Abstract
Background:
Development of health professionals with ability to integrate, synthesize, and apply knowledge gained through medical college is greatly hampered by the system of delivery that is compartmentalized and piecemeal. There is a need to integrate basic sciences with clinical teaching to enable application in clinical care.
Aim:
To study the benefit and acceptance of vertical integration of basic science in final year MBBS undergraduate curriculum.
Materials and Methods:
After Institutional Ethics Clearance, neuroanatomy refresher classes with clinical application to neurological diseases were held as part of the final year posting in two medical units. Feedback was collected. Pre- and post-tests which tested application and synthesis were conducted. Summative assessment was compared with the control group of students who had standard teaching in other two medical units. In-depth interview was conducted on 2 willing participants and 2 teachers who did neurology bedside teaching.
Results:
Majority (>80%) found the classes useful and interesting. There was statistically significant improvement in the post-test scores. There was a statistically significant difference between the intervention and control groups' scores during summative assessment (76.2 vs. 61.8 P < 0.01). Students felt that it reinforced, motivated self-directed learning, enabled correlations, improved understanding, put things in perspective, gave confidence, aided application, and enabled them to follow discussions during clinical teaching.
Conclusion:
Vertical integration of basic science in final year was beneficial and resulted in knowledge gain and improved summative scores. The classes were found to be useful, interesting and thought to help in clinical care and application by majority of students.
Keywords: Clinical teaching, undergraduate medical curriculum, vertical integration
INTRODUCTION
It is more than a century since Flexner published his report “Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching”[1] that reformed medical education in the United States, which Committed Medical Education to the German Tradition of Strong Biomedical Sciences followed by hands-on clinical training. Medical education has since evolved with many innovations introduced since then, which prompted the Carnegie Foundation for the Advancement of Teaching to Commission another report that was published in 2010. Two key recommendations from the report were “to integrate formal knowledge with clinical experience” and “to imbue habits of inquiry and improvement to achieve lifelong learning and excellence.”[2] Vertical integration as defined so clearly by Bradley and Mattick as a “…combination of basic and clinical sciences in such a way that the traditional divide between preclinical and clinical studies is broken down.”[3] Integration of basic sciences with clinical medicine during the initial years of medical undergraduate education is being done in many institutions with the advent of medical education reforms.[4] Clinicians often allude to basic sciences to improve student’s understanding of a patient’s clinical presentation and correlate it to the pathophysiology and anatomical localization of disease; however, the benefit of detailed basic science learning of the preclinical years of a medical student is not optimally utilized to better understanding, synthesis, and analysis of a patient’s problem. A refresher class of basic sciences which is completely contextual would benefit and achieve this purpose. Formal vertical integration during the final year is not currently practiced routinely probably due to the pressure of time which clinicians constantly face.[5] Vertical integration during the final year of an undergraduate curriculum can enable a deep understanding of the biological mechanisms and result in better synthesis and application of knowledge gained through the years in medical school. This study was planned to evaluate the benefit and acceptance of vertical integration in the final year of medical training from the students and the teachers' perspective.
MATERIALS AND METHODS
After Institutional Review Board approval, the students were informed about the study; the final year MBBS students were divided by convenience sampling as intervention and control arm based on the units they were posted in. The methodology is summarized in Figure 1.
Figure 1.

Methodology of study
Neuroanatomy refresher classes with clinical application to neurological diseases with case discussions were held as part of the final year posting in two medical units. Feedback on the classes was collected on 4 fields, grading the quality on a 0–10 scale along with an open column for comments and suggestions on improvement. Pre- and post-tests were conducted on the intervention group, before the classes and at the end of the 1-month posting. These questionnaires were clinical vignettes with questions that tested application and synthesis of knowledge in neurology.
Summative assessment marks in neurology clinical long case discussions were compared with the same of the control group who had standard teaching in other two medical units.
In-depth interview was conducted on 2 willing participants and 2 teachers.
Methods used to minimize bias
Triangulation of data from pre- and post-test scores to see if learning has happened, the comparison of summative assessment scores with the control group and the qualitative data collection by in-depth interviews and feedback forms were done to improve data standard and to prevent bias.
Data analysis
The quantitative data were entered onto Excel Microsoft software and qualitative data were transcribed from the recorder. Mean with standard deviations was calculated for feedback scores, pre- and post-test scores, and summative assessment. Student’s t-test was used to compare means between the intervention and control groups for the summative assessment, and pre- and post-test scores of the intervention group. A content analysis of qualitative data was performed for emerging themes.
RESULTS
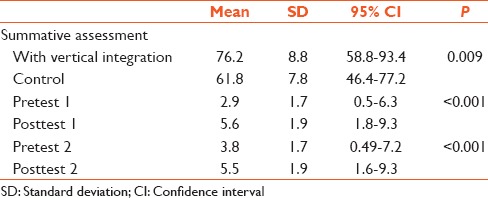
Thirty-one students of the final year MBBS batch of 60 students formed the intervention group. The feedback is summarized in Figure 2. The mean posttest scores which were done 1 month after the teaching, were significantly better than the pretest scores. The mean summative assessment score of the intervention group was significantly better than the control group [Table 1].
Figure 2.

Feedback scores
Table 1.
Scores in summative assessments and pre- and post-tests
The qualitative data analysis revealed four themes.
On the classes itself, the students felt that they were relevant, essential, short, simple, made more sense and were good revision.
On the theme of usefulness, the students felt that the class put things in perspective, helped them to localize, to synthesize, integrate and put together the clinical signs with anatomy, improved their understanding and helped make correlation with questions asked in history, and clinical presentation. They felt that they could exercise what they had learnt. They were motivated to go back and read neuroanatomy.
The second theme that emerged was the attitude of the students before and after the classes on approaching a patient with a neurological problem. Before the vertical integration, they felt that it was very confusing, were scared, to even ask doubts, were trying to recall what they had memorized, and were desperate to understand. Their attitude changed after the classes as they felt that they were more confident and sure of their answers and were not scared. More students worked up patients with neurological problems, and they could follow clinical discussions till the end, and the discussion progressed further than they did before. In their words,
“…Stroke was a monster that got easier to deal with…”
“…Could follow the discussion till the end otherwise few would be answering and others switched off.”
The fourth theme were suggestions for improvement where the students wanted more such classes with case discussions, for more subjects, more frequently. There were suggestions to use three dimensional images and video clips to improve content delivery. The student did feel that the importance of these classes might be lost on students if it were to be part of regular curriculum.
Teacher perceptions were along the same lines as the students with regard to the usefulness of the sessions. Additional benefits were interaction between different department teachers and identification of key areas for collaboration on other educational forums.
They expect the sessions to impact “future practice to avoids unnecessary investigations, deliver cost-effective care.” Teachers found that students were attentive and initiated discussions and asked valid doubts during the sessions and subsequent neurological bedside teaching sessions as basic concepts were clear. Feasibility and sustainability of the vertical integration were considered possible with cooperation between the departments. Training and commitment of faculty, coordination between different units and departments, and time were perceived as the major challenges in sustaining and extending vertical integration into other areas given the current milieu of the Medical Council of India curriculum and assessments. Suggestions for improvement included the use of descriptive media (radiological reconstruction images) during the class to improve visualization.
DISCUSSION
Vertical integration combines basic sciences knowledge and clinical bedside teaching in a synergy that deepens understanding of the basic science in the context of the clinical problem and stimulates intellectual curiosity. It makes learning holistic and more meaningful. It is essential to ease the transition from medical students to internship and residencies where application of knowledge is necessary. This study showed that vertical integration resulted in improvement in student’s synthesis and application of knowledge and retention that lasted at least 1 month. The students performed better in the bedside clinical assessment. The perceptions of the students were overwhelmingly positive. The students and the teachers perceived the sessions as useful and that it deepened understanding of the students and boosted their confidence. There were concerns raised about the sessions becoming “routine” and the resources required to maintain this teaching in terms of time, faculty training, cooperation, and coordination between departments.
Other studies where vertical integration has been done in a clinical setting have also revealed similar positive responses from the students; the students had preferred vertically integrated classes to basic science or bedside teaching alone.[6,7] The benefit extended to the teachers as well as they found the classes gratifying with discussions and doubts being raised by the students. The classes helped collaboration on other educational programs. Brynhildsen et al. have looked at student and teacher attitudes on an integrated curriculum after 10 years of practical experience with vertical integration.[8] The students scored horizontal integration as more important than vertical integration and the teachers especially the basic science teachers scored vertical integration higher.
The strength of this study is that both quantitative and qualitative methods have been used to triangulate data on benefit of vertical integration. The limitation is that we have done the study in one area (neurology and anatomy) of teaching clinical medicine. Collaboration and cooperation with other departments is necessary to extend these results to other portions of the curriculum. Pre- and post-tests were not one in the control group as the students were not willing to take them.
Complete shift to an integrated curriculum is probably the direction Indian Medical Education would take in the future with the current emphasis on introducing competency-based medical education. However even within the current framework of curriculum and assessment, it is feasible and useful to do vertical integration for selected topics. Vertical integration of basic science in the final year was beneficial and resulted in knowledge gain and improved summative scores. The classes were found to be useful, interesting and thought to help in clinical care and application by majority of students and improved collaboration among teachers.
CONCLUSION
Vertical integration of basic science in final year was beneficial and resulted in knowledge gain and improved summative scores. The classes were found to be useful, interesting and thought to help in clinical care and application by majority of students.
Financial support and sponsorship
Institutional Fluid Research Grant.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Barzansky B. Abraham Flexner and the era of medical education reform. Acad Med. 2010;85(9 Suppl):S19–25. doi: 10.1097/ACM.0b013e3181f12bd1. [DOI] [PubMed] [Google Scholar]
- 2.Irby D. Educating physicians for the future: Carnegie’s calls for reform. Med Teach. 2011;33:547–50. doi: 10.3109/0142159X.2011.578173. [DOI] [PubMed] [Google Scholar]
- 3.Bradley P, Mattick K. Integration of Basic and Clinical Sciences AMEE. UK: Peninsula College of Medicine and Dentistry; 2008. [Last accessed on 2016 Apr 21]. Available from: https://www.amee.org/getattachment/Conferences/AMEEPast-Conferences/AMEE-Conference-2008/Introduction-to-Medical-Education-Bradley-Mattick.pdf . [Google Scholar]
- 4.Brooks WS, Woodley KT, Jackson JR, Hoesley CJ. Integration of gross anatomy in an organ system-based medical curriculum: Strategies and challenges. Anat Sci Educ. 2015;8:266–74. doi: 10.1002/ase.1483. [DOI] [PubMed] [Google Scholar]
- 5.Li AS, Berger KI, Schwartz DR, Slater WR, Goldfarb DS. Facilitating the transition from physiology to hospital wards through an interdisciplinary case study of septic shock. BMC Med Educ. 2014;14:78. doi: 10.1186/1472-6920-14-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farah Z, Parvizi N. A new spin on vertical integration. Med Teach. 2013;35:79. doi: 10.3109/0142159X.2012.716568. [DOI] [PubMed] [Google Scholar]
- 7.Abu-Hijleh MF, Chakravarty M, Al-Shboul Q, Kassab S, Hamdy H. Integrating applied anatomy in surgical clerkship in a problem-based learning curriculum. Surg Radiol Anat. 2005;27:152–7. doi: 10.1007/s00276-004-0293-4. [DOI] [PubMed] [Google Scholar]
- 8.Brynhildsen J, Dahle LO, Behrbohm Fallsberg M, Rundquist I, Hammar M. Attitudes among students and teachers on vertical integration between clinical medicine and basic science within a problem-based undergraduate medical curriculum. Med Teach. 2002;24:286–8. doi: 10.1080/01421590220134105. [DOI] [PubMed] [Google Scholar]


