Abstract
Purpose
The association between initial molecular response and longer-term outcomes with nilotinib was examined.
Patients and Methods
Patients with imatinib-resistant or -intolerant chronic myeloid leukemia in chronic phase from the phase II nilotinib registration study with available postbaseline BCR-ABL1 transcript assessments were included (N = 237).
Results
BCR-ABL1 transcript levels (International Scale [IS]) at 3 months correlated with complete cytogenetic response (CCyR) by 24 months. Patients with BCR-ABL1 (IS) of > 1% to ≤ 10% at 3 months with nilotinib had higher cumulative incidence of CCyR by 24 months than patients with BCR-ABL1 (IS) of > 10% (53% v 16%). BCR-ABL1 (IS) at 3 months predicted major molecular response (MMR) by 24 months. Cumulative incidence of MMR by 24 months for patients with BCR-ABL1 (IS) of > 0.1% to ≤ 1%, > 1% to ≤ 10%, and > 10% was 65%, 27%, and 9%, respectively. These differences were observed for patients with or without baseline BCR–ABL1 mutations and for those with imatinib resistance or intolerance. Estimated event-free survival (EFS) rates at 24 months decreased with higher transcript levels at 3 months; patients with BCR-ABL1 (IS) of ≤ 1% had an estimated 24-month EFS rate of 82%, compared with 70% for patients with BCR-ABL1 (IS) of > 1% to ≤ 10% and 48% for patients with BCR-ABL1 (IS) of > 10%.
Conclusion
Patients with BCR-ABL1 (IS) of > 10% at 3 months had a lower cumulative incidence of CCyR and MMR and lower rates of EFS versus patients with BCR-ABL1 (IS) of ≤ 10%. Prospective studies may determine whether close monitoring or alternative therapies are warranted for patients with minimal initial molecular response.
INTRODUCTION
Resistance to the BCR-ABL1 tyrosine kinase inhibitor imatinib can develop through several mechanisms, but the most frequently identified acquired resistance results from point mutations in the BCR-ABL1 kinase domain. Nilotinib (Tasigna; Novartis, Basel, Switzerland) is an inhibitor of BCR-ABL1 kinase that was rationally designed to have greater specificity and potency than imatinib.1–3 Nilotinib is 30-fold more potent at inhibiting BCR-ABL1 in vitro than imatinib and is a highly selective BCR-ABL1 kinase inhibitor.1,2 Results from a single-arm, open-label phase II registration study demonstrated the efficacy and safety of nilotinib in patients with imatinib-resistant or -intolerant Philadelphia chromosome–positive chronic myeloid leukemia in chronic phase (Ph+ CML-CP)4,5 or Ph+ CML in accelerated phase (AP).6 Nilotinib was recently approved in more than 40 countries, including the United States, the European Union, Switzerland, and Japan, for treatment of patients with newly diagnosed Ph+ CML-CP based on results from the phase III randomized ENESTnd (Evaluating Nilotinib Efficacy and Safety in Clinical Trials–Newly Diagnosed Patients) trial, which showed the good tolerability and superior efficacy of nilotinib over imatinib.7
While undergoing treatment, patients with Ph+ CML-CP must be continually monitored to assess possible disease progression. Molecular monitoring provides important prognostic information. Achievement of a major molecular response (MMR; ≤ 0.1% according to the International Scale [IS]) within 18 months of imatinib treatment has been associated with delayed progression to AP/blast crisis (BC)8–10 and is considered an optimal response.11
The 3-month BCR-ABL1 level has been shown to be predictive of MMR in imatinib-treated patients, and most newly diagnosed patients who achieve BCR-ABL1 (IS) of ≤ 1.0% with imatinib subsequently achieve MMR.12 The value of molecular monitoring in the setting of nilotinib therapy after imatinib failure has not been defined. We conducted a post hoc analysis of the nilotinib phase II registration trial to explore the association between initial molecular response to nilotinib after imatinib failure and achievement of complete cytogenetic response (CCyR), MMR, and event-free survival (EFS) during therapy.
PATIENTS AND METHODS
Patient Population
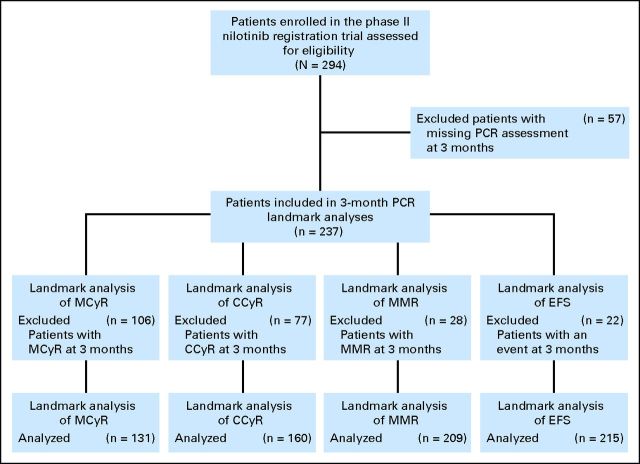
This post hoc analysis included adults (age ≥ 18 years) with imatinib-resistant or -intolerant Ph+ CML-CP enrolled onto a phase II open-label, single-treatment arm study with nilotinib who had any available postbaseline BCR-ABL1 transcript assessment, measured by real-time quantitative polymerase chain reaction (PCR), after initiation of nilotinib therapy (N = 294). Fifty-seven of the 294 patients enrolled had a missing PCR assessment at month 3 (no PCR assessment between study days 56 and 112) and were excluded from all landmark analyses performed on BCR-ABL1 transcript levels at month 3. Among these patients, 19 discontinued treatment before the 3-month PCR assessment (14 because of adverse events; three, disease progression; one, protocol violation; and one, consent withdrawal), seven had a PCR assessment before month 3 but no assessment afterward, and the remaining 31 did not have the 3-month PCR assessment but had assessments after 3 months. Hence, the patient population for the 3-month PCR landmark analyses consisted of 237 patients (Fig 1). Patient eligibility and trial design were previously described.4,5 This trial was registered at http://www.clinicaltrials.gov. as NCT00471497
Fig 1.
CONSORT diagram of patients included in the analysis. CCyR, complete cytogenetic response; EFS, event-free survival; MCyR, major cytogenetic response; MMR, major molecular response; PCR, polymerase chain reaction.
The current landmark analyses of response based on BCR-ABL1 transcript levels at month 3 also excluded patients who had already attained that response (Fig 1). Analysis of major CyR (MCyR) excluded 106 patients (45%; 106 of 237) who attained MCyR at month 3, analysis of CCyR excluded 77 patients (32%; 77of 237) who attained CCyR at month 3 or had BCR-ABL1 (IS) of ≤ 1% at month 3, and analysis of MMR excluded 28 patients (12%; 28 of 237) who achieved MMR at month 3. A BCR-ABL1 value of ≤ 1% correlates closely with the achievement of CCyR and was considered an appropriate surrogate in patients with missing cytogenetic data at 3 months.13,14 Additionally, analysis of EFS excluded 22 patients (9%; 22 of 237) with an event within the first 3 months.
Study Design
The overall design of the nilotinib registration study was described previously.4,5 After our exclusion criteria were applied, patients were grouped according to their level of BCR-ABL1 transcripts. BCR-ABL1 transcript levels at 3 months were used to perform landmark analyses to assess the association between initial molecular response and achievement of MCyR, CCyR, and MMR by 24 months as well as EFS. The categories for BCR-ABL1 transcript levels used for landmark analysis were: one, > 0.1% to ≤ 1%; two, > 1% to ≤ 10%; and three, > 10%. These categories are consistent with previous landmark analyses and were chosen because a BCR-ABL1 level of ≥ 10% at 3 months has been shown to be associated with poorer outcomes with imatinib,15,16 a BCR-ABL1 level of 1% is considered equivalent to CCyR,13,14 and the definition of MMR is BCR-ABL1 of ≤ 0.1% according to the IS.17–19 Thus, CCyR by 24 months was evaluated only in categories two and three because patients with BCR-ABL1 of ≤ 1% had already achieved CCyR.
Events were defined as loss of complete hematologic response or MCyR, progression to AP/BC, discontinuation because of progression to AP/BC, and death resulting from any cause during nilotinib therapy. BCR-ABL1 transcript levels at 1 month were also used to perform a landmark analysis to assess the association between initial molecular response and achievement of MCyR by 12 months. The 1-month landmark was chosen for this analysis because a large proportion of patients had achieved MCyR at month 3 of therapy and were excluded from the 3-month landmark analysis. Thirteen of 250 patients without MMR at month 1 achieved MCyR at month 1 and were excluded from the 1-month landmark analyses. In addition, patient response was stratified by BCR–ABL1 mutation status at baseline and by response to imatinib (resistant v intolerant).
Assessment of BCR–ABL1 Mutation Status
Peripheral blood samples were collected from patients at baseline before the start of treatment; at months 1, 2, and 3; and then every 3 months after nilotinib therapy was initiated. Patients with a baseline mutation were assessed every 3 months. For patients who did not have a baseline mutation, mutation assays were performed only when there was a significant (> two-fold to five-fold) rise in BCR-ABL1 transcript levels, based on the variability of the assay in each of the participating laboratories. RNA was extracted from total blood leukocytes and reverse transcribed. The BCR-ABL1 kinase domain (amino acids 230 to 490) was amplified by nested PCR using primers located in the BCR and ABL regions of the BCR–ABL1 gene. Mutations within this region were identified by direct sequencing, which allows for the reliable detection of mutant clones when they represent at least 20% of the total leukemic clone.20
Statistical Analysis
BCR-ABL1 transcript levels at 3 months were used to perform landmark analyses to assess the association between initial molecular response and cumulative incidence of MCyR, CCyR, and MMR by 24 months, as well as the association between initial molecular response and EFS. The cumulative incidence of response was displayed by an increasing step function. This curve increased each time a new responder was observed up to the best observed response rate by a certain time point. Event-free survival was estimated based on Kaplan-Meier analysis. For patients not experiencing an event, EFS was censored at the data analysis cutoff date for patients still receiving treatment or at the treatment discontinuation date.
The Cox proportional hazards model was used to provide the hazard ratio (HR) for the likelihood of response between groups of patients with different BCR-ABL1 transcript levels at 3 months, and the log-rank test was used for statistical comparisons. A test of the proportionality assumption was used by fitting a Cox model with BCR-ABL1 group indicator, and an artificial time-dependent covariate was created from the BCR-ABL1 indicator × time (t). Thus, the Wald test of H0: no effect on the time-dependent covariate was used to test the proportional hazards assumption. The log of negative log of estimated survivor function versus log of time was also used as a graphical method for checking the proportionality assumption. A similar approach was used in the 1-month landmark analysis.
RESULTS
Overall Efficacy
Patients were recruited to the study between April 21, 2005, and April 26, 2006. Data cutoff for this analysis was April 20, 2008. The overall population of the registration study had a median follow-up of 27.3 months (range, 0.7 to 36.0 months) at data cutoff. Nilotinib remained an effective and well-tolerated therapy for patients with imatinib-resistant or -intolerant Ph+ CML-CP at 24 months, with MCyR and CCyR rates of 59% and 44%, respectively; the 24-month Kaplan-Meier estimate of overall survival (OS) was 87%.4 Recently presented results demonstrated that the estimated OS rate was 78% at 48 months.21
Correlation Between BCR-ABL1 Transcript Levels and CyR
BCR-ABL1 levels at baseline and 3 months are shown in Appendix Table A1 (online only). There was a significant correlation between BCR-ABL1 transcript levels at 3 months and achievement of CCyR (Fig 2A). Patients with BCR-ABL1 (IS) of > 1% to ≤ 10% at 3 months had a higher cumulative incidence rate of CCyR by 24 months than patients with BCR-ABL1 (IS) of > 10% (Table 1; P < .001). On the basis of an analysis of time to CCyR, the likelihood of achieving CCyR at any time after 3 months was about 5× higher for patients with BCR-ABL1 (IS) of > 1% to ≤ 10% at 3 months than for patients with BCR-ABL1 (IS) of > 10% (HR, 4.9; 95% CI, 2.7 to 9.0; log-rank P < .001). Differences in the likelihood of achieving CCyR according to BCR-ABL1 levels at 3 months remained statistically significant when patients were stratified by previous imatinib treatment outcome (ie, resistance or intolerance; Table 1; Fig 2B) or presence of baseline mutation (ie, present or absent; Table 1; Fig 2C).
Fig 2.
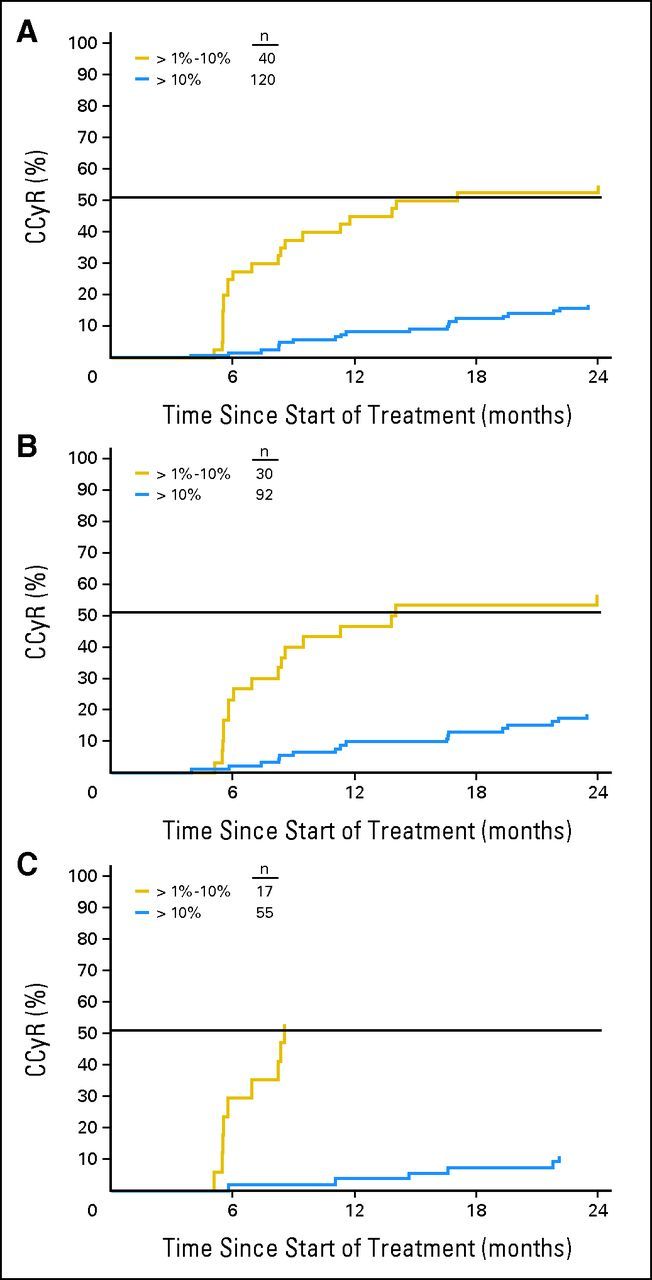
Cumulative incidence of complete cytogenetic response (CCyR) by BCR-ABL1 ratio at 3 months in (A) all patients, (B) imatinib-resistant patients, and (C) patients with a baseline mutation.
Table 1.
Cumulative Incidence of CCyR and MMR by 24 Months Based on Molecular Response at 3 Months
| Response | No. of Patients |
BCR-ABL1 at 3 Months (%)* |
HR† | 95% CI | P‡ | ||
|---|---|---|---|---|---|---|---|
| > 0.1% to ≤ 1% | > 1% to ≤ 10% | > 10% | |||||
| Patients achieving CCyR by 24 months§ | |||||||
| All | 160 | 53 | 16 | ||||
| > 10% v > 1% to ≤ 10% | 4.9 | 2.7 to 9.0 | < .001 | ||||
| With baseline mutation | 72 | 53 | 11 | ||||
| > 10% v > 1% to ≤ 10% | 8.2 | 2.9 to 23 | < .001 | ||||
| Without baseline mutation | 75 | 50 | 19 | ||||
| > 10% v > 1% to ≤ 10% | 3.5 | 1.5 to 8.1 | .002 | ||||
| Resistant | 122 | 53 | 17 | ||||
| > 10% v > 1% to ≤ 10% | 4.7 | 2.4 to 9.3 | < .001 | ||||
| Intolerant | 38 | 50 | 11 | ||||
| > 10% v > 1% to ≤ 10% | 6.1 | 1.5 to 26 | .006 | ||||
| Patients achieving MMR by 24 months∥ | |||||||
| All | 209 | 65 | 27 | 9 | |||
| > 1% to ≤ 10% v > 0.1% to ≤ 1% | 2.9 | 1.5 to 5.6 | .001 | ||||
| > 10% v > 1% to ≤ 10% | 3.8 | 1.8 to 8.2 | < .001 | ||||
| With baseline mutations | 83 | 86 | 32 | 9 | |||
| > 1% to ≤ 10% v > 0.1% to ≤ 1% | 3.8 | 1.2 to 12.1 | .018 | ||||
| > 10% v > 1% to ≤ 10% | 4.5 | 1.4 to 14.8 | .007 | ||||
| Without baseline mutations | 108 | 67 | 24 | 10 | |||
| > 1% to ≤ 10% v > 0.1% to ≤ 1% | 3.5 | 1.5 to 8.5 | .003 | ||||
| > 10% v > 1% to ≤ 10% | 2.9 | 1.0 to 8.5 | .036 | ||||
| Resistant | 150 | 63 | 28 | 9 | |||
| > 1% to ≤ 10% v > 0.1% to ≤ 1% | 2.9 | 1.2 to 7.0 | .011 | ||||
| > 10% v > 1% to ≤ 10% | 3.8 | 1.5 to 9.5 | .002 | ||||
| Intolerant | 59 | 67 | 27 | 10 | |||
| > 1% to ≤ 10% v > 0.1% to ≤ 1% | 2.7 | 0.9 to 8.0 | .064 | ||||
| > 10% v > 1% to ≤ 10% | 3.7 | 0.9 to 15.6 | .053 | ||||
Abbreviations: CCyR, complete cytogenetic response; HR, hazard ratio; IS, International Scale; MMR, major molecular response.
According to IS.
Cox proportional hazard model.
Log-rank test.
Excludes 32% of patients (77 of 237) who achieved CCyR at 3 months or had BCR-ABL1 (IS) of ≤ 1% at 3 months.
Excludes 12% of patients (28 of 237) who achieved MMR at 3 months.
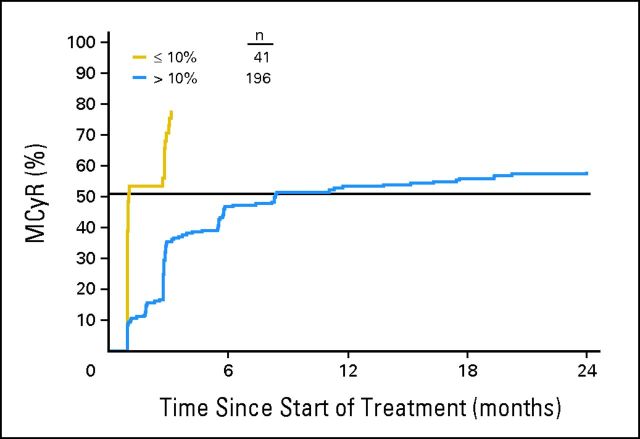
Similarly, there was a significant correlation between BCR-ABL1 transcript levels at 3 months and achievement of MCyR. However, a large proportion of patients (45%; 106 of 237) had achieved MCyR at month 3 and were excluded from this analysis. As a result, landmark analysis of MCyR was performed based on BCR-ABL1 transcript levels at month 1 of nilotinib therapy. Patients with BCR-ABL1 (IS) of ≤ 10% had a higher cumulative incidence rate of MCyR by 12 months compared with patients with BCR-ABL1 (IS) of > 10% (78% v 53%; Fig 3). On the basis of an analysis of time to MCyR, the likelihood of achieving MCyR at any time after 1 month was 2.4× higher for patients with BCR-ABL1 (IS) of ≤ 10% at 1 month than patients with BCR-ABL1 (IS) of > 10% (HR, 2.4; 95% CI, 1.6 to 3.6; log-rank P < .001).
Fig 3.
Cumulative incidence of major cytogenetic response (MCyR) by BCR-ABL1 ratio at 1 month (all patients).
Correlation Between 3-Month BCR-ABL1 Transcript Levels and MMR
BCR-ABL1 transcript levels at 3 months were highly predictive of MMR by 24 months (Fig 4A; Table 1). On the basis of an analysis of time to MMR, the likelihood of achieving MMR at any time after 3 months was about 4× higher for patients with BCR-ABL1 (IS) of > 0.1% to ≤ 1% at 3 months than patients with BCR-ABL1 (IS) of > 1% to ≤ 10% (HR, 3.8; log-rank P < .001) and approximately 3× higher for patients with BCR-ABL1 (IS) of > 1% to ≤ 10% at 3 months than patients with BCR-ABL1 (IS) of > 10% (HR, 2.9; log-rank P = .001). Differences in the likelihood of achieving MMR according to BCR-ABL1 levels at 3 months remained statistically significant when patients were stratified by resistance to previous imatinib treatment (Table 1; Fig 4B) or baseline mutation (ie, present or absent; Table 1; Fig 4C).
Fig 4.

Cumulative incidence of major molecular response (MMR) by BCR-ABL1 ratio at 3 months in (A) all patients, (B) imatinib-resistant patients, and (C) patients with a baseline mutation.
Correlation Between 3-Month BCR-ABL1 Transcript Levels and EFS Rates
The probability of EFS was also correlated with BCR-ABL1 transcript levels at 3 months. Estimated EFS rates at 24 months decreased with higher transcript levels at 3 months (Table 2). A statistically significant difference between BCR-ABL1 transcript levels and the estimated probability of EFS was observed for four subsets: one, patients with BCR-ABL1 (IS) of > 1% to ≤ 10% versus BCR-ABL1 (IS) of > 10% (log-rank P = .030); two, patients with a baseline mutation with BCR-ABL1 (IS) of ≤ 1% versus BCR-ABL1 (IS) of > 1% to ≤ 10% (log-rank P = .011); three, patients without a baseline mutation with BCR-ABL1 (IS) of > 1% to ≤ 10% versus BCR-ABL1 (IS) of > 10% (log-rank P = .052; borderline significance); and four, patients with imatinib intolerance with BCR-ABL1 (IS) of > 1% to ≤ 10% versus BCR-ABL1 (IS) of > 10% (log-rank P = .015).
Table 2.
EFS at 24 Months Based on Molecular Response at 3 Months
| Estimated EFS Rate for Patients at 24 Months* | No. of Patients |
BCR-ABL1 at 3 Months (%)† |
P‡ | ||
|---|---|---|---|---|---|
| ≤ 1% | > 1% to ≤ 10% | > 10% | |||
| All | 215 | 82 | 70 | 48 | |
| ≤ 1% v > 1% to ≤ 10% | .075 | ||||
| >1% to ≤ 10% v > 10% | .030 | ||||
| With baseline mutations | 74 | 100 | 54 | 36 | |
| ≤ 1% v > 1% to ≤ 10% | .011 | ||||
| >1% to ≤ 10% v > 10% | .58 | ||||
| Without baseline mutations | 123 | 81 | 82 | 59 | |
| ≤ 1% v > 1% to ≤ 10% | .91 | ||||
| >1% to ≤ 10% v > 10% | .052 | ||||
| Resistant | 152 | 75 | 64 | 47 | |
| ≤ 1% v > 1% to ≤ 10% | .14 | ||||
| >1% to ≤ 10% v > 10% | .19 | ||||
| Intolerant | 63 | 89 | 91 | 54 | |
| ≤ 1% v > 1% to ≤ 10% | .71 | ||||
| >1% to ≤ 10% v > 10% | .015 | ||||
Abbreviations: EFS, event-free survival; IS, International Scale.
Excludes 9% (22 of 237) of patients who had an event within the first 3 months.
According to IS.
Log-rank test.
DISCUSSION
In imatinib-resistant and -intolerant patients with CML-CP treated with nilotinib, BCR-ABL1 transcript levels at 3 months correlated significantly with CCyR and MMR by 24 months, as well as with EFS. Generally, patients with BCR-ABL1 transcript levels < 10% at 3 months achieved higher rates of MMR, CCyR, and MCyR by 24 months. The poorer responses for patients with BCR-ABL1 (IS) of > 10% was independent of BCR–ABL1 mutation status and of whether patients commenced nilotinib because of imatinib intolerance or resistance. This suggests that initial molecular response is a compelling predictor of later response. Furthermore, with an EFS rate of approximately 50% at 24 months, BCR-ABL1 (IS) of > 10% at 3 months may be an indicator for consideration of a search for an appropriate donor for allogeneic stem-cell transplantation.
Because a considerable number of the best-responding patients (ie, those who achieved responses within the first 3 months of nilotinib therapy) were excluded from these landmark analyses, the effect of early molecular responses on longer-term outcomes, especially MCyR, may be underestimated at the 3-month landmark. To address this, we performed a landmark analysis according to BCR-ABL1 transcript levels at 1 month. The patients who failed to achieve a BCR-ABL1 value of at least 10% by 1 month had a significantly lower probability of achieving MCyR by 12 months. This is an important finding because it was demonstrated in an analysis of 113 patients receiving nilotinib (n = 43) or dasatinib (n = 70) after imatinib failure that patients achieving MCyR by 12 months had a significant survival advantage.22
The finding that early reduction of BCR-ABL1 to < 1% correlated with early achievement of MMR during nilotinib therapy is consistent with previous reports examining the prognostic significance of early molecular response to imatinib therapy. Early molecular response to imatinib therapy is strongly associated with a higher probability of achieving MMR.23 Furthermore, the degree of molecular response at early time points was associated with a high MMR rate and low rate of disease-related events. In a study conducted at the MD Anderson Cancer Center, for example, patients who achieved a BCR-ABL1 ratio of ≤ 1% by 3 months had higher MMR rates and lower event rates than those who did not achieve this milestone.24 Other analyses of large randomized trials have confirmed the relationship between the degree of molecular response at early time points and progression to both AP/BC and EFS.13,25 Importantly, early achievement of MMR with imatinib therapy was associated with more durable responses, which in turn were associated with prolonged progression-free survival.26–30
In this post hoc analysis of the nilotinib registration study, we demonstrated that patients who achieve early molecular responses during nilotinib therapy may have an increased probability of improved long-term outcomes. The benefit of early molecular response has also been observed in results from the phase III ENESTnd trial. In this study, nilotinib therapy provided earlier and deeper molecular responses than did imatinib treatment, resulting in lower rates of progression to AP/BC by 12 months. Longer follow-up at 2431 and 3632 months confirmed the benefits of early molecular response, including a reduced incidence of mutations. The study is ongoing.
It should be noted that some baseline factors may influence the BCR-ABL1 value at 3 months. For example, patients with mutations less sensitive to nilotinib (T315I, Y253H, E255V/K, and F359V/C) at baseline have lower response rates and higher progression rates compared with patients without a baseline mutation or patients with other baseline mutations, and clinicians are advised against selecting nilotinib therapy for these patients.33 In addition, patients who entered the nilotinib registration study because of imatinib intolerance generally had better outcomes than those who entered because of imatinib resistance.4,5 It was for these reasons that we chose to independently analyze the effect of BCR-ABL1 (IS) levels at 3 months on longer-term outcomes in four patient subgroups (with baseline mutation, without baseline mutation, resistant, and intolerant). In all of these groups, our study demonstrated that BCR-ABL1 values of > 10% (IS) at 3 months identified those with subsequent poor response.
Ultimately, the exact clinical importance of these findings in patients with imatinib resistance and intolerance needs confirmation. This study did not evaluate the impact of changing therapy at 3 months, and this question can only be properly addressed in a prospective clinical trial. Longer follow-up is required to assess the association between 3-month BCR-ABL1 transcript levels and outcomes such as progression-free survival and OS. Nevertheless, this study indicates that molecular analysis is an important assessment for patients treated with kinase inhibitor therapy. Molecular analysis provides significant prognostic information when measured within the first few months of initiation of nilotinib therapy after imatinib failure, which is independent of BCR-ABL1 mutation status at commencement of nilotinib. Patients who do not have a reduction of BCR-ABL1 (IS) to ≤ 10% at 3 months during nilotinib therapy, after imatinib failure, may benefit from close monitoring or alternative therapy, which should be prospectively investigated.
Acknowledgment
We thank Michelle Boehm, PhD, Daniel Hutta, PhD, and Erinn Goldman, PhD, for medical editorial assistance with this article.
Appendix
Table A1.
BCR-ABL1 Ratios at Baseline and Month 3*
| Characteristic | Baseline |
Month 3 |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| All patients (N = 237) | ||||
| No. of patients | 202† | 237 | ||
| BCR-ABL1 transcript level | ||||
| Mean | 75.5 | 25.6 | ||
| SD | 133.1 | 39.6 | ||
| Median | 40.2 | 11.6 | ||
| 25th to 75th percentiles | 19.5-72.0 | 1.1-30.7 | ||
| Minimum to maximum | 0.0-1,243 | 0.0-241 | ||
| BCR-ABL1 ratio | ||||
| > 0.1% to 1% | 5 | 2.5 | 31 | 13.1 |
| > 1% to 10% | 17 | 8.4 | 55 | 23.2 |
| > 10% | 176 | 87.1 | 123 | 51.9 |
| Patients with baseline mutation (n = 86)‡ | ||||
| No. of patients | 74† | 86 | ||
| BCR-ABL1 transcript level | ||||
| Mean | 92.8 | 34.9 | ||
| SD | 165.7 | 45.5 | ||
| Median | 41.9 | 19.4 | ||
| 25th to 75th percentiles | 28.5-78.2 | 7.6-40.4 | ||
| Minimum to maximum | 1.9-1,243 | 0.0-236 | ||
| BCR-ABL1 ratio | ||||
| > 0.1% to 1% | 0 | 0 | 7 | 8.1 |
| > 1% to 10% | 3 | 4.1 | 19 | 22.1 |
| > 10% | 71 | 95.9 | 57 | 66.3 |
| Patients without baseline mutation (n = 132)‡ | ||||
| No. of patients | 123† | 132 | ||
| BCR-ABL1 transcript level | ||||
| Mean | 66.2 | 20.0 | ||
| SD | 111.6 | 34.1 | ||
| Median | 35.8 | 5.6 | ||
| 25th to 75th percentiles | 13.9-64.9 | 0.3-27.3 | ||
| Minimum to maximum | 0.0-931 | 0.0-241 | ||
| BCR-ABL1 ratio | ||||
| > 0.1% to 1% | 5 | 4.1 | 21 | 15.9 |
| > 1% to 10% | 14 | 11.4 | 29 | 22.0 |
| > 10% | 100 | 81.3 | 58 | 43.9 |
| Resistant patients (n = 165) | ||||
| No. of patients | 140† | 165 | ||
| BCR-ABL1 transcript level | ||||
| Mean | 85.4 | 28.5 | ||
| SD | 152.1 | 39.9 | ||
| Median | 41.4 | 14.9 | ||
| 25th to 75th percentiles | 23.6-77.6 | 2.4-34.9 | ||
| Minimum to maximum | 0.0-1,243 | 0.0-236 | ||
| BCR-ABL1 ratio | ||||
| > 0.1% to 1% | 2 | 1.4 | 16 | 9.7 |
| > 1% to 10% | 11 | 7.9 | 40 | 24.2 |
| > 10% | 126 | 90 | 94 | 57.0 |
| Intolerant patients (n = 72) | ||||
| No. of patients | 62† | 72 | ||
| BCR-ABL1 transcript level | ||||
| Mean | 53.4 | 18.7 | ||
| SD | 70.2 | 38.2 | ||
| Median | 36.5 | 2.6 | ||
| 25th to 75th percentiles | 16.3-54.0 | 0.3-25.6 | ||
| Minimum to maximum | 0.0-375 | 0.0-241 | ||
| BCR-ABL1 ratio | ||||
| > 0.1% to 1% | 3 | 4.8 | 15 | 20.8 |
| > 1% to 10% | 6 | 9.7 | 15 | 20.8 |
| > 10% | 50 | 80.6 | 29 | 40.3 |
Abbreviation: SD, standard deviation.
According to International Scale.
35 patients (12 with baseline mutation, nine without, 25 resistant, 10 intolerant) had missing BCR-ABL1 assessments at baseline.
19 patients had missing mutation analyses at baseline.
Footnotes
Supported by Novartis.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
Clinical trial information: NCT00471497.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: Ariful Haque, Novartis (C); Yaping Shou, Novartis (C); Richard C. Woodman, Novartis (C) Consultant or Advisory Role: Susan Branford, Bristol-Myers Squibb (C), Novartis (C); Hagop M. Kantarjian, Novartis (C); Giovanni Martinelli, Bristol-Myers Squibb (C), Genzyme (C), Novartis (C), Pfizer (C); Jerald P. Radich, ARIAD Pharmaceuticals (C), Bristol-Myers Squibb (C), Novartis (C), Pfizer (C); Giuseppe Saglio, Bristol-Myers Squibb (C), Novartis (C), Pfizer (C); Andreas Hochhaus, ARIAD Pharmaceuticals (U), Bristol-Myers Squibb (C), Novartis (C), Pfizer (C); Timothy P. Hughes, ARIAD Pharmaceuticals (C), Bristol-Myers Squibb (C), Novartis (C); Martin C. Müller, Bristol-Myers Squibb (C), Novartis (C) Stock Ownership: Ariful Haque, Novartis; Yaping Shou, Novartis; Richard C. Woodman, Novartis Honoraria: Susan Branford, Bristol-Myers Squibb, Novartis; Dong-Wook Kim, Bristol-Myers Squibb, Novartis; Simona Soverini, Bristol-Myers Squibb, Novartis; Giovanni Martinelli, Bristol-Myers Squibb, Novartis; Giuseppe Saglio, Bristol-Myers Squibb, Novartis; Andreas Hochhaus, Bristol-Myers Squibb, Novartis, Pfizer; Martin C. Müller, Bristol-Myers Squibb, Novartis Research Funding: Susan Branford, Bristol-Myers Squibb, Novartis; Dong-Wook Kim, ARIAD Pharmaceuticals, Bristol-Myers Squibb, Novartis, Pfizer; Hagop M. Kantarjian, Bristol-Myers Squibb, Novartis, Pfizer; Giovanni Martinelli, Novartis; Jerald P. Radich, Novartis; Andreas Hochhaus, Bristol-Myers Squibb, Novartis, Pfizer; Timothy P. Hughes, ARIAD Pharmaceuticals, Bristol-Myers Squibb, Novartis; Martin C. Müller, Bristol-Myers Squibb, Novartis Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Ariful Haque, Yaping Shou, Richard C. Woodman, Hagop M. Kantarjian, Jerald P. Radich, Giuseppe Saglio, Andreas Hochhaus, Timothy P. Hughes
Provision of study materials or patients: Dong-Wook Kim, Simona Soverini, Hagop M. Kantarjian, Jerald P. Radich, Martin C. Müller
Collection and assembly of data: Susan Branford, Simona Soverini, Ariful Haque, Yaping Shou, Giovanni Martinelli, Jerald P. Radich, Giuseppe Saglio, Andreas Hochhaus, Martin C. Müller
Data analysis and interpretation: Susan Branford, Dong-Wook Kim, Ariful Haque, Yaping Shou, Richard C. Woodman, Hagop M. Kantarjian, Jerald P. Radich, Giuseppe Saglio, Andreas Hochhaus, Timothy P. Hughes, Martin C. Müller
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Weisberg E, Manley PW, Breitenstein W, et al. Characterization of AMN107, a selective inhibitor of native and mutant Bcr-Abl. Cancer Cell. 2005;7:129–141. doi: 10.1016/j.ccr.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 2.Golemovic M, Verstovsek S, Giles F, et al. AMN107, a novel aminopyrimidine inhibitor of Bcr-Abl, has in vitro activity against imatinib-resistant chronic myeloid leukemia. Clin Cancer Res. 2005;11:4941–4947. doi: 10.1158/1078-0432.CCR-04-2601. [DOI] [PubMed] [Google Scholar]
- 3.Manley PW, Drueckes P, Fendrich G, et al. Extended kinase profile and properties of the protein kinase inhibitor nilotinib. Biochim Biophys Acta. 2010;1804:445–453. doi: 10.1016/j.bbapap.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Kantarjian HM, Giles FJ, Bhalla KN, et al. Nilotinib is effective in patients with chronic myeloid leukemia in chronic phase following imatinib resistance or intolerance: 24-month follow-up results. Blood. 2011;117:1141–1145. doi: 10.1182/blood-2010-03-277152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kantarjian HM, Giles F, Gattermann N, et al. Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood. 2007;110:3540–3546. doi: 10.1182/blood-2007-03-080689. [DOI] [PubMed] [Google Scholar]
- 6.le Coutre P, Ottmann OG, Giles F, et al. Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is active in patients with imatinib-resistant or -intolerant accelerated-phase chronic myelogenous leukemia. Blood. 2008;111:1834–1839. doi: 10.1182/blood-2007-04-083196. [DOI] [PubMed] [Google Scholar]
- 7.Saglio G, Kim DW, Issaragrisil S, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362:2251–2259. doi: 10.1056/NEJMoa0912614. [DOI] [PubMed] [Google Scholar]
- 8.Hughes TP, Kaeda J, Branford S, et al. Frequency of major molecular responses to imatinib or interferon alfa plus cytarabine in newly diagnosed chronic myeloid leukemia. N Engl J Med. 2003;349:1423–1432. doi: 10.1056/NEJMoa030513. [DOI] [PubMed] [Google Scholar]
- 9.Press RD, Love Z, Tronnes AA, et al. BCR-ABL mRNA levels at and after the time of a complete cytogenetic response (CCR) predict the duration of CCR in imatinib mesylate-treated patients with CML. Blood. 2006;107:4250–4256. doi: 10.1182/blood-2005-11-4406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Druker BJ, Guilhot F, O'Brien SG, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355:2408–2417. doi: 10.1056/NEJMoa062867. [DOI] [PubMed] [Google Scholar]
- 11.Baccarani M, Cortes J, Pane F, et al. Chronic myeloid leukemia: An update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol. 2009;27:6041–6051. doi: 10.1200/JCO.2009.25.0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hughes TP, Branford S, White DL, et al. Impact of early dose intensity on cytogenetic and molecular responses in chronic- phase CML patients receiving 600 mg/day of imatinib as initial therapy. Blood. 2008;112:3965–3973. doi: 10.1182/blood-2008-06-161737. [DOI] [PubMed] [Google Scholar]
- 13.Hughes TP, Hochhaus A, Branford S, et al. Long-term prognostic significance of early molecular response to imatinib in newly diagnosed chronic myeloid leukemia: An analysis from the International Randomized Study of Interferon versus STI571 (IRIS) Blood. 2010;116:3758–3765. doi: 10.1182/blood-2010-03-273979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ross DM, Branford S, Moore S, et al. Limited clinical value of regular bone marrow cytogenetic analysis in imatinib-treated chronic phase CML patients monitored by RQ-PCR for BCR-ABL. Leukemia. 2006;20:664–670. doi: 10.1038/sj.leu.2404139. [DOI] [PubMed] [Google Scholar]
- 15.Hughes T, Kim D, Martinelli G, et al. Early molecular response to nilotinib in patients who failed imatinib is associated with a higher probability of cytogenetic response in chronic myeloid leukemia (CML) Haematologica. 2010;95:54. abstr 0135. [Google Scholar]
- 16.Wang L, Pearson K, Ferguson JE, et al. The early molecular response to imatinib predicts cytogenetic and clinical outcome in chronic myeloid leukaemia. Br J Haematol. 2003;120:990–999. doi: 10.1046/j.1365-2141.2003.04200.x. [DOI] [PubMed] [Google Scholar]
- 17.Hughes T, Deininger M, Hochhaus A, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: Review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108:28–37. doi: 10.1182/blood-2006-01-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Branford S, Cross NC, Hochhaus A, et al. Rationale for the recommendations for harmonizing current methodology for detecting BCR-ABL transcripts in patients with chronic myeloid leukaemia. Leukemia. 2006;20:1925–1930. doi: 10.1038/sj.leu.2404388. [DOI] [PubMed] [Google Scholar]
- 19.Müller MC, Erben P, Saglio G, et al. Harmonization of BCR-ABL mRNA quantification using a uniform multifunctional control plasmid in 37 international laboratories. Leukemia. 2008;22:96–102. doi: 10.1038/sj.leu.2404983. [DOI] [PubMed] [Google Scholar]
- 20.Branford S, Rudzki Z, Walsh S, et al. Detection of BCR-ABL mutations in patients with CML treated with imatinib is virtually always accompanied by clinical resistance, and mutations in the ATP phosphate-binding loop (P-loop) are associated with a poor prognosis. Blood. 2003;102:276–283. doi: 10.1182/blood-2002-09-2896. [DOI] [PubMed] [Google Scholar]
- 21.le Coutre PD, Giles FJ, Pinilla-Ibarz J, et al. Nilotinib in imatinib-resistant or -intolerant patients (pts) with chronic myeloid leukemia in chronic phase (CML-CP): 48-month follow-up results of a phase 2 study. Blood. 2011;118:1610. doi: 10.1038/leu.2012.181. abstr 3770. [DOI] [PubMed] [Google Scholar]
- 22.Tam CS, Kantarjian H, Garcia-Manero G, et al. Failure to achieve a major cytogenetic response by 12 months defines inadequate response in patients receiving nilotinib or dasatinib as second or subsequent line therapy for chronic myeloid leukemia. Blood. 2008;112:516–518. doi: 10.1182/blood-2008-02-141580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Branford S, Rudzki Z, Harper A, et al. Imatinib produces significantly superior molecular responses compared to interferon alfa plus cytarabine in patients with newly diagnosed chronic myeloid leukemia in chronic phase. Leukemia. 2003;17:2401–2409. doi: 10.1038/sj.leu.2403158. [DOI] [PubMed] [Google Scholar]
- 24.Quintás-Cardama A, Kantarjian H, Jones D, et al. Delayed achievement of cytogenetic and molecular response is associated with increased risk of progression among patients with chronic myeloid leukemia in early chronic phase receiving high-dose or standard-dose imatinib therapy. Blood. 2009;113:6315–6321. doi: 10.1182/blood-2008-07-166694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanfstein B, Müller MC, Hehlmann R, et al. Early molecular and cytogenetic response is predictive for long-term progression-free and overall survival in chronic myeloid leukemia (CML) Leukemia. 2012;26:2096–2102. doi: 10.1038/leu.2012.85. [DOI] [PubMed] [Google Scholar]
- 26.Iacobucci I, Saglio G, Rosti G, et al. Achieving a major molecular response at the time of a complete cytogenetic response (CCgR) predicts a better duration of CCgR in imatinib-treated chronic myeloid leukemia patients. Clin Cancer Res. 2006;12:3037–3042. doi: 10.1158/1078-0432.CCR-05-2574. [DOI] [PubMed] [Google Scholar]
- 27.Cortes J, Talpaz M, O'Brien S, et al. Molecular responses in patients with chronic myelogenous leukemia in chronic phase treated with imatinib mesylate. Clin Cancer Res. 2005;11:3425–3432. doi: 10.1158/1078-0432.CCR-04-2139. [DOI] [PubMed] [Google Scholar]
- 28.Paschka P, Müller MC, Merx K, et al. Molecular monitoring of response to imatinib (Glivec) in CML patients pretreated with interferon alpha. Low levels of residual disease are associated with continuous remission. Leukemia. 2003;17:1687–1694. doi: 10.1038/sj.leu.2403033. [DOI] [PubMed] [Google Scholar]
- 29.Press RD, Galderisi C, Yang R, et al. A half-log increase in BCR-ABL RNA predicts a higher risk of relapse in patients with chronic myeloid leukemia with an imatinib-induced complete cytogenetic response. Clin Cancer Res. 2007;13:6136–6143. doi: 10.1158/1078-0432.CCR-07-1112. [DOI] [PubMed] [Google Scholar]
- 30.Kantarjian H, O'Brien S, Shan J, et al. Cytogenetic and molecular responses and outcome in chronic myelogenous leukemia: Need for new response definitions? Cancer. 2008;112:837–845. doi: 10.1002/cncr.23238. [DOI] [PubMed] [Google Scholar]
- 31.Kantarjian HM, Hochhaus A, Saglio G, et al. Nilotinib versus imatinib for the treatment of patients with newly diagnosed chronic phase, Philadelphia chromosome-positive, chronic myeloid leukaemia: 24-month minimum follow-up of the phase 3 randomised ENESTnd trial. Lancet Oncol. 2011;12:841–851. doi: 10.1016/S1470-2045(11)70201-7. [DOI] [PubMed] [Google Scholar]
- 32.Saglio G, LeCoutre PD, Pasquini R, et al. Nilotinib versus imatinib in patients (pts) with newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia in chronic phase (CML-CP): ENESTnd 36-month (mo) follow-up. Blood. 2011;118:208–209. abstr 452. [Google Scholar]
- 33.Hughes T, Saglio G, Branford S, et al. Impact of baseline BCR-ABL mutations on response to nilotinib in patients with chronic myeloid leukemia in chronic phase. J Clin Oncol. 2009;27:4204–4210. doi: 10.1200/JCO.2009.21.8230. [DOI] [PMC free article] [PubMed] [Google Scholar]