Abstract
A high prevalence of uncontrolled hypertension among blacks is a major cause of racial health disparities in the US. We established a community/academic partnership to improve hypertension control in blacks receiving medical care at a federally qualified health center in Milwaukee. The defining components of our program included the following: 6 group sessions (1/month) designed to motivate and empower patients to manage their blood pressure, based on the American Heart Association’s Simple Seven curriculum; active involvement of a community health worker; and ongoing participation of a Community Advisory Board. The study design included a matched control group not exposed to the intervention. Patients in both groups received their usual medical care. Overall, compared to baseline, systolic blood pressure decreased at both 6 and 12 months (p< 0.004), however, the reduction of blood pressure in the intervention and control groups did not differ significantly (p=0.62). Based on written responses to a questionnaire and structured focus group interviews after completing the 6 month program, participants reported that the intervention was effective. In retrospect, they suggested that more attention might have been given to spirituality and stress reduction. Larger and longer term studies will be required to evaluate the added value of this type of intervention.
The high prevalence of hypertension among blacks in the US is a leading cause of racial health disparities (1–4). Based on National Health and Nutrition Examination Survey (NHANES) data, in 2011–2012 the age adjusted prevalence of hypertension was 42.1% in non-Hispanic blacks and 28.0% in non-Hispanic whites (4). Between 2003 and 2010, hypertension awareness rates did not differ between blacks and whites (80.8% and 79.1%, respectively) and the percentages of black and white hypertensives on drug treatment (71.9% and 71.2%, respectively) did not differ, however, hypertension was controlled in a lower percentage of blacks (43.9%) than whites (48.6%) (5). In a separate analysis of 2001–2006 NHANES data (6), the prevalence of uncontrolled hypertension in blacks (27.4%) was higher than in whites (17.0%) or Mexican Americans (20.2%). Based on data from the 1995–2010 National Hospital Discharge Survey, blacks had higher rates of preventable hospitalizations for hypertension than whites (334 per 100,000 vs 87.4 per 100,000, respectively (7). In 2011, the age-adjusted cerebrovascular disease death rate (deaths per 100,000 population) in Milwaukee County was 60.41 for blacks and 30.96 for whites; the age adjusted death rate for “hypertensive heart disease” was 32.17 for blacks and 15.23 for whites (8). The relatively large number of blacks with uncontrolled hypertension suggests that more emphasis is needed on developing effective treatment strategies for blacks.
In 2008, the International Society of Hypertension in Blacks convened a panel of clinicians and researchers to develop recommendations for addressing hypertension-related health disparities by promoting better hypertension management in African Americans. The panel recommended culturally sensitive lifestyle interventions that emphasize patient self-management supported by providers, family, and the community (9). Consistent with this recommendation, in 2010 we established a community-academic partnership to develop a culturally appropriate pilot program to improve blood pressure control in blacks with uncontrolled hypertension. The purpose of this report is to describe the development, implementation, and evaluation of this pilot program.
METHODS
Study overview
The study was conducted with patients receiving medical care at Progressive Community Health Centers, a federally qualified health center that operates two clinics in Milwaukee. In 2010, these clinics provided care to 8,600 patients—80% were black, 35% reported incomes at or below 200% of the poverty level, 71% were on Medicaid, and 17% were uninsured. Hypertension was the most prevalent leading medical diagnosis (11% of patients), and blood pressure was uncontrolled in 46% of those with hypertension,
The design of the study included both an intervention group and a control group of blacks with uncontrolled hypertension. The two groups were selected from separate clinic sites, and both groups received their usual medical care provided by the clinics. The intervention included active involvement of a community health worker and a series of six group sessions (one/month) designed to empower and enable patients to be active participants in managing their blood pressure. Change in blood pressure was the primary trial endpoint.
Identification of patients
For the intervention group, three cohorts of blacks with uncontrolled hypertension (three consecutive visits with systolic blood pressures >140 mmHg and/or diastolic > 90 mmHg in non-diabetics, >130 mmHg systolic and/or >80 mmHg diastolic in diabetics) were recruited from a single clinic staffed by 3 physicians and 3 additional primary health care providers. At that site, combining results of the three 6-month cohorts, a total of 270 potentially eligible patients with uncontrolled hypertension were invited to participate. They received a packet containing a letter detailing the research study and consent forms was mailed to interested patients. The community health worker (CHW) then contacted the patients again to field questions about study participation and offer convenient meeting times. She followed up with reminder calls, sent bus tickets and remained available for questions. Of those invited, 75 initially agreed to attend the first group session, and of those, 41 actually did participate; 36 attended at least 5 of the 6 group sessions. An additional 5 patients attended fewer than 5 group sessions but maintained at least weekly telephone contact with the CHW. All participants provided signed informed consent, and the protocol was approved by a Froedtert Hospital/Medical College of Wisconsin Institutional Review Board.
The control group of patients with uncontrolled hypertension was identified from a patient panel followed at a separate Progressive Health Center clinic site, staffed by 1 physician and 1 additional primary health care provider. Similar to identification of intervention patients, the designation of uncontrolled hypertension was based on elevated blood pressure measured during each of 3 consecutive clinic visits. Control patients were matched with intervention patients on the basis of age, sex, blood pressure, BMI, and diabetes. Control patients were not seen by study personnel, and their data were abstracted from their usual clinic records.
Intervention
The CHW, a black woman, functioned as a lay leader for the intervention. This was a full time position with fringe benefits. She had no other responsibilities. The individual in this position did not have a college degree but had a long history in primary education before becoming an AHEC certified Community Health Worker. She was also certified through the Living Well with Chronic Diseases program (10). During the intervention, she reinforced individual patient action plans with weekly telephone calls to each participant. She assessed goals, reminded patients about scheduled group sessions, and provided encouragement. She served as a confidant, a source of information, and facilitated communication between patients, social workers, and healthcare providers.
The program included six group sessions. These sessions took place in a centrally located community room, in close proximity to the usual care clinic, provided by a neighborhood non-profit agency. Transportation costs were supported by provision of bus tickets or in some instances by provision of patients’ insurance. Standardized blood pressure and weight were measured at each session, and patients were asked a series of questions about diet, exercise, and action planning. In addition to providing peer support, the group sessions addressed well described barriers to treatment, lack of self-management support, lack of social support, and differences in culture–based health perceptions. The curriculum for the six sessions, based on Life’s Simple Seven Program (11), was as follows: a) hypertension overview, led by a physician; b) “get active”, led by a physical therapist; c) “eat healthy”, led by a local chef; d) “lower cholesterol”, led by a bionutritionist; e) smoking cessation, led by a social worker; e ) “healthy weight”, led by a nurse. At each group session, patients received an action plan, culturally appropriate colorful handouts, and were encouraged to set an attainable goal regarding each topic. A healthy snack was provided at each session. Additional incentives included a blood pressure monitor, pedometer, portion plate, “flavor bag,” recipes, nutrition information, cookbook, a stress ball, and for those who attended five group sessions, a $50 gift card.
A Community Advisory Board was established to inform the recruitment process, to review the study’s progress and barriers, and to provide guidance in selecting and developing culturally sensitive educational materials and strategies related to health promotion and hypertension. The Board was comprised of representatives from nonprofit organizations with a stake in Milwaukee’s at-risk black community. Membership included one representative from each of the following: the American Heart Association, a neighborhood Health Alliance, the Wisconsin Primary Health Care Association, and a community representative who is a locally recognized chef and who personally has hypertension. The Board met a total of 11 times during the course of the study, more frequently in the planning phases and subsequently quarterly.
Program evaluation: statistical analysis
Comparisons of baseline and 6-month results were made by selecting the data from the baseline visit and visits within a 5–7 month interval for each study subject. For early entrants into the program, 12 month follow-up data (11–13 month interval) are also included. This statistical model takes advantage of multiple measurements on each subject to make balanced comparisons of the 6 and 12 month changes. The model averages multiple measures in each 2 month window and adjusts for repeated measures. For patients in the intervention group, all blood pressure measurements obtained in both the study clinic and usual care clinic were included in the analysis. Blood pressures in the two clinic sites did not differ significantly. Generalized linear models using generalized estimating equations (GEE) to adjust for repeated measure were used to test for treatment effect over time for the outcome measures of systolic and diastolic blood pressures and weight (12, 13). A compound symmetric form was used for the covariance matrix. The GEE method adjusts for both the repeated measures, and for the possibility of multiple measurements within each time-window. Baseline and demographic data were compared using t-tests and chi-square tests. These analyses were performed using SAS version 9.3 (The SAS Institute, Cary, NC).
Program evaluation: qualitative analysis
After each of the three study cohorts completed the six month program, subjects were asked to complete a written survey questionnaire and were invited to participate in a structured focus group interview facilitated by a community social worker. The social worker was a member of Progressive Community Health Centers’ staff, and was not otherwise involved in the study. She was an experienced facilitator. In total, 36 subjects (9–15/group) participated in the focus groups, and 35 completed the survey questionnaire. Focus groups capitalized on communication among research participants in order to generate additional data which may not have surfaced during one-on-one discussions. Interviews were transcribed and analyzed using the following coding process: 1) open coding to reveal recurrent ideas across interviews, 2) axial coding to reveal themes generated from recurring ideas, and 3) examination of the inter-relationships among ideas and themes.
RESULTS
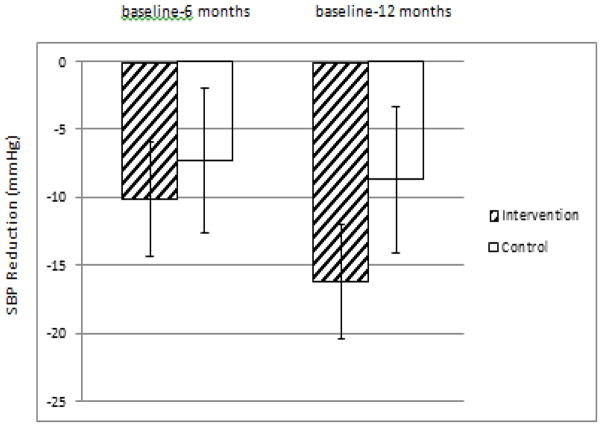
The control and intervention groups were matched for age, sex, BMI, prevalence of diabetes, and smoking history (Table 1). At baseline, systolic blood pressure was higher (p=0.021) in the intervention group (Table 2). A group-by-time interaction was not statistically significant (p=0.62), indicating that the change in blood pressure at both 6 and 12 months did not differ comparing intervention and control groups. However, analyzing each group separately, blood pressure decreased significantly in the intervention group but not in the control group. Compared to baseline, at the end of 6 months systolic blood pressure in the intervention group decreased by 10.1 mmHg ± 3.2 SE in the intervention group (p< 0.002) and by 7.3 mmHg ± 5.0 SE in the control group (p=0.14); at 12 months, systolic blood pressure decreased by 16.2 mmHg ±5.2 SE in the intervention group (p< 0.002) and by 8.7 mmHg ± 5.7 SE in the control group (p=0.13) (Figure 1). At 6 and 12 months, compared to baseline, there were no significant changes in diastolic blood pressure or body weight in either of the 2 groups.
Table 1.
Baseline data in intervention and control groups
| Intervention (n=41) | Control (n=42) | |
|---|---|---|
| Female (%) | 56 | 55 |
| Age (years) | 55.8 ± 7.1 (SD) | 56.0 ± 7.0 |
| BMI (kg/m2) | 35.8 ± 9.5 | 35.9 ± 9.7 |
| Diabetes (%) | 61 | 57 |
| Tobacco | ||
| Never (%) | 42 | 48 |
| Yes (%) | 10 | 10 |
| Quit (%) | 49 | 43 |
Table 2.
Mean (95% CI) blood pressures and weights in the intervention and control groups at baseline and 6 months.
| Intervention Group (n=41) | Control Group (n=42) | ||
|---|---|---|---|
| SBP (mmHg) | Baseline | 154 (147, 160) | 142 (136, 149) # |
| 6 months | 144 (138, 149) | 135 (128, 142) | |
| 6-month change | −10.2 (−16.4, −3.8)* | −7.3 (−17.0, 2.4) | |
| DBP (mmHg) | Baseline | 85 (78, 85) | 86 (82, 89) |
| 6 months | 82 (78, 85) | 84 (80, 89) | |
| 6-month change | −4.0 (−9.7, 1.6) | −0.9 (−6.5, 4.7) | |
| Weight (lbs) | Baseline | 217 (201, 234) | 231 (211, 250) |
| 6 months | 217 (200, 233) | 229 (208, 249) | |
| 6-month change | −0.7 (−3.3, 1.8) | −2.1 (−6.2, 1.9) |
p <0.002 compared to baseline value in same group
p =0..021 compared to intervention group
Figure 1.
Reductions of systolic blood pressure at 6 and 12 months in intervention and control groups.
Overall, participants found the program effective and would recommend it to friends and family (Table 3). They valued the opportunity to be involved in research and health improvement strategies. Most reported that they made efforts to actively participate in the program and to adopt healthier lifestyles. Strengths of the program included its structure and the instructional strategies utilized. Participants valued opportunities to acquire information and tools aimed at improving health. Participants emphasized the importance of trust building with healthcare providers. The program engaged participants in a way which kept them involved in the program, created a cohort of learners which encouraged participation of those who had been reluctant to participate in group discussions in the past, and provided information which could be shared with others. Participants felt empowered working as partners with health care providers in developing specific recommendations. The most useful sessions were those which focused on reading labels, sleep habits, growing herbs, exercise, and managing salt and sugar intakes. These particular sessions appealed to participants because they provided practical strategies which could be immediately implemented. In retrospect, participants suggested more attention might have been given to spirituality and stress reduction.
Table 3.
Summary of participant responses to focus group survey (n= number of respondents)
| Very satisfied | Satisfied | Neutral | Unsatisfied | Very Unsatisfied | |
|---|---|---|---|---|---|
| Overall, how satisfied were you with the sessions? | 25 | 8 | 0 | 0 | 2 |
| Definitely | Probably | Not Sure | Probably Not | Definitely Not | |
| Should length of sessions increase to 90 minutes? | 12 | 10 | 6 | 5 | 2 |
| Would you recommend our program to friends and family members? | 25 | 8 | 0 | 0 | 0 |
| A Great Deal | Much | Some what | Little | None | |
|---|---|---|---|---|---|
| daily | 2–3 days | once a week | once a month | ||
| How much effort did you put into participating in the program? | 21 | 8 | 1 | 5 | 0 |
| How much effort did you put into making an action plan? | 9 | 17 | 7 | 0 | 1 |
| How much effort did you put into following your action plan? | 14 | 10 | 9 | 0 | 1 |
| How much effort did you put into changing you cooking habits? | 17 | 13 | 3 | 0 | 1 |
| How much effort did you put into increasing your exercise habits? | 10 | 19 | 5 | 0 | 1 |
| How much effort did you put into quitting smoking? | 8 | 4 | 5 | 2 | 9 |
| How much effort did you put into maintain/ attaining a healthy weight? | 20 | 8 | 4 | 2 | 0 |
| How much effort did you put into taking blood pressure medications/ working with your health care provider? | 25 | 7 | 1 | 2 | 0 |
Reported lifestyle changes attributable to the program included such items as: removing salt from homes and replacing it with healthier seasonings; reviewing food labels in order to manage salt intake; negotiating with physicians about prescribed medications; replacing high sugar foods with lower sugar foods; reducing portion sizes for participants and family members living in the same household; using blood pressure monitors to manage blood pressure and increased levels of exercise.
Barriers to attendance at the group sessions included additional serious health conditions, and family and/or work obligations. One participant had a fatal myocardial infarction during the program. His data are not included in the analysis.
DISCUSSION
The defining components of the program included a community-academic partnership, ongoing participation of a Community Advisory Board, active involvement of a community health worker in patient care, and a series of group sessions designed to incentivize and empower patients to manage their blood pressure. The hypertension control strategies were designed to address previously described barriers. Based on a group-by-time analysis, the reductions of systolic blood pressure in the intervention and control groups did not differ significantly. However, when considered separately, blood pressure decreased significantly only in the intervention group. The favorable trend in the control group may have been a reflection of increased attention to hypertension guidelines by healthcare providers, since they were aware of this ongoing pilot project.
In conjunction with resources of an academic medical center, the community/academic partnership engaged community representatives in developing and implementing specific strategies to address a health care concern of the community. This partnership was determined to be meaningful, based on partners’ responses to PARTNER TOOL, a program that analyzes, records, and tracks networks to enhance relationships (14). Other investigators have also observed that engaging the community in this way, integrating a community health worker in the team, and providing services in the locale of study participants are important contributors to the success of the intervention (15), Not unexpectedly, engaging the community and the concept of “patient centeredness” in research have become priorities for funding agencies (16, 17).
Several recent studies have evaluated similar strategies to improve hypertension control in community settings. For example, a community/academic health center partnership has documented the effectiveness of community health workers in the care of people with hypertension, including blacks (18). Community health workers can bridge cultural and social gaps between health care providers and the patients they serve. As previously reported, the effectiveness of community health workers was evaluated in 8 randomized trials focusing on poor, urban blacks (19). Significant improvements in controlling blood pressure were reported in 7 of these 8 trials. Community health workers are recognized in the Patient Protection and Affordable Care Act as important members of the healthcare workforce.
In general, programs teaching self-management are more effective than information-only patient education in improving clinical outcomes (20). Lay-led self care support groups have been shown to be effective in improving self-efficacy and to be cost-effective among patients with long-term conditions (21, 22) The effectiveness of self-management in achieving hypertension control has been well documented (23).
Other studies have highlighted additional challenges to implementing hypertension control recommendations in the primary care setting. In a recent feasibility study in a small community health center in Finland, hypertension control was not improved by attempts to optimize antihypertensive drug therapy, introduction of home blood pressure monitoring, and lifestyle guidance with family practitioners and nurses serving as interventionists (24). The authors suggest that failure of this intervention might be related to fiscal constraints, limited personnel resources, and the absence of financial and academic incentives for the health care providers.
The Counseling African Americans to Control Hypertension (CAATCH) trial is an ongoing trial designed to compare the effectiveness of a multilevel, multicomponent, evidence-based intervention with usual care in improving blood pressure control among hypertensive blacks who receive care in community health centers (25, 26). Patients at the intervention sites received patient education, home blood pressure monitoring, and monthly lifestyle counseling. Physicians at these sites attended monthly hypertension case rounds, and received feedback on their patients’ home blood pressure readings and chart audits. At the end of 12 months, the blood pressure control rates were similar in the intervention and usual care groups (27).
A majority of patients in the CAATCH trial had adverse lifestyle behaviors, co-morbidities, psychosocial barriers to hypertension control, and reported non-adherence to medications (28). Younger men were more likely to be non-adherent.. Patients who reported self-efficacy were more likely to report that they were adherent to antihypertensive medications, whereas patients with depressive symptoms were more likely to be non-adherent. These observations confirm previous reports of the divergent associations of self-efficacy and depression with medication adherence in hypertensive blacks.
The primary barrier to hypertension control in blacks is related to the implementation of recommendations, rather than to lack of awareness of the recommendations and their beneficial effects (28). Developing effective strategies for hypertension control is dependent on understanding the barriers to implementation. As discussed by others, recognition of the importance of the implementation step has spawned a new area of inquiry—implementation science (29). The goal is to understand why an intervention is or is not effective in a specific environment. In this pilot study, we observed that ultimately, some barriers proved too prohibitive for patients to participate or continue with the program. This often was due to personal crises such as employment, housing transition, family crises, or severe illness, rather than circumstantial issues such as lack of transportation or childcare. Other factors found to be associated with adherence in hypertensive blacks include social support, comorbidity, patient-provider communication, and health care discrimination (28).
In summary, in this pilot study, blood pressure control improved in the patients who participated in the group sessions. Because hypertension control also improved in the control group, larger and longer term studies will be required to evaluate the added value of this type of intervention. Based on results of this pilot study, additional suggestions to consider for the content of the group sessions in future programs include the following: incorporation of topics related to patient-physician relationships and trust building, which facilitates an awareness of the importance of working with physicians to manage health by controlling illnesses; provision of more individualized diet plans; incorporation of culture-specific food choices; inclusion of information about supplements and non-prescription alternatives which decrease blood pressure; and acknowledgment that there may be relevant spiritual components which contribute to well-being
Acknowledgments
This study was supported by the Healthier Wisconsin Partnership Program (Project #2010-D-51) and by the National Center for Advancing Translational Science, National Institutes of Health, through grant number 8UL1TR00055.
Footnotes
Clinical trial registration url: http:Clinicatrials.gov.
Unique identifier: NCTO1910857
References
- 1.Center for Disease Control & Prevention. Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002. MMWR. 2005;54:7–9. [PubMed] [Google Scholar]
- 2.Hajjar I, Kotchen TAS. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 198802000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 3.Egan BM, Zhao Y, Axon RN. US tends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 4.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. Centers for Disease Control and Prevention; Oct, 2013. NCHS Data Brief, No. 133. http:www.cdc,giv/nchs/data/databriefs/db/133.htm. [PubMed] [Google Scholar]
- 5.Center for Disease Control and Prevention. Racial/ethnic disparities in the awareness, treatment and control of hypertension—United States, 2003–2010. MMWR. 2013;62:351–355. [PMC free article] [PubMed] [Google Scholar]
- 6.Redmond N, Baer HJ, Hicks LS. Health behaviors and racial disparity in blood pressure control in the National Health and Nutrition examination Survey. Hypertension. 2011;57:383–389. doi: 10.1161/HYPERTENSIONAHA.110.161950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Will JC, Yoon PW. Preventable hospitalizations for hypertension: establishing a baseline for monitoring racial differences in rates. Preventing Chronic Disease: Public Health Research, Practice, and Policy. 2013 Feb 14;10 doi: 10.5888/pcd10.120165. http://www.cdc.gov/pck/issues/2013/12_0165.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.http://wish.wisconsin.gov/results
- 9.Scisney-Matlock M, Bosworth HB, Giger JN, et al. Strategies for implementing and sustaining therapeutic lifestyle changes as part of hypertension management in African Americans. Postgrad Med. 2009;121:147–159. doi: 10.3810/pgm.2009.05.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Bandura A, Gonzalez VM, Laurent DD, Holman HR. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39:1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 11.http://mylifecheck.heart.org/Default.aspx?NavID=1&CultureCode=en-US.
- 12.McCullagh P, Neider JA. Generalized linear models. 2. London: Chapman & Hall; 1989. [Google Scholar]
- 13.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 14. [Accessed 9/24/2014]; http://www.partnertool.net.
- 15.Stuart-Shor EM, Berra KA, Kamau MW, Kumanyika SK. Behavioral strategies for cardiovascular risk reduction in diverse and underserved racial/ethnic groups. Circulation. 2012;125:171–184. doi: 10.1161/CIRCULATIONAHA.110.968495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmed SM, Palermo AS. Community engagement in research: frameworks for education and peer review. Am J Pub Health. doi: 10.2105/AJPH,2009.178137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Selby JV, LIpstein SH. PCORI at 3 years; progress, lessons, and plans. N Engl J Med. 2014;370:592–595. doi: 10.1056/NEJMp1313061. [DOI] [PubMed] [Google Scholar]
- 18.Levine DM, Bone LR, Hill MN, et al. The effectiveness of a community academic health center partnership in decreasing the level of blood pressure in an urban African American population. Ethn Dis. 2003;13:354–361. [PubMed] [Google Scholar]
- 19.Brownstein JN, Chowdhury FM, Norris S, et al. Am J Prev Med. 2007;32:435–447. doi: 10.1016/j.amepre.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy A, Reeves D, Bower P, Lee V, Middleton E, Richardson Gardner C, Gately C, Rogers A. The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: a pragmatic randomized controlled trial. J Epidemiol Community Health. 2007;61:254–261. doi: 10.1136/jech.2006.053538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Long KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Gonzalez VVM, Laurent DD, Holman HR. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;38:1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 23.McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet. 2010 doi: 10.1016/SO140-6736(10)60964. [DOI] [PubMed] [Google Scholar]
- 24.Niranen TJ, Leino K, Puukka P, Kantola I, Karanko H, Jula AM. Lack of impact of a comprehensive intervention on hypertension in the primary care setting. Am J Hyperten. 2014;27:489–496. doi: 10.1093/ajh/hpt204. [DOI] [PubMed] [Google Scholar]
- 25.Ogedegbe C, Tobin JN, Fernandez S, Cerin W, Diaz-Gloster M, Cassells A, Khalida C, Pickering T, Schoenthaler A, Ravenell J. Counseling African Americans o Control Hypertension (CAATCH) Trial: a multi-level intervention to improve blood pressure contron in hypertensive blacks. Circulation: Cardiovascular Quality and Outcomes. 2009;2:249–256. doi: 10.1161/CIRCOUTCOMES.109.849976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fernandez S, Tobin JN, Cassells A, Diaz-Gloster M, Kalida C, Ogedegbe G. The Counseling African Americans to Control Hypertension (CAATCH) Trial. Baseline demographic, clinical, psychosocial, and behavioral characteristics. Implement Sci. 2011 doi: 10.1186/1748-5908-6-100. doi:10:1186/1748-5908-6-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogedegbe G, Tobin JN, Fernandez S, Cassells A, Diaz-Gloster M, Khalida C, Pickering T, Schwartz J. Counseling African Americans to Control Hypertension (CAATCH): cluster randomized clinical trial main effects. Circulation. 129:2044–2051. doi: 10.1161/CIRCULATIONAHA.113.006650. 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewis LM, Schoenthaler AM, Ogedegbe G. Patient factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. J Clin Hyperten. 2012;14:250–255. doi: 10.1111/j.1751-7176.2012.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whittle J. Implementing programs to improve hypertension management in typical practice settings: not as easy as it sounds. Am J Hyperten. 2014;27:291–293. doi: 10.1093/ajh/hpt237. [DOI] [PMC free article] [PubMed] [Google Scholar]