Abstract
Context:
Recognition of the importance of informatics to the practice of pathology has surged. Training residents in pathology informatics have been a daunting task for most residency programs in the United States because faculty often lacks experience and training resources. Nevertheless, developing resident competence in informatics is essential for the future of pathology as a specialty.
Objective:
The objective of the study is to develop and deliver a pathology informatics curriculum and instructional framework that guides pathology residency programs in training residents in critical pathology informatics knowledge and skills and meets Accreditation Council for Graduate Medical Education Informatics Milestones.
Design:
The College of American Pathologists, Association of Pathology Chairs, and Association for Pathology Informatics formed a partnership and expert work group to identify critical pathology informatics training outcomes and to create a highly adaptable curriculum and instructional approach, supported by a multiyear change management strategy.
Results:
Pathology Informatics Essentials for Residents (PIER) is a rigorous approach for educating all pathology residents in important pathology informatics knowledge and skills. PIER includes an instructional resource guide and toolkit for incorporating informatics training into residency programs that vary in needs, size, settings, and resources. PIER is available at http://www.apcprods.org/PIER (accessed April 6, 2016).
Conclusions:
PIER is an important contribution to informatics training in pathology residency programs. PIER introduces pathology trainees to broadly useful informatics concepts and tools that are relevant to practice. PIER provides residency program directors with a means to implement a standardized informatics training curriculum, to adapt the approach to local program needs, and to evaluate resident performance and progress over time.
Keywords: ACGME informatics milestones, Informatics, Informatics training, pathology GME informatics curriculum, pathology informatics essentials for residents, pathology residency training
INTRODUCTION
Informatics has never been more relevant to the specialty and practice of pathology. Generating and managing information derived from processing, analysis, and interpretation of patient specimens form the core of the mission of pathology to provide information that is crucial to patient care. Over the years, informatics has had multiple definitions. Medical informatics is the science of how to use data, information, and knowledge to improve human health and delivery of health-care services.[1] The College of American Pathologists (CAP) defines clinical informatics as the application of information management in health care to promote safe, efficient, effective, personalized, and responsive care.[2] The domain of pathology informatics includes clinical informatics and extends to involve information- and technology-intensive elements that are unique to pathology.[3,4] Pathology informatics activities have application at the individual, institutional, community, and population levels.[2]
Experience and observation confirm that informatics training in pathology residency programs is often absent, or when offered, inconsistent from program to program and frequently lacking in depth, breadth, and structure, particularly in comparison to more traditional areas of pathology training.[5,6] To address the need for informatics training in pathology residency programs, three organizations—Association of Pathology Chairs (APC), Association for Pathology Informatics (API), and CAP—convened a joint work group of pathology informatics experts and authorities in pathology Graduate Medical Education (GME). This work group, led by a core team of informatics and education leaders from the three organizations, developed and released the Pathology Informatics Essentials for Residents (PIER), a novel and flexible curriculum for educating pathology residents in informatics. PIER offers both a curriculum and instructional process for incorporating informatics training into pathology residency programs. This article describes the rationale for PIER, its development process, the PIER curriculum and Resource Toolkit, and PIER's companion change management strategy.
RATIONALE
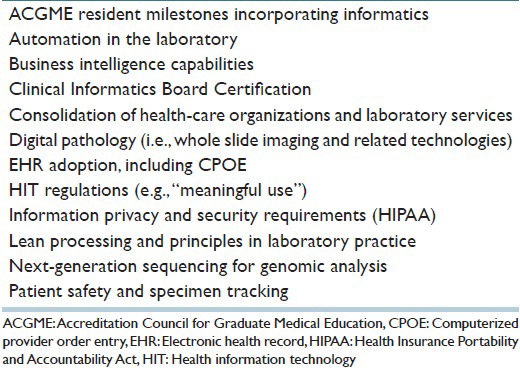
The recognition of the importance of informatics to the specialty and practice of pathology has surged in recent years.[7] Computers, laboratory information systems, and data management have been familiar to pathologists for decades because they are integral to pathology as a specialty.[8] Numerous factors drive the prominence of informatics in pathology practice, including rapid information technology changes, increased electronic health record adoption, and novel laboratory methods such as molecular tests, prioritized patient safety initiatives to minimize misidentification errors, increased health information technology-related regulations, and changing business needs [Table 1]. The increasing role and recognition of informatics in contemporary pathology practice presents a strong argument that acquisition of a basic knowledge of informatics should be part of the preparation of future pathologists.
Table 1.
Factors driving the prominence of informatics in pathology practice (alpha order)
In line with the observations above, expectations for pathology residency programs to train their residents in informatics are increasing. Training residents in informatics has been a daunting task for most programs in the United States because of the absence of a standardized curriculum, the limited number of faculty with informatics expertise, numerous competing subject matter priorities and practical time constraints, and the rapid pace of change to the content due to both technologic advances and evolving regulatory needs. These challenges notwithstanding the pathology community recognize the mandate for appropriate exposure and training in informatics to enable the advancement and transformation of the practice of pathology.[7,9,10]
APPROACH
The CAP, APC, and API formed a collaborative partnership in 2013 to address the need to educate pathology residents about informatics. The three organizations jointly convened a work group of twenty pathologists with expertise in informatics and/or in GME to help develop the PIER curriculum for residents. The intent was to design a program that could be implemented in essentially any pathology residency program, whether or not that program had a local pathologist informaticist on the faculty. The workgroup researched and developed 38 peer-reviewed outcome statements identifying the knowledge and skills that all residents should have in pathology informatics to practice pathology upon completion of their residency program. The group also reviewed core content for the new certifying Board Examination in Clinical Informatics, which is cosponsored by the American Board of Pathology.[11]
For training delivery purposes, the outcomes were organized into 4 groups, named the PIER Essentials, presenting the recommended sequence for residents to build their pathology informatics knowledge and skills over time [Figure 1].
Figure 1.
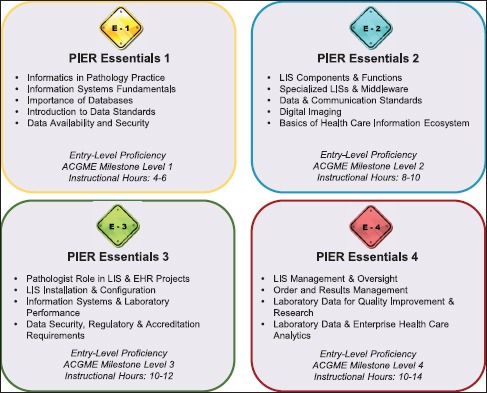
Pathology Informatics Essentials for Residents – Curriculum Scope and Sequence (PIER Release 1). Abbreviations: ACGME, Accreditation Council for Graduate Medical Education. EHR: Electronic Health Record, LIS: Laboratory Information Systems, PIER: Pathology Informatics Essentials for Residents
During the development process, work group members mapped the PIER Essentials to the Accreditation Council for GME (ACGME) Milestones.[12] The milestones represent the knowledge, skills, attitudes, and other attributes for each of the ACGME competencies that all pathology residents are expected to achieve in the course of their training.[12] Milestone systems-based practice 7 (SBP7) deals specifically with competencies related to clinical informatics in anatomic pathology-clinical pathology (AP-CP).[12] The relationship of the PIER Essentials to Milestone SBP7 is illustrated in Figure 2.
Figure 2.
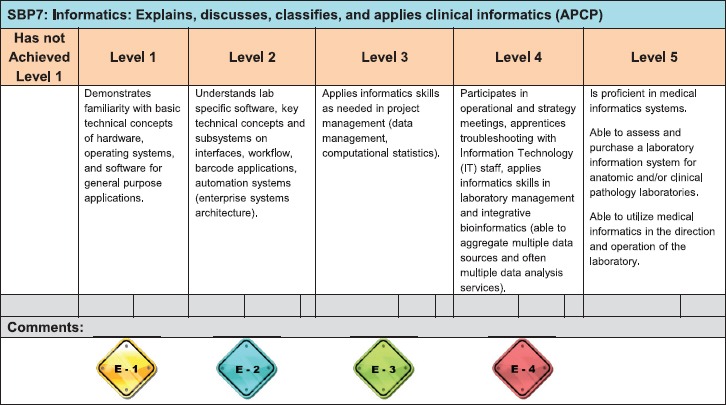
Pathology Informatics Essentials for Residents – Mapped to Accreditation Council for Graduate Medical Education Pathology Informatics Milestone SBP7 for Systems-Based Practice Competency (PIER Release 1). Abbreviations: APCP, Anatomic Pathology and Clinical Pathology. PIER: Pathology Informatics Essentials for Residents, SBP7: Pathology Milestone Systems-Based Practice Subcompetency 7
The work group identified key learning resources for the informatics topics in each of the PIER Essentials, such as book and journal references and online training modules. The group also developed practical exercises aimed at reinforcing informatics knowledge with hands-on experience. This work formed the basis of the PIER Resource Toolkit, an interactive set of three instructional process tools that support delivery of each of the four PIER Essentials [Figures 3–5].
Figure 3.
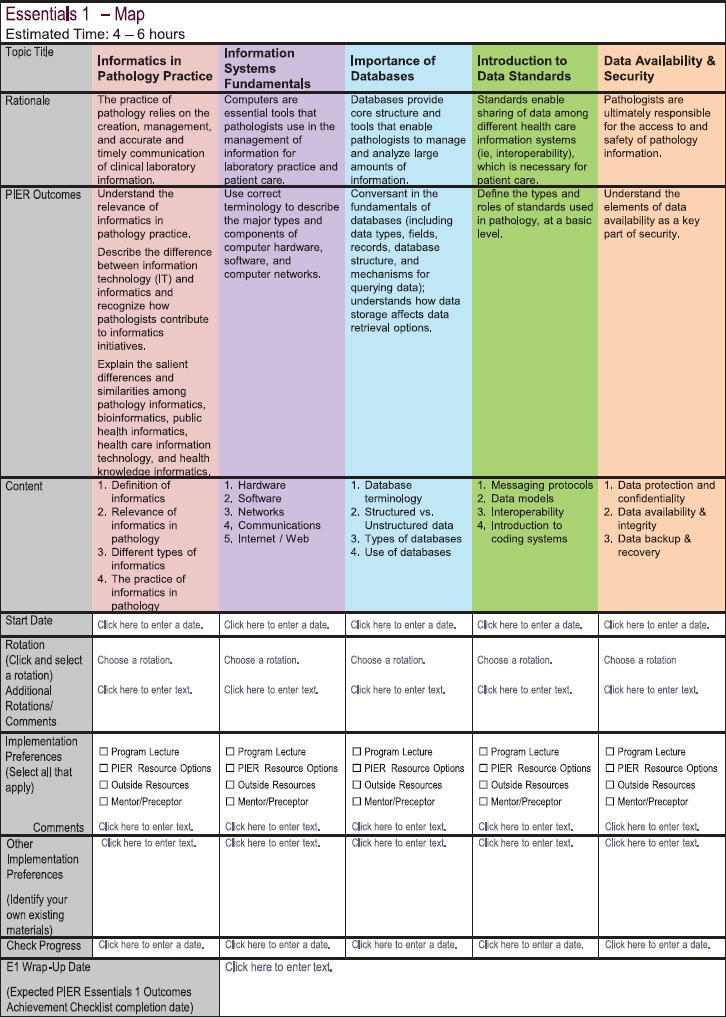
Pathology Informatics Essentials for Residents – Essentials 1 Map (PIER Release 1 – subject to change in Release 2 [summer, 2016]). Abbreviations: E1, Essentials 1, PIER: Pathology Informatics Essentials for Residents
Figure 5.
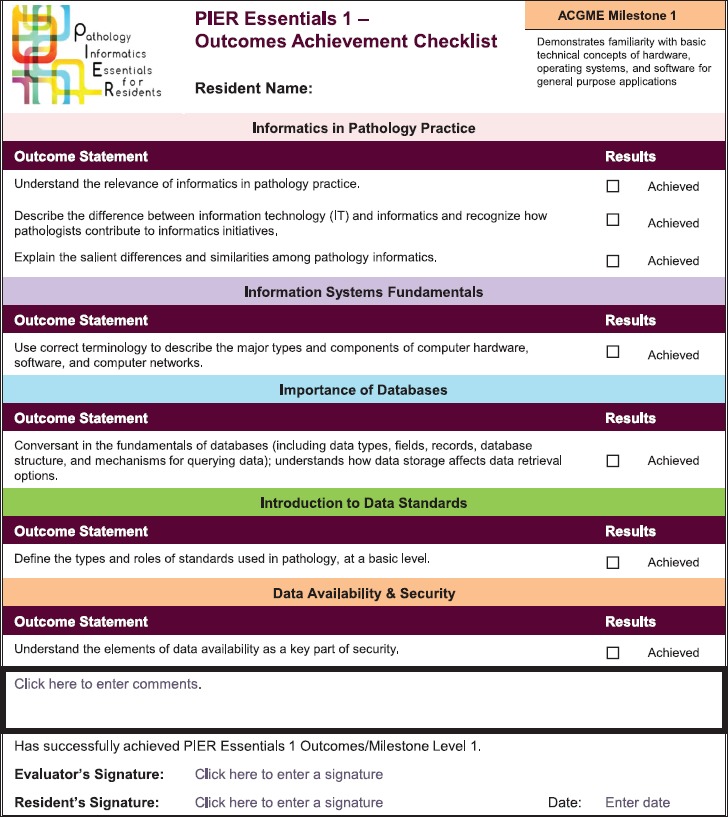
Pathology Informatics Essentials for Residents – Essentials 1 Outcomes Achievement Checklist (PIER Release 1 – subject to change in Release 2 [summer, 2016]). ACGME: Accreditation Council for Graduate Medical Education, PIER: Pathology Informatics Essentials for Residents
The workgroup met regularly through conference calls from January to September 2014. A subset of the work group met in person to finalize the curriculum and instructional framework (i.e., PIER Essentials) and curated list of associated resource options and to determine the structure of the PIER Resource Toolkit. A core team of informatics and education leaders from CAP, APC, and API provided oversight and project management throughout the development process and continued to manage the initiative.
RESULTS
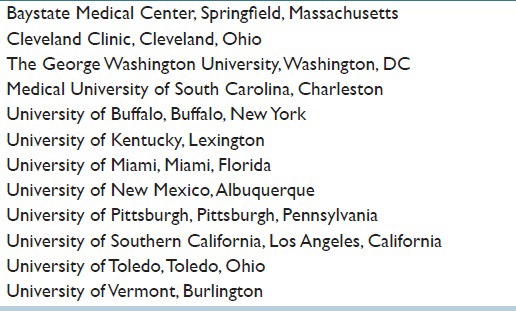
The PIER prototype (Release 0) was introduced at the July 2014 APC Annual Meeting. PIER Release 1 was made available to all residency programs on the APC Website in September 2014 and was concurrently alpha tested by 12 residency programs [Table 2] during that academic year. Preliminary alpha test findings indicate that PIER is effective. Release 2 is currently in development and scheduled for release in summer 2016. PIER's content relevance is intended to be maintained via new releases, updating the subject matter and instructional process tools for program directors, and faculty to provide continuously improved informatics training to their residents while continuing to meet ACGME Informatics Milestone requirements.
Table 2.
Pathology Informatics Essentials for Residents alpha test residency programs
Pathology Informatics Essentials for Residents Essentials
The PIER Essentials present up-to-date pathology informatics training topics based on 38 peer-reviewed outcome statements [Appendix 1]. PIER aims to integrate informatics education into pathology residents’ AP-CP rotations and into residency activities related to management, quality assurance, and control, regulatory, and accreditation issues. PIER Essentials also include aspects of laboratory information and systems in the greater health-care information domain, including electronic health records [Figure 1].
The PIER Essentials successively build on each other with increasing complexity as indicated by the stated proficiency levels. Residency programs may control the timing by year to suit the scheduling availability of postgraduate year (PGY) 1 to PGY 4 residents; however, it is important that the order is followed because the knowledge and skills build in sequence. The estimated instructional hours for each PIER Essentials are based on the approximate time it takes to complete the recommended approach for each of the topics in each of the Essentials. The number of instructional hours may be adjusted on the basis of the final number and type of resource options and instructional strategies selected by the program director.
Alignment with Accreditation Council for Graduate Medical Education Milestone Systems-based Practice 7
The four PIER Essentials are mapped to Levels 1–4 in ACGME Pathology Informatics Milestone SBP7 as “explains, discusses, classifies, and applies clinical informatics” [Figure 2]. PIER focuses on preparing all residents to achieve Levels 1–4 during residency and is an effective resource for aspiring informatics specialists to develop prerequisite pathology informatics knowledge and skills before advanced training or fellowships.
While PIER enables residents to meet ACGME Milestone SBP7 Levels 1–4, the PIER outcome statements specify a complete set of pathology informatics knowledge and skills that a resident needs to have upon completion of his/her residency program to practice pathology [Appendix 1]. PIER is scoped and sequenced to achieve the outcomes which are more specific and more directly aligned with practice needs than the high-level Milestone statements.
ACGME Milestone Level 5 is beyond PIER's purpose and scope. The ACGME defines Level 5 as follows: “The resident has advanced beyond performance targets set for residency and is demonstrating ‘aspirational’ goals which might describe the performance of someone who has been in practice for several years. It is expected that only a few exceptional residents will reach this level”;[12] PIER focuses on preparing residents to achieve Levels 1–4 during residency and is not intended for residents or fellows pursuing advanced training in informatics.
Pathology Informatics Essentials for Residents Materials
PIER materials consist of two key components: Instructional Resource Guide and Resource Toolkit. These and other support materials are freely available to download from http://www.apcprods.org/PIER (accessed April 6, 2016). The Instructional Resource Guide orients program directors to PIER's rationale and approach, PIER Essentials, and PIER Resource Toolkit. The Resource Toolkit provides three interactive tool templates that program directors and residents can use to plan, customize, implement, and manage the four PIER Essentials. These tools include (1) an Essentials Map that identifies the topics, topic rationale, key outcomes, topic content, rotation options, and delivery options for each of the Essentials [Figure 3]; (2) PIER resource options that include a recommended set of reference resources and practical training exercises for each topic [Figure 4]; and (3) an Essentials Outcomes Achievement Checklist that tracks accomplishment of each outcome statement; successful completion of each of the Essentials indicates achievement of the corresponding ACGME Milestone level [Figure 5].
Figure 4.
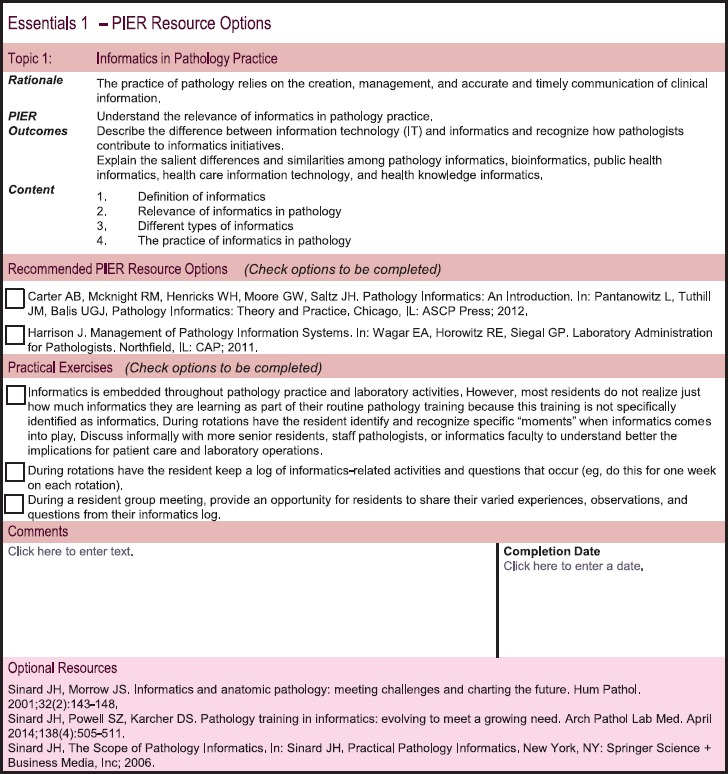
Pathology Informatics Essentials for Residents – Essentials 1 Resource Options (PIER Release 1 – subject to change in Release 2 [summer, 2016]). PIER: Pathology Informatics Essentials for Residents
PIER provides the curriculum and process for residency programs to develop and customize their own self-study modules, lecture series, and blended learning units. Users can add and maintain their own tools and content in their Resource Toolkit electronic files. PIER is flexible and scalable for programs to best meet their local needs, philosophy, and circumstances. Because of the importance of learning the principles and practice of informatics in the context of actual pathology practice, PIER is designed as a longitudinal experience for residents, with learning activities and practical, hands-on exercises spanning the 4 years of AP-CP or 3 years of straight AP-CP residency and can be embedded in existing AP-CP rotations.
Flexible Design
The overarching goal of PIER is that residents build basic competency in pathology informatics. PIER recognizes that the GME pathology informatics space is growing with a variety of diverse topics, approaches, and materials at varying costs and from multiple providers. Because programs have varied internal expertise, budgets, and education strategy preferences, PIER has built-in design agility, is free of charge, and includes only no cost and relatively low-cost learning resources. PIER also serves as a framework for other informatics training content. The curriculum can be supplemented with a variety of additional teaching resources and tools from internal and external providers as they become available.
IMPLEMENTATION
PIER is supported by a four-phase, multiyear change management strategy designed to test and support delivery of GME informatics training across all US pathology residency programs. The change management strategy engages and supports residency programs in the successful implementation of PIER incrementally over time recognizing that programs will have varying adoption types [Table 3] and motivations. As such, program directors can leverage the PIER curriculum and instructional process tools to guide the training decisions that are most appropriate to their program.
Table 3.
Pathology Informatics Essentials for Residents change management framework
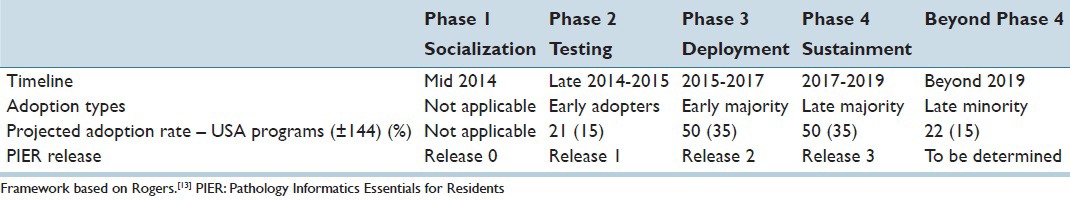
The change management framework and associated terminology (e.g., early adopters, early majority, late majority, late minority) developed for PIER is adapted from Diffusion of Innovations.[13] The adoption phases, timeline, forecasted adoption rate, and PIER release schedule are presented in Table 3. The communication and engagement methods for each phase are influenced by the adoption attributes of the residency programs in a given phase. Implementing PIER by applying proven innovation diffusion and change management practices should increase PIER's usage as the key stakeholders are engaged and supported during the four phases. The application of the model referenced above as related to the development of PIER is described below.
Phase 1: Socialization
During this phase, PIER and its prototype (Release 0) was introduced to residency program directors and chairs at the July 2014 APC Annual Meeting, and PIER's informational Web page on APC's Website was launched. PIER was presented to department chairs at the APC regional meetings (September to October 2014) and featured in the APC September 2014 issue of the Paths to Progress newsletter. PIER was also presented locally by CAP members at multiple academic institutions (August to November 2014). As a result, key stakeholders were informed and educated about PIER and were invited to evaluate it for use at their own institutions.
Phase 2: Testing/Validation
At the July 2014 APC Annual Meeting, more than thirty pathology residency programs expressed a desire to participate in an alpha test to validate PIER Release 1, initially released to all residency programs in September 2014. Alpha test programs were selected to achieve diversity on criteria that included program size, access to informatics experts/faculty, and geographic location. Twelve programs [Table 2] participated in data collection events between November 2014 and October 2015. Data collection events included online surveys, phone interviews, and virtual focus groups. Nine additional residency programs indicated that they used PIER Release 1 and participated in an online survey. Based on valuable feedback received from these 21 programs, PIER Release 2 is in development and will be available by summer 2016. From this group of “early adopters,” PIER champions, consisting of both program directors and residents, have emerged and are expected to play a key role in attracting “early majority” residency programs.
Phase 3: Deployment
The goal of deployment is to attract and motivate the “early majority” group of programs (n = 50) to adopt PIER during a 2-year cycle time (July 2015–June 2017). The “early majority” group tends to rely upon the “early adopters” for social proof and usage validation before making a decision. Communications and engagement methods currently in development will provide the “early majority” program directors with the information and experiences of the “early adopter” alpha test programs necessary to support them in their decision-making process.
Phase 4: Sustainment
The goal of Phase 4 is similar to Phase 3 yet recognizes that the “late majority” is characteristically a conservative and/or skeptical group. The intention is to attract and motivate the “late majority” program directors (n = 50) to adopt PIER during the subsequent 2-year cycle time (July 2017–June 2019). The approach will feature evidence of resident outcome achievement and details of the successes of “early adopter” and “early majority” programs. The communication and engagement plan will be developed in late 2016, applying lessons learned from Phase 3 (deployment).
Each phase of the change management strategy is specific to the adoption attributes of the program population. Overall, the change management strategy seeks to attract pathology residency programs to use PIER as a best practice curriculum standard and helpful instructional resource, to advocate for its consideration and proper use, to support PIER's adoption and ongoing use across residency programs, and to support use of any and all relevant materials in the delivery of GME informatics training and education. Further to the latter point, PIER is not a commercial product and has no commercial ties.
DISCUSSION
As early as 1977, Aller et al.[14] described the benefits of computerization for the pathology laboratory. Korpman[15] described how pathologists are well-suited to play a leadership role as information managers in health-care organizations. Friedman[16] first used the term “pathology informatics” in describing the need for a locus of responsibility and expertise in informatics within pathology departments. Sinard and Morrow[17] described a vision of the pathologist as an information integrator at the center of diagnostics in patient care. Not surprisingly, a 2007 survey of pathology group leaders[18] cited informatics as one of the most important skill sets for newly hired pathologists. In the current era of information-rich medical practice, and with the development of new informatics-intensive laboratory technologies such as electronic health record-related meaningful use requirements, digital pathology, next-generation sequencing, and computational pathology, demand will increase on the pathology community to invest in informatics initiatives and resources, train more pathology informaticists, and educate all pathology residents about informatics.
There have been several recent initiatives highlighting the importance of effective education in informatics for pathology residents. The ACGME's development and adoption of Milestone SBP7 [Figure 2] has formalized the need for training in informatics for all pathology residents and achievement of an acceptable level of competency by all residents in the course of their training. A new subspecialty Board Certification in Clinical Informatics, cosponsored by the American Board of Pathology and the American Board of Preventive Medicine, is now available. While the new board certification does not relate to residency training per se, it reflects an endorsement of the importance of informatics in medicine and specifically in pathology practice. The core content for the certifying Board Examination in Clinical Informatics was previously published;[11] this content was examined and analyzed during the preparation of PIER.
As based on several surveys that examined informatics training in pathology residency programs[5,6] and on anecdotal feedback received by APC's residency program directors’ section, informatics training in pathology residency programs has been largely suboptimal. While some programs have developed novel methods, such as virtual rotations and wikis, to expose their residents to informatics,[19,20] most programs in the United States are not teaching their pathology residents adequately.
During the past 25 years, there have been multiple proposals for elements of a curriculum in informatics for pathology residents.[4,7,21,22,23,24,25,26,27] In general, these proposals have focused on topics centered largely on information technology. In 2003, a comprehensive curriculum that detailed learning objectives and skill sets in informatics for pathology residents were published.[4] This included recommendations for demonstrating knowledge of and competence in informatics topic areas that are germane to pathology practice. Harrison[28] described in detail the questions and methods for evaluating informatics training in a pathology residency program. More recently, Rao and Gilbertson[27] described their institution's approach to incorporating informatics experiences into general pathology residency training.
None of these training proposals have been widely implemented, at least partly because other priorities compete with informatics for time during residency training, there is a perceived lack of informatics resources and training materials, and pathology faculty generally lacks informatics expertise.[29] The CAP, APC, and API considered that these resource gaps might be mitigated at least in part by a standardized, expert-endorsed, practice-oriented pathology informatics curriculum. The fact that PIER was developed by and is supported by the CAP, APC, and API likely accounts for the keen interest in PIER so far received from the pathology community at-large and the current level of willingness of program directors to implement PIER.
Overall, the PIER curriculum provides a useful and reliable subject matter framework for pathology residency programs regarding “what to teach” and low-cost options for “how to teach it.” PIER was not intended to provide off-the-shelf, prepackaged content to teach informatics. For this content, programs rely on available resources (e.g., textbooks, literature, online information) and/or materials (e.g., didactic lectures, handouts, exercises, demonstrations) developed by the individual programs themselves or available from outside sources. Each residency program will make cost/benefit decisions on the basis of their own available resources. Program directors can refer the PIER curriculum to determine which instructional materials they want to make or buy, using the instructional process tools to document and track their decisions.
Identifying reasonable subject management scope for residents in pathology informatics training was challenging. The field of informatics is broad and encompasses many diverse topics, and these topics continue to evolve and expand rapidly as a result of advancing technology and emerging regulations. At the outset, the PIER work group believed that trying to educate pathology residents about all of these topics in the limited time available during residency was impractical and unnecessary, and hence, they researched and developed the 38 peer-reviewed outcome statements[30] identifying the competence that a resident should have in pathology informatics upon completion of his/her residency program.
Informatics has been incorporated into residency training in other medical specialties.[31,32,33] The objective for some of these specialties was to familiarize their residents with clinical information technology applications that could enhance their productivity in clinical practice.[34] Evaluation of these approaches proved to be invaluable as it influenced important decisions regarding PIER's format and curriculum. For example, because residents did not find detailed background in information technology to be of immediate clinical value, more attention was directed toward teaching practical skills and reinforcing these during clinical residency.
The working group made decisions about the scope of informatics topics suitable to include, in general, resident training. Many topics that might be considered by some to be pathology informatics topics, such as computer programming, database administration, advanced statistics, and bioinformatics, were identified to be out of scope for PIER. The working group had difficulty in deciding how best to position and cover the field that has been termed computational pathology.[9] While all working group members agreed that in this “big data” era of health care, there is an opportunity for pathology to take the lead,[9] the field of computational pathology is still emerging, the methods used are beyond basic informatics (e.g., it can involve advanced computational modeling or machine learning), and it is not yet in routine use in most pathology laboratories. As a result, computational pathology was incorporated only as a minor component in PIER Essentials 2 [Figure 1]. That said, “many of the other topics within PIER are expected to help prepare pathology residents to eventually use computational pathology in their future practice, should the need arise.”
The primary target audience for PIER is pathology residency program directors and administrators who have responsibility for training residents and preparing them generally for practice. Secondary audiences may include undergraduate medical education directors and students interested in knowing or understanding what is required in pathology informatics for a resident. PIER is also anticipated to be a useful resource for aspiring specialists to develop prerequisite pathology informatics knowledge and skills before advanced training or fellowships in pathology and/or clinical informatics. Although practicing pathologists may also use PIER as a resource for continuing education in informatics, it was not designed specifically for this purpose.
To date, PIER has been well-received by the pathology community and the alpha test programs. Alpha test program directors reported that PIER effectively supports residency training programs in implementing/improving informatics training; the PIER Essentials include highly relevant and important training topics; PIER allocates time for training on those topics; it includes recommended learning resources and practical exercises; the Outcomes Achievement Checklists provide a useful tool for documenting Milestone achievement.[35] In addition, alpha test residents, faculty, and program directors reported an increase in residents’ knowledge/skill related to the PIER outcome statements. Most alpha test program representatives report that they would be willing to recommend PIER to other programs.[35]
Although program directors who participated in the PIER alpha test report satisfaction with PIER, they continue to raise the same implementation concerns reported in the literature to date. Lack of time and faculty expertise are the greatest challenges for implementing PIER.[35] It is difficult to work new topics into an existing curriculum and a set training schedule that is already fully scheduled. The time issue is compounded by the lack of available off-the-shelf, prepackaged pathology informatics training materials. Regarding the second greatest challenge reported, many pathology departments currently lack sufficient numbers of faculty members skilled in informatics. In the context of family medicine residency, it has been shown that successful education of residents in informatics depends on making sure the teachers themselves are skilled in the use of information technology tools.[36] Although nonpathology faculty and staff, such as information technology or laboratory information system support staff members, are available in some departments to assist in informatics teaching, pathology residency programs do not necessarily have ready access to these types of instructors.
CONCLUSIONS
PIER is a highly adaptable curriculum and instructional framework that pathology residency programs may use to address the pressing need for informatics training for all pathology residents. This standardized, yet flexible, curriculum is designed to align with the relevant ACGME Pathology Milestones and can be implemented in residency programs of varying size and with diverse needs, settings, and resources. There are practical implementation challenges with curriculum additions, particularly lack of time and faculty expertise. The hope is that program directors and pathology informatics experts can work to solve these challenges together in the near future. The intention is that PIER will be widely adopted by program directors and it will help to better prepare all pathology residents for the modern practice of pathology.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
We recognize and gratefully acknowledge the members of the PIER work group: Walter H. Henricks, MD (Co-leader); Liron Pantanowitz, MD (Co-leader); Donald S. Karcher, MD (core team); Raymond D. Aller, MD; Philip J. Boyer, MD, PhD; Victor B. Brodsky, MD; Alexis B. Carter, MD; Rajesh C. Dash, MD; Michael D. Feldman, MD, PhD; John R. Gilbertson, MD; James H. Harrison Jr, MD, PhD; Anil V. Parwani, MD, PhD; Suzanne Z. Powell, MD; Michael W. Riben, MD; Rodney A. Schmidt, MD, PhD; John H. Sinard, MD, PhD; Enrique Terrazas, MD; J. Allan Tucker, MD; J. Mark Tuthill, MD, MS; and Myra Wilkerson, MD. We thank Ann Neumann, PhD, Vice President, CAP Learning, and Priscilla Markwood, Executive Director of the Association of Pathology Chairs, for their thoughtful leadership, education expertise, and review of this manuscript. We also thank Sue Plath, MA; Trish Glover, MS; and Arlene Thompson, MSEd of CAP Learning for guiding us through the process of developing the PIER curriculum and the change management strategy and for reviewing this manuscript.
APPENDIX
Appendix 1
The Pathology Informatics Essentials for Residents (PIER) outcomes for achievement statements were sourced from the Informatics Competency developed by the College of American Pathologists (CAP). The CAP Competency Model[30] is a peer-reviewed set of knowledge and skill statements written by experts in the various areas of pathology. Its intended audience is practicing pathologists for use in determining their professional development needs and also to guide CAP learning in the development of Graduate Medical Education (GME) activities.
Pathology Informatics Essentials for Residents Outcomes for Achievement
This section presents the master list of 38 statements identifying the knowledge and skills that a resident should have upon completion of his/her residency program to practice pathology.
These outcomes are organized into seven topic areas; they are not organized in the sequence in which a resident would learn them. This list provides a useful master list of the outcomes by topics, independent of the sequence in which they are taught. For resident training purposes, the outcomes are organized into the four PIER Essentials, displaying the recommended sequence for residents to successfully build their pathology informatics knowledge and skills over time [Figure 1].
Technology Fundamentals
Understand the relevance of informatics in pathology practice
Explain the salient differences and similarities among pathology informatics, bioinformatics, public health informatics, and healthcare information technology and health knowledge informatics
Use correct terminology to describe the major types and components of computer hardware, software, and computer networks
Be conversant in the fundamentals of databases, including data types, fields, records, database structure, and mechanisms for querying data; understand how data storage affects data retrieval options
Recognize the advantages of standardized terminology for creating interchangeable data, which can be retrieved and summarized
Define the key features of communication standards used in pathology, such as Health Level 7 (HL7) and Digital Imaging and Communications in Medicine
Define the types and roles of standards used in pathology, at a basic level
Understand the basics of the standards development process (includes International Organization for Standardization organizations such as HL7 and also other processes important in standards development such as Integrating the Healthcare Enterprise and Office of the National Coordinator for Health Information Technology)
Understand how patient and asset identification standards and tracking systems are used to improve patient safety and laboratory workflow
Recognize applications of ancillary information systems to optimize clinical, operational, and financial performance of the laboratory (e.g., middleware, financial systems, and business intelligence).
Laboratory Information Management in Health Systems
Recognize what laboratory information systems (LISs) are, what they do, and the role they play in efficient laboratory operations and health-care delivery
Identify opportunities to modify the LIS to improve operations
Understand capabilities and limitations of electronic interfaces between an LIS and instrumentation, middleware, and other information systems
Anticipate (and recommend remediation for) issues, potential problems, and challenges in electronic health record (EHR) handling of laboratory test results
Anticipate (and recommend remediation for) issues, potential problems, and challenges in EHR handling of laboratory test orders
Articulate the role and connections of the LIS within the network of health-care information systems (i.e., the local health-care information ecosystem)
Describe middleware, how it relates to the LIS, and roles for middleware in laboratory operations
Understand the special difficulties of information flow to and from the local information ecosystem (e.g., for outreach programs) and strategies for overcoming the obstacles
Understand the elements of data availability as a key part of security
Follow technology developments and identify opportunities for improving the security and quality of patient data.
Data Analysis and Management Tools
Recognize limitations and information gaps resulting from the limitations of the data analysis capability of LISs
Contribute to the definition and creation of integrated health-care data sets from multiple disparate sources to support useful, accurate, and reliable data analysis
Contribute to the analysis and interpretation of integrated pathology and enterprise data sets for improving care quality and increasing the efficiency of care delivery.
Digital Pathology
Use digital imaging systems such as whole slide imaging (WSI), telemicroscopy, and image analysis (as appropriate to practice setting)
Understand potential role, use, and limitations of WSI in the laboratory environment
Determine the appropriate digital image resolution for a particular need/purpose
Determine the appropriate telemicroscopy technology to use for a particular application.
Ongoing Laboratory System Management
Work with information systems personnel to ensure that reports are properly formatted (e.g. synoptic format and other standardized formats as appropriate)
Supervise the LIS team in the creation and updating of the LIS procedure manual
Understand the process and requirements for test definition and other information maintenance in the LIS.
Accreditation and Regulatory Compliance
Maintain compliance with electronic information management requirements of regulatory and/or accreditation agencies (focus on regulatory perspective, management, and inspection perspective of topic)
Follow technology developments and identify opportunities for improving the security and quality of patient data
Interpret new regulations to determine how they affect laboratory information management needs and the role of the laboratory within the health care system
Adhere to Health Insurance Portability and Accountability Act and other security and privacy requirements for the communication and storage of patient data (e.g., correct use of password-protected accounts, firewalls, digital certificates, encryption, and 2-factor authentication)
Recognize situations under which information technology may be subject to the US Food and Drug Administration regulation (e.g., blood banking and WSI)
Comply with positive patient identification processes/protocols.
Selection and Installation of Laboratory Systems
Explain the role and responsibility of pathologists with regard to the selection, oversight, and use of informatics systems in the function of the modern pathology laboratory
Provide input to the LIS selection team to ensure that an optimal fit between a purchased system and departmental needs is attained.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2016/7/1/27/185673
REFERENCES
- 1.What is Informatics? American Medical Informatics Association. [Last updated on 2011 Apr 14, Last accessed on 2016 Apr 01]. Available from: https://www.amia.org/fact-sheets/what-informatics .
- 2.Clinical Informatics Strategy. College of American Pathologists. [Last updated on 2013 Aug 16, Last accessed on 2016 Apr 06]. Available from: http://www.cap.org/ShowProperty?nodePath=/UCMCon/Contribution%20Folders/WebContent/pdf/clinical-informatics-strategy.pdf .
- 3.Sinard JH. Practical Pathology Informatics. New York: Springer Science + Business Media, Inc; 2006. [Google Scholar]
- 4.Henricks WH, Boyer PJ, Harrison JH, Tuthill JM, Healy JC. Informatics training in pathology residency programs: Proposed learning objectives and skill sets for the new millennium. Arch Pathol Lab Med. 2003;127:1009–18. doi: 10.5858/2003-127-1009-ITIPRP. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg-Kahn B, Healy JC. Medical informatics training in pathology residency programs. Am J Clin Pathol. 1997;107:122–7. doi: 10.1093/ajcp/107.1.122. [DOI] [PubMed] [Google Scholar]
- 6.Henricks WH, Healy JC. Informatics training in pathology residency programs. Am J Clin Pathol. 2002;118:172–8. doi: 10.1309/4CE8-N2MX-DFG6-N8H9. [DOI] [PubMed] [Google Scholar]
- 7.Sinard JH, Powell SZ, Karcher DS. Pathology training in informatics: Evolving to meet a growing need. Arch Pathol Lab Med. 2014;138:505–11. doi: 10.5858/arpa.2013-0328-RA. [DOI] [PubMed] [Google Scholar]
- 8.Park S, Parwani AV, Aller RD, Banach L, Becich MJ, Borkenfeld S, et al. The history of pathology informatics: A global perspective. J Pathol Inform. 2013;4:7. doi: 10.4103/2153-3539.112689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Louis DN, Gerber GK, Baron JM, Bry L, Dighe AS, Getz G, et al. Computational pathology: An emerging definition. Arch Pathol Lab Med. 2014;138:1133–8. doi: 10.5858/arpa.2014-0034-ED. [DOI] [PubMed] [Google Scholar]
- 10.Naritoku WY, Alexander CB, Bennett BD, Black-Schaffer WS, Brissette MD, Grimes MM, et al. The pathology milestones and the next accreditation system. Arch Pathol Lab Med. 2014;138:307–15. doi: 10.5858/arpa.2013-0260-SA. [DOI] [PubMed] [Google Scholar]
- 11.Gardner RM, Overhage JM, Steen EB, Munger BS, Holmes JH, Williamson JJ, et al. Core content for the subspecialty of clinical informatics. J Am Med Inform Assoc. 2009;16:153–7. doi: 10.1197/jamia.M3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The pathology milestone project. J Grad Med Educ. 2014;6(1 Suppl 1):182–203. doi: 10.4300/JGME-06-01s1-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rogers EM. Diffusion of Innovations. 5th ed. New York: Free Press; 2003. [Google Scholar]
- 14.Aller RD, Robboy SJ, Poitras JW, Altshuler BS, Cameron M, Prior MC, et al. Computer-assisted pathology encoding and reporting system (CAPER) Am J Clin Pathol. 1977;68:715–20. doi: 10.1093/ajcp/68.6.715. [DOI] [PubMed] [Google Scholar]
- 15.Korpman RA. Using the computer to optimize human performance in health care delivery. The pathologist as medical information specialist. Arch Pathol Lab Med. 1987;111:637–45. [PubMed] [Google Scholar]
- 16.Friedman BA. Informatics as a separate section within a department of pathology. Am J Clin Pathol. 1990;94(4 Suppl 1):S2–6. [PubMed] [Google Scholar]
- 17.Sinard JH, Morrow JS. Informatics and anatomic pathology: Meeting challenges and charting the future. Hum Pathol. 2001;32:143–8. doi: 10.1053/hupa.2001.23057. [DOI] [PubMed] [Google Scholar]
- 18.Brimhall BB, Wright LD, McGregor KL, Hernandez JS. Critical leadership and management skills for pathology practice. Arch Pathol Lab Med. 2007;131:1547–54. doi: 10.5858/2007-131-1547-CLAMSF. [DOI] [PubMed] [Google Scholar]
- 19.Kang HP, Hagenkord JM, Monzon FA, Parwani AV. Residency training in pathology informatics: A virtual rotation solution. Am J Clin Pathol. 2009;132:404–8. doi: 10.1309/AJCP6YXB6ODKTDQI. [DOI] [PubMed] [Google Scholar]
- 20.Park S, Parwani A, Macpherson T, Pantanowitz L. Use of a wiki as an interactive teaching tool in pathology residency education: Experience with a genomics, research, and informatics in pathology course. J Pathol Inform. 2012;3:32. doi: 10.4103/2153-3539.100366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haber MH, Clifford SS, Britton CT. A management informatics rotation for pathology residents. Am J Clin Pathol. 1991;95(4 Suppl 1):S38–41. [PubMed] [Google Scholar]
- 22.Buffone GJ, Beck JR. Informatics. A subspecialty in pathology. Am J Clin Pathol. 1993;100:75–81. doi: 10.1093/ajcp/100.1.75. [DOI] [PubMed] [Google Scholar]
- 23.Balis UJ, Aller RD, Ashwood ER. Informatics training in U.S. pathology residency programs Results of a survey. Am J Clin Pathol. 1993;100(4 Suppl 1):S44–7. [PubMed] [Google Scholar]
- 24.Becich MJ, Gross W, Schubert E, Blank G. Building an informatics training program for pathology. Semin Diagn Pathol. 1994;11:237–44. [PubMed] [Google Scholar]
- 25.Harrison JH, Jr, Stewart J., 3rd Training in pathology informatics: Implementation at the University of Pittsburgh. Arch Pathol Lab Med. 2003;127:1019–25. doi: 10.5858/2003-127-1019-TIPIIA. [DOI] [PubMed] [Google Scholar]
- 26.Kim JY, Gudewicz TM, Dighe AS, Gilbertson JR. The pathology informatics curriculum wiki: Harnessing the power of user-generated content. J Pathol Inform. 2010;1 doi: 10.4103/2153-3539.65428. pii: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rao LK, Gilbertson JR. Longitudinal engagement of pathology residents: A proposed approach for informatics training. Am J Clin Pathol. 2014;142:748–54. doi: 10.1309/AJCPWJ61RERWEDIK. [DOI] [PubMed] [Google Scholar]
- 28.Harrison JH., Jr Pathology informatics questions and answers from the University of Pittsburgh pathology residency informatics rotation. Arch Pathol Lab Med. 2004;128:71–83. doi: 10.5858/2004-128-71-PIQAAF. [DOI] [PubMed] [Google Scholar]
- 29.Riben M. The challenge of integrating informatics training during residency. Am J Clin Pathol. 2014;142:732–4. doi: 10.1309/AJCPZK30STQFJHSH. [DOI] [PubMed] [Google Scholar]
- 30.Competency Model for Pathologists. College of American Pathologists. [Last updated on 2013 Mar 16, Last accessed on 2016 Apr 01]. Available from: https://www.learn.cap.org/homearticle1.aspx .
- 31.Jerant AF. Training residents in medical informatics. Fam Med. 1999;31:465–72. [PubMed] [Google Scholar]
- 32.Zelnick CJ, Nelson DA. A medical informatics curriculum for 21st century family practice residencies. Fam Med. 2002;34:685–91. [PubMed] [Google Scholar]
- 33.Siddiqui KM, Weiss DL, Dunne AP, Branstetter BF. Integrating imaging informatics into the radiology residency curriculum: Rationale and example curriculum. J Am Coll Radiol. 2006;3:52–7. doi: 10.1016/j.jacr.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 34.Moidu K, Leehy MA, Steinberg I, Einreinhofer S, Falsone JJ, Cleary J, et al. Informatics integration in a medical residency program: Early experiences. Proc AMIA Annu Fall Symp. 1996:55–9. [PMC free article] [PubMed] [Google Scholar]
- 35.College of American Pathologists, Association of Pathology Chairs, Association for Pathology Informatics. PIER Alpha Test Executive Summary; Published February, 2016. [Last accessed on 2016 April 04]. Available from: https://www.apc.memberclicks.net/assets/docs/pier/pier%20alpha%20test%20exec%20summary.pdf .
- 36.Cartwright CA, Korsen N, Urbach LE. Teaching the teachers: Helping faculty in a family practice residency improve their informatics skills. Acad Med. 2002;77:385–91. doi: 10.1097/00001888-200205000-00006. [DOI] [PubMed] [Google Scholar]


