Abstract
The aim of this study is to review and compare survival/success rate of dental implants inserted in autogenous and allogenic bone blocks (ALBs). A PubMed search was performed from January 1990 to June 2014 limited to English language and human studies. Studies that reported treatment outcome of implants inserted in augmented alveolar ridges with autogenous or ALBs were included. Primary search identified 470 studies. For autogenous bone block (ABB) 36 articles and for ALB 23 articles met the inclusion criteria. Evidence on implant survival/success rate of both techniques was limited to observational studies with relatively small sample sizes. Study design, treatment methods, follow-ups, defect location, and morphology varied among studies. The range of implant survival and success rates in ABB was from 73.8% to 100% and 72.8% to 100%, respectively. The corresponding numbers for ALB were 95.3–100% and 93.7–100%, respectively. A definite conclusion could not be reached. Future studies with long-term follow-ups are required to further elucidate this issue.
Keywords: Allografts, alveolar bone grafting, alveolar bone loss, alveolar ridge augmentation, dental implantation
INTRODUCTION
Dental implants are an alternative treatment for replacement of missing teeth. To achieve optimum treatment outcome with dental implants, sufficient bone should be available to support and stabilize them.[1,2] Alveolar bone defects occur due to periodontitis, trauma, tumors, or resorption following tooth extraction and need augmentation before placement of dental implants.[3,4] Augmentation of atrophic jaws can be performed using autogenous[5] or tissue engineered bone grafts[6,7] or guided bone regeneration.[8] Autogenous block used as onlay bone graft is considered as the “gold standard” for reconstruction of atrophic ridges.[9,10] Autogenous grafts can be harvested from intraoral or extraoral donor sites. Intraoral donor sites such as symphysis, lateral ramus, and tuberosity are associated with less morbidity and resorption[11] when compared to extraoral donor sites.[12,13] However, the larger the defect of the jaw, the greater the need for an extraoral donor site such as the iliac crest, calvarium, and tibia. Autogenous donor site morbidities and limitations[14] such as transient paresthesia, costs, and hospitalization[15,16] prompted the need for allogenic human bone. Allogenic blocks are categorized based on their preparation process. The preparation process along with sterilization of allografts is performed to reduce immune response and inhibit disease transmission.[17] Fresh frozen bone allografts (FFBAs) induce a stronger immune response compared to freeze-dried bone allografts (FDBA).[18,19] However, freeze drying decreases the mechanical properties of the bone block.[17,20] Clinical application of these materials has been reported in some case series.[17,18] However, successful integration and remodeling of these bone substitutes have been an issue of debate.[21]
Although the use of allogenic bone block (ALB) is tempting, treatment outcome in comparison with autogenous bone block (ABB) has never been reviewed to provide scientific evidence for clinical application. Herein, we review survival and success rates of dental implants inserted in ALB and ABB.
MATERIALS AND METHODS
Study design
In the current review, studies that reported treatment outcome of implants (survival/success rates) inserted in augmented alveolar ridges with ABB or ALB in humans were included. Inlay bone grafting was excluded and only onlay use of bone blocks was evaluated. In addition, studies which used growth factors or stem cells in conjugation with bone grafts were excluded. Studies that used various augmentative techniques and did not report implant survival/success rates of onlay bone blocks separately were also excluded. The study design was not a criterion of inclusion for this attentive review and any clinical research was included. Studies on cases with the primary cause of alveolar defect being neoplasm, osteoradionecrosis, or congenital malformations were also excluded.
Search strategy
An electronic search of the literature in PubMed was carried out from January 1990 to June 2014 limited to English language and human studies. The following search terms were used based on PICO model:
Patient: Human.
Intervention: AND (“onlay graft*” OR “onlay bone graft*” OR “iliac crest” OR “ilium” OR “allograft bone*” OR “autograft bone*” OR “bone transplant*” OR “block graft*” OR “block bone*” OR “block autograft*” OR “block allograft*” OR “fresh frozen bone*” OR “freeze dried bone*” AND (implant OR implants).
Control: No term was used for the control group to include studies which reported only the results of on technique.
Outcome: AND (survival OR complication* OR failure* OR success*).
Primary selection including screening titles and abstracts was based on the inclusion criteria and full texts of all eligible studies were obtained. The authors reviewed full texts. Searching and screening process was performed by two reviewers independently and any disagreement was discussed by a third reviewer. Among different reports of one experiment, only the latest report, which revealed the most relevant information with respect to the measurements of this review, was included.
Data extraction included implant survival/success rate, treatment complications, and histological evaluations.
Quality assessment
During data extraction, the quality assessment of the included articles was undertaken by the authors according to the following parameters:[22] Proper randomization (yes/no); presence of both control and test groups (yes/no); surgeon blinded to treatment (yes/no/unclear); blindness to outcome (yes/no/unclear); follow-up completion (yes [withdrawal or dropout explanation]/no). Similar to the search process, quality assessment was also done by two reviewers independently and any disagreement was discussed by a third reviewer.
The experiments were then grouped as either low risk of bias (bias unlikely to influence the outcomes) if all criteria were met; medium risk of bias if three or four criteria were met; or high risk of bias (bias that might weakens confidence in results) if three or more criteria were not met.
RESULTS
Electronic search of the literature yielded a total of 635 articles, of which 57 were included [Figure 1]. Thirty-six out of 57 were related to ABB and 23 to ALB. Two studies compared both techniques.[23,24] Due to the lack of randomized clinical trials and a wide range of study designs, data reporting, recipient site and morphology, defect diameter, graft type, etc., a quantitative outcome measurement could not perform.
Figure 1.
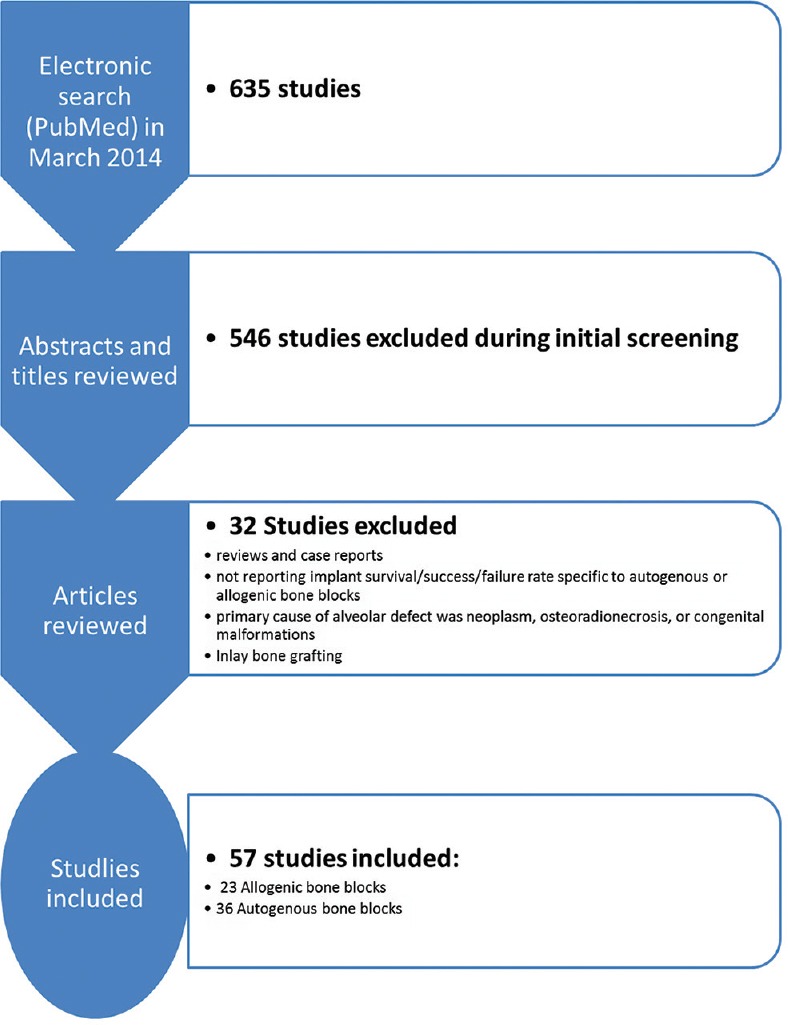
Literature search strategy
The results of the literature review (patients and methods, implant survival rate, complication, and histologic evaluation) are presented separately for each type of the bone block.
AUTOGENOUS BONE BLOCK
Patients and methods
Thirty-six studies that fit this category are displayed in Table 1. Assessing quality of the reviewed publications demonstrated that most of the articles were retrospective studies. Overall, 872 patients who needed alveolar ridge augmentation before implant placement were treated with ABB. Among the studies that reported the type of edentulism, 247 cases were partially edentulous and 205 patients were totally edentulous.
Table 1.
Summary of autogenous bone block studies
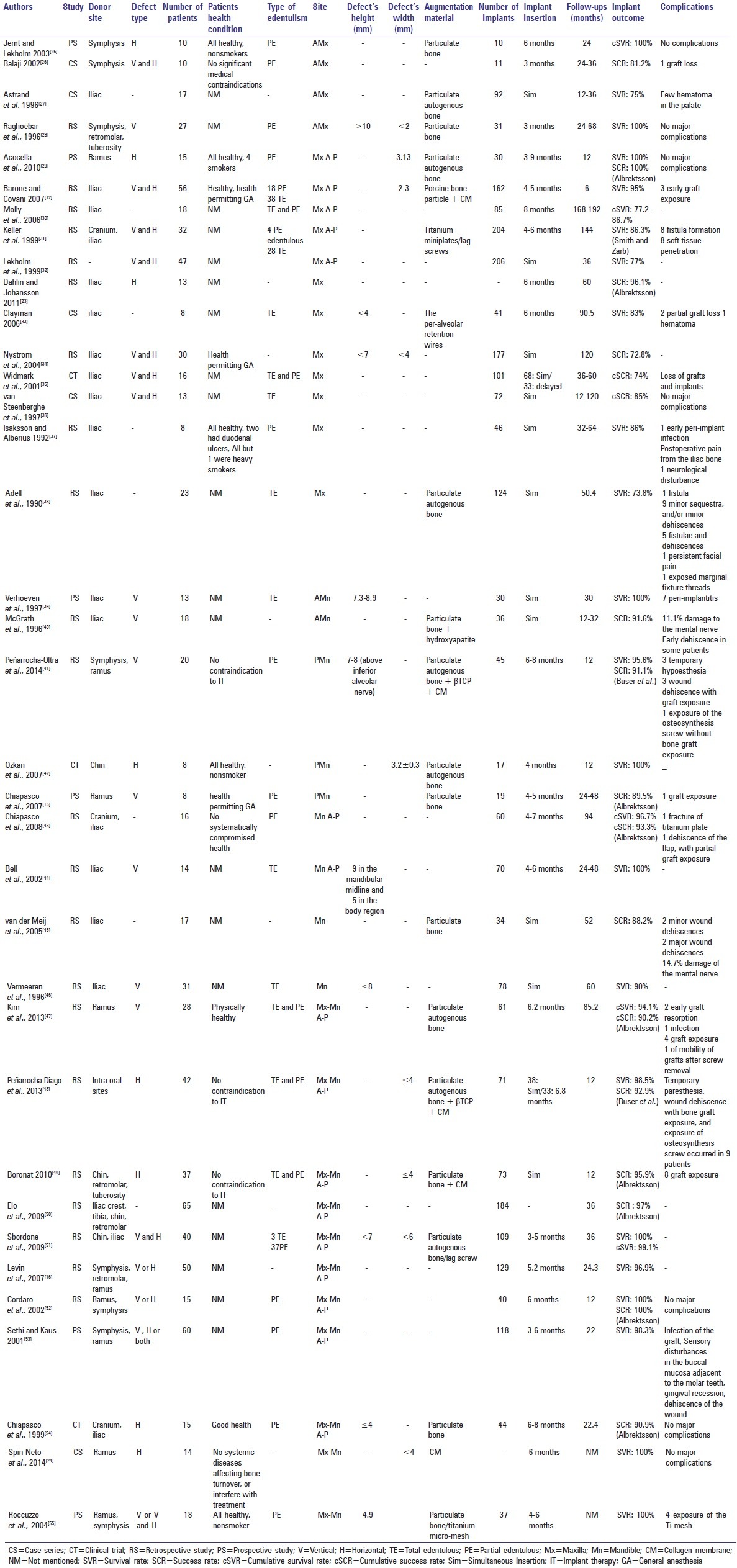
Graft-recipient site was exclusively in the maxilla in 16 studies including 343 patients[12,23,25,26,27,28,29,30,31,32,33,34,35,36,37,38] and exclusively in the mandible in nine studies including 145 patients.[15,39,40,41,42,43,44,45,46] In three studies (36 patients), only the posterior mandible was reconstructed[15,41,42] and in four studies (64 patients) the defects were located in anterior maxillary area.[25,26,27,28] Defects were augmented mostly vertically (height range: 3–10 cm)[28,39,40,41,15,44,46,47,55] and horizontal augmentation was performed in fewer patients (width range: 2–6).[23,25,29,42,48,49] In ten studies, both horizontal and vertical augmentation had been performed.[12,26,31,32,34,35,36,51,53,55]
Intraoral sites (mental symphysis, mandibular body/ramus, and maxillary tuberosity) were the primary source of autogenous bone (362 patients) followed by Iliac crest in 295 patients. The calvarium was the graft source in three studies;[31,43,54] however, the number of used calvarial grafts was not reported. The harvested bone was used alone as a block bone graft in 419 patients (48% of the cases). Particulate bone (autogenous, allogenic, or synthetic) was used in combination with block graft in 399 patients. Collagen membrane and titanium mesh were used in 169 and 50 patients, respectively.
Outcome
Implant success and survival rates
The included studies involved insertion of 2,647 implants; of which, 968 were inserted simultaneously with grafts. Survival rates ranging from 73.8% to 100% over 12–192 months were reported in 19 studies.[12,16,24,25,27,28,29,30,31,32,33,37,38,39,41,42,43,44,46,47,48,51,52,53,55] Success rates of 72.8–100% were reported in 12 studies.[23,26,29,34,35,36,40,41,15,43,45,47,48,49,50,52,54] Criteria for implant success rate were based on Albrektsson et al.'s criteria[56] in nine[29,15,43,47,49,50,52,54] and Buser et al.'s[57] criteria in two of them.[41,48] Among studies that only treated maxillary defects, survival and success rates of implants ranged from 73.8% to 100%[12,25,27,28,29,30,31,32,33,37,38] and 72.8% to 100%,[23,26,29,34,35,36] respectively. In studies on the mandible, the corresponding numbers ranged from 90% to 100%[39,41,42,43,44,46,47] and 88.2% to 93.3%,[40,41,15,43,45] respectively. Survival and success rates of implants inserted in the anterior zone of the maxilla were from 75% to 100%[25,27,28] and 81.2%,[26] respectively. In the posterior mandible, the corresponding numbers were 95.6–100%[41,42] and 89.5–91.1%,[15,41] respectively. Studies that harvested bone grafts from intraoral sites reported 94.1% to 100%[16,24,25,28,29,41,42,47,48,52,53,55] and 81.2% to 100%[26,29,41,15,47,48,49,52] implant survival and success rates, respectively. The corresponding ranges for extraoral donor sites were 73.8–100%[12,27,30,31,33,37,38,39,43,44,46] and 72.8–96.1%,[23,34,35,36,40,43,45,54] respectively.
Complications
Most of the studies did not report complications or stated no major complications. Other studies reported few occurrences of minor complications including peri-implantitis,[37,39] exposure of the membrane,[55] exposure of the graft,[12,15,41,43,47,48,49] infection,[31,38,47] soft tissue dehiscence,[31,38,40,41,43,45,48] hematoma,[27,33] discomfort,[37,38] and graft loss.[26,33,35]
Neurosensory disturbance as a major complication was mostly associated with intraoral donor sites.[40,41,45,48] McGrath et al.[40] and van der Meij et al.[45] reported mental nerve damage in 11.1% and 14.7% of patients, respectively. In a study by Isaksson et al.,[37] one patient had neurological disturbances following bone harvesting from the iliac crest.
Histological evaluation
Bone graft integration was histologically evaluated in two studies both using mandibular lateral ramus bone blocks.[24,29] The nonvital bone was 57.75%[29] and 55.9%[24] of total tissue volume; 27.6% vital bone and 16.4% connective tissue formation were reported by Spin-Neto et al.[24]
ALLOGENIC BONE BLOCK
Patients and methods
Twenty-three studies that fit this category are displayed in Table 2. Assessment of the quality of the reviewed publications demonstrated that most of the articles were case series. Overall, 532 patients who needed alveolar ridge augmentation prior to implant placement were treated by means of ALB. Among the studies reported, the type of edentulism in 209 cases was partially edentulous and only 15 patients were totally edentulous.
Table 2.
Summary of allogenic bone block studies
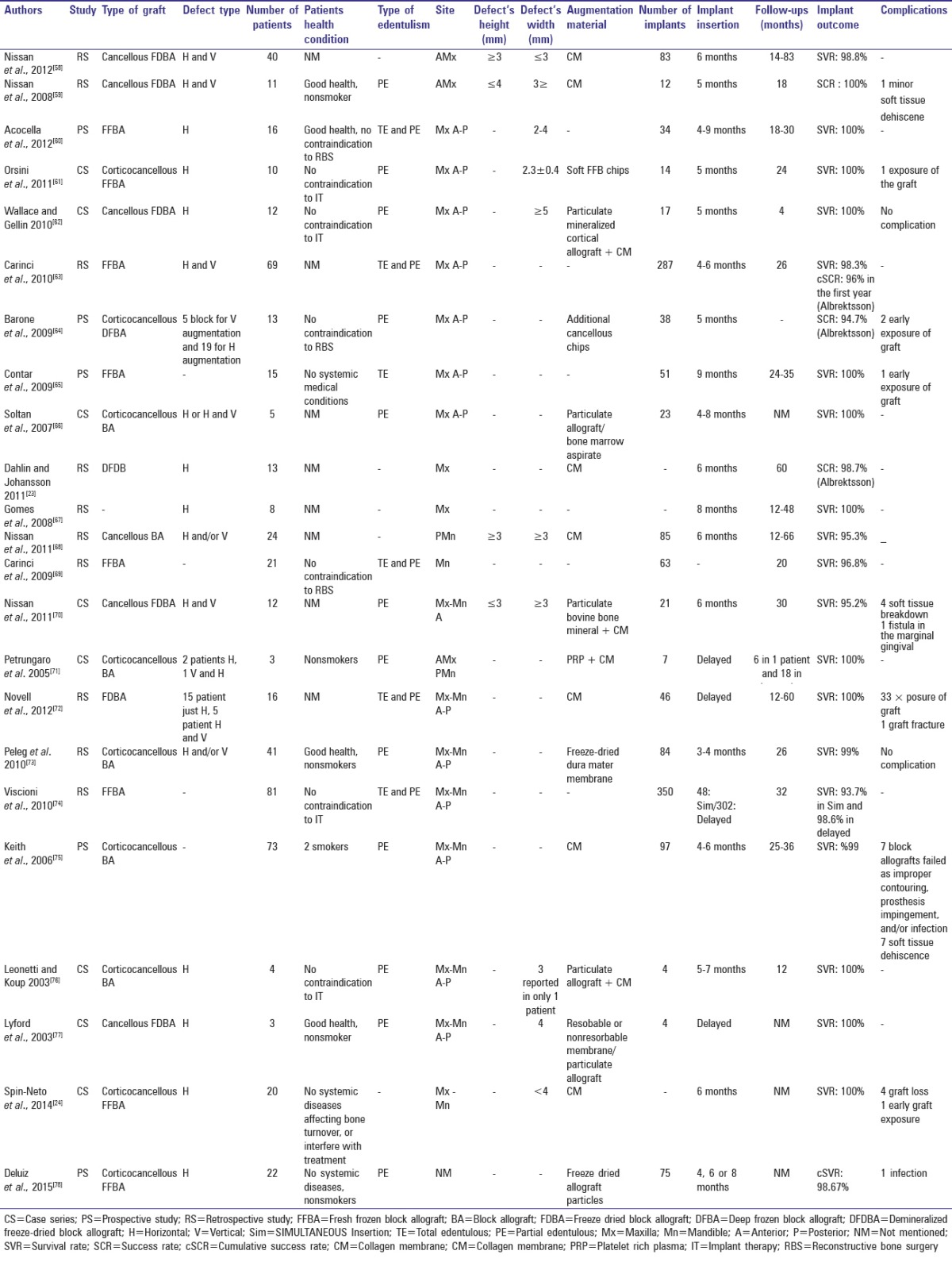
The recipient site was exclusively the maxilla in 11 studies (212 patients)[23,58,59,60,61,62,63,64,65,66,67] and exclusively the mandible in two studies (45 patients).[68,69] In one study (24 patients), only the posterior mandible[68] was reconstructed and in two studies (51 patients) the defects were located only in the anterior maxilla.[58,59] Most defects underwent horizontal augmentation (width range: 2–5 cm)[23,24,60,61,62,64,66,67,72,73,76,77,78] and vertical augmentation was performed in fewer patients (height range: 3–4 cm).[64,68,73] In nine studies, both horizontal and vertical augmentations were performed.[58,59,63,66,68,72,73]
Different kinds of allograft bone blocks were used. FFBA was the most common type (254 patients) followed by FDBA (94 patients). The block bone was used alone in 210 patients (39.5% of the cases). Particulate bone (allogenic and xenogenic) was applied in combination with block graft in 81 patients. Resorbable/nonresorbable membranes (272 patients), platelet-rich plasma (three patients),[71] or bone marrow aspirate (five patients)[66] was also used.
Outcome
Implant success and survival rates
The included studies involved insertion of 1395 implants; of which, 48 were inserted simultaneously with the graft. Survival rates ranging from 95.3% to 100% over 12–60 months were reported in 19 studies.[24,58,60,61,62,63,65,66,67,68,69,70,71,72,73,74,75,76,77,78] Success rates of 94.7–100% were reported in four of the studies.[23,59,63,64] Criteria for implant success rate were based on Albrektsson et al.'s criteria[56] in three of them[23,63,64] while other studies did not mention the success criteria. Among studies that only treated maxillary defects, survival and success rates of implants ranged from 98.3% to 100%[58,60,61,62,63,65,66,67] and 94.7% to 100%,[23,59,63,64] respectively. In studies on the mandible, the implant survival rate ranged from 95.3% to 100%.[24,68,69,70,71,72,73,74,75,76,77,78] No study reported implant success rate in the mandible. Survival of implants inserted in the anterior zone of the maxilla was between 98.8%[58] and 100%.[60] In the posterior mandible, implant survival rate was 95.3%.[68]
Complications
Most of the studies did not report complications and no major complications were recorded. Other studies reported few occurrences of minor complications including graft exposure,[24,61,64,65,72] graft loss,[24,72,75] soft tissue dehiscence,[59,70,75] and infection.[70,75,78]
Histological evaluation
Bone graft integration was histologically evaluated in 11 studies,[24,58,60,61,65,66,68,71,75,76,78] mostly revealing incorporation and remodeling of block allograft with no inflammatory response. However, Acocella et al.[60] reported poor cellular activity and poor amounts of newly formed bone with no signs of rapid revascularization of the recipient site. In the cited article, osteoclasts were rarely detected and a mixture of fibrous and new bone formation was observed at the graft recipient site interface in some cases. The presence of a large number of osteocytes trapped within the mineralized matrix, angiogenesis, and few osteonic structures was reported by Orsini et al.[61]
The amount of nonvital bone, vital bone, and soft tissue ranged from 26% to 61.96%, 8.4% to 44%, and 27% to 48.4%, respectively.[24,58,60,61,66,68] The new bone presented features of mainly woven and lamellar bone with large marrow spaces.[60,75]
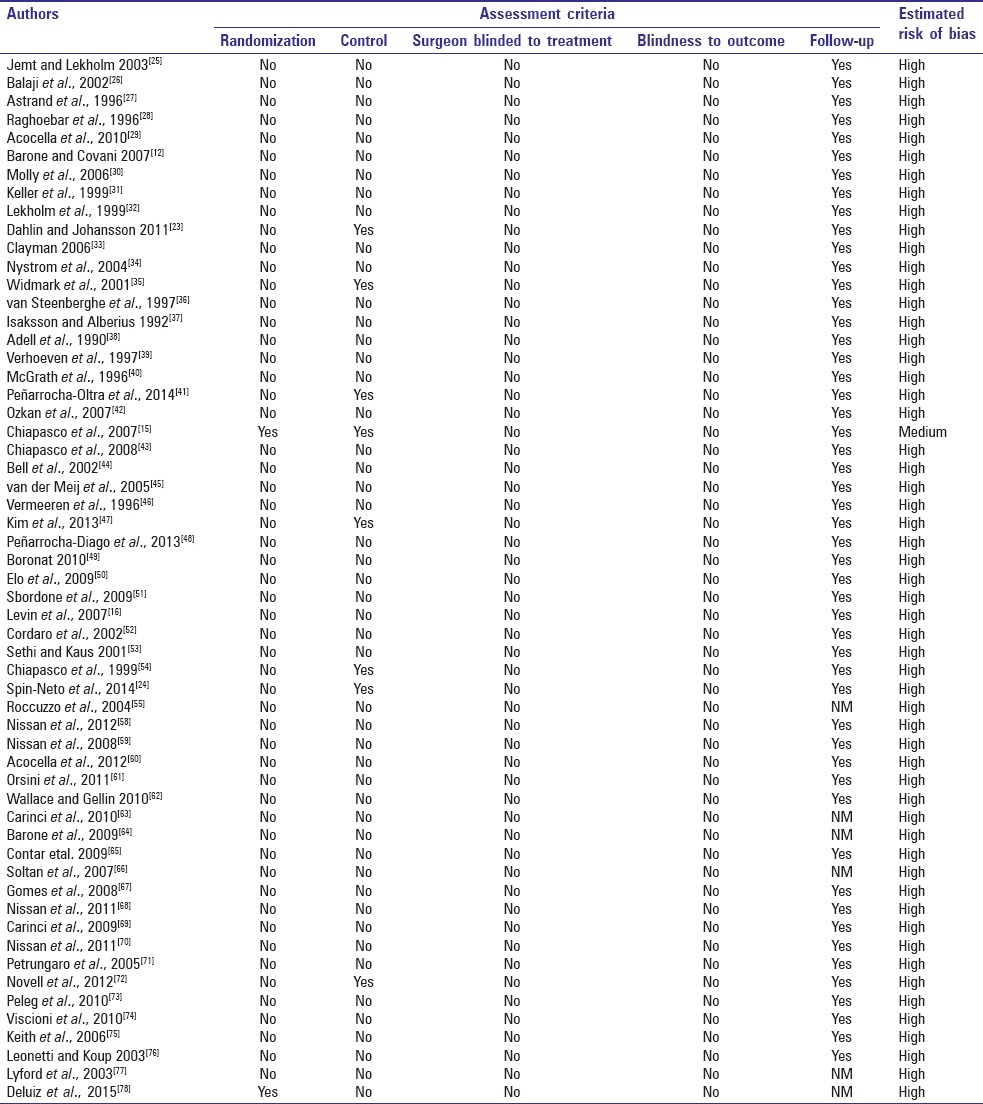
QUALITY ASSESSMENT
Estimated risk of bias for each study is reported in Table 3 that shows that almost all included studies had a high risk of bias.
Table 3.
Quality assessment
DISCUSSION
Autogenous onlay grafts are considered the gold standard treatment for alveolar defects. Systematic reviews on survival rates for dental implants in ABB augmented alveolar ridges showed various study designs.[79,80] Due to limitations of ABB, onlay grafting with allogenic blocks has been recently evaluated. However, reviews on ALB reported a lack of evidence for the establishment of its treatment efficacy.[81,82] The current review compared implant treatment outcomes between ABB and ALB. Most biocompatible substitutes can be integrated into the host bone due to minimal inflammatory response, but only the remodeled tissue can be named a successful bone graft. The normal remodeling process of the jaw usually takes more than 12 months.[4]
Keith et al.[75] reported implant survival rate of 99% when only seven out of 82 ALBs failed. Duration of follow-up was not mentioned for three ABB[24,50,55] and five ALB groups.[24,64,66,77,78] Wallace and Gellin[62] had reported 4 months follow-up. Carinci et al.[63] showed that cumulative implant success rate decreased from 96% in the 1st year to 40% in 4 years due to crestal bone loss. Follow-ups for ALB were relatively shorter than ABB (12–192 months vs. 12–60 months).
The resorption rate of ALB was three times more than that of ABB at 6 months.[83] Occlusal force or accumulation of microbial plaque may cause micro-fractures in a nonremodelable bone block and cause weakness in maintaining crestal bone around dental implants.[84] Deluiz et al.[78] demonstrated that significantly different resorption rates of allografts occur during 4–8 months of healing.
ABB harvested from intraoral donor sites showed higher implant survival than extraoral donor sites (94.1–100%[16,24,25,28,29,41,42,47,48,52,53,55] vs. 73.8–100%).[12,27,30,31,33,37,38,39,44,45,47] In this group, implants placed in reconstructed mandibles survived longer than implants in reconstructed maxillae (90–100%[39,41,42,43,44,46,47] vs. 73.8–100%).[12,25,27,28,29,30,31,32,33,37,38]
Simultaneous implant placement had a frequency higher than 36% in ABB groups. Survival of simultaneously placed dental implants was higher than those placed in ALB after a healing period (93.7% vs. 98.6%).[74] Peñarrocha-Diago et al.[48] reported 98.5% survival rate for both delayed and simultaneously inserted implants in autografts harvested from intraoral sites.
Recipient site analysis and matching is an important variable in the interpretation of results of augmentative techniques. ALB was mostly used for horizontal bone augmentation or defects limited to one or two teeth. No report of ALB could be found in the treatment of posterior mandible in our review; most were found in the anterior maxilla. Graft resorption occurred more in the mandible than in the maxilla.[52] Dimension and location of the recipient site influence treatment outcomes.[85]
Particulate bone with collagen membrane has been used with ALB in comparison to ABB (48% vs. 39.5%). The addition of PRP to ALB resulted in 100% survival of implants.[71]
Two trials compared implant treatment outcomes between ALB and ABB.[23,24] Horizontal augmentation of defects <4 mm width resulted in 100% implant survival rate for both techniques.[24] Five-year follow-up of the horizontal augmentation of the maxilla revealed 96.1% and 98.7% success rates for implants inserted in ABB and ALB, respectively.[23]
Low incidence of complications related to onlay bone grafting was observed in both techniques. Paresthesia was mostly transient and related to intraoral donor sites.[40,41,45,48] In addition, pain and discomfort were reported in few studies following block harvesting from the iliac crest.[37,38]
Histological evaluation in two articles revealed that more than half of the tissue volume was nonvital graft remnants.[24,29] Acocella et al.[29] demonstrated reduction of nonvital bone and final remodeling with time. A wide range of remodeling has been reported (8.4%[24] to 44%[68]). While most studies revealed proper integration of ALB, some studies reported no regenerative and remodeling activity with a high percentage of nonvital bone.[24,60] Formation of fibrous tissue, which was reported in some cases at the graft recipient site interface, could reduce graft survival.[60] Goldberg and Stevenson[86] mentioned delayed vascularization of ALB and longer implant healing periods.
Comparing histological integration of ABB and ALB, Spin-Neto et al.[24] reported that larger amounts of both nonvital and vital bone and lesser amounts of soft connective tissue were observed in the ABB group. No difference was observed between the groups in either bone-to-implant contact or the bone area between implant threads.[24]
CONCLUSION
Due to the lack of controlled clinical trials, a definite consensus cannot be reached regarding the success and survival of implants placed in defects reconstructed with autogenic versus ALB. Wide ranges of implant success and survival have been reported for both techniques. The main concern regarding ABB is donor site complications and for ALB is the integration of the graft. Future studies with longer follow-ups are required to further elucidate these issues.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hirsch JM, Brånemark PI. Fixture stability and nerve function after transposition and lateralization of the inferior alveolar nerve and fixture installation. Br J Oral Maxillofac Surg. 1995;33:276–81. doi: 10.1016/0266-4356(95)90037-3. [DOI] [PubMed] [Google Scholar]
- 2.Khojasteh A, Eslaminejad MB, Nazarian H, Morad G, Dashti SG, Behnia H, et al. Vertical bone augmentation with simultaneous implant placement using particulate mineralized bone and mesenchymal stem cells: A preliminary study in rabbit. J Oral Implantol. 2013;39:3–13. doi: 10.1563/AAID-JOI-D-10-00206. [DOI] [PubMed] [Google Scholar]
- 3.Shayesteh YS, Khojasteh A, Siadat H, Monzavi A, Bassir SH, Hossaini M, et al. A comparative study of crestal bone loss and implant stability between osteotome and conventional implant insertion techniques: A randomized controlled clinical trial study. Clin Implant Dent Relat Res. 2013;15:350–7. doi: 10.1111/j.1708-8208.2011.00376.x. [DOI] [PubMed] [Google Scholar]
- 4.Shabestari GO, Shayesteh YS, Khojasteh A, Alikhasi M, Moslemi N, Aminian A, et al. Implant placement in patients with oral bisphosphonate therapy: A case series. Clin Implant Dent Relat Res. 2010;12:175–80. doi: 10.1111/j.1708-8208.2009.00150.x. [DOI] [PubMed] [Google Scholar]
- 5.Khojasteh A, Mohajerani H, Momen-Heravi F, Kazemi M, Alikhasi M. Sandwich bone graft covered with buccal fat pad in severely atrophied edentulous maxilla: A clinical report. J Oral Implantol. 2011;37:361–6. doi: 10.1563/AAID-JOI-D-09-00141.1. [DOI] [PubMed] [Google Scholar]
- 6.Jafarian M, Eslaminejad MB, Khojasteh A, Mashhadi Abbas F, Dehghan MM, Hassanizadeh R, et al. Marrow-derived mesenchymal stem cells-directed bone regeneration in the dog mandible: A comparison between biphasic calcium phosphate and natural bone mineral. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e14–24. doi: 10.1016/j.tripleo.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Khojasteh A, Behnia H, Hosseini FS, Dehghan MM, Abbasnia P, Abbas FM. The effect of PCL-TCP scaffold loaded with mesenchymal stem cells on vertical bone augmentation in dog mandible: A preliminary report. J Biomed Mater Res B Appl Biomater. 2013;101:848–54. doi: 10.1002/jbm.b.32889. [DOI] [PubMed] [Google Scholar]
- 8.Khojasteh A, Soheilifar S, Mohajerani H, Nowzari H. The effectiveness of barrier membranes on bone regeneration in localized bony defects: A systematic review. Int J Oral Maxillofac Implants. 2013;28:1076–89. doi: 10.11607/jomi.2925. [DOI] [PubMed] [Google Scholar]
- 9.Morad G, Khojasteh A. Cortical tenting technique versus onlay layered technique for vertical augmentation of atrophic posterior mandibles: A split-mouth pilot study. Implant Dent. 2013;22:566–71. doi: 10.1097/01.id.0000433590.33926.af. [DOI] [PubMed] [Google Scholar]
- 10.Khojasteh A, Behnia H, Shayesteh YS, Morad G, Alikhasi M. Localized bone augmentation with cortical bone blocks tented over different particulate bone substitutes: A retrospective study. Int J Oral Maxillofac Implants. 2012;27:1481–93. [PubMed] [Google Scholar]
- 11.Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997;12:767–76. [PubMed] [Google Scholar]
- 12.Barone A, Covani U. Maxillary alveolar ridge reconstruction with nonvascularized autogenous block bone: Clinical results. J Oral Maxillofac Surg. 2007;65:2039–46. doi: 10.1016/j.joms.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 13.Le B, Burstein J, Sedghizadeh PP. Cortical tenting grafting technique in the severely atrophic alveolar ridge for implant site preparation. Implant Dent. 2008;17:40–50. doi: 10.1097/ID.0b013e318166d503. [DOI] [PubMed] [Google Scholar]
- 14.Scheerlinck LM, Muradin MS, van der Bilt A, Meijer GJ, Koole R, Van Cann EM. Donor site complications in bone grafting: Comparison of iliac crest, calvarial, and mandibular ramus bone. Int J Oral Maxillofac Implants. 2013;28:222–7. doi: 10.11607/jomi.2603. [DOI] [PubMed] [Google Scholar]
- 15.Chiapasco M, Zaniboni M, Rimondini L. Autogenous onlay bone grafts vs. alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: A 2-4-year prospective study on humans. Clin Oral Implants Res. 2007;18:432–40. doi: 10.1111/j.1600-0501.2007.01351.x. [DOI] [PubMed] [Google Scholar]
- 16.Cordaro L, Amadé DS, Cordaro M. Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clin Oral Implants Res. 2002;13:103–11. doi: 10.1034/j.1600-0501.2002.130113.x. [DOI] [PubMed] [Google Scholar]
- 17.Giannoudis PV, Dinopoulos H, Tsiridis E. Bone substitutes: An update. Injury. 2005;36(Suppl 3):S20–7. doi: 10.1016/j.injury.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 18.Strong DM, Friedlaender GE, Tomford WW, Springfield DS, Shives TC, Burchardt H, et al. Immunologic responses in human recipients of osseous and osteochondral allografts. Clin Orthop Relat Res. 1996;326:107–14. doi: 10.1097/00003086-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Ehrler DM, Vaccaro AR. The use of allograft bone in lumbar spine surgery. Clin Orthop Relat Res. 2000;371:38–45. doi: 10.1097/00003086-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Bhatt RA, Rozental TD. Bone graft substitutes. Hand Clin. 2012;28:457–68. doi: 10.1016/j.hcl.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 21.McAllister BS, Haghighat K. Bone augmentation techniques. J Periodontol. 2007;78:377–96. doi: 10.1902/jop.2007.060048. [DOI] [PubMed] [Google Scholar]
- 22.Khojasteh A, Kheiri L, Motamedian SR, Nadjmi N. Regenerative medicine in the treatment of alveolar cleft defect: A systematic review of the literature. J Craniomaxillofac Surg. 2015;43:1608–13. doi: 10.1016/j.jcms.2015.06.041. [DOI] [PubMed] [Google Scholar]
- 23.Dahlin C, Johansson A. Iliac crest autogenous bone graft versus alloplastic graft and guided bone regeneration in the reconstruction of atrophic maxillae: A 5-year retrospective study on cost-effectiveness and clinical outcome. Clin Implant Dent Relat Res. 2011;13:305–10. doi: 10.1111/j.1708-8208.2009.00221.x. [DOI] [PubMed] [Google Scholar]
- 24.Spin-Neto R, Stavropoulos A, Coletti FL, Faeda RS, Pereira LA, Marcantonio E., Jr Graft incorporation and implant osseointegration following the use of autologous and fresh-frozen allogeneic block bone grafts for lateral ridge augmentation. Clin Oral Implants Res. 2014;25:226–33. doi: 10.1111/clr.12107. [DOI] [PubMed] [Google Scholar]
- 25.Jemt T, Lekholm U. Measurements of buccal tissue volumes at single-implant restorations after local bone grafting in maxillas: A 3-year clinical prospective study case series. Clin Implant Dent Relat Res. 2003;5:63–70. doi: 10.1111/j.1708-8208.2003.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 26.Balaji SM. Management of deficient anterior maxillary alveolus with mandibular parasymphyseal bone graft for implants. Implant Dent. 2002;11:363–9. doi: 10.1097/00008505-200211040-00016. [DOI] [PubMed] [Google Scholar]
- 27.Astrand P, Nord PG, Branemark PI. Titanium implants and onlay bone graft to the atrophic edentulous maxilla: A 3-year longitudinal study. Int J Oral Maxillofac Surg. 1996;25:25–9. doi: 10.1016/s0901-5027(96)80007-5. [DOI] [PubMed] [Google Scholar]
- 28.Raghoebar GM, Batenburg RH, Vissink A, Reintsema H. Augmentation of localized defects of the anterior maxillary ridge with autogenous bone before insertion of implants. J Oral Maxillofac Surg. 1996;54:1180–5. doi: 10.1016/s0278-2391(96)90346-8. [DOI] [PubMed] [Google Scholar]
- 29.Acocella A, Bertolai R, Colafranceschi M, Sacco R. Clinical, histological and histomorphometric evaluation of the healing of mandibular ramus bone block grafts for alveolar ridge augmentation before implant placement. J Craniomaxillofac Surg. 2010;38:222–30. doi: 10.1016/j.jcms.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 30.Molly L, Quirynen M, Michiels K, van Steenberghe D. Comparison between jaw bone augmentation by means of a stiff occlusive titanium membrane or an autologous hip graft: A retrospective clinical assessment. Clin Oral Implants Res. 2006;17:481–7. doi: 10.1111/j.1600-0501.2006.01286.x. [DOI] [PubMed] [Google Scholar]
- 31.Keller EE, Tolman DE, Eckert S. Surgical-prosthodontic reconstruction of advanced maxillary bone compromise with autogenous onlay block bone grafts and osseointegrated endosseous implants: A 12-year study of 32 consecutive patients. Int J Oral Maxillofac Implants. 1999;14:197–209. [PubMed] [Google Scholar]
- 32.Lekholm U, Wannfors K, Isaksson S, Adielsson B. Oral implants in combination with bone grafts. A 3-year retrospective multicenter study using the Brånemark implant system. Int J Oral Maxillofac Surg. 1999;28:181–7. [PubMed] [Google Scholar]
- 33.Clayman L. Implant reconstruction of the bone-grafted maxilla: Review of the literature and presentation of 8 cases. J Oral Maxillofac Surg. 2006;64:674–82. doi: 10.1016/j.joms.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 34.Nyström E, Ahlqvist J, Gunne J, Kahnberg KE. 10-year follow-up of onlay bone grafts and implants in severely resorbed maxillae. Int J Oral Maxillofac Surg. 2004;33:258–62. doi: 10.1006/ijom.2003.0512. [DOI] [PubMed] [Google Scholar]
- 35.Widmark G, Andersson B, Carlsson GE, Lindvall AM, Ivanoff CJ. Rehabilitation of patients with severely resorbed maxillae by means of implants with or without bone grafts: A 3- to 5-year follow-up clinical report. Int J Oral Maxillofac Implants. 2001;16:73–9. [PubMed] [Google Scholar]
- 36.van Steenberghe D, Naert I, Bossuyt M, De Mars G, Calberson L, Ghyselen J, et al. The rehabilitation of the severely resorbed maxilla by simultaneous placement of autogenous bone grafts and implants: A 10-year evaluation. Clin Oral Investig. 1997;1:102–8. doi: 10.1007/s007840050020. [DOI] [PubMed] [Google Scholar]
- 37.Isaksson S, Alberius P. Maxillary alveolar ridge augmentation with onlay bone-grafts and immediate endosseous implants. J Craniomaxillofac Surg. 1992;20:2–7. doi: 10.1016/s1010-5182(05)80187-8. [DOI] [PubMed] [Google Scholar]
- 38.Adell R, Lekholm U, Gröndahl K, Brånemark PI, Lindström J, Jacobsson M. Reconstruction of severely resorbed edentulous maxillae using osseointegrated fixtures in immediate autogenous bone grafts. Int J Oral Maxillofac Implants. 1990;5:233–46. [PubMed] [Google Scholar]
- 39.Verhoeven JW, Cune MS, Terlou M, Zoon MA, de Putter C. The combined use of endosteal implants and iliac crest onlay grafts in the severely atrophic mandible: A longitudinal study. Int J Oral Maxillofac Surg. 1997;26:351–7. doi: 10.1016/s0901-5027(97)80796-5. [DOI] [PubMed] [Google Scholar]
- 40.McGrath CJ, Schepers SH, Blijdorp PA, Hoppenreijs TJ, Erbe M. Simultaneous placement of endosteal implants and mandibular onlay grafting for treatment of the atrophic mandible. A preliminary report. Int J Oral Maxillofac Surg. 1996;25:184–8. doi: 10.1016/s0901-5027(96)80026-9. [DOI] [PubMed] [Google Scholar]
- 41.Peñarrocha-Oltra D, Aloy-Prósper A, Cervera-Ballester J, Peñarrocha-Diago M, Canullo L, Peñarrocha-Diago M. Implant treatment in atrophic posterior mandibles: Vertical regeneration with block bone grafts versus implants with 5.5-mm intrabony length. Int J Oral Maxillofac Implants. 2014;29:659–66. doi: 10.11607/jomi.3262. [DOI] [PubMed] [Google Scholar]
- 42.Ozkan Y, Ozcan M, Varol A, Akoglu B, Ucankale M, Basa S. Resonance frequency analysis assessment of implant stability in labial onlay grafted posterior mandibles: A pilot clinical study. Int J Oral Maxillofac Implants. 2007;22:235–42. [PubMed] [Google Scholar]
- 43.Chiapasco M, Colletti G, Romeo E, Zaniboni M, Brusati R. Long-term results of mandibular reconstruction with autogenous bone grafts and oral implants after tumor resection. Clin Oral Implants Res. 2008;19:1074–80. doi: 10.1111/j.1600-0501.2008.01542.x. [DOI] [PubMed] [Google Scholar]
- 44.Bell RB, Blakey GH, White RP, Hillebrand DG, Molina A. Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J Oral Maxillofac Surg. 2002;60:1135–41. doi: 10.1053/joms.2002.34986. [DOI] [PubMed] [Google Scholar]
- 45.van der Meij EH, Blankestijn J, Berns RM, Bun RJ, Jovanovic A, Onland JM, et al. The combined use of two endosteal implants and iliac crest onlay grafts in the severely atrophic mandible by a modified surgical approach. Int J Oral Maxillofac Surg. 2005;34:152–7. doi: 10.1016/j.ijom.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 46.Vermeeren JI, Wismeijer D, van Waas MA. One-step reconstruction of the severely resorbed mandible with onlay bone grafts and endosteal implants. A 5-year follow-up. Int J Oral Maxillofac Surg. 1996;25:112–5. doi: 10.1016/s0901-5027(96)80053-1. [DOI] [PubMed] [Google Scholar]
- 47.Kim JW, Cho MH, Kim SJ, Kim MR. Alveolar distraction osteogenesis versus autogenous onlay bone graft for vertical augmentation of severely atrophied alveolar ridges after 12 years of long-term follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:540–9. doi: 10.1016/j.oooo.2013.06.037. [DOI] [PubMed] [Google Scholar]
- 48.Peñarrocha-Diago M, Aloy-Prósper A, Peñarrocha-Oltra D, Guirado JL, Peñarrocha-Diago M. Localized lateral alveolar ridge augmentation with block bone grafts: Simultaneous versus delayed implant placement: A clinical and radiographic retrospective study. Int J Oral Maxillofac Implants. 2013;28:846–53. doi: 10.11607/jomi.2964. [DOI] [PubMed] [Google Scholar]
- 49.Boronat A, Carrillo C, Penarrocha M, Pennarocha M. Dental implants placed simultaneously with bone grafts in horizontal defects: A clinical retrospective study with 37 patients. Int J Oral Maxillofac Implants. 2010;25:189–96. [PubMed] [Google Scholar]
- 50.Elo JA, Herford AS, Boyne PJ. Implant success in distracted bone versus autogenous bone-grafted sites. J Oral Implantol. 2009;35:181–4. doi: 10.1563/1548-1336-35.4.181. [DOI] [PubMed] [Google Scholar]
- 51.Sbordone L, Toti P, Menchini-Fabris G, Sbordone C, Guidetti F. Implant survival in maxillary and mandibular osseous onlay grafts and native bone: A 3-year clinical and computerized tomographic follow-up. Int J Oral Maxillofac Implants. 2009;24:695–703. [PubMed] [Google Scholar]
- 52.Levin L, Nitzan D, Schwartz-Arad D. Success of dental implants placed in intraoral block bone grafts. J Periodontol. 2007;78:18–21. doi: 10.1902/jop.2007.060238. [DOI] [PubMed] [Google Scholar]
- 53.Sethi A, Kaus T. Ridge augmentation using mandibular block bone grafts: Preliminary results of an ongoing prospective study. Int J Oral Maxillofac Implants. 2001;16:378–88. [PubMed] [Google Scholar]
- 54.Chiapasco M, Abati S, Romeo E, Vogel G. Clinical outcome of autogenous bone blocks or guided bone regeneration with e-PTFE membranes for the reconstruction of narrow edentulous ridges. Clin Oral Implants Res. 1999;10:278–88. doi: 10.1034/j.1600-0501.1999.100404.x. [DOI] [PubMed] [Google Scholar]
- 55.Roccuzzo M, Ramieri G, Spada MC, Bianchi SD, Berrone S. Vertical alveolar ridge augmentation by means of a titanium mesh and autogenous bone grafts. Clin Oral Implants Res. 2004;15:73–81. doi: 10.1111/j.1600-0501.2004.00998.x. [DOI] [PubMed] [Google Scholar]
- 56.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 57.Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990;1:33–40. doi: 10.1034/j.1600-0501.1990.010105.x. [DOI] [PubMed] [Google Scholar]
- 58.Nissan J, Marilena V, Gross O, Mardinger O, Chaushu G. Histomorphometric analysis following augmentation of the anterior atrophic maxilla with cancellous bone block allograft. Int J Oral Maxillofac Implants. 2012;27:84–9. [PubMed] [Google Scholar]
- 59.Nissan J, Romanos GE, Mardinger O, Chaushu G. Immediate nonfunctional loading of single-tooth implants in the anterior maxilla following augmentation with freeze-dried cancellous block allograft: A case series. Int J Oral Maxillofac Implants. 2008;23:709–16. [PubMed] [Google Scholar]
- 60.Acocella A, Bertolai R, Ellis E, 3rd, Nissan J, Sacco R. Maxillary alveolar ridge reconstruction with monocortical fresh-frozen bone blocks: A clinical, histological and histomorphometric study. J Craniomaxillofac Surg. 2012;40:525–33. doi: 10.1016/j.jcms.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 61.Orsini G, Stacchi C, Visintini E, Di Iorio D, Putignano A, Breschi L, et al. Clinical and histologic evaluation of fresh frozen human bone grafts for horizontal reconstruction of maxillary alveolar ridges. Int J Periodontics Restorative Dent. 2011;31:535–44. [PubMed] [Google Scholar]
- 62.Wallace S, Gellin R. Clinical evaluation of freeze-dried cancellous block allografts for ridge augmentation and implant placement in the maxilla. Implant Dent. 2010;19:272–9. doi: 10.1097/ID.0b013e3181e5d2a1. [DOI] [PubMed] [Google Scholar]
- 63.Carinci F, Brunelli G, Franco M, Viscioni A, Rigo L, Guidi R, et al. A retrospective study on 287 implants installed in resorbed maxillae grafted with fresh frozen allogenous bone. Clin Implant Dent Relat Res. 2010;12:91–8. doi: 10.1111/j.1708-8208.2008.00133.x. [DOI] [PubMed] [Google Scholar]
- 64.Barone A, Varanini P, Orlando B, Tonelli P, Covani U. Deep-frozen allogeneic onlay bone grafts for reconstruction of atrophic maxillary alveolar ridges: A preliminary study. J Oral Maxillofac Surg. 2009;67:1300–6. doi: 10.1016/j.joms.2008.12.043. [DOI] [PubMed] [Google Scholar]
- 65.Contar CM, Sarot JR, Bordini J, Jr, Galvão GH, Nicolau GV, Machado MA. Maxillary ridge augmentation with fresh-frozen bone allografts. J Oral Maxillofac Surg. 2009;67:1280–5. doi: 10.1016/j.joms.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 66.Soltan M, Smiler D, Prasad HS, Rohrer MD. Bone block allograft impregnated with bone marrow aspirate. Implant Dent. 2007;16:329–39. doi: 10.1097/ID.0b013e31815c8ef4. [DOI] [PubMed] [Google Scholar]
- 67.Gomes KU, Carlini JL, Biron C, Rapoport A, Dedivitis RA. Use of allogeneic bone graft in maxillary reconstruction for installation of dental implants. J Oral Maxillofac Surg. 2008;66:2335–8. doi: 10.1016/j.joms.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 68.Nissan J, Marilena V, Gross O, Mardinger O, Chaushu G. Histomorphometric analysis following augmentation of the posterior mandible using cancellous bone-block allograft. J Biomed Mater Res A. 2011;97:509–13. doi: 10.1002/jbm.a.33096. [DOI] [PubMed] [Google Scholar]
- 69.Carinci F, Brunelli G, Zollino I, Franco M, Viscioni A, Rigo L, et al. Mandibles grafted with fresh-frozen bone: An evaluation of implant outcome. Implant Dent. 2009;18:86–95. doi: 10.1097/ID.0b013e318192cbbe. [DOI] [PubMed] [Google Scholar]
- 70.Nissan J, Mardinger O, Strauss M, Peleg M, Sacco R, Chaushu G. Implant-supported restoration of congenitally missing teeth using cancellous bone block-allografts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:286–91. doi: 10.1016/j.tripleo.2010.04.042. [DOI] [PubMed] [Google Scholar]
- 71.Petrungaro PS, Amar S. Localized ridge augmentation with allogenic block grafts prior to implant placement: Case reports and histologic evaluations. Implant Dent. 2005;14:139–48. doi: 10.1097/01.id.0000163805.98577.ab. [DOI] [PubMed] [Google Scholar]
- 72.Novell J, Novell-Costa F, Ivorra C, Fariñas O, Munilla A, Martinez C. Five-year results of implants inserted into freeze-dried block allografts. Implant Dent. 2012;21:129–35. doi: 10.1097/ID.0b013e31824bf99f. [DOI] [PubMed] [Google Scholar]
- 73.Peleg M, Sawatari Y, Marx RN, Santoro J, Cohen J, Bejarano P, et al. Use of corticocancellous allogeneic bone blocks for augmentation of alveolar bone defects. Int J Oral Maxillofac Implants. 2010;25:153–62. [PubMed] [Google Scholar]
- 74.Viscioni A, Rigo L, Franco M, Brunelli G, Avantaggiato A, Sollazzo V, et al. Reconstruction of severely atrophic jaws using homografts and simultaneous implant placement: A retrospective study. J Oral Implantol. 2010;36:131–9. doi: 10.1563/AAID-JOI-D-09-00025. [DOI] [PubMed] [Google Scholar]
- 75.Keith JD, Jr, Petrungaro P, Leonetti JA, Elwell CW, Zeren KJ, Caputo C, et al. Clinical and histologic evaluation of a mineralized block allograft: Results from the developmental period (2001-2004) Int J Periodontics Restorative Dent. 2006;26:321–7. [PubMed] [Google Scholar]
- 76.Leonetti JA, Koup R. Localized maxillary ridge augmentation with a block allograft for dental implant placement: Case reports. Implant Dent. 2003;12:217–26. doi: 10.1097/01.id.0000078233.89631.f8. [DOI] [PubMed] [Google Scholar]
- 77.Lyford RH, Mills MP, Knapp CI, Scheyer ET, Mellonig JT. Clinical evaluation of freeze-dried block allografts for alveolar ridge augmentation: A case series. Int J Periodontics Restorative Dent. 2003;23:417–25. [PubMed] [Google Scholar]
- 78.Deluiz D, Oliveira LS, Pires FR, Tinoco EM. Time-dependent changes in fresh-frozen bone block grafts: Tomographic, histologic, and histomorphometric findings. Clin Implant Dent Relat Res. 2015;17:296–306. doi: 10.1111/cid.12108. [DOI] [PubMed] [Google Scholar]
- 79.Rocchietta I, Fontana F, Simion M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: A systematic review. J Clin Periodontol. 2008;35(8 Suppl):203–15. doi: 10.1111/j.1600-051X.2008.01271.x. [DOI] [PubMed] [Google Scholar]
- 80.Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants. 2009;24(Suppl):237–59. [PubMed] [Google Scholar]
- 81.Waasdorp J, Reynolds MA. Allogeneic bone onlay grafts for alveolar ridge augmentation: A systematic review. Int J Oral Maxillofac Implants. 2010;25:525–31. [PubMed] [Google Scholar]
- 82.Araújo PP, Oliveira KP, Montenegro SC, Carreiro AF, Silva JS, Germano AR. Block allograft for reconstruction of alveolar bone ridge in implantology: A systematic review. Implant Dent. 2013;22:304–8. doi: 10.1097/ID.0b013e318289e311. [DOI] [PubMed] [Google Scholar]
- 83.Spin-Neto R, Stavropoulos A, Dias Pereira LA, Marcantonio E, Jr, Wenzel A. Fate of autologous and fresh-frozen allogeneic block bone grafts used for ridge augmentation. A CBCT-based analysis. Clin Oral Implants Res. 2013;24:167–73. doi: 10.1111/j.1600-0501.2011.02324.x. [DOI] [PubMed] [Google Scholar]
- 84.Pelker RR, Friedlaender GE. Biomechanical aspects of bone autografts and allografts. Orthop Clin North Am. 1987;18:235–9. [PubMed] [Google Scholar]
- 85.Khojasteh A, Morad G, Behnia H. Clinical importance of recipient site characteristics for vertical ridge augmentation: A systematic review of literature and proposal of a classification. J Oral Implantol. 2013;39:386–98. doi: 10.1563/AAID-JOI-D-11-00210. [DOI] [PubMed] [Google Scholar]
- 86.Goldberg VM, Stevenson S. Natural history of autografts and allografts. Clin Orthop Relat Res. 1987;225:7–16. [PubMed] [Google Scholar]


