Abstract
The treatment of choice for necrotic teeth with immature root is apexification, which is induction of apical closure to produce more favorable conditions for conventional root canal filling. The most commonly advocated medicament is calcium hydroxide although recently considerable interest has been expressed in the use of mineral trioxide aggregate (MTA). MTA offers the option of a two-visit apexification procedure so that the fragile tooth can be restored immediately. However, difficulty in placing the material in the wide apical area requires the use of an apical matrix. Materials such as collagen, calcium sulfate, and hydroxyapatite have been used for this purpose. This article describes the use of resorbable suture material to form the apical matrix which offers many advantages over the contemporary materials.
Keywords: Apexification, matrix, mineral trioxide aggregate, resorbable suture
INTRODUCTION
Management of immature root with a necrotic pulp and apical periodontitis is a challenging task. The infected root canal space cannot be disinfected with the standard protocol. Obturation of the root canal is difficult because of lack of apical barrier for containing the root filling material. Treatment of choice in such cases is the apexification procedure, i.e., establishing an apical barrier. Calcium hydroxide has been widely used for the induction of hard tissue barrier. However, this material requires 5–20 months to form the hard tissue barrier.[1] It has also been shown that the use of calcium hydroxide weakens the resistance of the dentin to fracture.[2] In recent times, mineral trioxide aggregate (MTA) has gained widespread popularity for the apexification procedure. It produces apical hard tissue formation with significantly greater consistency than calcium hydroxide.[3] MTA, a biocompatible material, can be used to create a physical barrier. It also helps in the formation of bone and periodontium around its interface.[4] A bonded restoration can be placed without any delay, thus reducing the possibility of root fractures. Various authors have reported clinical success using MTA for one-visit apexification. The major disadvantage of MTA is its manipulation due to which its placement in the wide apical area is difficult to achieve. A matrix can be used in apexification procedures against which MTA can be placed and condensed. Use of an apical matrix allows for the predictable placement and judicious use of this expensive material. Several materials have been recommended to create a matrix including calcium sulfate, hydroxyapatite, resorbable collagen, and platelet-rich fibrin.[5,6,7] In this case series, we are presenting two cases of MTA apexification using polyglactin-based resorbable suture material as the apical matrix.
CASE REPORTS
Case 1
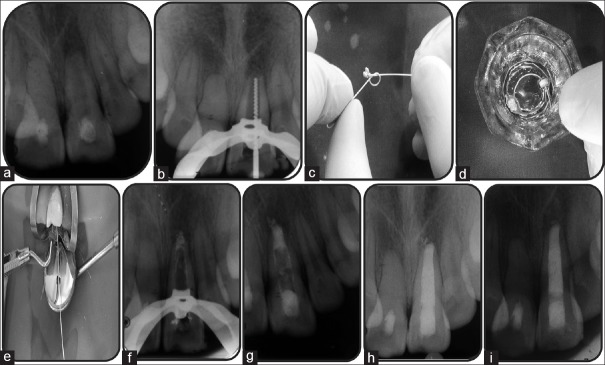
A 16-year-old male patient reported with a chief complaint of discolored maxillary left central incisor. History revealed that the patient had suffered trauma 8 years back and undergone treatment in a private clinic. The medical history was not significant. Clinical examination revealed grayish discoloration of tooth 21 and attempted access preparation in the same tooth. The tooth did not demonstrate any abnormal mobility or sensitivity to percussion. Both cold and electric sensibility tests failed to elicit any response. Periapical radiograph showed well-defined periapical radiolucency and wide open apex in relation to tooth 21 [Figure 1a]. The final diagnosis was pulpal necrosis with chronic apical periodontitis in relation to tooth 21. After discussing different treatment options with the patient's parents, we opted to go for MTA apexification with the use of an apical matrix. Written consent was obtained from the guardian of the patient. After rubber dam isolation, the tooth 21 was accessed and working length was established radiographically [Figure 1b]. Root canal was chemo-mechanically debrided with circumferential filing using the International Organization for Standardization (ISO) 80 K-file (Dentsply Maillefer, Switzerland) in conjunction with copious amount of 0.5% sodium hypochlorite (Shivam Industries, India). A volume of 3 ml of 17% ethylenediaminetetraacetic acid (EDTA) solution (Prevest Denpro, India) was used for smear layer removal. ApexCal medicament paste (Ivoclar Vivadent AG Schaan, Liechtenstein) was placed in the root canal, and access cavity was restored with Temp Paste (Pyrex Exports, India). One week later, tooth was again accessed under rubber dam isolation, and copious amount of normal saline was used to remove any remnants of the calcium hydroxide medicament. Canal was thoroughly dried with absorbent paper points (Meta BioMed, Korea). Polyglactin-based resorbable suture material Vicryl (Johnson and Johnson Ltd., India) was used for the formation of apical matrix. One end of the suture material was modified to form a mesh, whereas the other end is left as such so that it could be used to adjust the position of apical matrix [Figure 1c]. Suture material was saturated with iodine-based radiographic contrast medium iopamidol (Bracco, Italy) for 10 min to render it radio-opaque [Figure 1d]. The matrix was gently placed on working length with the help of preselected hand pluggers [Figure 1e], and its position was verified using radiographs [Figure 1f]. Any adjustment required was done using the hand pluggers or free end of the suture material. White MTA Angelus (Angelus, Londrina, PR, Brazil) was mixed according to manufacturer's instructions and using hand pluggers, gently condensed against the matrix to form 4 mm of apical plug [Figure 1g]. After placing a moist cotton pellet, the access cavity was restored with Temp Paste (Pyrex Exports, India). Next day, root canal was obturated using lateral condensation of Gutta-percha (Meta BioMed, Korea) and AH-Plus root canal sealer (Dentsply Detrey GMBH, Germany), and tooth was restored with Brilliant NG bonded resin restoration (Coltene/Whaledent, Switzerland) [Figure 1h]. The patient was recalled after 3 months for clinical and radiographic evaluation. At the follow-up visit, clinical examination revealed normal mobility, probing depths, and normal function without symptoms. Radiograph demonstrated the resorption of the apical matrix and healing periapical lesion [Figure 1i].
Figure 1.
(a) Preoperative, (b) working length radiograph, (c-f) formation and placement of suture matrix, (g) mineral trioxide aggregate plug, (h) immediate postoperative, and (i) 3 month follow-up
Case 2
A 15-year-old female patient presented with the chief complaint of discomfort while chewing in front region of upper jaw. Patient gave a history of traumatic incident 9 years back for which she had visited a private clinic. Medical history was insignificant. Clinical examination revealed slightly grayish discolored tooth 21 and previously attempted treatment in the same tooth. The tooth was tender to percussion. Tooth also did not respond to cold and electric pulp vitality tests. Intraoral periapical radiograph showed a well-defined periapical radiolucency surrounding the wide open apex of tooth 21 [Figure 2a]. Diagnosis was pulpal necrosis with chronic apical periodontitis. After detailed discussion with the patient, we decided to perform MTA apexification procedure. Written consent was obtained from the patient's parents. After rubber dam isolation, tooth was assessed and working length determined using the radiograph [Figure 2b]. Root canal debridement was done using ISO 80 K-file (Dentsply Maillefer, Switzerland) and 0.5% sodium hypochlorite (Shivam Industries, India). A volume of 3 ml of 17% EDTA solution (Prevest Denpro, India) was used for smear layer removal. Root canal was medicated with ApexCal paste (Ivoclar Vivadent AG Schaan, Liechtenstein) for 1 week. After 1 week, 4 mm of MTA plug was formed by condensing white MTA Angelus (Angelus, Londrina, PR, Brazil) against Vicryl suture (Johnson and Johnson Ltd., India) apical matrix [Figure 2c and d]. Next day, the tooth was obturated using laterally condensed Gutta-percha (Meta BioMed, Korea) and AH-Plus (Dentsply Detrey GMBH, Germany) [Figure 2e]. Bonded composite resin Brilliant NG (Coltene/Whaledent, Switzerland) was used for definitive restoration. At the 3-month follow-up visit, the patient was asymptomatic, and the tooth showed no tenderness on percussion. Periapical radiograph revealed resorbed apical matrix and healing periapical lesion in relation to tooth 21 [Figure 2f].
Figure 2.
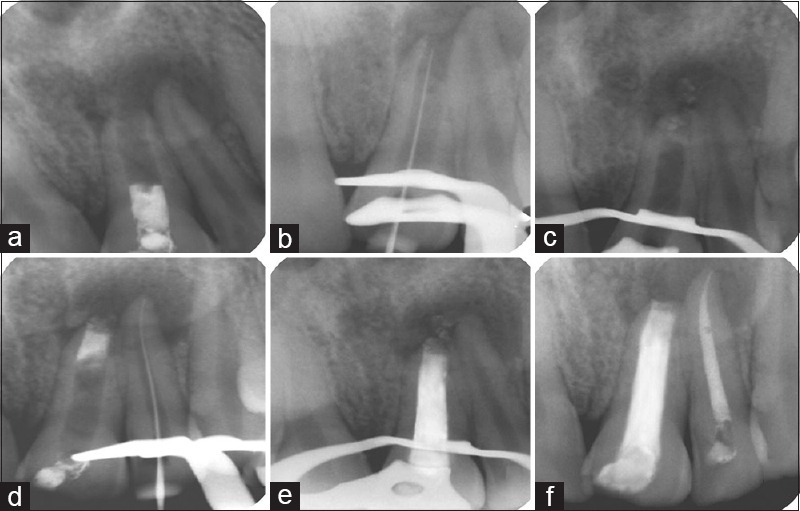
(a) Preoperative, (b) working length determination, (c) suture matrix in place, (d) mineral trioxide aggregate plug, (e) immediate postoperative, and (f) 3 month follow-up
DISCUSSION
Apexification is defined as a method to induce a calcified barrier in a root with an open apex or the continued apical development of an incomplete root in teeth with necrotic pulp. This barrier is mandatory to allow the compaction of the root filling material. Calcium hydroxide has been considered as an efficient material for this purpose.[8] This chemical has several disadvantages such as difficulty of the patient's recall management and delay in the treatment.[9] Furthermore, there is a risk of tooth fracture after dressing with calcium hydroxide for extended periods.[2] The most promising alternative to calcium hydroxide is MTA.[10] The advantages of this material are (i) reduction in treatment time, (ii) immediate restoration of the tooth, (iii) no adverse effect on the mechanical properties of root dentin. In a prospective study, apexification treatment with MTA showed a high prevalence of healing and apical closure.[11] The main disadvantage of MTA is its difficult manipulation. Placement of the material in a wide open area is a challenging task and also there is a risk of extruding this expensive material into periapical tissues. Lemon advocated the use of a matrix when the diameter of the perforation is larger than 1 mm to prevent the extrusion of sealing material. Similarly, a matrix can be used for the predictable placement of MTA in apexification procedures. Use of matrix provides a base against which the MTA can be packed.[12] Various materials have been advocated to be used as a matrix, for example, calcium sulfate, hydroxyapatite, collagen, platelet-rich fibrin. However, the materials mentioned are either not cost-effective or technique sensitive. Calcium sulfate has a very short setting time of 2 min.[13] Hydroxyapatite is an expensive material. The common limitation shared by these materials is that once placed their position can't be adjusted as required. These problems have been solved by the novel technique used in our cases. We used Vicryl, a resorbable suture material to form the apical matrix. Vicryl is a synthetic absorbable suture material composed of 90% polyglycolic acid and 10% polylactic acid. It resorbs within 56–70 days by hydrolysis.[14] It has better tissue reaction than catgut sutures.[15] It is commonly used in subcutaneous, intracutaneous, abdominal, and thoracic surgeries. However, the suture material lacks the radio-opacity which makes it difficult to be viewed in the radiographs. Iopamidol was used in our technique to impart radio-opacity to the suture material. It is a water soluble nonionic iodine-based contrast medium which is routinely used for angiography, arteriography, contrast-enhanced computed tomography, and urography. However, a proper history of the patient and sensitivity test should be done before using it. In our technique, one end of the suture material was used for the matrix formation, whereas other end was kept outside the tooth so that the placement of the matrix can be adjusted as required. No other known technique has this provision. After the matrix was placed at the desired position, the free end of the suture was cutoff and then MTA was condensed against it. The apical matrix mentioned here in our study is cost-effective, easily available, and provides for adjustment of its position.
CONCLUSION
Resorbable suture with a contrast agent may be used as a matrix for MTA placement but properly designed clinical trials with long-term follow-up are mandatory to support this novel technique as there is no evidence of such procedure available in the literature presently. Research concentrating on the effect of suture material and contrast media on the healing kinetics can further through some light on this technique.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sheehy EC, Roberts GJ. Use of calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: A review. Br Dent J. 1997;183:241–6. doi: 10.1038/sj.bdj.4809477. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18:134–7. doi: 10.1034/j.1600-9657.2002.00097.x. [DOI] [PubMed] [Google Scholar]
- 3.Shabahang S, Torabinejad M, Boyne PP, Abedi H, McMillan P. A comparative study of root-end induction using osteogenic protein-1, calcium hydroxide, and mineral trioxide aggregate in dogs. J Endod. 1999;25:1–5. doi: 10.1016/S0099-2399(99)80388-4. [DOI] [PubMed] [Google Scholar]
- 4.Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP. Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys. J Endod. 1997;23:225–8. doi: 10.1016/S0099-2399(97)80051-9. [DOI] [PubMed] [Google Scholar]
- 5.Alhadainy HA, Himel VT, Lee WB, Elbaghdady YM. Use of a hydroxylapatite-based material and calcium sulfate as artificial floors to repair furcal perforations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:723–9. doi: 10.1016/s1079-2104(98)90211-6. [DOI] [PubMed] [Google Scholar]
- 6.Bargholz C. Perforation repair with mineral trioxide aggregate: A modified matrix concept. Int Endod J. 2005;38:59–69. doi: 10.1111/j.1365-2591.2004.00901.x. [DOI] [PubMed] [Google Scholar]
- 7.Yadav P, Pruthi PJ, Naval RR, Talwar S, Verma M. Novel use of platelet-rich fibrin matrix and MTA as an apical barrier in the management of a failed revascularization case. Dent Traumatol. 2015;31:328–31. doi: 10.1111/edt.12168. [DOI] [PubMed] [Google Scholar]
- 8.Chosack A, Sela J, Cleaton-Jones P. A histological and quantitative histomorphometric study of apexification of nonvital permanent incisors of vervet monkeys after repeated root filling with a calcium hydroxide paste. Endod Dent Traumatol. 1997;13:211–7. doi: 10.1111/j.1600-9657.1997.tb00042.x. [DOI] [PubMed] [Google Scholar]
- 9.Dominguez Reyes A, Muñoz Muñoz L, Aznar Martín T. Study of calcium hydroxide apexification in 26 young permanent incisors. Dent Traumatol. 2005;21:141–5. doi: 10.1111/j.1600-9657.2005.00289.x. [DOI] [PubMed] [Google Scholar]
- 10.Witherspoon DE, Ham K. One-visit apexification: Technique for inducing root-end barrier formation in apical closures. Pract Proced Aesthet Dent. 2001;13:455–60. [PubMed] [Google Scholar]
- 11.Simon S, Rilliard F, Berdal A, Machtou P. The use of mineral trioxide aggregate in one-visit apexification treatment: A prospective study. Int Endod J. 2007;40:186–97. doi: 10.1111/j.1365-2591.2007.01214.x. [DOI] [PubMed] [Google Scholar]
- 12.Rafter M, Baker M, Alves M, Daniel J, Remeikis N. Evaluation of healing with use of an internal matrix to repair furcation perforations. Int Endod J. 2002;35:775–83. doi: 10.1046/j.1365-2591.2002.00566.x. [DOI] [PubMed] [Google Scholar]
- 13.Khatavkar RA, Hegde VS. Use of a matrix for apexification procedure with mineral trioxide aggregate. J Conserv Dent. 2010;13:54–7. doi: 10.4103/0972-0707.62629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aston SJ, Rees TD. Vicryl sutures. Aesthetic Plast Surg. 1976;1:289–93. doi: 10.1007/BF01570263. [DOI] [PubMed] [Google Scholar]
- 15.Conn J, Jr, Oyasu R, Welsh M, Beal JM. Vicryl (polyglactin 910) synthetic absorbable sutures. Am J Surg. 1974;128:19–23. doi: 10.1016/0002-9610(74)90228-1. [DOI] [PubMed] [Google Scholar]