Abstract
Background:
Hip fractures are associated with significant morbidity and mortality in the nursing home. Our objective was to describe the incidence rate (IR) of hip fracture according to age, sex, and race in a nationwide sample of long-stay nursing home residents.
Methods:
Using 2007–2010 Medicare claims data linked with the Minimum Data Set, we identified 892,837 long-stay residents (≥100 days in the same nursing facility) between May 1, 2007 and April 30, 2008. Hip fractures were defined using Part A diagnostic codes (ICD-9). Residents were followed from the date they became a long-stay resident until the first event of death, discharge, hip fracture, or 2 years of follow-up.
Results:
Mean age was 84 years (range 65–113 years), and 74.5% were women. 83.9% were white and 12.0% were black. The overall IR of hip fracture was 2.3/100 person years. The IR was similar in men and women across age groups. The IR of hip fracture was highest in Native Americans aged 85 years or older (3.7/100 person years), in whites (2.6/100 person years), and during the first 100 days of institutionalization (2.7/100 person years). IRs of hip fracture were lowest in blacks (1.3/100 person years).
Conclusions:
In nursing home residents surviving 100 days or more in a facility, the incidence of hip fracture is high, particularly among older white, Native American, and newly admitted residents. This is the first nationwide study to provide sex- and age-specific estimates among U.S. nursing home residents, and it underscores the magnitude of the problem.
Keywords: Nursing home, Hip fracture, Incidence rate, Race
Each year in the United States, nearly 300,000 persons experience a hip fracture (1). Nursing home residents are at a twofold greater risk of hip fracture as compared with community dwellers (2,3). Risk of rehospitalization at 1 year is more than 10-fold greater among nursing home residents with a recent hip fracture as compared with residents without fracture (4). In addition, hip fractures in the nursing home lead to infections and pressure ulcers (5,6), functional decline (7,8), and poor quality of life (8). Not surprisingly, mortality is high following a hip fracture in the nursing home: one in every three nursing home residents will die within 180 days of a hip fracture, and one in every two male residents will die within the same time period (9).
Despite the gravity of hip fractures in the nursing home setting, no prior studies have estimated the incidence of fracture in U.S. nursing homes using nationwide data. Rather, prior studies have selected residents as part of a trial (10) or from a single state (11), which could result in biased and poorly generalizable estimates of hip fracture. An accurate nationwide estimate of hip fracture in nursing home residents according to age and sex is important, because it can inform screening strategies, future interventions, and national policies aimed at ameliorating this problem. Our objective then, was to describe the incidence rate (IR) of hip fracture according to age, sex, and race in a national sample of long-stay nursing home residents.
Methods
Participants
For our source population, 100% sample of Medicare Part A claims from 2007 to 2010 was linked to nursing home resident assessments using unique, individual identifiers for all nursing home residents enrolled in a fee-for-service Medicare program (12). We defined a long-stay nursing home resident as someone who spent 100 days or more in the same nursing facility with no more than 10 consecutive days outside the facility. In the United States, persons are eligible for long-stay nursing home care if they have a chronic illness or physical or mental disability that requires assistance, and they cannot retain adequate support in the community.
Among more than 9 million persons identified with a Medicare Fee-for-service Part A claim, we identified a dynamic cohort of 1,461,472 residents that met our definition of a long-stay resident at any time between May 1, 2007 and April 30, 2008. Seventy-two percent of the cohort met our definition of long stay on May 1, 2007, whereas the remainder were “newly admitted” and qualified as long stay by April 30, 2008. We excluded the following residents from our sample: 46,584 residents without 6 months of Medicare Part A enrollment and 147,755 residents enrolled in Medicare Advantage, who do not have claims data available to ascertain hip fractures; 109,043 residents younger than 65 years; and 76,480 residents enrolled in Hospice. Because this study is part of a project to develop a screening tool for fracture, we additionally excluded 18,467 residents without a Minimum Data Set (MDS) assessment within 100 days of study entry and 169,634 residents without a Part D prescription drug claim while in the nursing home. The final sample size was 892,837 long-stay residents.
Hip Fracture
Incident hip fractures were ascertained using Medicare Part A claims data. A hip fracture was defined as a hospitalization with the primary or secondary International Classification of Diseases, 9th edition (ICD-9) diagnosis of hip fracture (820.xx), with or without an accompanying procedural code (13). The estimated positive predictive value using a similar definition is 98%, with sensitivity of 96% (14). To be sure that we were including only new fractures that occurred while in the nursing home, we excluded fractures if the resident had a hospitalization for a hip fracture in the previous 100 days.
Other Characteristics
In order to describe our population, we obtained demographic information on age, sex, and self-reported race from the Medicare Enrollment file. Residents were grouped into the following age categories: 65–69 years, 70–74 years, 75–79 years, 80–84 years, 85–89 years, 90–94 years, or 95 years or older. Race was categorized as white, black, Hispanic, Asian, Native American, or other (15).
Information on functional status, as defined by the 28-point Katz Activities of Daily Living (ADL) Scale, was obtained from the MDS assessment closest to and before a resident became long stay (ie, Day 100 in the same nursing facility or May 1, 2007 for residents previously qualifying as long stay). Higher ADL scores indicate greater functional dependence. Cognitive status was ascertained using a similar approach with the Cognitive Performance Scale (16).
Statistical Analysis
Residents were followed from May 1, 2007 or the date they became a long-stay resident until the time of the first event of incident hip fracture, death, 60 days following discharge, or until 2 years from the index date. The IR of hip fracture (17) was calculated as the total number of hip fractures divided by 100 person years of follow-up time. IRs were calculated separately according to age, sex, and race. In secondary analyses, we calculated the IR of hip fracture according to functional and cognitive status and the IR of hip fracture in the first 100 days of institutionalization among the subset of newly admitted residents who survived 100 days.
Results
A total of 892,837 residents met our criteria for being “long stay.” The mean age of the residents in the cohort was 84 years (range 65–113 years), and 74.4% were women. In terms of race, 83.9% were white, 12.0% were black, and 4.1% were identified as other. During a mean follow-up of 1.8 years, 3.3% of the long-stay nursing home residents experienced a hip fracture, whereas 40.2% died and 10.4% were discharged alive without a hip fracture. Functional status, as measured by the mean ADL score, was slightly better in men as compared with that in women across age groups (mean score 13.6 in men aged 65–74 years compared with 14.8 in women; 14.7 in men aged 75–84 years compared with 15.4 in women; and 14.7 in men aged 85 years or older compared with 15.8 in women).
Table 1 describes the characteristics of the study population according to whether the resident experienced a hip fracture, death, or discharge during follow-up. A greater percentage of residents with a hip fracture and residents who died were aged 85 years and older, were female, and were of white race, compared with residents who were discharged or remained alive without a hip fracture.
Table 1.
Demographic Characteristics of 892,837 Long-stay Nursing Home Residents According to Whether They Experienced a Hip Fracture During Follow-up
| Experienced a Hip Fracture | Died Without a Hip Fracture | Discharged Without a Fracture | Alive Without a Fracture | |
|---|---|---|---|---|
| (n = 29,358) | (n = 358,790) | (n = 93,014) | (n = 411,675) | |
| Age (y) | ||||
| 65–69 | 1,273 (4.3) | 14,128 (3.9) | 9,747 (10.5) | 31,396 (7.6) |
| 70–74 | 2,072 (7.1) | 23,964 (6.7) | 11,718 (12.6) | 43,391 (10.5) |
| 75–79 | 3,993 (13.6) | 42,852 (11.9) | 15,783 (17.0) | 65,552 (15.9) |
| 80–84 | 6,589 (22.4) | 72,247 (20.1) | 19,958 (21.5) | 92,107 (22.4) |
| 85–89 | 7,654 (26.1) | 91,642 (25.5) | 19,382 (20.8) | 95,716 (23.3) |
| 90–94 | 5,552 (18.9) | 74,055 (20.6) | 11,803 (12.7) | 60,198 (14.6) |
| 95 and older | 2,225 (7.6) | 39,902 (11.1) | 4,623 (5.0) | 23,315 (5.7) |
| Female (%) | 22,857 (77.9) | 259,200 (72.2) | 66,681 (71.7) | 315,530 (76.6) |
| Race* (%) | ||||
| White | 26,586 (90.8) | 309,181 (86.4) | 73,381 (79.1) | 340,067 (82.8) |
| Black | 1,740 (5.9) | 36,790 (10.3) | 14,457 (15.6) | 54,473 (13.3) |
| Hispanic | 458 (1.6) | 5,293 (1.5) | 2,433 (2.6) | 7,552 (1.8) |
| Asian | 220 (0.8) | 3,314 (0.9) | 1,242 (1.3) | 4,421 (1.1) |
| Native American | 147 (0.5) | 1,232 (0.3) | 580 (0.6) | 1,566 (0.4) |
| Other | 140 (0.5) | 1,944 (0.5) | 725 (0.8) | 2,694 (0.7) |
*Among 890,636 residents (99.8%) with known race.
The overall IR of hip fractures among long-stay nursing home residents was 2.3/100 person years. Table 2 presents the IRs of hip fracture based on age and sex. Among women, the IR of hip fracture was 1.5/100 person between the ages of 65 and 69 years, increasing to 2.7/100 person years in women between the ages of 90 and 94 years. The IR of hip fracture was similar in men and women across age groups.
Table 2.
Incidence Rates of Hip Fracture in Long-stay Nursing Home Residents According to Age and Sex
| Age (y) | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Residents (n) | Hip Fractures (n) | Follow-up Time (y) | IR (per 100 person years) | Residents (n) | Follow-up time (y) | Hip Fractures (n) | IR (per 100 person years) | |
| 65–69 | 29,680 | 699 | 45,396 | 1.5 | 26,864 | 40,220 | 574 | 1.4 |
| 70–74 | 47,837 | 1,331 | 72,774 | 1.8 | 33,308 | 48,621 | 741 | 1.5 |
| 75–79 | 85,514 | 2,817 | 128,881 | 2.2 | 42,666 | 60,141 | 1,176 | 2.0 |
| 80–84 | 140,688 | 5,070 | 208,379 | 2.4 | 50,213 | 68,010 | 1,519 | 2.2 |
| 85–89 | 170,447 | 6,240 | 245,926 | 2.5 | 43,947 | 56,361 | 1,414 | 2.5 |
| 90–94 | 128,015 | 4,737 | 176,665 | 2.7 | 23,593 | 28,464 | 815 | 2.9 |
| 95 and older | 62,087 | 1,963 | 79,774 | 2.5 | 7,978 | 8,997 | 262 | 2.9 |
Note: IR = incidence rate.
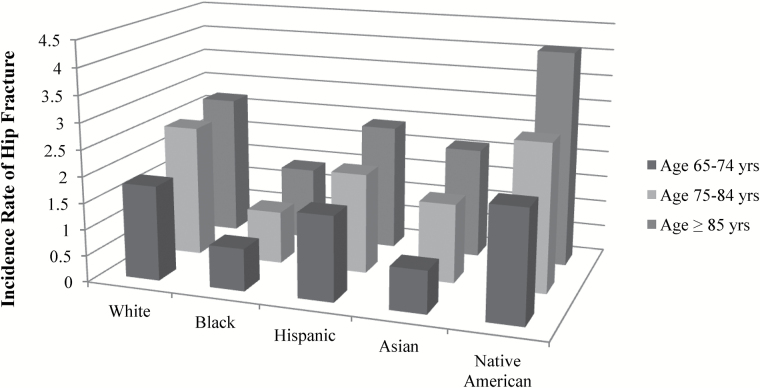
Figure 1 displays the IRs of hip fracture according to race and age. Rates of hip fracture increased with advancing age in all races. The IR of hip fracture was highest in Native Americans aged 85 years or older (3.7/100 person years) and whites (2.6/100 person years). IRs of hip fracture were lowest in blacks (1.3/100 person years in residents aged 85 years or older) and intermediate in Asians (2.2/100 person years) and Hispanics (2.1/ 100 person years) of the same age.
Figure 1.
Incidence rate of hip fracture in U.S. nursing home residents according to age and race.
Supplementary Table 1 describes the IRs of hip fracture according to functional and cognitive status. Rates of hip fracture decreased as ADL impairment increased. Low rates of fracture were observed in residents with very severe cognitive impairment (0.5 hip fracture/100 person years).
Among newly admitted long-stay residents who survived 100 days (n = 253,367), 1,877 experienced a hip fracture during the first 100 days of institutionalization. The IR of hip fracture in the first 100 days was 2.7/100 person years (2.1/100 person years in men and 3.0/100 person years in women).
Discussion
Overall, we found that the incidence of hip fracture in U.S. long-stay nursing home residents was high: 2.3/100 person years. Based on the fact that there are 1 million long-stay nursing home residents on any given day in the United States, 23,000 nursing home residents will fracture their hip each year, and one nursing home resident will fracture their hip every 23 minutes. Assuming that the average direct cost of a hospitalization for a hip fracture in a nursing home resident is $28,913 (18), the total direct cost to Medicare of hip fractures in long-stay residents alone totals more than 665 million dollars annually. Further, it suggests that 8% of all hip fractures in the United States occur in long-stay nursing home residents.
This is the first nationwide study to provide age-, sex-, and race-specific estimates of the incidence of hip fracture among long-stay nursing home residents in the United States. Rates of hip fracture increased with advancing age, and rates were greater in white and Native American residents as compared with those in blacks and other racial groups. Rates of fracture were also higher in the first 100 days of institutionalization. Rates of fracture were similar in male and female nursing home residents across age groups and despite comparable functional status. Fracture rates were low in residents with very severe cognitive or functional impairment.
Numerous studies have found that nursing home residents are at greater risk of hip fracture as compared with community dwellers of the same age. The high incidence of hip fracture that we observed in our study is consistent with these findings, particularly among young nursing home residents and men. For instance, we found an IR of hip fracture of 1.5 and 1.4/100 person years in women and men aged 65–69 years in our nursing home cohort. Estimates of the IR of hip fracture in U.S. community-dwelling women and men aged 65–79 years are much lower: 0.40–0.79 and 0.15–0.39/100 person years, respectively (19,20). In older male nursing home residents, the IR of hip fracture remains greater than the IR in community dwellers (2.5/100 person years in male nursing home residents aged 85–89 years as compared with 1.1–2.1/100 person years in community-dwelling men of similar age) (19,20). In contrast, in older female nursing home residents the incidence of hip fracture more closely approximates community dwellers: 2.5/100 person years in female residents aged 85–89 years as compared with an IR of 2.2–3.3/100 person years in community-dwelling women of similar age (19,20).
Because the high incidence of fracture in male and female nursing home residents is likely related to the burden of comorbidities and cognitive impairment, nursing homes must strive to provide optimal care to minimize fracture incidence in this setting. A few studies have found that poor quality indicators, such as a high resident to staff ratio and physical restraint use, are associated with an increased risk of falls in the nursing home (21,22). Future studies should consider whether variation in fracture incidence exists between nursing home facilities.
Few existing studies have specifically described the IR of hip fracture among nursing home residents. A prospective study in Maryland including 1,427 female nursing home residents from 47 facilities estimated the incidence of hip fracture as high as 4.4/100 person years (10). It is possible that rates of fracture are higher in this study because the study required consent and dual-energy x-ray absorptiometry screening, potentially selecting for women at higher risk of fracture. In other studies of nursing home residents that used claims data to ascertain fracture, the rate of fracture was high. A study of more than 42,000 nursing home residents in Germany estimated the incidence of hip fracture as 4.3 and 3.1/100 person years, in women and men, respectively (23). A study conducted in a single U.S. state estimated the incidence of hip fracture in nursing home residents to be more similar to that of our study (2.9/100 person years) (11). Differences in our findings may be explained because other cohorts included residents admitted for short-stay rehabilitation, or because of differences in age, sex, and race between the cohorts.
Prior studies provide conflicting evidence on whether fracture rates differ in men and women in the nursing home. Two large German studies reported the incidence of hip fracture to be greater in women as compared with that in men (23,24), whereas the study in a single U.S. state reported a similar rate in male and female nursing home residents (11). We also found similar rates of hip fracture in male and female nursing home residents across age groups. This finding does not appear to be explained by functional status, as men had a similar functional performance, as measured by the ADL score, as compared with women across all age groups and regardless of outcome.
Few studies have described the incidence of fracture in Native Americans, and none in the nursing home setting. The Nordic Research on Ageing (NORA) study found that the incidence of all fracture types in Native American women was similar to the incidence in whites and Hispanics; however, this was based on a total of 23 fractures in Native Americans, with only six hip fractures (25). Leslie and colleagues described higher age- and sex-adjusted rates of hip and other osteoporotic fractures in Canadian First Nations as compared with other races (26). We also found that the rate of fracture was higher in Native Americans as compared with that in all other ethnic groups. The higher rate of fracture could be due to differences in bone mineral density (BMD) between races: a small subset of the Women’s Health Initiative (WHI) found that BMD at the spine and total body was lower in Native Americans from Arizona as compared with whites, although BMD at the hip was similar between groups (27). In a geographically diverse study of 1,708 Native American women with BMD measured by peripheral dual-energy x-ray absorptiometry or heel ultrasound, BMD was similar in Native Americans and whites across age groups (25). Nonetheless, tribal variation in BMD is likely, and thus it is possible the observed differences in fracture rates are explained by BMD. Alternatively, Native American nursing home residents may have less favorable hip geometry (28), or they may have other fracture risk factors such as falls, alcoholism (29), or diabetes (30) which could explain their higher risk of hip fractures. If there are differences in the quality of the facilities used by Native Americans, such as excess psychotropic medication use, this could also explain the high fracture rates observed in this ethnic group.
Strengths of our study include a very large sample of U.S. nursing home residents from all 50 states with claims data available to ascertain hip fractures. Claims data were linked with the MDS, allowing us to identify subgroups of residents with low rates of fracture, such as residents with very severe cognitive or functional impairment. In addition, the residential history file allows certainty that our sample includes residents that are truly long-stay and not just short-stay rehabilitation or skilled nursing facility residents.
This study also has several potential limitations. First, hip fractures were not confirmed with medical records. Prior studies suggest that Medicare claims data is a valid means to ascertain hip fracture, but it is possible that we have underestimated the incidence of fracture if some nursing home residents with hip fracture were treated palliatively and never admitted to the hospital. Second, we did not include residents enrolled in a managed care Medicare program or residents without Medicare Part D. Approximately 12%–13% of U.S. nursing home residents are enrolled in a managed care plan or are not enrolled in Medicare Part D, and our results may not generalize to these residents. Finally, long-stay residents in countries other than the United States may have more or less functional impairment and risk factors for fracture, and our results may not generalize to other countries.
In conclusion, approximately 8% of hip fractures in the United States occur among long-stay nursing home residents. Despite the seriousness of this problem, there are no guidelines on how to screen for hip fracture risk in the nursing home setting. Our study suggests that the risk of fracture differs according to age, race, duration of institutionalization, and cognitive and functional status. Therefore, we suggest the development of a screening tool that includes these factors and that is both practical and valid in the nursing home setting in an effort to prevent these debilitating fractures.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
This work was funded by grants from the National Institute on Aging (1 R01 AG045441 and 5 P01 AG027296-05).
Supplementary Material
Acknowledgments
These analyses were presented in part as an abstract on May 15, 2015 at the American Geriatrics Society annual meeting in National Harbor, MD.
References
- 1. Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010(29):1–20,24. [PubMed] [Google Scholar]
- 2. Brennan nee Saunders J, Johansen A, Butler J, et al. Place of residence and risk of fracture in older people: a population-based study of over 65-year-olds in Cardiff. Osteoporos Int. 2003;14(6):515–519. [DOI] [PubMed] [Google Scholar]
- 3. Norton R, Campbell AJ, Reid IR, et al. Residential status and risk of hip fracture. Age Ageing. 1999;28(2):135–139. [DOI] [PubMed] [Google Scholar]
- 4. Zimmerman S, Chandler JM, Hawkes W, et al. Effect of fracture on the health care use of nursing home residents. Arch Intern Med. 2002;162(13):1502–1508. [DOI] [PubMed] [Google Scholar]
- 5. Berry SD, Samelson EJ, Bordes M, Broe K, Kiel DP. Survival of aged nursing home residents with hip fracture. J Gerontol A Biol Sci Med Sci. 2009;64(7):771–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baumgarten M, Margolis DJ, Orwig DL, et al. Pressure ulcers in elderly patients with hip fracture across the continuum of care. J Am Geriatr Soc. 2009;57(5):863–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dharmarajan TS, Tankala H, Patel B, Sipalay M, Norkus EP. Outcome in ambulatory status immediately following hip fracture surgery in the acute setting: a comparison of nursing home residents and community older adults. J Am Med Dir Assoc. 2001;2(3):115–119. [PubMed] [Google Scholar]
- 8. Beaupre LA, Jones CA, Johnston DW, Wilson DM, Majumdar SR. Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: prospective cohort study. J Am Geriatr Soc. 2012;60(7):1268–1273. doi:10.1111/j.1532-5415.2012.04033.x [DOI] [PubMed] [Google Scholar]
- 9. Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med. 2014;174(8):1273–1280. doi:10.1001/jamainternmed.2014.2362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chandler JM, Zimmerman SI, Girman CJ, et al. Low bone mineral density and risk of fracture in white female nursing home residents. JAMA. 2000;284(8):972–977. doi:10.1001/jama.284.8.972 [DOI] [PubMed] [Google Scholar]
- 11. Sugarman JR, Connell FA, Hansen A, Helgerson SD, Jessup MC, Lee H. Hip fracture incidence in nursing home residents and community-dwelling older people, Washington State, 1993–1995. J Am Geriatr Soc. 2002;50(10):1638–1643. [DOI] [PubMed] [Google Scholar]
- 12. Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents’ long-term care histories(*). Health Serv Res. 2011;46:120–137. doi:10.1111/j.1475-6773.2010.01194.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ray WA, Griffin MR, Fought RL, Adams ML. Identification of fractures from computerized Medicare files. J Clin Epidemiol. 1992;45(7):703–714. [DOI] [PubMed] [Google Scholar]
- 14. Rigler SK, Ellerbeck E, Whittle J, Mahnken J, Cook-Wiens G, Shireman TI. Comparing methods to identify hip fracture in a nursing home population using Medicare claims. Osteoporos Int. 2011;22(1):57–61. doi:10.1007/s00198-010-1264-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McBean AM. Improving Medicare’s data on race and ethnicity. Medicare Brief. 2006(15):1–7. [PubMed] [Google Scholar]
- 16. Hartmaier SL, Sloane PD, Guess HA, Koch GG, Mitchell CM, Phillips CD. Validation of the Minimum Data Set Cognitive Performance Scale: agreement with the Mini-Mental State Examination. J Gerontol A Biol Sci Med Sci. 1995;50(2):M128–M133. [DOI] [PubMed] [Google Scholar]
- 17. Rothman KJ, GS, Lash TL. (eds.). Modern Epidemiology. 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008:758. [Google Scholar]
- 18. Quigley PA, Campbell RR, Bulat T, Olney RL, Buerhaus P, Needleman J. Incidence and cost of serious fall-related injuries in nursing homes. Clin Nurs Res. 2012;21(1):10–23. doi:10.1177/1054773811414180 [DOI] [PubMed] [Google Scholar]
- 19. Samelson EJ, Zhang Y, Kiel DP, Hannan MT, Felson DT. Effect of birth cohort on risk of hip fracture: age-specific incidence rates in the Framingham Study. Am J Public Health. 2002;92(5):858–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Looker AC, Dawson-Hughes B, Tosteson AN, Johansson H, Kanis JA, Melton LJ., 3rd Hip fracture risk in older US adults by treatment eligibility status based on new National Osteoporosis Foundation guidance. Osteoporos Int. 2011;22(2):541–549. doi:10.1007/s00198-010-1288-0 [DOI] [PubMed] [Google Scholar]
- 21. Leland NE, Gozalo P, Teno J, Mor V. Falls in newly admitted nursing home residents: a national study. J Am Geriatr Soc. 2012;60(5):939–945. doi:10.1111/j.1532-5415.2012.03931.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Capezuti E, Evans L, Strumpf N, Maislin G. Physical restraint use and falls in nursing home residents. J Am Geriatr Soc. 1996;44(6):627–633. [DOI] [PubMed] [Google Scholar]
- 23. Rapp K, Becker C, Cameron ID, et al. Femoral fracture rates in people with and without disability. Age Ageing, 2012;41(5):653–658. doi:10.1093/ageing/afs044 [DOI] [PubMed] [Google Scholar]
- 24. Rapp K, Becker C, Lamb SE, Icks A, Klenk J. Hip fractures in institutionalized elderly people: incidence rates and excess mortality. J Bone Miner Res. 2008;23(11):1825–1831. doi:10.1359/jbmr.080702 [DOI] [PubMed] [Google Scholar]
- 25. Barrett-Connor E, Siris ES, Wehren LE, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20(2):185–194. [DOI] [PubMed] [Google Scholar]
- 26. Leslie WD, Derksen S, Metge C, et al. Fracture risk among First Nations people: a retrospective matched cohort study. CMAJ. 2004;171(8):869–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chen Z. Comparative findings in bone mineral density among postmenopausal Native American women and postmenopausal white women residing in Arizona. Bone. 1998;23:S592. [Google Scholar]
- 28. Leslie WD, Metge CJ, Weiler HA, Doupe M, Wood Steiman P, O’Neil JD. Bone density and bone area in Canadian Aboriginal women: the First Nations Bone Health Study. Osteoporos Int. 2006;17(12):1755–1762. [DOI] [PubMed] [Google Scholar]
- 29. Shield KD, Gmel G, Kehoe-Chan T, Dawson DA, Grant BF, Rehm J. Mortality and potential years of life lost attributable to alcohol consumption by race and sex in the United States in 2005. PLoS One. 2013;8(1):e51923 doi:10.1371/journal.pone.0051923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Will JC, Strauss KF, Mendlein JM, Ballew C, White LL, Peter DG. Diabetes mellitus among Navajo Indians: findings from the Navajo Health and Nutrition Survey. J Nutr. 1997;127(10 suppl):S2106–S2113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.