Abstract
Introduction:
The action of nicotine to suppress body weight is often cited as a factor impacting smoking initiation and the failure to quit. Despite the weight-suppressant effects of nicotine, smokers and nonsmokers report equal daily caloric intake. The weight-suppressive effects of nicotine in animal models of smoking are poorly understood. Furthermore, the Food and Drug Administration has authority to implement a policy markedly reducing nicotine levels in cigarettes; such a reduction could reduce smoking behavior, but have detrimental effects on body weight. The aim of this investigation was to examine the effects of self-administered nicotine on body weight and food intake in rats.
Methods:
In Experiment 1, rats with ad libitum access to chow responded for intravenous infusions of nicotine (60 µg/kg/infusion) or saline in daily 1-hour sessions; body weight and 24-hour food intake were measured. Experiment 2 tested the effects of subcutaneous injections of nicotine on food intake. In Experiment 3, rats were food restricted and self-administered nicotine across a range of doses (3.75–60 µg/kg/infusion) while body weight was measured. In Experiment 4, rats self-administered 60 µg/kg/infusion nicotine before reduction to one of several doses (1.875–15 µg/kg/infusion) for 50 days.
Results:
Self-administered nicotine suppressed weight gain independent of food intake. In food restricted rats, self-administered nicotine dose-dependently suppressed body weight gain. In rats self-administering 60 µg/kg/infusion nicotine, dose reduction increased body weight.
Conclusions:
Self-administered nicotine, even at low doses, suppressed body independent of food intake; this may have important implications for nicotine reduction policy.
Implications:
The results of the present studies demonstrate that self-administered nicotine suppresses body weight independent of food intake in rats. Further, the present studies establish that self-administered nicotine suppresses body weight even at very low doses and that reduction of nicotine dose results in weight gain. These results have important implications for nicotine reduction policy.
Introduction
There is an inverse relationship between smoking and body weight, such that smokers weigh less than nonsmokers but gain an average of 10 pounds in the first year of abstinence.1,2 Many smokers cite weight loss as a primary reason for smoking and weight gain for the inability to quit.3–5
Nicotine is the primary psychoactive constituent in cigarettes and researchers have suggested that nicotine in cigarettes is most likely responsible for the body weight suppression observed in smokers.6–11 Studies utilizing rodent models have generally reported that nicotine exposure, primarily via subcutaneous continuous infusion or repeated daily injections, results in a dose-dependent suppression of body weight8,12 and decreased food intake.12–14 Despite reports that nicotine delivery can increase physical activity15,16 and metabolic rate,17 the body weight-suppressant effects of nicotine are generally discussed as secondary to a suppression of caloric intake.11 This conclusion, however, is at odds with data from the clinical literature suggesting that smokers and nonsmokers have equal daily caloric intake.18,19 The vast majority of experiments examining the effects of nicotine on food intake and body weight have utilized experimenter-administered nicotine, which can produce different effects than self-administered nicotine.20 However, few investigators have utilized self-administration procedures to examine the impact of nicotine on food intake or body weight.
The current experiments evaluated the impact of self-administered nicotine, across a range of doses, on body weight and food intake in adult male rats. Results demonstrated that self-administered nicotine suppressed body weight gain independent of food intake and this effect was observed at very low doses. An additional experiment investigated the impact of reducing nicotine dose on body weight; results revealed that reduction of nicotine dose from a large self-administered dose to very low doses resulted in substantial weight gain. These data are important in the context of a reduction of nicotine content in cigarettes, a potential approach to reducing the abuse potential of cigarettes.21 The current data provide novel insight into the consequences of nicotine on body weight and offer important implications for the impact of nicotine reduction policy on body weight regulation.
Methods
Subjects
Male Sprague-Dawley rats (Harlan Farms, IN, weighing between 200 and 300g upon arrival; approximately 7–9 weeks old) were housed individually in hanging-wire cages on a reverse light-dark 12:12 hour cycle (lights off at 07:00 AM) in a temperature-controlled facility (between 68 and 70°F). Rats had free access to standard rodent chow (Purina Rat chow 5001) and water, unless noted otherwise. All procedures were approved by the University of Pittsburgh Institutional Animal Care and Use Committee.
Drugs
Nicotine hydrogen tartrate salt (Sigma, St Louis, MO) was dissolved in 0.9% saline. Doses of nicotine used for self-administration were 1.875, 3.75, 7.5, 15, and 60 µg/kg/infusion, and for subcutaneous injection, the doses were 0.3 and 1.0mg/kg (expressed as freebase).
In a subset of experiments (Experiments 3 and 4), a cocktail of cigarette constituents was included in the intravenous nicotine solution. The selected doses of the cocktail of cigarette constituents were based on previous studies,22,23 and/or were indexed to a standard dose of nicotine, based on their relative concentrations in cigarette smoke, that supports robust self-administration behavior (30 µg/kg/infusion). The doses used in select self-administration studies were as follows: acetaldehyde (16 µg/kg/infusion), harman (0.1 µg/kg/infusion), norharman (0.3 µg/kg/infusion), anabasine and nornicotine (0.9 µg/kg/infusion), and anatabine, myosmine, and cotinine (0.09 µg/kg/infusion).
The pH of solutions was adjusted to 7.0 (±0.2) using a dilute sodium hydroxide solution. All solutions used in self-administration studies were passed through a 0.22 µm filter to ensure sterility. All intravenous infusions were delivered in approximately 1 second (0.1ml/kg/infusion). Subcutaneous injections were delivered at 1ml/kg.
Procedures
Surgery
After at least 7 days of habituation post-arrival, rats were anesthetized with isoflurane (2%–3% in 100% O2) and implanted with catheters into the right jugular vein, as described previously.24,25 Rats were allowed to recover for a minimum of 5 days before self- administration procedures. During the surgical recovery period, catheters were flushed once daily with 0.1ml sterile saline containing heparin (30U/ml), timentin (66.67mg/ml), and streptokinase (9.333U/ml). Thereafter, catheters were flushed with 0.1ml heparinized saline (10U/ml) and heparinized saline (30U/ml) containing timentin (66.67mg/ml) prior to and following the self-administration sessions, respectively.
Self-Administration
Thirty-eight operant chambers (30.5cm × 24.1 cm×21.0cm; ENV-008CT; Med-Associates) enclosed inside sound-attenuating chambers, equipped with two nose-poke holes located on the same wall (2.5cm in diameter and 5cm above the floor), two white stimulus lights (3.5cm in diameter, located 6.5cm above each nose-poke hole), a houselight, and a fan were used in the current studies. An infusion pump was located outside of each chamber, which delivered intravenous infusions during self-administration sessions through tubing connected to each rat’s catheter. This tubing was protected in a metal encasing, attached to a swivel system that allowed relatively unrestricted movement.
During daily (7d/wk) 1-hour self-administration sessions, fulfilling the required nose-poke responses into the active portal resulted in one infusion of nicotine. Infusions were accompanied by a 15-second cue light illuminated above the active nose-poke portal and an unsignaled 1-minute timeout, where responses were recorded but had no scheduled consequence. Throughout the 1-hour sessions, responses into the inactive nose-poke portal were recorded but had no consequences. In experiments that used food restriction (Experiments 2 and 3) the allotted food amount (20g/d) was in the home cage when the rat returned from its self-administration session. For self-administration studies, rats in nicotine groups included in analyses passed a patency test, which required displaying physical signs of ataxia within 5 seconds of intravenous injections of chloral hydrate (up to 60mg/rat) or methohexital (5mg/kg). In all experiments, baseline body weights were counterbalanced across drug groups.
Experiment 1: The Effect of Self-Administered Nicotine on Body Weight and Food Intake
Rats were implanted with intravenous catheters and assigned to self-administer nicotine (60 µg/kg/infusion, n = 11) or saline (n = 8). Rats weighed 316.6±2.1g at the start of self-administration. Rats were allowed to respond for drug infusions on a fixed-ratio (FR) 2 schedule of reinforcement for 20 consecutive days. Body weight was measured daily before the self-administration session. Food intake was measured daily over the 23-hour period in the home cage, accounting for spillage.
Experiment 2: The Effect of Subcutaneous Nicotine Injection on Food Intake
Given that the results of Experiment 1 are unexpected, the effect of subcutaneous injection of nicotine on food intake was measured in a separate group of rats to replicate previous reports.12–14 Rats weighing on average 362.8±2.7g were assigned to a group and injected with nicotine (0, 0.3, or 1.0mg/kg, s.c.; n = 8 per group) at the onset of the dark cycle. Food intake was measured 1, 3, 6, and 24 hours post-injection, accounting for spillage.
Experiment 3: The Effect of a Range of Self-Administered Nicotine Doses on Body Weight Under Mild Food Restriction
Given the results of Experiment 1, and that the majority of self-administration studies are performed in rats under mild food restriction,26 the effect of self-administered nicotine on body weight was analyzed from a previously reported experiment.27 All rats were food restricted to ~80% of their ad libitum intake (20g/d) at least 5 days before self-administration procedures began. Rats were randomly assigned to self-administer nicotine at one of five doses: 60 µg/kg/infusion (n = 65), 15 µg/kg/infusion (n = 17), 7.5 µg/kg/infusion (n = 15), 3.75 µg/kg/infusion (n = 12), or 0 µg/kg/infusion (n = 17). In this experiment, the nicotine solution contained a cocktail of constituents found in cigarette smoke. Each drug group differed by nicotine concentration, but the cocktail concentrations remained consistent across different nicotine doses. Rats weighed 268.7±1.5g on the first day of the experimental period. Rats acquired self-administration of nicotine on a FR1 for 1 day, FR2 for 7 days, and escalated to FR5 for the remainder of the study.27 Body weight was measured daily and evaluated for 20 days of self-administration.
To test the possibility that the addition of cigarette constituents could impact body weight regulation, a separate group of rats were food restricted (20g/d) and responded on an FR2 schedule of reinforcement for infusions of nicotine (60 µg/kg/infusion) without (n = 8) or with (n = 11) the cocktail described above, with one minor change. Examination of dosages selected in papers cited by Clemens et al.,22 the paper on which the original cocktail solutions were based, suggested that the concentrations of the anatabine and anabasine should be reversed.23 Thus, the cocktail solution contained 0.9 µg/kg/infusion of anatabine and 0.09 µg/kg/infusion anabasine, along with the other constituents. Average body weight at the start of self-administration was 298.1±4.9g. Body weight was measured daily and evaluated for 10 days of self-administration.
Experiment 4: The Effect of Nicotine Dose Reduction on Body Weight Gain
Body weight regulation following nicotine dose reduction was evaluated post hoc from a previously published study from our laboratory.28 Food restricted (20g/d) rats learned to self-administer infusions of nicotine (60 µg/kg/infusion + cocktail) for 17 days before immediate reduction of nicotine dose, with cocktail doses remaining constant, to one of the following doses: 15 (n = 10), 7.5 (n = 11), 3.75 (n = 11), 1.875 (n = 10), or 0 (n = 13) µg/kg/infusion. Rats responded on an FR5 schedule of reinforcement for the reduction phase of the experiment. Rats weighed 279.6±2.2g at the start of dose reduction. The control group remained on 60 µg/kg/infusion nicotine with cocktail, which is referred to as “Maintained” (n = 11).
Statistics
Data for each experiment were analyzed separately and are expressed as means ± SEM. All statistical analyses were performed using SPSS. Comparisons between drug group and session (self-administration experiments) or day (feeding experiments) were analyzed by mixed-design and repeated measures analysis of variance (ANOVA) tests to account for the within-subjects design of the experiments while testing for between-subjects effects of nicotine dose groups. In tests of repeated measures where Mauchly’s Sphericity tests were significant, the data were Greenhouse–Geisser corrected; degrees of freedom reflect this correction where appropriate. Correlations were assessed using a two-tailed Pearson’s correlation. The α-level for all tests was set at 0.05. Where appropriate, a Bonferroni adjustment was made to account for the comparison of saline control to many nicotine dose groups. The α-levels were adjusted to 0.0125 and 0.01 for Experiments 3 and 4, respectively, resulting in an overall type I error rate of 0.05.
Results
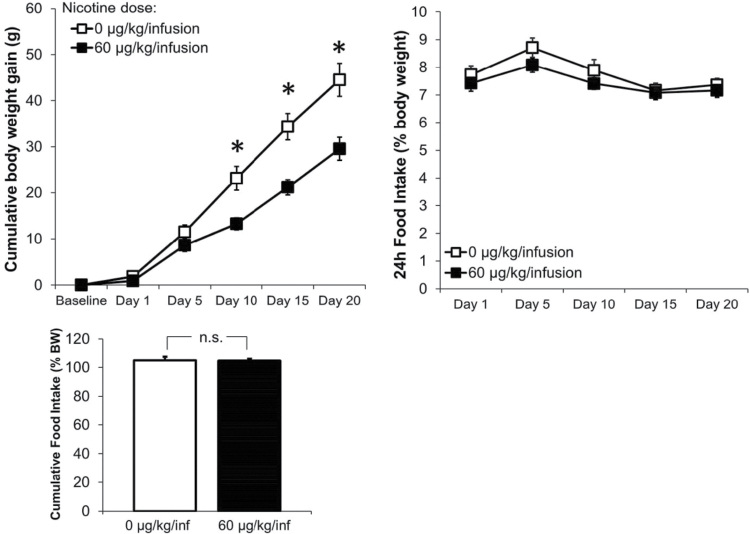
Experiment 1: Self-Administered Nicotine Suppressed Body Weight Gain but not Food Intake
Rats self-administering 60 µg/kg/infusion nicotine earned significantly more infusions (8.3±1.0; F 1,18 = 26.776, P < .001) than the saline group (1.9±0.3), averaged over the final 3 days of self-administration (Supplementary Figure 1). Self-administered 60 µg/kg/infusion nicotine suppressed body weight gain compared to intravenous infusions of saline (Figure 1). An ANOVA comparing groups on every fifth day revealed significant differences between groups on Days 10, 15, and 20 (Fs1,18 > 12.535, Ps < .003). There were no significant differences in food intake (expressed as a percentage of body weight) between nicotine and saline groups across days (P = .831, Figure 1). There were no differences in grams of food consumed between groups (P = .627; saline = 26.3±0.7g; nicotine = 24.5±0.7g on Day 20). Additionally, cumulative food intake during the 20 days of self-administration did not differ between groups when expressed as a percentage of body weight (Figure 1) or in total grams consumed (P = .105).
Figure 1.
Effects of self-administered nicotine on body weight and food intake. Body weight gain and food intake in rats that self-administered 0 (n = 11) or 60 (n = 8) µg/kg/infusion nicotine. Self-administered 60 µg/kg/infusion nicotine significantly suppressed cumulative body weight gain, but not 24-hour food intake, expressed as a percentage of body weight. There was no impact of self-administered nicotine cumulative food intake over the 20-day self-administration period. * indicate P < .05, between 0 and 60 µg/kg/infusion nicotine.
Experiment 2: Subcutaneously Administered Nicotine Suppressed Food Intake
The highest dose of nicotine tested, 1.0mg/kg, s.c., significantly suppressed food intake by approximately 10% at 3, 6, and 24 hours post-injection (Supplementary Figure 2). Repeated measures ANOVA revealed a significant effect of time (F 1.833,1 = 908.890, P < .001) with no significant interaction between time and drug group (P = .071); post hoc tests revealed significant differences between saline and 1.0mg/kg nicotine at 3, 6, and 24 hours (Ps < .006). There was no significant impact of 0.3mg/kg nicotine on food intake at any time point.
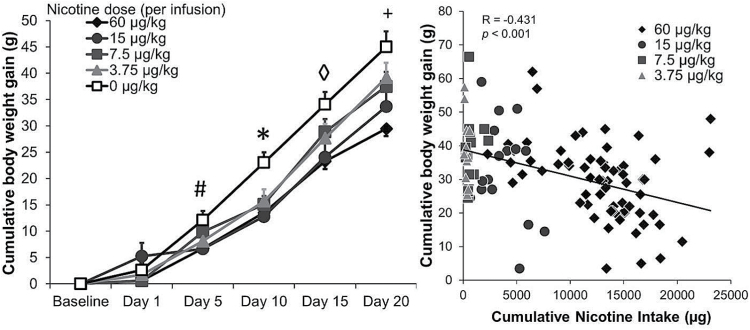
Experiment 3: Self-Administered Nicotine Suppressed Body Weight Gain When Food was Held Constant and Restricted
Self-administered nicotine dose-dependently suppressed body weight gain when food was held constant and restricted (Figure 2). Repeated measures ANOVA revealed a significant main effect of day (F 2.78,1 = 430.846, P < .001) and significant nicotine group by day interaction (F 11.121,4 = 3.702, P < .001). Comparisons between groups on every fifth day showed significant effects of nicotine group on Days 5, 10, 15, and 20 (Ps < .008). Analyses further revealed that saline was significantly different from: 60 µg/kg/infusion on Days 5, 10, 15, and 20; 15 µg/kg/infusion on days 10, 15, and 20; 7.5 µg/kg/infusion on Days 10 and 20; and 3.75 µg/kg/infusion on Day 10 (all Ps < .0125). Additionally, on Day 20, body weight gain in the 60 µg/kg/infusion group was significantly different from 0, 3.75, and 7.5 µg/kg/infusion groups (all Ps < .017). There was a significant negative correlation between cumulative nicotine intake and cumulative body weight gain (Figure 2; P < .001). It is noteworthy that total nicotine intake in this experiment is much higher than total nicotine intake reported in Experiment 1, which is likely explained by the differences in feeding status.29 Rats under food restriction acquire self-administration behavior more quickly and respond at higher rates.26 In a separate group of rats testing the impact of the addition of constituent chemicals on body weight regulation, there was no significant difference in body weight gain between no cocktail (25.8±8.5g) and cocktail groups (28.4±5.1g) after 10 days of self-administration (P = .99).
Figure 2.
Effects of a range of self-administered nicotine doses on body weight gain. Body weight gain in rats that self-administered 0 (n = 17), 3.75 (n = 12), 7.5 (n = 15), 15 (n = 17), or 60 (n = 65) µg/kg/infusion nicotine. In rats whose food intake was held restricted and constant, self-administered nicotine dose-dependently suppressed body weight gain. Across all doses, there was a negative correlation between cumulative nicotine intake and cumulative body weight gain on Day 20. # indicates 0 µg/kg/infusion different from 60 µg/kg/infusion, * indicates 0 µg/kg/infusion different from all nicotine doses, ◊ indicates 0 µg/kg/infusion different from 15 and 60 µg/kg/infusion, and + indicates 0 µg/kg/infusion different from 7.5, 15, and 60 µg/kg/infusion; all Ps < .0125.
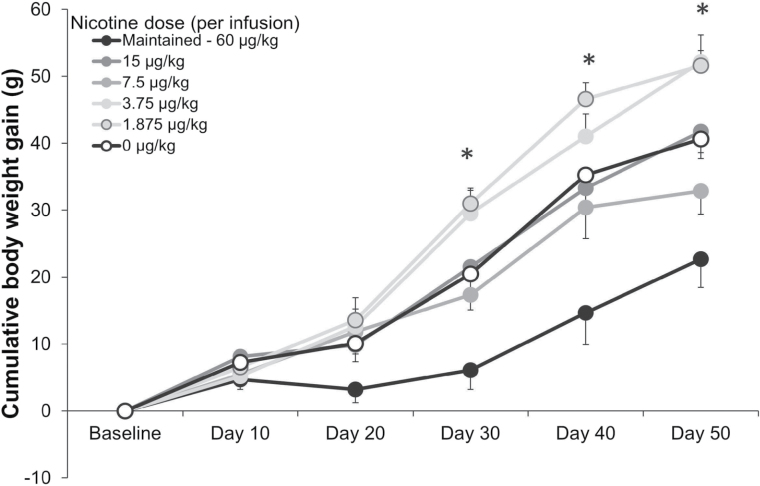
Experiment 4: Reduction of Nicotine Dose Results in Body Weight Gain Independent of Food Intake
Reduction of nicotine dose from 60 µg/kg/infusion caused significant weight gain compared to Maintained group (60 µg/kg/infusion) self-administration (Figure 3). Infusions earned in the 7.5 and 15 µg/kg/infusion were similar to the Maintained group following the reduction, but there was a significant reduction of infusions earned in all other groups, such that the 3.75 and 1.875 µg/kg/infusion groups responded similarly to saline.28 Repeated measures ANOVA revealed a main effect of day (F 2.753,1 = 145.818, P < .001) and a significant interaction between day and dose group (F 13.764,5 = 2.802, P = .001). Planned comparisons to identify differences between groups every 10th day revealed significant effects of groups on days 30, 40, and 50 (Ps < .002). Post hoc analyses showed that the Maintained group was significantly different from 1.875 and 3.75 µg/kg/infusion on Days 30, 40, and 50.
Figure 3.
Effects of nicotine dose reduction on body weight gain. Body weight gain in rats where dose was reduced from 60 µg/kg/infusion to: Maintained at 60 (n = 11), 15 (n = 10), 7.5 (n = 11), 3.75 (n = 11), 1.875 (n = 10), or 0 (n = 13) µg/kg/infusion nicotine. Reduction of nicotine dose resulted in significant increases in body weight gain compared to constant self-adminstration of 60 µg/kg/infusion nicotine. * indicates 60 µg/kg/infusion different from 3.75 and 1.875 µg/kg/infusion. All Ps < .01.
Discussion
The present data are the first to demonstrate that self-administered nicotine, across a range of doses, suppresses body weight independent of food intake. These data have important implications for the understanding of the impact of nicotine on body weight and for nicotine regulatory policy. The negative correlation between nicotine intake and body weight gain indicates that total nicotine exposure directly impacts body weight regulation. While it has been reported that smokers and nonsmokers have equal daily caloric intake,18 this is the first report to our knowledge of nicotine suppressing body weight independent of changes in food intake in a rat self-administration model.
The current data support the view that nicotine, at least when self-administered by adult male rats in daily 1-hour sessions, suppresses body weight without simultaneous decreases in food intake. These data differ from a large body of work demonstrating that nicotine suppresses body weight, with the common conclusion made that this is primarily driven by a reduction in food intake.12–14 Nearly all of these studies have used subcutaneous or intraperitoneal injection or continuous subcutaneous infusion of large doses of nicotine, beyond the range that rats would self-administer.30 It is typical that subcutaneous delivery of nicotine at a dose of 1.0–1.5mg/kg suppresses food intake.12,14 However, seminal work by Grunberg and colleagues8 reported that large doses of nicotine delivered via constant subcutaneous infusion in osmotic minipumps (4–12mg/kg/d) had no impact on food intake, though resulted in large, dose-dependent suppression of body weight. Furthermore, it is noteworthy that rats develop tolerance to the anorectic effects of daily subcutaneous injections of nicotine.31 While blood and brain nicotine levels and the time course of absorption differs between intravenous and subcutaneous delivery,30 the total amount of nicotine delivered may directly affect feeding behavior. Indeed, it is worth noting that the lowest dose of experimenter-administered nicotine that significantly suppressed food intake (1.0mg/kg, s.c.) is larger than the total amount of nicotine self-administered in a 1-hour session by rats fed ad libitum standard rodent chow (ranging from 0.2 to 0.8mg/kg daily). Additionally, noncontingent nicotine increases corticosterone (CORT) levels compared to self-administered nicotine.20 Elevation of CORT results in the suppression of food intake.32,33 Therefore, it is possible that increased CORT levels caused by noncontingent nicotine administration contributes to suppression of food intake, and the absence of this increased CORT during nicotine self-administration allows for the suppression of body weight with no effect on food intake.
To our knowledge, there are few reports on the effects of intravenously infused nicotine on feeding behavior. In contrast with the data presented here, the published studies used 23-hour extended access self-administration sessions in which rats were trained to respond for food (45mg pellets) in the operant chamber. In a report from Grebenstein et al.,34 noncontingent delivery of 60 μg/kg/infusion nicotine during extended access sessions suppressed body weight gain by ~50% and reduced the number of pellets consumed by approximately 20% over 23 hours. The suppression of food intake by noncontingent nicotine delivery may be directly related to the elevation of CORT following experimenter-administered nicotine, as mentioned above. In a more recent study, however, Bunney (nèe Grebenstein) et al.35 extended these results by demonstrating that self-administration of 60 μg/kg/infusion nicotine in 23-hour sessions suppressed chow pellet intake, replicating work by O’Dell and colleagues.36
The differences between the effects of self-administered nicotine on food intake in 1-hour limited access and 23-hour extended access sessions could be due to several reasons. First, total nicotine intake in 23-hour sessions is typically greater than in 1-hour sessions. In the extended access experiments described above, nicotine intake ranged from ~1.0 to 2.0mg/kg per day.34–36 It is possible that total nicotine exposure of at least 1.0mg/kg causes a suppression of food intake, as noted with the current subcutaneous experiment described above. Second, repeated nicotine infusions over 23-hour expose rats to many spikes in plasma nicotine levels over a prolonged time course each day. Feeding may be suppressed following each infusion only when plasma nicotine levels are high. Therefore, a suppression of daily food intake by intravenous nicotine is detectable in an extended access procedure, when plasma nicotine levels remain elevated for a longer time period and can contribute to a large cumulative reduction in food intake. However, in these 23-hour sessions, rats take the majority of their daily infusions during the active, dark phase.36 Grebenstein et al.34 report that the reduction in 23-hour food intake by nicotine is largely driven by suppression of food intake during the light cycle, making the possibility that spikes in nicotine plasma levels contribute to food intake suppression unlikely. Regardless, the magnitude of nicotine-induced food intake suppression reported34,35 cannot account for total amount of body weight gain suppression, indicating that intravenous nicotine exposure suppresses body weight gain independent of food intake, at least in part, in an extended access procedure.
There are several advantages of the use of limited access self-administration procedures. First, these procedures allow for the examination of the effects of self-administered nicotine on body weight and food intake in the absence of nicotine dependence and withdrawal. The current data are the first to demonstrate an impact of self-administered nicotine on body weight using a procedure that does not result in nicotine dependence. This is important, as it emphasizes that the effects of nicotine, and potentially nicotine reduction, on body weight will likely be observed in nondependent smokers. Second, utilization of the 1-hour self-administration procedure allows for examining the impact of nicotine on energy expenditure in the absence of changes in food intake. While it is clear a combination of changes in metabolism,17 physical activity,15,16 and potentially food intake,12–14,35,36 contribute to nicotine-induced suppression of body weight, no other procedure removes the suppression of food intake as a confound; this is critical as clinical literature indicates food intake of human smokers does not differ from nonsmokers.19 Third, the use of limited access procedures further demonstrates that the effects of self-administered nicotine are likely dependent upon the daily cumulative effects of nicotine and not singular, isolated spikes in plasma nicotine levels.
When food intake was restricted and held constant, as is standard in most self-administration procedures, self-administered nicotine resulted in a dose-dependent suppression of body weight. These data further emphasize that the body weight-suppressant effects of self-administered nicotine can occur independent of changes in food intake. Across all nicotine doses, there was a negative correlation between nicotine intake and body weight gain, indicating that nicotine exposure directly contributes to the magnitude of body weight suppression. We have previously reported that 3.75 μg/kg/infusion nicotine is subthreshold for reinforcement (ie, rats respond at a similar rate for 0 and 3.75 μg/kg/infusion) and that 7.5 μg/kg/infusion nicotine is at threshold, such that only approximately 60% of rats will acquire stable self-administration behavior.27 In rats that did not meet standard self-administration criteria at these low doses of nicotine, the nicotine delivered in the few infusions they received suppressed body weight gain. Rats in these groups received very low total daily doses of nicotine (ranging from 8.5 to 15 μg/kg daily), likely as a result of general exploratory behavior and not as a result of primary reinforcement. Therefore, it is likely that the threshold for body weight suppression by nicotine is lower than for reinforcement. These data suggest that doses below the threshold for primary reinforcement may still function to suppress body weight, potentially motivating continued use in weight-concerned smokers following the implementation of a nicotine reduction policy. These results are particularly important regarding the initiation of smoking, as such data from human smokers would become available following the implementation of FDA-mandated nicotine product standards.
Although it is generally accepted that nicotine is the primary constituent in cigarettes responsible for weight loss,11 we conducted an additional experiment to rule out the possibility that a cocktail of select constituents in cigarette smoke may have impacted the results of Experiments 3 and 4. This experiment compared weight gain in rats self-administering nicotine alone and nicotine in the presence of the additional constituents. There was no impact of the addition of the other cigarette constituents on body weight gain, indicating that nicotine, and not the other chemicals, contributes to the body weight suppression reported here.
Body weight can be regulated by changes in energy intake (calorie consumption) and energy output (energy expenditure). In the current studies, self-administered nicotine suppressed body weight gain independent of food intake, indicating that nicotine likely regulates body weight through increased energy expenditure. This notion is consistent with reports that acute and chronic experimenter-administered injections of nicotine have been shown to increase physical activity17,37 and basal metabolism.17 In rodents, the doses of nicotine used in studies reporting increased energy expenditure are within the range that suppresses food intake, making it difficult to establish an independent role for suppression of food intake or increased energy expenditure in the effect of nicotine on body weight regulation. Nonetheless, it is clear that at moderate experimenter-administered doses, nicotine can increase energy expenditure, which likely contributes to the body weight-suppressant effects reported here. Future experiments monitoring metabolism in a self-administration model are warranted. Data from smokers suggest that nicotine can increase metabolic rate,38 further supporting for the idea that self-administered nicotine (via intravenous infusions in rats or via cigarette smoke in humans) may suppress body weight through increased energy expenditure.
The FDA has authority to regulate the nicotine content of cigarettes to a low level,39 which may have unintended consequences on body weight.40 Smoking cessation results in weight gain,1,41 and rodents gain weight following the cessation of chronic subcutaneous42,43 and intravenous34 nicotine exposures. However, whether reduction of nicotine to a dose below a reinforcing threshold results in body weight gain in rodents was previously unexplored. Reduction of nicotine dose resulted in significant increases in body weight gain in food restricted rats. These data indicate that reduction of nicotine exposure by reducing the dose available in each infusion results in body weight gain independent of food intake, suggesting that the reduction of nicotine content in cigarettes (thereby reducing total nicotine exposure per cigarette) may result in weight gain in current smokers following a potential mandated reduction of nicotine content in cigarettes.
The results of these experiments provide new insight into the understanding of the body weight suppressant effects of nicotine. In a rodent self-administration model of human smoking, nicotine robustly suppressed body weight gain without concurrent reductions in food intake. These data align with reports from smokers suggesting that the observed body weight differences in smokers and nonsmokers are independent of changes in daily caloric intake. The ability of self-administered nicotine to suppress body weight gain independent of food intake is dose-dependent and occurs at very low doses below the threshold for reinforcing behavior. Reduction of nicotine dose results in body weight gain independent of food intake. These data have important implications for nicotine reduction policy, as they suggest that reduction of nicotine in cigarettes to a level that will not maintain smoking will likely cause significant weight gain in current smokers. However, in new smokers low nicotine levels may still reduce body weight, possibly motivating continued use and maintaining exposure to harmful chemicals in cigarette smoke.
Supplementary Material
Supplementary Figures 1 and 2 can be found online at http://www.ntr.oxfordjournals.org
Funding
Research reported in this publication was supported by the National Institute on Drug Abuse and FDA Center for Tobacco Products (CTP) (U54 DA031659 awarded to ECD and AFS). The funding source had no other role other than financial support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Deanne Buffalari and Rachel Schassburger for helpful feedback in discussing the experiments; as well as, Emily Pitzer, Josh Alberts, Samantha Cwalina, Alexandra Kenefake, Jessica Pelland, Hangil Seo, E. Corina Andriescu, Dora Danko, Nicole Silva, and Isha Vasudeva for their assistance in conducting experimental sessions.
References
- 1. Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. N Engl J Med. 1991;324(11):739–745. doi:10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- 2. Audrain-McGovern J, Benowitz NL. Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther. 2011;90(1):164–168. doi:10.1038/clpt.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pomerleau CS, Zucker AN, Stewart AJ. Characterizing concerns about post-cessation weight gain: results from a national survey of women smokers. Nicotine Tob Res. 2001;3(1):51–60. doi:10.1080/14622200020032105. [DOI] [PubMed] [Google Scholar]
- 4. Rosenthal L, Carroll-Scott A, Earnshaw VA, et al. Targeting cessation: understanding barriers and motivations to quitting among urban adult daily tobacco smokers. Addict Behav. 2013;38(3):1639–1642. doi:10.1016/j.addbeh.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Veldheer S, Yingst J, Foulds G, et al. Once bitten, twice shy: concern about gaining weight after smoking cessation and its association with seeking treatment. Int J Clin Pract. 2014;68(3):388–395. doi:10.1111/ijcp.12332. [DOI] [PubMed] [Google Scholar]
- 6. Grunberg NE. Nicotine, cigarette smoking, and body weight. Br J Addict. 1985;80(4):369–377. [DOI] [PubMed] [Google Scholar]
- 7. Grunberg NE, Bowen DJ. The role of physical activity in nicotine’s effects on body weight. Pharmacol Biochem Behav. 1985;23(5):851–854. [DOI] [PubMed] [Google Scholar]
- 8. Grunberg NE, Bowen DJ, Morse DE. Effects of nicotine on body weight and food consumption in rats. Psychopharmacology (Berl). 1984;83(1):93–98. [DOI] [PubMed] [Google Scholar]
- 9. Grunberg NE, Bowen DJ, Winders SE. Effects of nicotine on body weight and food consumption in female rats. Psychopharmacology (Berl). 1986;90(1):101–105. [DOI] [PubMed] [Google Scholar]
- 10. Winders SE, Grunberg NE. Effects of nicotine on body weight, food consumption and body composition in male rats. Life Sci. 1990;46(21):1523–1530. [DOI] [PubMed] [Google Scholar]
- 11. Zoli M, Picciotto MR. Nicotinic regulation of energy homeostasis. Nicotine Tob Res. 2012;14(11):1270–1290. doi:10.1093/ntr/nts159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mineur YS, Abizaid A, Rao Y, et al. Nicotine decreases food intake through activation of POMC neurons. Science. 2011;332(6035):1330–1332. doi:10.1126/science.1201889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Miyata G, Meguid MM, Varma M, Fetissov SO, Kim HJ. Nicotine alters the usual reciprocity between meal size and meal number in female rat. Physiol Behav. 2001;74(1–2):169–176. [DOI] [PubMed] [Google Scholar]
- 14. Bellinger LL, Wellman PJ, Harris RB, Kelso EW, Kramer PR. The effects of chronic nicotine on meal patterns, food intake, metabolism and body weight of male rats. Pharmacol Biochem Behav. 2010;95(1):92–99. doi:10.1016/j.pbb.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 15. Faraday MM, O’Donoghue VA, Grunberg NE. Effects of nicotine and stress on locomotion in Sprague-Dawley and Long-Evans male and female rats. Pharmacol Biochem Behav. 2003;74(2):325–333. [DOI] [PubMed] [Google Scholar]
- 16. Faraday MM, Scheufele PM, Rahman MA, Grunberg NE. Effects of chronic nicotine administration on locomotion depend on rat sex and housing condition. Nicotine Tob Res. 1999;1(2):143–151. [DOI] [PubMed] [Google Scholar]
- 17. de Morentin PBM, Whittle AJ, Ferno J, et al. Nicotine induces negative energy balance through hypothalamic AMP-activated protein kinase. Diabetes. 2012;61(4):807–817. doi:10.2337/db11-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perkins KA. Effects of tobacco smoking on caloric intake. Br J Addict. 1992;87(2):193–205. [DOI] [PubMed] [Google Scholar]
- 19. Perkins KA, Epstein LH, Stiller RL, et al. Acute effects of nicotine on hunger and caloric intake in smokers and nonsmokers. Psychopharmacology (Berl). 1991;103(1):103–109. [DOI] [PubMed] [Google Scholar]
- 20. Donny EC, Caggiula AR, Rose C, Jacobs KS, Mielke MM, Sved AF. Differential effects of response-contingent and response-independent nicotine in rats. Eur J Pharmacol. 2000;402(3):231–240. [DOI] [PubMed] [Google Scholar]
- 21. Hatsukami DK, Benowitz NL, Donny E, Henningfield J, Zeller M. Nicotine reduction: strategic research plan. Nicotine Tob Res. 2013;15(6):1003–1013. doi:10.1093/ntr/nts214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clemens KJ, Caille S, Stinus L, Cador M. The addition of five minor tobacco alkaloids increases nicotine-induced hyperactivity, sensitization and intravenous self-administration in rats. Int J Neuropsychopharmacol. 2009;12(10):1355–1366. doi:10.1017/S1461145709000273. [DOI] [PubMed] [Google Scholar]
- 23. Smith TT, Schaff MB, Rupprecht LE, et al. Effects of MAO inhibition and a combination of minor alkaloids, beta-carbolines, and acetaldehyde on nicotine self-administration in adult male rats. Drug Alcohol Depend. 2015;155:243–252. doi:10.1016/j.drugalcdep.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Donny EC, Caggiula AR, Knopf S, Brown C. Nicotine self-administration in rats. Psychopharmacology (Berl). 1995;122(4):390–394. [DOI] [PubMed] [Google Scholar]
- 25. Donny EC, Caggiula AR, Mielke MM, et al. Nicotine self-administration in rats on a progressive ratio schedule of reinforcement. Psychopharmacology (Berl). 1999;147(2):135–142. [DOI] [PubMed] [Google Scholar]
- 26. Rupprecht LE, Smith TT, Schassburger RL, Buffalari DM, Sved AF, Donny EC. Behavioral mechanisms underlying nicotine reinforcement. Curr Top Behav Neurosci. 2015;24:19–53. doi:10.1007/978-3-319-13482-6_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smith TT, Schassburger RL, Buffalari DM, Sved AF, Donny EC. Low-dose nicotine self-administration is reduced in adult male rats naive to high doses of nicotine: implications for nicotine product standards. Exp Clin Psychopharmacol. 2014;22(5):453–459. doi:10.1037/a0037396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Smith TT, Levin ME, Schassburger RL, Buffalari DM, Sved AF, Donny EC. Gradual and immediate nicotine reduction result in similar low-dose nicotine self-administration. Nicotine Tob Res. 2013;15(11):1918–1925. doi:10.1093/ntr/ntt082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Donny EC, Caggiula AR, Mielke MM, Jacobs KS, Rose C, Sved AF. Acquisition of nicotine self-administration in rats: the effects of dose, feeding schedule, and drug contingency. Psychopharmacology (Berl). 1998;136(1):83–90. [DOI] [PubMed] [Google Scholar]
- 30. Matta SG, Balfour DJ, Benowitz NL, et al. Guidelines on nicotine dose selection for in vivo research. Psychopharmacology (Berl). 2007;190(3):269–319. doi:10.1007/s00213-006-0441-0. [DOI] [PubMed] [Google Scholar]
- 31. Caggiula AR, Epstein LH, Antelman SM, et al. Conditioned tolerance to the anorectic and corticosterone-elevating effects of nicotine. Pharmacol Biochem Behav. 1991;40(1):53–59. [DOI] [PubMed] [Google Scholar]
- 32. Calvez J, Fromentin G, Nadkarni N, et al. Inhibition of food intake induced by acute stress in rats is due to satiation effects. Physiol Behav. 2011;104(5):675–683. doi:10.1016/j.physbeh.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 33. Maniam J, Morris MJ. The link between stress and feeding behaviour. Neuropharmacology. 2012;63(1):97–110. doi:10.1016/j.neuroph arm.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 34. Grebenstein PE, Thompson IE, Rowland NE. The effects of extended intravenous nicotine administration on body weight and meal patterns in male Sprague-Dawley rats. Psychopharmacology (Berl). 2013;228(3):359–366. doi:10.1007/s00213-013-3043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bunney PE, Burroughs D, Hernandez C, LeSage MG. The effects of nicotine self-administration and withdrawal on concurrently available chow and sucrose intake in adult male rats. Physiol Behav. 2016;154:49–59. doi:10.1016/j.physbeh.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. O’Dell LE, Chen SA, Smith RT, et al. Extended access to nicotine self-administration leads to dependence: Circadian measures, withdrawal measures, and extinction behavior in rats. J Pharmacol Exp Ther. 2007;320(1):180–193. doi:10.1124/jpet.106.105270. [DOI] [PubMed] [Google Scholar]
- 37. Elliott BM, Faraday MM, Phillips JM, Grunberg NE. Effects of nicotine on elevated plus maze and locomotor activity in male and female adolescent and adult rats. Pharmacol Biochem Behav. 2004;77(1):21–28. [DOI] [PubMed] [Google Scholar]
- 38. Perkins KA. Metabolic effects of cigarette smoking. J Appl Physiol (1985). 1992;72(2):401–409. [DOI] [PubMed] [Google Scholar]
- 39. US Congress. Family Smoking Prevention and Tobacco Control Act. U.S. Government Printing Office; 2009. www.gpo.gov/. [Google Scholar]
- 40. Rupprecht LE, Donny EC, Sved AF. Obese smokers as a potential subpopulation of risk in tobacco reduction policy. Yale J Biol Med. 2015;88 (3):289–294. [PMC free article] [PubMed] [Google Scholar]
- 41. Veldheer S, Yingst J, Zhu J, Foulds J. Ten-year weight gain in smokers who quit, smokers who continued smoking and never smokers in the United States, NHANES 2003–2012. Int J Obes (Lond). 2015;39 (12):1727–1732. doi:10.1038/ijo.2015.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Levin ED, Morgan MM, Galvez C, Ellison GD. Chronic nicotine and withdrawal effects on body weight and food and water consumption in female rats. Physiol Behav. 1987;39(4):441–444. [DOI] [PubMed] [Google Scholar]
- 43. Malin DH, Lake JR, Newlin-Maultsby P, et al. Rodent model of nicotine abstinence syndrome. Pharmacol Biochem Behav. 1992;43(3):779–784. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.