This trial aimed to improve psychological distress, meet supportive care needs, and enhance quality of life of patients with colorectal cancer. SurvivorCare (SC) comprised educational materials, needs assessment, a survivorship care plan, an end-of-treatment session, and follow-up telephone calls. Patients were followed up at 2 and 6 months. Adding SC to usual care did not have a beneficial effect on outcome measures, but patients in the SC group were more satisfied with care.
Keywords: Colorectal cancer, Survivors, Distress, Quality of life, Nurse, Randomized controlled trial
Abstract
Introduction.
Colorectal cancer (CRC) and its treatments can cause distressing sequelae. We conducted a multicenter randomized controlled trial aiming to improve psychological distress, supportive care needs (SCNs), and quality of life (QOL) of patients with CRC. The intervention, called SurvivorCare (SC), comprised educational materials, needs assessment, survivorship care plan, end-of-treatment session, and three follow-up telephone calls.
Methods.
At the end of treatment for stage I–III CRC, eligible patients were randomized 1:1 to usual care (UC) or to UC plus SC. Distress (Brief Symptom Inventory 18), SCNs (Cancer Survivors’ Unmet Needs measure), and QOL (European Organization for Research and Treatment of Cancer [EORTC] QOL questionnaires C30 and EORTC CRC module CR29) were assessed at baseline and at 2 and 6 months (follow-up 1 [FU1] and FU2, respectively). The primary hypothesis was that SC would have a beneficial effect on distress at FU1. The secondary hypotheses were that SC would have a beneficial effect on (a) SCN and QOL at FU1 and on (b) distress, SCNs, and QOL at FU2. A total of 15 items assessed experience of care.
Results.
Of 221 patients randomly assigned, 4 were ineligible for the study and 1 was lost to FU, leaving 110 in the UC group and 106 in the SC group. Patients’ characteristics included the following: median age, 64 years; men, 52%; colon cancer, 56%; rectal cancer, 35%; overlapping sites of disease, 10%; stage I disease, 7%; stage II, 22%; stage III, 71%. Baseline distress and QOL scores were similar to population norms. Between-group differences in distress at FU1 (primary outcome) and at FU2, and SCNs and QOL at FU1 and FU2 were small and nonsignificant. Patients in the SC group were more satisfied with survivorship care than those in the UC group (significant differences on 10 of 15 items).
Conclusion.
The addition of SC to UC did not have a beneficial effect on distress, SCNs, or QOL outcomes, but patients in the SC group were more satisfied with care.
Implications for Practice:
Some survivors of colorectal cancer report distressing effects after completing treatment. Strategies to identify and respond to survivors’ issues are needed. In a randomized controlled trial, the addition of a nurse-led supportive care package (SurvivorCare) to usual post-treatment care did not impact survivors’ distress, quality of life, or unmet needs. However, patients receiving the SurvivorCare intervention were more satisfied with survivorship care. Factors for consideration in the design of subsequent studies are discussed.
Introduction
Worldwide, an estimated 1.4 million people were diagnosed with colorectal cancer (CRC) in 2012 [1]. Australia, New Zealand, Europe, and North America have the highest incidences, although the disease is also common in developing countries [1]. In the U.S., as in Australia, 5-year relative survival is approximately 65% [2]. There are an estimated 1.3 million survivors of CRC in the U.S. [2].
Patients frequently report a range of distressing consequences as a result of CRC and its treatment. These include persistent physical side effects such as fatigue [3–8], bowel and urinary problems [5, 7, 9–16], sexual dysfunction [4, 7–9, 11, 15], sleep problems [4, 5], and neuropathy [3, 11]. Patients are at risk for surgical complications, such as bowel obstruction, hernia, and fistula formation [17]. CRC survivors report elevated levels of psychological distress and depression [7, 13, 14, 18–21]. Fear of cancer recurrence is common [4, 7, 8, 22, 23]. Patients with rectal cancer and those who have more complex therapy appear to experience greater problems [9, 10, 15, 20].
Many of these issues may persist for years after completing treatments [9, 10, 12, 19, 24]. Many survivors do not return or have a delayed return to full-time work [8, 25]. Not infrequently, survivors report financial concerns [5, 24]. Unsurprisingly, the quality of life (QOL) of CRC survivors is impaired compared with the general population, especially regarding physical [6, 8, 9, 12], role [6, 26], emotional [5, 10], and social functioning [5, 6, 10, 21, 26].
Survivors frequently report unmet needs, including the need for more comprehensive, coordinated care; more information; and psychological support, particularly to manage the fear of cancer recurrence [16, 22, 27–29]. Current models of post-treatment care do not adequately address survivors’ concerns [30].
Psychological distress after cancer treatment can be severe and long-lasting if not identified and managed appropriately [31]. Patients with CRC who have significant distress are more likely to use emergency department and inpatient hospital services [32]. Physical and psychosocial consequences of treatment can have a debilitating impact on QOL, further contributing to distress. The intervention in this study aimed to identify and address patients’ distress and unmet needs, with the primary goal being to reduce the level of distress.
Agencies such as the Institute of Medicine and the American Society of Clinical Oncology have emphasized the need for research to evaluate interventions to better meet the needs of survivors [31, 33]. However, little survivorship research has focused on CRC [34]. We sought to evaluate the effectiveness of an innovative supportive care intervention (SurvivorCare), comprising survivorship educational materials, a tailored survivorship care plan (SCP), an individually tailored end-of-treatment consultation and telephone follow-up, for people with potentially cured CRC, aiming to reduce psychological distress and unmet needs in the 6 months following treatment completion. SurvivorCare was developed to identify and respond to survivors’ concerns, normalize end-of-treatment experience, prepare them for the post-treatment phase, link them to appropriate support services, and support self-management [35].
The SurvivorCare intervention was tested with 10 CRC survivors [35]. There was a high consent rate (83%) to the pilot study, and minimal attrition. Survivors considered the intervention to be appropriate, relevant, and useful. A number of participants were experiencing clinical levels of distress at baseline (30%). All participants reported unmet needs.
Our primary hypothesis was that CRC survivors allocated to the SurvivorCare intervention would report a significant relative benefit for psychological distress compared with survivors in the control group from baseline to follow-up 1 (2 months after either randomization to the usual care group or the first intervention session for the SurvivorCare group). We also hypothesized that, compared with patients in the control group, patients allocated to SurvivorCare would report significant beneficial effect for unmet psychological and informational needs, and QOL from baseline to follow-up 1, and sustained improvement in psychosocial outcomes over 6 months.
Patients and Methods
This article reports on a multisite, multistate, randomized controlled trial. Development and pilot data [35], and the full study protocol have been published [36].
Setting
The study was undertaken at 18 sites across three states in Australia. Recruiting sites were in major metropolitan, regional, and rural areas in both public and private settings. Ethical approval was obtained covering all sites. The trial was registered (ACTRN12610000207011).
Participants
To be eligible, the following was required of participants: (a) have a confirmed diagnosis of colon or rectal cancer; (b) have stage I, II, or III disease; (c) be treated with curative intent with surgery with or without radiation or chemotherapy; (d) be older than age 18 years; and (e) be able to understand English (many measures were available only in English). Exclusion criteria were (a) significant cognitive or psychological difficulties; (b) being too unwell to participate, as determined by the patient’s treatment team; (c) past history of malignancy other than nonmelanomatous skin cancer; and (d) enrollment in a conflicting supportive care trial.
Recruitment Process
Patients were approached 0 to 6 months before the end of treatment (although they were randomly assigned to a study group as close to end of treatment as possible) or up to 6 months after the end of treatment. Patients were randomly assigned 1:1 to either usual care or SurvivorCare. Allocation was balanced by site using a minimization method and participants were randomly assigned and notified of allocation after completion of consent and baseline questionnaires.
Intervention Group: SurvivorCare
The intervention comprised four main components: (a) information package, (b) nurse-led, face-to-face end-of-treatment session; (c) a tailored SCP; and (d) telephone follow-up [36]. Intervention nurses received training in all aspects of the protocol, including prevention of diffusion into usual care. We audiotaped sessions for quality assurance [36].
Information Package
The package included a DVD (Just Take It Day to Day) [37], a general information booklet for cancer survivors (Life After Cancer), and a question prompt list (QPL). These were based on initial focus-group work with patients with cancer and with health professionals [38]. The QPL comprised 70 questions covering common issues CRC survivors encounter in the first year following treatment, listed in 10 sections. Domains were based on a review of the literature and concerns identified in our previous focus-group work [38].
Nurse-Led Face-to-Face Session
An individualized, nurse-led, end-of-treatment session aimed to respond to the patient’s individual and pertinent concerns, attain a sense of closure on treatment, prepare people for the survivorship phase, and introduce telephone follow-up. It was guided by the survivor’s responses to the QPL, indicated concerns and goals, and completion of the distress thermometer [39]. The session included discussion of a tailored SCP, common survivorship issues, and a healthy lifestyle. A detailed manual specifying the precise content of the intervention was developed. The session took place in a private hospital clinic room, and lasted approximately 60 minutes.
Survivorship Care Plan
The SCP included details of the cancer diagnosis, treatments, health promotional advice, supportive care, and psychosocial elements, as well as recommendations for follow-up. A copy of the SCP was sent to the patient’s primary care physician. In preliminary work, we asked CRC survivors and health professionals to evaluate a draft SCP, based upon the Institute of Medicine (IOM) template [40]. From these results, we refined the content of the SCP and developed a computer-based SCP for ease of completion.
Nurse-Led Telephone Follow-Up
These sessions occurred 1, 3, and 7 weeks after the first intervention session. The sessions revisited issues discussed during the end-of-treatment session and addressed any other survivor issues.
Usual Care/Control Group
Participants allocated to usual care received care according to the treating center or practitioner’s usual practice. Key elements of the intervention were not routinely provided (i.e., DVD and booklet, QPL, SCP, and face-to-face and telephone sessions).
Data Collection Procedure
Participants completed a baseline questionnaire on the day of randomization and two subsequent follow-up questionnaires at 2 months (FU1) and 6 months (FU2) after the face-to-face session for the intervention group or after randomization for the usual care group.
Demographic Information
Data included age, sex, marital status, postcode, occupation, and education level.
Medical Records
Data included cancer type, stage, and treatment.
Outcome Measures
Outcome measures were psychometrically sound, acceptable, responsive, and have been used in this population.
Psychological Distress
The Brief Symptom Inventory 18 (BSI-18) was selected as the primary outcome measure [41]. It comprises 18 items answered on a 5-point scale to measure global distress. Subscales assess anxiety, depression, and somatization. The BSI was chosen as the primary outcome measure because it has been used widely in patients with cancer and is known to be responsive to change.
Survivors’ Unmet Needs
The Cancer Survivors’ Unmet Needs measure (CaSUN) [42] was used to assess survivors’ unmet needs. It includes 35 unmet need items, 6 positive change items, and an open-ended question.
Quality of Life
The European Organization for Research and Treatment of Cancer core questionnaire (EORTC QLQ C-30) [43], together with the CRC module (EORTC QLQ CR-29) [44], was used to measure QOL.
Perceptions of Care
Perceptions of post-treatment care were assessed with a survey developed specifically for this study. Items were generated based on elements of ideal survivorship care [31]. These items were piloted in interviews with eight cancer survivors and two family caregivers of patients with cancer. The pilot sample agreed that items were relevant and acceptable. Minor changes were made to the wording of items. The survey consisted of 15 items with a 5-point Likert response scale ranging from strongly disagree to strongly agree.
Sample Size Requirements
The primary outcome was psychological distress as assessed by the BSI-18 Global Severity Index (GSI), an 18-item scale with a possible range of 72. We based our sample size calculations on 80% power, a 2-sided t test with an α-level of 0.05, a difference between groups of 3.6 points on the primary outcome (or 5% of the instrument range) [45] at the first follow-up, and a standard deviation of 8.6 [41] (a standardized difference of 0.42). This is considered a clinically important difference [45]. Given these specifications, the required sample size was 180 patients (or 90 patients per arm). Assuming attrition of up to 10%, 200 patients were required (100 patients per arm).
Statistical Methods
Unless otherwise stated, analyses were conducted in SPSS Statistics for Windows version 21.0 (IBM Corp., Armonk, NY, http://www-01.ibm.com). Descriptive statistics were used to summarize outcome measure completion rates, missing items for completed forms, and baseline demographic and clinical characteristics of patients randomized to each study arm. Possible differential attrition was assessed by comparing basic demographic and clinical characteristics of patients who dropped out of the trial and continuing participants using t tests (or Mann–Whitney U) and chi-square tests, as appropriate.
Outcome analysis was by intention to treat. Analysis of multi-item scales was carried out by fitting a linear mixed model to each outcome separately. Models were estimated by maximum likelihood and included a fixed group by time effect and no random effects (cell means models) [46]. An unstructured covariance type was used to model the covariance structure among repeated measures. Group comparisons at postbaseline time points were performed using contrasts within the models. Multi-item scales included the BSI-18 GSI, the QLQ-C30 functional and symptom scales and the following QLQ-CR29 scales: body image, urinary frequency, blood and mucus in stool and stool frequency.
Mann-Whitney U tests were used to compare groups on single items from the EORTC QLQ-C30 and QLQ-CR29 [47] and the Perceptions of Care measure at postbaseline time points. These were conducted with R (reference index version 3.1.0 “Spring Dance”) [48] using the “coin” package [49].
For the analysis of the primary outcome at the first follow-up, α was set at 0.05 (2-tailed). Hochberg’s modified Bonferroni procedure [50] was applied to significance tests for secondary outcomes (83 total: BSI-18, 1; CaSun, 6; QLQ-C30, 30; QLQ-CR29, 46) to guard against false-positive conclusions. Hochberg’s procedure was also applied to tests of items comprising the Perceptions of Care measure (15 total). The p value adjustment was calculated in R.
Results
Trial Profile
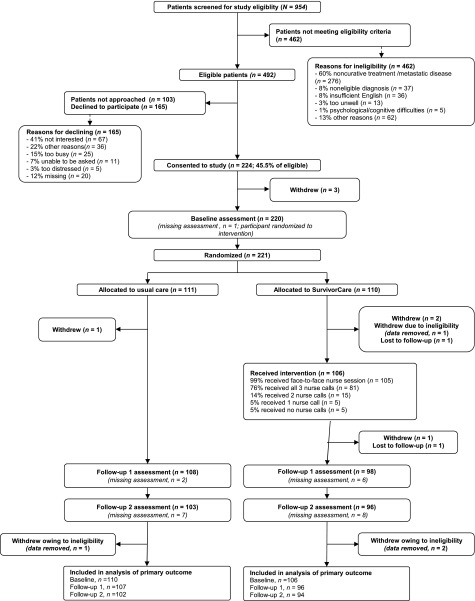
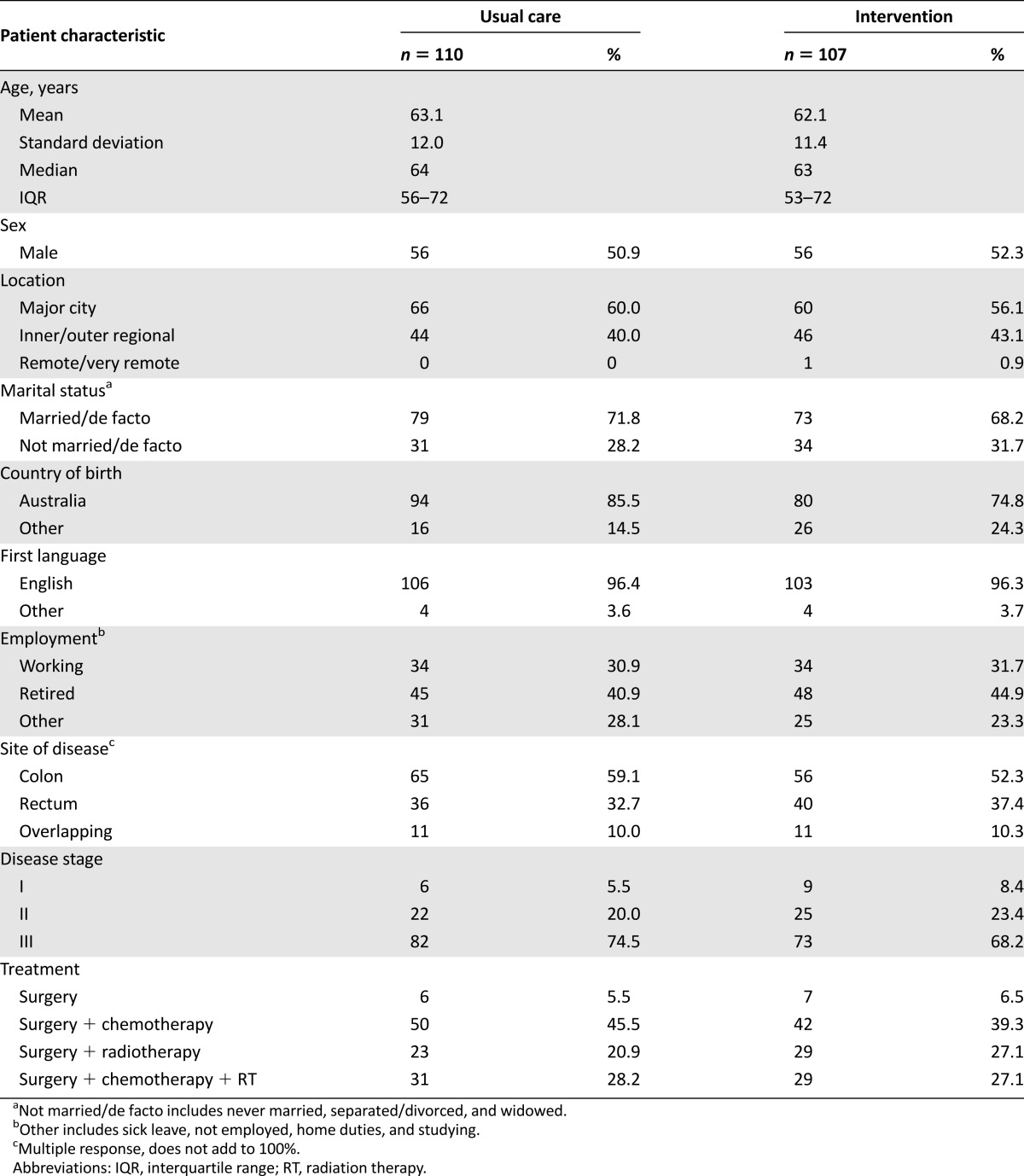
Of 492 patients who were eligible for the study (Fig. 1), 389 were approached and 224 consented to participate (58% consent rate). The median number of days between end of treatment and baseline assessment was 11 days (interquartile range [IQR]: −2 to 55 days) for patients randomized to usual care and 3 days (IQR: −2 to 41 days) for patients randomized to the intervention. Baseline characteristics are provided in Table 1. Groups appeared well balanced at baseline.
Figure 1.
Study flow chart.
Table 1.
Patient demographic and clinical characteristics
Intervention Fidelity
Of 106 intervention participants, 105 participated in the nurse-led end-of-treatment session (Fig. 1). All nurse-led sessions occurred after randomization, but five participants attended the session before finishing treatment. Intervention checklists were completed for 97 of the 105 intervention participants. Of these 97, 72 (74%) had watched the DVD, 81 had read the booklet, and 81 had completed the QPL before the first nurse-led session. Furthermore, 92 of this 97 received a copy of their SCP at this session.
The majority of intervention participants (81 of 106; 76%) received all 3 nurse-led telephone follow-up calls; 15 (14%) received 2 calls, 5 (5%) received 1, and 5 (5%) received none.
Diffusion Into Usual Care
Nine of the usual-care participants (9%) received the DVD; however, only 3 watched it. Twenty-two usual-care participants received the booklet. A majority (16 of 22) read the booklet.
Outcome Measure Availability
Apart from some outcomes assessed by the QLQ-CR29, most patients provided data on every outcome at all scheduled assessments (≥98% at baseline and ≥88% at postbaseline assessments; supplemental online Appendix 1). There were minimal missing items on completed forms (≤3% for the BSI, CaSUN, and QLQ-C30; and ≤5% for the Perceptions of Care questionnaire; supplemental online Appendix 2).
Outcome Analysis
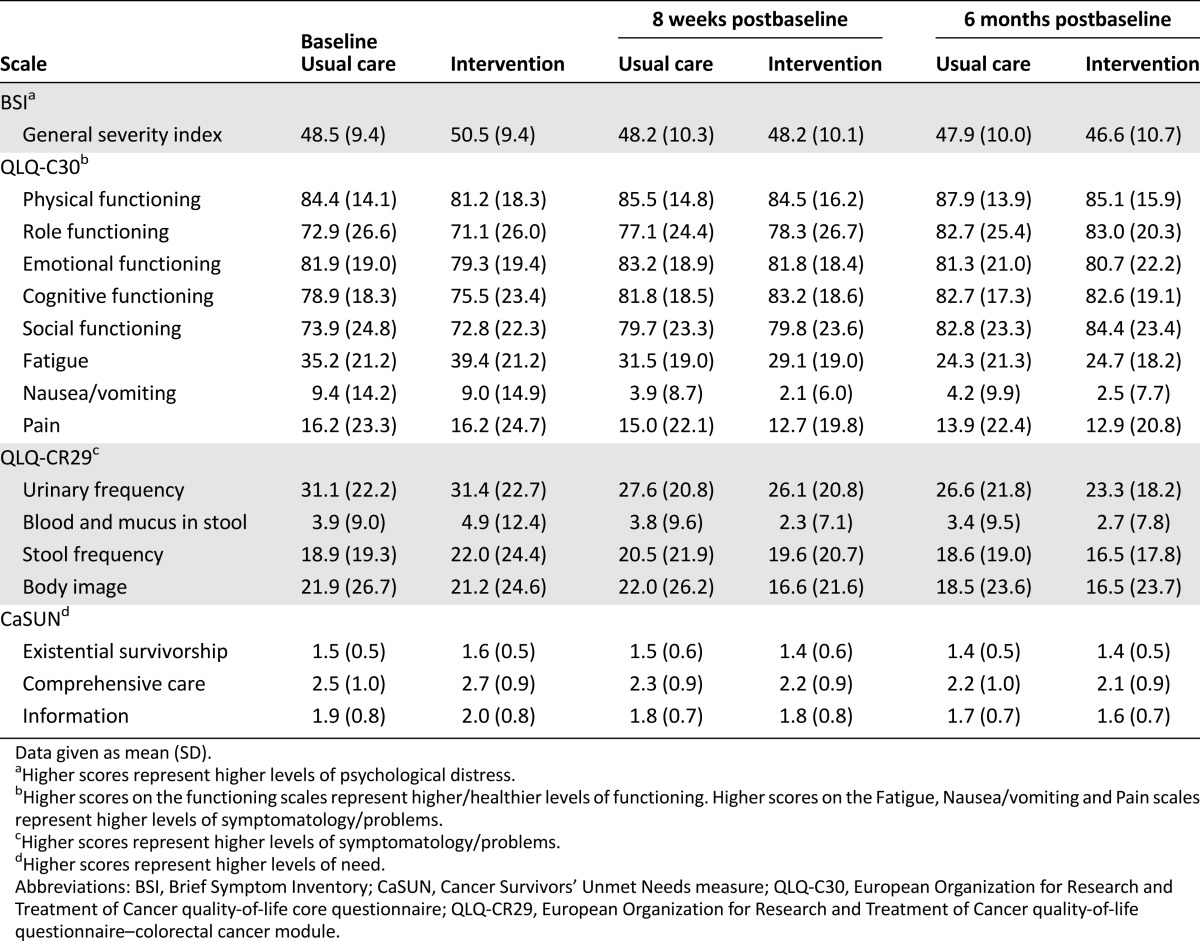
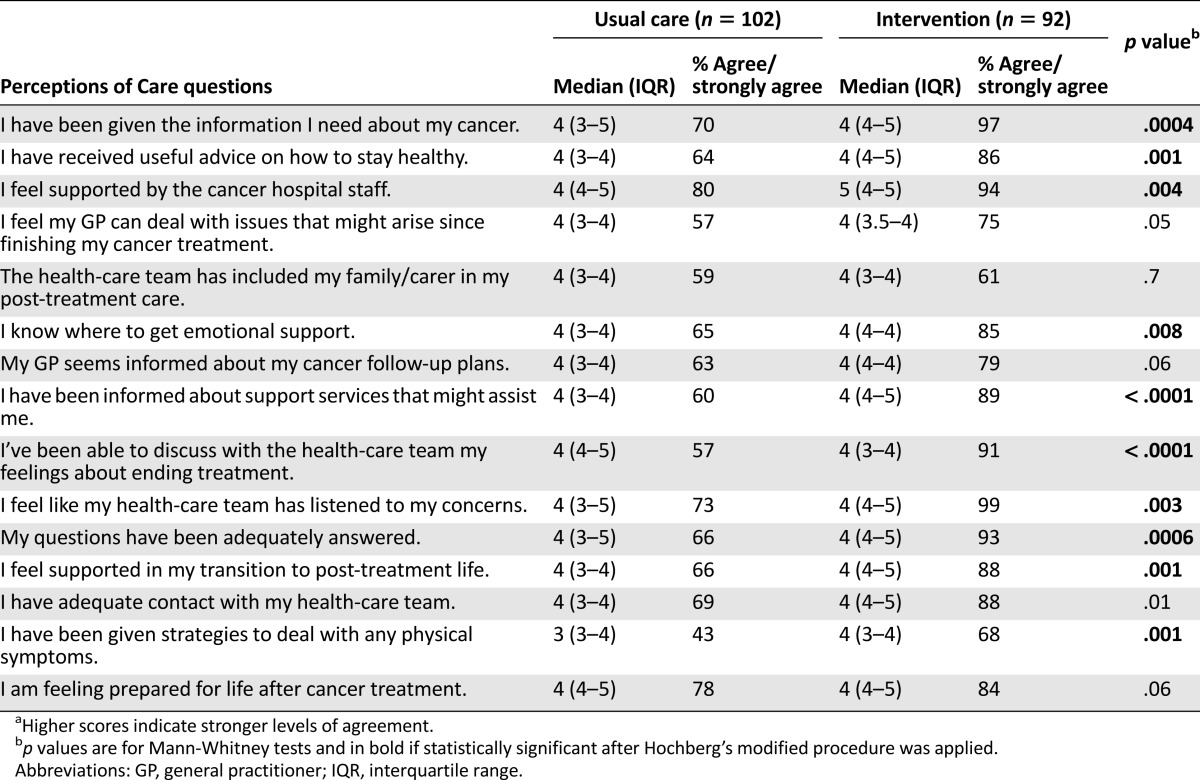
For brevity and ease of reading, full results are presented for outcomes assessed by multi-item scales and the Perceptions of Care measure only. Descriptive data for outcomes assessed by multi-item scales are provided in Table 2. Results from mixed models are provided in Table 3. Results for the Perceptions of Care are provided in Table 4. Results for outcomes assessed by single items are summarized in text, but tables of descriptive data and test results are provided in supplemental online Appendix 3.
Table 2.
Descriptive data for study outcomes assessed by multi-item scales by group at scheduled assessments
Table 3.
Mixed-model estimates of mean difference from usual care with 95% confidence intervals at postbaseline assessments for outcomes assessed by multi-item scales
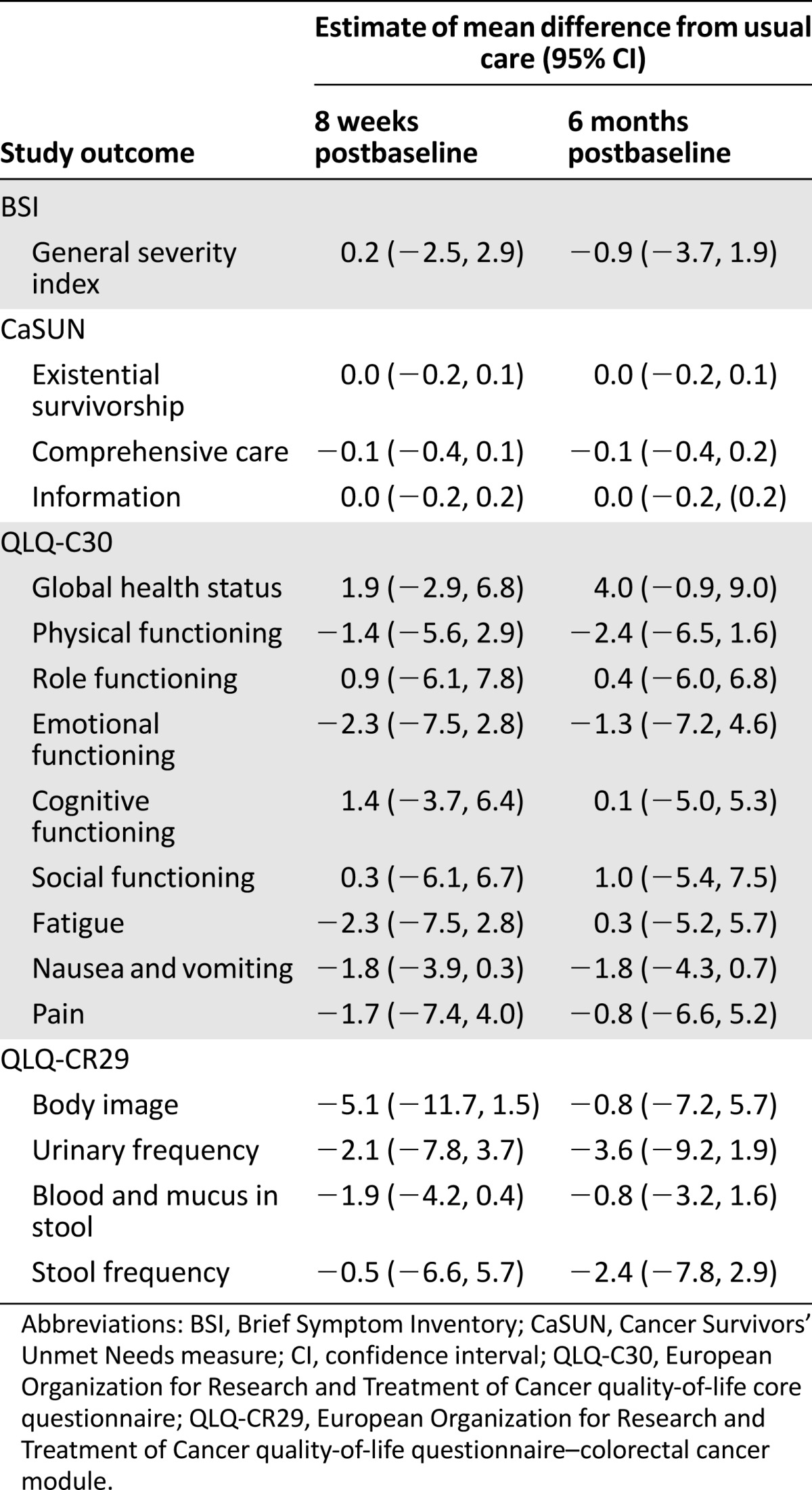
Table 4.
Descriptive data and results of Mann-Whitney tests for the Perceptions of Care measurea
Primary Outcome
Study groups reported similar levels of psychological distress 2 months postbaseline (Table 2). The estimate of the difference between groups was very small and not statistically significant (difference: 0.2; 95% CI: −2.5 to 2.9).
Secondary Outcomes
Psychological Distress
Study groups also reported similar levels of psychological distress at the second follow-up (Table 2). The estimate of the difference between groups at this time was small and not significant (Table 3).
Cancer Survivor Needs
Estimates of mean differences between groups in existential survivorship, comprehensive care, and information needs at both follow-up times were small and not significant (Table 3).
Health-Related Quality of Life
At 2 months and 6 months postbaseline, study groups reported similar levels of overall QOL and functioning as assessed by the QLQ-C30 (Table 2). They also reported similar levels of symptoms and problems as assessed by the QLQ-C30 (Table 2) and QLQ-CR29 (supplemental online Appendix 3). All between-group differences were small and not significant (Table 3; supplemental online Appendix 3).
Perceptions of Care
Participants in the intervention group were more satisfied with care provided than usual-care participants (Table 4). Median scores for most items were the same, but interquartile ranges indicated that more intervention participants “agreed” or “strongly agreed” with item content than did usual-care participants.
Discussion
A proportion of CRC survivors encounter a broad range of issues after completing treatment, despite ongoing follow-up care. We designed a nurse-led supportive care intervention to better meet the needs of survivors, and evaluated this in a randomized controlled trial. We hypothesized that the intervention would reduce distress, improve QOL, and reduce unmet needs. We found no significant effect of the intervention on these endpoints. However, people who received the SurvivorCare intervention were more satisfied with many aspects of post-treatment care than those who received usual care.
Whereas previous studies have reported elevated distress [7, 13, 14, 21, 23], levels of psychological distress were low in this group of CRC survivors [51], similar to that of the general population. Our pilot study had suggested that a proportion of CRC survivors had significant levels of distress [35]. In a study reported after we commenced SurvivorCare, Grunfeld and colleagues also found low levels of distress in a randomized study that assessed the impact of SCPs for breast cancer survivors [52]. Even if an intervention were known to be effective at reducing distress, it would be difficult to demonstrate this in a population with low baseline levels. Floor effects are increasingly recognized in studies seeking to address distress [53].
It is possible that SurvivorCare may be an effective intervention for a more targeted population, perhaps those with higher levels of distress, or those with greater levels of unmet need. White and colleagues recently reported results from a randomized controlled trial of a telephone-based peer support program for women with a BRCA 1 or 2 mutation [54]. The study enrolled women with high levels of distress, who expressed a need for peer support, and demonstrated a reduction in distress following the intervention. The number of people with high levels of distress at baseline was low and did not permit an exploration of the effect of the SurvivorCare intervention within this or other subsets of patients.
Participants generally had good QOL. Other studies also indicate that, overall, long-term survivors experience good QOL [13, 26, 55], and have overall health and levels of psychological morbidity consistent with population norms [29]. Jansen and colleagues have queried the sensitivity of QOL instruments to adequately reflect survivors’ experiences, reflecting on “the finding of good psychological QOL in long-term CRC survivors despite the presence of higher depression rates and distress regarding cancer” [12]. This is important because it underscores the issue of how to assess the impact of an intervention that is intended to improve well-being. We assessed distress as the primary outcome because we were concerned that measures of QOL or unmet need may not be sensitive to improved survivor well-being. Grunfeld and colleagues have also queried the most appropriate endpoints for similar studies [52]. Related to this, the SurvivorCare intervention may have been quite different for individual patients: One patient may have prioritized management of symptoms, such as diarrhea; another may have needed help to return to work. Choosing an appropriate endpoint for such a tailored intervention is challenging.
Patients in the study reported a range of needs. Unmet needs are associated with decreased QOL [56, 57]. A prospective longitudinal study found that 30% of survivors reported more than 5 unmet needs at the end of treatment, and this did not improve for 60% at 6 months [27]. The most frequently endorsed unmet needs were psychological needs and dealing with the fear of cancer recurrence [27].
Patients reported the need for comprehensive care [51]. They indicated a need for understandable and up-to-date information, help to manage side effects and complications of treatment, and help managing worries about the cancer coming back. While the needs scale did not show a difference between the two arms, on the experience-of-care measure, patients in the intervention were more likely to endorse that they had received information that was important to their care and had received adequate emotional support. Interestingly, the two items that relate to the primary care physician being better informed indicated no difference between the two arms. This might suggest that the nurse-led component may have been more useful than the SCP. Whether the intervention may have been more effective if delivered by other health professionals or by a multidisciplinary team is unknown.
People in the usual-care group did not appear to receive key elements of the intervention, including information materials, an SCP, end-of-treatment session, or telephone follow-up. Although we did not audio record all aspects of usual care, it is likely that care did not include provision of survivorship information nor needs assessment. Survivors reported significant unmet needs in both arms of the study. Whether usual care of CRC survivors is significantly different between Australia and other countries is unknown.
In the U.S., the median age at diagnosis of CRC is 69 years [2]. Eighty-two percent of CRC survivors are age 60 years or older and 61% are age 70 years or older [2]. The majority of CRC survivors have coexisting medical illnesses [9, 58]. QOL is strongly impacted by comorbidities, aging, weight, and chronic medical conditions [14]. Our intervention did not specifically target the management of other medical conditions. It is possible that an effective intervention might need to consider these broader health issues. Potentially, primary care may have an important role in improving survivor well-being. Studies suggest that primary care is an acceptable alternative to specialist or hospital-based care [59], including for CRC survivors [60].
Although not specifically for CRC survivors, Andreyev and colleagues have reported results from an algorithm-based approach to the management of patients with treatment-related gastrointestinal symptoms as a consequence of previous pelvic radiotherapy [61]. Patients were randomized to nurse-led, algorithm-based treatment, gastroenterologist-led treatment, or to usual care. Patients who received the algorithm-based intervention had greater improvements than patients who received usual care. The authors concluded that nurse-led, algorithm-based care was appropriate for most people. Although there are similarities to SurvivorCare, perhaps a strategy targeting people with high symptom burden and using an algorithm-based strategy may be more effective.
Conclusion
This intervention failed to show an improvement in survivors’ levels of distress or QOL; levels of distress were low and QOL was generally quite good in the study cohort. However, survivors who received the novel supportive care intervention reported improved satisfaction with many aspects of post-treatment care. This suggests that the intervention has useful elements. Future studies should carefully consider the choice of study endpoints and might consider enriching the target population for survivors with significant issues or unmet needs.
See http://www.TheOncologist.com for supplemental material available online.
This article is available for continuing medical education credit at CME.TheOncologist.com.
Supplementary Material
Acknowledgments
This study was funded jointly by the Victorian State Government through the Victorian Cancer Agency and by beyondblue, and the Australian Government through Cancer Australia, and was awarded through the Priority-driven Collaborative Cancer Research Scheme (Grant 628581).
This study was presented, in part, at the annual meeting of the American Society of Clinical Oncology (May 29–June 2, 2015; Chicago, IL), the International Conference on Cancer Nursing (July 8–11, 2015; Vancouver, Canada), and the Cancer Survivorship Symposium, jointly coordinated by the American Academy of Family Physicians, the American College of Physicians, and the American Society of Clinical Oncology (January 15–16, 2016; San Francisco, CA).
Author Contributions
Conception/Design: Michael Jefford, Karla Gough, Sanchia Aranda, Phyllis Butow, Jane Young, Mei Krishnasamy, Dorothy King, Penelope Schofield
Provision of study material or patients: Michael Jefford, Lahiru Russell, Anna Ugalde, Andrew Strickland, Michael Franco, Robert Blum, Catherine Johnson, Vinod Ganju, Jeremy Shapiro, Geoffrey Chong, Julie Charlton, Andrew Haydon
Collection and/or assembly of data: Michael Jefford, Lahiru Russell, Jo Phipps-Nelson, Anna Ugalde, Andrew Strickland, Michael Franco, Robert Blum, Catherine Johnson, Vinod Ganju, Jeremy Shapiro, Geoffrey Chong, Julie Charlton, Andrew Haydon, Penelope Schofield
Data analysis and interpretation: Michael Jefford, Karla Gough, Allison Drosdowsky, Lahiru Russell, Sanchia Aranda, Phyllis Butow, Jo Phipps-Nelson, Jane Young, Mei Krishnasamy, Anna Ugalde, Dorothy King, Penelope Schofield
Manuscript writing: Michael Jefford, Karla Gough, Allison Drosdowsky, Lahiru Russell, Sanchia Aranda, Phyllis Butow, Jo Phipps-Nelson, Jane Young, Mei Krishnasamy, Anna Ugalde, Dorothy King, Andrew Strickland, Michael Franco, Robert Blum, Catherine Johnson, Vinod Ganju, Jeremy Shapiro, Geoffrey Chong, Julie Charlton, Andrew Haydon, Penelope Schofield
Final approval of manuscript: Michael Jefford, Karla Gough, Allison Drosdowsky, Lahiru Russell, Sanchia Aranda, Phyllis Butow, Jo Phipps-Nelson, Jane Young, Mei Krishnasamy, Anna Ugalde, Dorothy King, Andrew Strickland, Michael Franco, Robert Blum, Catherine Johnson, Vinod Ganju, Jeremy Shapiro, Geoffrey Chong, Julie Charlton, Andrew Haydon, Penelope Schofield
Disclosures
Jo Phipps-Nelson: CSL Limited (OI); Michael Franco: Mundipharma (H). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 3.Pettersson G, Berterö C, Unosson M, et al. Symptom prevalence, frequency, severity, and distress during chemotherapy for patients with colorectal cancer. Support Care Cancer. 2014;22:1171–1179. doi: 10.1007/s00520-013-2069-z. [DOI] [PubMed] [Google Scholar]
- 4.Baker F, Denniston M, Smith T, et al. Adult cancer survivors: How are they faring? Cancer. 2005;104(suppl):2565–2576. doi: 10.1002/cncr.21488. [DOI] [PubMed] [Google Scholar]
- 5.Arndt V, Merx H, Stegmaier C, et al. Quality of life in patients with colorectal cancer 1 year after diagnosis compared with the general population: A population-based study. J Clin Oncol. 2004;22:4829–4836. doi: 10.1200/JCO.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 6.Kopp I, Bauhofer A, Koller M. Understanding quality of life in patients with colorectal cancer: Comparison of data from a randomised controlled trial, a population based cohort study and the norm reference population. Inflamm Res. 2004;53(suppl 2):S130–S135. doi: 10.1007/s00011-004-0361-6. [DOI] [PubMed] [Google Scholar]
- 7.Phipps E, Braitman LE, Stites S, et al. Quality of life and symptom attribution in long-term colon cancer survivors. J Eval Clin Pract. 2008;14:254–258. doi: 10.1111/j.1365-2753.2007.00842.x. [DOI] [PubMed] [Google Scholar]
- 8.Schag CA, Ganz PA, Wing DS, et al. Quality of life in adult survivors of lung, colon and prostate cancer. Qual Life Res. 1994;3:127–141. doi: 10.1007/BF00435256. [DOI] [PubMed] [Google Scholar]
- 9.Downing A, Morris EJ, Richards M, et al. Health-related quality of life after colorectal cancer in England: A patient-reported outcomes study of individuals 12 to 36 months after diagnosis. J Clin Oncol. 2015;33:616–624. doi: 10.1200/JCO.2014.56.6539. [DOI] [PubMed] [Google Scholar]
- 10.Caravati-Jouvenceaux A, Launoy G, Klein D, et al. Health-related quality of life among long-term survivors of colorectal cancer: A population-based study. The Oncologist. 2011;16:1626–1636. doi: 10.1634/theoncologist.2011-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Denlinger CS, Barsevick AM. The challenges of colorectal cancer survivorship. J Natl Compr Canc Netw. 2009;7:883–893. doi: 10.6004/jnccn.2009.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jansen L, Koch L, Brenner H, et al. Quality of life among long-term (≥5 years) colorectal cancer survivors--systematic review. Eur J Cancer. 2010;46:2879–2888. doi: 10.1016/j.ejca.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 13.Ramsey SD, Berry K, Moinpour C, et al. Quality of life in long term survivors of colorectal cancer. Am J Gastroenterol. 2002;97:1228–1234. doi: 10.1111/j.1572-0241.2002.05694.x. [DOI] [PubMed] [Google Scholar]
- 14.Trentham-Dietz A, Remington PL, Moinpour CM, et al. Health-related quality of life in female long-term colorectal cancer survivors. The Oncologist. 2003;8:342–349. doi: 10.1634/theoncologist.8-4-342. [DOI] [PubMed] [Google Scholar]
- 15.Di Fabio F, Koller M, Nascimbeni R, et al. Long-term outcome after colorectal cancer resection. Patients’ self-reported quality of life, sexual dysfunction and surgeons’ awareness of patients’ needs. Tumori. 2008;94:30–35. doi: 10.1177/030089160809400107. [DOI] [PubMed] [Google Scholar]
- 16.Nikoletti S, Young J, Levitt M, et al. Bowel problems, self-care practices, and information needs of colorectal cancer survivors at 6 to 24 months after sphincter-saving surgery. Cancer Nurs. 2008;31:389–398. doi: 10.1097/01.NCC.0000305759.04357.1b. [DOI] [PubMed] [Google Scholar]
- 17.Liu L, Herrinton LJ, Hornbrook MC, et al. Early and late complications among long-term colorectal cancer survivors with ostomy or anastomosis. Dis Colon Rectum. 2010;53:200–212. doi: 10.1007/DCR.0b013e3181bdc408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lynch BM, Steginga SK, Hawkes AL, et al. Describing and predicting psychological distress after colorectal cancer. Cancer. 2008;112:1363–1370. doi: 10.1002/cncr.23300. [DOI] [PubMed] [Google Scholar]
- 19.Chambers SK, Meng X, Youl P, et al. A five-year prospective study of quality of life after colorectal cancer. Qual Life Res. 2012;21:1551–1564. doi: 10.1007/s11136-011-0067-5. [DOI] [PubMed] [Google Scholar]
- 20.Graça Pereira M, Figueiredo AP, Fincham FD. Anxiety, depression, traumatic stress and quality of life in colorectal cancer after different treatments: A study with Portuguese patients and their partners. Eur J Oncol Nurs. 2012;16:227–232. doi: 10.1016/j.ejon.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Krouse RS, Herrinton LJ, Grant M, et al. Health-related quality of life among long-term rectal cancer survivors with an ostomy: Manifestations by sex. J Clin Oncol. 2009;27:4664–4670. doi: 10.1200/JCO.2008.20.9502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J Cancer Surviv. 2013;7:300–322. doi: 10.1007/s11764-013-0272-z. [DOI] [PubMed] [Google Scholar]
- 23.Deimling GT, Bowman KF, Sterns S, et al. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15:306–320. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- 24.Arndt V, Merx H, Stegmaier C, et al. Restrictions in quality of life in colorectal cancer patients over three years after diagnosis: A population based study. Eur J Cancer. 2006;42:1848–1857. doi: 10.1016/j.ejca.2006.01.059. [DOI] [PubMed] [Google Scholar]
- 25.Short PF, Vasey JJ, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer. 2005;103:1292–1301. doi: 10.1002/cncr.20912. [DOI] [PubMed] [Google Scholar]
- 26.Ramsey SD, Andersen MR, Etzioni R, et al. Quality of life in survivors of colorectal carcinoma. Cancer. 2000;88:1294–1303. [PubMed] [Google Scholar]
- 27.Armes J, Crowe M, Colbourne L, et al. Patients’ supportive care needs beyond the end of cancer treatment: A prospective, longitudinal survey. J Clin Oncol. 2009;27:6172–6179. doi: 10.1200/JCO.2009.22.5151. [DOI] [PubMed] [Google Scholar]
- 28.Salz T, Baxi SS, Blinder VS, et al. Colorectal cancer survivors’ needs and preferences for survivorship information. J Oncol Pract. 2014;10:e277–e282. doi: 10.1200/JOP.2013.001312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harrison SE, Watson EK, Ward AM, et al. Primary health and supportive care needs of long-term cancer survivors: A questionnaire survey. J Clin Oncol. 2011;29:2091–2098. doi: 10.1200/JCO.2010.32.5167. [DOI] [PubMed] [Google Scholar]
- 30.Earle CC, Ganz PA. Cancer survivorship care: Don’t let the perfect be the enemy of the good. J Clin Oncol. 2012;30:3764–3768. doi: 10.1200/JCO.2012.41.7667. [DOI] [PubMed] [Google Scholar]
- 31.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 32.Himelhoch S, Weller WE, Wu AW, et al. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004;42:512–521. doi: 10.1097/01.mlr.0000127998.89246.ef. [DOI] [PubMed] [Google Scholar]
- 33.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology statement: Achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31:631–640. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aziz NM, Rowland JH. Cancer survivorship research among ethnic minority and medically underserved groups. Oncol Nurs Forum. 2002;29:789–801. doi: 10.1188/02.ONF.789-801. [DOI] [PubMed] [Google Scholar]
- 35.Jefford M, Lotfi-Jam K, Baravelli C, et al. Development and pilot testing of a nurse-led posttreatment support package for bowel cancer survivors. Cancer Nurs. 2011;34:E1–E10. doi: 10.1097/NCC.0b013e3181f22f02. [DOI] [PubMed] [Google Scholar]
- 36.Jefford M, Aranda S, Gough K, et al. Evaluating a nurse-led survivorship care package (SurvivorCare) for bowel cancer survivors: Study protocol for a randomized controlled trial. Trials. 2013;14:260. doi: 10.1186/1745-6215-14-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karahalios A, Baravelli C, Carey M, et al. An audiovisual information resource to assist in the transition from completion of potentially curative treatment for cancer through to survivorship: A systematic development process. J Cancer Surviv. 2007;1:226–236. doi: 10.1007/s11764-007-0022-1. [DOI] [PubMed] [Google Scholar]
- 38.Jefford M, Karahalios E, Pollard A, et al. Survivorship issues following treatment completion--results from focus groups with Australian cancer survivors and health professionals. J Cancer Surviv. 2008;2:20–32. doi: 10.1007/s11764-008-0043-4. [DOI] [PubMed] [Google Scholar]
- 39.Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494–1502. doi: 10.1002/cncr.20940. [DOI] [PubMed] [Google Scholar]
- 40.Baravelli C, Krishnasamy M, Pezaro C, et al. The views of bowel cancer survivors and health care professionals regarding survivorship care plans and post treatment follow up. J Cancer Surviv. 2009;3:99–108. doi: 10.1007/s11764-009-0086-1. [DOI] [PubMed] [Google Scholar]
- 41.Zabora J, BrintzenhofeSzoc K, Jacobsen P, et al. A new psychosocial screening instrument for use with cancer patients. Psychosomatics. 2001;42:241–246. doi: 10.1176/appi.psy.42.3.241. [DOI] [PubMed] [Google Scholar]
- 42.Hodgkinson K, Butow P, Hunt GE, et al. The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: The CaSUN (Cancer Survivors’ Unmet Needs measure) Psychooncology. 2007;16:796–804. doi: 10.1002/pon.1137. [DOI] [PubMed] [Google Scholar]
- 43.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 44.Whistance RN, Conroy T, Chie W, et al. Clinical and psychometric validation of the EORTC QLQ-CR29 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer. 2009;45:3017–3026. doi: 10.1016/j.ejca.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 45.Ringash J, O’Sullivan B, Bezjak A, et al. Interpreting clinically significant changes in patient-reported outcomes. Cancer. 2007;110:196–202. doi: 10.1002/cncr.22799. [DOI] [PubMed] [Google Scholar]
- 46.Fairclough DL. Design and Analysis of Quality of Life Studies in Clinical Trials. 2nd ed. Boca Raton, FL: Chapman & Hall/CRC; 2010. [Google Scholar]
- 47.Curran D, Aaronson N, Standaert B, et al. Summary measures and statistics in the analysis of quality of life data: An example from an EORTC-NCIC-SAKK locally advanced breast cancer study. Eur J Cancer. 2000;36:834–844. doi: 10.1016/s0959-8049(00)00056-3. [DOI] [PubMed] [Google Scholar]
- 48.R Core Team. R: A language and environment for statistical computing. Available from R Foundation for Statistical Computing, Vienna, Austria, website: http://www.R-project.org/, 2014.
- 49.Hothorn T, Hornik K, van de Wiel MA, Zeileis A. Implementing a class of permutation tests: The coin package. J Stat Softw. 2008;28:1–23. [Google Scholar]
- 50.Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–802. [Google Scholar]
- 51.Russell L, Gough K, Drosdowsky A, et al. Psychological distress, quality of life, symptoms and unmet needs of colorectal cancer survivors near the end of treatment [published correction appears in J Cancer Surviv 2015;9:471] J Cancer Surviv. 2015;9:462–470. doi: 10.1007/s11764-014-0422-y. [DOI] [PubMed] [Google Scholar]
- 52.Grunfeld E, Julian JA, Pond G, et al. Evaluating survivorship care plans: Results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29:4755–4762. doi: 10.1200/JCO.2011.36.8373. [DOI] [PubMed] [Google Scholar]
- 53.Linden W, Girgis A. Psychological treatment outcomes for cancer patients: What do meta-analyses tell us about distress reduction? Psychooncology. 2012;21:343–350. doi: 10.1002/pon.2035. [DOI] [PubMed] [Google Scholar]
- 54.White VM, Young MA, Farrelly A, et al. Randomized controlled trial of a telephone-based peer-support program for women carrying a BRCA1 or BRCA2 mutation: Impact on psychological distress. J Clin Oncol. 2014;32:4073–4080. doi: 10.1200/JCO.2013.54.1607. [DOI] [PubMed] [Google Scholar]
- 55.Bloom JR, Petersen DM, Kang SH. Multi-dimensional quality of life among long-term (5+ years) adult cancer survivors. Psychooncology. 2007;16:691–706. doi: 10.1002/pon.1208. [DOI] [PubMed] [Google Scholar]
- 56.Hansen DG, Larsen PV, Holm LV, et al. Association between unmet needs and quality of life of cancer patients: A population-based study. Acta Oncol. 2013;52:391–399. doi: 10.3109/0284186X.2012.742204. [DOI] [PubMed] [Google Scholar]
- 57.Yost KJ, Hahn EA, Zaslavsky AM, et al. Predictors of health-related quality of life in patients with colorectal cancer. Health Qual Life Outcomes. 2008;6:66. doi: 10.1186/1477-7525-6-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khan NF, Mant D, Carpenter L, et al. Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: A database study. Br J Cancer. 2011;105(suppl 1):S29–S37. doi: 10.1038/bjc.2011.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lewis RA, Neal RD, Williams NH, et al. Follow-up of cancer in primary care versus secondary care: Systematic review. Br J Gen Pract. 2009;59:e234–e247. doi: 10.3399/bjgp09X453567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wattchow DA, Weller DP, Esterman A, et al. General practice vs surgical-based follow-up for patients with colon cancer: Randomised controlled trial. Br J Cancer. 2006;94:1116–1121. doi: 10.1038/sj.bjc.6603052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Andreyev HJ, Benton BE, Lalji A, et al. Algorithm-based management of patients with gastrointestinal symptoms in patients after pelvic radiation treatment (ORBIT): A randomised controlled trial. Lancet. 2013;382:2084–2092. doi: 10.1016/S0140-6736(13)61648-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.