Abstract
This study aimed to investigate the impact of a brief psychologically informed physiotherapy training (PIPT) course on physiotherapists’ attitudes and beliefs towards working with people with chronic pain. Specifically, the training aimed to help the participants better recognise the role of psychosocial factors in chronic pain and to better target the key processes of the psychological flexibility (PF) model in their treatment interactions. A total of 26 physiotherapists working in an outpatient musculoskeletal (MSK) department participated in the 7-hour training session. A total of 25 participants completed self-report questionnaires on attitudes and beliefs, burnout and PF-relevant processes pre- and post-training. The pre- and post-measures were completed on the day of training. PIPT was associated with significant changes in the expected direction in physiotherapists’ attitudes towards treatment of people with chronic pain, including a moderate effect size on the Health Care Provider–Pain and Impairment Relationship Scale (HC-PAIRS) (decreased biomedical scores) and a large effect size on the Pain Attitudes and Beliefs Scale for Physiotherapists (PABS-PT) (increased biopsychosocial scores and decreased biomedical scores). In conclusion, brief PIPT could help physiotherapists working in non-specialist centres with complex patients, many of whom present with significant emotional distress and pain-related disability. Further research is required to determine whether the changes in attitudes detected in this study translate into clinical practice and whether changes are maintained over a follow-up period.
Keywords: Psychological flexibility, physiotherapy, chronic pain, Acceptance and Commitment Therapy, training
Introduction
Pain that persists longer than expected can be difficult to treat. While a small proportion of patients with chronic pain are referred to specialist multidisciplinary pain services, the majority are treated in secondary care.1 Indeed, pain is the main symptom reported by patients presenting to musculoskeletal (MSK) physiotherapy departments.2 It has been recognised for many years that such patients may present with significant emotional distress including anger, fear and depression as well as pain-related disability and require a physical and psychological approach to treatment.3,4 However, most MSK services in the United Kingdom do not include direct access to a multidisciplinary team (MDT) approach although it is clear that chronic pain is associated with psychological and social complexities in many if not most cases.4 Indeed, 51% of pain patients report anxiety or depression at referral.4 For these reasons, it is important that physiotherapists within MSK services are provided with skills to address some of the psychosocial needs that accompany chronic pain.
A biomedical disease model of pain and disability with its focus on tissue pathology can lead to treatment aimed at finding and treating specific biological causes of pain. A biopsychosocial approach recognises that pain does not have to be a sign of pathology, that disability can be maintained long after the initial pathology has healed and that pain is influenced by social and psychological factors as well as by biological ones. Adopting a biopsychosocial orientation is widely accepted as the best approach to the management of non-specific low back pain.3,5 Such treatment focuses on a return to function, rather than pain reduction.6 Although Health Care Professionals’ (HCPs’) attitudes and beliefs are rarely in the extreme of either approach,7 studies suggest that physiotherapists with a more biomedical orientation are more likely to view daily activity as harmful and to limit activities for chronic pain patients compared to those with a more biopsychosocial orientation.6 These attitudes have been shown to be associated with physiotherapists’ clinical decision making and to affect the advice they provide to patients.8,9 Several studies have shown that training can change therapists’ attitudes, beliefs and practices towards people with chronic pain.3,10,11
For many years, Cognitive Behavioural Therapy (CBT) principles have been incorporated into many physiotherapists’ practice as part of their biopsychosocial approach to treating chronic pain.3,12,13 More recently, a form of CBT called Contextual CBT or Acceptance and Commitment Therapy (ACT) is being increasingly used in specialist MDT pain centres and has a growing evidence base in chronic pain.14–16 ACT is a clinical application of the psychological flexibility (PF) model. Put simply, the approach teaches people skills in engaging in goal-directed actions in the presence of ongoing pain. This is achieved by increasing PF. PF refers to the capacity for actions to be guided by values and goals, rather than thoughts, feelings and sensations, and is sometimes referred to as reflecting behaviour that is ‘open, aware and active’.15,17,18 The model incorporates six interrelated processes that are targeted in treatment to increase PF: acceptance, cognitive defusion, present moment awareness, self as context, values and committed action.17 As an example, patients learn to be more open to unpleasant sensations, including pain, thoughts, emotions and memories while doing such things as physical activities, a process called acceptance. They also learn new ways to respond to thoughts such as ‘I’m damaging myself’ so that these thoughts are a less dominant influence on their behaviour, a process called cognitive defusion. In turn, acceptance and cognitive defusion skills can help patients engage in activities that serve their goals and desires in life, a process called values-based action. Further description of each of these processes is beyond the scope of the present article; McCracken and Vowles19 give a useful overview. In summary, the PF model is an application of the biopsychosocial approach to chronic pain and represents an opportunity for physiotherapists to further develop their skills.
As well as having an evidence base in patient populations, there is evidence for the benefits of these PF-based skills in clinicians too in terms of (1) their own wellbeing and (2) their treatment delivery. As such, addressing PF in clinicians themselves is relevant and important. McCracken and Yang20 showed that processes of acceptance, mindfulness and values-based action in rehabilitation workers (including physiotherapists) appear positively associated with their health and functioning. This is relevant to this study because MSK outpatient settings can be demanding and stressful and workers in such settings can be at risk of emotional exhaustion and burnout.20 Two studies21,22 have demonstrated that burnout symptoms among HCPs can be reduced using a brief intervention consistent with PF. Similarly, Bond and Bunce23 demonstrated that brief (3 half days) training sessions based on the PF model were effective in the management of worksite stress. Preliminary results from McCracken and Yang’s20 study suggest that HCPs’ own acceptance and PF are relevant to how they respond to patients showing suffering and distress when they might be feeling helpless or powerless as a practitioner.20 Working with people in pain and distress, and sometimes feeling unable to change this, is of course relevant to HCPs working with people with chronic pain. For example, it can feel more comfortable to send a patient for a repeat X-ray than to be open to the discomfort that accompanies discussing with the patient that more investigations and interventions may not help the pain to resolve. In another study,24 attending a 1-day ACT workshop was demonstrated to be associated with changes in drug and alcohol counsellors’ clinical practice post-workshop. Taking these studies together, it is plausible to suggest that a brief PF workshop may have benefits for clinician wellbeing, as well as their clinical practice.
The purpose of this study was to examine the impact of brief psychologically informed physiotherapy training (PIPT) designed to increase knowledge and competence of physiotherapists working with people with chronic pain. Specifically, the training aimed to help them better recognise the role of psychosocial factors in chronic pain and to better incorporate the key processes of PF in their treatment interactions. This study also aimed to investigate levels of burnout and acceptance among the physiotherapists attending training and to assess whether a brief PIPT experience can serve to enhance PF/acceptance in therapists themselves and potentially impact their own wellbeing.
Method
Participants
A total of 26 physiotherapists working in an MSK service within an outpatient physiotherapy department participated in the training. The training was offered as part of the department’s in-service training programme. Mean age of participants was 34.88 years (standard deviation (SD): 10.22). In all, 84.6% were female and 15.4% were male. Ethnic background was 76.9% White, 3.8% Bangladeshi, 3.8% Black African, 3.8% Indian and 11.5% ‘other’. Average year of education was 17.27 years (SD: 2.29), with 34.6% of participants having postgraduate education in pain. Average number of years spent working in health care was 11.44 years (SD: 9.94). A total of 76.9% were working full-time and 23.1% part-time, with 30.23 (SD: 7.55) being the average number of hours of patient contact per week. Job bandings were as follows: 23.1% band 5, 23.1% band 6, 30.8% band 7 and 23.1% band 8.
Training content
Two physiotherapists and a psychologist from INPUT Pain Management Unit, a specialist pain unit at St Thomas’ Hospital, London, delivered the single 7-hour PIPT session. The training day had been piloted with a different group of participants previously. The training was designed to be clinically relevant for MSK physiotherapists and to provide them skills in treatment methods consistent with the PF model that could be applied in individual and group treatment. The aim was not to train the physiotherapists to be psychologists as such, but rather to provide them a selected set of skills that were deemed to fall within the potential range of usual practice for the profession. The training was interactive and included experiential learning and a question and answer session. The following was covered during the training:
Recognition of barriers to engagement in activity with pain (examples of barriers are anxiety and fear of increased pain). This was done experientially, with participants exploring movements in anxiety-inducing mock-up scenarios.
Flexible and targeted use of pain education. The ways in which education about chronic pain can be used to facilitate PF and goal engagement were discussed. Caveats were highlighted (e.g. when education feeds into avoidance and cognitive fusion). Methods and metaphors for effective education about chronic pain were shared.
The majority of the day was devoted to skills training for applying methods that target the core PF processes of values, acceptance, contact with the present moment, cognitive defusion and committed action. For example, participants were introduced to mindful movement which includes the core processes of acceptance, contact with the present moment and defusion. Participants were invited to explore some movements, becoming aware of the sensations, thoughts, emotions, urges, memories and so on that occurred as they did so. Participants were guided to allow or ‘make room for’ these experiences, including unpleasant ones, with curiosity and without attempting to change them.
Measures and analysis
Participants completed self-report measures before and after the training, on the same day. Later, paired t-tests on pre- and post-training session scores were carried out of the following questionnaires.
Health Care Provider–Pain and Impairment Relationship Scale
This questionnaire measures HCPs’ beliefs about the relationship between low back pain and function.25,26 Example items are ‘All of chronic back pain patients’ problems would be solved if their pain would go away’ and ‘Chronic back pain patients cannot go about normal life activities when they are in pain’. In the version used in this study,25 items are rated on a 6-point scale (totally disagree to totally agree). Three items are reverse scored. Higher scores indicate a stronger belief that pain and disability are directly associated and that disability and avoidance of activities are inevitable consequences of pain. The scale was developed in the United States and adequate psychometric properties have been demonstrated in US26,27 and Dutch25 samples. The Health Care Provider–Pain and Impairment Relationship Scale (HC-PAIRS) was used with physiotherapy students,28 and the authors suggest it is sensitive to change; students’ scores on the measure changed following a teaching module on chronic pain (although the number of students followed up was limited).
Pain Attitudes and Beliefs Scale for Physiotherapists
This questionnaire measures treatment orientation towards care of patients with low back pain.6,7 In the revised version used in this study,6 19 items are rated on a 6-point rating scale (totally disagree to totally agree). There are two subscales: biomedical (example item: back pain indicates the presence of organic injury) and biopsychosocial or ‘behavioural’ (example item: functional limitations associated with back pain are the result of psychosocial factors). Higher scores on each subscale indicate greater endorsement of that treatment orientation. The Pain Attitudes and Beliefs Scale for Physiotherapists (PABS-PT) was developed in the Netherlands. Its psychometric properties have been assessed6,7 and the measure has been used to explore the link between attitudes and treatment recommendations,6 including in physiotherapy students.29
Acceptance and Action Questionnaire
This questionnaire measures general psychological acceptance or experiential avoidance, depending on the direction in which the scores are interpreted.30 It essentially reflects the degree to which an individual is willing to remain in contact with private experiences (including thoughts and feelings), without trying to avoid or alter these experiences. Items include ‘I worry about not being able to control my worries and feelings’ and ‘I’m afraid of my feelings’. Each of the seven items is scored on a scale from 1 (never true) to 7 (always true), and scores are summed to give an overall score. In this study, higher scores indicate greater experiential avoidance or psychological inflexibility and lower scores indicate greater acceptance and PF. The measure has sound psychometric properties.30 The Acceptance and Action Questionnaire-II (AAQ-II) and an earlier version (AAQ31) have been used in studies of workplace wellbeing and burnout,32 including in HCPs,20,22 and to examine the effects of a brief ACT training session on clinical practice.24
Maslach Burnout Inventory
Three questions on aspects of burnout, based on items from the Maslach Burnout Inventory, were asked.33 These three questions were previously used in a study of rehabilitation workers by McCracken and Yang.20 The items are ‘I feel emotionally drained from my work’, ‘I feel I’m positively influencing other people’s lives through my work’ and ‘I feel I treat some patients as if they were impersonal “objects”’. Participants respond on a 0 (never) to 10 (all of the time) rating scale. As in McCracken and Yang’s20 study, the items were not summed.
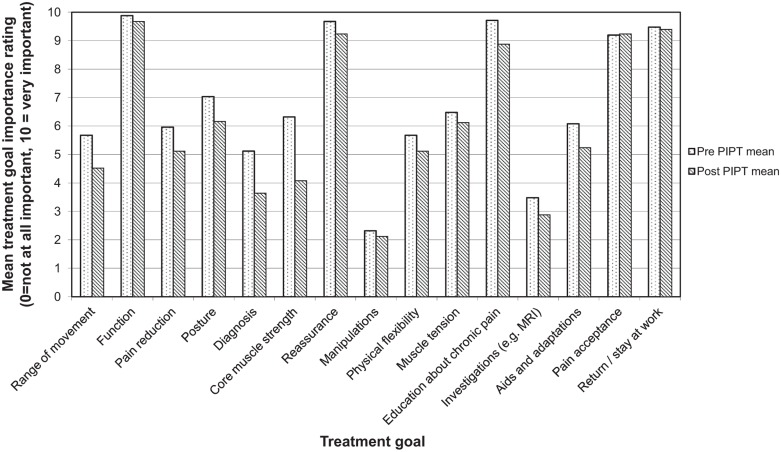
In addition, independently devised questions rating the importance of several treatment goals when working with chronic pain patients were asked. Examples of treatment goals include pain reduction and function. Participants were asked to rate the importance of each treatment goal on a scale of 0 (not important) to 10 (very important). Finally, participants were asked an open question, ‘What makes it hard to achieve treatment goals with chronic pain patients?’, to examine some of the barriers identified by physiotherapists to working effectively with chronic pain patients.
Results
Pre- and post-training measures were completed for 25 participants due to one person leaving the training day early. See Table 1 for means, standard deviations and effect sizes. HC-PAIRS scores demonstrated statistically significant reductions between pre-training and post-training, in the expected direction with a moderate effect size. PABS-PT scores demonstrated statistically significant changes between pre-training and post-training scores, in the expected direction with large effect sizes; biopsychosocial scores significantly increased and biomedical scores significantly decreased between pre-training and post-training. There were no statistically significant differences on the AAQ-II between pre- and post-training or on the Maslach Burnout Inventory items.
Table 1.
Mean scores (standard deviations) pre- and post-PIPT.
| Measure | Pre-PIPT mean (SD) | Post-PIPT mean (SD) | t | p | Effect size (d) |
|---|---|---|---|---|---|
| HC-PAIRS | 31.72 (5.49) | 27.6 (6.49) | 2.798 | 0.010* | 0.75 |
| PABS-PT (biomedical subscale) | 26.84 (5.31) | 21.92 (5.93) | 4.954 | 0.000* | 0.93 |
| PABS-PT (biopsychosocial subscale) | 36.72 (4.72) | 40.92 (3.94) | −4.706 | 0.000* | 0.89 |
| AAQ-II | 16.68 (7.92) | 17.52 (8.64) | −1.610 | 0.121 | 0.11 |
| Maslach Burnout Inventory Item 1 | 5.28 (2.07) | 4.96 (2.13) | 1.317 | 0.200 | 0.15 |
| Maslach Burnout Inventory Item 2 | 6.80 (1.94) | 7.28 (1.59) | −1.423 | 0.168 | 0.25 |
| Maslach Burnout Inventory Item 3 | 1.52 (1.39) | 1.56 (1.61) | −0.214 | 0.832 | 0.03 |
PIPT: psychologically informed physiotherapy training; SD: standard deviation; HC-PAIRS: Health Care Provider–Pain and Impairment Relationship Scale; PABS-PT: Pain Attitudes and Beliefs Scale for Physiotherapists; AAQ-II: Acceptance and Action Questionnaire-II.
Statistically significant change (p < 0.05).
Independently devised questions identified the relative importance of different treatment goals and showed some treatment priorities changed following PIPT (see Table 2 and Figure 1). Specifically, importance ratings dropped significantly for range of movement, posture, diagnosis, core muscle strength, reassurance, education about chronic pain and aids and adaptations.
Table 2.
Treatment goals pre- and post-PIPT (N = 25).
| Treatment goal | Pre-PIPT mean (SD) | Post-PIPT mean (SD) | t | p | Effect size (d) |
|---|---|---|---|---|---|
| Range of movement | 5.68 (2.08) | 4.52 (2.22) | 2.910 | 0.008* | 0.56 |
| Function | 9.88 (0.33) | 9.68 (0.69) | 1.414 | 0.170 | 0.61 |
| Pain reduction | 5.96 (2.51) | 5.12 (2.35) | 1.899 | 0.070 | 0.33 |
| Posture | 7.04 (2.44) | 6.16 (2.46) | 2.916 | 0.008* | 0.36 |
| Diagnosis | 5.12 (3.23) | 3.64 (2.10) | 3.334 | 0.003* | 0.46 |
| Core muscle strength | 6.32 (2.67) | 4.08 (2.47) | 5.315 | 0.000* | 0.84 |
| Reassurance | 9.68 (0.69) | 9.24 (1.09) | 2.400 | 0.024* | 0.64 |
| Manipulations | 2.32 (2.14) | 2.12 (1.92) | 0.679 | 0.503 | 0.09 |
| Physical flexibility | 5.68 (1.70) | 5.12 (2.33) | 1.241 | 0.227 | 0.33 |
| Muscle tension | 6.48 (1.87) | 6.12 (2.37) | 1.000 | 0.327 | 0.19 |
| Education about chronic pain | 9.72 (0.68) | 8.88 (1.51) | 2.765 | 0.011* | 1.24 |
| Investigations (e.g. MRI) | 3.48 (2.65) | 2.88 (2.28) | 1.643 | 0.113 | 0.23 |
| Aids and adaptations | 6.08 (2.29) | 5.24 (2.67) | 2.545 | 0.018* | 0.37 |
| Pain acceptance | 9.20 (1.08) | 9.24 (0.97) | −0.153 | 0.880 | −0.04 |
| Return/stay at work | 9.48 (0.92) | 9.40 (0.91) | 0.359 | 0.723 | 0.09 |
PIPT: psychologically informed physiotherapy training; SD: standard deviation; MRI: magnetic resonance imaging.
Statistically significant change (p < 0.05).
Figure 1.
Mean treatment goal importance ratings pre- and post-PIPT.
Ratings of the importance of pain reduction reduced, but this was not quite statistically significant. Function, pain acceptance and return to work were identified as highly important treatment goals at both time points; their importance ratings did not change significantly post-PIPT.
Responses to the question ‘What makes it hard to achieve treatment goals with chronic pain patients?’ included lack of acceptance of pain, psychosocial issues (including stress and family situations), patients’ poor understanding of chronic pain and the role of investigations, patients’ unrealistic goals, organisational pressures and clinicians’ lack of training and experience. Lack of acceptance of pain was the most commonly cited response followed by patients’ expectations from physiotherapy treatment.
Discussion
This study demonstrates that brief psychologically informed training is associated with changes (in a biopsychosocial direction) in physiotherapists’ attitudes and beliefs towards treatment of chronic pain patients. Specifically, HC-PAIRS scores demonstrated statistically significant reductions at post-training, in the expected direction, with a moderate effect size. PABS-PT scores demonstrated statistically significant changes at post-training, in the expected direction, with large effect sizes; biopsychosocial scores significantly increased and biomedical scores significantly decreased. Consistent with this shift, some treatment goal importance ratings (e.g. for diagnosis and posture) decreased significantly post-training. Taken together, these results indicate that, after the training, the physiotherapists were less likely to assume disability is an inevitable consequence of pain and that treatment should aim at pain reduction. This is consistent with previous research that attitudes and beliefs can be altered by education and training.28
Several studies have demonstrated that HCPs’ attitudes are associated with the treatment recommendations they make to patients6,29 and that brief training can change both.10 As such, it is plausible to suggest that the changes detected in this study may translate to changes in clinical practice, away from the training environment. However, further follow-up would be necessary to ascertain this.
This brief training is relevant in the current climate where most patients with chronic pain will not be referred to specialist pain centres. Physiotherapists frequently work with patients who are distressed or fearful, without the benefit of the MDT and as such need to be skilled in a biopsychosocial approach to treatment. The style and methods taught are highly applicable in a busy MSK setting where physiotherapists face considerable time and resource constraints. For example, approaching movement with a patient using acceptance processes does not take longer than a routine exercise programme. Equally, focusing on activities in a fashion that is linked to values can be easily incorporated into physiotherapists’ existing skill-set and complements the goal-setting work they already do.
Although other brief training studies have shown changes on measures of PF/acceptance and burnout, the present study did not show changes post-training on these measures. One explanation may be that the period between the pre- and post-measures was too short to show changes. For example, it is arguable that shifts in response to the question ‘I feel I treat some patients as if they are impersonal “objects”’ would only happen after spending time with patients, away from the training environment. Further research could investigate whether burnout and AAQ-II scores change after a follow-up period back in the clinical environment and/or whether these could be more successfully targeted by future training.
This study has several limitations. First and foremost, no assessment was made of the translation of changes in attitudes into changes in clinical practice. Related to this, measures were taken on the day of training and it is unclear whether these would be maintained over a longer period. Second, there was no control group (i.e. a group who did not receive PIPT) and no random allocation; therefore, we cannot directly attribute changes to the PIPT. At the same time, this research design seems appropriate for this stage of research as a step towards further research. Although participants were asked about their treatment goals when working with patients with chronic pain, this was not done using a standardised measure, and as such, the reported changes are limited in their interpretability. These results could be strengthened through more in-depth use of qualitative methods, such as questions about barriers to integrating a biopsychosocial approach in practice and the acceptability of the PF approach to physiotherapists. Future research could also investigate the usefulness of this training in other (non-MSK) physiotherapy departments as the skills are likely to be highly transferable. Finally, the study design here is unable to isolate the effects of the training separate from other potential effects happening concurrently and there was no blinding used during any stage of delivery, assessment or analyses to assure elimination of any potential researcher biases. Better controlled training trials may be considered in the future.
In conclusion, an innovative, brief training session referred to here as PIPT was associated with changes in attitudes and beliefs of MSK physiotherapists. The study demonstrates that the model appears relevant to physiotherapists and can be introduced within a day to a group who are not experienced in the approach. This is important in the current climate where more and more complex patients appear to be seen by non-specialist units.
Acknowledgments
The authors would like to thank all the physiotherapists who participated in this study. Thanks also to Nicky Wilson (Consultant Physiotherapist), Tricia Hill (Head of Physiotherapy, Kings College Hospital) and Jacky Jones (Head of Physiotherapy Guys and St Thomas’ Physiotherapy Department).
Footnotes
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
References
- 1. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006; 10(4): 287–333. [DOI] [PubMed] [Google Scholar]
- 2. Smart K, Doody C. The clinical reasoning of pain by experienced musculoskeletal physiotherapists. Man Ther 2007; 12: 40–49. [DOI] [PubMed] [Google Scholar]
- 3. Main CJ, George SZ. Psychologically informed practice for management of low back pain: future direction in practice and research. Phys Ther 2011; 91(5): 820–824. [DOI] [PubMed] [Google Scholar]
- 4. National Pain Audit. Final report 2010-2012, http://www.nationalpainaudit.org/media/files/NationalPainAudit-2012.pdf (2012, accessed 6 August 2015).
- 5. Roditi D, Robinson ME. The role of psychological interventions in the management of patient with chronic pain. Psychol Res Behav Manag 2011; 4: 41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Houben RM, Ostelo RW, Vlaeyen JW, et al. Health care providers’ orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. Eur J Pain 2005; 9: 173–183. [DOI] [PubMed] [Google Scholar]
- 7. Ostelo RW, Stomp-van den Berg SG, Vlaeyen JW, et al. Health care provider’s attitudes and beliefs towards chronic low back pain: the development of a questionnaire. Man Ther 2003; 8(4): 214–222. [DOI] [PubMed] [Google Scholar]
- 8. Bishop A, Foster NE, Thomas E, et al. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain 2008; 135(1–2): 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Magalhães MO, Costa LOP, Cabral CMN, et al. Attitudes and beliefs of Brazilian physical therapists about chronic low back pain: a cross-sectional study. Rev Bras Fisioter 2012; 16(3): 248–253. [DOI] [PubMed] [Google Scholar]
- 10. Domenech J, Sánchez-Zuriaga D, Segura-Ortí E, et al. Impact of biomedical and biopsychosocial training sessions on the attitudes, beliefs, and recommendations of health care providers about low back pain: a randomised clinical trial. Pain 2001; 152(11): 2557–2563. [DOI] [PubMed] [Google Scholar]
- 11. Overmeer T, Boersma K, Denison E, et al. Does teaching physical therapists to deliver a biopsychosocial treatment program result in better patient outcomes? A randomized controlled trial. Phys Ther 2011; 91: 804–819. [DOI] [PubMed] [Google Scholar]
- 12. Beissner K, Henderson CR, Jr, Papaleontiou M, et al. Physical therapists’ use of cognitive-behavioral therapy for older adults with chronic pain: a nationwide survey. Phys Ther 2009; 89(5): 456–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol 2014; 69(2): 153–166. [DOI] [PubMed] [Google Scholar]
- 14. Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: an experiential approach to behavior change. New York: Guilford Press, 1999. [Google Scholar]
- 15. Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: the process and practice of mindful change, 2nd ed. New York: Guilford Press, 2012. [Google Scholar]
- 16. Hann KE, McCracken LM. A systematic review of randomized controlled trials of Acceptance and Commitment Therapy for adults with chronic pain: outcome domains, design quality, and efficacy. J Context Behav Sci 2014; 3: 217–227. [Google Scholar]
- 17. Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther 2006; 44(1): 1–25. [DOI] [PubMed] [Google Scholar]
- 18. McCracken LM, Morley S. The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J Pain 2014; 15(3): 221–234.24581630 [Google Scholar]
- 19. McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain. Am Psychol 2014; 69(2): 178–187. [DOI] [PubMed] [Google Scholar]
- 20. McCracken LM, Yang S-Y. A contextual cognitive behavioural analysis of rehabilitation workers’ health and well-being: influences of acceptance, mindfulness, and values-based action. Rehabil Psychol 2008; 53(4): 479–485. [Google Scholar]
- 21. Mackenzie CS, Poulin PA, Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl Nurs Res 2006; 19(2): 105–109. [DOI] [PubMed] [Google Scholar]
- 22. McConachie DAJ, McKenzie K, Morris PG, et al. Acceptance and mindfulness-based stress management for support staff caring for individuals with intellectual disabilities. Res Dev Disabil 2014; 35(6): 1216–1227. [DOI] [PubMed] [Google Scholar]
- 23. Bond FW, Bunce D. Mediators of change in emotion-focused and problem-focused worksite stress management interventions. J Occup Health Psychol 2000; 5: 156–163. [DOI] [PubMed] [Google Scholar]
- 24. Varra AA, Hayes SC, Roget N, et al. A randomized control trial examining the effect of acceptance and commitment training on clinician willingness to use evidence-based pharmacotherapy. J Consult Clin Psychol 2008; 76(3): 449–458. [DOI] [PubMed] [Google Scholar]
- 25. Houben RM, Vlaeyen JW, Peters M, et al. Health care providers’ attitudes and beliefs towards common low back pain: factor structure and psychometric properties of the HC-PAIRS. Clin J Pain 2004; 20: 37–44. [DOI] [PubMed] [Google Scholar]
- 26. Rainville J, Bagnall D, Phalen L. Health care providers’ attitudes and beliefs about functional impairments and chronic back pain. Clin J Pain 1995; 11: 287–295. [DOI] [PubMed] [Google Scholar]
- 27. Rainville J, Carlson N, Polatin P, et al. Exploration of physicians’ recommendations for activities in chronic low back pain. Spine 2000; 25: 2210–2220. [DOI] [PubMed] [Google Scholar]
- 28. Latimer J, Mahler C, Refshauge K. The attitudes and beliefs of physiotherapy students to chronic back pain. Clin J Pain 2004; 20: 45–50. [DOI] [PubMed] [Google Scholar]
- 29. Houben RM, Gijsen A, Peterson J, et al. Do health care providers’ attitudes towards back pain predict their treatment recommendations? Differential predictive validity of implicit and explicit attitude measures. Pain 2005; 114: 491–498. [DOI] [PubMed] [Google Scholar]
- 30. Bond FW, Hayes SC, Baer RA, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther 2011; 42: 676–688. [DOI] [PubMed] [Google Scholar]
- 31. Hayes SC, Strosahl KD, Wilson KG, et al. Measuring experiential avoidance: a preliminary test of a working model. Psychol Rec 2004; 54: 553–578. [Google Scholar]
- 32. Flaxman P, Bond FW. A randomised worksite comparison of acceptance and commitment therapy and stress inoculation training. Behav Res Ther 2010; 48(8): 816–820. [DOI] [PubMed] [Google Scholar]
- 33. Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav 1981; 2: 99–113. [Google Scholar]