Abstract
Background.
Back pain and falls are common health conditions among older U.S. women. The extent to which back pain is an independent risk factor for falls has not been established.
Methods.
We conducted a prospective study among 6,841 community-dwelling U.S. women at least 65 years of age from the Study of Osteoporotic Fractures (SOF). Baseline questionnaires inquired about any back pain, pain severity, and frequency in the past year. During 1 year of follow-up, falls were summed from self-reports obtained every 4 months. Two outcomes were studied: recurrent falls (≥2 falls) and any fall (≥1 fall). Associations of back pain and each fall outcome were estimated with risk ratios (RRs) and 95% confidence intervals (CIs) from multivariable log-binomial regression. Adjustments were made for age, education, smoking status, fainting history, hip pain, stroke history, vertebral fracture, and Geriatric Depression Scale.
Results.
Most (61%) women reported any back pain. During follow-up, 10% had recurrent falls and 26% fell at least once. Any back pain relative to no back pain was associated with a 50% increased risk of recurrent falls (multivariable RR = 1.5, 95% CI: 1.3, 1.8). Multivariable RRs for recurrent falls were significantly elevated for all back pain symptoms, ranging from 1.4 (95% CI: 1.1, 1.8) for mild back pain to 1.8 (95% CI: 1.4, 2.3) for activity-limiting back pain. RRs of any fall were also significantly increased albeit smaller than those for recurrent falls.
Conclusions.
Older community-dwelling women with a recent history of back pain are at increased risk for falls.
Keywords: Pain, Falls, Epidemiology
Back pain lasting at least 1 day in the past 3 months is reported by nearly 30% of U.S. adults aged 65 years and older (1) and leads to 30 million office visits annually in adults of any age (2). Back pain is the most prevalent type of musculoskeletal pain reported by older adults, with higher prevalence than pain in the knees, hips, or any other joint (3), and is often severe enough to restrict usual activities (4). Among older adults, back pain often co-occurs with limitations in physical functioning, such as difficulty standing or walking short distances, and with depressive symptoms (5–9). In turn, poor physical and mental functioning are well-documented risk factors for falls (10–12), suggesting that older adults with back pain may be at high risk for falls.
Given the high prevalence and medical burden of back pain, knowledge about its relation to fall risk could be beneficial for planning public health and therapeutic interventions. However, the association of back pain and fall risk has not been adequately evaluated in prospective studies. Previous investigations used different definitions of back pain, with some assessing only chronic back pain (13,14) and others assessing any back pain (15,16). Consequently, effects of back pain location, severity, and frequency on fall risk remain unknown. Moreover, associations of back pain and fall risk may be sex specific. Among older adults, women more often report back pain and injuries from falls than men (3,4,17).
To determine the associations of back pain with the risk of falls among community-dwelling older women, we used existing prospectively collected data from the Study of Osteoporotic Fractures (SOF) cohort. We hypothesized that any observed associations of back pain and fall risk would be explained, at least in part, by poor physical function, depressive symptoms, or other possible intermediate factors such as use of pain or other central nervous system active medications (18).
Methods
Participants
Between September 1986 and October 1988, 9,704 White women aged 65 years and older completed an enrollment visit in SOF, a nationwide prospective cohort study of risk factors for fractures and falls (19). Briefly, women were recruited from community-based listings in Baltimore, MD; Minneapolis, MN; Portland, OR; and Pittsburgh PA. Women needing assistance to walk or with bilateral hip replacements were ineligible. In addition, Black women initially were not recruited because of their low hip fracture rates. Institutional Review Boards at each site approved the study. All participants gave written informed consent.
From January 1989 through December 1990, the 9,339 participants alive and active in SOF were invited to complete a second visit (Visit 2) and comprehensive questionnaire. Visit 2 served as the “baseline” for this analysis.
Back Pain Assessment
On the baseline questionnaire, women reported whether they had any back pain in the past 12 months. Those with back pain marked on a drawing of the posterior torso where their back pain usually occurred (upper, middle, or lower back). We categorized pain locations as low back only, upper or mid back only, and low back plus mid or upper back, and number of pain sites as 1, 2, or 3. Those reporting back pain were asked about severity (mild, moderate, or severe), frequency (rarely/some of the time, most of the time/always), and whether they limited their usual activities because of back pain (yes, no).
Other Baseline Measures
Questionnaires also elicited information on age, education, cigarette smoking, drinks of alcohol per week, and self-rated health. History of physician-diagnosed conditions included Parkinson’s disease, stroke, and osteoarthritis. Women also reported whether in the past 12 months they had any falls, fainting episodes, or hip pain. Instrumental activities of daily living (IADL) was coded as self-reported difficulty with at least one of the following five activities: walking 2–3 blocks, climbing 10 steps, preparing meals, doing heavy housework, and shopping for groceries or clothes. Depressive symptoms were assessed with the validated 15-item Geriatric Depression Scale (GDS) (20).
Participants were interviewed about medication use in the past 12 months with separate questions to ascertain medications used for sleep, for anxiety, and for pain (including for “arthritis, headaches, and other discomfort”). Participants underwent four physical performance measures: usual walking pace (m/s), chair stand time (s), ability to hold tandem stands with eyes open and with eyes closed for 10 seconds, and grip strength (kg) with a handheld dynamometer (Preston Grip Dynamometer,Tokyo, Japan). Body mass index (kg/m2) was calculated from height and weight measured by study staff. Presence of vertebral fracture was determined from spine radiographs obtained at enrollment (21).
Fall Outcomes
Every 4 months (tri-annually) after baseline, participants reported the number of times they fell in the past 4 months on brief questionnaires. Nonresponders were telephoned to obtain their fall information. In each tri-annual interval, more than 99% provided complete fall information. Each participant was followed for falls through her first three tri-annual questionnaires (about 12 months). Each woman’s number of falls was summed across the three questionnaires. The primary outcome measure was 1-year risk (cumulative incidence) of recurrent falls, defined as ≥2 falls during follow-up. The secondary outcome measure was 1-year risk of any fall.
Analytic Cohort
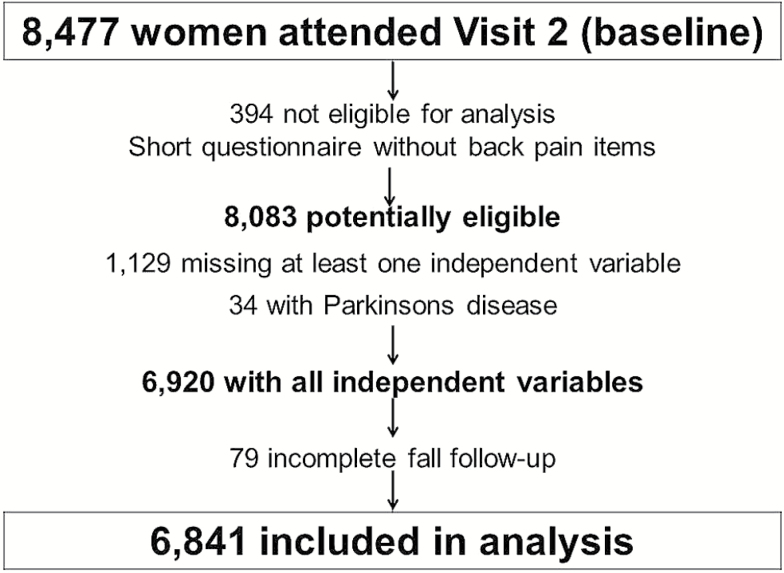
Of the 8,477 baseline participants, 8,083 (95%) completed the questionnaire containing back pain items. We excluded 1,129 missing at least one other independent variable deemed necessary for this analysis, 34 reporting Parkinson’s disease, and 79 with incomplete falls data, leaving an analytic cohort of 6,841 women (Figure 1).
Figure 1.
Analytic cohort selection from the Study of Osteoporotic Fractures, a prospective study of U.S. women aged 65 years and older.
Statistical Analysis
Analyses were conducted using SAS software version 9.4 (SAS Institute Inc, Cary, NC). Baseline characteristics in the analytic cohort were compared according to back pain severity using one-way analysis of variance for continuous variables or chi-square tests for categorical variables. Risk ratios (RRs) and 95% confidence intervals (CIs) were estimated as the measure of association between back pain and fall risk from multivariable log-binomial regression models with a robust variance estimator (22), using no back pain as the referent.
We built separate models for each fall outcome using well-established variable selection procedures and change-in-estimate methods appropriate for epidemiologic analyses (23,24). First, we constructed a base model adjusted for age and confounders. Variables in descriptive analyses that were associated with at least one back pain variable, a fall outcome, or both were assessed as possible confounders. Variables retained in the base model as confounders are shown in Table 2 footnotes. Second, we evaluated the extent to which associations of back pain and fall risk from the base models were further explained by possible intermediate factors (24). Possible intermediate factors examined were as follows: each physical performance measure, IADL difficulty, GDS score, pain medications, anxiety medications, and sleep medications. We added each variable one at a time to the base models and computed the percent attenuation in the RRs. We planned to retain in the final model the potential intermediate variables whose inclusion in the base model attenuated the RR by at least 10%. However, no variables met this criterion. The largest attenuation (8%) in RRs occurred with control for GDS, which was retained in the final model. Presenting RRs before and after adjustment for possible intermediate variables facilitates inference about their effects on the association of interest (24). Therefore, we report RRs before (Table 2) and after GDS adjustment (Figure 2).
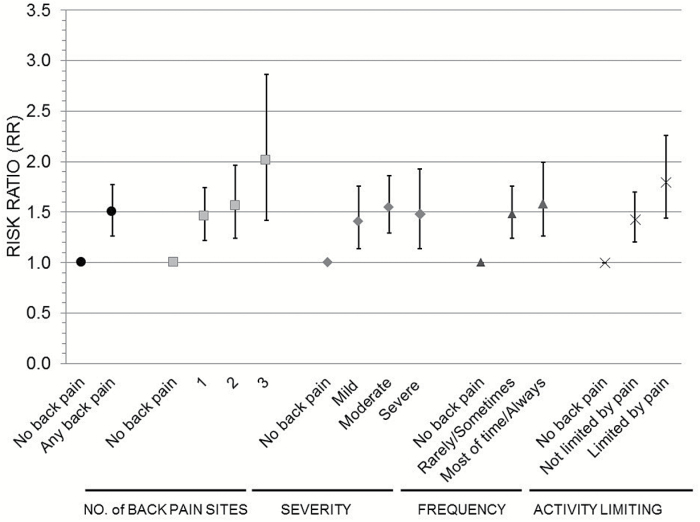
Figure 2.
Risk ratios (RRs) for recurrent falls in relation to back pain among older women: final model estimates. RR point estimates are represented as (●) any back pain in the past 12 months, (■) number of pain sites, (♦) pain severity, (▲) pain frequency, and (×) activity liming back pain. Error bars are 95% confidence intervals. RRs are adjusted for baseline age, education, cigarette smoking, fainting episodes, hip pain, history of stroke, and geriatric depression scale.
Finally, we conducted stratified analyses to determine whether baseline age (<75 years, ≥ 75 years), hip pain (yes, no), or fall history (yes, no) modified the associations of back pain and fall risk. Tests of multiplicative interaction were performed.
In sensitivity analyses, we observed that use of an analytic cohort with complete data did not bias the results. Supplementary Tables 1–3 confirm that mean age, prevalence of back pain, risk of each fall outcome, and RRs (95% CI) from the confounding adjusted models in the analytic cohort were comparable with those from cohorts successively restricted to important study variables. Therefore, we present results only for the analytic cohort.
Results
Back pain in the past 12 months was reported by 61% of the participants. Among those with back pain, 50% had low back pain only, 5% had pain in all three locations, 14% reported severe pain, 24% reported pain most of the time/always, and 22% reported that they limited usual activities because of pain. Participants reporting back pain differed from those who reported no back pain on most characteristics examined, except for current alcohol consumption (Table 1).
Table 1.
Distributions of Baseline Characteristics According to Back Pain Severity Among 6,841 Women Aged 65 Years or Older
| Characteristic | No back pain | Back Pain Severity | ||
|---|---|---|---|---|
| Mild | Moderate | Severe | ||
| 2,670 (39%) | 1,174 (17%) | 2,406 (35%) | 591 (9%) | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Age (years) | 73.1 (5.0) | 73.1 (4.8) | 73.3 (4.9) | 73.7 (5.1) |
| Body mass index (kg/m2) | 25.9 (4.3) | 26.1 (4.4) | 26.5 (4.7) | 27.1 (5.4) |
| Usual walking pace (m/s) | 0.9 (0.2) | 0.9 (0.2) | 0.9 (0.2) | 0.8 (0.2) |
| Chair stand time (s) | 11.5 (3.9) | 11.7 (3.7) | 12.6 (4.7) | 14.3 (7.1) |
| Grip strength (kg) | 19 (5) | 19 (5) | 19 (5) | 18 (5) |
| Geriatric depression scale (15 point maximum) | 1.2 (1.8) | 1.4 (1.8) | 1.9 (2.2) | 2.4 (2.7) |
| % | % | % | % | |
| College education | 39 | 48 | 36 | 34 |
| Cigarette smoking | ||||
| Current | 8 | 6 | 8 | 11 |
| Past | 30 | 31 | 33 | 33 |
| Alcohol consumption | ||||
| 1–7 drinks/week | 52 | 50 | 52 | 46 |
| >7 drinks/week | 5 | 5 | 5 | 4 |
| Fair–very poor self-rated health | 9 | 12 | 19 | 26 |
| Stroke history | 2 | 2 | 3 | 6 |
| Arthritis history | 50 | 62 | 74 | 76 |
| Fainting in past year | 3 | 3 | 4 | 9 |
| Fell in the past year | 25 | 30 | 33 | 35 |
| Vertebral fracture | 17 | 17 | 22 | 24 |
| Hip pain | 15 | 27 | 55 | 54 |
| ≥1 IADL difficulty | 9 | 10 | 16 | 33 |
| Tandem stands | ||||
| Eyes open <10 s | 7 | 7 | 8 | 10 |
| Eyes closed <10 s | 34 | 32 | 36 | 40 |
| Anxiety medication use | 8 | 11 | 16 | 25 |
| Sleep medication use | 11 | 15 | 20 | 26 |
| Pain medication use | 52 | 57 | 71 | 75 |
Notes: IADL = instrumental activities of daily living.
During the 1-year follow-up, 664 (10%) had recurrent falls and 1,805 (26%) had any fall. After adjustment for age and confounders, RRs were significantly elevated for any back pain in relation to recurrent falls (Table 2). Compared with peers without back pain, women with any back pain were at 1.6-fold increased risk of recurrent falls. Recurrent fall risk remained significantly elevated for all locations of back pain, number of pain sites, and each category of severity, frequency, and activity-limiting back pain. Similarly, RRs for any fall were significantly elevated for all categories of back pain, although these estimates were smaller than RRs for recurrent falls.
Table 2.
Risk Ratios (RRs) for Falls in Relation to Back Pain Among Older Women: Base Model (confounding adjusted) Estimates
| Back Pain Characteristic | N | Recurrent (≥2) Falls | Any Fall | ||||
|---|---|---|---|---|---|---|---|
| % with ≥2 falls | Age-adjusted RR | Multivariable RR (95% CI)* | % with any fall | Age-adjusted RR | Multivariable RR (95% CI)† | ||
| No back pain | 2,670 | 7 | 1.0 (ref.) | 1.0 (ref.) | 22 | 1.0 (ref.) | 1.0 (ref.) |
| Any back pain | 4,169 | 12 | 1.66 | 1.55 (1.31, 1.83) | 29 | 1.29 | 1.23 (1.13, 1.35) |
| Location | |||||||
| No back pain | 2,670 | 7 | 1.0 (ref.) | 1.0 (ref.) | 22 | 1.0 (ref.) | 1.0 (ref.) |
| Low back only | 2,070 | 11 | 1.54 | 1.43 (1.18, 1.74) | 28 | 1.23 | 1.18 (1.07, 1.31) |
| Mid or upper back only | 1,168 | 12 | 1.66 | 1.59 (1.29, 1.97) | 29 | 1.29 | 1.24 (1.11, 1.39) |
| Low back plus mid or upper back | 931 | 13 | 1.91 | 1.75 (1.40, 2.19) | 32 | 1.43 | 1.34 (1.19, 1.51) |
| No. of back pain sites | |||||||
| No back pain | 2,670 | 7 | 1.0 (ref.) | 1.0 (ref.) | 22 | 1.0 (ref.) | 1.0 (ref.) |
| 1 | 3,050 | 11 | 1.58 | 1.49 (1.25, 1.78) | 28 | 1.26 | 1.21 (1.10, 1.33) |
| 2 | 917 | 12 | 1.73 | 1.63 (1.30, 2.05) | 30 | 1.34 | 1.27 (1.12, 1.44) |
| 3 | 202 | 17 | 2.47 | 2.19 (1.55, 3.08) | 36 | 1.60 | 1.50 (1.23, 1.83) |
| Severity | |||||||
| No back pain | 2,670 | 7 | 1.0 (ref.) | 1.0 (ref.) | 22 | 1.0 (ref.) | 1.0 (ref.) |
| Mild | 1,174 | 10 | 1.50 | 1.43 (1.15, 1.78) | 29 | 1.31 | 1.25 (1.11, 1.40) |
| Moderate | 2,406 | 12 | 1.71 | 1.60 (1.33, 1.92) | 29 | 1.30 | 1.24 (1.12, 1.36) |
| Severe | 589 | 12 | 1.76 | 1.61 (1.24, 2.10) | 28 | 1.24 | 1.18 (1.02, 1.37) |
| Frequency | |||||||
| No back pain | 2,670 | 7 | 1.0 (ref.) | 1.0 (ref.) | 22 | 1.0 (ref.) | 1.0 (ref.) |
| Rarely / some of time | 3,160 | 11 | 1.59 | 1.51 (1.27, 1.79) | 29 | 1.29 | 1.24 (1.13, 1.36) |
| Most of time / always | 1,009 | 13 | 1.88 | 1.72 (1.37, 2.15) | 29 | 1.29 | 1.21 (1.06, 1.37) |
| Limited by back pain | |||||||
| No back pain | 2,670 | 7 | 1.0 (ref.) | 1.0 (ref.) | 22 | 1.0 (ref.) | 1.0 (ref.) |
| No‡ | 3,239 | 10 | 1.51 | 1.45 (1.22, 1.73) | 28 | 1.23 | 1.19 (1.09, 1.31) |
| Yes | 930 | 15 | 2.16 | 1.96 (1.57, 2.43) | 34 | 1.50 | 1.39 (1.23, 1.57) |
Notes: CI = confidence interval; ref = referent level.
*Adjusted for age, education, cigarette smoking, fainting episodes, hip pain, and history of stroke.
†Adjusted for age, education, cigarette smoking, fainting episodes, hip pain, and prevalent vertebral fracture.
‡Back pain that did not limit usual activities.
The addition of potential intermediate variables one at a time to the confounding adjusted (base) models did not strongly attenuate the RRs. For recurrent falls, change in the confounding adjusted RRs ranged from 0.6% to −8.2%. GDS adjustment produced the largest attenuation, with reductions of about 8% in RRs for back pain at three sites (−8.2%), severe back pain (−8.1%), back pain most of the time/always (−8.1%), and limiting usual activities (−8.2%). Adjustment for variables other than GDS attenuated the RRs by −5.5% or less. For the any fall endpoint, RRs changed by 0.8% to −4.4% when adjusted for each individual potential intermediate variable. Although adjustment for GDS produced the greatest attenuation in the RRs, reductions were modest (−1.6% to −4.4%).
In the final models with GDS included, all back pain categories remained independently associated with recurrent fall risk (Figure 2). For any falls, the RRs from final models adjusted for GDS were not materially changed from those reported in Table 2 (data not shown).
In stratified analyses (Table 3), any back pain was strongly associated with risk of recurrent falls among women 65–74 years but not among women 75 years or older. However, age did not affect the association of any back pain and risk of any fall. Neither history of falls nor history of hip pain modified associations of back pain with either fall endpoint.
Table 3.
Risk Ratios (RRs) for Falls in Relation to Back Pain According to Baseline Age, Fall History, and Hip Pain
| Strata | ≥2 Falls | p Interaction | Any Fall | p Interaction | ||
|---|---|---|---|---|---|---|
| No Back Pain | Any Back Pain | No Back Pain | Any Back Pain | |||
| Multivariable RR (95% CI)* | Multivariable RR (95% CI)† | |||||
| Age <75 years | 1.0 (ref.) | 1.7 (1.4, 2.2) | 1.0 (ref.) | 1.3 (1.1, 2.4) | ||
| Age ≥75 years | 1.0 (ref.) | 1.2 (0.9, 1.6) | .02 | 1.0 (ref.) | 1.2 (1.0, 1.3) | .36 |
| No falls in prior year | 1.0 (ref.) | 1.5 (1.2, 1.9) | 1.0 (ref.) | 1.2 (1.1, 1.4) | ||
| Fell in prior year | 1.0 (ref.) | 1.3 (1.1, 1.7) | .47 | 1.0 (ref.) | 1.2 (1.0, 1.3) | .89 |
| No hip pain in prior year | 1.0 (ref.) | 1.5 (1.3, 1.9) | 1.0 (ref.) | 1.2 (1.1, 1.4) | ||
| Hip pain in prior year | 1.0 (ref.) | 1.3 (1.0, 1.9) | .54 | 1.0 (ref.) | 1.1 (1.0, 1.4) | .54 |
*Adjusted for age, education, cigarette smoking, fainting episodes, hip pain, history of stroke, and geriatric depression scale (GDS). Age was not included in models within age strata; hip pain was not included in models within hip pain strata.
†Adjusted for age, education, cigarette smoking, fainting episodes, hip pain, prevalent vertebral fracture, and GDS. Age was not included in models within age strata; hip pain was not included in models within hip pain strata.
Discussion
Back pain emerged as an independent risk factor for falls, especially recurrent falls, in this large cohort of older U.S. women. Fall risk was significantly increased for pain in three sites throughout the back and for all categories of back pain, especially, frequent pain and pain that limited usual activities. However, even back pain in just one location, or pain that was mild, occurred rarely or sometimes, or did not limit usual activities was associated with significantly increased fall risk. Contrary to our hypothesis, these associations remained independent of physical performance, IADL difficulty, depressive symptoms, and medication use for anxiety, sleep, or pain. The association of back pain with risk of recurrent falls may depend on age.
Recent meta-analyses of prospective studies show that any bodily pain or joint pain in any location are associated with 40%–71% greater odds of any fall (25,26) and 60%–80% greater odds of recurrent falls (25,27). In addition, chronic musculoskeletal pain is an independent fall risk factor in prospective studies among community-dwelling older U.S. adults (13,14). Compared with no chronic pain, chronic multisite musculoskeletal pain was associated with 1.5-fold increased risk of any falls in adults aged 70 years or older (13) and by 1.7-fold among older disabled women (14). These associations were independent of adjustment for physical performance and use of psychoactive or pain medications and other fall risk factors (13,14). The associations that we observed between back pain and falls are compatible with previous work, both in magnitude and independence from other factors.
In contrast to results for overall musculoskeletal pain and fall risk, prior reports on the association of back pain itself and fall risk have been null (13–16). Our results may diverge from these observations for a number of reasons including differences in ascertainment of back pain, fall follow-up methods, and the cohorts studied. For example, back pain obtained with a numeric rating scale as part of an overall chronic pain assessment was unrelated to fall risk (13). In contrast, our study showed that frequent back pain (occurring most of the time/always) was positively associated with both fall outcomes. In another study among older disabled women, chronic back and chest pain were combined together, precluding assessment of the relation between back pain only and fall risk (14). In the other reports examining any back pain, falls were assessed only once at the end of a 3- to 4-year follow-up period (15,16). In these studies, incomplete ascertainment of falls during the entire follow-up period could explain the null results. Finally, some reports combined results for women and men or included only older disabled women (13,14). Thus, our study is perhaps the largest and most complete to date regarding back pain and fall risk among community-dwelling older U.S. women.
Neither baseline fall history nor report of hip pain modified associations of back and fall risk in this cohort. Likewise, RRs for any fall were similar within age strata. However, age appeared to modify the relation between back pain and recurrent fall risk such that the association was strongest among the younger women. It is possible that this finding is due to chance, because the p value for the test of interaction was modest. Alternatively, it is well known that age is a strong fall risk factor (10,11). Thus, among very old women, back pain appears to be less important than other fall risk factors in the etiology of recurrent fall risk.
Altered postural responses to back pain represent a possible pathway underlying the association of back pain and fall risk. Studies using force plate measurements indicate that subjects with back pain have aberrant postural response to loss of balance, including trunk muscle stiffening and inadequate use of hip joints (28–30). Trunk muscle stiffening heightens the likelihood of falling by simultaneously inhibiting compensatory use of the hip joints to regain balance and increasing reliance on ankle joints (31). Force plate measurements indicative of poor standing balance are associated with higher risk of falls (32), but associations between back pain, postural control, and falls specifically among older women remain to be determined.
Psychological responses to back pain provide another possible pathway. In a small sample of older women, those with low back pain scored on average significantly higher on a fear of movement scale and significantly lower on a balance self-efficacy scale than those without low back pain (33). In turn, fear of falling and activity avoidance both were associated with increased fall risk among community-dwelling elderly adults (34–36). However, the extent to which fear of falling or fear avoidance behavior could explain any relation between back pain and fall risk in older women is currently unknown.
This study has several limitations. First, recall of falls over 3–6 months is reasonably accurate (37,38) but may underestimate fall frequency compared with diaries (39). If any inaccuracies in fall reports in SOF were random with respect to back pain, then the RRs we observed could be underestimated. Alternatively, if participants with back pain subsequently experienced falls that caused back pain to recur or worsen, then their fall reports may be more accurate than those without prior back pain. Such systematic differences in fall reports, if they existed, would have overestimated the RRs. Second, although we had data on vertebral fractures, an important cause of back pain (21), we had no data on other spinal degenerative conditions. However, in older women or in cohorts that included women, back pain prevalence was similar in those with and without spinal degenerative conditions (40–43). Thus, these conditions are unlikely to strongly confound the association between back pain and fall risk. Third, medications were assessed by self-report and could be misclassified. Finally, SOF is composed of generally healthy, community-dwelling White women, so these results may not be applicable to other populations.
Although back pain may not exist as the only site of bodily pain, it is a common complaint in older adults with real societal and medical burden (1–4). Elucidating the negative health consequences of back pain is critical to designing effective clinical treatment and intervention strategies. In this context, our results extend previous work by showing that back pain is an independent risk factor for falls, especially recurrent falls, in the ensuing year among community-dwelling older White women. Clinicians may consider assessing fall risk in older women who present with any back pain, even pain that is mild or does not limit usual activities. Whether back pain treatment reduces fall risk in this population should be examined.
Supplementary Material
Please visit the article online at http://gerontologist.oxfordjournals.org/ to view supplementary material.
Funding
The Study of Osteoporotic Fractures is supported by the National Institute on Aging through grant numbers R01 AG005407, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, and R01 AG027576.
Conflict of Interest
Peggy M. Cawthon serves as a consultant to Eli Lilly and KineMed and has received grants from GSK, IMS Health, Merck, and KineMed. Richard A. Deyo has received royalties from UpToDate for authoring topics on low back pain, serves on the Board of Directors for the non-profit organization Informed Medical Decisions Foundation, and has received grant funding for back pain research from the NIH, AHRQ, and PCORI. Una E. Makris has received funding for pain research from the NIH.
All other authors: none declared.
Supplementary Material
References
- 1. Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976). 2006;31:2724–2727. [DOI] [PubMed] [Google Scholar]
- 2. Licciardone JC. The epidemiology and medical management of low back pain during ambulatory medical care visits in the United States. Osteopath Med Prim Care. 2008;2:11. doi:10.1186/1750-4732-2-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patel KV, Guralnik JM, Dansie EJ, Turk DC. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154:2649–2657. doi:10.1016/j.pain.2013.07.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Makris UE, Fraenkel L, Han L, Leo-Summers L, Gill TM. Epidemiology of restricting back pain in community-living older persons. J Am Geriatr Soc. 2011;59:610–614. doi:10.1111/j.1532-5415.2011.03329.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Edmond SL, Felson DT. Function and back symptoms in older adults. J Am Geriatr Soc. 2003;51:1702–1709. [DOI] [PubMed] [Google Scholar]
- 6. Weiner DK, Haggerty CL, Kritchevsky SB, et al. How does low back pain impact physical function in independent, well-functioning older adults? Evidence from the Health ABC Cohort and implication for the future. Pain Med. 2003;4:311–320. [DOI] [PubMed] [Google Scholar]
- 7. Di Iorio A, Abate M, Guralnik JM, et al. From chronic low back pain to disability, a multifactorial mediated pathway: the InCHIANTI study. Spine (Phila Pa 1976). 2007;32:E809–E815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rudy TE, Weiner DK, Lieber SJ, Slaboda J, Boston JR. The impact of chronic low back pain on older adults: a comparative study of patients and controls. Pain. 2007;131:293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhu K, Devine A, Dick IM, Prince RL. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine (Phila Pa 1976). 2007;32:2012–2018. [DOI] [PubMed] [Google Scholar]
- 10. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. [DOI] [PubMed] [Google Scholar]
- 11. Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261:2663–2668. [PubMed] [Google Scholar]
- 12. Whooley MA, Kip KE, Cauley JA, Ensrud KE, Nevitt MC, Browner WS. Depression, falls, and risk of fracture in older women. Arch Intern Med. 1999;159:484–90. [DOI] [PubMed] [Google Scholar]
- 13. Leveille SG, Jones RN, Kiely DK, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302:2214–2221. doi:10.1001/jama.2009.1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Leveille SG, Bean J, Bandeen-Roche K, Jones R, Hochberg M, Guralnik JM. Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc. 2002;50:671–678. [DOI] [PubMed] [Google Scholar]
- 15. Woo J, Leung J, Lau E. Prevalence and correlates of musculoskeletal pain in Chinese elderly and the impact on 4-year physical function and quality of life. Public Health. 2009;123:549–556. doi:10.1016/j.puhe.2009.07.006 [DOI] [PubMed] [Google Scholar]
- 16. Muraki S, Akune T, Oka H, et al. Physical performance, bone and joint diseases, and incidence of falls in Japanese men and women: a longitudinal cohort study. Osteoporos Int. 2013;24:459–466. doi:10.1007/s00198-012-1967-0 [DOI] [PubMed] [Google Scholar]
- 17. CDC. Self-reported falls and fall-related injuries among persons aged greater than or equal to 65 years—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:225–229. doi:10.1016/j.jsr.2008.05.002 [PubMed] [Google Scholar]
- 18. Ensrud KE, Blackwell TL, Mangione CM, et al. Central nervous system active medications and risk for falls in older women. J Am Geriatr Soc. 2002;50:1629–1637. [DOI] [PubMed] [Google Scholar]
- 19. Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. N Engl J Med. 1995;332:767–773. [DOI] [PubMed] [Google Scholar]
- 20. Yesavage JA. Geriatric Depression Scale. Psychopharmacol Bull. 1988;24:709–711. [PubMed] [Google Scholar]
- 21. Ettinger B, Black DM, Nevitt MC, et al. Contribution of vertebral deformities to chronic back pain and disability. J Bone Miner Res. 1992;7:449–456. [DOI] [PubMed] [Google Scholar]
- 22. Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. [DOI] [PubMed] [Google Scholar]
- 23. Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79:340–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rothman K, Greenland S. Modern Epidemiology. 2nd ed Philadelphia, PA: Lippincott-Raven Publishers; 1998. (pp. 122–123). [Google Scholar]
- 25. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–668. doi:10.1097/EDE.0b013e3181e89905 [DOI] [PubMed] [Google Scholar]
- 26. Stubbs B, Binnekade T, Eggermont L, Sepehry AA, Patchay S, Schofield P. Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95:175–187.e9. doi:10.1016/j.apmr.2013.08.241 [DOI] [PubMed] [Google Scholar]
- 27. Stubbs B, Schofield P, Binnekade T, Patchay S, Sepehry A, Eggermont L. Pain is associated with recurrent falls in community-dwelling older adults: evidence from a systematic review and meta-analysis. Pain Med. 2014;15:1115–1128. doi:10.1111/pme.12462 [DOI] [PubMed] [Google Scholar]
- 28. Henry SM, Hitt JR, Jones SL, Bunn JY. Decreased limits of stability in response to postural perturbations in subjects with low back pain. Clin Biomech. 2006;21:881–892. [DOI] [PubMed] [Google Scholar]
- 29. Jones SL, Henry SM, Raasch CC, Hitt JR, Bunn JY. Individuals with non-specific low back pain use a trunk stiffening strategy to maintain upright posture. J Electromyogr Kinesiol. 2012;22:13–20. doi:10.1016/j.jelekin.2011.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mok NW, Brauer SG, Hodges PW. Hip strategy for balance control in quiet standing is reduced in people with low back pain. Spine (Phila Pa 1976). 2004;29:E107–E112. [DOI] [PubMed] [Google Scholar]
- 31. Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Aging. 2006;35(Suppl. 2):ii7–ii11. [DOI] [PubMed] [Google Scholar]
- 32. Pajala S, Era P, Koskenvuo M, Kaprio J, Törmäkangas T, Rantanen T. Force platform balance measures as predictors of indoor and outdoor falls in community-dwelling women aged 63-76 years. J Gerontol A Biol Sci Med Sci. 2008;63:171–178. [DOI] [PubMed] [Google Scholar]
- 33. Champagne A, Prince F, Bouffard V, Lafond D. Balance, falls-related self-efficacy, and psychological factors among older women with chronic low back pain: a preliminary case-control study. Rehabil Res Pract [Internet]. 2012;2012:430374 doi:10.1155/2012/430374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–1335. [DOI] [PubMed] [Google Scholar]
- 35. Delbaere K, Crombez G, Vanderstraeten G, Willems T, Cambier D. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33:368–373. [DOI] [PubMed] [Google Scholar]
- 36. Pluijm SM, Smit JH, Tromp EA, et al. A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: results of a 3-year prospective study. Osteoporos Int. 2006;17:417–425. [DOI] [PubMed] [Google Scholar]
- 37. Hale WA, Delaney MJ, Cable T. Accuracy of patient recall and chart documentation of falls. J Am Board Fam Pract. 1993;6:239–242. [PubMed] [Google Scholar]
- 38. Mackenzie L, Byles J, D’Este C. Validation of self-reported fall events in intervention studies. Clin Rehabil. 2006;20:331–339. [DOI] [PubMed] [Google Scholar]
- 39. Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36:613–616. [DOI] [PubMed] [Google Scholar]
- 40. Vogt MT, Rubin D, Valentin RS, et al. Lumbar olisthesis and lower back symptoms in elderly white women. The Study of Osteoporotic Fractures. Spine (Phila Pa 1976). 1998;23:2640–2647. [DOI] [PubMed] [Google Scholar]
- 41. Kauppila LI, Eustace S, Kiel DP, Felson DT, Wright AM. Degenerative displacement of lumbar vertebrae. A 25-year follow-up study in Framingham. Spine (Phila Pa 1976). 1998;23:1868–1873. [DOI] [PubMed] [Google Scholar]
- 42. Kalichman L, Kim DH, Li L, Guermazi A, Berkin V, Hunter DJ. Spondylolysis and spondylolisthesis: prevalence and association with low back pain in the adult community-based population. Spine. 2009;34:199–205. doi:10.1097/BRS.0b013e31818edcfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009;9:545–550. doi:10.1016/j.spinee.2009.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.