Abstract
Men’s tendency to delay health help-seeking is largely attributed to masculinity, but findings scarcely focus on African-American men who face additional race-related, help-seeking barriers. Building principally on reactance theory, we test a hypothesized model situating racial discrimination, masculinity norms salience, everyday racism (ERD), racial identity (RI), sense of control (SOC) and depressive symptomatology as key barriers to African-American men’s health help-seeking. 458 African-American men were recruited primarily from U.S. barbershops in the Western and Southern regions. The primary outcome was Barriers to Help-Seeking Scale (BHSS) scores. The hypothesized model was investigated with confirmatory factor and path analysis with tests for measurement invariance. Our model fit was excellent χ2(4,N = 457) = 3.84, p > .05; CFI = .99; TLI = 1.00; RMSEA = .00, and 90% CI [.00, .07] and operated equivalently across different age, income, and education strata. Frequent ERD and higher MNS contributed to higher BHHS scores. The relationship between ERD exposure and BHHS scores was partially mediated by diminished SOC and greater depressive symptomatology. Interventions aimed at addressing African-American men’s health help-seeking should not only address masculinity norms, but also threats to sense of control, and negative psychological sequelae induced by everyday racism.
Keywords: masculinity, men’s health, health disparities, help-seeking, African Americans
Introduction
In the U.S., men shoulder a significant amount of chronic disease burden 1 and have more abridged life-spans than women.2 Researchers partly attribute these disparate health outcomes to men’s tendency to “watch and wait” or delay help-seeking even when symptoms signal probable serious illness.3,4 Several studies affirm that men, relative to women, often fail to obtain preventive screenings, secure a usual source of care, and get timely medical interventions. 5–8 According to the most recent age-adjusted estimates, men made significantly fewer ambulatory healthcare visits (258 per 100) than women (342 per 100).9 Ambulatory visits are an important first point of contact for healthcare system contact among men. Thus, delayed health help-seeking creates missed opportunities for early chronic disease detection and the provision of critical health counseling. Delayed help-seeking and ensuing male health disparities also produce a significant impact on the U.S. national economy. 10 For example, Thorpe et al. calculated that of the $447.6 billion spent on the direct medical care costs for African American men, $24.2 billion of the overall costs is in excess expenditures.10 Equally as devastating are the socioemotional impacts on the women, partners, and children when the men they care about perish prematurely from preventable conditions. Thus, identifying barriers to health help-seeking among men is not only critical to reducing overall male health disparities but also to improving the vitality of families and our nation at large.
The potential negative impacts associated with delayed male health help-seeking are likely even more pronounced for African-American men who despite narrowing Black-White life-expectancy gaps, 11,12 live shorter lives than non-Hispanic White women, African-American women, and non-Hispanic White men.2 African-American men’s death rates from heart disease, some cancers (e.g., lung), and other health conditions amenable to preventive interventions are also significantly higher than those experienced by non-Hispanic White men.13–16 While these disparaging African-American male health outcomes are not solely attributable to help-seeking delays, they are less likely to manifest when the conditions driving them are detected and treated early. Indeed, multiple extant studies affirm that women from most racial/ethnic groups and non-Hispanic White men are significantly more likely to seek help for health problems than African-American men.17–21 Even in light of this compelling evidence, studies investigating barriers to African-American men’s health help-seeking are scarce and most of what we know at the population level stems from studies focused on psychological services use.22 Reducing barriers to help-seeking among African American men requires a broader health focus and specific attention to the unique factors driving delays among this group. The current study addresses this scientific gap.
Men are not biologically hardwired to delay help-seeking. Rather, barriers to men’s health help-seeking are socially determined. In this paper, we test a model built principally on reactance theory 23, which suggests that individuals are more likely to resist help-seeking when they confront life events that diminish sense of control (SOC), threaten freedom, and induce negative psychological states. Reactance theory is rooted in the assumption that salient aspects of identity shape the evaluation and appraisal of potentially threatening events. Such threatening events, hypothetically lead individuals to engage in activities designed to reclaim identity and restore personal SOC. Health behaviors, including help-seeking, are generally shaped by SOC.24,25 Masculinity norms, or shared cultural expectations about male behavior, 26 have a profound influence on men’s identities and help-seeking delays.3,27,28 As a multidimensional set of social prescriptions, masculinity norms theoretically encourage men to avoid help-seeking, display emotional stoicism or toughness, cope autonomously, and maintain a high sense of control even in the face of negative life experiences.29–31 Addis and Mahalik’s 3 seminal paper was the first to suggest a conceptual linkage between masculinity, male help-seeking, and reactance theory. Their conceptualization suggests that unmitigated internalization of masculinity norms contributes to men’s threat appraisal, coping response, and help-seeking behavior. They further suggest that a primary reason for help-seeking avoidance is that events, symptoms, or external cues signaling healthcare need also potentially threaten masculine identity, diminish SOC, and increase men’s need to engage in behavior designed to restore freedom. We assert that a similar process is at play for African American men.
To be certain, men who score higher on measures assessing dimensions of masculinity norms generally have less favorable help-seeking attitudes, 32–35 seek help for psychological problems less often, 34 and in some cases fail to obtain routine health examinations.36 African-American men also cite masculinity as a potential barrier to help-seeking. 37–40 Yet, the vast majority of investigations explore the influence of masculinity norms on help-seeking in predominately non-Hispanic White male samples and some report somewhat inconsistent findings.41 Study inconsistencies likely result from the way masculinity norms are typically measured and defined.42 For instance, researchers often measure how much men endorse a set of statements about prescribed or proscribed masculinity norms (e.g., Men should not reveal their worries to others) instead of assessing whether such norms are salient aspects of men’s identities. Theorists 43 suggest that measuring salience or the level of importance individuals place on social identities is key to understanding whether they govern actual behavioral outcomes (e.g., help-seeking). Definitions of masculinity among African-American men also vary from those characteristically applied to non-Hispanic white males 44 and there is significant intragroup variation in how even the most salient masculinity norms impact African-American men’s health-related behaviors. 41 Assessing the identity salience of masculinity norms provides a better approximation of whether men might invoke them when making health decisions or if doing so produces significant barriers to their health help-seeking. What is also needed are studies that investigate potential intermediary mechanisms linking masculinity norms to health help-seeking barriers among African-American men. We address these evidentiary gaps.
Masculinity is but one potentially salient factor contributing to African-American men’s help-seeking motivations. In fact, when study samples include African-American men, they often omit race-related factors cited as additional help-seeking barriers for this vulnerable population. 45–49 Studies in this vein lack the kind of specificity warranted to develop wholly effective, targeted interventions for African-American men. To advance intervention development, investigations are needed that explore how masculinity norms operate in tandem with social by-products of race to impact African American men’s help-seeking. Addressing prior scientific omissions, we include race-related factors and use Broman’s seminal work to define them as a constellation of experiences and practices shaped by the context of discriminatory treatment or unjust social arrangements.50 We also rely on descriptions by researchers who define race-related factors as those governing individual internalization of or response to discriminatory treatment (i.e., identity). Our study incorporates three race-related factors implicated in prior research as core dynamics of African American men’s threat appraisal and help-seeking: racial identity, race-related stress events, and John Henryism.51–53
Racial identity refers to “the significance and qualitative meaning that individuals attribute to their membership within their racial group.” 51 Racial identity is associated with African-American men’s help-seeking, 46,47,54–58 impacts sense of control or mastery 59,60 and is an important resource employed by African-Americans to appraise and cope with race-related stress events. 61 Race-related stress events are significant barriers to African-American men’s healthcare use 62,63 and minimize their trust in medical organizations and providers. 64,65 Cheatham and colleagues’ 66 review unearthed racism-related stress events as prominent help-seeking barriers among African-American men. Compared to African-American women, African-American men disproportionately report experiencing race-related stress,39,67–69 which theorists suggest generally threaten this group’s SOC and masculine identity. 70,71 A robust body of literature also affirms race-related stress or discrimination subsequently instigates depressed mood.62,72–80 Some authors suggest that diminished help-seeking among African-American men can be explained by their tendency to invoke certain kinds of behavioral coping dispositions. 20 John Henryism refers to behavioral coping disposition that is characterized by a self-perception that individuals can overcome demands with persistence, and hard work.52 John Henryism can hamper African-American men’s health help-seeking by promoting unmitigated self-reliance, and a sense that treatment-seeking denotes a weakness or character flaw. 81 Hence, we account for this behavioral coping disposition in the current study.
The Current Study
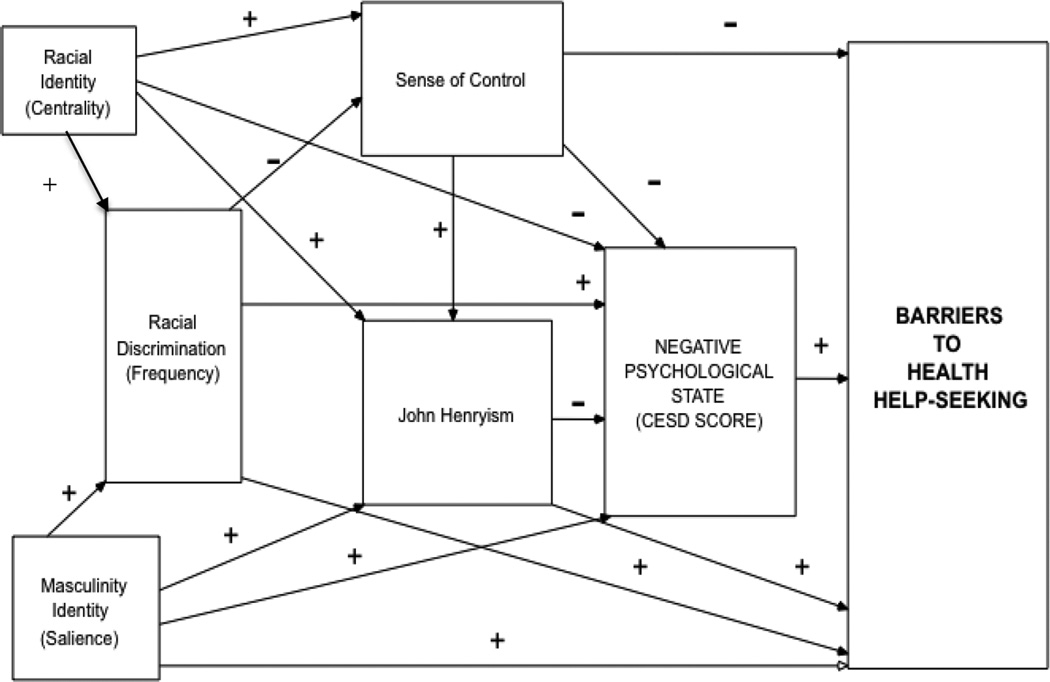
We test a hypothesized model predicting barriers to health help-seeking among African-American men (Figure 1) based primarily on reactance theory. 23 Specifically, we conceptualize barriers to health help-seeking as reactance to threatened masculinity identity and race-related stress events. Thus, we expect that a high degree of masculinity norms salience 82 and frequent race-related stress events will be associated with more barriers to health help-seeking (Hypothesis 1). This conceptualization is consistent with other theories of masculinity and African-American men’s health.83 Our model focuses on those race-related stress events characterized as “everyday racial discrimination” (ERD) because of their chronicity, persistence, and well-established relationship with negative psychological states.78,80,84,85 We also focus on one specific negative psychological state most consistently associated with ERD, depressed mood.80 Explicitly, we suggest that men with higher MNS will report more reactance (e.g., greater barriers to health help-seeking) because they experience help-seeking as more threatening to their masculine identity (Hypothesis 1). We also imply that men who report more frequent ERD will report more barriers to health help-seeking because these experiences persistently diminish their SOC, chronically instigate negative psychological states, and potentiate the invocation of identity-restorative coping dispositions (e.g., John Henryism)(Hypothesis 2). Similarly, our model proposes that African American men with higher racial identity (RI) scores will as a key factor in African American men’s help-seeking motivations. Masculinity norms endorsement is associated with depressed mood among men 86,87and with African-American men’s John Henryisim.88,85 Hence, our hypothesized model positions SOC, depressed mood states, and John Henryism 88 as key intermediary mechanisms linking MNS and ERD to barriers to health help-seeking (Hypothesis 2). We also, assert that racial identity positively impacts help-seeking indirectly through its tendency to increase SOC and diminish depressed mood. (Hypothesis 3).
Figure 1.
Hypothesized Path Model of African-American Men’s Barriers to Health Help-Seeking
Methods
Participants
Data for this study were taken from the African-American Men’s Health and Social Life Study (AAMHSL 2007–2010). The study sample included 458 community-residing African-American men (age ≥18 years) recruited from barbershops (80.7%) and a Historically Black College (HBU) (19.3%) in the West and South regions of the United States. The HBU student population was 77% African American and 33% male. Informed consent was obtained from each participant before they completed the surveys.
Procedures
Participants were recruited using flier advertisements, direct contact, and word-of-mouth. We prioritized barbershops because they are proven effective sites for recruiting African-American men from diverse socioeconomic statuses. 89 Recruitment efforts focused on “high volume” businesses (i.e. having a wait time of 30–60 minutes and serving a minimum of 30 customers daily) characterized by African American male community informants as popular. We focused on “high volume” shops because they provided ample wait times for men to complete surveys before receiving their haircuts. Study staff initially approached barbershops in-person or by telephone, and followed-up with more detailed information about the study including a copy of the survey and consent forms. Barbershop owners and barbers were invited to provide feedback about the survey content, length, and form, which was subsequently incorporated. Following this process, signed letters of support were obtained from barbershop owners. The receptionist or barber invited patrons to participate in a study about African-American men’s health; participants 18 years or older and who self-identified as African-American were eligible to complete the survey. Of the men approached in barbershops, 90% verbally consented to participate; most completed the survey during the wait time. The most frequently cited reason for nonparticipation was time constraint. Men who completed the survey in the barbershop received a voucher for a free haircut, valued at $25. In academic settings, we used similar procedures to recruit in places of high congregation (e.g., student unions, cafeterias, conference exhibit halls); 86% of the men approached completed the survey and received a $25 gift card. The study recruitment staff at barbershops and academic institutions consisted of African American women and men. All study procedures were reviewed and approved by the Institutional Review Board at The University of North Carolina at Chapel Hill
Measures
Independent and control variables
Sociodemographic characteristics
Sociodemographic characteristics assessed in this study were: age, level of education, relationship, employment, and insurance status, current residence, annual income, usual source of healthcare, and self-report of physician diagnosed chronic medical conditions.
Racial Identity (Centrality)
Racial identity was assessed with the 8-item Centrality scale of the Multidimensional Inventory of Black Identity (MIBI). 90 The Centrality scale measures the importance of being African-American to respondents’ identity. We focus on the racial centrality dimension of the MIBI because it has been linked to both the appraisal and mental health outcomes associated with racial discrimination experiences. 61,91 Participants endorse items such as, “In general, being Black is an important part of my self-image” on a 7-point Likert scale ranging from 1=Strongly Disagree to 7= Strongly Agree. The Centrality scale has been shown to have good internal consistency 92 and has been validated across diverse Black populations. 92,93 The Centrality scale has been shown to have good internal consistency 92 and has been validated across diverse Black populations. 90,92,93 The Centrality Scale has demonstrated good concurrent validity 90 and internal consistency in prior research studies internal consistency. 94,95For this study, Cronbach’s α was 0.88.
Masculinity Norms Salience
Masculinity norms salience was assessed with the 9-item Masculinity Norms Salience scale, constructed from previous qualitative work on masculinity meaning among African-American men.96 The Masculinity Norms Salience scale assesses the importance of traditional masculinity norms (e.g., having power and courage) to men’s identity. This scale has been used in other published studies assessing African-American men’s healthcare delays41 and is included because identity theorists propose that salience determines one’s commitment to norms and the likelihood that they will be invoked during stress appraisal and response.97,98 A mean score was computed from responses ranging from 1 (“not at all important”) to 5 (“extremely important”) (Cronbach’s α = 0.80). Higher mean scores on each of the scale indicate greater masculinity norms salience.
Everyday Racial Discrimination
To assess everyday racial discrimination, we used the 18-item Daily Life Experience 99 subscale of the Racism and Life Experiences Scales (RaLes). 100,101 Participants are asked to report the frequency of their experiences of “micro-aggressions” such as “Being treated rudely or disrespectfully” due to race on a scale ranging from 0=Never to 5=Once a week or more. The RaLes has been shown to have sound psychometric properties among African-Americans 100. The RaLes has demonstrated concurrent validity and correlates positively with the Index of Race-Related Stress, a conceptually similar measure and has also shown internal consistency (Cronbach’s α=0.83 to 0.90) in a community-based sample of Blacks 102. For this study, Cronbach’s α was 0.95.
Sense of Control
We assessed participants’ sense of control with the 7-item Sense of Mastery scale, which measures the degree to which individuals perceive having control over their lives.103 A sample item from the scale is “I have little control over the things that happen to me” and participants’ response options range from 1=Strongly Agree to 4=Strongly Disagree. The scale has shown satisfactory reliability and validity 104,105 and has demonstrated utility in African-American samples. 106,107. the concurrent validity of the Sense of Mastery, though previous studies have reported Cronbach’s α of 0.79 108 Cronbach’s α was 0.79.
John Henryism
We evaluated participants’ endorsement of John Henryism coping using the 12-item John Henryism Scale for Active Coping (JHAC12). 52 The JHAC12 is a trait-based measure of individuals’ general coping tendencies. Participants endorse items such as “Sometimes I feel that if anything is going to be done right, I have to do it myself” using response options anchored at 1=Completely False and 5=Completely True. Though we could not find an evaluation of its concurrent validity, the JHAC12 has been shown to be a valid and reliable measure of active coping among African-Americans.109 Previous studies report Cronbach’s α ranging from 0.60 to 0.80 in community-based samples of African-Americans. 110Cronbach’s α was 0.87 in the current study.
Depressed mood
We assessed depressed mood with the Center for Epidemiological Studies Depression Scale (CES-D).111 Participants indicate the frequency of emotions such as “I was happy” on a scale ranging from 0=Rarely or none of the time to 3=Most or all of the time. The CES-D is a well-established self-report measure of depressive symptomatology. It has been widely used in research studies with diverse populations and has demonstrated satisfactory validity and reliability among African-Americans. 112 There is support for the concurrent validity of the CES-D, which has shown a strong correlation with the Hamilton Clinician’s Rating Scale in a clinical sample.111 The CES-D has been shown to have a Cronbach’s α of 0.85 111 and has shown similar internal consistency estimates among African-Americans 113. Cronbach’s α was 0.79.
Outcome variable
Barriers to Help-Seeking Scale (BHSS)
We used the -item Barriers to Help-Seeking Scale to assess participants’ perceived barriers to seeking professional help for physical and mental health concerns (BHSS). 114 The BHSS presents respondents with a hypothetical situation in which they are in pain, and then asks them to indicate how much reasons such as “I’d feel better about myself knowing that I didn’t need help from others” would present barriers to seeking help. The original version of the BHSS comprised 54 items designed to identify a reason why an individual would refuse to seek out help to alleviate pain in his or her body. Forty-four of these items pertained to general health seeking, whereas eight additional items focused on targeted barriers specific to medical intervention (e.g., It’s difficult for me to talk with doctors and healthcare professionals). The BHSS consists of five subscales: (1) Need for Control and Self-Reliance, (2) Minimizing Problem and Resignation, (3) Concrete Barriers and Distrust of Caregivers, (4) Privacy, and (5) Emotional Control. Response options were anchored at 0=None and 4=All. The authors of the scale have demonstrated the scale’s reliability (Cronbach’s α=0.94–0.95) and its criterion, construct, and convergent validity in samples of undergraduate men.114 For the current study, the Cronbach’s α was 0.96.
Statistical Analyses
Descriptive analyses and zero-order correlations were calculated for all the study variables. We also examined confirmatory factor analysis 115,115 models that included each of BHSS items. These models were used to try and replicate the five-factor solution originally reported by Mansfield et al.116 We analyzed the five-factor CFA model across the entire sample and examined analogous CFA models for each of the different levels of age, income, and education prior to performing tests for MI.117,1 Tests for MI were conducted to evaluate whether the BHHS displayed a factor structure similar to the five-factor solution reported by Mansfield et al.116 and to assess whether the BHHS operates equivalently in African-American men across different levels of age, education, and income.118,119 Tests for MI were conducted using Mplus 5.2 120 with theta parameterization and robust weighted least squares estimation (WLSMV estimation), and methods recommended by Millsap and Yun-Tein121 for ordered-categorical data. The first level of invariance was configural invariance or the test of equal form across different groups.119 The second level of invariance testing was metric invariance or a test for equal factor loadings, and the third and final level of invariance included a test for equal factor loadings and thresholds across separate groups.121 Goodness of fit indices evaluated included the chi-square, comparative fit index (CFI), root-mean square error of approximation (RMSEA), and modification indices. Model fit indices and cut-off values for the fit indices selected were based on criteria primarily specified by Hu and Bentler.122 In particular, Hu and Bentler122 recommended that acceptable values for model fit indices include: RMSEA ≤ .08, CFI ≥ .95, and TLI ≥ .05. Because prior research has indicated that chi-square and chi-square difference tests are highly influenced by sample size118 tests for MI were performed using an alpha level of .01.
A BHSS scale derived from our CFA models was examined using path analysis models designed to assess the overall fit of our hypothesized model using the total BHSS score as the primary outcome. Next, we performed regression diagnostics before testing each study hypothesis and analyzing the proposed barriers to health help-seeking model. In particular, we examined Mahalanobis distance and variance inflation factors (VIFs) to ensure that there were no influential or outlying observations, and to assess multicollinearity among the study variables.123 We also performed tests for model equivalence124 to determine whether the associations among predictors and the BHSS scale generate from the CFA and multiple group CFA models operated equivalently across different levels of age (18–29; 30–39; and 40+ years), income, and education. Model equivalence was first tested by examining a restricted model where each of the regression paths was constrained to be equal across the different levels of age. Next, we examined models where the same regression paths were freely estimated across the different categories or levels of age. A chi-square difference test was then used to determine whether model equivalence could be established, or whether membership in different age groups moderated associations among the predictors and outcomes in the proposed reactance theory model. We compared chi-square values, parameter estimates, and standard errors from a model using full information maximum likelihood (FIML) to a model with a robust maximum likelihood (MLR) estimator used to correct for non-normality. Similar tests for model equivalence were run separately for different levels of income and education.
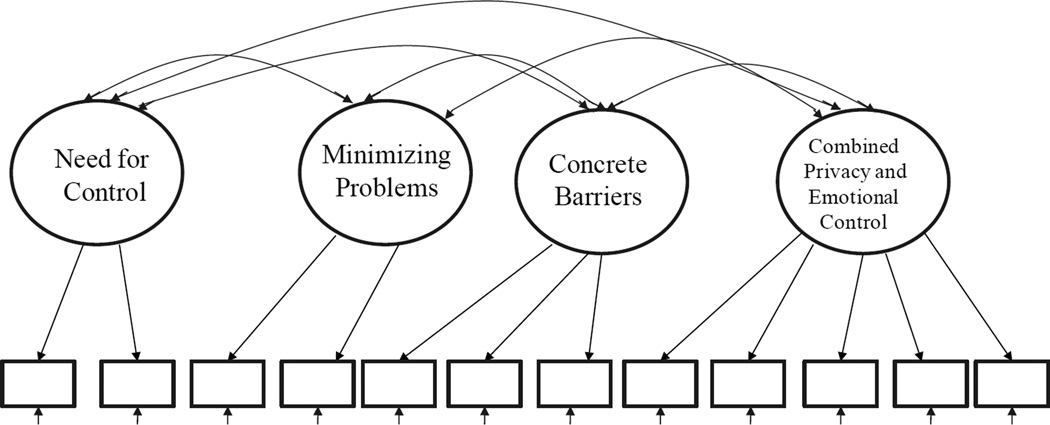
Preliminary Analyses
It was concluded that a five-factor solution did not perform well for a number of BHSS items. Further analyses revealed a linear dependency between two of the five factors (privacy and emotional control), such that the two factors had a correlation that was close to one. Thus, a four-factor solution (see Figure 3) was created by combining the latent variables privacy and emotional control into a single latent factor. The four-factor CFA model provided an excellent fit to the data: χ2(30,N = 446) = 59.08, p < .05; CFI = .99; TLI = .99; RMSEA = .04. After examining the four-factor CFA model, additional multiple-group, four-factor CFA models were used to test for MI across age, education, and income groups. .Once MI or partial MI 125 was established across the different levels of age, education, and income, we averaged the set of BHSS items that were used in the four-factor CFA model to create subscale scores and a total score (α = .91). Utilizing the total score created from the four-factor CFA model, correlations were computed for each of the study variables (See Table 2.)
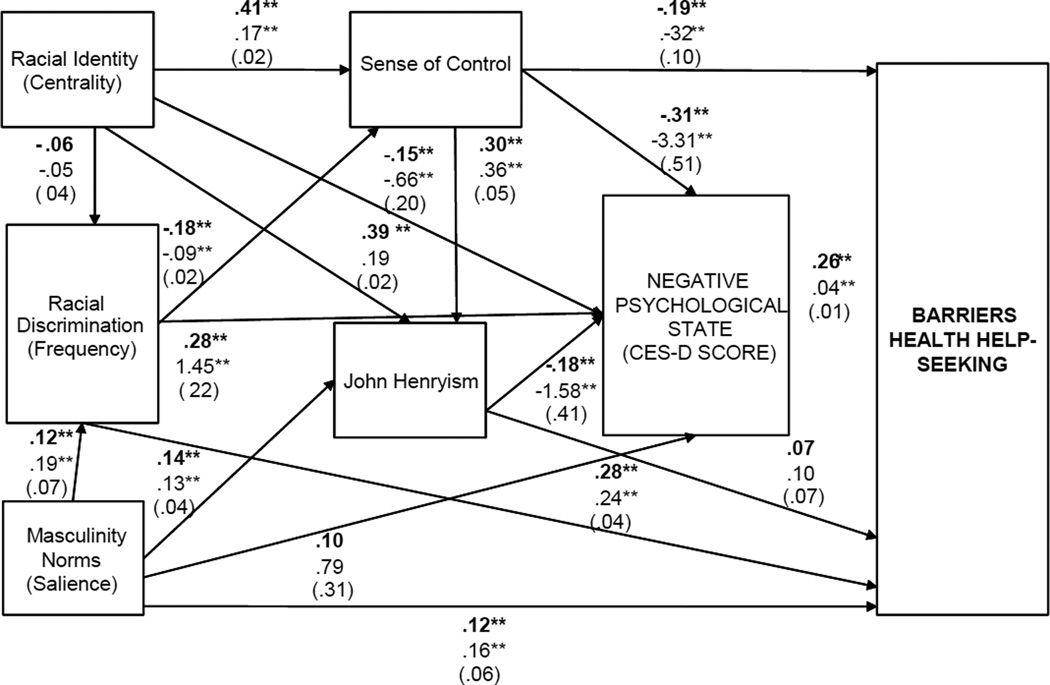
Figure 3.
Results for Hypothesized Path Model of African American Men’s Barriers to Health Help-Seeking
Note ** p < .01, * p < .05. Results in bold are standardized path coefficients. The standard errors for unstandardized results are displayed in parentheses.
Table 2.
Squared Multiple Correlations for Study Outcomes
| Study Variable | R-Squared |
|---|---|
| 1. BHSS Total Score | .32** |
| 2. Negative Psychological State (CES-D Score) | .41** |
| 3. John Henryism | .36** |
| 4. Sense of Control | .21** |
| 5. Everyday Racial Discrimination | .02 |
Notes.
p < .01,
p < .05.
We then used this score as the outcome measure in subsequent regression and path models. Preliminary results from our tests for normality indicated that the four-factor BHHS scores significantly departed from normality. Consequently, we obtained confidence intervals for mediated effects, and robust estimators that correct for inflated chi-square values and biased standard errors resulting from non-normality,126 which cannot be used to estimate bootstrap confidence intervals. Results from tests for MI revealed that model equivalence was also established across the different levels or categories of income and education. The chi-square values and standard errors did not differ substantially when comparing models estimated using FIML versus the MLR estimator. Therefore, the final analyses were performed using FIML estimation, which has the benefit that it uses all available cases in a dataset, and it generates parameter estimates that are less biased compared to missing data techniques such as listwise deletion.127
Results
Descriptive Statistics
Zero-order correlations between the BHSS score and the other study variables are displayed in Table 1. Descriptive analyses, including means and standard deviations for each study variable used in the final analyses are also shown in Table 1. Participants were fairly young (M=31 years) and most men (36.1%) had attained a high school education or less. Most were unmarried (78.1%), currently employed (78.1%), and uninsured (64.6%). The men, who primarily reside in the South (75%), reported low to modest annual incomes, with most (41%) earning less than $20,000. Lastly, more men reported a usual source of care (51.9%) and had no self-reported chronic conditions (63.3%).
Table 1.
Descriptive Statistics and Zero-Order Correlations among the Study Variables
| Study Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| 1. BHHS Total Score | 1.61 | .98 | -- | .45** | −.13** | −.36** | −.10* | .43** | .20** |
| 2. Negative Psychological State (CES-D Scores) | 12.41 | 6.11 | -- | −.41** | −.52** | −.40** | .40** | .09+ | |
| 3. John Henryism | 3.87 | .69 | -- | .46** | .52** | −.07 | .16** | ||
| 4. Sense of Control | 2.92 | .58 | -- | .42** | −.20** | −.01 | |||
| 5. Racial Identity (Centrality) | 5.37 | 1.40 | -- | −.06 | .07 | ||||
| 6. Everyday Racial Discrimination | 1.89 | 1.17 | -- | .12* | |||||
| 7. Masculinity Norms (Salience) | 3.47 | .75 | -- |
Notes.
p < .01,
p < .05,
p < .10
Testing the Overall Fit of our Hypothesized Barriers to Health Help-seeking Scale (BHSS) Model
Overall fit for our hypothesized model was excellent: χ2(3,N = 457) = 2.04, p > .05; CFI = 1.00; TLI = 1.00; RMSEA = .00, and 90% CI [.00, .07]. A path diagram for the hypothesized model, including standardized and unstandardized results is shown in Figure 3. Squared multiple correlations or R2 values for each study outcome are displayed in Table 2. Results from the chi-square difference test indicated that the constrained model provided a better fit to the data compared to the model where each of the regression paths was freely estimated. Thus, results suggested that our hypothesized model operated equivalently across the different age categories, and that the associations among the predictors and outcomes were not moderated by age.
H1: Higher MNS and More Frequent ERD Will Be Associated with More Barriers to Health Help-seeking
We first tested whether men with higher MNS and more frequent ERD had higher BHSS scores. Findings revealed that men with higher MNS reported more BHSS (b = .16, p< .005). ERD was also positively related to BHSS, such that men who experienced more frequent ERD had higher BHSS scores (b = .24, p< .001).
H2: SOC, Depressed mood, and John Henryism will be Key Intermediary Mechanisms between MNS, ERD, and BHHS
Findings from the hypothesized model revealed that African-American men with higher SOC had lower BHSS scores (b = −.32, p< .005). Put another way, men with low SOC reported greater barriers to health help seeking. Moreover, men with high CESD scores or more depressed mood reported increased barriers to help seeking (b = .04, p< .001). Based on 1,000 bootstrap samples, the 95% BC bootstrap confidence interval (CI) for the indirect or mediated relationship between ERD and BHSS passing through both SOC and CESD was [.01, .02]. The 95% CI for the mediated relation between ERD and BHSS through SOC was [.01, .06], and the CI for the indirect relation passing through only CESD was [.03, .10], suggesting partial mediation.
Results revealed that there was not a significant relationship between JH and BHSS scores. After examining 95% BC bootstrap CIs, results suggested that the combined indirect effect of MNS on BHSS passing through both JH and CESD was [−.02, −.00]. At the same time, results revealed that there was not a significant relationship between JH and the BHSS scale, nor was the relationship between masculinity identity salience and BHSS mediated by JH [−.01, .05].
H3: SOC and Depressed mood will be Key Intermediary Mechanisms between Racial Identity and BHHS
Results indicated there was a negative association between race identity (i.e., centrality) and ERD, but this result was not significant (b = −05, p>.05).We also examined whether the relationship between racial centrality and BHSS was mediated by SOC and CESD scores. Results demonstrated that men with higher race centrality reported greater SOC (b = .17, p< .001) and JH (b = .19, p< .001). Results also indicated that men with higher race centrality had lower CES-D scores (b = −.66, p< .005). Findings from 95% BC bootstrap CIs showed the combined indirect or mediated impact of racial centrality on BHSS passing through both SOC and CES-D scores was [−.04, −.01]. Results from the 95% CIs also suggested that the relationship between racial centrality and BHSS was fully mediated by SOC [−.10, −.02] and CESD [−.05, −.01], respectively.
Discussion
The purpose of our study was to test a theory-driven model of barriers of health help-seeking among African-American men. Many of our hypothesized relationships were supported through analysis. Overall, we found support for conceptualizing African-American men’s diminished health help-seeking as reactance or an attempt to restore autonomy, freedom, and sense of control in the face of persistent social identity threats.
Consistent with other findings,30,34 our results affirm that masculinity norms can mitigate African-American men’s health help-seeking. However, this study demonstrates that measuring the salience of masculinity norms is just as important as assessing how frequently men endorse them. In fact, our findings suggest that measuring masculinity norms in isolation without mutual consideration of race-related factors and exposures may lead to miscalculations about their weight in African American men’s help-seeking motivations. This might result in designing interventions that place heavy emphasis on masculinity norms change but that fail to address race-related factors that work in tandem to exacerbate or mitigate them. Previous researchers have drawn similar conclusions indicating the need to move measurement beyond gender prescriptions to gain better insight about when they are invoked and if they impact health behavior. 42,128
We found specifically that the relationship between masculinity norms and health help-seeking barriers among African-American men is not always direct, nor is it the only pathway of influence. For example, our hypothesis that depressed mood states mediate the relationship between masculine norms salience and barriers to help-seeking was also supported. It appears from our findings that when masculinity norms are salient, they produce the most significant health help-seeking barriers when African-American men are depressed. Others have found depression to figure prominently in African-American men’s healthcare seeking behaviors.36,129 Similarly, the current study suggests that the most psychologically vulnerable African-American men may be at greatest risk for delayed health help-seeking. Also, these findings imply that health interventions designed to disrupt men’s reliance on masculinity norms discouraging health help-seeking might have their greatest collective impact when directed at this more psychologically vulnerable group. Thus, while our findings expand the accumulating evidence-base documenting the impact of masculinity on men’s health behavior, they also push back on static assumptions about how they exert this influence.
Our results suggest that diminished health help-seeking is not purely a reactance to masculinity threats. African-American men face a number of race-related threats that are theorized to work in tandem with masculinity to impact their health behavior.83 We found that the most significant health help-seeking barriers arose among African-American men who reported more frequent exposure to everyday racial discrimination. We also found that men with more frequent everyday racial discrimination reported more barriers to health help-seeking. These findings also support a key assertion of reactance theory that health help-seeking barriers manifest most strongly for African American men in the presence of potentially threatening events. While evidence of the detrimental effects of everyday racial discrimination on health behaviors is not new, these results do paint a more nuanced understanding by delineating the intermediary roles played by sense of control, depressed mood, and coping dispositions in African-American men’s help-seeking attitudes. In this way, we speak to the growing call for studies moving beyond documenting direct associations towards delineating mechanism driving them.130
Sense of control emerged as a critical intermediary mechanism in our hypothesized model. Though we were not surprised to learn that lower sense of control was associated with greater barriers to health help-seeking, we were struck by the number of significant linkages it had to our model factors. African-American men in our sample reporting the most frequent exposure to everyday racial discrimination had the most diminished sense of personal mastery and control. These findings are consistent with what researchers surmise from prior studies.131,132 Adding to this evidence-base, we demonstrated that diminished sense of control stemming from everyday racial discrimination may in turn lead to more health help-seeking barriers. Changing exposure to everyday racial discrimination requires structural interventions, which should be mounted but may prove challenging even a so-called “post-racial” context. Sense of control or mastery, however, is modifiable and while pushing for structural change, health interventionists might also focus on enhancing sense of control among African-American men. Higher sense of personal control can also be protective against racial discrimination for African-American men. 72 Our findings support intervening on diminished feelings of control and power may to also protect African-American men from other pernicious health- effects of everyday racial discrimination documented in the literature.99,133,134 As demonstrated by the significant positive association between sense of control and John Henryism, some this protection may be afforded via its impact on coping dispositions. John Henryism can be a double-edged sword for African-American men because relying on this coping disposition may lead to unmitigated self-reliance and thus unintentionally mitigate help-seeking in the face of health threats. Thus, interventionists should be cautious in promoting or amplifying its habitual use.
Our study found that racial identity serves as a key appraisal mechanism in relation to race-related stress events like everyday racial discrimination. Black men with less race centrality reported more frequent occurrences of everyday racial discrimination. As hypothesized, higher race centrality was also shown to be positively associated with sense of control and negatively associated with depressed mood. Finally, sense of control and depressed mood were found to have a significant mediating effect between the relationship between race centrality and barriers to help-seeking among our study participants. In addition to playing its hypothesized role in stress appraisal, racial identity seems to exert its influence on help-seeking via sense of control. Specifically, our findings indicate that African-American men for whom racial identity figures more prominently into their self-concept may experience less negative impact from racial discrimination due to a higher sense of control over their environment. That is, they may feel more personal control despite encountering race-related threats. Prior research demonstrates the potential health buffering effects of racial identity.135 Although we did not explore this buffering effect in the current study, our findings similarly supports the notion that racial identity is a key enhancing component of African-American men’s help-seeking. Understanding how centrality of racial membership increases one’s sense of control and subsequent depressed mood should be investigated further and leveraged when developing interventions aimed at increasing Black men’s engagement in the health care system.
Like many cross-sectional investigations, our study is limited in its capacity to specify causal relationships between our study variables. Clearly, a more robust association between our model factors and barriers to health help-seeking might be established with longitudinal data. We also did not obtain our sample through methods that would assure that participants were nationally representative. However, the sociodemographic characteristics of our sample are similar to that found in the national population of African-American men.136,137 Recruiting African American men primarily from specific barbershops and academic institutions may have introduced some selection bias. For example, the mean age of our sample suggests that our hypothesized model may be more explanatory young adult African American males. However, we are encouraged by the sociodemographic distribution of our sample and its similarities to that of African American men at the population-level. Equally, we feel confident that recruitment primarily from barbershops is a study strength and provides a closer approximation of the general population than typical college subject pools relied upon by researchers investigating help-seeking barriers. Future studies may want to introduce randomization and a broader array of recruitment sites to ensure fuller representation. Masculinity’s influence on men’s help-seeking is context-dependent 138 and certain dimensions of masculinity (e.g., self-reliance) reduce preventive screening delays among African-American men. 139 Similarly, racial identity and masculinity is multidimensional and we only explored one dimension in our analysis. Thus, future studies will want to assess impacts on help-seeking contributed by a wider range of masculinity and racial identity dimensions. Lastly, the measure of health help-seeking is not disease or condition specific and barriers may vary according to perceived or actual condition severity, with hopes that the reducing costly help-seeking delays and the health disparities they ultimately generate among African American men.
Despite these limitations, our findings have several notable strengths. First, to our knowledge, this is one of the first studies to explore the factor structure of the BHSS among African-American men. We also extend the evidence-base by taken a theory-driven, empirical approach to investigating barriers to health help-seeking among African-American men. We used a community-based data collection strategy that allowed us to engage African-American men who are perhaps the most underserved by formal healthcare organizations.
Conclusions
Reducing health disparities and inequities among African-American men is hinged on timely help-seeking. However, if we want to improve disparate health outcomes among African-American men then we have to address everyday racial discrimination experiences that chip away at their help-seeking motivations. We also have to devise, implement, and sustain policies that address the deep entrenchment of racial discrimination in structures where African-American men live, work, play, obtain healthcare, and get educated. Ultimately, delayed health help-seeking among African-American men might also be more effectively addressed if it were understood less as stereotypical male healthcare avoidance and more as a protective strategy mounted in the face of clear and present social threat.
Figure 2.
Four-factor CFA model for Barriers to Health Help-Seeking Scale Items
Acknowledgments
Data collection for this research was supported by the Robert Wood Johnson Foundation Health & Society Scholars Program, and The University of North Carolina Cancer Research Fund. Additional research and salary support during the preparation of this manuscript was provided to the first author from the National Institute for Minority Health and Health Disparities (Award # 1L60MD002605-01), National Cancer Institute (Grant # 3U01CA114629-04S2), and CFAR (Grant # P30 AI50410).The first author is currently supported by the National Institutes of Drug Abuse (Grant # 1K01 DA032611-01A1).The first author wishes to thank current and past members of the UNC Men’s Health Research Lab: Derrick Matthews, Travis Melvin, Justin Smith, Allison Mathews, Dr. Keon Gilbert, Melvin R. Muhammad, and Donald Parker for their assistance with data collection for the African-American Men’s Health & Social Life Study. The first author also thanks Dr. Amani Nuru-Jeter, Keith Hermanstyne, and Adebiyi Adesina for their assistance with data collection.
Footnotes
Measurement invariance or measurement equivalence is defined as the “degree to which measurements conducted under different conditions yield equal measures of the same attributes” (Meade and Bauer, 2007, p. 611). Tests for ME/I are generally used to answer questions concerning whether individuals from different groups interpret a measure in a conceptually similar manner. Put another way, measurement invariance pertains to whether there is consistency of measurement across subgroups of a given population, and if the operationalization of a construct has the same meaning under different conditions.
Contributor Information
Wizdom Powell, Email: wizdomp@email.unc.edu, University of North Carolina at Chapel Hill.
Leslie B. Adams, Email: adamslb@live.unc.edu, University of North Carolina at Chapel Hill.
Yasmin Cole-Lewis, Email: ycolelew@umich.edu, University of Michigan – Ann Arbor.
Amma Agyemang, Email: agyemangaa@vcu.edu, Virginia Commonwealth University.
Rachel D. Upton, Email: rupton@air.org, American Institutes for Research.
References
- 1.Singh-Manoux A, Gueguen A, Ferrie J, et al. Gender Differences in the Association Between Morbidity and Mortality Among Middle-Aged Men and Women. Am J Public Health. 2008 Dec 1;98(12):2251–2257. doi: 10.2105/AJPH.2006.107912. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy S, Kochanek K, Xu J. Deaths: Final data for 2012. National vital statistics. 2015 [PubMed] [Google Scholar]
- 3.Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. American Psychologist. 2003;58(1):5. doi: 10.1037/0003-066x.58.1.5. [DOI] [PubMed] [Google Scholar]
- 4.Mansfield AK, Addis ME, Mahalik JR. “ Why Won’t He Go to the Doctor?”: The Psychology of Men’s Help Seeking. International Journal of Men’s Health. 2003;2(2):93–109. [Google Scholar]
- 5.Cherry DK, Woodwell DA, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2005 summary. Advance data. 2007;2007(387):1–39. [PubMed] [Google Scholar]
- 6.Sandman D, Simantov E, An C, Fund C, Harris L. Out of touch: American men and the health care system. Commonwealth Fund New York. 2000 [Google Scholar]
- 7.Viera A, Thorpe J, Garrett J. Effects of sex, age, and visits on receipt of preventive healthcare services: a secondary analysis of national data. BMC Health Serv Res. 2006;6(1):15. doi: 10.1186/1472-6963-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for US Adults: National health interview survey, 2010. Vital and Health Statistics. Series 10, Data from The National Health Survey. 2012;(252):1–207. [PubMed] [Google Scholar]
- 9.Ashman J, Hing E, Talwalkar A. Variation in Physician Office Visit Rates by Patient Characteristics and State, 2012. NCHS data brief. 2015;(212):1–8. [PubMed] [Google Scholar]
- 10.Thorpe RJ, Jr, Richard P, Bowie JV, LaVeist TA, Gaskin DJ. Economic burden of men’s health disparities in the United States. International Journal of Men’s Health. 2013;12(3) [Google Scholar]
- 11.Harper S, Lynch J, Burris S, Davey Smith G. Trends in the Black-White Life Expectancy Gap in the United States, 1983–2003. J Am Med Assoc. 2007 Mar 16;297:1224–1232. doi: 10.1001/jama.297.11.1224. 2007. [DOI] [PubMed] [Google Scholar]
- 12.Xu J, Murphy S, Kochanek K. Deaths: final data for 2013. National Vital Statistics Reports. 2015;64(2) [PubMed] [Google Scholar]
- 13.Barnett E, Casper ML, Halverson JA, et al. Men and heart disease an atlas of racial and ethnic disparities in mortality. Morgantown, W. Va: Office for Social Environment and Health Research, West Virginia University; 2000. [Google Scholar]
- 14.Thom T, Haase N, Rosamond W, et al. Heart Disease and Stroke Statistics--2006 Update: A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006 Feb 14;113(6):e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. 2006. [DOI] [PubMed] [Google Scholar]
- 15.American Cancer Society. Colorectal Cancer Facts & Figures 2008–2010. Atlanta: 2008. [Google Scholar]
- 16.American Cancer Society. Cancer Facts & Figures for African Americans 2009–2010. Atlanta: 2009. [Google Scholar]
- 17.Neighbors HW, Howard CS. Sex differences in professional help seeking among adult Black Americans. American Journal of Community Psychology. 1987;15(4):403–417. doi: 10.1007/BF00915210. [DOI] [PubMed] [Google Scholar]
- 18.Gourash N. Help-seeking: A review of the literature. American Journal of Community Psychology. 1978;6(5):413–423. doi: 10.1007/BF00941418. [DOI] [PubMed] [Google Scholar]
- 19.Moller-Leimkuhler AM. Barriers to help-seeking by men: a review of sociocultural and clinical literature with particular reference to depression. Journal of Affective Disorders. 2002;71(1–3):1–9. doi: 10.1016/s0165-0327(01)00379-2. [DOI] [PubMed] [Google Scholar]
- 20.Neighbors HW. The help-seeking behavior of black Americans: a summary of findings from the National Survey of Black Americans. Journal of the National Medical Association. 1988;80(9):1009. [PMC free article] [PubMed] [Google Scholar]
- 21.Zoratti EM, Havstad S, Rodriguez J, Robens-Paradise Y, Lafata JE, McCarthy B. Health service use by African Americans and Caucasians with asthma in a managed care setting. American journal of respiratory and critical care medicine. 1998;158(2):371. doi: 10.1164/ajrccm.158.2.9608039. [DOI] [PubMed] [Google Scholar]
- 22.Neighbors HW, Caldwell C, Williams DR, et al. Race, ethnicity, and the use of services for mental disorders: results from the National Survey of American Life. Archives of general psychiatry. 2007;64(4):485–494. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- 23.Brehm JW. A Theory of Psychological Reactance. Oxford England: Academic Press; 1966. [Google Scholar]
- 24.Kleinberg A, Aluoja A, Vasar V. Social support in depression: structural and functional factors, perceived control and help-seeking. Epidemiology and psychiatric sciences. Dec. 2013;22(4):345–353. doi: 10.1017/S2045796013000504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gabay G. Perceived control over health, communication and patient-physician trust. Patient education and counseling. 2015 Jun;29 doi: 10.1016/j.pec.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 26.Spence JT, Helmreich RL. Masculinity and femininity: Their psychological dimensions, correlates, and antecedents. Austin, TX: University of Texas Press; 1978. [Google Scholar]
- 27.Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. Journal of Advanced Nursing. 2005;49(6):616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- 28.Fish JA, Prichard I, Ettridge K, Grunfeld EA, Wilson C. Psychosocial factors that influence men’s help-seeking for cancer symptoms: a systematic synthesis of mixed methods research. Psycho-Oncology. 2015;24(10):1222–1232. doi: 10.1002/pon.3912. [DOI] [PubMed] [Google Scholar]
- 29.Courtenay WH. Constructions of masculinity and their influence on men’s well-being: a theory of gender and health. Social Science & Medicine. 2000;50(10):1385–1401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 30.Mahalik JR, Good GE, Englar-Carlson M. Masculinity scripts, presenting concerns, and help seeking: Implications for practice and training. Professional Psychology: Research and Practice. 2003;34(2):123. [Google Scholar]
- 31.Levant RF, Hirsch LS, Celentano E, Cozz TM. The male role: An investigation of contemporary norms. Journal of Mental Health Counseling. 1992;14(3):325–337. [Google Scholar]
- 32.Sánchez FJ, Bocklandt S, Vilain E. The relationship between help-seeking attitudes and masculine norms among monozygotic male twins discordant for sexual orientation. Health Psychology. 2013;32(1):52–56. doi: 10.1037/a0029529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Himmelstein MS, Sanchez DT. Masculinity impediments: Internalized masculinity contributes to healthcare avoidance in men and women. Journal of Health Psychology. 2014 Oct 7;:2014. doi: 10.1177/1359105314551623. [DOI] [PubMed] [Google Scholar]
- 34.Vogel DL, Heimerdinger-Edwards SR, Hammer JH, Hubbard A. “Boys don’t cry”: Examination of the links between endorsement of masculine norms, self-stigma, and help-seeking attitudes for men from diverse backgrounds. Journal of Counseling Psychology. 2011;58(3):368–382. doi: 10.1037/a0023688. [DOI] [PubMed] [Google Scholar]
- 35.Yousaf O, Popat A, Hunter MS. An investigation of masculinity attitudes, gender, and attitudes toward psychological help-seeking. Psychology of Men & Masculinity. 2014 [Google Scholar]
- 36.Hammond WP, Matthews D, Corbie-Smith G. Psychosocial Factors Associated With Routine Health Examination Scheduling and Receipt Among African American Men. Journal of the National Medical Association. 2010 Apr;102(4):276–289. doi: 10.1016/s0027-9684(15)30600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wade JC. Masculinity ideology, male reference group identity dependence, and African American men’s health-related attitudes and behaviors. Psychology of Men & Masculinity. 2008;9(1):5. [Google Scholar]
- 38.Griffith DM, Allen JO, Gunter K. Social and cultural factors influence African American men’s medical help seeking. Research on Social Work Practice. 2010 1049731510388669. [Google Scholar]
- 39.Watkins DC, Green BL, Rivers BM, Rowel KL. Depression and black men: implications for future research. The Journal of Men’s Health & Gender. 2006;3(3):227–235. [Google Scholar]
- 40.Watkins DC, Walker RL, Griffith DM. A meta-study of Black male mental health and well-being. Journal of Black Psychology. 2009:1–29. [Google Scholar]
- 41.Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. J Gen Intern Med. Dec. 2010;25(12):1300–1308. doi: 10.1007/s11606-010-1481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Griffith DM, Gunter K, Watkins DC. Measuring masculinity in research on men of color: Findings and future directions. American Journal of Public Health. 2012;102(S2):S187–S194. doi: 10.2105/AJPH.2012.300715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stryker S, Serpe RT. Personality, roles, and social behavior. Springer; 1982. Commitment, identity salience, and role behavior: Theory and research example; pp. 199–218. [Google Scholar]
- 44.Hammond WP, Mattis JS. Being a Man About It: Manhood Meaning Among African American Men. Psychology of Men & Masculinity. 2005;6(2):114–126. [Google Scholar]
- 45.Scott LD, Jr, McMillen JC, Snowden LR. Informal and Formal Help Seeking Among Older Black Male Foster Care Youth and Alumni. Journal of Child and Family Studies. 2015;24(2):264–277. doi: 10.1007/s10826-013-9832-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richman LS, Kohn-Wood LP, Williams DR. The role of discrimination and racial identity for mental health service utilization. Journal of Social and Clinical Psychology. 2007;26(8):960–981. [Google Scholar]
- 47.Townes DL, Chavez-Korell S, Cunningham NJ. Reexamining the relationships between racial identity, cultural mistrust, help-seeking attitudes, and preference for a Black counselor. Journal of Counseling Psychology. 2009;56(2):330–336. [Google Scholar]
- 48.White AM. Gender role conflict and racial identity as indicators of Black men’s help seeking attitudes, ProQuest Information & Learning. 2002 [Google Scholar]
- 49.Buser JK. Treatment-seeking disparity between African Americans and Whites: Attitudes toward treatment, coping resources, and racism. Journal of Multicultural Counseling and Development. 2009;37(2):94. [Google Scholar]
- 50.Broman CL. Race-related factors and life satisfaction among African Americans. Journal of Black Psychology. 1997;23(1):36–49. [Google Scholar]
- 51.Sellers RM, Smith MA, Shelton JN, Rowley SJ, Chavous TM. Multidimensional model of racial identity: A reconceptualization of African American racial identity. Personality and Social Psychology Review. 1998;2(1):18. doi: 10.1207/s15327957pspr0201_2. [DOI] [PubMed] [Google Scholar]
- 52.James SA. John Henryism and the health of African-Americans. Culture, medicine and psychiatry. 1994;18(2):163–182. doi: 10.1007/BF01379448. [DOI] [PubMed] [Google Scholar]
- 53.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans - A biopsychosocial model. American Psychologist. 1999 Oct;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 54.Longshore D. Help-seeking by African American drug users: A prospective analysis. Addictive Behaviors. 1999;24(5):683–686. doi: 10.1016/s0306-4603(98)00111-7. [DOI] [PubMed] [Google Scholar]
- 55.Delphin ME, Rollock D. University alienation and African American ethnic identity as predictors of attitudes toward, knowledge about, and likely use of psychological services. Journal of College Student Development. 1995;36(4):337–346. [Google Scholar]
- 56.Paris M, Jr, Añez LM, Bedregal LE, Andrés-Hyman RC, Davidson L. Help Seeking and Satisfaction among Latinas: The Roles of Setting, Ethnic Identity, and Therapeutic Alliance. Journal of Community Psychology. 2005;33(3):299–312. [Google Scholar]
- 57.Wallace BC, Constantine MG. Africentric cultural values, psychological help-seeking attitudes, and self-concealment in African American college students. Journal of Black Psychology. 2005;31(4):369–385. [Google Scholar]
- 58.So DW, Gilbert S, Romero S. Help-seeking attitudes among African American college students. College Student Journal. 2005;39(4):806. [Google Scholar]
- 59.Hughes M, Demo DH. Self-perceptions of Black Americans: Self-esteem and personal efficacy. American Journal of Sociology. 1989:132–159. [Google Scholar]
- 60.Oler CH. Psychotherapy with Black clients’ racial identity and locus of control. Psychotherapy: Theory, Research, Practice, Training. 1989;26(2):233. [Google Scholar]
- 61.Sellers RM, Caldwell CH, Schmeelk-Cone KH, Zimmerman MA. Racial Identity, Racial Discrimination, Perceived Stress, and Psychological Distress among African American Young Adults. Journal of Health and Social behavior. 2003;44(3):302–317. [PubMed] [Google Scholar]
- 62.Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. Journal of general internal medicine. 2007;22(3):389–395. doi: 10.1007/s11606-006-0057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cheatham CT, Barksdale DJ, Rodgers SG. Barriers to health care and health seeking behaviors faced by Black men. Journal of the American Academy of Nurse Practitioners. 2008;20(11):555–562. doi: 10.1111/j.1745-7599.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 64.Hammond WP. Psychosocial Correlates of Medical Mistrust Among African American Men. American Journal of Community Psychology. 2010 Mar;45(1–2):87–106. doi: 10.1007/s10464-009-9280-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Medical Care Research and Review. 2000;57(4 suppl):146–161. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- 66.Cheatham CT, Barksdale DJ, Rodgers SG. Barriers to health care and health-seeking behaviors faced by Black men. Journal of the American Academy of Nurse Practitioners. 2008;20(11):555–562. doi: 10.1111/j.1745-7599.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 67.Watkins DC, Hudson DL, Caldwell CH, Siefert K, Jackson JS. Discrimination, Mastery, and Depressive Symptoms Among African American Men. Res Soc Work Pract. 2011 May;21(3):269–277. doi: 10.1177/1049731510385470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pieterse AL, Carter RT. An examination of the relationship between general life stress, racism-related stress, and psychological health among black men. Journal of Counseling Psychology. 2007;54(1):101. [Google Scholar]
- 69.Utsey SO, Payne Y. Psychological impacts of racism in a clinical versus normal sample of African American men. Journal of African American Studies. 2000;5(3):57–72. [Google Scholar]
- 70.Franklin AJ. Invisibility syndrome and racial identity development in psychotherapy and counseling African American men. The Counseling Psychologist. 1999;27(6):761. [Google Scholar]
- 71.Franklin AJ, Boyd-Franklin N. Invisibility syndrome: A clinical model of the effects of racism on African-American males. American Journal of Orthopsychiatry. 2000;70(1):33–41. doi: 10.1037/h0087691. [DOI] [PubMed] [Google Scholar]
- 72.Watkins DC, Hudson DL, Howard Caldwell C, Siefert K, Jackson JS. Discrimination, Mastery, and Depressive Symptoms Among African American Men. Research on Social Work Practice. 2011;21(3):269. doi: 10.1177/1049731510385470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. 1996/10/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Blanchard J, Lurie N. RESPECT: Patient reports of disrespect in the healthcare setting and its impact on care. Journal of Family Practice. 2004;53(9):721–731. [PubMed] [Google Scholar]
- 75.Van Houtven CH, Voils CI, Oddone EZ, et al. Perceived discrimination and reported delay of pharmacy prescriptions and medical tests. Journal of general internal medicine. 2005;20(7):578–583. doi: 10.1111/j.1525-1497.2005.0123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Trivedi AN, Ayanian JZ. Perceived discrimination and use of preventive health services. Journal of general internal medicine. 2006;21(6):553–558. doi: 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Social Science & Medicine. 2006;63(6):1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 78.Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. American Journal of Public Health. 2006;96(7):1265. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Crawley LVM, Ahn DK, Winkleby MA. Perceived medical discrimination and cancer screening behaviors of racial and ethnic minority adults. Cancer Epidemiology Biomarkers & Prevention. 2008;17(8):1937. doi: 10.1158/1055-9965.EPI-08-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alvidrez J, Snowden LR, Kaiser DM. The experience of stigma among Black mental health consumers. Journal of health care for the poor and underserved. 2008;19(3):874–893. doi: 10.1353/hpu.0.0058. [DOI] [PubMed] [Google Scholar]
- 82.Pence BW, Gaynes BN, Atashili J, et al. Feasibility, safety, acceptability, and preliminary efficacy of measurement-based care depression treatment for HIV patients in Bamenda, Cameroon. AIDS and behavior. 2014 Jun;18(6):1142–1151. doi: 10.1007/s10461-014-0727-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hammond WP, Fleming PJ, Villa-Torres L. Everyday racism as a threat to the masculine social self: Framing investigations of African American male health disparities. 2016 [Google Scholar]
- 84.Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA. Perceived discrimination and mental health symptoms among Black men with HIV. Cultural diversity & ethnic minority psychology. 2011 Jul;17(3):295–302. doi: 10.1037/a0024056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Matthews DD, Hammond WP, Nuru-Jeter A, Cole-Lewis Y, Melvin T. Racial Discrimination and Depressive Symptoms Among African-American Men: The Mediating and Moderating Roles of Masculine Self-Reliance and John Henryism. Psychology of Men & Masculinity. 2013 Jan;14(1):35–46. doi: 10.1037/a0028436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cournoyer RJ, Mahalik JR. Cross-sectional study of gender role conflict examining college-aged and middle-aged men. Journal of Counseling Psychology. 1995;42(1):11. [Google Scholar]
- 87.Good GE, Mintz LB. Gender role conflict and depression in college men: Evidence for compounded risk. Journal of Counseling & Development. 1990;69(1):17–21. [Google Scholar]
- 88.Kraft AD, Quimbo SA, Solon O, Shimkhada R, Florentino J, Peabody JW. The Health and Cost Impact of Care Delay and the Experimental Impact of Insurance on Reducing Delays. The Journal of Pediatrics. 2009;155(2):281–285.e281. doi: 10.1016/j.jpeds.2009.02.035. 8// [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hart A, Bowen DJ. The feasibility of partnering with African-American barbershops to provide prostate cancer education. Ethnicity and Disease. 2004;14(2):269–273. [PubMed] [Google Scholar]
- 90.Sellers RM, Rowley SAJ, Chavous TM, Shelton JN, Smith MA. Multidimensional Inventory of Black Identity: A preliminary investigation of reliability and constuct validity. Journal of Personality and Social Psychology. 1997;73(4):805. [Google Scholar]
- 91.Sellers RM, Copeland-Linder N, Martin PP, Lewis RH. Racial identity matters: The relationship between racial discrimination and psychological functioning in African American adolescents. Journal of Research on Adolescence. 2006;16(2):187–216. [Google Scholar]
- 92.Vandiver BJ, Worrell FC, Delgado-Romero EA. A Psychometric Examination of Multidimensional Inventory of Black Identity (MIBI) Scores. Assessment. 2009;16(4):337. doi: 10.1177/1073191109341958. [DOI] [PubMed] [Google Scholar]
- 93.Walsh JJ. The multidimensional inventory of Black identity: A validation study in a British sample. Journal of Black Psychology. 2001;27(2):172. [Google Scholar]
- 94.Cokley KO, Helm K. Testing the construct validity of scores on the Multidimensional Inventory of Black Identity. Measurement and Evaluation in Counseling and Development. 2001;34(2):80. [Google Scholar]
- 95.Sellers RM, Smith MA, Shelton JN, Rowley SA, Chavous TM. Multidimensional model of racial identity: A reconceptualization of African American racial identity. Personality and Social Psychology Review. 1998;2(1):18–39. doi: 10.1207/s15327957pspr0201_2. [DOI] [PubMed] [Google Scholar]
- 96.Hammond WP, Mattis JS. Being a man about It: Manhood meaning among African American men. Psychol Men Masc. 2005;6(2):114–126. [Google Scholar]
- 97.Hogg MA, Terry DJ, White KM. A Tale of Two Theories: A Critical Comparison of Identity Theory with Social Identity Theory. Soc Psychol Q. 1995;58(4):255–269. [Google Scholar]
- 98.Sheldon S, Serpe RT. Identity Salience and Psychological Centrality: Equivalent, Overlapping, or Complementary Concepts? Soc Psychol Q. 1994;57(1):16–35. [Google Scholar]
- 99.Chae DH, Lincoln KD, Adler NE, Syme SL. Do experiences of racial discrimination predict cardiovascular disease among African American men? The moderating role of internalized negative racial group attitudes. Social Science & Medicine. 2010;71(6):1182–1188. doi: 10.1016/j.socscimed.2010.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Harrell S. The racism and life experiences scales (RaLES-Revised) Unpublished manuscript. 1997 [Google Scholar]
- 101.Harrell SP. A Multidimensional Conceptualization of Racism Related Stress: Implications for the Well Being of People of Color. American Journal of Orthopsychiatry. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- 102.Utsey SO, Ponterotto JG. Development and validation of the Index of Race-Related Stress (IRRS) Journal of Counseling Psychology. 1996;43(4):490. [Google Scholar]
- 103.Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social behavior. 1978:2–21. [PubMed] [Google Scholar]
- 104.Marshall GN, Lang EL. Optimism, self-mastery, and symptoms of depression in women professionals. Journal of Personality and Social Psychology. 1990;59(1):132. doi: 10.1037//0022-3514.59.1.132. [DOI] [PubMed] [Google Scholar]
- 105.Rosenfield S. Factors contributing to the subjective quality of life of the chronic mentally ill. Journal of Health and Social behavior. 1992:299–315. [PubMed] [Google Scholar]
- 106.Ennis NE, Hobfoll SE, Schr^der KEE. Money doesn’t talk, it swears: how economic stress and resistance resources impact inner-city women’s depressive mood. American Journal of Community Psychology. 2000;28(2):149–173. doi: 10.1023/A:1005183100610. [DOI] [PubMed] [Google Scholar]
- 107.Jang Y, Borenstein AR, Chiriboga DA, Mortimer JA. Depressive symptoms among African American and White older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(6):P313. doi: 10.1093/geronb/60.6.p313. [DOI] [PubMed] [Google Scholar]
- 108.Kaplan L, Boss P. Depressive symptoms among spousal caregivers of institutionalized mates with Alzheimer’s: Boundary ambiguity and mastery as predictors. Family Process. 1999;38(1):85–103. doi: 10.1111/j.1545-5300.1999.00085.x. [DOI] [PubMed] [Google Scholar]
- 109.Anita FF, Ron EFD, Patrice G, Maria ML, Schneiderman N. Assessing the reliability and validity of the John Henry active coping scale in an urban sample of African Americans and white Americans. Ethnicity and Health. 2003;8(2):147–161. doi: 10.1080/13557850303563. [DOI] [PubMed] [Google Scholar]
- 110.Fernander A, Schumacher M. An examination of socio culturally specific stress and coping factors on smoking status among African American women. Stress and Health. 2008;24(5):365–374. [Google Scholar]
- 111.Radloff LS. The CES-D Scale: A Self Report Depression Scale for Research in the General. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 112.Conerly RC, Baker F, Dye J, Douglas CY, Zabora J. Measuring depression in African American cancer survivors: The reliability and validity of the Center for Epidemiologic StudyóDepression (CES-D) scale. Journal of health psychology. 2002;7(1):107. doi: 10.1177/1359105302007001658. [DOI] [PubMed] [Google Scholar]
- 113.Roberts RE. Reliability of the CES-D scale in different ethnic contexts* 1. Psychiatry Research. 1980;2(2):125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 114.Mansfield AK, Addis ME, Courtenay W. Measurement of Men’s Help Seeking: Development and Evaluation of the Barriers to Help Seeking Scale. Psychology of Men & Masculinity. 2005;6(2):95. [Google Scholar]
- 115.Watt MH, Ranby KW, Meade CS, et al. Posttraumatic stress disorder symptoms mediate the relationship between traumatic experiences and drinking behavior among women attending alcohol-serving venues in a South African township. Journal of studies on alcohol and drugs. 2012 Jul;73(4):549–558. doi: 10.15288/jsad.2012.73.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mansfield AK, Addis ME, Courtenay W. Measurement of Men’s Help Seeking: Development and Evaluation of the Barriers to Help Seeking Scale. Psychology of Men & Masculinity. 2005;6(2):95–108. [Google Scholar]
- 117.Meade AW, Bauer DJ. Power and precision in confirmatory factor analytic tests of measurement invariance. Structural Equation Modeling. 2007;14(4):611–635. [Google Scholar]
- 118.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling. 2002;9(2):233–255. [Google Scholar]
- 119.Vandenberg RJ, Lance CE. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational Research Methods. 2000;3(1):4–70. [Google Scholar]
- 120.Muthén L, Muthén BO. Mplus Statistical Analysis with latent variables-User’s guide. 5th. Los Angeles, CA: 1998–2007. [Google Scholar]
- 121.Millsap RE, Yun-Tein J. Assessing factorial invariance in ordered-categorical measures. Multivariate Behavioral Research. 2004;39(3):479–515. [Google Scholar]
- 122.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- 123.Chatterjee S. Regression Analysis by Example. 4th. New York: John Wiley & Sons; 2006. [Google Scholar]
- 124.Raver CC, Gershoff ET, Aber JL. Testing equivalence of mediating models of income, parenting, and school readiness for White, Black, and Hispanic children in a national sample. Child development. 2007;78(1):96–115. doi: 10.1111/j.1467-8624.2007.00987.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Byrne BM, Shavelson RJ, Muthén B. Testing for the equivalence of factor covariance and mean structures: The issue of partial measurement invariance. Psychological bulletin. 1989;105(3):456. [Google Scholar]
- 126.Finney SJ, DiStefano C. Non-normal and categorical data in structural equation modeling. Structural equation modeling: A second course. 2006:269–314. [Google Scholar]
- 127.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological methods. 2002;7(2):147. [PubMed] [Google Scholar]
- 128.Mahalik JR, Locke BD, Ludlow LH, et al. Development of the Conformity to Masculine Norms Inventory. Psychology of Men and Masculinity. 2003;4(1):3–25. [Google Scholar]
- 129.Hammond WP, Mohottige D, Chantala K, Hastings JF, Neighbors HW, Snowden L. Determinants of usual source of care disparities among African American and Caribbean Black men: findings from the National Survey of American Life. Journal of health care for the poor and underserved. 2011 Feb;22(1):157–175. doi: 10.1353/hpu.2011.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Williams DR, Mohammed SA. Racism and Health II: A Needed Research Agenda for Effective Interventions. American Behavioral Scientist. 2013 Aug;57(8):1200–1226. doi: 10.1177/0002764213487341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Broman CL, Mavaddat R, Hsu S-y. The experience and consequences of perceived racial discrimination: A study of African Americans. Journal of Black Psychology. 2000;26(2):165–180. [Google Scholar]
- 132.Brown TN, Williams DR, Jackson JS, et al. “Being black and feeling blue”: The mental health consequences of racial discrimination. Race and Society. 2000;2(2):117–131. [Google Scholar]
- 133.Fang CY, Myers HF. The effects of racial stressors and hostility on cardiovascular reactivity in African American and Caucasian men. Health Psychology. 2001;20(1):64. doi: 10.1037//0278-6133.20.1.64. [DOI] [PubMed] [Google Scholar]
- 134.Chae DH, Epel ES, Nuru-Jeter AM, et al. Discrimination, mental health, and leukocyte telomere length among African American men. Psychoneuroendocrinology. 2016;63:10–16. doi: 10.1016/j.psyneuen.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sellers RM, Shelton JN. The role of racial identity in perceived racial discrimination. Journal of Personality and Social Psychology. 2003;84(5):1079. doi: 10.1037/0022-3514.84.5.1079. [DOI] [PubMed] [Google Scholar]
- 136.U.S. Census Bureau. 2009. [Google Scholar]
- 137.U.S. Department of Labor. 2008. [Google Scholar]
- 138.Mansfield AK, Addis ME, Mahalik JR. “Why Won’t He Go to the Doctor?”: The Psychology of Men’s Help Seeking. International Journal of Men’s Health. 2003;2(2):93–109. [Google Scholar]
- 139.Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. Journal of general internal medicine. 2010:1–9. doi: 10.1007/s11606-010-1481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]