Abstract
Background:
This study contributes to dialogue on quality versus quantity of life by examining years older persons can expect to live in various states of pain.
Methods:
Data from seven waves of the Health and Retirement Study; N = 26,896; age 55+. Estimations using the Interpolative Markov Chain approach apply probability transitions to multistate life table functions. Two estimates are interpreted: (i) population-based, which provide population averages aggregated across baseline states and (ii) status-based, which provide independent estimates by baseline state. Age- and sex-specific years with no pain, milder nonlimiting, and severe or limiting pain are reported as is percent of life in states of pain.
Results:
Females have higher life expectancy than males but similar expectations of pain-free life. Total life expectancy varies only slightly by baseline pain states but pain-free life expectancy varies greatly. For example, an 85-year-old female pain-free at baseline expects 7.04 more years, 5.28 being pain-free. An 85-year-old female with severe pain at baseline expects 6.42 years with only 2.66 pain-free. Percent of life with pain decreases by age for those pain-free at baseline and increases for those with pain at baseline.
Conclusion:
Pain is moderately associated with quantity of or total life but substantially and importantly associated with quality of or pain-free life.
Keywords: Aging, Longevity, Demography, Health and Retirement Survey, Multistate life tables, Interpolative Markov Chains, Quality of life
Recent years has seen a proliferation of pain research concentrated on older persons (1,2). This emerging field has been investigating a range of topics including how older persons experience and cope with pain, determinants of pain in old age, its underlying causes, pain management, pain as a risk factor for functional limitations, depression, mortality and other health outcomes, and the association between pain and dementia (3). Motivations for focusing pain studies specifically on older persons include a higher prevalence relative to younger age groups and clinical and theoretical differences in the ways in which pain is interpreted by and affects older versus younger persons. There are also broad demographic reasons for a rise in interest on aging and pain. Rapid population aging, defined as an increase in the number and proportion of populations that are in old age, is ongoing in every corner of the world (4). Population aging is normally accompanied by increasing life expectancies and increasing numbers of older old, for instance age 85+. These changes are eliciting concerns about whether adding years to life means adding healthy and quality years (5,6). Pain is an important component of these concerns.
Broadly speaking, pain has long been implicated as a contributor to both quantity and quality of life (7–9). Domains of life quality most impacted upon by pain are the related areas of physical functioning and disability (10). Research has suggested that the prevalence of pain, while increasing with age through younger and middle adult ages, may plateau in early old age (11). Other research has indicated that an inverse association between pain and physical functioning strengthens with advancing age, making the connection between pain and quality of life particularly relevant for older persons (12). Global Burden of Disease data has indicated musculoskeletal disorders and low back pain to be among the greatest contributors to years lost to disability worldwide (13). Sex differences in this link exist. Age-specific prevalence of musculoskeletal pain, specifically as a result of osteoarthritis, a condition very prevalent among older persons, is substantially higher among females (14,15). In sum, despite variation by age and sex, pain is a consistent factor affecting disability among older persons and is implicated in onset, progression, and recovery of physical mobility restrictions, and in turn quality of life.
The current study contributes to the dialogue on quality versus quantity of life by examining years of life that older persons can expect to live in pain. The demographic practice of estimating life expectancy across states of health has been effective for estimating levels and trends in disability-free life across populations (16,17). The study uses a multistate life-table approach to estimate years lived across states of pain by age and sex for the U.S. population aged 55+. The approach applies transition probabilities, which are probabilities of changing health states over a time period, to life-tables. The technique is particularly useful when longitudinal panel data can be employed to assess transitions across conditions characterized by frequent movements into and out of health states since such conditions will be commonly experienced at some point in life. Pain is one such condition (18–20). In addition to moving into and out of pain, recovery and movement into and out of more and less severe states is usual (18,21). Consequently, pain is a common experience for older persons; onset, progression, and recovery are common; the majority will experience pain at some time; and, estimates of pain expectancy, absent from the aging and pain literature thus far, are useful for assessing impact of pain on population health.
Methods
Data
Data are from 2000 to 2012 waves of the Health and Retirement Study (HRS). HRS is a national longitudinal panel survey conducted every 2 years. In 2000, when the sample was 53 and older, HRS began following up individuals in nursing homes. We employ the 55+ population since each biennial sample from 2000, when weighted, is representative of the total U.S. population in that age group. The sample consists of 17,382 persons aged 55 or older in 2000 plus 9,514 who were part of the 2004 or 2010 add-on or were aged-in, that is, were younger than 55 in 2000 or when first interviewed but turned 55 for a subsequent wave (total N = 26,896). HRS response rates are close to 90%. Documentation can be found on the HRS website (22). The HRS is a good data source for investigating pain expectancy for several reasons, notably: it is generalizable; it documents dates of death matched to the National Death Index; and, it consists of identical pain items across waves.
Measures
Three survey questions about pain are used. The first asked whether respondents are “often troubled with pain.” If yes, they were asked: “how bad is the pain most of the time: mild, moderate or severe?” and “does the pain make it difficult for you to do normal activity?” From 2000 to 2012, 33.3% report being troubled by pain. Of those troubled, 24.0% report their pain is severe, and 45.0% report their pain makes it difficult to conduct normal activities. We derive a three-category outcome with the following attributes: no pain, pain that is mild/moderate and does not limit activity (referred to as milder pain), and pain that is severe or limits activity (referred to as severe pain).
Dates of death are recorded in HRS “tracker files” (23). Month and year were taken during “exit” interviews conducted with next of kin. Dates are matched to the National Death Index. For about 6% with missing dates of death, a date is imputed (24). To examine reliability of mortality in HRS, we compared life expectancy using HRS data, measured between 2000 and 2012, with U.S. life expectancy in 2005 published by the CDC (25). Our data map almost precisely to the CDC report.
Analytical Strategy
Multistate life-table estimations of total, pain, and pain-free life expectancy, with pain divided into milder nonlimiting and severe or limiting, are conducted using the Interpolative Markov Chain (IMaCh) approach (26,27). IMaCh is frequently employed to examine life and healthy life expectancy across populations, to investigate population level impacts of disability risk factors, and to assess population health changes over time (16,28–31). IMaCh produces “population-based” estimates, which aggregates total population across baseline states providing average population expectancies, and “status-based,” which provide independent estimates by baseline state.
IMaCh estimation involves several steps: (i) Multinomial logistic regression derives parameters for health transition log odds. We included age and sex as covariates and tested interactions between age and sex. At baseline, a subject belongs to one of three states: no pain, milder, or severe. From each state, there are four possible transitions: retention of same state, improvement (eg, milder to no pain), deterioration (eg, milder to severe), or death. One equation is estimated for each baseline state. (ii) Parameters are translated into age- and sex-specific transition probabilities. (iii) Transition probabilities are inputted into multistate life-table functions (32). The result is person years lived in states of pain by age and sex and total life expectancy. Two types of results are shown below: number of years with no, milder, or severe pain, with the sum being total life expectancy, and percent of remaining life expected in pain states.
Results
Population-Based Estimates
Table 1 shows distributions for age and sex at baseline according to pain at baseline. Those with pain are more likely to be female although there is little variation in mean age across baseline pain states.
Table 1.
Distributions for Age and Sex of Baseline Sample According to Pain at Baseline
| Pain at Baseline | ||||
|---|---|---|---|---|
| No Pain | Milder | Severe | Total | |
| N | 18,786 | 2,572 | 5,538 | 26,896 |
| % female | 52.9 | 55.4 | 63.5 | 55.3 |
| Mean age (SD) | 65.9 (9.9) | 65.6 (10.1) | 65.4 (10.3) | 65.8 (10.0) |
Table 2 displays population-based estimates for males and females for ages 55, 65, 75, and 85 with 95% confidence intervals (CIs). A 55-year-old male has a life expectancy of 24.7 years (95% CI: 24.3–25.0); 17.3 years (95% CI: 17.0–17.6) are pain-free; 2.8 (95% CI: 2.7–3.0) are with milder pain; and 4.5 (95% CI: 4.3–4.7) are with severe pain. Females at age 55 have a higher life expectancy at 27.4 (95% CI: 27.0–27.7) years, but almost the same expectation for pain-free years. This means extra years of life for females at age 55 are years with pain. Females at age 85 live more years than males in all three states.
Table 2.
Population-Based Estimates for Expectation of Life Pain-Free and With Pain by Selected Ages and Sex, With 95% CIs in Parentheses
| Life Expected | |||||
|---|---|---|---|---|---|
| Sex | Age | Pain-Free | Milder Pain | Severe Pain | Total |
| Males | 55 | 17.3 (17.0–17.6) | 2.8 (2.7–3.0) | 4.5 (4.3–4.7) | 24.7 (24.3–25.0) |
| 65 | 11.8 (11.5–12.0) | 1.9 (1.8–2.0) | 3.0 (2.9–3.1) | 16.7 (16.4–16.9) | |
| 75 | 7.2 (7.1–7.4) | 1.1 (1.1–1.2) | 1.8 (1.7–1.9) | 10.2 (9.9–10.4) | |
| 85 | 4.0 (3.9–4.2) | 0.6 (0.6–0.6) | 1.0 (0.9–1.1) | 5.6 (5.4–5.8) | |
| Females | 55 | 17.3 (16.9–17.6) | 3.1 (3.0–3.2) | 7.0 (6.8–7.3) | 27.4 (27.0–27.7) |
| 65 | 12.1 (11.9–12.4) | 2.1 (2.0–2.2) | 4.8 (4.7–5.00) | 19.1 (18.8–19.3) | |
| 75 | 7.7 (7.5–7.9) | 1.3 (1.2–1.4) | 3.0 (2.9–3.1) | 12.1 (11.8–12.3) | |
| 85 | 4.4 (4.3–4.6) | 0.7 (0.7–0.8) | 1.7 (1.6–1.8) | 6.9 (6.7–7.1) | |
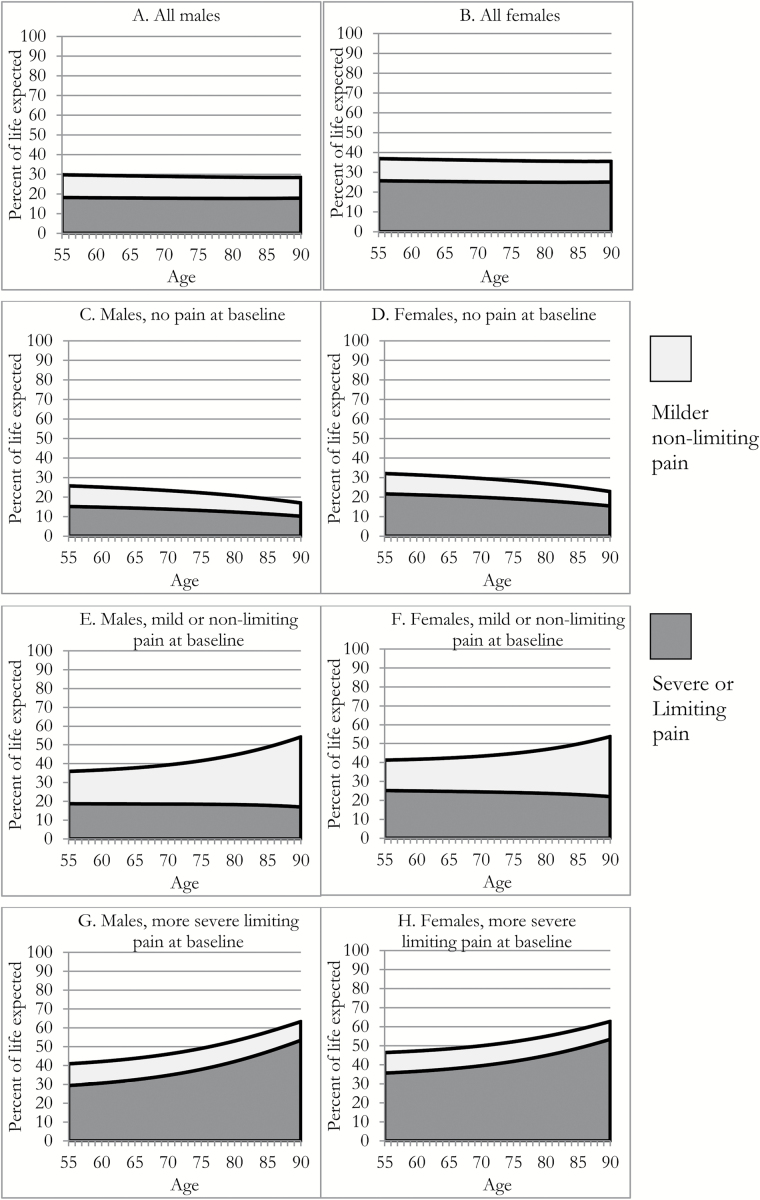
Figure 1A and B shows percent of remaining life in different pain states across ages 55–90. Shades indicate percent of remaining life with milder and with severe pain. The height of the two indicates total percent of life expected with pain. About the same percent is lived with and without pain, with milder pain, and with severe pain, across ages. There is, however, sex variation. While both males and females, at any age, expect around 11% of remaining life to be with milder pain, for severe pain, it is 18% for males compared to 25% for females. In total, males aged 55–90 live 29% of remaining life with pain and about 71% pain-free compared to about 36% and 64% for females.
Figure 1.
Population and status-based estimates for percent of remaining life expected with pain. (A and B) indicates the percent of remaining life expected to be lived with milder nonlimiting and severe or limiting pain by age and sex, for the total population estimated from population-based multistate life table modeling. (C and D) indicates these percentage for the subset of the population that report no pain at baseline, estimated from status-based multistate life table modeling. (E and F) indicates these percentage for the subset of the population that report milder nonlimiting pain at baseline, estimated from status-based multistate life table modeling. (G and H) indicates these percentage for the subset of the population that report severe or limiting pain at baseline, estimated from status-based multistate life table modeling.
Status-Based Estimates
Table 3 shows that total life expectancy varies only slightly across baseline states. For instance, males at age 55 that are pain-free at baseline have a life expectancy of 24.9 (95% CI: 24.6–25.3) compared to 24.6 (95% CI: 24.3–25.0) for those with milder pain and 23.6 (95% CI: 23.2–24.0) for those with severe pain. As such, a 55-year-old male that has severe pain at baseline will live on average 1.3 fewer years, or about 5% fewer, than a similarly aged male pain-free at baseline. Similar to males, life expectancy for females does not vary much across baseline states. An 85-year-old female pain-free can expect 7.0 (95% CI: 6.9–7.2) years compared to 7.0 (95% CI: 6.7–7.2) for a similarly aged female with milder pain and 6.4 (95% CI: 6.2–6.6) if she has severe pain. The 85-year-old female with severe pain therefore lives 0.6 fewer total years, or about 9% fewer, than a similarly aged female that is pain-free.
Table 3.
Status-Based Estimates of Expectation of Life Pain-Free and With Pain by Selected Ages and Sex, With 95% CIs in Parentheses
| Life Expected | |||||
|---|---|---|---|---|---|
| Sex | Age | Pain-Free | Milder Pain | Severe Pain | Total |
| Baseline State: Pain-Free | |||||
| Males | 55 | 18.5 (18.2–18.8) | 2.6 (2.5–2.7) | 3.8 (3.7–3.9) | 24.9 (24.6–25.3) |
| 65 | 12.8 (12.6–13.1) | 1.7 (1.6–1.8) | 2.4 (2.3–2.5) | 17.0 (16.7–17.7) | |
| 75 | 8.1 (7.9–8.3) | 0.9 (0.9–1.0) | 1.4 (1.3–1.4) | 10.4 (10.2–10.6) | |
| 85 | 4.6 (4.5–4.8) | 0.4 (0.4–0.5) | 0.7 (0.6–0.7) | 5.7 (5.6–5.9) | |
| Females | 55 | 18.8 (18.5–19.1) | 2.9 (2.8–3.0) | 6.0 (5.8–6.2) | 27.6 (27.3–28.0) |
| 65 | 13.5 (13.2–13.7) | 1.9 (1.9–2.0) | 4.0 (3.9–4.1) | 19.4 (19.1–19.6) | |
| 75 | 8.8 (8.7–9.0) | 1.1 (1.9–1.2) | 2.4 (2.3–2.5) | 12.3 (12.1–12.6) | |
| 85 | 5.3 (5.1–5.4) | 0.6 (0.5–0.6) | 1.2 (1.1–1.3) | 7.0 (6.9–7.2) | |
| Baseline State: Milder | |||||
| Males | 55 | 15.8 (15.5–16.1) | 4.2 (4.1–4.4) | 4.6 (4.4–4.8) | 24.6 (24.3–25.0) |
| 65 | 10.4 (10.1–10.6) | 3.2 (3.1–3.3) | 3.1 (3.0–3.2) | 16.7 (16.4–17.0) | |
| 75 | 6.0 (5.8–5.8) | 2.4 (2.3–2.4) | 1.9 (1.8–2.0) | 10.2 (9.9–10.4) | |
| 85 | 2.8 (2.7–3.1) | 1.7 (1.7–1.8) | 1.0 (0.9–1.1) | 5.6 (5.4–5.9) | |
| Females | 55 | 16.1 (15.8–16.4) | 4.4 (4.3–4.5) | 6.9 (6.7–7.1) | 27.4 (27.1–27.8) |
| 65 | 11.0 (10.8–11.3) | 3.4 (3.3–3.5) | 4.7 (4.6–4.9) | 19.1 (18.9–19.4) | |
| 75 | 6.7 (6.5–6.9) | 2.5 (2.4–2.6) | 2.9 (2.8–3.1) | 12.2 (11.9–12.4) | |
| 85 | 3.5 (3.3–3.7) | 1.9 (1.8–1.9) | 1.6 (1.5–1.7) | 7.0 (6.7–7.2) | |
| Baseline State: Severe | |||||
| Males | 55 | 14.0 (13.6–14.2) | 2.7 (2.6–2.8) | 6.9 (6.7–7.1) | 23.6 (23.2–24.0) |
| 65 | 8.7 (8.5–9.0) | 1.8 (1.7–1.8) | 5.0 (4.9–5.2) | 15.5 (15.2–15.8) | |
| 75 | 4.7 (4.5–4.9) | 1.0 (1.0–1.1) | 3.5 (3.4–3.6) | 9.2 (8.9–9.4) | |
| 85 | 2.1 (2.0–2.2) | 0.5 (0.5–0.6) | 2.4 (2.3–2.5) | 5.0 (4.8–5.2) | |
| Females | 55 | 14.3 (14.0–14.6) | 2.9 (2.8–3.0) | 9.5 (9.3–9.7) | 26.7 (26.3–27.1) |
| 65 | 9.4 (9.2–9.7) | 1.9 (1.9–2.0) | 6.9 (6.7–7.1) | 18.3 (18.0–18.6) | |
| 75 | 5.4 (5.2–5.6) | 1.2 (1.1–1.2) | 4.7 (4.6–4.9) | 11.3 (11.1–11.6) | |
| 85 | 2.7 (2.5–2.8) | 0.6 (0.6–0.7) | 3.1 (3.0–3.2) | 6.4 (6.2–6.6) | |
In contrast to total life, life expected with and without pain varies greatly across baseline state (Table 3). For instance, pain-free expectancy for a 55-year-old male is 18.5 (95% CI: 18.2–18.8) if he is pain-free at baseline, 15.8 (95% CI: 15.5–16.1) if he has milder pain at baseline, and 14.0 (95% CI: 13.6–14.2) if he has severe pain. Therefore, the 55-year-old pain-free male lives 4.5 more pain-free years, or about 24% more, than his 55-year-old counterpart with severe pain. Differences in pain-free years are more dramatic in older ages. An 85-year-old female pain-free at baseline can expect 5.3 (95% CI: 5.1–5.4) pain-free years, but only 2.7 (95% CI: 2.5–2.8) if she has severe pain at baseline. Further, the 85-year-old female pain-free at baseline can expect 1.2 (95% CI: 1.1–1.3) years of life with severe pain, but 3.1 (95% CI: 3.0–3.2) severe pain years if she has severe pain at baseline. Said differently, the 85-year-old female with severe pain lives 1.9 more years with severe pain, or about 160% more, than her counterpart pain-free at baseline.
Figure 1C–H translates status-based results into percent of life in states of pain. Variations by age are substantial and differ considerably across baseline states. For those pain-free at baseline, the percent of remaining life with either milder or more severe pain decreases with age. For instance, a 55-year-old male pain-free at baseline can expect 26% of remaining life with pain, while a 90-year-old pain-free male can expect only 17% with pain. The percentages for a 55-year-old female are 32% at age 55 and 23% at age 90. But, the percent with pain increases with age among those with pain at baseline. The increase, and whether it is with milder or severe pain, depends on baseline state. With milder pain at baseline, the percent of life with milder pain increases with age, for males and females, while the percent with severe pain remains fairly stable. In comparison, for those with severe pain, the percent with severe pain increases with age while the percent with milder pain remains stable. The increase in percent of life with severe pain is particularly sharp for those in this state at baseline. For males, the percent of remaining life with severe pain increases from 29% to 53% between ages 55 and 90. For females, the increase is from 36% to 53%. Note that while 55-year-old females with severe pain live a greater proportion of life with severe pain than do men, by very old ages, the percentages are similar.
Discussion
In this study, multistate life-tables were used to estimate pain-free life expectancy and expectancy with milder and severe pain among Americans aged 55+. A 55-year-old male can expect 24.7 years of life, of which 17.3 are pain-free, 2.8 are with milder, and 4.5 are with severe pain. A similarly aged female has greater longevity—27.4 years—but extra years are lived with pain—3.1 with milder and 7.0 with severe pain. Thus, while the pain-free life expectancy of males and females across ages is about equal, females live more years with pain, and with more severe pain. As males and females age, life expectancy decreases. But, proportion of life expected with pain does not change. These population-based findings are in line with previous literature indicating a plateau effect, or that pain prevalence remains stable throughout old age (1,11,33).
Status-based results divide the population into baseline states and reveal heterogeneity in pain burden. Baseline pain has little impact on total life expectancy. A 55-year-old female pain-free can expect only 1 more total year of life than her age counterpart with severe pain. In contrast, life expected to be lived pain-free and with severe pain is affected by baseline state. The 55-year-old female with severe pain lives 4½ fewer pain-free years and 3½ more severe pain years than her pain-free counterpart. By 90, the great majority of remaining years of life are lived pain-free for those without pain at baseline, but with severe pain for those with severe pain at baseline.
Because the association between age and remaining life with pain is inconsistent across baseline states, the often cited plateau effect is heterogeneous. The proportion of remaining life with milder or severe pain decreases with age if pain-free at baseline. The proportion with milder pain increases with age for those with milder pain at baseline, and the proportion with severe pain increases with age for those with severe pain at baseline. As one example, a 55-year-old female pain-free will live 22% of remaining life with severe pain compared to 36% for a similarly aged female with severe pain. By age 90, this percentage decreases to 15% for pain-free women but increases to 53% for women with severe pain. Thus, a woman with severe pain has several disadvantages. She will live a greater proportion of her life with severe pain, and the older she gets the larger this proportion becomes.
The possible reasons for decreases in pain-free life expectancy among those with pain at baseline are many. Pain may be indicative of life-long lingering conditions. Common conditions that lead to pain are not always life threatening, such as osteoarthritis. At the same time, pain itself can have adverse effects that can lead to continuing pain and comorbidity. Research has indicated pain sensitivity itself can set in motion inflammatory responses that themselves result in pain (34). Future research should extend upon our findings to explore causes and consequences of the association between baseline pain and pain-free life expectancy.
Limitations of this study include challenges involved in interpreting self-assessments of pain across some demographic subgroups. It is difficult to assess pain among those experiencing sensory deficits and/or cognitive impairments. To be generalizable to the entire population, the current study included those living in nursing homes. However, institutionalized may be vulnerable to dementia, which can affect pain reporting (35). Males, females, and different racial and ethnic groups report pain differently (36). Medical interventions can affect the experience of pain. Given the increase in polypharmacy among older persons (37), the interaction between medication use and reported pain should be examined in future research. Still, self-report remains the most common way to assess pain presence and prevalence in research.
In conclusion, this study suggested that while pain is only moderately associated with quantity of life, it is more substantially and importantly associated with quality of life. In some ways, this result stands in contrast to studies that have linked pain to mortality (8). In our study, pain is shown to relate to lower life expectancy, but only slightly so. Rather, pain relates more robustly to pain-free life expectancy such that, in a sense, pain begets pain. Those with pain are destined to spend a large percentage of their remaining lives with pain and of those years, a large percentage with severe pain. Therefore, while our study does not specifically show transitions into and out of pain states, the findings suggest that recovery, particularly long-term, from severe pain is infrequent. This has implications for pain coping strategies among older persons. Clearly, while primary prevention of pain is important, our study infers that pain management is also essential for the maintenance of quality of life (38).
Further, these findings have implications on a societal level. A common discourse in the aging literature is whether added years of life are bringing with them added years of life quality. The term compression of morbidity is often used to describe the notion that increasing lifespan and reductions in life expected with disability are associated (39). The compression of morbidity debate has not considered life expected with and without pain. The debate would benefit from first better situating pain within the disablement process, and second, better elucidating the association between pain and disability in old age. This study suggests a compression may depend upon reducing the proportion of population that begins old age with pain.
Funding
Data for this study come from the Health and Retirement Study sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan.
Conflict of Interest
The authors confirm no conflicts of interest.
References
- 1. Gibson SJ, Lussier D. Prevalence and relevance of pain in older persons. Pain Med. 2012;13(suppl 2):S23–S26. doi:10.1111/j.1526-4637.2012.01349.x [DOI] [PubMed] [Google Scholar]
- 2. Gagliese L. Pain and aging: The emergence of a new subfield of pain research. J Pain. 2009;10:343–353. doi:10.1016/j.jpain.2008.10.013 [DOI] [PubMed] [Google Scholar]
- 3. Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17:417–31, v. doi:10.1016/S0749-0690(05)70078-1 [DOI] [PubMed] [Google Scholar]
- 4. Zimmer Z, McDaniel S. Global ageing in the twenty-first century: An introduction. In: McDaniel S and Zimmer Z, eds. Global Ageing in the Twenty-First Century: Challenges, Opportunities and Implications. Surrey, UK: Ashgate; 2013:1–12. [Google Scholar]
- 5. Jacobzone S. Coping with aging: International challenges. Health Aff (Millwood). 2000;19:213–225. doi:10.1377/hlthaff.19.3.213 [DOI] [PubMed] [Google Scholar]
- 6. Lloyd-Sherlock P. Population ageing in developed and developing regions: Implications for health policy. Soc Sci Med. 2000;51:887–895. doi:10.1016/S0277-9536(00)00068-X [DOI] [PubMed] [Google Scholar]
- 7. Feeny D, Huguet N, McFarland BH, Kaplan MS, Orpana H, Eckstrom E. Hearing, mobility, and pain predict mortality: A longitudinal population-based study. J Clin Epidemiol. 2012;65:764–777. doi:10.1016/j.jclinepi.2012.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Torrance N, Elliott AM, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14:380–386. doi:10.1016/j.ejpain.2009.07.006 [DOI] [PubMed] [Google Scholar]
- 9. Niv D, Kreitler S. Pain and quality of life. Pain Pract. 2001;1:150–161. doi:10.1046/j.1533-2500.2001.01016.x [DOI] [PubMed] [Google Scholar]
- 10. Soldato M, Liperoti R, Landi F, et al. Non malignant daily pain and risk of disability among older adults in home care in Europe. Pain. 2007;129:304–310. doi:10.1016/j.pain.2006.10.016 [DOI] [PubMed] [Google Scholar]
- 11. Patel KV, Guralnik JM, Dansie EJ, Turk DC. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154:2649–2657. doi:10.1016/j.pain.2013.07.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi:10.1046/j.1532-5415.2003.51152.x [DOI] [PubMed] [Google Scholar]
- 13. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. doi:10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wijnhoven HA, de Vet HC, Picavet HS. Explaining sex differences in chronic musculoskeletal pain in a general population. Pain. 2006;124:158–166. doi:10.1016/j.pain.2006.04.012 [DOI] [PubMed] [Google Scholar]
- 15. Leveille SG, Penninx BW, Melzer D, Izmirlian G, Guralnik JM. Sex differences in the prevalence of mobility disability in old age: The dynamics of incidence, recovery, and mortality. J Gerontol B Psychol Sci Soc Sci. 2000;55:S41–S50. doi:10.1093/geronb/55.1.S41 [DOI] [PubMed] [Google Scholar]
- 16. Crimmins EM, Hayward MD, Hagedorn A, Saito Y, Brouard N. Change in disability-free life expectancy for Americans 70-years-old and older. Demography. 2009;46:627–646. doi:10.1353/dem.0.0070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cambois E, Robine JM, Hayward MD. Social inequalities in disability-free life expectancy in the French male population, 1980-1991. Demography. 2001;38:513–524. doi:10.1353/dem.2001.0033 [DOI] [PubMed] [Google Scholar]
- 18. Maxwell CJ, Dalby DM, Slater M, et al. The prevalence and management of current daily pain among older home care clients. Pain. 2008;138:208–216. doi:10.1016/j.pain.2008.04.007 [DOI] [PubMed] [Google Scholar]
- 19. Rottenberg Y, Jacobs JM, Stessman J. Prevalence of pain with advancing age brief report. J Am Med Dir Assoc. 2015;16:264.e1–264.e5. doi:10.1016/j.jamda.2014.12.006 [DOI] [PubMed] [Google Scholar]
- 20. Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: A prevalence study. Pain. 2001;89:127–134. doi:10.1016/S0304-3959(00)00355-9 [DOI] [PubMed] [Google Scholar]
- 21. Eriksen J, Ekholm O, Sjøgren P, Rasmussen NK. Development of and recovery from long-term pain. A 6-year follow-up study of a cross-section of the adult Danish population. Pain. 2004;108:154–162. doi:10.1016/j.pain.2003.12.018 [DOI] [PubMed] [Google Scholar]
- 22. Health and Retirement Study. Health and Retirement Study: A Longitudinal Study of Health, Retirement, and Aging Sponsored by the National Institute on Aging. University of Michigan; 2015. http://hrsonline.isr.umich.edu Accessed April 13, 2015. [Google Scholar]
- 23. Health and Retirement Study. Tracker 2012, Early, Version 1.0, June, 2014, Data Description. Available at http://hrsonline.isr.umich.edu/index.php?p=shoavail&iyear=ZS. Accessed February 18, 2016. [Google Scholar]
- 24. Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: A national longitudinal study. Soc Sci Med. 2012;74:907–914. doi:10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Arias E, Rostron BL, Tejada-Vera B. United States life tables, 2005. Natl Vital Stat Rep. 2010;58:1–132. [PubMed] [Google Scholar]
- 26. Lievere A, Brouard N, Heathcote C. The estimation of health expectancies from cross-longitudinal surveys. Math Pop Stud. 2003;10:211–248. doi:10.1080/713644739 [Google Scholar]
- 27. Saito Y, Robine J-M, Crimmins EM. The methods and materials of health expectancy. Stat J IAOS. 2014;30:209–223. doi:10.3233/SJI-140840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jagger C, Matthews R, Matthews F, Robinson T, Robine JM, Brayne C; Medical Research Council Cognitive Function and Ageing Study Investigators The burden of diseases on disability-free life expectancy in later life. J Gerontol A Biol Sci Med Sci. 2007;62:408–414. [DOI] [PubMed] [Google Scholar]
- 29. Kaneda T, Zimmer Z, Tang Z. Socioeconomic status differentials in life and active life expectancy among older adults in Beijing. Disabil Rehabil. 2005;27:241–251. doi:10.1080/09638280400006481 [DOI] [PubMed] [Google Scholar]
- 30. Lièvre A, Alley D, Crimmins EM. Educational differentials in life expectancy with cognitive impairment among the elderly in the United States. J Aging Health. 2008;20:456–477. doi:10.1177/0898264308315857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Minicuci N, Noale M, Pluijm SMF, et al. Disability-free life expectancy: A cross-national comparison of six longitudinal studies on aging. The CLESA project. Eur J Ageing. 2004;1:37–44. doi:10.1007/s10433-004-0002-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Crimmins EM, Hayward MD, Saito Y. Changing mortality and morbidity rates and the health status and life expectancy of the older population. Demography. 1994;31:159–175. doi:10.2307/2061913 [PubMed] [Google Scholar]
- 33. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL., 3rd Sex, gender, and pain: A review of recent clinical and experimental findings. J Pain. 2009;10:447–485. doi:10.1016/j.jpain.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Watkins LR, Maier SF, Goehler LE. Immune activation: The role of pro-inflammatory cytokines in inflammation, illness responses and pathological pain states. Pain. 1995;63:289–302. doi:10.1016/0304-3959(95)00186-7 [DOI] [PubMed] [Google Scholar]
- 35. Scherder E, Herr K, Pickering G, Gibson S, Benedetti F, Lautenbacher S. Pain in dementia. Pain. 2009;145:276–278. doi:10.1016/j.pain.2009.04.007 [DOI] [PubMed] [Google Scholar]
- 36. Jacobs JM, Hammerman-Rozenberg R, Cohen A, Stessman J. Chronic back pain among the elderly: Prevalence, associations, and predictors. Spine (Phila Pa 1976). 2006;31:E203–E207. doi:10.1097/01.brs.0000206367.57918.3c [DOI] [PubMed] [Google Scholar]
- 37. Charlesworth CJ, Smit E, Lee DS, Alramadhan F, Odden MC. Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Gerontol A Biol Sci Med Sci. 2015;70: 989–995. doi:10.1093/gerona/glv013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Katz N. The impact of pain management on quality of life. J Pain Symptom Manage. 2002;24(suppl 1):S38–S47. doi:10.1016/S0885-3924(02) 00411-6 [DOI] [PubMed] [Google Scholar]
- 39. Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi:10.1056/NEJM198007173030304 [DOI] [PubMed] [Google Scholar]