Abstract
Intra-arterial nimodipine (IAN) has shown a promising effect on cerebral vasospasm (CV) after aneurysmal subarachnoid haemorrhage. At our institution, Rigshospitalet, IAN treatment has been used since 2009, but the short- and long-term clinical efficacy of IAN has not yet been assessed. The purpose was to evaluate the efficacy and clinical outcome of IAN treatment of symptomatic CV, and to assess the predictors of clinical outcome. Medical records of 25 patients undergoing a total of 41 IAN treatment sessions were retrospectively reviewed. Data on angiographic results, blood-flow velocities and the clinical condition before and after the IAN treatment were recorded. Predictors of the clinical outcome were assessed with a linear regression model. Positive angiographic response was achieved in 95.1% of 41 IAN treatment sessions. Flow-velocity measurements showed no relationship with angiographic responses of IAN. The immediate clinical improvement was observed in three patients (12%). Five patients (20%) had a favourable outcome at discharge and at three-month follow-up; 10 patients (40%) had a moderate to poor outcome; and the rest (40%) died. Increased number of affected vessels and number of procedures carried out per patient, and a trend toward an increased delay time from symptomatic CV to confirming angiographic CV and thus instituting IAN treatment predicted the poor clinical outcome. IAN treatment appears to be effective in reversing angiographic CV. However, it is not always effective in reversing clinical deterioration, as several other factors including treatment delay affect the clinical course.
Keywords: Subarachnoid haemorrhage, cerebral vasospasm, intra-arterial nimodipine
Introduction
Cerebral vasospasm (CV) is a feared and potentially life-threatening complication in patients following aneurysmal subarachnoid haemorrhage (SAH). Angiographic CV is observed in up to 70% of patients, typically between 4–14 days after the initial bleeding, and leads to symptomatic brain ischaemia and/or new infarction on radiographic imaging in about 30% of these patients.1,2 Treatment of CV and prevention of delayed cerebral ischaemia (DCI) is therefore a main goal in the management of patients surviving from SAH. However, despite maximal contemporary therapy and neurocritical care, about 30% of these patients die, another 30% survive with significant disability, and the rest of them recover with little or no long-term disability.3
Current medical strategies for prevention and treatment of CV including endovascular therapies with vasodilators and triple-H (i.e. hypertension, hypervolaemia, haemodilution) are suboptimal,2,4–8 as the exact mechanisms leading to CV are not yet fully elucidated.2,9 At the moment, nimodipine, a calcium channel blocker, remains the only drug proved by the US Food and Drug Administration, which is recommended as the first-line treatment and prevention of CV and improvement of outcomes after SAH.10,11 Although nimodipine exhibits neuroprotective as well as vasodilatory benefits,2 some patients deteriorate further and develop severe symptomatic CV. In the last decade, a number of clinical trials have investigated nimodipine infused directly in the spastic arteries (intra-arterial nimodipine (IAN)), and found it to be effective in reversing angiographic CV, although overall clinical outcome differs through the literature.12–18 At our institution, Rigshospitalet, IAN treatment has been used as the method of choice since 2009 whenever endovascular treatment of CV was indicated. However, the short- and long-term clinical efficacy of IAN has not yet been assessed.
The purpose of this study was to retrospectively evaluate the efficacy and clinical outcome of IAN treatment of symptomatic CV, which is refractory to the haemodynamic treatment, and to assess the predictors of the clinical outcome.
Materials and methods
Data collection
Between December 2009–May 2012, 325 adults with evidence of SAH on computerized tomography (CT) scan were admitted to the neurosurgical intensive care unit (ICU) at the University Hospital, Rigshospitalet, in Copenhagen, Denmark. Only patients presenting with a ruptured intracranial aneurysm on CT angiogram (CTA), suffering from symptomatic CV refractory to the haemodynamic therapy, and receiving IAN treatment were reviewed. Twenty-eight patients were identified. Among them, three patients were treated with a combination of percutaneous transluminal angioplasty (PTA) and IAN, and were excluded to avoid confound bias on clinical outcome, as PTA has also shown to have beneficial effect.19 A total of 25 patients met the inclusion criteria and constituted the study population. Data on these patients was extracted from a computerized database and reviewed retrospectively including demographic data, clinical condition at admission based on World Federation of Neurological Surgeons (WFNS) grade I–V,20 amount and distribution of subarachnoid blood detected by admission CT by using the modified Fisher scale 1–4,21 and aneurysm location as well as aneurysm treatment. Onset, location and severity of CV, number of affected vessels, procedure specifics such as dosage of IAN per vessel and per procedure, and number of repeated procedures were recorded. To assess the efficacy of IAN treatment, the clinical response within 24 h (e.g. level of consciousness based on Glasgow Coma Scale (GCS) and neurological condition), the angiographic response as well as effects on blood flow-velocity of the middle cerebral artery (MCA) determined by transcranial Doppler (TCD) ultrasonography were examined. The clinical outcome was assessed using the modified Rankin scale (mRS) score at discharge and at three-month follow-up.22 Informed consent was obtained from patients or legal representative for patients with impaired consciousness at the time of their clinical work-up. The Board of Health Committee and Data inspectorate approved the study. All the necessary precautions were taken to protect the identities of the patients in the study.
Patient management and monitoring
All patients underwent either surgical or endovascular obliteration of the ruptured aneurysm within 48 h after the initial bleeding except seven patients who were hospitalized 3–14 days after onset of SAH. Nimodipine was administrated, orally or intravenously, in a dose of 60 mg every 4 h in 21 days according to a standardized SAH-protocol. Maintenance of euvolaemia was achieved by administration of intravenous isotonic crystalloid. When flow-velocity of the MCA exceeded 120 cm/s (a TCD cut-off value), triple-H therapy was initiated for inducing prophylactic hypervolaemia and elevating the mean arterial pressure by 20%. Flow-velocity measurements were performed at least once daily to monitor possible vasospastic activity. Flow-velocity <120 cm/s was defined as normal, 120–150 cm/s as mild, 150–200 cm/s as moderate and >200 cm/s as severe. Lindegaard ratio was not measured routinely in all patients, and is therefore not mentioned further in the study. The clinical condition was assessed by continuous neurological examinations including GCS scores.
Diagnosis of CV and IAN treatment
Cerebral vasospasm was suspected, if patients demonstrated at least one of the following: (a) a decreased level of consciousness and/or disorientation with a decrease of at least two points on the GCS score from baseline, (b) new focal neurological deficits (cranial nerve palsy, hemiparesis and/or speech disturbances), and/or (c) flow-velocity >120 cm/s. Neurological deterioration was the main trigger for suspicion of CV, followed by an increase in flow-velocity; the last was mainly applied to patients with ventilator support. Possible causes of neurological deterioration such as presence of ischaemia, re-bleeding or hydrocephalus on CT scan, electrolyte disturbance, seizures or hypoxia were eliminated prior to CTA, which was usually performed within 24 h of onset of symptomatic CV. Degree of angiographic CV was assessed on a digital subtraction angiography semi-quantitatively and subjectively and classified as ‘none/mild’ when arterial narrowing was <25% of the arterial diameter, ‘moderate’ when narrowing was 25–50%, or ‘severe’ when narrowing >50%.
Patients were found eligible for IAN treatment only if they showed angiographic CV in territories compatible with their neurological deficits and/or with elevated mean flow-velocity. After dilution with 0.9% saline to obtain a solution of 0.01 mg/ml, nimodipine was administrated as an infusion over 20–40 minutes through a microcatheter placed in the affected vessel. Post-nimodipine angiograms were performed 10–30 min after each session. Two neuroradiologists evaluated the angiographic results separately, and disagreement was resolved by consensus. Each vessel was evaluated as ‘responsive’ or ‘non-responsive’, and the overall angiographic result was graded as ‘good response’, ‘no response’ or ‘mixed response’. If persistence or recurrence of CV was suspected, a new CTA was performed, and IAN treatment was repeated after the verification of angiographic CV and progressive neurological deterioration.
Clinical evaluation
Immediate clinical response and flow-velocity measurements within 24 h after IAN treatment were recorded. The change in the clinical condition was graded as ‘improved’, ‘unchanged’ or ‘worsened’. The clinical outcome at discharge from the hospital and at three-month follow-up was assessed using the mRS score (no questionnaire).22 A score ≤2 was considered as a good outcome.
Statistical analysis
Data analysis was performed with the statistical software package IBM SPSS version 20.0. Descriptive data was presented as median values with interquartile range (IQR) in parentheses, as data was not normally distributed. A p-value of less than 0.05 was accepted as statistically significant. Our primary dependent variable was mRS score, which was investigated in a linear regression model based on following predictor variables: age, WFNS grade, Fisher scale, aneurysm location, severity of CV, number of affected vessels, angiographic response and number of repeated procedures. Significance of time delay in diagnosis of angiographic CV and thus instituting IAN treatment was assessed as well.
Results
Clinical assessment
Demographic data, WFNS grade, Fisher scale, and location of aneurysm are presented in Table 1. Surgical clipping was performed in seven (28%) patients and endovascular occlusion was performed in 18 (72%) patients. All patients developed neurological deterioration such as decreased level of consciousness, hemiparesis, aphasia or other new focal neurological signs between 4–13 days after onset of SAH (median, eight days; IQR 6–9 days). Among them, two (8%) patients already had neurological deficits at the time of aneurysm treatment and one (4%) due to carotid artery dissection two days prior to symptomatic CV. One (4%) patient (no. 17) was admitted to the hospital 14 days after the initial bleeding and already had developed left-sided arm paresis and leg paralysis due to CV. In one (4%) patient (no. 15), who was artificially ventilated, the suspicion of CV was raised by elevated flow-velocity measurements only, which was the main indication for angiography. The neurological deterioration did not respond to the haemodynamic treatment. Onset of occurrence of CV and neurological deterioration including flow-velocity measurements are summarized in Table 2.
Table 1.
Patient characteristics.
| Demographic data | |
| Age, median (years) | 52 |
| Female sex, no. (%) | 20 (80%) |
| Risk factors, no. (%) | |
| Hypertension | 13 (52%) |
| Smoking | 14 (56%) |
| Alcohol abuse | 3 (12%) |
| Drug abuse | 1 (4%) |
| WFNS grade I–V, no. (%) | |
| I, II and III | 15 (60%) |
| IV and V | 10 (40%) |
| Fisher grade 1–4, no. (%) | |
| 1 and 2 | 3 (12%) |
| 3 and 4 | 22 (88%) |
| Location of aneurysm, no. (%) | |
| ACoA | 9 (36%) |
| ACA | 2 (8%) |
| MCA | 4 (16%) |
| ICA | 4 (16%) |
| PCA | 1 (4%) |
| BA | 4 (16%) |
| PICA | 1 (4%) |
| Surgical or endovascular obliteration, no. (%) | |
| Coils | 14 (56%) |
| Clips | 7 (28%) |
| Stent | 3 (12%) |
| Coils/stent | 1 (4%) |
ACA: anterior cerebral artery; ACoA: anterior communicating artery; BA: basilar artery; CV: cerebral vasospasm; ICA: internal cerebral artery; MCA: middle cerebral artery; PCA: posterior cerebral artery; PICA: posterior inferior cerebral artery; WFNS: World Federation of Neurological Surgeons.
Table 2.
The severity of cerebral vasospasm (CV) and location, neurological deficit including flow velocity (FV), angiographic and clinical responses to the intra-arterial nimodipine (IAN) treatment and clinical outcome at discharge and at three-month follow-up (FU).
| Patient/ session no. | Onset of sCV (day) | Neurological deficits | Location of aCV | Severity of aCV | IAN dose per session (mg) | Angiographic response | Clinical response | mRS scores at | |
|---|---|---|---|---|---|---|---|---|---|
| Discharge | 3-month FU | ||||||||
| 1.1 | 10 | L hemiparesis, 5 days later R hemiparesis, FV 70 cm/s | L MCA, ACA, ICA | Severe | 3.0 | Good | Worsened | ||
| 1.2 | +Aphasia, FV 178 cm/s | L MCA, ACA, ICA | Severe | 3.0 | Good | Unchanged | |||
| 1.3 | Sedated, FV 190 cm/s | L MCA, ACA, ICA | Severe | 3.0 | Mixed response | Unchanged | 5 | 4 | |
| 2.1 | 9 | Fluctuating DLC, L arm paresis, FV 182 cm/s | MCAs, ACAs, ICAs | Severe | 4.0 | Good | Worsened | ||
| 2.2 | +Seizures, FV 260 cm/s | ACAs, MCA | Severe | 4.0 | Good | Worsened | 4 | 3 | |
| 3.1 | 11 | Fluctuating DLC, FV 187 cm/s | R MCA | Moderate | 3.2 | No response | Unchanged | 1 | 0 |
| 4.1 | 7 | R hemiparesis, facial nerve palsy, visual axis deviation, FV 100 cm/s | L ACA, MCA | Moderate | 4.0 | Good | Unchanged | 5 | 4 |
| 5.1 | 9 | Fluctuating DLC, L leg paresis, FV 193 cm/s | PCT | Severe | 4.0 | Good | Worsened | 6 | – |
| 6.1 | 5 | Fluctuating DLC, aphasia, FV 180 cm/s | L MCA, ACAs, ICAs | Severe | 4.0 | Good | Worsened | 6 | – |
| 7.1 | 11 | Fluctuating DLC | L MCA, MCAs, ICAs, PCT | Severe | 4.0 | Mixed response | Unchanged | ||
| 7.2 | +FV 97 cm/s | R ACA, MCA, ICA | Severe | 2.0 | Good | Unchanged | 5 | 3 | |
| 8.1 | 6 | Fluctuating DLC aphasia, FV 348 cm/s | ACAs, MCAs, ICAs, PCT | Severe | 4.0 | Good | Worsened | ||
| 8.2 | Sedated | ACAs, MCAs, ICAs, PCT | Severe | 6.0 | Good | Worsened | 5 | 6 | |
| 9.1 | 5 | DLC, L hemiparesis facial nerve palsy, aphasia, FV 235 cm/s | ACAs, MCAs, ICAs | Severe | 6.0 | Good | Worsened | ||
| 9.2 | Sedated | ACAs, MCAs, ICAs | Severe | 6.0 | Good | Unchanged | 5 | 3 | |
| 10.1 | 5 | DLC, R hemiparesis, aphasia | ACAs, MCAs, ICAs | Severe | 4.8 | Good | Unchanged | ||
| 10.2 | DLC, R hemiparesis, aphasia | ACAs, MCAs, ICAs | Severe | 5.0 | Mixed response | Unchanged | 5 | 1 | |
| 11.1 | 7 | Fluctuating DLC, R hemiparesis, aphasia | PCT | Moderate | 4.0 | Good | Unchanged | ||
| 11.2 | +Visial axis deviation | PCT | Severe | 4.0 | Good | Unchanged | 4 | 3 | |
| 12.1 | 10 | DLC, FV 156 cm/s | R ACA, MCAs, ICAs | Severe | 3.0 | Good | Unchanged | 6 | – |
| 13.1 | 11 | DLC, R hemiparesis, FV 190 cm/s | ACA, MCAs, ICA | Moderate | 4.4 | Good | Unchanged | ||
| 13.2 | DLC, R hemiparesis | ACAs, MCAs, ICAs | Moderate | 5.0 | Good | Worsened | 6 | – | |
| 14.1a | 6 | DLC, R hemiparesis, facial nerve palsy, aphasia, FV 230 cm/s | ACAs, MCAs, ICAs | Severe | 4.0 | Good | Worsened | 6 | – |
| 15.1 | 9 | Sedated, FV 230 cm/s | ACAs, MCAs, ICAs | Severe | 5.0 | Mixed response | Worsened | 6 | – |
| 16.1 | 9 | Fluctuating DLC, FV 183 cm/s | ACAs | Moderate | 4.5 | Mixed response | Unchanged | 3 | 2 |
| 17.1 | 13 | L hemiparesis/paralysis | ACAs, MCAs, ICAs | Severe | 4.0 | Good | Worsened | ||
| 17.2 | +Aphasia, FV 250 cm/s | R ACA, MCA, ICA, PCT | Severe | 4.0 | Good | Worsened | 6 | – | |
| 18.1 | 8 | DLC, aphasia, FV 145 cm/s | ACAs, MCAs, ICAs | Severe | 5.0 | Good | Unchanged | ||
| 18.2 | +FV 313 cm/s | L MCA, ICA, ACAs | Severe | 4.0 | Good | Unchanged | |||
| 18.3 | Sedated, FV 257 cm/s | ACAs, MCAs, ICAs | Severe | 5.0 | Good | Unchanged | |||
| 18.4 | Sedated, FV 290 cm/s | L ACA, MCA, ICA | Severe | 4.0 | Mixed response | Unchanged | 5 | 5 | |
| 19.1 | 8 | DLC, aphasia, FV 226 cm/s | L MCA | Moderate | 4.0 | No response | Improved | 3 | 2 |
| 20.1 | 5 | Pronation/extension pattern, FV 110 cm/s | R ACA, MCA, ICA | Moderate | 3.0 | Good | Worsened | ||
| 20.2 | +R hemiparalysis, L arm paresis, FV 130 cm/s | R ACA, MCA, ICA | Severe | 3.0 | Good | Unchanged | 5 | 3 | |
| 21.1 | 9 | DLC, FV 180 cm 7s | ACAs, ICAs | Severe | 4.0 | Good | Improved | 4 | 2 |
| 22.1 | 6 | DLC, aphasia | L ACA, ICA, MCAs | Moderate | 4.0 | Good | Unchanged | 5 | 4 |
| 23.1 | 6 | DLC | L ACA, MCAs, ICAs | Severe | 4.0 | Mixed response | Improved | 5 | 3 |
| 24.1 | 4 | DLC | ACAs, MCAs, ICAs, PCT | Severe | 6.0 | Good | Unchanged | ||
| 24.2 | +R hemiparesis, FV 200 cm/s | ACAs, MCAs, ICAs, PCT | Severe | 6.0 | Good | Worsened | 6 | – | |
| 25.1 | 6 | DLC, FV 197 cm/s | L ICA, ACAs, MCAs, PCT | Moderate | 6.0 | Mixed response | Worsened | ||
| 25.2 | +R hemiparesis, extensor plantar reflex, FV 237 cm/s | L ACA, MCA, ICA, PCT | Moderate | 6.0 | Good | Worsened | 6 | – | |
ACA: anterior cerebral artery; aCV: angiographic cerebral vasospasm; DLC: decreased level of consciousness; FU: follow-up; IAN: intra-arterial nimodipine; ICA: internal cerebral artery; L: left circulation; MCA: middle cerebral artery; PCT: posterior circulatory territory; R: right circulation; sCV: symptomatic cerebral vasospasm.
By accident IAN injected in the right ICA for a few seconds causing transient drop in blood pressure. The treatment is repeated with the same dose.
Angiography and IAN treatment
Diagnostic cerebral angiography was performed within 24 h after onset of symptomatic CV in all patients except nine (36%), in whom it was performed later due to their fluctuating neurological condition. The median time delay from the occurrence of symptomatic CV to CTA was 14.5 h (IQR, 2.9–38.1 h). In most cases, angiographic CV diffusely involved all vessels on both sides of the circulation, while in six cases (24%) only one side was affected involving 1–3 vessels. Overall, the degree of CV was severe in 16 (64%) patients and moderate in nine (36%). No one had a mild degree of CV. In addition, seven (28%) patients showed signs of incipient hypodensities on their CT scans. Using a linear regression model with a significance p = 0.048; adjusted R2 = 0.241, severity of CV was significant associated with an increased number of affected vessels (p = 0.004), but not with age (p = 0.50), Fisher scale (p = 0.85) and aneurysm treatment (p = 0.54). Severity of CV and number of affected vessels including anatomic distribution are presented in Table 2.
Forty-one IAN treatment sessions were performed in 25 patients (range, 1-4 treatment sessions per patient), in which 173 vessels were evaluated. The median time delay from angiographic CV to IAN treatment was 3.0 h (IQR, 2–9.5 h). Median dose of nimodipine was 4 mg per session (range, 2–6 mg per session), while the largest single dose per vessel was 4 mg (median, 2 mg; range, 1–4 mg). Complete reversal of CV was successfully achieved in 31 (75.6%) treatments (Figure 1); partial reversal was noted in eight (19.5%) (Figure 2), while two (4.9%) showed no effect. There was no significant correlation between the degree of CV and angiographic response to IAN (p = 0.24). Worsening of CV did not occur during the procedures. No signs of haemodynamic instability due to IAN infusion or other procedure-related complications were observed. However, in one (4%) patient (no. 14), a dosage of 2 mg nimodipine was accidently injected in a few seconds causing transient drop in blood pressure. Dose per procedure, number of repeated procedures and angiographic effects are summarized in Table 2.
Figure 1.
Patient no. 24. Lateral angiogram of the internal cerebral artery (ICA) showing (a) cerebral vasospasm (CV); (b) after intra-arterial nimodipine (IAN) infusion, an increase in diameter of the vessels is observed.
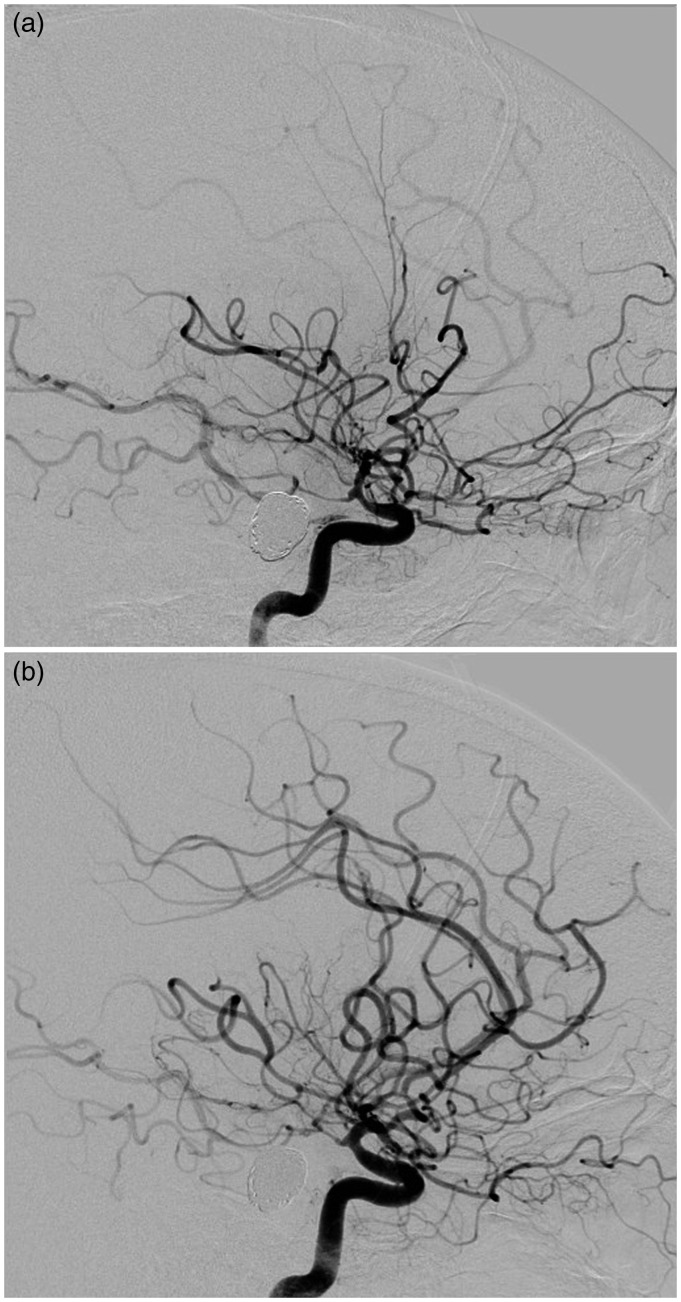
Figure 2.
Patient no. 12. Anteroposterior angiograms of (a) the left and (b) right internal cerebral arteries (ICAs) showing cerebral vasospasm (CV). After intra-arterial nimodipine (IAN) infusion, (c) the left side demonstrates an increase in diameter of the vessels, while (d) the right side shows a mixed response.
TCD measurements
Complete results for flow-velocity measurements before and after IAN treatment within 24 h were available for review in only 13 (32%) of 41 procedures. Mean velocities decreased by 37 cm/s in eight (20%) procedures, unchanged in one (2%), and increased by 34 cm/s in four (10%). There was no correlation between flow-velocity measurements and angiographic responses to IAN.
Clinical evaluation within 24 h after treatment, at discharge and at three-month follow-up
The clinical condition remained unchanged for 12 (48%) patients, although all of them but one showed angiographic response to IAN treatment. Three (12%) patients showed clinical improvement based on GCS scores and/or neurologically, two of them with none and mixed responses to IAN. Ten (40%) patients experienced a worsening in their clinical conditions both consciously and neurologically; among them, six (24%) had developed new neurological deficits. Two (8%) had seizures at the time of wake-up call. Three (12%) patients never regained consciousness and died a few days later; all three had showed angiographic response to IAN, two of them with mixed response. In 12 (48%) patients, new cerebral infarctions were observed on CT scan hours to a few days after the IAN treatment.
At discharge, only one (4%) patient showed a good clinical outcome (mRS 1). Two (8%) patients had a moderate outcome (mRS 3) and 13 (52%) a poor outcome (mRS 4–5). Nine (36%) patients died during hospitalization, eight (32%) of them as a consequence of extensive cerebral infarction secondary to CV (mRS 6). At the three-month follow-up, another four (16%) patients showed a favourable outcome (mRS 1–2), six (24%) had a moderate outcome (mRS 3), and one more (4%) had died (mRS 6). Data on the clinical evaluation is presented in Table 2.
Observing a linear regression model (p = 0.007, adjusted R2 = 0.654), significant predictors of a poorer clinical outcome (mRS 4–6) were an increased number of affected vessels (p = 0.003) and an increased number of procedures carried out per patient (p = 0.04), and the angiographic response of IAN (p = 0.01). Looking at the time frame from symptomatic CV to confirming angiographic CV, we saw a trend toward a poorer clinical outcome with increasing time (p = 0.13).
Discussion
Cerebral vasospasm following an aneurysmal SAH continues to be a leading cause of morbidity and mortality.3 We retrospectively reviewed 25 patients treated with IAN infusions for medically refractory symptomatic CV, and found that IAN treatment was effective in reducing angiographic CV in 95.1% of 41 treatment sessions, with complete reversal in 75.6% and partial reversal in 19.5%. However, the efficacy of treatment was temporary, and required repeated treatment sessions in 13 (52%) patients, and was not always followed by clinical improvement. Only three (12%) patients demonstrated an immediate clinical improvement after treatment, and only one (4%) had a good clinical outcome at the time of discharge. Eight (32%) of nine deceased patients died during hospitalization. At three-month follow-up, another four (16%) patients showed a clinical improvement, while one (4%) more had died. Overall, five (20%) patients had a favourable long-term outcome (mRS 0–2), 10 (40%) had moderate to poor outcome (mRS 3–5), and 10 (40%) patients had died (mRS 6) (Table 2).
Several clinical trials have evaluated the efficacy of IAN treatment for symptomatic CV.12–18 These studies have reported post-IAN angiographic vessel dilatation in 43.3–82.8% of sessions, clinical improvement in 11.1–88.9% of patients, and 61.1–88.9% with a favourable short- or long-term outcome (Table 3). Biondi et al.12 were the first to assess the efficacy of IAN. The authors reported post-IAN angiographic response in 13 (43.3%) of 30 treatment sessions and clinical improvement in 19 (76%) of 25 patients. Eighteen (72%) had a favourable long-term outcome (mRS 0–2). Their angiographic results are in line with our study. We reported complete reversal of angiographic CV in 75.6% of sessions, and in addition partial reversal of CV was seen in 19.5%. However, our angiographic results did not correlate with the clinical improvement and the overall clinical outcome was less satisfactory, compared to Biondi et al.12 Hänggi et al.15 investigated the efficacy of IAN in 26 patients as well. In eight (31%) patients, no angiographic improvement was seen, and therefore these were excluded from the study. Using cerebral perfusion CT (PCT), the authors reported an improved time to peak and mean transit time a day after the procedure. Although the efficacy of IAN was transient, and 11 (61%) of 18 patients developed additional infarction, 11 (61%) patients revealed a good clinical condition at time of discharge, which is remarkable compared to our study. However, some of these studies are confounded by the combined use of IAN and papaverine or balloon angioplasty, which might explain in part for the clinical improvement reported in the studies.14–16
Table 3.
Studies with cerebral vasospasm (CV) after aneurysmal subarachnoid haemorrhage (SAH) and intra-arterial nimodipine (IAN) treatment.
| Author/year | Study design | Patient no. | Session no. | Dose of IAN per vessel | Angiographic improvement | Clinical improvement | The clinical outcome (mRS≤2 and GOS≥4) at discharge | The clinical outcome (mRS≤2 and GOS≥4) at follow-up |
|---|---|---|---|---|---|---|---|---|
| Biondi et al., 200412 | Retrospective | 25 | 30 | 1–3 mg | 43.3% | 76% | – | 72% |
| Cho et al., 201113 | Retrospective | 42 | 101 | 3–6 mg | 82.2% | 68.3% | 76.2% | 84.6% |
| Dehdashti et al., 201114 | Retrospective | 10 | 15 | 1–4 mg | 80% | 60% | – | 70% |
| Hänggi et al., 200815,a | Prospective | 18 | 26 | 0.8–3.2 mg | 77.3% | 11.1% | 61.1% | 61.1% |
| Hui and Lau, 200516,b | Retrospective | 9 | 10 | 2–4 mg | 66.6% | 88.9% | 88.9% | 77.8% |
| Kim et al., 200917 | Retrospective | 19 | 53 | 1–3 mg | 79.2% | 68.4% | 78.9% | – |
| Kim et al., 201218 | Prospective | 29 | 29 | 1–3 mg | 82.8% | 72.4% | 75.9% | – |
| Our study, 2015 | Retrospective | 28 | 45 | 1–4 mg | 95.6% | 21.4% | 10.7% | 28.6% |
GOS: Glasgow Outcome Scale; mRS: modified Rankin scale.
Only 18 of 26 patients and 22 of 42 procedures are included in the analysis due to no measurable angiographic effect in 20 (47.6%) procedures among eight (30.7%) patients.
The mean percentage increase in arterial diameter.
Angiographic improvement includes results with moderate and major effect.
We are the second group of researchers to evaluate the influence of time delay in diagnosing and instituting the IAN treatment after onset of symptomatic CV. In our study, an increasing time delay from symptomatic CV to angiographic CV showed a trend toward a poorer outcome with a median time of 14.5 h. The median delay time from angiographic CV to the IAN treatment was 3.0 h. Grotenhuis et al.23 was the first to report that the IAN treatment was ineffective when administrated only a few hours after the onset of CV. However, the authors used only small dosage of nimodipine ranging from 0.068–1.0 mg, which could account at least in part for the observed lack of effect. Biondi et al.12 performed the diagnostic CTA and IAN treatment within 24 h of onset of symptomatic CV, with the mean delay time of 18 ± 6 h. The dosage of IAN per vessel consisted of 1–3 mg. Despite time delay in the diagnostic process, thus instituting the treatment, the authors demonstrated a clinical improvement in 76% of patients after IAN. Similarly, Linfante et al.7 investigated the efficacy of IA nicardipine in 22 patients. A total of 46 endovascular sessions with intra-arterial nicardipine were performed within 48 h after onset of symptoms in 21 patients, and within 72 h in one patient. At the time of discharge, half of patients were reported to be independent functionally (mRS 0–2). In our study, time delays were much less than reported by Biondi et al.12 and Linfante et al.7 and with a dosage of IAN per vessel (range, 1–4 mg) similar to Biondi et al.12 However, despite angiographic response in 95.1% of treatment sessions only a few patients showed clinical improvement. The discrepancy between angiographic response and unsatisfactory clinical results could be explained by the fact that parenchymal damage has already occurred due to ischaemia resulting from CV in spite of angiographic response to endovascular treatment with IAN. Furthermore, evidence from a rat model indicated that reperfusion of parenchyma injured by an ischaemic insult might lead to further injury;24–26 this phenomenon could be one of the reasons why the uses of endovascular therapies are associated with a poorer outcome despite substantial vessel dilatation in some instances, as seen in our study.
TCD is often used as a surrogate diagnostic tool to detect CV. We found no correlation between flow-velocities and angiographic responses to IAN, although data of TCD measurements was missing in most cases. Kim et al.17 observed a decrease in flow-velocity in 29 of 33 sessions. In contrast, Hänggi et al.15 noticed a significant increase in flow-velocity one day after IAN infusion (p = 0.03). Wolf et al.27 was unable to detect CV with TCD in two patients and reflect the treatment course in four patients. The interpretation of the TCD analysis leaves some room for speculation. Estimation of flow-velocity could vary from minute to minute, and might be influenced by anatomic details such as vascular anatomy, vessel diameters and cerebral blood flow. Influence of pathological conditions such as an increased intracranial pressure or oedema, or systemic haemodynamic effects during triple-H therapy such as changes in cardiac output or blood pressure could affect the speed and waveform of cerebral blood flow as well. In addition, the accuracy of this technique is quite operator-dependent with high intra-variability, and suboptimal insonation might inhibit the detection of high flow-velocities.28–30 Vora et al.31 reported that only very low or very high MCA velocities (e.g. <120 cm/s or >200 cm/s) negatively or positively predicted angiographic and symptomatic CV in a reliable manner, and intermediate velocities had a lower predictive value and were poorly discriminative.
Vasodilatation by intra-arterial drug infusion also has been performed with other agents. Papaverine is the first intra-arterial agent reported to reverse angiographic CV.6 However, it is associated with a considerable number of several adverse side effects such as elevation of intracranial pressure,32 worsening of CV33 and thrombocytopaenia.34 One study compared the angiographic effect of papaverine and nimodipine and reported that there was no significant difference between these two groups, although the effect of papaverine was more pronounced, dilating at least one vessel in every patient, while nimodipine was ineffective in 16% of patients.35 Intra-arterial nicardipine infusion has shown to be effective without increasing intracranial pressure.36 However, a transient decrease in blood pressure and an increase in heart rate may occur.7,36 Intra-arterial verapamil infusion is also reported to dilate spastic vessels without causing changes in haemodynamic circulation or intracranial pressure.6 However, it needs to be evaluated in larger series to confirm its efficacy. PTA is highly effective in relieving focal CV, and has a continuous effect on narrowed vessels. However, the technique is limited to proximal vessels, and requires expert neurointerventionists due to the significant risks of artery rupture, dissection and local thrombosis.19,37 One study compared the clinical outcome of IAN treatment with PTA, but the authors did not find significant differences in these two groups.38
Limitations
The study has several important limitations including its retrospective design and the small number of patients due to it being a single centre study, which may limit generalizability. There was no control group. It is not clear whether the change in the clinical condition after IAN infusion was due to the effect of the treatment or just a natural course. Quantitative measurement of vessel diameter on pre- and post-nimodipine angiograms was not available as mm (±standard deviation), but only as ±effect. TCD data were missing before and after IAN infusions in several patients making it more difficult to estimate the absolute correlation between TCD and angiographic results. Data on monitoring systemic haemodynamic effects and intracranial pressure during IAN sessions were not investigated, and therefore we were unable to quantify the effect of IAN on these areas.
Conclusion and perspectives
Although there are several limits in this retrospective study, we can conclude that IAN treatment appears to be effective in reversing angiographic CV. However, the relationship between angiographic and clinical responses was not convincing, as the treatment is ineffective in reversing clinical deterioration caused by DCI. Several factors such as increased numbers of affected vessels and procedures carried out per patient predicted the clinical outcome negatively. In addition, an increasing time delay in diagnostic process of CV and thus instituting treatment might contribute to a poorer clinical outcome. Clearly, early detection and rapid treatment of CV are needed before ischaemic damage occurs. Future studies with continued assessment of cerebral blood flow might help optimize the timing of IAN treatment and to assess the real efficacy of the IAN treatment in patients with symptomatic CV after SAH.
Acknowledgements
The study is dedicated to the late Professor Bertil Romner, Department of Neurosurgery, Rigshospitalet, who originally conceived and designed the study. A Bashir and the late Bertil Romner conceived and designed the study. A Bashir reviewed patient data and wrote the first and subsequent drafts of the manuscript. A Wagner and M Cortsen evaluated pre- and post-angiograms. M Andresen conducted the statistical analysis. J Bartek Jr, M Andresen, A Wagner, M Cortsen and V Eskesen participated in critical revision and writing of the article. All authors have seen and approved the final version.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2012; 43: 1711–1737. [DOI] [PubMed] [Google Scholar]
- 2.Treggiari-Venzi MM, Suter PM, Romand J-A. Review of medical prevention of vasospasm after aneurysmal subarachnoid hemorrhage: a problem of neurointensive care. Neurosurgery 2001; 48: 249–262. [DOI] [PubMed] [Google Scholar]
- 3.Washington CW, Zipfel GJ. Detection and monitoring of vasospasm and delayed cerebral ischemia: a review and assessment of the literature. Neurocrit Care 2011; 15: 312–317. [DOI] [PubMed] [Google Scholar]
- 4.Clouston JE, Numaguchi Y, Zoarski GH, et al. Intraarterial papaverine infusion for cerebral vasospasm after subarachnoid hemorrhage. AJNR Am J Neuroradiol 1995; 16: 27–38. [PMC free article] [PubMed] [Google Scholar]
- 5.Fraticelli AT, Cholley BP, Losser M-R, et al. Milrinone for the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke 2008; 39: 893–898. [DOI] [PubMed] [Google Scholar]
- 6.Keuskamp J, Murali R, Chao KH. High-dose intraarterial verapamil in the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Neurosurg 2008; 108: 458–463. [DOI] [PubMed] [Google Scholar]
- 7.Linfante I, Delgado-Mederos R, Andreone V, et al. Angiographic and hemodynamic effect of high concentration of intraarterial nicardipine in cerebral vasospasm. Neurosurgery 2008; 63: 1080–1087. [DOI] [PubMed] [Google Scholar]
- 8.Treggiari MM, Walder B, Suter PM, et al. Systematic review of the prevention of delayed ischemic neurological deficits with hypertension, hypervolemia, and hemodilution therapy following subarachnoid hemorrhage. J Neurosurg 2003; 98: 978–984. [DOI] [PubMed] [Google Scholar]
- 9.Kassell NF, Sasaki T, Colohan AR, et al. Cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Stroke 1985; 16: 562–572. [DOI] [PubMed] [Google Scholar]
- 10.Barker FG, 2nd, Ogilvy CS. Efficacy of prophylactic nimodipine for delayed ischemic deficit after subarachnoid hemorrhage: A metaanalysis. J Neurosurg 1996; 84: 405–414. [DOI] [PubMed] [Google Scholar]
- 11.Koenig MA. Management of delayed cerebral ischemia after subarachnoid hemorrhage. Continuum (Minneap Minn) 2012; 18: 579–597. [DOI] [PubMed] [Google Scholar]
- 12.Biondi A, Ricciardi GK, Puybasset L, et al. Intraarterial nimodipine for the treatment of symptomatic cerebral vasospasm after aneurysmal subarachnoid hemorrhage: Preliminary results. AJNR Am J Neuroradiol 2004; 25: 1067–1076. [PMC free article] [PubMed] [Google Scholar]
- 13.Cho W-S, Kang H-S, Kim JE, et al. Intraarterial nimodipine infusion for cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage. Interv Neuroradiol 2011; 17: 169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dehdashti AR, Binaghi S, Uske A, et al. Intraarterial nimodipine for the treatment of symptomatic vasospasm after aneurysmal subarachnoid hemorrhage: A preliminary study. Neurol India 2011; 59: 810–816. [DOI] [PubMed] [Google Scholar]
- 15.Hänggi D, Turowski B, Beseoglu K, et al. Intraarterial nimodipine for severe cerebral vasospasm after aneurysmal subarachnoid hemorrhage: Influence on clinical course and cerebral perfusion. AJNR Am J Neuroradiol 2008; 29: 1053–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hui C, Lau KP. Efficacy of intraarterial nimodipine in the treatment of cerebral vasospasm complicating subarachnoid haemorrhage. Clin Radiol 2005; 60: 1030–1036. [DOI] [PubMed] [Google Scholar]
- 17.Kim JH, Park IS, Park KB, et al. Intraarterial nimodipine infusion to treat symptomatic cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Korean Neurosurg Soc 2009; 46: 239–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim S-S, Park D-H, Lim D-J, et al. Angiographic features and clinical outcomes of intraarterial nimodipine injection in patients with subarachnoid hemorrhage-induced vasospasm. J Korean Neurosurg Soc 2012; 52: 172–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muizelaar JP, Zwienenberg M, Rudisill NA, et al. The prophylactic use of transluminal balloon angioplasty in patients with Fisher grade 3 subarachnoid hemorrhage: A pilot study. J Neurosurg 1999; 91: 51–58. [DOI] [PubMed] [Google Scholar]
- 20.Drake CG, Hunt WE, Sano K, et al. Report of World Federation of Neurological Surgeons Committee on a Universal Subarachnoid Hemorrhage Grading Scale. J Neurosurg 1988; 68: 985–986. [DOI] [PubMed] [Google Scholar]
- 21.Claassen J, Bernardini GL, Kreiter K, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: The Fisher scale revisited. Stroke 2001; 32: 2012–2020. [DOI] [PubMed] [Google Scholar]
- 22.Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: A literature review and synthesis. Stroke 2007; 38: 1091–1096. [DOI] [PubMed] [Google Scholar]
- 23.Grotenhuis JA, Bettag W, Fiebach BJO, et al. Intracarotoid slow bolus injection of nimodipine during angiography for treatment of cerebral vasospasm after SAH. A preliminary report. J Neurosurg 1984; 61: 231–2340. [DOI] [PubMed] [Google Scholar]
- 24.Vibulsresth S, Dietrich D, Busto R, et al. Failure of nimodipine to prevent ischemic neuronal damage in rats. Stroke 1987; 18: 210–216. [DOI] [PubMed] [Google Scholar]
- 25.Gotoh O, Mohamed AA, McCulloch J, et al. Nimodipine and the haemodynamic and histopathological consequences of middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab 1986; 6: 321–331. [DOI] [PubMed] [Google Scholar]
- 26.Snape MF, Baldwin HA, Cross AJ, et al. The effects of chlormethiazole and nimodipine on cortical infarct area after focal cerebral ischemia in the rat. Neuroscience 1993; 53: 837–844. [DOI] [PubMed] [Google Scholar]
- 27.Wolf S, Martin H, Landscheidt JF, et al. Continuous selective intraarterial infusion of nimodipine for therapy of refractory cerebral vasospasm. Neurocrit Care 2010; 12: 346–351. [DOI] [PubMed] [Google Scholar]
- 28.Lysakowski C, Walder B, Costanza MC, et al. Transcranial Doppler versus angiography in patients with vasospasm due to a ruptured aneurysm. A systematic review. Stroke 2001; 32: 2292–2298. [DOI] [PubMed] [Google Scholar]
- 29.Mills JN, Mehta V, Russin J, et al. Advanced imaging modalities in the detection of cerebral vasospasm. Neurol Res Int 2013; 2013: 415960 doi: 10.1155/2013/415960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Staalsø JM, Edsen T, Romner B, et al. Transcranial Doppler velocimetry in aneurysmal subarachnoid haemorrhage: intra- and interobserver agreement and relation to angiographic vasospasm and mortality. Br J Anaesth 2013; 110: 577–585. [DOI] [PubMed] [Google Scholar]
- 31.Vora YY, Suarez-Almazor M, Steinke DE, et al. Role of transcranial Doppler monitoring in the diagnosis of cerebral vasospasm after subarachnoid hemorrhage. Neurosurgery 1999; 44: 1237–1247. discussion 47–58. [PubMed] [Google Scholar]
- 32.McAuliffe W, Townsend M, Eskridge JM, et al. Intracranial pressure changes induced during papaverine infusion for treatment of vasospasm. J Neurosurg 1995; 83: 430–434. [DOI] [PubMed] [Google Scholar]
- 33.Clyde BL, Firlik AD, Kaufmann AM, et al. Paradoxical aggravation of vasospasm with papaverine infusion following aneurysmal subarachnoid hemorrhage. Case report. J Neurosurg 1996; 84: 690–695. [DOI] [PubMed] [Google Scholar]
- 34.Miller JA, Cross DT, Moran CJ, et al. Severe thrombocytopenia following intraarterial papaverine administration for treatment of vasospasm. J Neurosurg 1995; 83: 435–437. [DOI] [PubMed] [Google Scholar]
- 35.Kerz T, Boor S, Beyer C, et al. Effect of intraarterial papaverine or nimodipine on vessel diameter in patients with cerebral vasospasm after subarachnoid hemorrhage. Br J Neurosurg 2012; 26: 517–524. [DOI] [PubMed] [Google Scholar]
- 36.Tejada JG, Taylor RA, Ugurel MS, et al. Safety and feasibility of intra-arterial nicardipine for the treatment of subarachnoid hemorrhage-associated vasospasm: Initial clinical experience with high-dose infusions. AJNR Am J Neuroradiol 2007; 28: 844–848. [PMC free article] [PubMed] [Google Scholar]
- 37.Linskey ME, Horton JA, Rao GR, et al. Fatal rupture of the intracranial carotid artery during transluminal angioplasty for vasospasm induced by subarachnoid hemorrhage. Case report. J Neurosurg 1991; 74: 985–990. [DOI] [PubMed] [Google Scholar]
- 38.Aburto-Murrieta Y, Marquez-Romero JM, Bonifacio-Delgadillo D, et al. Endovascular treatment: Balloon angioplasty versus nimodipine intra-arterial for medically refractory cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Vasc Endovascular Surg 2012; 46: 460–465. [DOI] [PubMed] [Google Scholar]