Abstract
Oxidative stress has been shown to contribute to the development of age-related macular degeneration (AMD). MicroRNAs (miRNA) are small non-coding RNA molecules that function in RNA silencing and post-transcriptional regulation of gene expression. We showed miR-17-3p to be elevated in macular RPE cells from AMD patients and in ARPE-19 cells under oxidative stress. Transfection of miR-17-3p mimic in ARPE-19 induced cell death and exacerbated oxidative lethality that was alleviated by miR-17-3p inhibitor. The expression of antioxidant enzymes manganese superoxide dismutase (MnSOD) and thioredoxin reductase-2 (TrxR2) were suppressed by miR-17-3p mimic and reversed by miR-17-3p inhibitor. These results suggest miR-17-3p aggravates oxidative damage-induced cell death in human RPE cells, while miR-17-3p inhibitor acts as a potential protector against oxidative stress by regulating the expression of antioxidant enzymes.
Introduction
Age-related macular degeneration is the leading cause of irreversible blindness among the elderly in developed countries. Although therapeutic strategies for the less prevalent neovascular form exist, therapies for the more prevalent non-neovascular (“dry”) form are lacking. A better understanding its pathogenesis may guide researchers towards the development of novel therapies. It has been postulated that oxidative stress [1–4] and inflammation [5–13] play a critical role in AMD pathogenesis. Retinal pigment epithelium (RPE) cells are extremely important to photoreceptor function, being responsible for the recycling of the visual pigments and in phagocytosis of photoreceptor outer segments [14,15]. Due to its location in a highly oxygenated and lit environment, RPE is at high risk for oxidative injury that could lead to cellular dysfunction, inflammation, and eventually cell death [2–4,16–20].
There are several enzymes responsible for oxidative stress management, such as superoxide dismutase (SOD) and thioredoxin reductase. Among the three SOD isoforms, MnSOD is the essential mitochondrial antioxidant enzyme. It has been demonstrated that RPE cells deriving from MnSOD-deficient mice are more susceptible to oxidative stress than wild-type RPE cells [21]. Three well characterized isoenzymes of thioredoxin reductases, namely cytosolic TrxR1, mitochondrial TrxR2, and testicular TrxR3 are flavoproteins that reduce thioredoxin, a major protein involved in the reduction of cellular oxidative stress[22,23]. TrxR2 controls H2O2 emission by maintaining the level of active thioredoxin [24], which has been show efficiently decreased RPE cell death caused by oxidative stress [25]. Overall, dysfunction of antioxidant enzymes can cause ROS accumulation, and ROS defense systems have been shown to be important in RPE [26–36]. Consequently, the regulation of antioxidant enzymes is important in the study of AMD, as efficient antioxidant defense systems are needed to protect the RPE cells.
MicroRNAs (miRNAs) are small non-coding RNAs that play an essential role in regulating gene expression, either by degrading messenger RNA (mRNA) or stalling translation [37]. They can be generated from either the 5p or 3p or both arms of pre-miRNA, and depending on which arm they are generated from, they are notated as: miR-#-5p or miR-#-3p [38]. These molecules have been proven to be involved in extensive pathological processes, including angiogenesis, oxidative stress, immune response and inflammation [39–42], all of which are critical processes in age-related macular degeneration (AMD). MicroRNA-30b has previously been shown to impair oxidative stress mechanisms in ARPE-19 [43], whereas miR-9 has been shown to be upregulated by a retinoic acid analogue in the same cells [44]. Using human iPSC-derived RPE cells under Paraquat stress, Garcia et al. showed upregulation of miR-146a and miR-29a, downregulation of miR-144, miR-200a and miR-21, whereas a biphasic response was seen on miR-27b [45]. We previously reported that miR-23 enhances RPE cell resistance to oxidative stress damage and is downregulated in macular RPE cells from AMD patients [46]. miR-17-3p is a member of miR-17/92 cluster, originally found to be involved in tumorigenesis, but more recently, members of this cluster have been shown to be involved in many aging disorders [47]. Although most of the work regarding miR17-3p has focused on regulation of cell proliferation pathways, a study using prostate cancer cell lines demonstrated that miR-17-3p is also involved in regulating antioxidant enzymes [48]. In this study, we aim to explore the role of miR-17-3p in ARPE-19 cell viability and antioxidant enzyme production under oxidative stress, a major factor in AMD pathogenesis.
Materials and Methods
Cell culture
Human donor eyes from AMD patients (70–90 years old) and age-matched controls were acquired from the Minnesota Lions Eye Bank (Saint Paul, MN), in accordance with the provisions of the Declaration of Helsinki for research involving human tissues. Macular RPE cells were isolated as explained previously [49]. Briefly, cornea, anterior segment, vitreous, and neural retina were carefully removed without disturbing the RPE layer. The dissection was performed by an 8-mm sterile trephine punch through the RPE cell layer, Bruch’s membrane, and choroid, centered on the macula. RPE cells from this region were collected as macular RPE cells. Subsequently, the RPE cells were dissociated after trypsin digestion (30 minutes at 37°C) in pre-warmed medium (DMEM/F12; Cat#11330–057, Gibco, Grand Island, NY). Centrifugation of cells for 5 minutes was carried at 168 × g at 4°C. Supernatant was carefully aspirated and the cell pellet was re-suspended in DMEM medium. To guarantee the purity of RPE cells during the isolating procedure, the isolated cells were analyzed morphologically and stained with cytokeratin-18 antibody, which confirmed that the percentage of RPE cells was more than 97%.
Human retinal pigment epithelium and ARPE-19 cells (CRL-2302, ATCC, Manassas, VA) were cultured in medium (DMEM/F-12; Cat#11330–057, Gibco, Grand Island, NY) supplemented with 10% fetal bovine serum (FBS; Cat#10438–026, Gibco, Grand Island, NY) and penicillin-streptomycin (100 U/mL-100μg/ml; Cat#15140, Gibco, Grand Island, NY) at 37°C in a humidified 5% CO2 incubator.
miRNA transfection
ARPE-19 cells were cultured in DMEM/F12 medium to reach 70% confluence, and transfection was performed for functional analysis. miR-17-3p mimic (Cat#4464066, Life technologies), antisense miR-17-3p mimic (inhibitor, Cat#4464084, Life technologies), scrambled mimic (sc-mimic, Cat#4464058, Life technologies), and scrambled inhibitor (sc-inhibitor, Cat#4464076, Life technologies) were transfected into ARPE-19 cells with Lipofectamine® RNAiMAX (Cat#13778030, Invitrogen, Carlsbad, CA) according to the manufacturer’s manual, respectively. The final concentration of miRNAs was 20 nM. Cells were then incubated for 72 h in a humidified incubator with 5% CO2 at 37°C until utilized for experiments.
H2O2 and TBH treatment
ARPE-19 cells were seeded to a density of 3.5 ×105/ml in 6-well plates, and cultured in medium supplemented with 10% fetal bovine serum and penicillin-streptomycin. Twenty-four hours later, cells at 90~100% confluence were exposed to H2O2 (25, 50, 100, or 200μM) (Cat#H-1009, Sigma-Aldrich, St.Louis, MO) and tert-Butyl hydrogen peroxide solution, TBH (Cat#458139, 37.5, 75, or 150μM) (Sigma-Aldrich, St. Louis, MO) diluted in cell culture medium (DMEM/F12; Cat#11330–057, Gibco, Grand Island, NY) without fetal bovine serum or phenol red.
Cell viability assay
Cell viability was determined by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenylt-etrazolium bromide (MTT, Cat#M6494, Molecular Probes, Eugene, OR) assay. Specifically, after the incubation, the cell medium was aspirated from the 96-well plate. Cells were then washed with Dulbecco’s Phosphate Buffer Saline (DPBS; Cat#17-515Q, Lonza, Walkersville, MD) twice and treated with 0.5mg/ml MTT. Following 3 hours of incubation at 37°C, the MTT solution was aspirated and 100μl of hydrochloride-isopropanol (0.04N) (Cat#258148, Cat#109827, Sigma-Aldrich, St. Louis, MO) was added to each well. Plates were incubated for 15 minutes on a shaker and absorbance was read at 590nm using a SpectraMax 190 microplate reader (Molecular Devices, Sunnyvale, CA).
Determination of miR-17-3p expression level
Primary cultured macular RPE or ARPE-19 cells were seeded at 2×105/ well in 6-well plates and incubated to 80% confluence. Primary cultured RPE cells were then harvested at passage 3. Total RNA was extracted from RPE cells (miRNeasy Mini kit; Cat#217004, QIAGEN, Germany). Complementary DNA (cDNA) was synthesized using predesigned TaqMan miRNA Assays (Applied Biosystems, Foster City, CA) and the Reverse Transcription Kit (Cat#4368814, Applied Biosystems, Foster City, CA) for miRNA after total RNA extraction according to the manufacturer’s instructions. Briefly, the reaction contained a volume of 5μl RNA extract, 3μl of reverse transcription (RT) primer, and 7μl master mix. RT reactions were performed on a Thermal cycler (Bio-Rad, Hercules, CA) under the following conditions: 16°C for 30 min, 42° C for 30 min, 85°C for 5 min, and 4°C on hold. All TaqMan assays were run in triplicate on an AB Step One Plus real-time PCR system using TaqMan Universal PCR Master Mix II without UNG (Cat#4440040, Applied Biosystems, Foster City, CA). Real-time PCR cycling conditions consisted of 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60°C for 1 min.
Western blot
Total protein was extracted from cultured ARPE-19 cells using NP40 cell lysis buffer (Cat#FNN0021, Invitrogen, Frederick, MD), and the concentration was calculated by DC protein assay (Cat#500–0016, Bio-Rad, Philadelphia, PA). Equivalent amounts of extracted protein were loaded into each well and electrophoresed on a Nupage 4–12% Bis-Tris gel (Cat#NP0335BOX, Novex, Carlsbad, CA), then transferred to a 0.2μm PVDF membrane (Cat#ISEQ00010, Millipore, Billerica, MA), blocked with non-fat dry milk (Cat#9999, Cell signaling, Danvers, MA) and incubated with primary antibodies against MnSOD (Cat#16956, Abcam, Cambridge, MA) at 1:2000, TrxR2 (Cat#sc-46278, Santa Cruz Biotechnology, Dallas, TX) at 1:250, and GAPDH (Cat#5174, Cell Signaling Technology, Danvers, MA) at 1:1000, for 2 hours. The membrane was washed 3 times for 10 minutes each time and incubated with secondary antibodies at 1:10000 for 1.5 hours. After washing, membranes were incubated with the chemiluminescent substrate (Cat#RPN2235, ECL Select western blotting detection reagents, GE Healthcare Life Sciences, Piscataway, NJ) for 5 minutes. Band signals were detected by an image-scanning densitometer (ChemiDoc imaging system; Bio-Rad) and quantitated by Image J 2.0.
TUNEL (terminal deoxynucleotidyl transferase-mediated dUTP nick-end labelling) staining
ARPE-19 cells were washed with PBS once and then fixed in 4% paraformaldehyde in PBS for 10 min at room temperature (25°C). After two washes in PBS for 5 minutes each, cells were post-fixed in cooled ethanol-acetic acid (v:v, 2:1) and stained using an In Situ Apoptosis Detection Kit (Cat#S7110, Millipore, Temecula, CA) according to the manufacturer’s protocol. The cell nuclei were counterstained with DAPI (4’, 6-diamidino-2-phenylindole, Cat#62248, Life technologies). The number of TUNEL-positive cells was counted and processed for statistical analysis.
Statistical analysis
Statistical analysis was performed on GraphPad Prism 7.0a. Statistically significant differences between two groups were assessed using Student’s t-test. One-way ANOVA followed by Tukey’s post-hoc test was applied to multiple group comparisons. Differences with p<0.05 were considered statistically significant.
Results
miR-17-3p expression increases in macular RPE cells from AMD patients
A microarray assay previously performed by our group showed that miR-17-3p expression level increases in macular RPE cells of AMD patients’ donor eyes compared to age-matched normal control donor eyes. To confirm this data, total RNA was isolated from macular RPE cells of each AMD donor eye (n = 5) and age-matched normal control eye (n = 5). miR-17-3p expression level was analyzed by qRT-PCR. Fig 1 illustrates that miR-17-3p was significantly upregulated (p<0.05) in macular RPE cells from AMD donor eyes compared to controls (1.4-fold). It suggests that increased miR-17-3p expression may be associated with AMD.
Fig 1. Differential miR-17-3p expression in macular RPE cells from AMD patients and normal controls.

Expression levels of miR-17-3p in macular RPE cells from AMD and age-matched normal control donor eyes were analyzed by qRT-PCR. The expression levels are shown relative to control values in five independent experiments. Results are displayed as mean ± SD. *p<0.05.
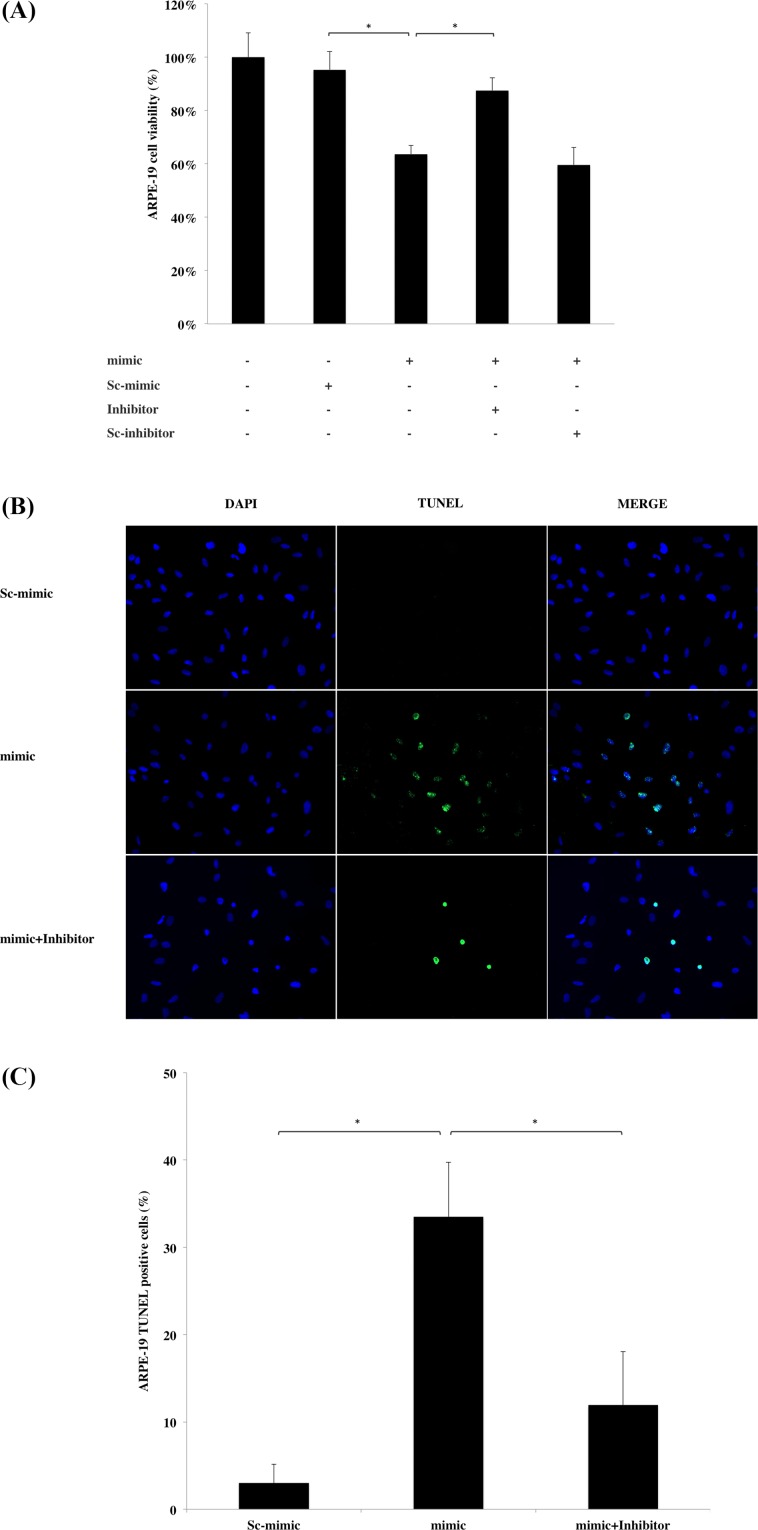
miR-17-3p causes ARPE-19 cell death
Due to the fact that miR-17-3p was upregulated in macular RPE cells from AMD patients, we hypothesized that it may be implicated in AMD pathogenesis. Since RPE cell atrophy and death are features of AMD, we assessed cell viability by MTT assay following miR-17-3p transfection into ARPE-19 cells. miR-17-3p mimic sequence transfection caused significant reduction in cell viability (63.7%) compared to scrambled sequence (95.4%), and this effect was partially reversed by co-transfection with miR-17-3p-specific inhibitor (87.5%), but not a scrambled inhibitor (Fig 2A). Moreover, the ratio of TUNEL-positive cells/total cells in the miR-17-3p transfected group was 30.5% higher compared to the scrambled sequence group, while co-transfection with the inhibitor abrogated miR-17-3p cell death (Fig 2B and 2C). These results indicate that miR-17-3p induces ARPE-19 cell death.
Fig 2. Effect of miR-17-3p on ARPE-19 cell viability.
(A) ARPE-19 cells were transfected with miR-17-3p mimic (mimic), scrambled miR-17-3p mimic (sc-mimic), miR-17-3p antisense (inhibitor) or scrambled miR-17-3p antisense (sc-inhibitor) as indicated for 72 hours. Cell viability was assessed by MTT assay. The mimic sequence transfection reduced cell viability compared to scrambled sequence (sc-mimic); however, decreased cell viability was reversed by co-transfection with miR-17-3p inhibitor. Data shown as mean ± SD. (n = 8) (B) After 72 hours of transfection, cell death was evaluated by TUNEL staining. Representative images were chosen from three independent experiments. (C) The average number of TUNEL positive cells from different transfection groups was counted from six random microscope fields. Results are displayed as mean ± SD. *p<0.05.
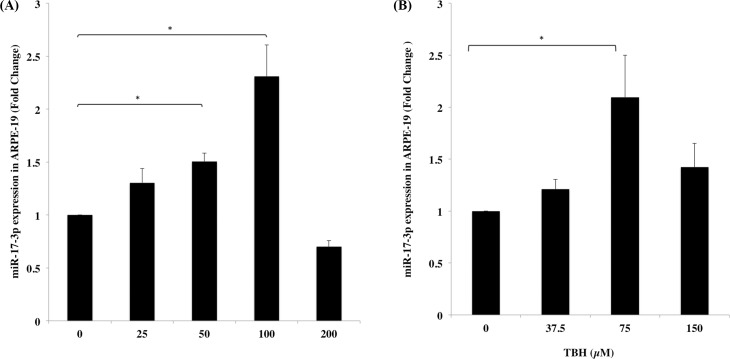
Increased expression of miR-17-3p in ARPE-19 under oxidative stress
Since oxidative stress has been linked to RPE senescence and AMD [50], we sought to evaluate miR-17-3p expression in RPE cells under oxidative stress. It was found that miR-17-3p was raised 1.3-, 1.5- and 2.3-fold in ARPE-19 cells after treatment with increasing concentrations of H2O2 (25, 50, 100μM) compared with the untreated control respectively (Fig 3A). Meanwhile, treatment with a similar oxidant stimulus, TBH, exhibited an analogous increase of miR-17-3p expression ranging from 1.2- to 2-fold compared with the untreated control (Fig 3B). However, doses higher than 100μM of H2O2 and 75μM of TBH failed to increase miR-17-3p expression, most likely due to cytotoxicity. These results indicate that miR-17-3p can be up regulated in ARPE-19 cells in the presence of oxidizing stimuli.
Fig 3. Expression of miR-17-3p in ARPE-19 cells under increasing amounts of oxidative stress.
ARPE-19 cells were treated with different concentrations of H2O2 (0, 25, 50, 100, 200μM) or TBH (0, 37.5, 75, 150μM) for 6 hours. miR-17-3p expression levels were determined by qRT-PCR in both H2O2 (A) and TBH (B) treated group. Results are displayed as mean ± SD. *p<0.05.
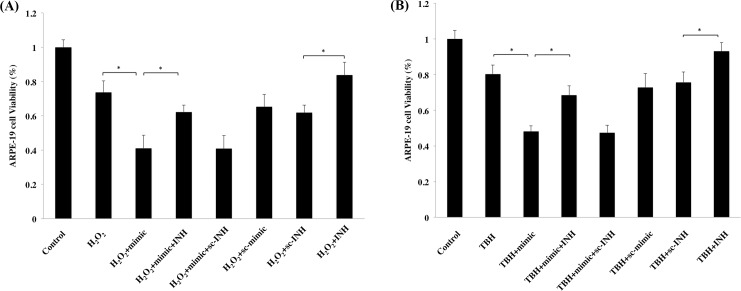
miR-17-3p increases vulnerability of RPE cells to oxidative stress
Since miR-17-3p was shown to cause cell death in ARPE-19 cells, and its expression was upregulated under oxidative stress, we speculated that miR-17-3p could potentially augment RPE cell death under oxidative stress. ARPE-19 cells were differentially transfected with miR-17-3p (mimic) or co-transfected with miR-17-3p antisense (inhibitor) for 72 hours, and then treated with H2O2 (100μM) or TBH (75μM) for 9 hours. Cell viability was assessed by MTT assay, which showed that cell death increased to 26.3% and 19.6% after H2O2 and TBH treatment, respectively, compared with the untreated group. Transfection with miR-17-3p mimic further increased this value to 58.9% and 51.8%, respectively (Fig 4A and 4B), whereas transfection with miR-17-3p inhibitor but not scrambled inhibitor was able to reverse H2O2 and TBH toxicity (37.7% and 31.5% of cell death by co-transfection with inhibitor in the H2O2 and TBH treated groups, respectively). Moreover, transfection with miR-17-3p antisense (INH) alone but not scrambled inhibitor (sc-INH) alone was able to partially reverse H2O2 or TBH toxicity (Fig 4). These data suggest that miR-17-3p can increase ARPE-19 cell vulnerability to oxidative stress and miR-17-3p antisense plays a protective role under oxidative stress.
Fig 4. miR-17-3p increases vulnerability of RPE cells to oxidative stress.
ARPE-19 cells were transfected with miR-17-3p (mimic) or miR-17-3p antisense (inhibitor, INH) as indicated for 72 hours, and then treated with (A) H2O2 (100μM) or (B) TBH (75μM) for 9 hours. Cell viability was then determined by MTT assay. Data are shown as mean ± SD. (n = 8) *p<0.05.
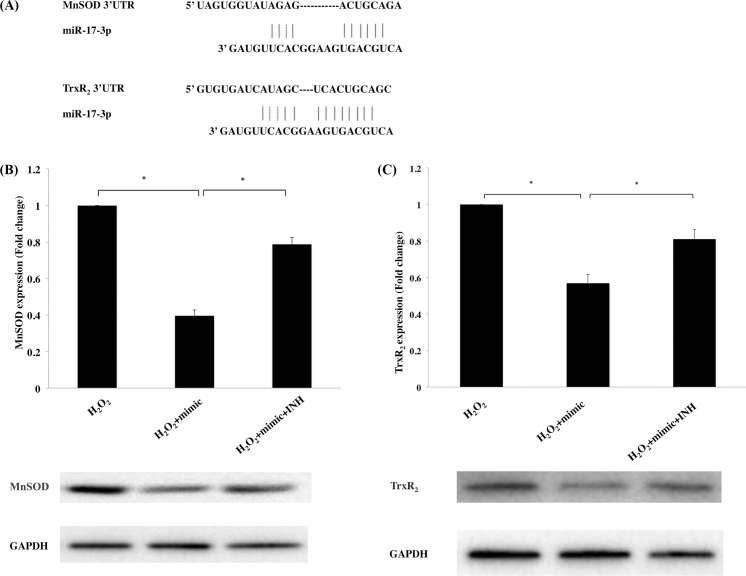
miR-17-3p reduced the expression of MnSOD and TxR2 in ARPE-19 cells under oxidative stress
To explore the potential targets of miR-17-3p, which are responsible for the increased vulnerability under oxidative stress, we performed a bioinformatics sequence analysis and found that two antioxidant enzymes, MnSOD and TrxR2, possess binding sites of miR-17-3p at the 3’untranslated regions (3’ UTR) of mRNA (Fig 5A), which is validated by Xu et al. using luciferase assay [48]. miR-17-3p mimic transfection reduced MnSOD and TrxR2 protein expression levels to 39.6% and 56.9% respectively compared to a transfection control. Furthermore, antisense-miR-17-3p was able to reverse MnSOD and TrxR2 downregulations to 78.7% and 81.0%, respectively (Fig 5B and 5C). Collectively, these results demonstrate that miR-17-3p is a negative regulator of two important antioxidant enzymes in ARPE-19 cells.
Fig 5. Effect of miR-17-3p on MnSOD and TrxR2 expression levels under oxidative stress in ARPE-19 cells.
(A) Prediction of the interaction between miR-17-3p and MnSOD/TrxR2 mRNA 3’ UTR. ARPE-19 cells were transfected with mimic or inhibitor (INH) for 72 hours and then treated with H2O2 (100μM) for 6 hours. MnSOD (B) and TrxR2 (C) protein expression were assessed by Western blot analysis. Data are shown the mean ± SD from 3 independent experiments. *p<0.05
Discussion
Our study provides evidence that miR-17-3p is elevated in macular RPE cells of AMD patients and is cytotoxic to ARPE-19 cells. This cytotoxic effect can be partially reversed by the inhibitor of miR-17-3p. Furthermore, the expression level of miR-17-3p increases under oxidative stress, and it increases ARPE-19 vulnerability to oxidative stress by downregulating the mitochondrial antioxidant enzymes MnSOD and TrxR2. This effect can be abolished by the inhibitor of miR-17-3p.
There are only a few studies examining the role of miRNA in dry AMD. Our 2011 study [46] was the first to show that miR-23 is downregulated in human AMD eyes and its putative protective effect is mediated by downregulation of the Fas ligand. A year later, Lukiw et al. [51] showed that several miRNAs, including miRNA-9, miRNA-125b, miRNA-146a and miRNA-155, were upregulated in both Alzheimer’s disease and AMD, and they were common to the pathogenetic mechanism of complement factor H (CFH) deficiency which drives inflammatory neurodegeneration. In 2014, Murad et al. [52] reported that miR-184 was significantly downregulated in primary RPE cells isolated from AMD donors, and its downregulation resulted in impaired autophagy and dysfunction of the RPE. More recently, Szemraj et al. [53] showed that there is an altered serum profile of miRNA in wet versus dry AMD patients, suggesting a potential role for miRNAs as novel biomarkers. Our current study shows that miR-17-3p not only is upregulated in the RPE cells of AMD patients, but it also increases vulnerability to oxidative stress in vitro and causes ARPE-19 death itself, suggesting that miR-17-3p may be contributing to the reduced RPE viability caused by oxidative stress in AMD patients.
RPE degeneration in AMD has been strongly linked to oxidative stress [54]. Oxidative stress can be induced by exposing of cells to oxidant generators, such as H2O2 or TBH. H2O2, one of the major free radicals and a precursor of highly oxidizing, tissue-damaging radicals, has been known to cause RPE damage and cell death [55]. Moreover, H2O2 triggers changes in the expression of multiple genes, which are involved in ROS-mediated RPE cell death and apoptosis [46,55,56]. TBH is a short-chain organic hydro peroxide, also used as an oxidant for investigating mechanisms of cellular alterations resulting from oxidative stress in cells and tissues, such as the RPE [57]. We found that miR-17-3p was elevated in ARPE-19 cells after treatment with increasing concentrations of oxidizing reagents H2O2 and TBH. Multiple oxidation-sensitive genes and factors are induced in RPE cells exposed to ROS [58,59]. Alterations in gene expression in response to oxidative stress have been extensively studied at transcriptional levels [60,61], however it is accepted that post-transcriptional regulation of gene expression is also very important [62]. MicroRNAs serve as significant post-transcriptional regulators of gene expression.
Evidence stemming from prior studies in prostate cancer cells as well as from our bioinformatic analysis suggests that antioxidant enzymes MnSOD and TrxR2 act as targets of miR-17-3p [48]. MnSOD, a ROS scavenger, plays a vital role in promoting cell survival under stressful conditions, and several studies have confirmed that the decrease in cell viability observed under oxidative stress is correlated with MnSOD downregulation [21,63]. Moreover, some exogenous antioxidants, such as estrogen and progesterone, exhibit their antioxidant function by increasing the expression of mitochondrial-localized gene products, such as MnSOD and Bcl-2, which display antioxidant activities [64–66]. Verline et al. found that MnSOD knockdown in mice leads to oxidative damage of RPE cells, and more importantly, the appearance of certain key features of AMD [67]. The mitochondrial enzyme TrxR2 preserves thioredoxin in a reduced state, thereby playing a key role in maintaining the cellular redox environment [68]. Inhibition of TrxR2 in mitochondria isolated from guinea pigs, as well as in mouse cardiomyocytes, resulted in increased H2O2 production [24]. This correlates with our findings, as cell viability was reduced with miR-17-3p mimic transfection under oxidative stress, in parallel with MnSOD and TrxR2 downregulation.
Due to increased miR-17-3p levels in AMD eyes in combination with the fact that miR-17-3p can specifically downregulate MnSOD and TrxR2 expression, its role as a mediator for RPE susceptibility to oxidative stress in AMD should not be overlooked. Interestingly, another recent study by Haque et al. [43] showed that in ARPE-19 cells, a sublethal dose of H2O2 upregulated miR-30b, which inhibited catalase, another anti-oxidant enzyme. Furthermore, a miR-30b antagonist protected RPE cells from oxidative stress, concurring with our findings after using miR-17-3p.
miR-17-3p is a member of miR-17/92 cluster which is extensively studied in tumorigenesis [69]. Most of the work on miR17-3p has thus been focused on studying the regulation of cell proliferation pathways. More recently though, studies have shown more varied effects of miR-17-3p, such as involvement in development and spinal progenitor cells [70], induction by TNF alpha and LPS in HeLa cells [71], downregulating flk-1 in endothelial cells [72], suppressing epithelial to mesenchymal transformation of ovarian epithelial cells [73], inhibiting fibroblast senescence [74] and being downregulated in the plasma of Alzheimer patients [75]. More relevant to our work, it has been shown that miR-17-3p downregulates important anti-oxidant enzymes, such as manganese superoxide dismutase, glutathione peroxidase-2 and thioredoxin reductase-2 (TrxR2) in prostate cancer cell lines [48] and blood mononuclear cells [76]. To confirm the previous studies, our bioinformatic sequence analysis found that there is a putative binding site for the miR-17-3p in the mRNA 3’untranslated regions of MnSOD and TrxR2 (Fig 5A) that is verified by in vitro experiments (Fig 5B and 5C). The mechanism by which oxidative stress regulates miR-17-3p levels remains elusive. It is interesting to note that downregulation of c-Myc suppresses pri-miR-17/92 cluster expression [77] and that c-Myc is downregulated by peroxiredoxin 1, which is involved under oxidative stress [78]. Although this mechanism has not been studied in RPE cells or in AMD, it is a promising target for future investigation.
In conclusion, this study demonstrates increased miR-17-3p expression in human AMD eyes. It also shows that miR-17-3p expression is increased by oxidative stimuli and that it has detrimental effects on RPE antioxidant defense mechanisms by downregulating the anti-oxidant enzymes MnSOD and TrxR2. Therefore, inhibition of miR-17-3p could be a novel therapeutic approach to protect RPE cells from oxidative stress.
Acknowledgments
This work was supported by: NEI R21EY023079-01A1 (DGV); the Yeatts Family Foundation (DGV, JWM); the Loefflers Family Fund (DGV, JWM); the 2013 Macula Society Research Grant award (DGV); a Physician Scientist Award (DGV), an unrestricted grant (JWM) from the research to prevent blindness foundation; NEI grant EY014104 (Meei Core Grant); and Bayer Healthcare Global Ophthalmology Award (DEM). The authors would like to thank Kassandra Kosmidou for proofreading this manuscript.
Data Availability
Data are available from Dryad in the following temporary url: http://datadryad.org/review?doi=doi:10.5061/dryad.cf860
Funding Statement
This work was supported by: NEI R21EY023079-01A1 (DGV); the Yeatts Family Foundation (DGV, JWM); the Loefflers Family Fund (DGV, JWM); the 2013 Macula Society Research Grant award (DGV); a Physician Scientist Award (DGV), an unrestricted grant (JWM) from the research to prevent blindness foundation; NEI grant EY014104 (Meei Core Grant); and Bayer Healthcare Global Ophthalmology Award (DEM). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Solberg Y, Rosner M, Belkin M. The association between cigarette smoking and ocular diseases. Surv Ophthalmol n.d.;42:535–47. [DOI] [PubMed] [Google Scholar]
- 2.Hollyfield JG, Bonilha VL, Rayborn ME, Yang X, Shadrach KG, Lu L, et al. Oxidative damage-induced inflammation initiates age-related macular degeneration. Nat Med 2008;14:194–8. 10.1038/nm1709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollyfield JG. Age-related macular degeneration: the molecular link between oxidative damage, tissue-specific inflammation and outer retinal disease: the Proctor lecture. Invest Ophthalmol Vis Sci 2010;51:1275–81. 10.1167/iovs.09-4478 [DOI] [PubMed] [Google Scholar]
- 4.Beatty S, Koh H-H, Phil M, Henson D, Boulton M. The Role of Oxidative Stress in the Pathogenesis of Age-Related Macular Degeneration. Surv Ophthalmol 2000;45:115–34. 10.1016/S0039-6257(00)00140-5 [DOI] [PubMed] [Google Scholar]
- 5.Whitmore SS, Sohn EH, Chirco KR, Drack A V, Stone EM, Tucker BA, et al. Complement activation and choriocapillaris loss in early AMD: implications for pathophysiology and therapy. Prog Retin Eye Res 2015;45:1–29. 10.1016/j.preteyeres.2014.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klein RJ, Zeiss C, Chew EY, Tsai J-Y, Sackler RS, Haynes C, et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005;308:385–9. 10.1126/science.1109557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hageman GS, Anderson DH, Johnson L V, Hancox LS, Taiber AJ, Hardisty LI, et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci U S A 2005;102:7227–32. 10.1073/pnas.0501536102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson L V, Leitner WP, Rivest AJ, Staples MK, Radeke MJ, Anderson DH. The Alzheimer’s A beta -peptide is deposited at sites of complement activation in pathologic deposits associated with aging and age-related macular degeneration. Proc Natl Acad Sci U S A 2002;99:11830–5. 10.1073/pnas.192203399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang JCC, Cao S, Wang A, To E, Law G, Gao J, et al. CFH Y402H polymorphism is associated with elevated vitreal GM-CSF and choroidal macrophages in the postmortem human eye. Mol Vis 2015;21:264–72. [PMC free article] [PubMed] [Google Scholar]
- 10.Lad EM, Cousins SW, Van Arnam JS, Proia AD. Abundance of infiltrating CD163+ cells in the retina of postmortem eyes with dry and neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2015;253:1941–5. 10.1007/s00417-015-3094-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ambati J, Atkinson JP, Gelfand BD. Immunology of age-related macular degeneration. Nat Rev Immunol 2013;13:438–51. 10.1038/nri3459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Penfold PL, Madigan MC, Gillies MC, Provis JM. Immunological and aetiological aspects of macular degeneration. Prog Retin Eye Res 2001;20:385–414. [DOI] [PubMed] [Google Scholar]
- 13.Dib B, Lin H, Maidana DE, Tian B, Miller JB, Bouzika P, et al. Mitochondrial DNA has a pro-inflammatory role in AMD. Biochim Biophys Acta—Mol Cell Res 2015;1853:2897–906. 10.1016/j.bbamcr.2015.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kevany BM, Palczewski K. Phagocytosis of retinal rod and cone photoreceptors. Physiology (Bethesda) 2010;25:8–15. 10.1152/physiol.00038.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun M, Finnemann SC, Febbraio M, Shan L, Annangudi SP, Podrez EA, et al. Light-induced oxidation of photoreceptor outer segment phospholipids generates ligands for CD36-mediated phagocytosis by retinal pigment epithelium: a potential mechanism for modulating outer segment phagocytosis under oxidant stress conditions. J Biol Chem 2006;281:4222–30. 10.1074/jbc.M509769200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brunk UT, Wihlmark U, Wrigstad A, Roberg K, Nilsson SE. Accumulation of lipofuscin within retinal pigment epithelial cells results in enhanced sensitivity to photo-oxidation. Gerontology 1995;41 Suppl 2:201–12. [DOI] [PubMed] [Google Scholar]
- 17.Becquet F, Goureau O, Soubrane G, Coscas G, Courtois Y, Hicks D. Superoxide inhibits proliferation and phagocytic internalization of photoreceptor outer segments by bovine retinal pigment epithelium in vitro. Exp Cell Res 1994;212:374–82. 10.1006/excr.1994.1157 [DOI] [PubMed] [Google Scholar]
- 18.Dorey CK, Delori FC, Akeo K. Growth of cultured RPE and endothelial cells is inhibited by blue light but not green or red light. Curr Eye Res 1990;9:549–59. [DOI] [PubMed] [Google Scholar]
- 19.He Y, Ge J, Burke JM, Myers RL, Dong ZZ, Tombran-Tink J. Mitochondria impairment correlates with increased sensitivity of aging RPE cells to oxidative stress. J Ocul Biol Dis Infor 2010;3:92–108. 10.1007/s12177-011-9061-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dong A, Xie B, Shen J, Yoshida T, Yokoi K, Hackett SF, et al. Oxidative stress promotes ocular neovascularization. J Cell Physiol 2009;219:544–52. 10.1002/jcp.21698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasahara E, Lin L-R, Ho Y-S, Reddy VN. SOD2 protects against oxidation-induced apoptosis in mouse retinal pigment epithelium: implications for age-related macular degeneration. Invest Ophthalmol Vis Sci 2005;46:3426–34. 10.1167/iovs.05-0344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flores LC, Ortiz M, Dube S, Hubbard GB, Lee S, Salmon A, et al. Thioredoxin, oxidative stress, cancer and aging. Longev Heal 2012;1:4 10.1186/2046-2395-1-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nishinaka Y, Masutani H, Nakamura H, Yodoi J. Regulatory roles of thioredoxin in oxidative stress-induced cellular responses. Redox Rep 2001;6:289–95. 10.1179/135100001101536427 [DOI] [PubMed] [Google Scholar]
- 24.Stanley BA, Sivakumaran V, Shi S, McDonald I, Lloyd D, Watson WH, et al. Thioredoxin reductase-2 is essential for keeping low levels of H(2)O(2) emission from isolated heart mitochondria. J Biol Chem 2011;286:33669–77. 10.1074/jbc.M111.284612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sugano E, Isago H, Murayama N, Tamai M, Tomita H. Different Anti-Oxidant Effects of Thioredoxin 1 and Thioredoxin 2 in Retinal Epithelial Cells. CELL Struct Funct 2013;38:81–8. [DOI] [PubMed] [Google Scholar]
- 26.Akeo K, Curran SA, Dorey CK. Superoxide dismutase activity and growth of retinal pigment epithelial cells are suppressed by 20% oxygen in vitro. Curr Eye Res 1988;7:961–7. [DOI] [PubMed] [Google Scholar]
- 27.Dorey CK, Khouri GG, Syniuta LA, Curran SA, Weiter JJ. Superoxide production by porcine retinal pigment epithelium in vitro. Invest Ophthalmol Vis Sci 1989;30:1047–54. [PubMed] [Google Scholar]
- 28.Newsome DA, Dobard EP, Liles MR, Oliver PD. Human retinal pigment epithelium contains two distinct species of superoxide dismutase. Invest Ophthalmol Vis Sci 1990;31:2508–13. [PubMed] [Google Scholar]
- 29.Del Vecchio PJ, Shaffer JB. Regulation of antioxidant enzyme expression in LPS-treated bovine retinal pigment epithelial and corneal endothelial cells. Curr Eye Res 1991;10:919–25. [DOI] [PubMed] [Google Scholar]
- 30.Oliver PD, Newsome DA. Mitochondrial superoxide dismutase in mature and developing human retinal pigment epithelium. Invest Ophthalmol Vis Sci 1992;33:1909–18. [PubMed] [Google Scholar]
- 31.Wang M, Lam TT, Fu J, Tso MO. TEMPOL, a superoxide dismutase mimic, ameliorates light-induced retinal degeneration. Res Commun Mol Pathol Pharmacol 1995;89:291–305. [PubMed] [Google Scholar]
- 32.Tanito M, Masutani H, Kim Y-C, Nishikawa M, Ohira A, Yodoi J. Sulforaphane induces thioredoxin through the antioxidant-responsive element and attenuates retinal light damage in mice. Invest Ophthalmol Vis Sci 2005;46:979–87. 10.1167/iovs.04-1120 [DOI] [PubMed] [Google Scholar]
- 33.Yokoyama T, Yamane K, Minamoto A, Tsukamoto H, Yamashita H, Izumi S, et al. High glucose concentration induces elevated expression of anti-oxidant and proteolytic enzymes in cultured human retinal pigment epithelial cells. Exp Eye Res 2006;83:602–9. 10.1016/j.exer.2006.02.016 [DOI] [PubMed] [Google Scholar]
- 34.Sugano E, Isago H, Murayama N, Tamai M, Tomita H. Different anti-oxidant effects of thioredoxin 1 and thioredoxin 2 in retinal epithelial cells. Cell Struct Funct 2013;38:81–8. [DOI] [PubMed] [Google Scholar]
- 35.Sugano E, Murayama N, Takahashi M, Tabata K, Tamai M, Tomita H. Essential role of thioredoxin 2 in mitigating oxidative stress in retinal epithelial cells. J Ophthalmol 2013;2013:185825 10.1155/2013/185825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kasahara E, Lin L-R, Ho Y-S, Reddy VN. SOD2 protects against oxidation-induced apoptosis in mouse retinal pigment epithelium: implications for age-related macular degeneration. Invest Ophthalmol Vis Sci 2005;46:3426–34. 10.1167/iovs.05-0344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu L, Fan J, Belasco JG. MicroRNAs direct rapid deadenylation of mRNA. Proc Natl Acad Sci U S A 2006;103:4034–9. 10.1073/pnas.0510928103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guo L, Yu J, Yu H, Zhao Y, Chen S, Xu C, et al. Evolutionary and Expression Analysis of miR-#-5p and miR-#-3p at the miRNAs/isomiRs Levels. Biomed Res Int 2015;2015 10.1155/2015/168358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Raisch J, Darfeuille-Michaud A, Nguyen HTT. Role of microRNAs in the immune system, inflammation and cancer. World J Gastroenterol 2013;19:2985–96. 10.3748/wjg.v19.i20.2985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yildirim SS, Akman D, Catalucci D, Turan B. Relationship between downregulation of miRNAs and increase of oxidative stress in the development of diabetic cardiac dysfunction: junctin as a target protein of miR-1. Cell Biochem Biophys 2013;67:1397–408. 10.1007/s12013-013-9672-y [DOI] [PubMed] [Google Scholar]
- 41.Suárez Y, Sessa WC. MicroRNAs as novel regulators of angiogenesis. Circ Res 2009;104:442–54. 10.1161/CIRCRESAHA.108.191270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li Q-J, Chau J, Ebert PJR, Sylvester G, Min H, Liu G, et al. miR-181a is an intrinsic modulator of T cell sensitivity and selection. Cell 2007;129:147–61. 10.1016/j.cell.2007.03.008 [DOI] [PubMed] [Google Scholar]
- 43.Haque R, Chun E, Howell JC, Sengupta T, Chen D, Kim H. MicroRNA-30b-mediated regulation of catalase expression in human ARPE-19 cells. PLoS One 2012;7:e42542 10.1371/journal.pone.0042542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kutty RK, Samuel W, Jaworski C, Duncan T, Nagineni CN, Raghavachari N, et al. MicroRNA expression in human retinal pigment epithelial (ARPE-19) cells: increased expression of microRNA-9 by N-(4-hydroxyphenyl)retinamide. Mol Vis 2010;16:1475–86. [PMC free article] [PubMed] [Google Scholar]
- 45.Garcia TY, Gutierrez M, Reynolds J, Lamba DA. Modeling the Dynamic AMD-Associated Chronic Oxidative Stress Changes in Human ESC and iPSC-Derived RPE Cells. Invest Ophthalmol Vis Sci 2015;56:7480–8. 10.1167/iovs.15-17251 [DOI] [PubMed] [Google Scholar]
- 46.Lin H, Qian J, Castillo AC, Long B, Keyes KT, Chen G, et al. Effect of miR-23 on Oxidant-Induced Injury in Human Retinal Pigment Epithelial Cells. Invest Ophthalmol Vis Sci 2011;52:6308–14. 10.1167/iovs.10-6632 [DOI] [PubMed] [Google Scholar]
- 47.Mogilyansky E, Rigoutsos I. The miR-17/92 cluster: a comprehensive update on its genomics, genetics, functions and increasingly important and numerous roles in health and disease. Cell Death Differ 2013;20:1603–14. 10.1038/cdd.2013.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu Y, Fang F, Zhang J, Josson S, Clair WHS, Clair DKS. Mir-17* suppresses tumorigenicity of prostate cancer by inhibiting mitochondrial antioxidant enzymes. PLoS One 2010;5:1–8. 10.1371/journal.pone.0014356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lin H, Xu H, Liang F-Q, Liang H, Gupta P, Havey AN, et al. Mitochondrial DNA damage and repair in RPE associated with aging and age-related macular degeneration. Invest Ophthalmol Vis Sci 2011;52:3521–9. 10.1167/iovs.10-6163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marazita MC, Dugour A, Marquioni-Ramella MD, Figueroa JM, Suburo AM. Oxidative stress-induced premature senescence dysregulates VEGF and CFH expression in retinal pigment epithelial cells: Implications for Age-related Macular Degeneration. Redox Biol 2016;7:78–87. 10.1016/j.redox.2015.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lukiw WJ, Surjyadipta B, Dua P, Alexandrov PN. Common micro RNAs (miRNAs) target complement factor H (CFH) regulation in Alzheimer’s disease (AD) and in agerelated macular degeneration (AMD). Int J Biochem Mol Biol 2012;3:105–16. [PMC free article] [PubMed] [Google Scholar]
- 52.Murad N, Kokkinaki M, Gunawardena N, Gunawan MS, Hathout Y, Janczura KJ, et al. miR-184 regulates ezrin, LAMP-1 expression, affects phagocytosis in human retinal pigment epithelium and is downregulated in age-related macular degeneration. FEBS J 2014;281:5251–64. 10.1111/febs.13066 [DOI] [PubMed] [Google Scholar]
- 53.Szemraj J. Serum MicroRNAs as Potential Biomarkers of AMD. Med Sci Monit 2015;21:2734–42. 10.12659/MSM.893697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blasiak J, Petrovski G, Veréb Z, Facskó A, Kaarniranta K. Oxidative stress, hypoxia, and autophagy in the neovascular processes of age-related macular degeneration. Biomed Res Int 2014;2014:768026 10.1155/2014/768026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim M-H, Chung J, Yang J, Chung S-M, Kwag N-H, Yoo J-S. Hydrogen peroxide-induced cell death in a human retinal pigment epithelial cell line, ARPE-19. Korean J Ophthalmol 2003;17:19–28. 10.3341/kjo.2003.17.1.19 [DOI] [PubMed] [Google Scholar]
- 56.Lu L, Hackett SF, Mincey A, Lai H, Campochiaro PA. Effects of different types of oxidative stress in RPE cells. J Cell Physiol 2006;206:119–25. 10.1002/jcp.20439 [DOI] [PubMed] [Google Scholar]
- 57.Kučera O, Endlicher R, Roušar T, Lotková H, Garnol T, Drahota Z, et al. The Effect of tert-Butyl Hydroperoxide-Induced Oxidative Stress on Lean and Steatotic Rat Hepatocytes In Vitro. Oxid Med Cell Longev 2014;2014:1–12. 10.1155/2014/752506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weigel AL, Ida H, Boylan SA, Hjelmeland LM. Acute hyperoxia-induced transcriptional response in the mouse RPE/choroid. Free Radic Biol Med 2003;35:465–74. 10.1016/S0891-5849(03)00320-4 [DOI] [PubMed] [Google Scholar]
- 59.Alizadeh M, Wada M, Gelfman CM, Handa JT, Hjelmeland LM. Downregulation of Differentiation Specific Gene Expression by Oxidative Stress in ARPE-19 Cells. Invest Ophthalmol Vis Sci 2001;42:2706–13. [PubMed] [Google Scholar]
- 60.Weigel AL, Handa JT, Hjelmeland LM. Microarray analysis of H2O2-, HNE-, or tBH-treated ARPE-19 cells. Free Radic Biol Med 2002;33:1419–32. 10.1016/S0891-5849(02)01082-1 [DOI] [PubMed] [Google Scholar]
- 61.Vandenbroucke K, Robbens S, Vandepoele K, Inzé D, Van de Peer Y, Van Breusegem F. Hydrogen peroxide-induced gene expression across kingdoms: a comparative analysis. Mol Biol Evol 2008;25:507–16. 10.1093/molbev/msm276 [DOI] [PubMed] [Google Scholar]
- 62.Halbeisen RE, Galgano A, Scherrer T, Gerber AP. Post-transcriptional gene regulation: from genome-wide studies to principles. Cell Mol Life Sci 2008;65:798–813. 10.1007/s00018-007-7447-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fukui M, Zhu BT. Mitochondrial superoxide dismutase SOD2, but not cytosolic SOD1, plays a critical role in protection against glutamate-induced oxidative stress and cell death in HT22 neuronal cells. Free Radic Biol Med 2010;48:821–30. 10.1016/j.freeradbiomed.2009.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matsuoka A, Kizuka F, Lee L, Tamura I, Taniguchi K, Asada H, et al. Progesterone increases manganese superoxide dismutase expression via a cAMP-dependent signaling mediated by noncanonical Wnt5a pathway in human endometrial stromal cells. J Clin Endocrinol Metab 2010;95:E291–9. 10.1210/jc.2010-0619 [DOI] [PubMed] [Google Scholar]
- 65.Tripanichkul W, Sripanichkulchai K, Duce JA, Finkelstein DI. 17Beta-estradiol reduces nitrotyrosine immunoreactivity and increases SOD1 and SOD2 immunoreactivity in nigral neurons in male mice following MPTP insult. Brain Res 2007;1164:24–31. 10.1016/j.brainres.2007.05.076 [DOI] [PubMed] [Google Scholar]
- 66.Kowaltowski AJ, Fenton RG, Fiskum G. Bcl-2 family proteins regulate mitochondrial reactive oxygen production and protect against oxidative stress. Free Radic Biol Med 2004;37:1845–53. 10.1016/j.freeradbiomed.2004.09.005 [DOI] [PubMed] [Google Scholar]
- 67.Justilien V, Pang JJ, Renganathan K, Zhan X, Crabb JW, So RK, et al. SOD2 knockdown mouse model of early AMD. Investig Ophthalmol Vis Sci 2007;48:4407–20. 10.1167/iovs.07-0432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Myers CR, Myers JM. The effects of acrolein on peroxiredoxins, thioredoxins, and thioredoxin reductase in human bronchial epithelial cells. Toxicology 2009;257:95–104. 10.1016/j.tox.2008.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mogilyansky E, Rigoutsos I. The miR-17/92 cluster: a comprehensive update on its genomics, genetics, functions and increasingly important and numerous roles in health and disease. Cell Death Differ 2013;20:1603–14. 10.1038/cdd.2013.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen J-A, Huang Y-P, Mazzoni EO, Tan GC, Zavadil J, Wichterle H. Mir-17-3p Controls Spinal Neural Progenitor Patterning by Regulating Olig2/Irx3 Cross-Repressive Loop. Neuron 2011;69:721–35. 10.1016/j.neuron.2011.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jiang X, Li N. Induction of MiR-17-3p and MiR-160a by TNFα and LPS. Cell Biochem Funct 2011;29:164–70. 10.1002/cbf.1728 [DOI] [PubMed] [Google Scholar]
- 72.Yin R, Wang R, Guo L, Zhang W, Lu Y. MiR-17-3p inhibits angiogenesis by downregulating flk-1 in the cell growth signal pathway. J Vasc Res 2013;50:157–66. 10.1159/000345697 [DOI] [PubMed] [Google Scholar]
- 73.Liu T, Qin W, Huang Y, Zhao Y, Wang J. Induction of Estrogen-Sensitive Epithelial Cells Derived from Human-Induced Pluripotent Stem Cells to Repair Ovarian Function in a Chemotherapy-Induced Mouse Model of Premature Ovarian Failure. DNA Cell Biol 2013;32:130914053323001 10.1089/dna.2013.2032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Du WW, Li X, Li T, Li H, Khorshidi A, Liu F, et al. The microRNA miR-17-3p inhibits mouse cardiac fibroblast senescence by targeting Par4. J Cell Sci 2015;128:293–304. 10.1242/jcs.158360 [DOI] [PubMed] [Google Scholar]
- 75.Satoh JI, Kino Y, Niida S. MicroRNA-seq data analysis pipeline to identify blood biomarkers for Alzheimer's disease from public data. Biomark Insights 2015;10:21–31. 10.4137/BMIMI.S25132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Curti V, Capelli E, Boschi F, Nabavi SF, Bongiorno AI, Habtemariam S, et al. Modulation of human miR-17-3p expression by methyl 3-O-methyl gallate as explanation of its in vivo protective activities. Mol Nutr Food Res 2014:1–9. 10.1002/mnfr.201400007 [DOI] [PubMed] [Google Scholar]
- 77.Thomas M, Lange-Grünweller K, Hartmann D, Golde L, Schlereth J, Streng D, et al. Analysis of transcriptional regulation of the human miR-17-92 cluster; evidence for involvement of Pim-1. Int J Mol Sci 2013;14:12273–96. 10.3390/ijms140612273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Graves JA, Metukuri M, Scott D, Rothermund K, Prochownik E V. Regulation of reactive oxygen species homeostasis by peroxiredoxins and c-Myc. J Biol Chem 2009;284:6520–9. 10.1074/jbc.M807564200 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from Dryad in the following temporary url: http://datadryad.org/review?doi=doi:10.5061/dryad.cf860