Abstract
Background:
Nurses’ clinical competency plays an important role in the care of preterm infants. On the other hand, burnout is one of the most important factors in reducing the nurses’ efficiency. With regard to the importance of the role of nurses, and the vulnerability of the infants, the purpose of this study was to investigate the relationship between nurses’ burnout and clinical competency in NICUs.
Materials and Methods:
The descriptive cross-sectional study was conducted with the participation of 86 nurses working in the NICUs of hospitals in Isfahan, Iran. Census sampling method was used in the NICUs of educational hospitals in 2014. Data were collected by a questionnaire including demographic characteristics, Patricia clinical competency, and Maslach burnout scales. Data were analyzed by the statistical tests of independent t-test and Pearson correlations test with the significance level of α < 0.05.
Results:
Six dimensions of clinical competency and three dimensions of nurses’ burnout were assessed at three levels (weak, moderate, and strong levels). Statistical tests showed that clinical competency was at a moderate level in all fields. Of the dimensions of nurses’ burnout, emotional exhaustion was moderate, depersonalization was weak, and personal performance was strong. The results showed that nurses’ burnout and clinical competency in the NICUs were at a moderate level and had a significant negative relationship (r = −0.322, P = 0.003).
Conclusions:
Results showed that burnout had a negative relationship with competency. Therefore, managers are suggested to improve nurses’ competency and diminish their job burnout through better and more applicable planning.
Key words: Clinical competency, infant, job burnout, NICU, nurses, Iran
INTRODUCTION
Nowadays, the factors associated with high-risk pregnancies lead to an increasing trend of premature and low-weight-birth infants. The number of premature neonates requiring NICU hospitalization is increasing.[1] Nurses, as the biggest group of care providers for critical care, especially in the NICU, carry out most of the care.[2,3] Relatively huge increase in the number of NICUs and the improved progressive technology demand professional care from competent nurses.[2] Clinical competency is used as an index for evaluation and accreditation in the hospitals. It is of great importance in the NICU. Clinical competency is the wise application of technical and communicational skills, knowledge, clinical reasoning, emotions, and values in clinical setting.[4] It influences the quality of given nursing care. Full access to clinical competency enables the nurses to play their role and do their duties with a proper quality.[5] Several interpersonal factors (experience, opportunities, environment, personal characteristics, motivation, and theoretical knowledge) and extra-personal factors (rapid change of health monitoring system, necessity of giving safe and cost-effective services, promotion of public awareness, increase in expectation to receive high-quality care) are effective on nurses’ clinical competency.[3,6,7] Although motivation is an important factor in acquiring clinical competency, nurses believe that some occupational issues such as equality of competent and non-competent staff in managers’ viewpoint and no clear job description of nurses, as disappointing factors, have more negative effect on their motivation to attain clinical competency.[8] Research shows that these problems also exist in Iran and are accompanied with outcomes such as reduction of motivation and, in some cases, nurses’ burnout and quitting work.[9] Although there are studies on the factors effective in acquiring clinical competency and its effect on the quality of services and patients’ satisfaction, the association between clinical competency and job burnout as an important phenomenon in high-risk professions, especially nursing, has been less considered. Job burnout refers to physical and psychological boredom resulting from existing pressures at work, staffs’ reduction of physical power, and their frustration and isolation.[10] Rahmani et al. showed that about half of the nurses in Tabriz experience a high level of stress and job burnout.[11] Job burnout, in addition to its effect on various dimensions of individuals’ life, has negative impacts on patient care quality, nurses’ physical and mental health, and staff's treatment and official costs.[11,12] Research showed that in each working day, one out of seven staff experiences boredom and job burnout.[13] Probably, the nurses who experience high job burnout are less satisfied with their profession.[5] Nurses’ job burnout in pediatric ward and ICU is high.[5,12] Nevertheless, researchers’ search found no study on nurses’ clinical competency and their job burnout in the NICU. Therefore, it seemed necessary to investigate job burnout, clinical competency, and their association in NICU nurses. In addition, due to working and environmental conditions in the NICUs, it seems that the results of the present study will be different from those in adult wards. The present study aimed at investigation of the relationship between nurses’ burnout and clinical competency in the NICUs.
MATERIALS AND METHODS
This is a descriptive cross-sectional study conducted on 86 nurses working in the NICUs of educational hospitals affiliated to Isfahan University of Medical Sciences. In this study, the researchers, after following research ethics principles and obtaining permission from the authorities and Isfahan University of Medical Sciences ethics committee, referred to educational hospitals in Isfahan. The nurses who met the inclusion criteria were selected by census sampling. Informed consent was obtained based on the personal interest of the subjects to attend the study. In addition, the researcher assured the subjects about confidentiality of their information and their option of leaving the study whenever they liked. Subjects included all nurses working in the NICUs of educational hospitals in Isfahan with a bachelor's degree and over, who did not suffer from anxiety and depression and were not taking psychotropic medications.
Exclusion criteria were lack of interest to attend the study and being on any type of work leave at the time of data collection (unpaid vacation, delivery leave, and educational leave). It should be noted that nurses completed the questionnaires in all three working shifts. To describe the subjects, descriptive and analytical statistical tests including frequency distribution, central indexes, dispersion, independent t-test, and Pearson correlation coefficient with a significance level of α <0.05 were adopted. Data collection tool was a three-section questionnaire including demographic information, Patricia clinical competency, and Maslach job burnout questionnaire. The clinical competency questionnaire included six domains with 52 items on nurses’ activities; the six domains consisted of leadership (5 items), critical situations (7 items), education and cooperation (11 questions), administration and evaluation (7 items), making communication and interpersonal communication (12 items), and professional promotion (10 items). Through this tool, activities are evaluated by the scores of the items (1 = very good, 2 = good, 3 = acceptable, 4 = not so acceptable). Nurses’ clinical competency was evaluated by Patricia Schwirian method, so that the mean score was calculated in each domain, with scores ranging from 1 to 4, categorizing nurses’ clinical competency in three levels of weak, moderate, and strong. Mean scores less than 2 were considered as weak, scores between 2 and 3 as moderate, and mean scores over 3 were reported as strong. Job burnout questionnaire has 22 items in three domains of emotional exhaustion (9 items), depersonalization (5 items), and lack of personal performance (8 items), which are scored by a seven-point Likert's scale (never = 0, sometimes in a year (= 1, once a month = 2, sometimes in a month = 3, once a week = 4, some days in a week = 5, and everyday = 9), with scores ranging between 0 and 132. Job burnout scores between 45 and 88 showed moderate times of exposure and number 32≥ showed lower times of exposure. Job burnout dimensions were scored in such a way that in the domain of emotional exhaustion, scores ≤17 showed lower number of exposures, scores between 18 and 29 showed moderate exposure, and scores ≥30 showed higher number of exposures to emotional exhaustion. In the domain of depersonalization, scores ≤5 showed lower number of exposures, scores 6–11 showed moderate exposures, and scores ≥12 showed higher number of exposures to depersonalization. In the domain of personal performance, scores ≤40 showed low exposure, scores 34–39 showed moderate exposure, and scores ≥33 showed severe exposure.[5,12,14,15] Reliability of Maslach job burnout standard scale was firstly confirmed by Filian in Iran through test re-test (Cronbach's alpha coefficient of .78), and then, it was used in several Iranian studies.[16] Its validity and reliability were confirmed in several studies in Iran with the Cronbach alpha values reported as 0.71–0.90 and 0.60–0.80, respectively.[7,17] Maslach and Jackson calculated the internal reliability of each domain. Internal reliability was indicated by the Cronbach alpha of .71–.90 and the test re-test index of .60–.80. The internal reliability for each domain was as follows: r = 0.90 for emotional exhaustion, r = 0.79 for depersonalization, and r = 0.71 for personal performance. Its validity was reported to be high in various studies.[12] Najafi et al. reported the reliability of this test as Cronbach alpha = 0.86 and for its domains as 0.78, 0.89, and 0.83, respectively.[18] Validity and reliability of standard clinical competency questionnaire was investigated and confirmed by Shateri with a Cronbach alpha value of 0.94.[19]
RESULTS
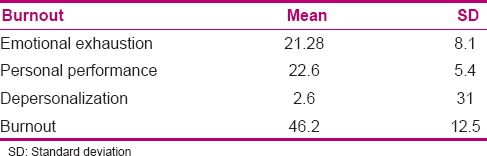
The findings showed that the mean age of the subjects was 34 (5.1) years and the mean work experience was 10 (8-4) years. Almost all subjects had a bachelor's degree and half of them liked to work in the NICU [Table 1]. Results showed that the mean score of job burnout was at a moderate level. It was at a moderate level in the domain of emotional exhaustion, at a strong level in lack of personal performance, and at a weak level in the domain of depersonalization [Table 2]. Clinical competency was investigated in the six domains at three levels of weak, moderate, and strong.
Table 1.
Frequency distribution of subjects’ baseline information (number, percent, mean, SD)
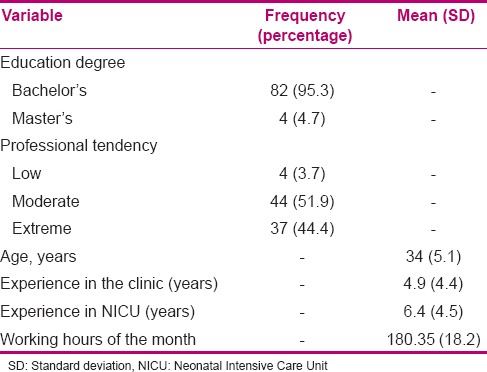
Table 2.
Mean (SD) of subjects’ job burnout and its domains
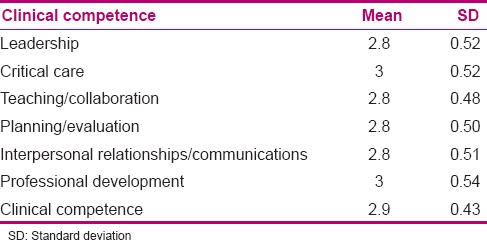
Results showed that clinical competency score was at a moderate level and nurses’ clinical competency was moderate in all domains (it was 3 and 2.9 in the domains of critical situation and professional promotion, respectively) [Table 3]. The goal of the study was to investigate the relationship between nurses’ burnout and clinical competency in the NICUs, and the results showed a negative correlation between these two variables (r = −0.322, P = 0.003).
Table 3.
Mean (SD) of nurses’ clinical competence and its domains
DISCUSSION
Results showed that not only nurses’ mean clinical competency score but also their clinical competency scores in its six domains were at a moderate level. Nurses’ clinical competency is of great importance in ICUs and NICUs as it is tightly associated with nursing care quality and patients’ health and life. Research in Iran showed that clinical competency was at a strong level among a few nurses in Iran.[19,20] In the present study, existence of working nurses with moderate clinical competency in the NICUs is notable, as clinical competency affects nursing care quality and clients’ safety and satisfaction. Neonates are the vulnerable class of society and are very susceptible clients who are hospitalized in NICUs. Therefore, their care providers should be at a high level of clinical competency. This issue should be notified, and more efficient steps should be taken to promote NICU nurses’ clinical competency to diminish the hazards imposed on neonates. In similar studies conducted in the NICUs in Iran, nurses’ clinical competency was reported to be moderate in most of the domains. It can be inferred that clinical competency in different domains is acquired in the student period, but it is not complete and it takes time to reach a proper level. The results of the present study and similar studies showing moderate clinical competency in critical situations, as well as the effect of nursing services on the quality of health services, especially in NICU, should be closely observed. Almost all patients hospitalized in NICUs are critical and need critical care. This point has been emphasized in many studies, as the level of skill in NICU is a basic foundation of clinical competency.[20] Moderate level of clinical competency of nurses in the domain of administration and evaluation, reported in the present study and similar studies, is of great importance, as it is the basis for decision making and is an important feature of evaluation and quality control. Empowerment of administration and patients’ proper evaluation result from the integration of education and clinical setting. As many situations in the NICUs need rapid decision making, ability of judgment, and administration and proper evaluation, NICU nurses should essentially have this skill.[19] Nurses’ moderate score of clinical competency in the domain of education is important, as nursing is higher in theoretical aspect, compared to clinical aspect, possibly due to less control of the educators and its own more sophistication.[21] NICU nurses’ moderate score of clinical competency in the domain of education could result from lack of emphasis on professional education as a component of nursing services. Nursing education in universities and continuing education classes in NICUs should provide a background for efficient and practical education to increase nurses’ skill in education and, consequently, improve NICU nurses’ clinical competency. Ability to make correct and efficient communication is an important feature that all healthcare staffs should have. Good professional relationships increase the efficiency of nurses, improve the conditions of patients and reduce costs and reduce patient anxiety leading role in increasing competence of occupational nurses. May lack good working relationship with colleagues of the causes of anxiety and tension in relations professional nurses in nursin. Tension is increased in ICUs with regard to the role of nurses and the need for decision making in critical conditions. Participation in communication skills courses and classes is a solution to diminish existing tension.[22] Professional promotion has been reported as moderate in Iran. As professional promotion and acquiring clinical competency in nursing are not only a constant process but also reflect individuals’ personal and professional progression, all nurses should achieve professional promotion, which is based on education, in order to acquire clinical competency.[23]
Results of the present study showed that job burnout mean score was moderate in the domain of emotional exhaustion and strong and weak in the domains of lack of personal performance and depersonalization, respectively. Meanwhile, in other studies, nurses’ job burnout was high, revealing that its dimensions were not appropriate.[16,24] Nurses’ job burnout shows a significant difference in various wards and has the highest level in NICUs.[5,8] In previous research, emotional exhaustion was reported not only to be most highly studied and investigated and to be more common among nurses working in ICU, compared to other wards, but also to be the first and the most common sign of job burnout.[25,26] Emotional evacuation exists among ICU nurses who spend long hours with critical patients.[13] With regard to working condition of NICU nurses, the present study showed better condition of the studied nurses concerning depersonalization, although in two other domains, especially personal performance, the condition was at a lower level. Therefore, through human resources, proper management such as determination of proper duties and strategies, balanced with nurses’ ability, new approaches for encouragement and motivation, and holding stress control workshop, the sense of commitment and positive feeling toward work and personal capability can be empowered in individuals.
In the present study conducted in NICU, nurses’ job burnout was at a moderate level. About 9.61% or 12.9 million premature infants are born annually around the world.[22] About 19,000 deaths occur due to complications such as premature birth, congenital anomalies, low weight, bacterial sepsis, asphyxia, and other birth complications. Most of these deaths occur in NICUs.[27] Therefore, it is a stressful environment for the nurses working there and predisposes the nurses to job burnout. With regard to neonates’ susceptibility and the effect of job burnout on nurses’ efficiency, the associated causes should be detected and modified. Investigation of job burnout and clinical competency in NICUs showed a negative correlation between clinical competency and job burnout at a weak level, but no similar study was found. Achieving a specific ability to care for a specific population needs experimental learning opportunities. Professional staff may have the ability and skill to take care of adults, but may lack the capability to take care of premature neonates.[28] Although the present study was conducted in NICU where the nurses have proper chance to obtain experience and learn in a real environment, existence of moderate job burnout in this ward due to environmental and working conditions of the nurses working in the ward can diminish opportunity to study and research leading to reduced clinical competency.
Increasing rate of birth of premature and low weight infants has increased NICU hospitalization, and scientific advancements and high technology have increased their survival. Therefore, professional care of the staff, especially nurses, in these wards is needed.
Existence of skillful, competent, and experienced nurses in NICUs is important. The factors associated with clinical competency should be considered more, since through recognition and control of these factors, proper strategies can be achieved to improve clinical competency.[18,22] There are important factors that lead to motivation for decision making in any level of services, such as the crucial role of clinical competency on nursing care quality, patients’ safety, and satisfaction and promotion of clinical competency through using experienced nurses to guide the fresh nurses or hiring nurses with higher clinical competency with a focus on nursing care quality. Therefore, increasing the clinical competency and reduction of job burnout, and ultimately, increasing the nursing care quality seem to be essential.[20,25] Our results showed an association between weak level of clinical competency and job burnout, while moderate level of clinical competency and job burnout in NICUs and their relationship should be investigated further.
Limitations
Low sample size was the limitation of this study, as it just recruited the nurses working in the NICUs affiliated to Isfahan University of Medical Sciences. Therefore, further studies with a higher sample size are suggested to compare the results with those of the present study.
CONCLUSION
Job burnout was reported to be moderate in this study, which is rational with regard to different nature of work in various wards. With regard to neonates’ susceptibility and the fact that job burnout affects nurses’ work notably, its causes should be detected and modified. Nurses’ clinical competency was reported as moderate in this study. Promotion of NICU nurses’ clinical competency needs promotion of its dimensions. This issue can be closely watched by nurse managers and planners to promote nurses’ clinical competency through education. Our results showed an inverse association between job burnout and clinical competency, such that more clinical competency brings about less job burnout among the staffs and vice versa. Managers are suggested to have better and more applicable programs and make a positive background for promotion of nurses’ clinical competency and reduction of their job burnout.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The researchers greatly appreciate all authorities in the Isfahan University of Medical Sciences and the nurses who helped them in this project.
REFERENCES
- 1.Malusky S, Donze A. Neutral head positioning in premature infants for intraventricular hemorrhage prevention: An evidence-based review. Neonatal Netw. 2011;30:381–96. doi: 10.1891/0730-0832.30.6.381. [DOI] [PubMed] [Google Scholar]
- 2.Cowan DT, Norman I, Coopamah VP. Competence in nursing practice: A controversial concept-a focused review of literature. Nurse Educ Today. 2005;25:355–62. doi: 10.1016/j.nedt.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Memarian R, Salsali M, Vanaki Z, Ahmadi F, Hajizadeh E. Professional ethics as an important factor in clinical competency in nursing. Nurse Ethics. 2007;14:203–14. doi: 10.1177/0969733007073715. [DOI] [PubMed] [Google Scholar]
- 4.Bahraini M, Moattari M, Akaberian SH, Mirzaie K. Determining nurses’ clinical competence in hospitals of Bushehr University of Medical Sciences by self-assessment method. Iranian South Med J. 2008;11:69–75. [Google Scholar]
- 5.Abdi F, Kaviani H, Khaghanizadeh M, Momeni A. Relationship between burnout and mental health. Tehran Univ Med J. 2007;65:65–75. [Google Scholar]
- 6.Berkow S, Virkstis K, Stewart J, Conway L. Assessing new graduate nurse performance. Nurs Educ. 2009;34:17–22. doi: 10.1097/01.NNE.0000343405.90362.15. [DOI] [PubMed] [Google Scholar]
- 7.Ghomi R. A Thesis Submitted to the Graguated Studies Office in Partial Fulfillment of the Requirement for the Degree in Neonatal Nursing. Tehran, Iran: Tehran University of Medical Sciences; 2013. Surveying the Nurses’ Clinical Competency, Working in Neonatal Intensive Care Unit (NICU) in Hospitals Affiliated to Tehran University of Medical Sciences; pp. 10–25. [Google Scholar]
- 8.Parsayekta Z, Ahmadi F, Tabari R. The factors influencing the clinical competence of the nurses. J Guilan Uni Med Sci. 2004;54:21–9. [Google Scholar]
- 9.Jaarsma T. Keeping Cardiac nurses on the job. Eur J Cardiovasc Nurs. 2003;2:93–4. doi: 10.1016/S1474-5151(03)00050-1. [DOI] [PubMed] [Google Scholar]
- 10.Esfandiyari GH. Investigation of burnout among nurses working in hospitals in Sanandaj. J Kurdistan Uni Med Sci. 2001;1:32. [Google Scholar]
- 11.Rahmani F, Rahmani D, Behshid M, Zamanzadeh V. The relationship between Public health communication, stress and burnout in nurses in Tabriz University of Medical Sciences. Iranian J Nur. 2010;23:1–2. [Google Scholar]
- 12.Nastizaie N, Vaezi M, Molazehi A, Hezaremoghadam M. The relationship between burnout and psychological health of staff handle all communications Zahedan. J Heal Res Yazd. 2008;7:49–57. [Google Scholar]
- 13.Almasian A, Rahim Kia A. Study of the relationship between leadership style and burnout in university staff 1390. Quart Res J Lorestan Uni Med Sci Yafteh. 2011;1:69–70. [Google Scholar]
- 14.Maleaky N, Bahbode Mogadam Z. A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Nursing Midwifery. Tehran, Iran: Tehran Medical Sciences; 1391. The Prevalence of Burnout and the Factors Related to the Midwives Hospitals to Tehran Medical Sciences; p. 42. [Google Scholar]
- 15.Hosseini M, Sharifzadeh G, Khazaei T. Occupational burnout in Birjand dentists. J Dent Med Heal Serv. 2011;24:113–20. [Google Scholar]
- 16.Filian A. Master's Thesis. Tehran, Iran: University of Medical Sciences, Tarbiat Modarres Nursing; 2010. Evaluation of Burnout and its Relation to Coping Strategies used by Nurses in Teaching Hospitals in Tehran. [Google Scholar]
- 17.Leiter MP, Maslach C. Burnout. Ency Men Heal. 1998;1:347–57. [Google Scholar]
- 18.Najafi M, Solati Dehkordy SK, Frvzbkhsh F. The relationship between job burnout and mental health among employees of Esfahan's Center for research and production of nuclear fuel. J Shahrekord Univ Med Sci. 2000;2:34–41. [Google Scholar]
- 19.Shateri M. Tehran University of Medical Sciences Faculty of Nursing and Midwifery: A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Nursing. Tehran, Iran: Tehran University of Medical Sciences; 2012. Evaluating Nurses Clinical Competency in Intensive Care Units on Tehran University Hospitals; pp. 22–6. [Google Scholar]
- 20.Aäri RL, Tarja S, Helena LK. Competence in intensive and critical care nursing: A literature review. Intensive Crit Care Nurs. 2008;24:78–89. doi: 10.1016/j.iccn.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 21.Sheikhi M, Fallahi KM, Mohammadi F, Oskouie F. Nurses experience of flourishing work environment in career advancement: A qualitative study. J Qazvin Univ Med Sci. 2015;18:55–62. [Google Scholar]
- 22.Istomina N, Suominen T, Razbadauskas A, Martinkënas A, Meretoja R, Leino-Kilpi H. Competence of nurses and factors associated with it. Medicina (Kaunas) 2011;47:230–7. [PubMed] [Google Scholar]
- 23.Oerman MH. Developing a professional portfolio in nursing. Orthop Nurs. 2002;21:73–8. doi: 10.1097/00006416-200203000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Richard J, Peter E. Nursing and healthcare management and police. J Adv Nurs. 2004;48:622–30. [Google Scholar]
- 25.Bradham KM. Empathy and Burnout in Nurses. Chicago: Institute for Clinical Social Work; 2008. pp. 78–102. [Google Scholar]
- 26.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 27.Brooks DM, Bradt J, Eyre L, Hunt A, Dileo C. Creative approaches for reducing burnout in medical personnel. The Arts in Psychotherapy. 2010;37:255–63. [Google Scholar]
- 28.Benner P. Using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bul Sci Tech and Soc. 2004;24:188–99. [Google Scholar]


