professional education the answer? Adv Health Sci Educ Theory Pract 2012; 17: 247–257. [DOI] [PubMed] [Google Scholar]
- 54. Cunningham FC, Ranmuthugala G, Plumb J, et al. Health professional networks as a vector for improving healthcare quality and safety: a systematic review. BMJ Qual Saf 2012; 21: 239–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Koes BW, van Tulder M, Lin CW, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010; 19: 2075–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lawlis TR, Anson J, Greenfield D. Barriers and enablers that influence sustainable interprofessional education: a literature review. J Interprof Care 2014; 28: 305–310. [DOI] [PubMed] [Google Scholar]
- 57. Ellis B, Johnson M, Taylor A. Education as part of wider health policy and improvement strategies. Br J Pain 2012; 6: 54–58. [DOI] [PMC free article] [PubMed] [Google Scholar]