Abstract
Patient: Male, 46
Final Diagnosis: Celiac crisis
Symptoms: Abdominal pain • chronic diarrhea • lightheadedness • weakness • weight loss
Medication: —
Clinical Procedure: —
Specialty: Gastroenterology and Hepatology
Objective:
Rare disease
Background:
Celiac disease is a hypersensitivity enteropathy that can have various presentations in adults. Rarely, patients can present with severe lab abnormalities, dehydration and weight loss caused by celiac disease – a celiac crisis.
Case Report:
A 46-year-old male with a past medical history significant for diabetes mellitus, type 2 (DM2) and recently treated Bell’s Palsy presented to the emergency room complaining of weakness, diarrhea and lightheadedness. On presentation, the patient had a systolic blood pressure (SBP) of 60 mm Hg and a lactic acidosis with pH of 7.28. Infectious etiologies of diarrhea were ruled out. The patient had an EGD which showed erythema of the duodenal bulb. Serum anti-gliadin and anti-TTG IgA were both elevated suggesting Celiac disease. Biopsies showed histopathology consistent with celiac disease. The patient’s diarrhea resolved after initiation of a gluten free diet. He gained 25 kilograms after discharge and did not require further hospitalizations for diarrhea.
Conclusions:
Celiac crisis is a very rare presentation of celiac disease in adults but nonetheless should be considered in patients with marked metabolic derangements in the setting of osmotic diarrhea. Treatment consists of a gluten free diet and may require management with steroids and total parenteral nutrition (TPN).
MeSH Keywords: Adult, Celiac Disease, Dehydration, Malnutrition, Weight Loss
Background
Celiac disease is a hypersensitivity enteropathy to the gluten protein that can lead to malabsorption. The disease is usually asymptomatic but common signs and symptoms are diarrhea, abdominal pain, nutrient deficiency and anemia [1–3]. Rarely, patients present with diarrhea causing profound dehydration, weight loss and metabolic abnormalities requiring hospitalization – a celiac crisis. Often, the crisis will take place after an inciting event – usually surgery, infection or pregnancy [4]. Although serological studies can screen for the disease, confirmatory testing in adults still requires EGD with biopsy. Biopsies classically show lymphocytic inflammation, villous atrophy, and crypt hyperplasia. The mainstay of treatment is the initiation of a gluten free diet [5].
Case Report
A 46 year old male with history of DM2, who was recently treated for Bell’s palsy with acyclovir and prednisone presented to the emergency room with symptomatic orthostasis after having five days of crampy left lower quadrant abdominal pain accompanied with up to 20 non-bloody bowel movements per day. On physical exam, he had an SBP of 60 mmHg and was tachycardic to 102. He had mild tenderness to palpation in the left lower quadrant of his abdomen without rebound or guarding. Notable lab abnormalities included: venous blood pH 7.28, Na 130 mmol/L, blood glucose 20.3 mmol/L, albumin 25 g/L, and hemoglobin 110 g/L. A CT Abdomen/Pelvis only showed distal small bowel thickening. Clostridium Difficile PCR and stool ova, parasites, and cultures were all negative. Serum, gastrin and VIP levels and urine 5-HIAA were also within normal limits. Because of continued diarrhea, upper and lower endoscopy were performed. Random biopsies from his colonoscopy showed mild chronic non-specific inflammation. However, his EGD showed linear erythema and erosions in the antrum, pylorus and duodenal bulb as well as scalloping of the second part of the duodenum (Figure 1). Biopsy of the duodenal bulb showed total villous atrophy and crypt hyperplasia (Figure 2) and lymphocytic infiltration (Figure 3). Celiac labs were notable for anti-TTG IgA elevated at 48 Units and anti-gliadin IgA 39 Units (reference range for both: 0–19 Units). Based on biopsy and serology, he was diagnosed with Marsh Stage IIIC celiac disease. He was started on a gluten-free diet and had significant improvement in his symptoms within 48 hours and was able to be discharged home without TPN or steroids. He was able to gain 25 kilograms over four months and did not require further hospitalizations for his diarrhea.
Figure 1.
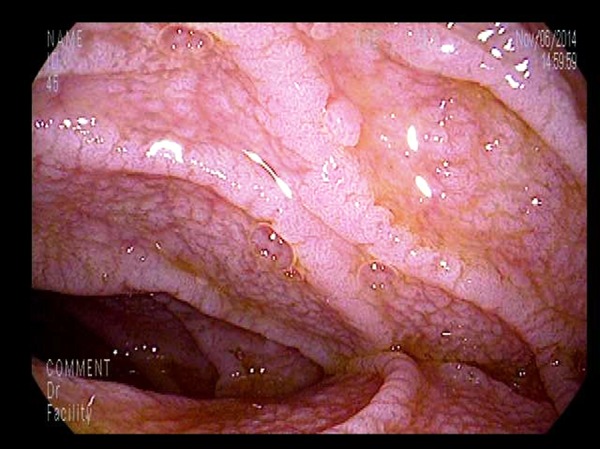
Endoscopic image of the second part of the duodenum; Scalloping is readily evident.
Figure 2.
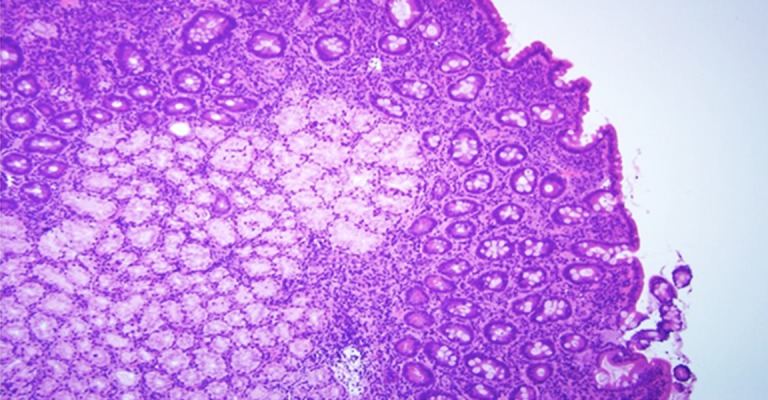
Villous atrophy and crypt hyperplasia present on duodenal biopsy. H&E stain, 20×.
Figure 3.
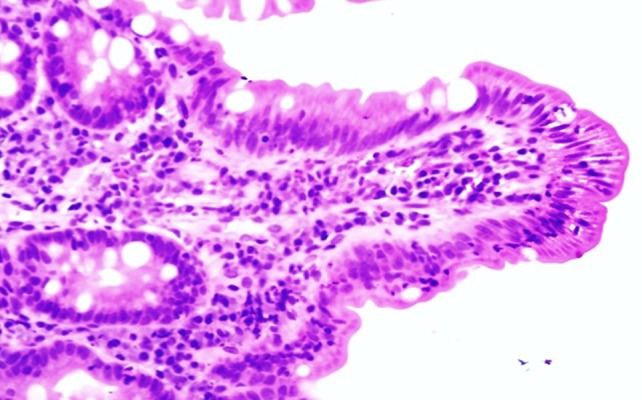
Significantly increased number of intraepithelial lymphocytes present on duodenal biopsy. H&E stain, 60×.
Discussion
Celiac crisis is very rare in adults. Fewer than thirty cases have been documented in the literature and the first case series was published just six years ago.
Adults usually present in their 5th or 6th decade of life. The most common symptoms are diarrhea, vomiting, tetany and lightheadedness with hypocalcemia being the most common metabolic abnormality. Weight loss has been previously documented up to 18 kilograms. Most patients will not be aware that they have Celiac disease before the crisis episode. Although it is still unclear what triggers this more aggressive disease course, current scientific evidence suggests to a combination of severe mucosal inflammation and immune activation. Approximately 50% of patients have an inciting event such as surgery, infection or pregnancy within months of their crisis [4].We believe the trigger in our patient’s case was his recent episode of Bell’s Palsy which was treated with acyclovir and steroids.
The increase in documented cases in non-pediatric patients has led to the proposal of the following diagnostic criteria for celiac crisis in adults [4]:
“Acute onset or rapid progression of gastrointestinal symptoms attributable to celiac disease requiring hospitalization and/or parenteral nutrition along with at least two of the following”:
Signs of severe dehydration – hemodynamic instability or orthostatic hypotension;
Neurologic dysfunction;
Renal dysfunction;
Metabolic acidosis defined as pH <7.35;
Albumin <30 g/L;
Abnormal electrolyte levels;
Weight loss >10 lbs.
Because of the severe presentation of the condition, the most commonly considered alternative diagnosis is infectious diarrhea. Therefore, a history of potential microbial exposures and objective laboratory data to exclude infectious etiologies should be obtained. Other conditions to consider that may mimic celiac disease are tropical sprue, AIDS enteropathy, food protein hypersensitivity, Whipple’s disease, intestinal lymphoma, collagenous sprue, small-bowel bacterial overgrowth, laxative abuse and pancreatic insufficiency [6]. The treatment for celiac crisis involves admission for intravenous hydration, electrolyte repletion and the institution of a gluten-free diet [5]. About half of patients will require the initiation of TPN and/or steroids. Depending on the severity of malnourishment, patients may need to be closely monitored for the development of refeeding syndrome [7]. For those requiring steroids, the mean total length of steroid treatment was 5 months [4]. The time to weight recovery ranges from 8–40 weeks [4] and despite significant morbidity, zero cases of death due to the illness have been reported in adults.
Conclusions
Celiac crisis can be difficult to diagnose in an adult presenting with severe acute diarrhea due to the rarity of the condition. Our case demonstrates the importance of considering this diagnosis as symptoms are likely to persist until a gluten free diet is initiated. Treatment with steroids and TPN can be considered for cases refractory to dietary modification.
Acknowledgments
We would like to thank Dr(s). Suman Setty and Grace Guzman for their interpretation of biopsies and assistance with obtaining digital images.
Footnotes
Statement
No financial disclosures.
References:
- 1.Rubio-Tapia A, Murray JA. Celiac disease. Curr Opin Gastroenterol. 2010;26(2):116–22. doi: 10.1097/MOG.0b013e3283365263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trier JS. Diagnosis of celiac sprue. Gastroenterology. 1998;115(1):211–16. doi: 10.1016/s0016-5085(98)70383-x. [DOI] [PubMed] [Google Scholar]
- 3.Green PH, Cellier C. Celiac disease. N Engl J Med. 2007;357(17):1731–43. doi: 10.1056/NEJMra071600. [DOI] [PubMed] [Google Scholar]
- 4.Jamma S, Rubio-Tapia A, Kelly CP, et al. Celiac crisis is a rare but serious complication of celiac disease in adults. Clin Gastroenterol Hepatol. 2010;8(7):587–90. doi: 10.1016/j.cgh.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolf I, Mouallem M, Farfel Z. Adult celiac disease presented with celiac crisis: Severe diarrhea, hypokalemia, and acidosis. J Clin Gastroenterol. 2000;30(3):324–26. doi: 10.1097/00004836-200004000-00026. [DOI] [PubMed] [Google Scholar]
- 6.Scanlon SA, Murray JA. Update on celiac disease – etiology, differential diagnosis, drug targets, and management advances. Clin Exp Gastroenterol. 2011;4:297–311. doi: 10.2147/CEG.S8315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Almeida Menezes M, Cabral V, Silva lorena SL. Celiac crisis in adults: A case report and review of the literature focusing in the prevention of refeeding syndrome. Rev Esp Enferm Dig. 2016;108 doi: 10.17235/reed.2016.4073/2015. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


