Abstract
Major hindrances to controlling the current childhood obesity epidemic include access to prevention and/or treatment programs that are affordable, provide minimal barriers for participation, and are available to the general public. Moreover, successful childhood obesity prevention efforts will require coordinated partnerships in multiple sectors such as government, health care, school/afterschool, and the community but very few documented sustainable programs currently exist. Effective, community-based health and wellness programs with a focus on maintaining healthy weight via physical activity and healthy eating have the potential to be a powerful referral resource for pediatricians and other healthcare professionals who have young patients who are overweight/obese. The Miami Dade County Department of Parks, Recreation and Open Spaces in partnership with the University of Miami UHealth Systems have created a “Park Prescription Program (Parks Rx 4HealthTM)” that formally coordinates pediatricians, families, parents, caregivers, and child/adolescents to provide daily obesity-prevention activities. This Parks Rx 4HealthTM program that we describe here allows UHealth pediatricians to seamlessly refer their overweight and obese patients to Fit2PlayTM, an evidence-based, park-based afterschool health and wellness program. Measurable outcomes that include body mass index, blood pressure, fitness, and nutrition knowledge are being collected at baseline and at 3-and 6-mo after referral to document patient progress. Results are then shared with the referring physician so they can follow up with the patient if necessary. Identifying successful models that integrate primary care, public health, and community-based efforts is important to accelerating progress in preventing childhood obesity. Effective, community-based health and wellness programs with a focus on physical activity and nutrition education could be a powerful referral resource for pediatricians who have obese patients.
Keywords: Obesity, Overweight, Prevention, Community-based, Children, Adolescents, Primary care
Core tip: Childhood obesity continues to be a vexing clinical and public health challenge and is an epidemic that will not be solved in silos. Instead, coordinated, collective partnerships in multiple sectors such as government, health care, school/afterschool, the family, and the community give the most promise for sustainability of healthy weight in children and adolescents. The described Parks Rx 4HealthTM program will enhance care coordination among pediatricians, families and community-based providers to encourage and monitor overweight/obese youth. It will be increasingly important to capitalize on existing resources such as local park systems to conduct prevention efforts to lower current obesity and related comorbidity trends.
INTRODUCTION
The United States (US) Department of Health and Human Services’ Healthy People 2020 Nutrition and Weight Status health indicator’s goal is to “promote health and reduce chronic disease risk through the consumption of healthful diets and achievement and maintenance of healthy body weights”[1]. This initiative identifies the reduction of overweight/obesity during childhood as 1 of 10 leading public-health priorities, yet the prevalence of childhood overweight/obesity in the US continues to be a vexing public health and clinical issue, especially among ethnic minorities and low income underserved subgroups who are at increased risk for adult onset type 2 diabetes and cardiovascular disease[2,3]. For obesity prevention efforts to be successful will require coordinated, collective partnerships in multiple sectors such as government, health care, school/afterschool, workplace, and the community, yet very few sustainable programs currently exist[4].
While coordination of care for childhood obesity prevention efforts are desperately needed, they are severely lacking. Primary care providers (PCPs, such as physicians, physician’s assistants, nurse practitioners, and/or registered nurses working in a primary care setting) and professionals working in out-of-school/afterschool-based settings have important roles in meeting national and international obesity prevention goals. PCPs traditionally measure patients’ growth and development and treat obesity and health-related conditions, but there is a recognized need to expand these roles to include advocacy, counseling, and referring patients and their families to community-based resources, and communicating with these community-based referrals about patient participation and progress[5,6].
The institute of medicine (IOM) in its 2012 report “Accelerating progress in obesity prevention”[7] includes the goal to “expand the role of health care providers in obesity prevention”. Health care providers/PCPs have a role in the following strategies recommended by the IOM to achieve this goal: (1) strategy 4-1: Provide standardized care and advocate for healthy community environments; (2) strategy 4-2: Ensure coverage of, access to, and incentives for routine obesity prevention, screening, diagnosis, and treatment; and (3) strategy 4-3: Encourage active living and healthy eating[7]. Similarly, the US preventive services task force recommendation statement says “PCPs should offer or refer children aged 6 years and older to intensive counseling and behavioral interventions to promote improvements in weight status”[8].
While the physician’s role in the identification and recruitment of children and families into obesity prevention or treatment interventions is often cited as important, the literature is limited in terms of existing models that are effective and sustainable. Published studies include primarily family-based counseling and treatment programs, lasting from eight weeks to a few months and include group education sessions for parents and children, home visits, follow-up telephone calls, automated messages, and/or other family-oriented activities[4,9]. Very few incorporate any technology enhancements (e.g., computer/tablet Parks Rx 4HealthTM registration, tablet/phone data entry capabilities, healthy text messaging programs) that encourage bi-directional communication between PCPs, families and community-based providers to track progress and attendance, and are designed for low income, ethnic minority groups in particular[10,11]. Yet studies report that parents perceived the community-based program as an extension of their pediatrician’s care due to the physician-referral of the program, and follow-up monitoring and care with patients[4] .
Park-based afterschool programs have the potential to be an ideal setting for childhood obesity-prevention PCP referrals. How the existence of community parks and their health and wellness programming is related to overall physical activity levels and health of its residents is just now gaining attention in the literature[12]. Another area of interest nationally is the concept of a “park prescription” program that links the healthcare system and public lands, such as local parks, to create healthier people[13,14]. However, none of these programs to date have: (1) linked PCPs to evidence-based programming in childhood obesity prevention efforts; and (2) have incorporated technology to create bidirectional communication between PCPs and community providers to track patient progress.
To answer the need for affordable and accessible obesity prevention and treatment programs in the community, the University of Miami Miller School of Medicine’s (UMMSM) Department of Pediatrics and the Miami Dade County Department of Parks, Recreation and Open Spaces (MDPROS) have collaborated over the past 8 years to successfully develop “Fit2PlayTM”, a 10-mo (entire school year) afterschool health and wellness program that is available to over 1500 low income, urban and suburban children annually at 35 parks in Miami Dade County (approximately 48% Hispanic, approximately 48% non-Hispanic black, mean age 9.3 years). Fit2PlayTM provides the ideal PCP-referral given its (1) evidence-based results[15-17]; (2) accessibility; it is offered in multiple locations (35 park locations all over the county); (3) affordability (can be free or sliding scale based on household income but not to exceed $35/wk, which is considerably less than comparable non-evidence based programs offered locally); and (4) acceptability and endorsement by our UMMMSM physicians for referrals. We describe below the formal Park Prescription (Parks Rx 4HealthTM) model that has been developed from this Fit2PlayTM evidence-based work.
STUDY METHODS
Study design
We are currently/prospectively conducting a Parks Rx 4HealthTM pilot study that will include a total of 50 families who visit UMMSM Pediatric Clinics (general pediatrics or pediatric endocrinology) and are referred to, and enrolled in the Fit-2-PlayTM afterschool program. During this pilot phase, the program is free to families that participate and is financially underwritten and trademarked by MDPROS. This study has been approved by the University of Miami Institutional Review Board. We describe the methods for this program in detail below.
Participants
The UMMSM Pediatric Clinics serve a very rich racially and ethnically diverse population of overweight/obese patients (approximately 1 out of every 3 and 1 out of every 2 ethnic minority patients are overweight/obese). Pediatricians ask patients if they are interested in participating in the Park Rx program if they meet the following inclusion criteria: (1) Child is between the ages of 6 and 14; (2) child body mass index (BMI) percentile is ≥ 85th %ile for age and sex[18], is physically inactive, has systolic and/or diastolic pre-hypertension or hypertension, or has a strong family history of type 2 diabetes and/or cardiovascular disease; (3) parent is willing to enroll their child in a Fit-2-PlayTM program that is located close to their child’s school or home and have them attend 5 d/wk (transportation provided); and (4) parent consent for child to participate. If a child has a medical condition that excludes them from the physical fitness testing component of the study then they are not referred to Fit-2-PlayTM.
PROCEDURES
Initial referral process
Pre-Parks Rx 4HealthTM program roll out focus groups among pediatricians identified the initial referral process as a critical point of buy-in for medical team members. They stated that if they had to pick just one key strategy that would increase program success, it would be that the in-house clinical referral process must be (1) seamless; (2) simple; and (3) short (no more than 1 min). Hence, an official Park Prescription website “landing page” was developed (Available from: URL: http://www.miamidade.gov/parks/rx4health.asp) that was loaded on all desktop computers in each patient room. This site can also be accessed via tablet, mobile phone, or laptop computer. This page gives specific information on park location, times, and how to live a heart-healthy life. Once the parent chooses the most convenient park location, the physician and family fill out a brief online registration form together (Available from: URL: http://www.miamidade.gov/parks/rx4-contact-form-youth-um.asp) that includes basic patient information. This preliminary registration form is sent electronically to the MDPROS wellness team (a centralized team of 6 health and wellness specialists/coaches). In turn, this team (1) within 24 h verifies that patient has been registered with Fit2PlayTM at the pre-identified park; (2) calls and emails/texts each parent with a welcome message; and (3) provide further assistance necessary to complete the registration process. Parents leave the pediatrician’s office with additional materials describing the details of the program and MDPROS Health and Wellness staff contact information.
Tracking of patients throughout their enrollment in Fit2PlayTM
All Park Prescription children have a baseline, 3- and 6-mo assessment battery completed (measurements described in detail below) by the park health and fitness team. In addition, children and parents receive encouraging text messages and emails from both their pediatricians and park coaches as they meet program milestones. Daily attendance is also recorded.
Description of Fit2PlayTM afterschool program physical activity and health and wellness/nutrition education components
Fit2PlayTM includes (1) 50-60 min of physical activity that incorporates multiple sports (soccer, kickball, flag football, dodgeball) and activities from Sports, Play and Active Recreation for Kids[19,20], an evidenced-based, outcome oriented structured active recreation program for children with a focus on developing and improving motor skills, movement knowledge, and social and personal skills; and (2) a health and wellness/nutrition education component where children participate in 30 min education lessons 1-2/times per week that incorporate EmpowerMe4Life[21], a nutrition education curriculum grounded in the American Heart Association’s scientific recommendations in promoting heart-healthy lifestyles. This curriculum promotes being several health messages (physical activity, nutrition, sleep, screen time) and has been expanded over the years to include modules for younger (ages 6-9) and older (ages 10-14) participants that include more in-depth materials.
Closing the communication loop between pediatricians and community-based providers
Every three months, pediatricians receive a patient “report card” (Figure 1) on primary clinical outcome measurements including height, weight and blood pressure. MDPROS Park Health and Wellness staff also include attendance numbers for the pediatrician’s review. MDPROS Parks Rx 4HealthTM software is pre-programmed to assist with a 6-mo pediatrician follow-up visit and sends pediatrician, parent and park staff scheduling reminders. This entire referral and follow-up process is shown visually in Figure 2.
Figure 1.
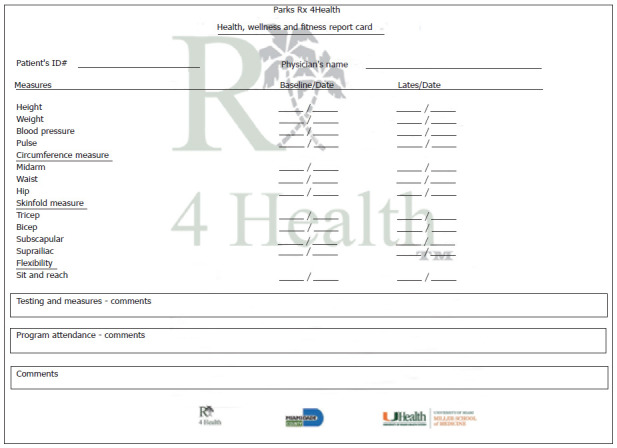
Park Rx 4HealthTM participant health report card.
Figure 2.
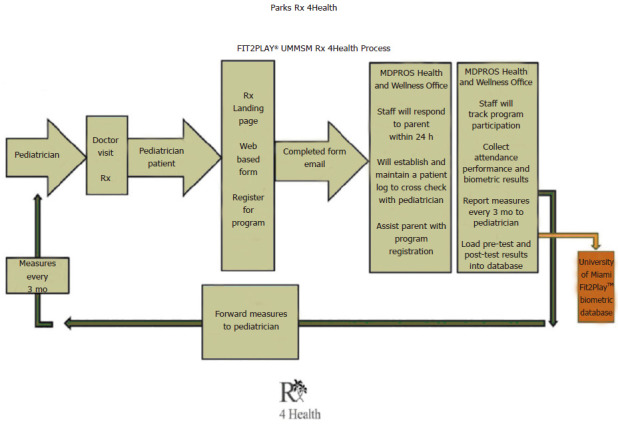
Park Rx 4HealthTM project flow.
MEASURES
Individual-level measures
MDPROS Parks Rx 4HealthTM software is programmed to collect/track the following measures on the children referred to Fit2PlayTM:
Demographic questionnaire: A baseline questionnaire captures (1) age, sex, and race/ethnicity for children and parents; (2) parent medical history; and (3) any other relevant medical and/or personal history (e.g., previous sports injuries, allergies); all of the following measures are taken at baseline and at the follow-ups.
Height and weight: Height (by stadiometer) and weight (by digital scale) are converted to age and sex adjusted BMI scores and percentiles[18,22].
Waist and hip circumference: Waist and hip circumferences are measured to the nearest 0.1 cm using a non-stretchable plastic tape measure by a standard method[23]. Waist circumference is measured over the navel at the end of gentle exhalation and hip circumference is measured at the maximum circumference over the buttocks. A total of three waist and hip circumference measures are taken for each child and the average used for the analysis.
Skinfold measurements: Bicep, triceps, subscapular, and suprailiac skinfold thicknesses are measured to the nearest 0.1 mm following standard procedures[22]. These 4 thickness values are combined and analyzed using the Durnin formula to estimate percent body fat[24].
Blood pressure: Blood pressure is taken using the American Heart Association Guidelines[25]. Each child has a total of 3 blood pressure measurements taken where the first one is dropped and the second two are averaged for analysis[26].
Physical fitness: The following battery of physical fitness tests[27] is conducted: (1) Sit and Reach[28]. The child sits on the floor with legs extended straight in front. Feet are placed against the front of the test box and are approximately 6 inches apart. The subject extends the arms forward, placing the index fingers of both hands together with knees straight. The score is the most distant point reached by the fingertips in the best of 3 trials; (2) Progressive Aerobic Cardiovascular Endurance Run (PACER) test[29]. The PACER test is a maximal aerobic fitness test and is a timed fitness run test. The test involves continuous running between the two lines in time to recorded beeps. The time between recorded beeps decrease each minute (level) requiring an increase in pace. The subjects continue until they are unable to keep pace with the beeps. Participants are compared to established national standards; (3) Timed Sit-ups[27]. For the sit-up test the child lies with knees bent and arms across the chest. The participant will complete as many sit-ups as possible in the 60 s allotted time period; (4) Timed Push-ups[27]. For the push-up test the participant completes as many push-ups as possible in the 60 s allotted time period; and (5) 400 Meter Run[27]. Shorter distance runs are included as options for younger children. Younger children can be prepared to run the mile (6-7 year olds - ¼ mile; 8-9 years old - ½ mile).
Mental health measures: The following 3 assessments are administered at initial enrollment and at the end of the school year or at the 6-mo follow-up only; (1) Rosenberg Self Esteem Scale[30], a simple 10 item questionnaire asking participants on a 4-level Likert Scale about how they feel about themselves. Self-esteem is one measure of a children’s overall mental health; (2) Social Anxiety Scale for Adolescents[31], a 22-item questionnaire that assesses participant’s level of social anxiety (how much they worry about what others think of them, etc.). Social anxiety disorder is common among youth, often emerging during adolescence and the benefits of participating in a park-based group afterschool program have not been previously described; and the (3) pediatric Quality of Life Inventory™[32] that assesses how the participant currently feels about their overall quality of life. The utility of pediatric quality of life measurement in population health outcome evaluation from the perspective of children in large pediatric populations has several distinct benefits beyond the clinical setting but has been largely unexplored in a park-based setting.
Process measures
Process measures are a priority as they are key in tracking the uptake of implementation (Table 1). Data are collected from pediatricians, park health and wellness specialists/coaches, and families (parents and child participants) by observations, self-report satisfaction surveys, focus groups, questionnaires and process surveys.
Table 1.
Abbreviated reach, effectiveness/efficacy, adoption, implementation, and maintenance item(s) and methods/approach/ measure
| Study topic area: Childhood obesity prevention via coordination of care, Parks Rx 4HealthTM | Study setting: Pediatric Primary Care Clinics, MDPROS-based afterschool Fit2PlayTM program |
| Dimensions/item | Method/approach/measure |
| Reach | |
| Characteristics of participants compared to non-participants or to target population | Proportion of family/patient referrals who register for Fit2PlayTM, continue to participate for entire 6 mo Proportion of pediatricians who make referrals via Parks Rx 4HealthTM |
| Effectiveness | |
| Measure of primary outcome with or w/o comparison to a public health goal | Proportion of youth participants who improve in above listed individual measures (BMI, BP, fitness, etc.) |
| Measure of broader outcomes (e.g., other outcomes, measure of life improvements, or potential negative outcome) | Mean improvement of cardiovascular health, physical activity levels, anthropometrics; satisfaction with Parks Rx 4HealthTM program |
| Adoption-setting level | |
| Characteristics of settings participating (comparison and intervention) compared to either: non participants or relevant resource data | Overall satisfaction with Parks Rx 4HealthTM program (pediatrician referral process, Fit2PlayTM program, family/child Fit2PlayTM participants/completers vs non-completers) |
| Use of qualitative methods to understand adoption at setting level | Focus group with pediatricians, park coaches and children; process evaluation with pediatricians, park coaches and parents |
| Implementation | |
| Percent of perfect delivery (adherence or consistency) | Pediatrician and Parent Satisfaction Survey, Parks Rx 4HealthTM adherence measure |
| Adaptations made to intervention during study | Focus groups with pediatricians and park coaches at end of study |
| Maintenance - individual level | |
| Measure of primary outcome at follow-up after final intervention contact | Proportion of children participants who continue in Fit2PlayTM Proportion of pediatricians who make Parks Rx 4HealthTM referrals |
| Qualitative data to understand long -term effects | Pediatrician, Family and Park Health and Wellness Coaches Satisfaction Survey |
| Maintenance - setting level | |
| Program is ongoing at ≥ 6 mo post-study funding | Proportion of pediatricians using Parks Rx 4HealthTM 3-mo post-pilot phase |
| Some measure/discussion of alignment to organization mission or sustainability | Adoption of Parks Rx 4HealthTM program by the National Recreation and Park Association, promotion by the American Academy of Pediatrics |
MDPROS: Miami Dade County Department of Parks, Recreation and Open Spaces; BMI: Body mass index.
It is critical that obesity prevention coordination efforts are guided by a clear framework. The reach, effectiveness/efficacy, adoption, implementation, and maintenance (RE-AIM) framework, highly compatible with development of community-based public health interventions[33-37] is used to guide our integration and dissemination of the Parks Rx 4HealthTM program. The dimensions of the framework, (1) reach (the absolute number, proportion, and representativeness of individuals who are willing to participate); (2) effectiveness (impact of an intervention on outcomes, including potential negative effects, quality of life, and economic outcomes); (3) adoption (absolute number, proportion, representativeness of settings and intervention agents willing to initiate a program); (4) implementation (intervention agents’ fidelity to various elements of an intervention’s protocol including consistency of delivery as intended, intervention time and cost); and (5) maintenance (extent to which a program/policy becomes institutionalized or part of the routine organizational practices and policies, but also has individual-level outcomes) all have applicability to the Parks Rx 4HealthTM program.
RE-AIM was initially designed to help evaluate interventions and public health programs, to produce a more balanced approach to internal and external validity, and to address key issues important for dissemination and generalization[33]. RE-AIM has been applied to policies[34,35] and community-based multilevel interventions[36], and to reduce health disparities in previous studies[37]. Within this framework, it has been recommended that childhood obesity interventions use multiple disciplines and perspectives in creating and implementing programs, integrate research and practice partnerships, and assess the potential of intervention strategies to reduce health disparities[36,37]. To date, the complexity of the community-based childhood obesity prevention intervention implementation process has not been well-studied or understood, especially in highly diverse communities. This is true particularly in low resource setting and for populations traditionally underrepresented in obesity prevention research, for which dissemination and implementation may not be a simple process, particularly when multiple entities are involved (PCPs, community-based programs, families)[37].
Data analysis
Proportions and means are the primary scales of the dependent outcomes used to evaluate program outcomes. While not the only statistical approach available, we chose to use the generalized linear model (GZLM) to model the impact of the Parks Rx 4HealthTM program for all the dependent effects. We chose this specific approach because much like the general linear model that allows for variation in type and scale characteristics of the independent effects, the GZLM extends this versatility to include various types of dependent variables. Rather than applying different statistical techniques based on the scale properties of the dependent variables (e.g., analysis of variance for continuous data, contingency tables for proportion, etc.), the GZLM model accounts for the scale type of the dependent variable via model specification. The relationship between the independent variables and the dependent outcomes are specified by way of a link function that defines the functional form of this relationship (e.g., when the dependent variable is a proportion, a logistic link function might be used). Through different specifications of the link and probability functions, one generalized model is used to examine the statistical relationships between the design parameters (i.e., independent variables) and the dependent variables, regardless of their scale properties. Additionally, statistical consideration is given to repeated measures which needs to be considered in the current Park Rx 4Health model. One of the major benefits of the program to pediatricians is that they can track how their patient is doing in the program throughout the school year and thus they request multiple data collection time points. Although an additional independent factor (i.e., time) can be included in the GZLM (i.e., generalized mixed model), the results may be better interpreted when analyzed as separate short and long-term models. This is an important issue in the current model, because the time lapse between the pre- and post-test measurement will vary by patient, and thus the introduction of an interim value may be important.
Measures taken at baseline will be included in the GZLM as covariates to insure pretest balance and as a control on regression to the mean. In studies involving weight loss or change, initial weight is a covariate that is often included in the statistical model since weight gain or loss is correlated with initial values. This dictates a statistical approach to the data analysis which accounts for the difference scores from baseline to post-treatment measurements as the dependent outcome using the baseline measurement as the covariate. SAS and JMP (SAS Institute, Cary, NC) are the primary statistical software packages used for all analyses.
Quality control
To ensure Park Rx program quality control, the following strategies are implemented: (1) MDPROS field staff are properly trained in standardized Parks Rx 4HealthTM methods of outcome measures and data collection; (2) activities, personnel, data and the database are well-organized and maintain proper documentation; and (3) all required reports to physicians are delivered in a timely manner. Appropriate data safety checks are conducted prior to, during, and after the completion of data collection activities such as adding upper and lower bounds to the possible ranges of outcome variables to decrease the incidence of data entry error. Prior to the initiation of any data collection, pilot runs involving measurement and data collection and entry mockups are used to establish process capability. Finally, MDPROS field teams conduct weekly field audits to ensure that all Parks Rx 4HealthTM data are recorded correctly and completely.
Lessons learned
There have been many important lessons learned as we continue in our roll out pilot phase of the UMMSM-MDPROS Parks Rx 4HealthTM program. At both a pre- and 4-mo follow-up focus group, our pediatrician team emphasized the importance of (1) a seamless and quick referral process and (2) receiving follow-up information on their patients to keep them engaged in the program. Because it is typical for a pediatrician to see their patients only once a year, the Parks Rx 4HealthTM program provides a significant incentive for their participation to learn about not only if they are consistently engaging in a healthy weight program, but they are gaining health benefits as well.
Another critical lesson learned is the importance of fluid team communication among the clinical, research and parks team members. During the first week of Parks Rx 4HealthTM roll out, the pediatrician team was experiencing a technical difficulty with the web-based registration form. This was quickly resolved by the MDPROS team through one simple telephone call. Communication between MDRPOS staff and Parks Rx 4HealthTM families and their children is also a critical component of program success. Parents like to hear their children are enjoying the program, and improving their health, as supported by their family pediatrician. Our Parks Rx 4HealthTM children like to hear they are doing well and enjoy being encouraged daily to pursue personal health goals.
Future plans
Our UMMSM-MDPROS Parks Rx 4HealthTM program will begin Phase II with summer 2016 referrals for the 2016-2017 school year. Additional components that will be included in this phase are (1) a 2-min video loop that will play in all patient rooms for parents/families to view that will feature children participating in Fit2PlayTM and describe their experiences during the program; (2) weekly nutrition and health and wellness materials that will go home on Fridays with Parks Rx 4HealthTM participants. Each week will feature one key nutrition and/or physical activity message; (3) the expansion of the UMMSM-MDPROS Parks Rx 4HealthTM website to include supplemental health and wellness materials and resources for families to access at any time; (4) family-based activities on weekends and after hours that both parents and children can participate in as a family. This is one of the major advantages of conducting such a program in a large urban parks system; the variety of activities available at minimum to no-cost while enjoying nature and the outdoors; and (5) the option of a consultation visit with a UMMSM faculty member to discuss family health and wellness goals and strategies to meet these goals.
Another area of scientific interest to the team is the contribution of genetics vs environment to the current childhood obesity epidemic, particularly because our patient population is so ethnically diverse and most have family origins from outside the United States. Genome-wide association studies in pediatric populations have produced evidence to indicate a genetic component involvement in the occurrence and development of obesity[38-41]. In particular, the fat mass and obesity-associated gene (FTO) has received increased attention for being associated with the development of obesity[42]. A recent meta-analysis of 12 studies (that included 5000 cases and 9853 controls) has shown that the FTO rs9939609 polymorphism is associated with the increased risk of obesity among children and adolescents[43]. However, the major proportion of study subjects were Caucasian, and FTO polymorphism have actually been shown to not affect BMI or the risk of obesity in African Americans[41], a population who has been consistently shown to be at greater risk for obesity vs Caucasians[2,3]. Given that the overwhelming majority of Park Rx 4Health patients are not Caucasian, and about half are non-Hispanic black, one must consider that the patient’s environment is having a greater impact on their weight than their genetic predisposition. For example, studies have shown that physical activity (vs sedentary behavior) counters the genetic predisposition to obesity[44]. These findings have major implications to the Park Rx 4Health program because its referral program Fit2PlayTM has daily non-stop physical activity as its cornerstone. So, perhaps if we do capture patients with a genetic predisposition to obesity we can influence a gene-environment interaction by keeping them consistently physically active during the pediatric years. While the literature on obesity-related gene-environment interactions is still immature, it will no doubt be an area of much scientific inquiry in the future as obesity continues to spread around the globe.
Park Rx 4HealthTM impact
Our UMMSM-MDPROS Parks Rx 4HealthTM program described here will move us closer to accomplishing the following Healthy People goals set by the State of FL: Goal 1: Help all children meet their full potential (“making sure children develop healthfully with regard to height, weight, etc.); Goal 2: Reduce mortality and morbidity in children (particularly from such chronic diseases as type 2 diabetes and cardiovascular disease); and Goal 3: Reduce disparities in child health outcomes[1]. Moreover, Section 4004(i) of the Affordable Care Act requires the Department of Health and Human Services to provide guidance to States regarding preventive and obesity-related services available to individuals enrolled in Medicaid/Children’s Health Insurance Program[45]. It also requires States to design public awareness campaigns to educate Medicaid enrollees, as well as those with other insurance carriers on the availability and coverage of such services. The Park Rx 4HealthTM program described here can help close the gap between patient needs and prevention service providers[46].
CONCLUSION
Identifying successful models that integrate primary care, public health and community-based efforts is important to accelerating progress in preventing childhood obesity. Effective, community-based health and wellness programs with a focus on physical activity and nutrition education could be a powerful referral resource for pediatricians who have obese patients.
Footnotes
Conflict-of-interest statement: No conflicts-of-interest to report for any authors.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Pediatrics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: April 29, 2016
First decision: May 13, 2016
Article in press: June 3, 2016
P- Reviewer: Sergi CM, Watanabe T S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
References
- 1.Office of Disease Prevention and Health Promotion. Disability and Health. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=9.
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011-2012. NCHS Data Brief. 2013;(131):1–8. [PubMed] [Google Scholar]
- 4.Vine M, Hargreaves MB, Briefel RR, Orfield C. Expanding the role of primary care in the prevention and treatment of childhood obesity: a review of clinic- and community-based recommendations and interventions. J Obes. 2013;2013:172035. doi: 10.1155/2013/172035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 6.Barlow SE, Dietz WH, Klish WJ, Trowbridge FL. Medical evaluation of overweight children and adolescents: reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110:222–228. [PubMed] [Google Scholar]
- 7.Committee on Accelerating Progress in Obesity Prevention and Institute of Medicine. Accelerating progress in obesity prevention: Solving the weight of the nation. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 8.Barnes M. Solving the problem of childhood obesity within a generation. Whitehouse Task Force on Childhood Obesity. 2010. [DOI] [PubMed] [Google Scholar]
- 9.Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr. 2007;19:354–361. doi: 10.1097/MOP.0b013e328151c3e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gance-Cleveland B, Gilbert LH, Kopanos T, Gilbert KC. Evaluation of technology to identify and assess overweight children and adolescents. J Spec Pediatr Nurs. 2010;15:72–83. doi: 10.1111/j.1744-6155.2009.00220.x. [DOI] [PubMed] [Google Scholar]
- 11.Khaylis A, Yiaslas T, Bergstrom J, Gore-Felton C. A review of efficacious technology-based weight-loss interventions: five key components. Telemed J E Health. 2010;16:931–938. doi: 10.1089/tmj.2010.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.West ST, Shores KA, Mudd LM. Association of available parkland, physical activity, and overweight in America’s largest cities. J Public Health Manag Pract. 2012;18:423–430. doi: 10.1097/PHH.0b013e318238ea27. [DOI] [PubMed] [Google Scholar]
- 13.Institute at the Golden Gate. Park Prescriptions. Profiles and resources for good health from the great outdoors [retrieved. 2016. p. Jan 9]. Available from: http://www.parksconservancy.org/assets/programs/igg/pdfs/park-prescriptions-2010.pdf. [Google Scholar]
- 14.National Recreation and Park Association. Park Prescriptions [retrieved 2016 Jan 9] Available from: http://www.nrpa.org/Grants-and-Partners/Recreation-and-Health/Park-Prescriptions/
- 15.Messiah SE, Diego A, Kardys J, Kirwin K, Hanson E, Nottage R, Ramirez S, Arheart KL. Effect of a park-based after-school program on participant obesity-related health outcomes. Am J Health Promot. 2015;29:217–225. doi: 10.4278/ajhp.120705-QUAN-327. [DOI] [PubMed] [Google Scholar]
- 16.Haney K, Messiah SE, Arheart KL, Hanson E, Diego A, Kardys J, Kirwin K, Nottage R, Ramirez S, Somarriba G, et al. Park-based afterschool program to improve cardiovascular health and physical fitness in children with disabilities. Disabil Health J. 2014;7:335–342. doi: 10.1016/j.dhjo.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Messiah SE, Arheart KL, Somarriba G, Diego A, Kardys J, Kirwin K, Hansen E, Nottage R, Ramirez S, Armstrong JH. How one of our nation’s greatest resources can help children maintain healthy weight and cardiovascular fitness: It starts in the parks (Feature platform presentation to the American Public Health Association Meeting; 2014 Nov 15-19. LA: New Orleans, 2014)! Available from: http//xueshu.baidu.com/s?wd=paperuri:(2f915938159918c25434e347a6ea8330)&filter=sc_long_sign&sc_ks_para=q=How+One+of+our+Nation's+Greatest+Resources+Can+Help+Children+Maintain+Healthy+Weight+and+Cardiovascular+Fitness:+It+Starts+in+the+Parks!&tn=SE_baiduxueshu_c1gjeupa&ie=utf-8&sc_us=17266751060184562072.
- 18.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 19.McKenzie TL, Sallis JF, Rosengard P. Beyond the stucco tower: Design, development, and dissemination of the SPARK physical education programs. Quest. 2009;61:114–127. [Google Scholar]
- 20.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell MF. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, Play and Active Recreation for Kids. Am J Public Health. 1997;87:1328–1334. doi: 10.2105/ajph.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alliance for a Healthier Generation. [accessed 2016 Mar 8] Available from: http: //www.healthiergeneration.org.
- 22.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Anthropometry Procedures Manual (2007) Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf.
- 23.Chumlea NC, Kuczmarski RJ. Using a bony landmark to measure waist circumference. J Am Diet Assoc. 1995;95:12. doi: 10.1016/s0002-8223(95)00003-8. [DOI] [PubMed] [Google Scholar]
- 24.Durnin JV, Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974;32:77–97. doi: 10.1079/bjn19740060. [DOI] [PubMed] [Google Scholar]
- 25.Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, Mahoney L, McCrindle B, Mietus-Snyder M, Steinberger J, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433–451. doi: 10.1161/HYPERTENSIONAHA.108.190329. [DOI] [PubMed] [Google Scholar]
- 26.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 27.President’s Council on Physical Fitness and Sports. 1985 National School Population Fitness Survey. Washington, DC: US Department of Health and Human Services, Public Health Service, Office of the Assistant Secretary for Health; 1986. [Google Scholar]
- 28.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 29.La Greca AM, Lopez N. Social anxiety among adolescents: linkages with peer relations and friendships. J Abnorm Child Psychol. 1998;26:83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]
- 30.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Castro-Piñero J, Chillón P, Ortega FB, Montesinos JL, Sjöström M, Ruiz JR. Criterion-related validity of sit-and-reach and modified sit-and-reach test for estimating hamstring flexibility in children and adolescents aged 6-17 years. Int J Sports Med. 2009;30:658–662. doi: 10.1055/s-0029-1224175. [DOI] [PubMed] [Google Scholar]
- 32.Léger LA, Lambert J. A maximal multistage 20-m shuttle run test to predict VO2 max. Eur J Appl Physiol Occup Physiol. 1982;49:1–12. doi: 10.1007/BF00428958. [DOI] [PubMed] [Google Scholar]
- 33.Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health. 2013;103:e38–e46. doi: 10.2105/AJPH.2013.301299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jilcott S, Ammerman A, Sommers J, Glasgow RE. Applying the RE-AIM framework to assess the public health impact of policy change. Ann Behav Med. 2007;34:105–114. doi: 10.1007/BF02872666. [DOI] [PubMed] [Google Scholar]
- 36.Glasgow RE, Dickinson P, Fisher L, Christiansen S, Toobert DJ, Bender BG, Dickinson LM, Jortberg B, Estabrooks PA. Use of RE-AIM to develop a multi-media facilitation tool for the patient-centered medical home. Implement Sci. 2011;6:118. doi: 10.1186/1748-5908-6-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glasgow RE, Askew S, Purcell P, Levine E, Warner ET, Stange KC, Colditz GA, Bennett GG. Use of RE-AIM to Address Health Inequities: Application in a low-income community health center based weight loss and hypertension self-management program. Transl Behav Med. 2013;3:200–210. doi: 10.1007/s13142-013-0201-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dina C, Meyre D, Gallina S, Durand E, Körner A, Jacobson P, Carlsson LM, Kiess W, Vatin V, Lecoeur C, et al. Variation in FTO contributes to childhood obesity and severe adult obesity. Nat Genet. 2007;39:724–726. doi: 10.1038/ng2048. [DOI] [PubMed] [Google Scholar]
- 39.Loos RJ, Bouchard C. FTO: the first gene contributing to common forms of human obesity. Obes Rev. 2008;9:246–250. doi: 10.1111/j.1467-789X.2008.00481.x. [DOI] [PubMed] [Google Scholar]
- 40.Liu C, Mou S, Cai Y. FTO gene variant and risk of overweight and obesity among children and adolescents: a systematic review and meta-analysis. PLoS One. 2013;8:e82133. doi: 10.1371/journal.pone.0082133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scuteri A, Sanna S, Chen WM, Uda M, Albai G, Strait J, Najjar S, Nagaraja R, Orrú M, Usala G, et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet. 2007;3:e115. doi: 10.1371/journal.pgen.0030115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, Elliott KS, Lango H, Rayner NW, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316:889–894. doi: 10.1126/science.1141634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Quan LL, Wang H, Tian Y, Mu X, Zhang Y, Tao K. Association of fat-mass and obesity-associated gene FTO rs9939609 polymorphism with the risk of obesity among children and adolescents: a meta-analysis. Eur Rev Med Pharmacol Sci. 2015;19:614–623. [PubMed] [Google Scholar]
- 44.Andreasen CH, Stender-Petersen KL, Mogensen MS, Torekov SS, Wegner L, Andersen G, Nielsen AL, Albrechtsen A, Borch-Johnsen K, Rasmussen SS, et al. Low physical activity accentuates the effect of the FTO rs9939609 polymorphism on body fat accumulation. Diabetes. 2008;57:95–101. doi: 10.2337/db07-0910. [DOI] [PubMed] [Google Scholar]
- 45.Medicaid. gov. Keeping American healthy [accessed. 2016. p. Jan 20]. Available from: http://www.medicaid.gov/medicaid-chip-program-information/by-topics/quality-of-care/reducing-obesity.html. [Google Scholar]
- 46.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 Suppl 4:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]