Abstract
Background:
Infertility predisposes the couples to mental and psychological problems such as anxiety, depression, anger, and partner abuse. This study aimed to investigate the association between infertility factors and the non-physical abuse between infertile spouses.
Materials and Methods:
This is a descriptive cross-sectional study conducted on 262 infertile couples (131 female and 131 male), selected through convenient sampling, who referred to infertility centers in Isfahan. Data were collected by Partner Abuse Scale: Non-physical (PASNP), designed to measure the non-physical abuse experienced in relationship with partner and Non-physical Abuse of Partner Scale (NPAPS), designed to measure the non-physical abuse delivered upon the partner. All data were analyzed through SPSS version 16.
Results:
Mean scores of NPAPS were 23.1% and 21.3% in men and women, respectively. Mean scores of PASNP were 13.8% and 20.3% among men and women, respectively. There was a significant difference in the mean scores of perceived non-physical partner abuse between men and women (P < 0.001). There was also a significant difference in the mean scores of perceived non-physical partner abuse and factor of infertility (P < 0.01).
Conclusions:
Perceived non-physical abuse and delivered non-physical abuse upon the partner were low among infertile couples. Women had a higher perception of abuse when the cause of infertility was female factor, compared to men. However, special attention should be paid to infertile couples. Marital counseling, besides infertility counseling, should be conducted for these couples.
Key words: Infertility, infertility factors, non-physical abuse, partner
INTRODUCTION
Opposite to the term fertility, there is another important aspect called infertility, which is defined as inability to conceive for at least 1 year after regular and unprotected sexual intercourse.[1] The causes for infertility can be generally categorized as male factor, female factor, combination, and unexplained or idiopathic factor.[2] The World Health Organization (WHO) reported mean infertility rate as 12–15% globally, with a prevalence of 24.9% in Iran in 2004.[3] Fertility is the outcome of thousands of biological processes in men and women. An imbalance in any of these systems leads to infertility and predisposes the couples to mental and psychological problems such as anxiety, depression, and mental pressure, which, at times, result in social problems such as domestic violence.[4] In various studies, it has been reported that the stressful experience of infertility is accompanied with a vast spectrum of psychological problems including impulsive behaviors and spread of anger, the feeling of helplessness and rejection, as well as marital problems.[5,6] Meanwhile, couples’ negative self-concept and low self-esteem drive them to have unreal and early expectations. On couples’ failure to achieve their unreal expectations (e.g., wishing to have a child), they try to relieve their discomfort by delivering violence upon their spouse.[7] Misbehavior is among the important issues associated with public health, which is not only observed in all geographical areas and religions and racial groups, but also in all levels of education, occupation, and economic and social classes.[8] Several studies have reported some factors associated with infertility that can predispose women to misbehavior and increase the rate of violence by twofold.[9] As infertility and its effects may vary in difference cultures, the prevalence of violence has been reported differently in various studies. Yildizhan et al. reported the rate of domestic violence incidence among infertile women as 33.6% in Turkey,[9] and this rate was reported as 61.8% in Iran.[10] Meanwhile, Leung et al. reported the incidence of violence to be only 1.8% in Hong Kong.[11] There are controversial results in the context of the effect of interventional factors such as infertility on the incidence of marital reactions. Most of the conducted studies investigated physical violence, although non-physical violence can lead to major complications and due to lack of studies in this subject. Therefore, the present study aimed at determining the association between infertility factors and non-physical partner abuse in infertile couples referring to infertility centers in Isfahan in 2013.
MATERIALS AND METHODS
This is a descriptive cross-sectional study conducted on 262 infertile couples (131 male and 131 female) who referred to the infertility centers of Isfahan and met the inclusion criteria. They were selected through convenient sampling. Inclusion criteria were primary infertility, infertility with a diagnosed cause, and absence of any diagnosed mental and psychological diseases. Data collection tool comprised a demographic characteristics questionnaire, and Non-physical Abuse of Partner Scale (NPAPS) as well as Partner Abuse Scale: Non-physical (PASNP), both of which include 25 items that were separately completed and measured for each subject.
NPAPS (25-item tool) is one of the care scales in which the concept of the abuser from the level of the abuse delivered to his/her partner is measured. It has been designed to measure the level or severity of non-physical abuse delivered upon the partner, based on the abuser's self report. PASNP is also a 25-item tool to measure the degree or severity of non-physical behavioral abuse delivered to the clients by their spouse or partner. These two questionnaires, designed by James Dublio and Garner to measure non-physical abuse, enjoy an excellent internal consistency with α = 0.90,[12] and were adopted for the first time in Iran. The present research was approved in Isfahan University of Medical Sciences and its related ethics committee. For questionnaire localization, four items were deleted. Reliability and validity of this questionnaire were established by face and content validity with the help of the academic members in nursing and midwifery school and school of educational sciences of Isfahan University. Its validity and reliability were confirmed with Cronbach alpha = 0.84. After obtaining an informed consent from the subjects, data were separately collected from couples in a peaceful and quiet place. Both questionnaires are scored based on a Likert's seven-point scale (1–7) as follows: Never (score 1), seldom (score 2), sometimes (score 3), usually (score 4), often (score 5), frequently (score 6), and always (score 7), with a calculated mean out of 100. The collected data were analyzed by descriptive statistics (mean, SD, Min, Max) and interventional statistics (independent t-test) in SPSS 16 with a significance level of P < 0.05. The results are presented in Tables 1–3.
Table 1.
Mean of NPAPS and PASNP in infertile couples
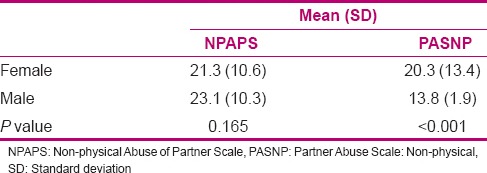
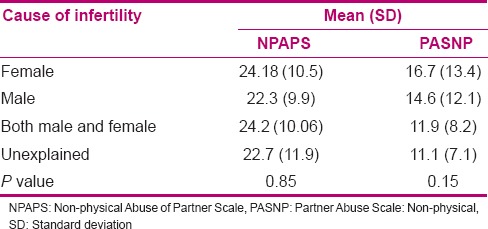
Table 3.
The relationship between infertility factors, and NPAPS and PASNP in men
RESULTS
Female and male subjects’ mean ages were 27.5 and 31.9 years, respectively. About 90.8% of the men and 26.9% of the women were working. The highest education level of the men and women was high school diploma (43.5% and 46.6%, respectively). Mean length of infertility was 4.5 years (ranging 1–26 years). The most common cause of infertility (31.3%) was male factor, and the least (17.5%) was combination factor. As shown in Table 1, the mean scores of NPAPS were 23.1 ± 10.3 in men and 21.3 ± 10.6 in women out of 100. The mean scores of PASNP were 13.8 ± 1.9 in men and 20.3 ± 13.4 in women out of 100. Independent t-test showed no significant difference in the mean scores of NPAPS between men and women (P = 0.165), although the mean scores of PASNP showed a significant difference between men and women (P < 0.001).
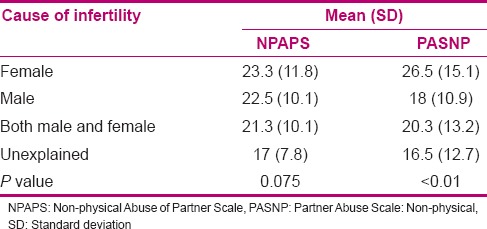
The highest scores of NPAPS and PASNP were 23.3 and 26.5 in female factor, while the lowest were 17 and 16.5 in idiopathic factor among infertile women. One-way analysis of variance (ANOVA) showed no significant association between infertility factor and score of NPAPS, while it showed a significant association between PASNP and female factor of infertility (P < 0.01) [Table 2]. The results showed that when the infertility factor was female factor or combination factor, NPAPS had the highest mean score of 20.2 among infertile men. Meanwhile, one-way ANOVA showed no significant association between infertility factor and the score of NPAPS (P = 0.85). When the female factors was a cause of infertility the highest score of PASNP (16.7) in men was observed. Meanwhile, one-way ANOVA showed no significant association between the factor of infertility and NPAPS in men (P = 0.15) [Table 3].
Table 2.
The relationship between infertility factors, and NPAPS and PASNP in women
DISCUSSION
The results of the present study showed that the most common cause of infertility was male factor, which is consistent with the studies of El Kissi et al.[13] and Chiaffarino et al.[14] Meanwhile, Volgsten et al., in Sweden, reported female factor, idiopathic factor, and male factor as the causes for infertility respectively.[15] Li et al., in a study conducted in China, reported idiopathic factor as the most common cause for infertility (43.9%), while female factor (20.8%), male factor (20.3%), and combined factor (15%) were ranked after that, respectively.[16] Direkavand Moghadam et al., in thier meta-analysis study, reported an equal rate for male and female factors of infertility.[17] With regard to the aforementioned studies, it is found that the prevalence of infertility has been reported differently in various studies. It should be noted that in references, the male factor was reported to be 25–40%, the female factor 40-55%, the combined factor 10%, and the idiopathic factor was reported as 10%.[2] Nowadays, there is an ascending trend for the male factor of infertility due to an increase in industrial occupations and more involvement of men in industries, as well as their contact with environmental and industrial pollutants.[18] Isfahan Infertility Center (from which most of the subjects were selected) acts as a referral infertility center where couples with a diagnosed infertility factor are referred from other cities to receive professional treatment and undergo fertility assistive techniques. This can be the reason for the high prevalence of male factor infertility found in the present study. There is no doubt that having a child plays a pivotal role in couples’ happiness in their marital life. When they are deprived from having their biological offspring in their common life, they not only miss the meaning in their life but also develop conflicts in their interpersonal communication,[19] which predisposes them to mental and psychological problems such as anxiety, depression, and mental pressure, consequently leading to domestic violence.[4] The results of the present study showed that NPAPS was lowered in women, compared to men, although the mean scores of NPAPS showed no significant difference between men and women. PASNP was also found to be more among women, compared to men, but its mean score showed a significant difference between men and women. Several studies showed that infertility and the attitude toward that puts the couples in an emotional crisis, and meantime, couples’ negative self-concept and low self-esteem drive them toward inappropriate behaviors such as violence to relieve their discomfort.[7] Other studies on domestic violence investigated the NPAPS just from the viewpoint of one of the couples. Meanwhile, in the present study, in addition to NPAPS, the adopted questionnaire investigated PASNP from the viewpoint of both the couples.
Akyuz et al., in a study on infertile women, showed a significant association between the score of violence and infertility factor in such a way that the level of violence was higher in infertility with female factor.[20] One study has reported the rate of domestic violence as 61.8% among infertile women, although all the participants were women with female factor infertility.[10] As the results of the present study showed no significant difference in the factor of infertility and NPAPS, and mean NPAPS was not high in women, it can be reasoned that as women with female factor infertility felt somehow defective, they manifested a higher PASNP, although they did not really undergo a higher behavioral abuse.
Hassanin et al. believe that infertility causes hopelessness in women and affects their marital relationship. They argue that infertile women are more predisposed to depression, anxiety, stress, and stressful events that can make a potential background for behavioral abuse.[21] One of the major goals of marriage in women is fertility, and infertility, in fact, ruins this value. Therefore, women accept to undergo difficult fertility techniques to preserve their condition, which may predispose them to many mental diseases, depression, and other psychological disorders.[22] On the other hand, infertile women face other threats such as a divorce or their spouse's remarriage,[15] which notably affect their PASNP.
CONCLUSION
The results showed that infertility can act as a factor to make the couples closer to each other and to have a mutual cooperation in infertility treatment, and generally improves their marital relationship, as their NPAPS and PASNP were found lower in this group of couples in the present study, compared to other studies. Meanwhile, in case of female factor infertility, women manifested a higher PASNP. Both couples should be simultaneously considered in fertility counseling sessions, as well as in medical and clinical treatments given by infertility centers and the associated professionals. In addition, infertility treatment should be accompanied with psychological treatments too.
Financial support and sponsorship
Department of Midwifery in Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors gratefully acknowledge support from the Department of Midwifery and Nursing and providers of Isfahan clinics.
REFERENCES
- 1.Speroff L, Fritz MA. Clinical Gynecologic Endocrinology and Infertility. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 2011. p. 1137. [Google Scholar]
- 2.Berek JS. Berek and Novak's Gynecology. 15th ed. Philadelphia: Lippincott Williams and Wilkins; 2012. p. 1970. [Google Scholar]
- 3.Vahidi S, Ardalan A, Mohammad K. The epidemiology of primary infertility in the Islamic Republic of Iran in 2004-5. J Reprod Infertil. 2006;7:243–51. [Google Scholar]
- 4.Aliyeh G, Laya F. Quality of life and its correlates among a group of infertile Iranian women. Med Sci Monit. 2007;13:CR313–7. [PubMed] [Google Scholar]
- 5.Monga M, Alexadrescu B, Katz S, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment and sexual function. Urology. 2004;63:126–30. doi: 10.1016/j.urology.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 6.Lee TY, Sun GH, Chao SC. The effect of an infertility diagnosis on the distress marital and sexual satisfaction between husbands and wives in Taiwan. Hum Reprod. 2001;16:1762–7. doi: 10.1093/humrep/16.8.1762. [DOI] [PubMed] [Google Scholar]
- 7.Etesami Pour R, Banihashemian K. Comparison of sex disorders couple abuse among fertile and infertile women. J Birjand Univ Med Sci. 2011;18:10–7. [Google Scholar]
- 8.The World Health Organization (WHO) Multi-country study on women health and domestic violence against women, initial results on prevalence, health out com and women's responses, 2005. [Last accessed on 2016 May 16]. Available from: http://www.who.int/reproductivehealth/publications/violence/24159358X/en/
- 9.Yildizhan R, Adali E, Kolusari A, Kurdoglu M, Yildizhan B, Sahin G. Domestic violence against infertilie women in Turkish setting. Int J Gynaecol Obstet. 2009;104:110–2. doi: 10.1016/j.ijgo.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Behboodi-Moghadam Z, Salsali M, Eftekhar-Ardabily H, Vaismoradi M, Ramezanzadeh F. Experiences of infertility through the lens of Iranian infertile women: A qualitative study. Jpn J Nurs Sci. 2013;10:41–6. doi: 10.1111/j.1742-7924.2012.00208.x. [DOI] [PubMed] [Google Scholar]
- 11.Leung TW, Ng EH, Leung WC, Ho PC. Intimate partner violence among infertile women. Int J Gynecol Obstet. 2003;83:323–4. doi: 10.1016/s0020-7292(03)00298-4. [DOI] [PubMed] [Google Scholar]
- 12.Corcoran K, Fischer J. Measures for Clinical Practice and Research: Couples, Families, and Children. 5th ed. New York, NY: Oxford University Press; 2013. pp. 149–53. [Google Scholar]
- 13.El Kissi Y, Romdhane AB, Hidar S, Bannour S, Ayoubi Idrissi K, Khairi H, et al. General psychopathology, anxiety, depression and self-esteem in couples undergoing infertility treatment: A comparative study between men and women. Eur J Obstet Gynecol Reprod Biol. 2013;167:185–9. doi: 10.1016/j.ejogrb.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 14.Chiaffarino F, Baldini MP, Scarduelli C, Bommarito F, Ambrosio S, D’Orsi C, et al. Prevalence and incidence of depressive and anxious symptom in couples undergoing assisted reproductive treatment in an Italian infertility department. Eur J Obstet Gynecol Reprod Biol. 2011;158:235–41. doi: 10.1016/j.ejogrb.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 15.Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist O, Sundström Poromaa I. Risk factors for psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Fertil Steril. 2010;93:1088–96. doi: 10.1016/j.fertnstert.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Li L, Zhang Y, Zeng D, Li F, Cui D. Depression in Chinese men undergoing different assisted reproductive technique treatment: Prevalence and risk factors. J Assist Reprod Genet. 2013;30:1161–7. doi: 10.1007/s10815-013-0057-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Direkavand Moghadam A, Delpisheh A, Sayehmiri K. The prevalence of infertility in Iran. Asystematic Review. IJOGI. 2013;16:1–7. [Google Scholar]
- 18.Sheiner EK, Sheiner E, Carel R, Potashnik G, Shoham-Vardi I. Potential association between male infertility and occupational psychological stress. J Occup Environ Med. 2002;44:1093–9. doi: 10.1097/00043764-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Tabrizi GH, Tabrizi S, Vatankhah M. Female Infertility Resulting in Sexual Disorders and Wife Abuse. Pazhuheshname-Ye Zanan (Women's Studies) 2011;1:1–9. [Google Scholar]
- 20.Akyuz A, Seven M, Sahiner G, Bilal B. Studying the effect of infertility on marital violence in Turkish women. Int J Fertil Steril. 2013;6:286–93. [PMC free article] [PubMed] [Google Scholar]
- 21.Hassanin IM, Abd-El-Raheem T, Shahin AY. Primary infertility and health-related quality of life in Upper Egypt. Int J Gynaecol Obstet. 2010;110:118–21. doi: 10.1016/j.ijgo.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 22.Sheikhan Z, Ozgoli G, Azar M, Hosseini F, Nasiri M, Amirii S. Prevalence of sexual violence among infertile women attended to. Tehran of infertility centers. J Shahid Beheshti School of Nurs Midwife. 2011;23:55–61. [Google Scholar]


