Abstract
Abdominal hernias are a common cause of bowel obstruction. The major types of abdominal hernias are external or abdominal wall hernias, which occur at areas of congenital or acquired weakness in the abdominal wall. An alternative entity is internal hernias, which are characterized by a protrusion of viscera through the peritoneum or mesentery. We herein present the case of a female peritoneal dialysis patient with bowel obstruction due to an internal hernia. Although an initial work-up did not lead to a correct diagnosis, an exploratory laparotomy revealed that she had intestinal herniation due to a defect in the broad ligament of the uterus, which was promptly corrected by surgery. The concerns about the perioperative dialytic management as well as the diagnostic problems regarding the disease that arose in our experience with the present patient are also discussed.
Keywords: peritoneal dialysis, internal hernia, ileus, broad ligament of the uterus, intestinal incarceration
Introduction
Abdominal hernias are a common cause of bowel obstruction. The major types of abdominal hernias are external or abdominal wall hernias, which occur at areas of congenital or acquired weakness in the abdominal wall.1 Thus, the occasional link between such pathologies and peritoneal dialysis (PD), which is associated with increased intra-abdominal pressure,2 may not be surprising.3 A different entity is internal hernias, which are characterized by a protrusion of the viscera through the peritoneum or mesentery4 and have been shown to account for approximately 0.5–5.8% of all cases of intestinal obstruction.4,5 In this report, we describe our experience with a PD patient who was diagnosed with a bowel obstruction due to intestinal herniation, which occurred as a result of a defect of the broad ligament of the uterus. The patient has given consent for publication of details and images in this report.
Case Report
A 65-year-old woman who was treated with continuous ambulatory PD (CAPD) was admitted with lower abdominal pain of 1-day duration, which was followed by intermittent nausea and vomiting. She had chronic renal failure due to chronic glomerulonephritis, and had been treated for 22 months with CAPD (four daily exchanges; 2 L of Midperiq® 135 × 4; Terumo Co.). A Tenckhoff catheter was implanted through a classic transverse surgical incision, with a favorable postoperative course. Peritonitis was not noticed after the initiation of CAPD. The patient’s blood parameters were acceptable, and her general condition was satisfactory. Her other medical history included hypertension, and she had undergone total hysterectomy because of a uterine myoma 15 years previously.
A physical examination conducted on admission revealed that she was alert and oriented, and had a body temperature of 36.6 °C. A clinical examination disclosed diffuse tenderness without peritoneal signs, while the abdomen was slightly distended and tympanic with diminished bowel sounds. The peritoneal fluid was clear, with a white blood cell (WBC) count of less than 50/mm3. The skin surrounding the peritoneal catheter, as well as the catheter’s exit site, was unremarkable without any signs of inflammation. A laboratory evaluation revealed the following findings: WBC, 6300/mm3; hemoglobin, 8.0 g/dL; hematocrit, 22.7%; platelet count, 28.5 × 104/mm3; blood urea nitrogen, 43 mg/dL; serum creatinine, 6.5 mg/dL; sodium, 137 mmol/L; potassium, 4.3 mmol/L; chloride, 104 mmol/L; and C-reactive protein, 0.44 mg/dL. Upright radiography showed some loops of dilated bowel with air-fluid levels (Fig. 1). Initially, a small bowel obstruction due to post-hysterectomy-related adhesion was suspected and she was managed conservatively. However, computed tomography (CT) of the abdomen, which was performed 2 days after admission, demonstrated discontinuity of the small bowel with a distended closed loop in the pelvic cavity (Fig. 2), suggesting that strangulation was the likely cause of the development of the bowel obstruction. She was therefore subjected to an exploratory laparotomy, which revealed incarcerated, small bowel herniation into the pouch of Douglas through a defect of the residual broad ligament of the uterus (Fig. 3A). Ten centimeters of the incarcerated bowel was slightly edematous (Fig. 3B); however, it was not ischemic and the entrapped bowel was freed using a bowel forceps, while the defect of the broad ligament was closed (Fig. 3C). No adhesion was observed between the adnexum and the small bowel. The PD catheter was also removed because the patient refused to continue with the PD. She started to receive hemodialysis (HD) three times per week via a right internal jugular vein catheter on the day after the operation. Finally, a wrist-arterio-venous fistula was created to provide permanent vascular access, and the periodic HD program was continued.
Figure 1.

Abdominal X-ray showing mildly dilated loops of the bowel without fecal impaction.
Figure 2.
(A) Contrast-enhanced CT showing the point of discontinuity in the small bowel in the pelvic cavity (arrow) and the collapsed distal ileal loops (arrowhead). (B) Scan at a slightly more cephalic position, revealing the swirling or centralizing of the mesenteric vessels and folds toward the point of the small bowel obstruction (arrow).
Figure 3.
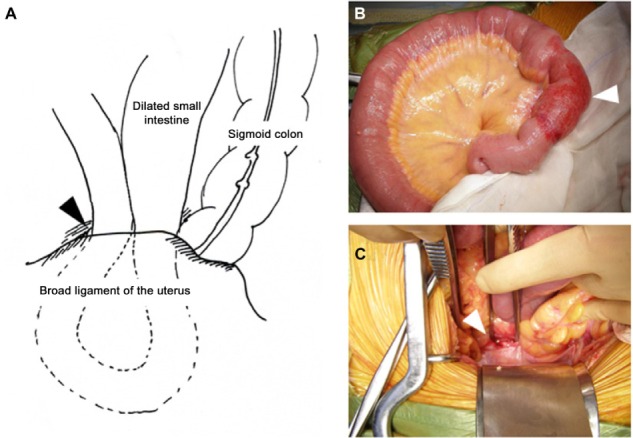
Findings of exploratory laparotomy. The schematic representation (A) shows the anatomy of the small bowel herniation (arrowhead) through a defect of the broad ligament of the uterus. A macroscopic view of the entrapped bowel (B) reveals the 10 cm of incarcerated bowel with slight edematous change (arrowhead). After freeing the small bowel (C), the defect of the broad ligament (arrowhead) was closed.
Discussion
Acute bowel obstruction is a common abdominal emergency. The majority of cases occur secondary to adhesion from prior surgery.6 The remaining cases may be due to neoplasms, abdominal wall hernias, and, in decreasing frequency, Crohn’s disease, volvulus, intussusception, bezoars, gallstones, trauma, and iatrogenic problems.7–9 Bowel obstruction is rarely attributed to internal hernias.4,5,7–9 Broad ligament hernias are extremely rare and account for only a few percent of internal hernia cases.4 In this regard, the paucity of literature describing the complications of internal hernias in patients who receive PD may not be surprising. To the best of our knowledge, this is the first report of a long-term PD patient with internal herniation that occurred because of a defect of the broad ligament of the uterus.
The broad ligaments of the uterus consist of layers of peritoneum that cover the intestinal and vesical surfaces, which are carried laterally in a tripod fashion to the side walls of the pelvis.10 Based on the nature of the defects, the hernias can be classified into two categories: the fenestra type, with defects in both peritoneal layers, and the pouch type, with defects in only one of the two layers.4,11 As seen in the current patient, the viscera may be allowed to pass through the defect with potential hernial strangulation in subjects with fenestra-type hernias; otherwise, such structures may be permitted to enter and become entrapped in the parametrium in patients with pouch-type hernias.4 The most common herniating viscus is the small intestine; less common structures include the sigmoid colon, ovaries, cecum, omentum, appendix, and the ureter.10 The youngest patient ever described was 16 years of age,12 while more than 85% of the cases have occurred in parous women.10 A defect of the broad ligament is often present in a unilateral portion, and several etiological factors for such defects have been suggested, including trauma during pregnancy or delivery, surgical injury, pelvic inflammatory disease, and congenital anomalies.4,10–14 In the current case, the etiology of the disease could be multifactorial since our patient had a history of pregnancy, delivery, and abdominal surgery. Although it is difficult to determine the precise contributions of each factor, we believe that the patient’s previous hysterectomy likely played a major role in the formation of the defect in the residual broad ligament. The tractive and/or stretching nature of PD, which is characterized by increased intra-abdominal pressure due to retention of dialysate, may have played an additional role in exacerbating the ligament fenestration, thereby predisposing our patient to the disease.
Hernias of the broad ligament have often been discovered at laparotomy for other reasons, and unless the defect is suspected after previous uteropexy the precise preoperative diagnosis of the disease is quite uncommon.10,15 This was also the case in the current patient. Indeed, a combination of the patient’s medical history, which included a hysterectomy and an abdominal X-ray that showed the dilated loops of the bowel, encouraged us to initially attribute the illness to postoperative adhesion. Plain film radiography does not help with the specific diagnosis because of its low sensitivity and specificity.16 Barium enema or other radiologic modalities, including CT, may occasionally lead to a correct diagnosis.10,17,18 The workup with the imaging analyses was not sufficient to allow a preoperative diagnosis of broad ligament herniation; however, the persistent ileus with the closed-loop obstruction, a CT finding that is suggestive of bowel strangulation,9 led us to perform prompt surgical treatment, which likely played a pivotal role in avoiding bowel ischemia, necrosis, and perforation, which would have required intestinal resection and resulted in various degrees of complication.10,19,20 Abdominal wall hernias, localized PD catheter-related adhesions, and sclerosing encapsulating peritonitis, all of which may require prompt surgical intervention, are regarded as disease-specific causes of small bowel obstruction in patients with PD.21–26 We believe that broad ligament herniation should always be regarded as the potential cause for the disease as well, especially in female patients who receive PD. This would lead to a high index of suspicion, prompt recognition, and immediate intervention, which are essential for reducing or preventing major morbidities of the disease.27 Considering the fact that our patient did not require bowel resection, it might have been possible for her to resume PD at an intermittent schedule using low-volume dialysates despite the concerns about the leakage of dialysate and dehiscence because of poor wound healing mediated by abdominal distension.2,28–32 Finally, there are no clear recommendations regarding either the interruption or withdrawal of PD after abdominal surgery,20,31,32 and we gave priority to the patient’s decision. The optimal therapeutic strategy for internal herniation in patients who receive PD may only be determined with the accumulation of experience from a larger number of cases similar to ours.
Footnotes
ACADEMIC EDITOR: Athavale Nandkishor, Associate Editor
PEER REVIEW: Four peer reviewers contributed to the peer review report. Reviewers’ reports totaled 532 words, excluding any confidential comments to the academic editor.
FUNDING: This study was supported in part by a Grant-in-Aid for Research on Advanced Chronic Kidney Disease, Practical Research Project for Renal Diseases, from the Japan Agency for Medical Research and development (AMED). The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Drafted the manuscript: NOT, TA. Contributed to the acquisition of the clinical data: AS, OS, SM, EK. Provided a detailed review of the contents and structure of the manuscript resulting in significant changes to the original document: AS, SM, DN. All authors have read and approved the final manuscript.
REFERENCES
- 1.Miller PA, Mezwa DG, Feczko PJ, Jafri ZH, Madrazo BL. Imaging of abdominal hernias. Radiographics. 1995;15(2):333–47. doi: 10.1148/radiographics.15.2.7761639. [DOI] [PubMed] [Google Scholar]
- 2.Bargman JM. Complications of peritoneal dialysis related to increased intraabdominal pressure. Kidney Int Suppl. 1993;40:S75–80. [PubMed] [Google Scholar]
- 3.García-Ureña MA, Rodríguez CR, Vega Ruiz V, et al. Prevalence and management of hernias in peritoneal dialysis patients. Perit Dial Int. 2006;26(2):198–202. [PubMed] [Google Scholar]
- 4.Takeyama N, Gokan T, Ohgiya Y, et al. CT of internal hernias. Radiographics. 2005;25(4):997–1015. doi: 10.1148/rg.254045035. [DOI] [PubMed] [Google Scholar]
- 5.Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186(3):703–17. doi: 10.2214/AJR.05.0644. [DOI] [PubMed] [Google Scholar]
- 6.Duron JJ, Silva NJ, du Montcel ST, et al. Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg. 2006;244(5):750–7. doi: 10.1097/01.sla.0000225097.60142.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simstein NL. Internal herniation through a defect of the broad ligament. Am Surg. 1987;53(5):258–9. [PubMed] [Google Scholar]
- 8.Megibow AJ, Balthazar EJ, Cho KC, Medwid SW, Birnbaum BA, Noz ME. Bowel obstruction: evaluation with CT. Radiology. 1991;180(2):313–8. doi: 10.1148/radiology.180.2.2068291. [DOI] [PubMed] [Google Scholar]
- 9.Paulson EK, Thompson WM. Review of small-bowel obstruction: the diagnosis and when to worry. Radiology. 2015;275(2):332–42. doi: 10.1148/radiol.15131519. [DOI] [PubMed] [Google Scholar]
- 10.Slezak FA, Schlueter TM. Hernia of the broad ligament. In: Nyhus LM, Conden RE, editors. Hernia. 4th ed. Philaderphia, PA: Lippincott; 1995. pp. 491–7. [Google Scholar]
- 11.Takayama S, Hirokawa T, Sakamoto M, et al. Laparoscopic management of small bowel incarceration caused by a broad ligament defect: report of a case. Surg Today. 2007;37(5):437–9. doi: 10.1007/s00595-006-3397-0. [DOI] [PubMed] [Google Scholar]
- 12.Rose D. Congenital bowel invagination into the broad ligament. Report of a case. Obstet Gynecol. 1963;21:218–9. [PubMed] [Google Scholar]
- 13.Nozoe T, Anai H. Incarceration of small bowel herniation through a defect of the broad ligament of the uterus: report of a case. Surg Today. 2002;32(9):834–5. doi: 10.1007/s005950200162. [DOI] [PubMed] [Google Scholar]
- 14.Haku T, Daidouji K, Kawamura H, Matsuzaki M. Internal herniation through a defect of the broad ligament of the uterus. Abdom Imaging. 2004;29(2):161–3. doi: 10.1007/s00261-003-0065-y. [DOI] [PubMed] [Google Scholar]
- 15.Cleator IG, Bowden WM. Bowel herniation through a defect of the broad ligament. Br J Surg. 1972;59(2):151–3. doi: 10.1002/bjs.1800590221. [DOI] [PubMed] [Google Scholar]
- 16.Agresta F, Michelet I, Candiotto E, Bedin N. Incarcerated internal hernia of the small intestine through a breach of the broad ligament: two cases and a literature review. JSLS. 2007;11(2):255–7. [PMC free article] [PubMed] [Google Scholar]
- 17.Kosaka N, Uematsu H, Kimura H, Yamamori S, Hirano K, Itoh H. Utility of multi-detector CT for pre-operative diagnosis of internal hernia through a defect in the broad ligament (2007: 1b) Eur Radiol. 2007;17(4):1130–3. doi: 10.1007/s00330-006-0449-1. [DOI] [PubMed] [Google Scholar]
- 18.Marraoui W, Petitcolin V, Bros S, Slim K, Garcier JM, Da Ines D. Internal hernia of the broad ligament: CT diagnosis for laparoscopic management. Diagn Interv Imaging. 2012;93(7–8):621–4. doi: 10.1016/j.diii.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 19.Kojima E, Inoue T, Sueyoshi K, et al. Removal of the peritoneal dialysis catheter because of gastrointestinal disease in patients on continuous ambulatory peritoneal dialysis: a single-center case series. Adv Perit Dial. 2011;27:77–81. [PubMed] [Google Scholar]
- 20.Torigoe T, Akiyama Y, Uehara T, Nakayama Y, Yamaguchi K. Laparoscopic colectomy for transverse colon cancer in an automated peritoneal dialysis patient: a case report. Int J Surg Case Rep. 2013;4(7):640–2. doi: 10.1016/j.ijscr.2013.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Varela GG, López-Loredo A, García León JF. Broad ligament hernia-associated bowel obstruction. JSLS. 2007;11(1):127–30. [PMC free article] [PubMed] [Google Scholar]
- 22.O’Connor JP, Rigby RJ, Hardie IR, et al. Abdominal hernias complicating continuous ambulatory peritoneal dialysis. Am J Nephrol. 1986;6(4):271–4. doi: 10.1159/000167174. [DOI] [PubMed] [Google Scholar]
- 23.Chung S, Chang YS, Park CW. Abdominal wall hernia during peritoneal dialysis. QJM. 2010;103(1):57–8. doi: 10.1093/qjmed/hcp080. [DOI] [PubMed] [Google Scholar]
- 24.Huraib SO. Intestinal obstruction as a complication of continuous ambulatory peritoneal dialysis: a case report. Saudi J Kidney Dis Transpl. 1995;6(3):304–7. [PubMed] [Google Scholar]
- 25.Hausmann MJ, Vorobiov M, Ovnat A. Small bowel obstruction due to localized Tenckhoff catheter-related adhesions. Perit Dial Int. 2002;22(3):431–3. [PubMed] [Google Scholar]
- 26.Nomoto Y, Kawaguchi Y, Kubo H, Hirano H, Sakai S, Kurokawa K. Sclerosing encapsulating peritonitis in patients undergoing continuous ambulatory peritoneal dialysis: a report of the Japanese Sclerosing Encapsulating Peritonitis Study Group. Am J Kidney Dis. 1996;28(3):420–7. doi: 10.1016/s0272-6386(96)90501-6. [DOI] [PubMed] [Google Scholar]
- 27.Nazzal MD, Kawamura N, El-Gazzaz G, Spaggiari M, Abu-Elmagd K. Peritoneal decortication: an innovative technique for treatment of obstructive sclerosing encapsulating peritonitis. Am Surg. 2015;81(4):E143–5. [PubMed] [Google Scholar]
- 28.Rocco M. Do abdominal hernias in peritoneal dialysis patients require repair? Semin Dial. 1999;12(5):398. [Google Scholar]
- 29.Del Peso G, Bajo MA, Costero O, et al. Risk factors for abdominal wall complications in peritoneal dialysis patients. Perit Dial Int. 2003;23(3):249–54. [PubMed] [Google Scholar]
- 30.Shah H, Chu M, Bargman JM. Perioperative management of peritoneal dialysis patients undergoing hernia surgery without the use of interim hemodialysis. Perit Dial Int. 2006;26(6):684–7. [PubMed] [Google Scholar]
- 31.Moffat FL, Deitel M, Thompson DA. Abdominal surgery in patients undergoing long-term peritoneal dialysis. Surgery. 1982;92(4):598–604. [PubMed] [Google Scholar]
- 32.Kleinpeter MA, Krane NK. Perioperative management of peritoneal dialysis patients: review of abdominal surgery. Adv Perit Dial. 2006;22:119–23. [PubMed] [Google Scholar]



