Abstract
Background:
Our existing undergraduate curriculum lacks developing competency for endotracheal intubation. Even though it is a lifesaving procedure, interns are exposed only during their posting in anesthesia or emergency medicine and so, when need arises, they fail to perform endotracheal intubation and it leads to catastrophes.
Aims and Objectives:
The aim of this study was to develop competency in interns for endotracheal intubation.
Materials and Methods:
A study was conducted on fifty interns of medical college. Lecture and demonstration were used for cognitive domain and one-to-one training and practice on manikin for affective and psychomotor domains, respectively. Live demonstration on patients was done whenever possible. Gain in knowledge was evaluated by pre- and post-test using standardized validated questionnaire. Skills were assessed by direct observation of procedural skill on manikin, split in steps: Laryngoscopy, intubation, and ventilation. Session was evaluated using feedback questionnaire and Likert scale.
Results:
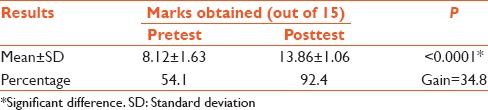
Interns showed mean marks of 8.12 ± 1.63 in pretest compared to 13.86 ± 1.06 of posttest with a gain of 34.8% (P = 0.0001), which is highly significant. Twenty-two percent interns completed all steps correctly in the first attempt, 62% in the second attempt, while 16% required third attempt to correctly complete all steps.
Conclusion:
This training developed competency for basic knowledge and practice of endotracheal intubation in interns adequately on manikin. Training for endotracheal intubation should be carried out at the beginning of internship before they go for clinical practice and repeated during their rotation of Anesthesia and Emergency Medicine Department, so they can retain their competency for it and can do later on whenever required.
Keywords: Competency, direct observation of procedural skills, endotracheal intubation, interns
INTRODUCTION
In our existing curriculum, medical graduates pass MBBS and do clinical work during internship, few of them select practice or job after that, but they are not competent for endotracheal intubation. Sometimes, they may know theory, but do not know how to apply when need arises and fail to do so.
Endotracheal intubation is a lifesaving procedure in emergency or critical situations. Even during residency, it is taught only in Anaesthesia and Emergency Medicine Department, so when any indication emerges, resident cannot perform intubation properly and may lose the patient. When resuscitation is done by nonanesthetic or nonemergency residents, for endotracheal intubation, they call or depend on anesthesia or emergency medicine residents and wait till they comes, but many a times, the patient’s condition cannot wait and leads to catastrophes.
Competency-based education is learner-centerd and helps interns for developing competency for endotracheal intubation. This will help them in future to do so whenever the need arises and a patient’s life can be saved. Accordingly, the present study was planned to develop competency in interns for endotracheal intubation and to assess that competency achieved.
MATERIALS AND METHODS
Approval from Institutional Review Board was taken. Interns of 2014–2015 batch of Smt. NHL Municipal Medical College formed the study group with a sample size of fifty interns. All interns were divided into three groups and each group was trained at different time with same faculty and resident. Before teaching, session was introduced and pretest taken by giving questionnaire set and answer sheet separately to all interns. Lecture was taken by powerpoint presentation. Any query related to knowledge of endotracheal intubation was solved at the end of the lecture. Procedure of endotracheal intubation was divided into three steps – laryngoscopy, intubation, and ventilation, and demonstrated to whole group. One-to-one demonstration and practice on manikin were carried out.
They were evaluated for affective and psychomotor skills by direct observation of procedural skills (DOPS). Postsession evaluation was done in the form of posttest questionnaire (same set of questions as pretest, 15 MCQs) for assessing cognitive domain. Training session was evaluated by using Likert scale questionnaire.
RESULTS
There was a definite gain in knowledge after the sessions, with highly significant statistical difference [Table 1].
Table 1.
Comparison of pre- and post-test results
For evaluation by DOPS, interns were given three attempts for all three steps. Attempt was considered as first if they done successfully, second if required assistance, and third if failed and done again successfully. Figure 1 shows the stepwise results of DOPS. It shows that 52% of interns were successful in laryngoscopy [Figure 2] at first attempt while 42% and 6% were successful at second and third attempts, respectively. Intubation was successful at first attempt in 54% of interns while 36% at second and 10% at third attempts. Ventilation with bag and mask was possible in all the interns (90% at first and 10% on second attempt) as no one required doing it again. In the procedure of endotracheal intubation, ventilation with bag and mask is more important to prevent hypoxia [Figure 3] and its consequences such as irreversible brain damage. As all interns had successfully done, it shows their immediate competency for that.
Figure 1.
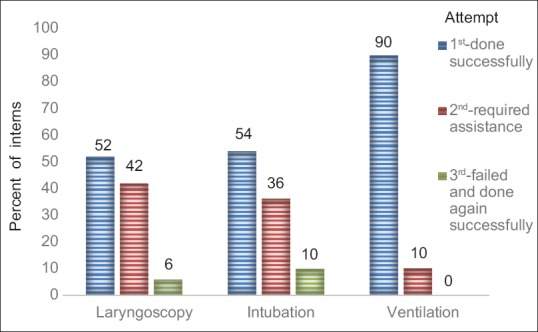
Direct observation of procedural skills result (stepwise)
Figure 2.

Interns performing laryngoscopy
Figure 3.

Interns performing bag and mask ventilation
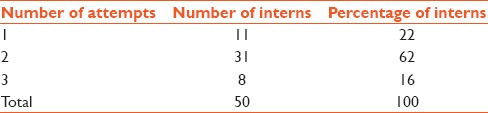
Of the 50 interns, 11 interns were able to perform all steps successfully in the first attempt, while 31 interns required help in any of the steps and 8 interns who failed it and done again successfully [Table 2]. Of all interns, 84% were able to perform intubation in the first or second attempt and 16% required third attempt and done it successfully again. Twenty-two percent interns were able to perform all steps in the first attempt and 62% required second attempt, means that it is a procedure that requires repeat training or exposure to that. However, all were able to do it in a single training that means that it is a procedure which can be done by them if they are adequately trained for that.
Table 2.
Results of directly observed procedural skills
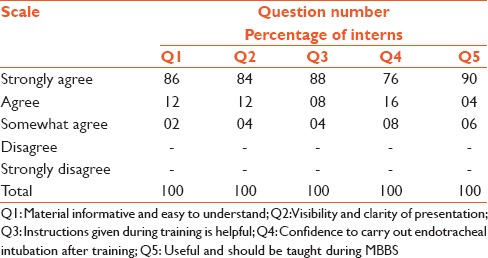
At the end of the session, evaluation was done using questionnaire with Likert scale from 1 to 5 where 1 denotes strongly agree and 5 denotes strongly disagree. The results show that all interns found the material informative and easy to understand. Eighty-four percent interns strongly agreed for visibility and clarity of presentation. All interns found that instructions given during training were helpful. Seventy-six percent interns strongly agreed for confident to carry out endotracheal intubation in future after hands-on training. All interns agreed that it is useful and should be taught before getting MBBS degree [Table 3].
Table 3.
Feedback questionnaire analysis
DISCUSSION
According to Vision 2015 by the Medical council of India,[1] all medical graduates should be able to manage the airway during emergency situations. Endotracheal intubation is the most effective method of securing the airway, but it is difficult to be competent without adequate training. Endotracheal intubation is taught in a series of steps to avoid cognitive overload.[2]
Owen and Plummer[3] trained 100 students and trainees for endotracheal intubation on models (mannequin) similar to us and found that they were more comfortable learning on models than patients. Salam et al.[4] done a cross-sectional study (2003–2005) and assessed competency in interns for endotracheal intubation. They found that even though its knowledge is compulsory during major clinical posting, out of 70% of interns, only 40% claimed about their competency of endotracheal intubation. They suggested the curriculum setter to think about core competency to be developed at house officer level. In our study, interns were previously not exposed to endotracheal intubation, but still shown better.
Bernhard et al.[5] (2007–2010) done a study on 21 residents for 1st year in anesthesia to perform 200 endotracheal intubation and assessed for associated success rate and number of attempts needed until successful in consecutive blocks of 25 procedures. They found a success rate of 67% in the first attempt compared to 83% after 200 number of intubation. Their overall success rate was 82% similar to 84% of our study. They also found that number of attempts for intubations were required less after the first 25 intubations (1.6 ± 0.8) compared to 1.3 ± 0.6 after 200 intubations (P = 0.0001). They have not mentioned about the technique and time period of training before evaluation, but our success rate is high compared to them in the first training, which shows efficacy of our training.
Kusel et al.[6] (2010–2012) studied the factors affecting the outcome of interns during anesthesia rotation for a period of 3 years. They observed that 80% were able to perform intubation and more than 80% were confident about intubation. Their result was similar to ours study. They also found that for more than 80% success rate, they required 29 procedures to be performed by interns indicating that repetition of practice or simulation should be done after some time for retention of skills. Dehmer et al.[7] did online survey in 156 4th year medical students for endotracheal intubation and found that out of 134 students, 83 never performed endotracheal intubation and more than 118 were not confident for it at all or without major assistance.
Mayo et al.[8] found poor performance for airway management in Advanced Cardiac Life Support (ACLS) certified interns at beginning of internship, which was found excellent after training as compared to beginning of internship. Katowa-Mukwato et al.[2] had conducted cross-sectional survey among 5th, 6th, and 7th year medical students, 2 months before the final examination and found that 19 students never performed endotracheal intubation and not confident for that. Eighteen students performed it only once and 12 students performed endotracheal intubation more than two times and they were confident for it. They found high correlation between experience and confidence. The student who had performed the procedure had improved rate of self-confidence. They were not allowed to perform endotracheal intubation frequently in emergency, so confidence level was low which would be required high for emergency management. They recommended simulation practice for lifesaving procedures such as endotracheal intubation to increase their confidence level, which we have done in our study.
Premadasa et al.[9] had done a study to determine the confidence for performing endotracheal intubation in new medical graduates who completed their internship. They found that out of 85 respondents, only 33% were confident to perform endotracheal intubation compared to 76% of our study. They concluded that interns should be trained adequately for it before completion of internship. Rothstein et al.[10] had done a study in interns of Emergency Medicine Department to assess for competency related to number of successful intubations and number of attempts. They have shown 86% success rate compared to 84% of ours, and a mean of 1.67 attempt compared to 22% in the first and 62% in the second attempt in our study.
Burch et al.[11] assessed 58 graduates of South African medical schools and found an average score of 67% for success compared to 84% of our study for endotracheal intubation. They concluded that most of the students were unable to perform it on entry to preregistration year and required further training.
CONCLUSION
This training developed competency for basic knowledge and practice of endotracheal intubation in interns adequately on manikin. Training for endotracheal intubation should be carried out at the beginning of internship when they go for clinical practice and repeated during their rotation of Anesthesia and Emergency Medicine Department. Hence, they retain competency for it and can do later on whenever required.
Recommendations
Training for endotracheal intubation should be carried out at the beginning of internship and can be repeated while their posting during Anaesthesia and Emergency Medicine Department, so they can retain their competency.
Limitations
There are some limitations in this study. Number of sample size is limited. As all interns were busy for preparing postgraduate entrance exams, they could not be followed up and trained again to retain their competency, otherwise repetition would have increased its effectiveness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are thankful to Dr. S. T. Malhan, The Medical Superintendent of our hospital and Dr. Pankaj R. Patel, The Dean of our medical college, for allowing and helping me in completing my project. I am also very thankful to Dr. Tiwari, Dr. D. V. Bala, and Dr. Alpesh, all from PSM Department, my residents, and group of faculties from Nodal Center for Faculty Development, Ahmedabad, for helping me in carrying out this study.
REFERENCES
- 1.Vision 2015. Medical Council of India; 2011. [Last accessed on 2016 Feb 28]. Available from: http://www.mciindia.org/tools/announcement/MCI_booklet.pdf .
- 2.Katowa-Mukwato P, Andrews B, Maimbolwa M, Lakhi S, Michelo C, Mulla Y, et al. Medical students' clerkship experiences and self-perceived competence in clinical skills. Afr J Health Prof Educ. 2015;6:155–60. doi: 10.7196/ajhpe.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owen H, Plummer JL. Improving learning of a clinical skill: The first year’s experience of teaching endotracheal intubation in a clinical simulation facility. Med Educ. 2002;36:635–42. doi: 10.1046/j.1365-2923.2002.01260.x. [DOI] [PubMed] [Google Scholar]
- 4.Salam A, Mohamad N, Moktar N. Assessment of medical graduates' competences. Malays J Med Sci. 2007;14:19. [Google Scholar]
- 5.Bernhard M, Mohr S, Weigand MA, Martin E, Walther A. Developing the skill of endotracheal intubation: Implication for emergency medicine. Acta Anaesthesiol Scand. 2012;56:164–71. doi: 10.1111/j.1399-6576.2011.02547.x. [DOI] [PubMed] [Google Scholar]
- 6.Kusel B, Farina Z, Aldous C. Anaesthesia training for interns at a metropolitan training complex: Does it make the grade? S Afr Fam Pract. 2014;56:201–5. [Google Scholar]
- 7.Dehmer JJ, Amos KD, Farrell TM, Meyer AA, Newton WP, Meyers MO. Competence and confidence with basic procedural skills: The experience and opinions of fourth-year medical students at a single institution. Acad Med. 2013;88:682–7. doi: 10.1097/ACM.0b013e31828b0007. [DOI] [PubMed] [Google Scholar]
- 8.Mayo PH, Hackney JE, Mueck JT, Ribaudo V, Schneider RF. Achieving house staff competence in emergency airway management: Results of a teaching program using a computerized patient simulator. Crit Care Med. 2004;32:2422–7. doi: 10.1097/01.ccm.0000147768.42813.a2. [DOI] [PubMed] [Google Scholar]
- 9.Premadasa I, Shehab D, Al-Jarallah KF, Thabib L. Confidence in performing core clinical skills: Preliminary results of a survey of trainees completing internship training in Kuwait. Bull Kuwait Inst Med Spec. 2007;6:48–50. [Google Scholar]
- 10.Rothstein J, Gullo J, Cuningham L, Murphy P, Sochor M. Training emergency medicine residents – The skill of endotracheal intubation: Comparison of human cadavers vs mannequins. Panamerican J Trauma Crit Care Emerg Surg. 2014;3:8. [Google Scholar]
- 11.Burch VC, Nash RC, Zabow T, Gibbs T, Aubin L, Jacobs B, et al. A structured assessment of newly qualified medical graduates. Med Educ. 2005;39:723–31. doi: 10.1111/j.1365-2929.2005.02192.x. [DOI] [PubMed] [Google Scholar]


