Abstract
Gorlin-Goltz syndrome due to its high variability in expression are often not diagnosed as the syndrome and often managed same as that of odontogenic keratocyst. But a more careful approach for the syndrome is needed as there is high chance of malignant changes owing to improper management of the syndrome. In this manuscript a case report of Gorlin-Goltz syndrome with the diagnostic features of the same in Indian population along with the difference in treatment protocol from treating an odontogenic keratocyst is described with review of literature
Keywords: Gorlin–Goltz syndrome, nevoid basal cell carcinoma syndrome, odontogenic keratocyst
INTRODUCTION
Gorlin–Goltz syndrome or nevoid basal cell carcinoma syndrome (NBCCS) is an autosomal dominant condition with high variability in expression. It is a highly penetrant genetic disorder. It is caused by mutations to patched PTCH1 which is a tumor suppressor gene located in 9q22, 3-q31. It has got an estimated prevalence of 1 in 57,000 to 1 in 256,000. Male to female ratio is 1:1. Gorlin and Goltz, in the year 1960, described the triad which includes multiple basal cell carcinoma, odontogenic keratocysts (OKC), and bifid ribs characteristic of the syndrome. In 1977, Rayner et al. added additional characteristics to the syndrome which include falx cerebri calcification or palmar/plantar pits. OKCs are the first ones likely to get diagnosed as they can be detected during the first decade of life. They occur almost in 80% NBCCSs. Early diagnosis of the syndrome is very important due to the susceptibility to neoplasm, and the syndrome can become very destructive as age progresses. Most often, the syndrome will go undiagnosed due to lack of proper investigations and problem targeted treatments. Here, we present a case report of a patient who has undergone previous surgical cyst removals but failed to get diagnosed with the syndrome.
CASE REPORT
A 28-year-old female patient was referred to our Department of Oral and Maxillofacial Surgery from a local dental clinic as her orthopantomogram (OPG) showed two radiolucencies in the mandible [Figure 1]. She had reported to the clinic with the complaint of pain in relation to the left lower back tooth region. She gave a history of the previous similar lesions in the maxilla, which were surgically removed along with impacted teeth in another hospital. Her previous medical records – X-ray computed tomography (CT) showed the previous lesions, which were associated with impacted teeth [Figure 2].
Figure 1.

Orthopantomogram
Figure 2.

Previous computed tomography
She gave no familial history of similar lesions. X-rays advised from our department revealed more findings. CT revealed persisting lesions in the previously operated sites [Figure 3] along with the lesions associated with the mandibular ramus region bilaterally. The mandibular lesions were also associated with impacted teeth.
Figure 3.

Current computed tomography
X-ray paranasal sinus (PNS) skull [Figure 4] revealed calcification of falx cerebri, and a miniplate fixation in relation to the maxillary region was seen in both OPG and PNS view.
Figure 4.

Paranasal sinus – skull
Chest X-ray revealed bifid ribs [Figure 5].
Figure 5.

Chest X-ray
On general examination, she exhibited mild macrocephaly, frontal bossing, hypertelorism with an intercanthal distance of about 43 mm, multiple nevi of size about 1 × 1 on the face [Figure 6].
Figure 6.

Extraoral examination
Clinical examination revealed the slight expansion of the lingual cortex of ramus in the left side. Maxillary regions revealed no clinical findings.
Cone beam computed tomography taken for the patient revealed the maxillary lesions extending almost half of the maxillary sinus with penetration of the posterior antral wall in the right side [Figures 7–9].
Figure 7.

Cone beam computed tomography
Figure 9.

Cone beam computed tomography-three-dimensional view
Figure 8.

Cone beam computed tomography-three-dimensional image
In the left maxillary region, the lesion was localized only in the posterior antral region.
Chest X-ray revealed spina bifida in relation to C-spine. She was clinically diagnosed as Gorlin–Goltz syndrome/NBCCS syndrome according to the clinical criteria of Kimonis et al. [Table 1].
Table 1.
Clinical characteristics of nevoid basal cell carcinoma syndrome found in this patient according to Kimonis et al. diagnostic criteria (Table 3)

It was decided to treat her by surgical enucleation of the lesions with the removal of impacted teeth along with chemical cauterization with Carnoy's solution under general anesthesia.
In the maxillary region, a crevicular incision was placed posterior to the premolar region extending posteriorly. Intraoperatively, buccal cortex was found intact on both sides. A bony window was created on the posterior antral wall, and the lesion was enucleated along with the entire lining enmass and chemical cauterization done with Carnoy's solution. A dense proteinaceous material such as keratin was found within the lesion [Figures 10 and 11].
Figure 10.
Bony window created on posterior antral wall
Figure 11.

Enucleation
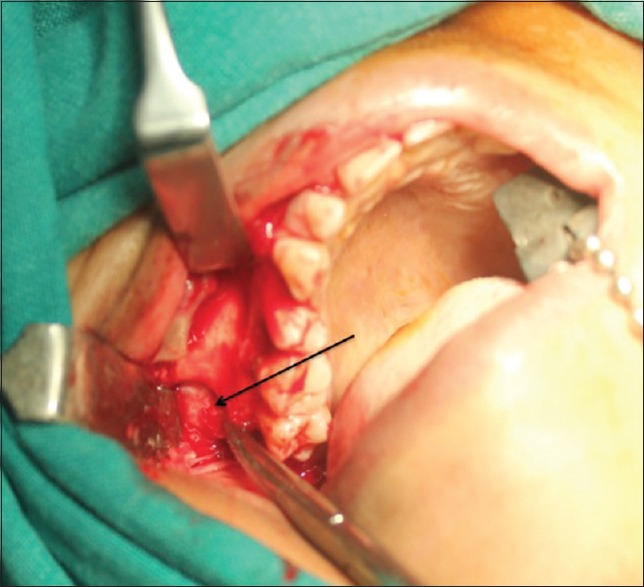
In the mandibular region, crevicular incision was placed posterior to the premolar region extending to the ramus region [Figure 12].
Figure 12.

Enucleation - mandibular lesion
The lesion was removed along with the impacted third molars, and chemical cauterization done with Carnoy's solution [Figure 13].
Figure 13.

Enucleated lesions from maxilla and mandible
The patient was put on a soft diet for 1 month owing to the extension of the lesion into the ramus and subsequent weakened bone. The patient was made aware of other systemic complications associated with the syndrome and advised to do necessary diagnostic tests.
All the specimens collected from the mandibular and maxillary regions were sent for histopathologic examination. All of them showed a corrugated parakeratinized cyst lining epithelium with a fibrovascular connective tissue capsule.
The connective tissue capsule showed the presence of satellite cysts, [Figure 14] and the cystic cavity showed flecks of keratin all of which confirmed the lesions as OKCs [Figure 15].
Figure 14.
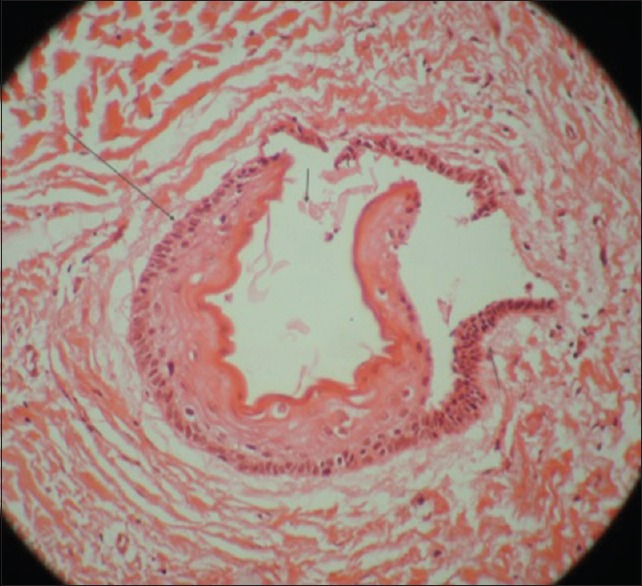
Satellite cyst
Figure 15.

Histopathologic slide view
DISCUSSION
NBCCS or Gorlin–Goltz syndrome is reported rarely in literature[1] and there has been a lack of awareness of the syndrome due to the rarity in Indian population. Syndrome associated keratocystic odontogenic tumors (KCOTs) are often treated in the same as treating nonsyndromic cases. Associated systemic signs can easily be missed due to the nonawareness of the syndrome. The features of the syndrome vary globally. The clinician should be aware of the features of the syndrome, which are more prevalent in his community as well as of different global population. Some of the major criteria of the syndrome are more aggressive when associated with the syndrome, for example – KCOTs, basal cell carcinoma syndrome, etc.
NBCCS usually represents its signs in the first and second decades of life, which mainly include multiple KCOTs. Although solitary keratocyst cases have also been reported17. The clinical features, which can be observed prenatally and/or neonatally, are cleft lips and palates and hypertelorism. Their number can vary from 1 to 30 with an average of 5 and has got a high rate of recurrence. KCOTs in NBCCS have a high rate of recurrence (60%) compared to nonsyndrome KCOTs (28%). The presence of daughter cyst, the friability of the lining, and the site of involvement contribute the high rate of recurrence. Surgical accessibility and surgeon's expertise minimize the rate of recurrence. Regular follow-up every year for 5 years and thereafter every 2 years has been recommended.
Basal cell carcinomas when associated with the syndrome are reported mostly in young patients and are found to involve even the nonexposed areas of the body.
Ovarian fibromas and cysts are seen in patients associated with the syndrome. They usually occur around 16–45 years of age. Medulloblastomas are seen in this syndromic patient within the first 2 years of life. Molecular genetic studies for PTCH1 gene mutations may be helpful in early diagnosis. PTCH1 is a tumor suppressor gene whose mutations can lead to increase in susceptibility to tumors.
Skeletal deformities can be bifid ribs or spina bifida. The frequency of bifid ribs was reported to be 30–60%. Calcification of falx cerebri is another most frequent feature with frequency 37–79% of NBCCS cases. The highest frequency is reported in the Australian population, which is about 92%. According to Kimonis et al.,[2] it is more in patients older than 20 years [Table 2].
Table 2.
Diagnostic criteria of nevoid basal cell carcinoma syndrome

According to the literature review[2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17] the features of the syndrome include craniofacial anomalies (frontal bossing, macrocephaly, bridging of sella turcica, hypertelorism, multiple OKC, High arched palate, impacted or ectopic teeth, bilateral coronoid hyperplasia and oligodontia), skeletal anomalies (rib anomalies, kyphosis/scoliosis, shortened fourth metacarpal, polydactyly/syndactyly, radiolucencies/pseudocysts in hand or feet, sloping shoulders, immobile thumbs), skin anomalies (basal cell carcinoma, palmar/plantar pitting), neurologic or central nervous system anomalies (medulloblastoma, meningioma, agenesis of corpus callosum, congenital hydrocephalus, intellectual disability) and other anomalies including genitourinary tract, cardiac and ophthalmologic anomalies. According to literature review we found that the features of the syndrome most commonly reported in indian literature in the descending order are impacted or ectopic tooth (100%), multiple odontogenic keratocysts (95.8%), rib anomalies (71%), hypertelorism (54%), frontal bossing (45.8%), basal cell carcinoma (41.6%), bridging of sella turcica (29%), macrocephaly (25%), polydactyly/syndactyly (21%).
CONCLUSION
NBCCS show variability in the expression. The patient we reported about presented with two major criteria (histologically proven OKC and bifid ribs) and three minor criteria (macrocephaly, frontal bossing, and falx cerebri calcification) which can be missed during routine dental examinations and investigations. Awareness about the syndrome plays a significant role in diagnosis. Clinical and radiographic features play a crucial role in diagnosis. Patients with the syndrome are susceptible for various complications such as malignancies if not dealt properly. As there is a defect in the tumor suppressor gene, they are more susceptible to malignancies if exposed to carcinogens. Proper counseling should be given to the patient regarding the expected complications of the syndrome. In the medical report, the details of the syndrome should be mentioned so that minimum diagnostic radiographs or those with lesser dose may be used in patient in future. The patient presented here is advised to regular follow-up with dermatologist, and with us.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gupta SR, Jaetli V, Mohanty S, Sharma R, Gupta A. Nevoid basal cell carcinoma syndrome in Indian patients: A clinical and radiological study of 6 cases and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:99–110. doi: 10.1016/j.tripleo.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 2.Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, et al. Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet. 1997;69:299–308. [PubMed] [Google Scholar]
- 3.Kamath A, Marquis L, Mehta TK. Basal cell nevus syndrome (Gorlin's syndrome) Indian J Dermatol Venereol Leprol. 1977;43:40–2. [PubMed] [Google Scholar]
- 4.Yesudian D, Krishnan SG, Jayaraman M, Janaki VR, Yesudian P. Atypical Gorlin's syndrome. Indian J Dermatol Venereol Leprol. 1995;61:314–6. [PubMed] [Google Scholar]
- 5.Chavan R, Phadke V, Joshi R, Khopkar U, Wadhwa S. Gorlin's syndrome. Indian J Dermatol. 1998;43:175–8. [Google Scholar]
- 6.Gupta A, Suri V, Gupta Y, Bhardwaj S. Gorlin's syndrome – A case report. JK Sci. 2000;2:55–7. [Google Scholar]
- 7.Gandage SG, Rahalkar M, Domkundwar S. Gorlin's syndrome – Radiographic and CT manifestations. Indian J Radiol Imaging. 2003;13:19–22. [Google Scholar]
- 8.Patil K, Mahima VG, Gupta B. Gorlin syndrome: A case report. J Indian Soc Pedod Prev Dent. 2005;23:198–203. doi: 10.4103/0970-4388.19010. [DOI] [PubMed] [Google Scholar]
- 9.Karthiga KS, Sivapatha Sundharam B, Manikandan R. Nevoid basal cell carcinoma syndrome. Indian J Dent Res. 2006;17:50–3. doi: 10.4103/0970-9290.29891. [DOI] [PubMed] [Google Scholar]
- 10.Rao S, Arulselvi S, Gupta K, Arora R, Shrivastava D. Nevoid basal cell carcinoma syndrome (Gorlin's syndrome): A case report. Indian J Pathol Microbiol. 2006;49:578–80. [PubMed] [Google Scholar]
- 11.Rai S, Gauba K. Jaw cyst-Basal cell nevus-Bifid rib syndrome: A case report. J Indian Soc Pedod Prev Dent. 2007;25:137–9. doi: 10.4103/0970-4388.36565. [DOI] [PubMed] [Google Scholar]
- 12.Kohli M, Kohli M, Sharma N, Siddiqui SR, Tulsi SP. Gorlin-Goltz syndrome. Natl J Maxillofac Surg. 2010;1:50–2. doi: 10.4103/0975-5950.69171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guruprasad Y, Prabhu PR. Gorlin-Goltz syndrome with situs oppositus. J Maxillofac Surg. 2010;1:58–62. doi: 10.4103/0975-5950.69167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rahman F, Tippu SR, Vatchala RM, Girish KL, Umesh K. Gorlin-Gotz syndrome (GGS) – Report of a rare case. Biomed Res. 2010;21:10–2. [Google Scholar]
- 15.Shivaswamy KN, Sumathy TK, Shyamprasad AL, Ranganathan C. Gorlin syndrome or basal cell nevus syndrome (BCNS): A case report. Dermatol Online J. 2010;16:6. [PubMed] [Google Scholar]
- 16.Baliga SD, Rao SS. Nevoid-basal cell carcinoma syndrome: A case report and overview on diagnosis and management. J Maxillofac Oral Surg. 2010;9:82–6. doi: 10.1007/s12663-010-0024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacDonald-Jankowski DS. Keratocystic odontogenic tumour: Systematic review. Dentomaxillofac Radiol. 2011;40:1–23. doi: 10.1259/dmfr/29949053. [DOI] [PMC free article] [PubMed] [Google Scholar]


