Abstract
Human immunodeficiency virus (HIV)–related pulmonary arterial hypertension has been found to be more prevalent in intravenous drug users. Our earlier cell-culture findings reported down-regulation of bone morphogenetic protein receptors (BMPRs) in combination with enhanced proliferation of human pulmonary arterial smooth muscle cells (PASMCs) in the presence of HIV–Trans-activator of transcription (Tat) and cocaine compared with either treatment alone. Here, we report physiologic evidence of significant increases in mean pulmonary arterial pressure in HIV-transgenic (Tg) rats intraperitoneally administered 40 mg/kg body weight cocaine (HIV-cocaine group) once daily for 21 days when compared with HIV-Tg rats given saline (HIV group) or wild-type (WT) Fischer 334 rats treated with (WT-cocaine group) and without cocaine (WT group). In addition, right ventricle systolic pressure was also found to be significantly higher in the HIV-cocaine rats compared with the WT group. Significant down-regulation in protein expression of BMPR-2 and BMPR-1B was observed in total lung extract from HIV-cocaine rats compared with the other three groups. Furthermore, the PASMCs isolated from HIV-cocaine rats demonstrated a higher level of proliferation and lower levels of apoptosis compared with cells isolated from other rat groups. Interestingly, corroborating our earlier cell-culture findings, we observed higher expression of BMPR-2 and BMPR-1B messenger RNA and significantly lower levels of BMPR-2 and BMPR-1B protein in HIV-cocaine PASMCs compared with cells isolated from all other groups. In conclusion, our findings support an additive effect of cocaine and HIV on smooth muscle dysfunction, resulting in enhanced pulmonary vascular remodeling with associated elevation of mean pulmonary arterial pressure and right ventricle systolic pressure in HIV-Tg rats exposed to cocaine.
Keywords: pulmonary hypertension, drug abuse, smooth muscle, bone morphogenetic protein receptor, human immunodeficiency virus-1
Clinical Relevance
We previously reported enhanced pulmonary vascular remodeling in the lungs of human immunodeficiency virus (HIV)–infected intravenous drug users, mainly cocaine abusers. Given that human samples are mostly confounded with various other risk factors, the current study, using a noninfectious HIV-transgenic rat model, demonstrates the direct effect of cocaine on pulmonary arteriopathy and HIV-related pulmonary arterial hypertension (PAH). These findings confirm that the HIV-infected intravenous drug use population is at greater risk for developing PAH, and the rat model may be used to understand the mechanisms and identify novel targets for future drug therapies.
Human immunodeficiency virus (HIV) infection continues to be a worldwide health concern. Modern treatment with antiretroviral therapy has improved the survival of patients in regard to infectious causes of death. However, other complications have surfaced with increased longevity, one of the most devastating being HIV-related (HR) pulmonary arterial hypertension (HRPAH) (1, 2). PAH from any cause is characterized by vascular remodeling (3) of pulmonary arteries that leads to an increase in mean pulmonary arterial pressure (mPAP) and pulmonary vascular resistance, followed by right ventricular failure and, ultimately, early mortality. Recent estimates indicate elevated systolic pulmonary artery pressure in 35% of patients with HIV by echocardiogram. This, however, is not the definitive diagnostic test, as any form of PAH requires a right-heart catheterization for diagnosis. When a confirmatory right-heart catheterization was performed, prevalence was found to be approximately 0.46% in the French registry (4, 5). Nevertheless, the burden of HRPAH in developing countries, such as those in Africa with approximately 23 million infected with HIV-1 and an estimated prevalence of HRPAH of 5% (6), could be overwhelming. Furthermore, a recent report by Quezada and colleagues (2) suggests a 10% prevalence of HRPAH in the cohort from Spain. No matter the route of infection, all patients with HIV have increased risk of developing pulmonary vascular dysfunction. However, it appears to be most common in those that have a history of intravenous drug abuse (intravenous drug users [IVDUs]), with as many as 59–70% of HRPAH cases arising from this group of patients (1, 2). To further confound the population, patients with HIV are also commonly coinfected with herpesvirus or hepatitis B/C virus. According to one report, human herpesvirus-8 is also related to PAH (7); however, no definitive relation of human herpesvirus-8 has been found in HIV-infected individuals with PAH (5). The presence of hepatitis C virus or other liver diseases is also common in IVDUs, and may lead to portopulmonary hypertension (another etiology of PAH) (8). Although neither our laboratory nor others observed significant relationships between Pneumocystis jirovecii pneumonia and pulmonary vascular remodeling in simian-immunodeficiency–infected macaques (9, 10), one report demonstrated development of pulmonary vasculopathy on Pneumocystis infection using a murine model (11).
Cocaine and other abused drugs have been shown to be an independent risk factor for the development of PAH (12). However, we have shown in previous work that HIV infection and intravenous drug use may work in concert to cause endothelial cell injury/dysfunction, as well as smooth cell proliferation/migration with subsequent vascular remodeling (10, 13, 14). This suggests a “multiple-hit” phenomenon. Our studies have shown down-regulation of tight junction proteins, resulting in endothelial injury and enhanced permeability with HIV-1 infection and/or cocaine use (13). Recently, we also demonstrated that cocaine and the HIV protein Trans-activator of transcription (Tat) decreased bone morphogenetic protein (BMP) receptor (BMPR) expression in human pulmonary arterial smooth muscle cells (PASMCs), leading to enhanced proliferation of pulmonary SMCs (15). Based on these previous results, we hypothesized that there would be an additive, in vivo effect of cocaine and HIV proteins on pulmonary vasculature remodeling and smooth muscle dysfunction.
To test our hypothesis, we used an NL4-3Δgag/pol HIV-transgenic (Tg) noninfectious rat model that is known to demonstrate clinical manifestations resembling those seen in HIV-1–infected patients, including pulmonary vascular remodeling (16, 17). Our laboratory and Lund and colleagues (17) previously reported pulmonary vascular remodeling and pulmonary hypertension, respectively, in this noninfectious HIV-Tg rat model. Here, we report significant augmentation in the mPAP and pulmonary arteriopathy accompanied by severe down-modulation of BMPR protein expression in 4- and 9-month-old HIV-Tg rats exposed to cocaine when compared with either HIV-Tg or wild-type (WT) rats injected with cocaine. This BMPR dysregulation was associated with a remarkable increase in the proliferation of rat pulmonary SMCs isolated from HIV-Tg rats exposed to cocaine, with a corresponding reduction in cell apoptosis.
Material and Methods
HIV-1–Tg and WT Rats
Male Fischer HIV-1 Tg rats containing a gag-pol deleted NL4-3 provirus that expresses HIV-1 proteins in lymphocytes and monocytes were purchased from ENVIGO (Indianapolis, IN). The 4- or 9-month-old rats (n = 5–7/group) were intraperitoneally administered 40 mg/kg body weight of cocaine (HIV-cocaine group) or saline (HIV group), once daily for 21 days. The cocaine dosage in rats was based on previous published results (18–20) as well as our preliminary findings, where we tested this dose for 7, 14, and 21 days. Age-matched WT F334 rats were also injected with either cocaine (WT-cocaine group) or saline (WT group) for comparison. The animals were housed at the University of Kansas Medical Center (Kansas City, KS) in strict accordance with the National Institutes of Health guidelines. See the online supplement for details on catheterization, hemodynamics, tissue harvesting, and isolation of rat arterial SMCs, as well as additional details on methodology.
Results
Cocaine Exacerbates the Increase in mPAP and Right Ventricular Systolic Pressure of HIV-Tg Rats
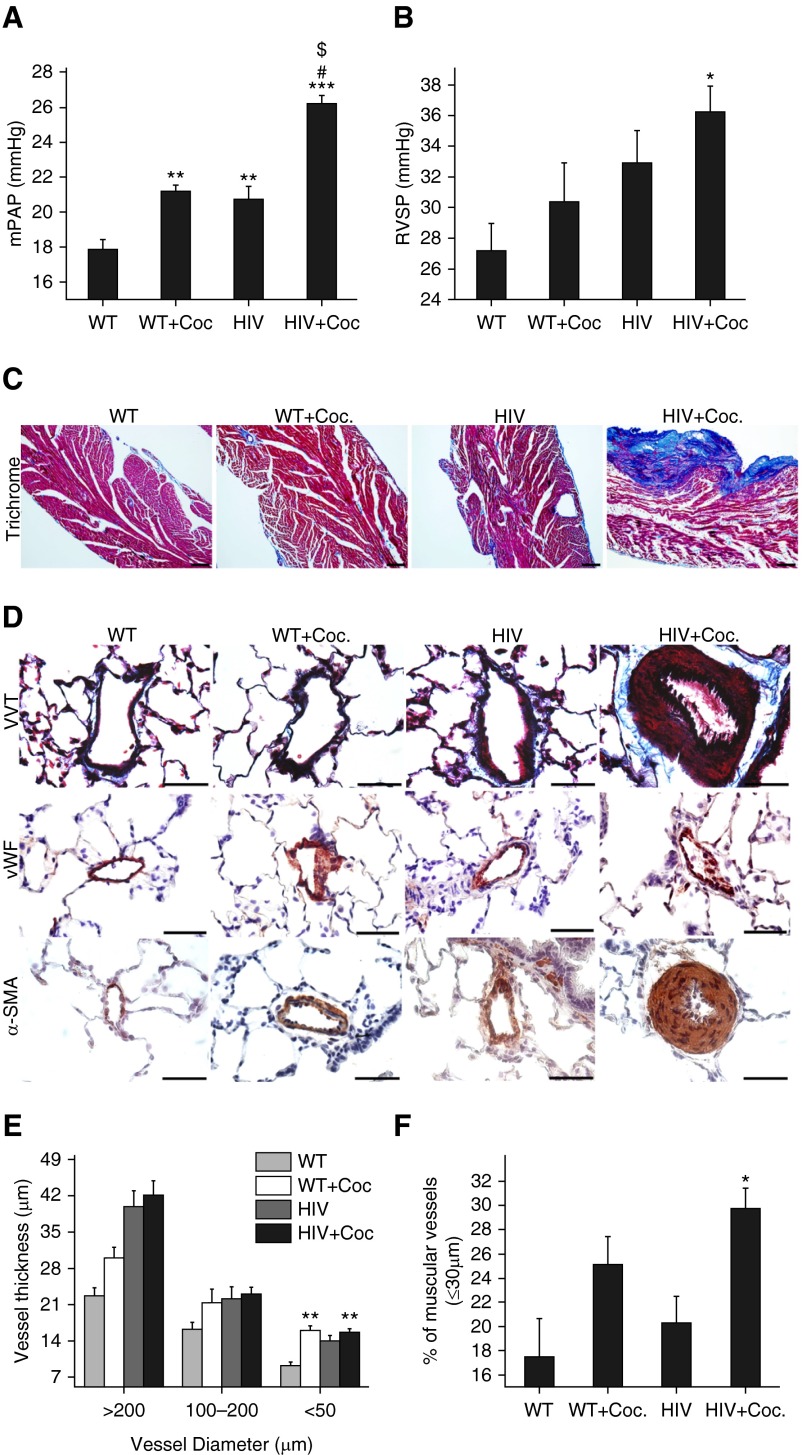
We compared hemodynamics measurements in 4- to 5-month-old HIV-Tg rats exposed to cocaine (HIV-cocaine group) or saline (HIV group) with age-matched WT rats with cocaine (WT-cocaine group) and without cocaine (WT group). As illustrated in Figure 1A, there was a significant increase in the mPAP in the arteries of WT-cocaine group rats compared with the WT group. Similarly, elevated mPAP was also observed in HIV group rats compared with the WT group. However, as expected, the highest increase in mPAP was seen in HIV-Tg rats exposed to cocaine. This increase was also significant when compared with the HIV or WT-cocaine groups. Furthermore, we used the right ventricular (RV) systolic pressure (RVSP) measurements to confirm the presence of PAH. On right-heart catheterization, we observed elevated RVSP in HIV with and without cocaine or WT-cocaine rats when compared with WT rats, although a significant increase in RVSP was only recorded in the HIV-cocaine group (Figure 1B).
Figure 1.
Hemodynamics and pulmonary arterial remodeling in 4-month-old human immunodeficiency virus (HIV)–transgenic (Tg) rats exposed to cocaine. The 4-month-old male Fischer HIV-Tg rats were administered 40 mg/kg body weight of cocaine (HIV + Coc. group) or saline (HIV group) daily for 21 days. Wild-type (WT) F334 rats with (WT + Coc. group) and without cocaine (WT group) were used for comparison. (A) Mean pulmonary arterial pressure (mPAP) and (B) right ventricle (RV) systolic pressure (RVSP) were measured after RV catheterization. Values are mean (±SEM) of n ≥ 6 per group. (C) Masson’s trichrome staining in snap-frozen, formaldehyde-fixed, paraffin-embedded heart sections. Scale bars: 100 μm. (D) Lungs were harvested, fixed, paraffin-embedded, and sectioned followed by staining for Verhoeff-Van trichrome (VVT), von Willebrand factor (vWF), and α-smooth muscle actin (α-SMA). Scale bars: 50 μm. (E) Thickening of vessels was assessed by measuring inner and outer diameter of various-sized vessels. Significant increase in the thickness of arteries with a diameter less than 50 μm was observed in the HIV + Coc. group. (F) α-SMA–positive vessels with an outer diameter less than 30 μm were counted per rat within each group (n = 5 rats/group) to determine the percentage of muscularization of intra-acinar vessels. *P < 0.05, **P < 0.01, and ***P < 0.001 versus WT, #P < 0.001 versus WT + Coc., $P < 0.001 versus HIV.
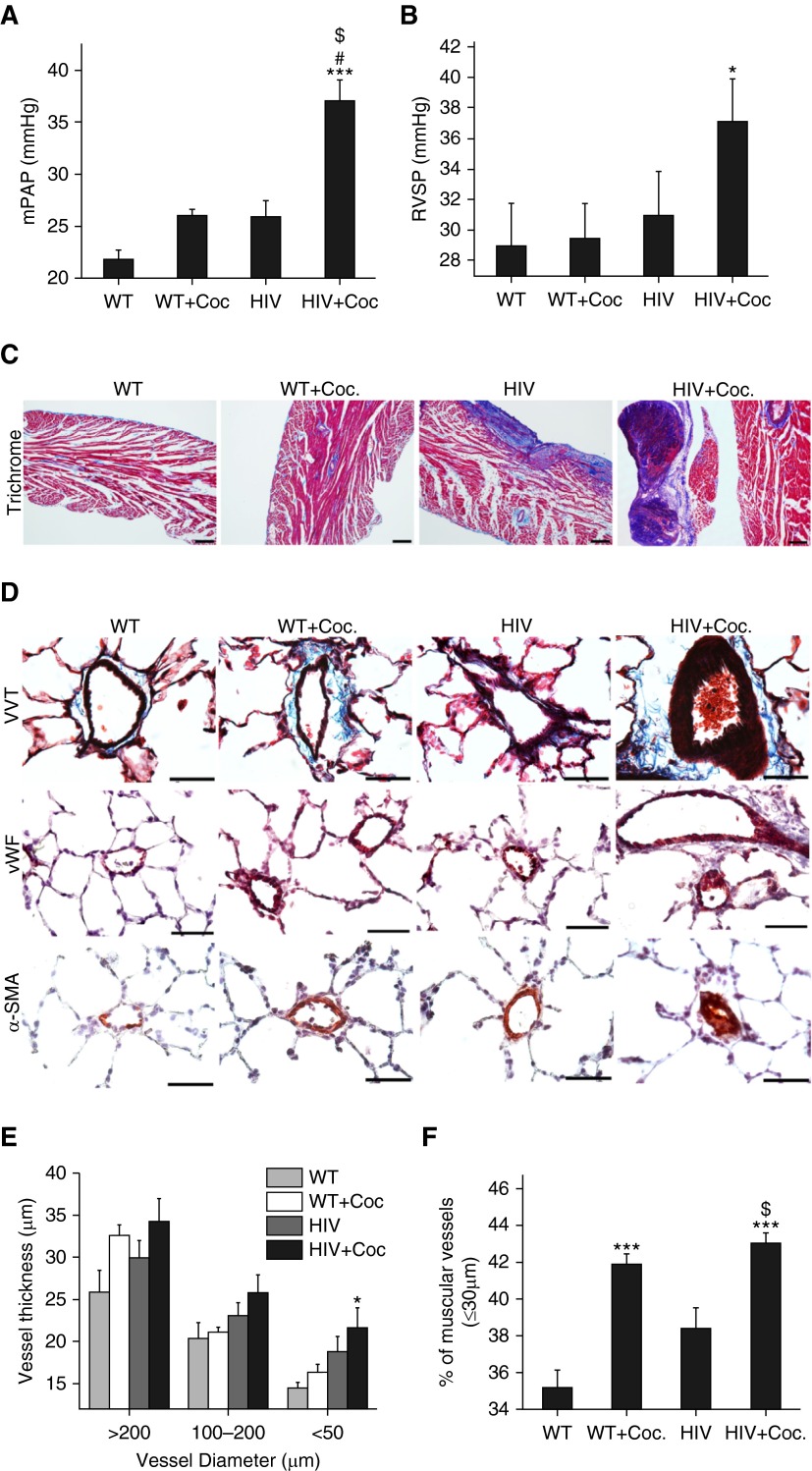
We also measured hemodynamics via right-heart catheterization in 9-month-old HIV-Tg rats in the same four groups (HIV-cocaine, HIV, WT-cocaine, and WT). mPAPs were significantly more elevated in the HIV-cocaine group than in any of the other three groups (Figure 2A). The WT-cocaine and the HIV group did have more elevated mPAP than the WT group, but not as significantly as the HIV-cocaine group. In addition, of note is that the average mPAP in the 9-month-old HIV-cocaine rats was more elevated than that in the 4- to 5-month-old group. As observed in the 4-month-old animals, there was a significant increase in the RVSP levels in the 9-month-old HIV-cocaine group compared with the WT group (Figure 2B). To investigate the RV response to these hemodynamic changes, we segregated half of the rats in each group for measurement of RV weight and half for cross-sectional analysis of RV thickness. As shown in Table E1 in the online supplement, we found an increase in RV weight/body weight on exposure of 9-month-old HIV-Tg rats to cocaine. However, this increase was not significant, as determined by multivariate analysis. Nevertheless, we observed a remarkable increase in the RV fibrosis among 4- and 9-month-old HIV-cocaine rats when compared with HIV or cocaine group rats, as indicated by the blue-colored Masson’s trichrome–stained collagen fibers shown in Figures 1C and 2C. Notably, there was a further increase in RV fibrosis in the 9-month-old HIV-cocaine rats compared with their 4-month-old counterparts. Fibrosis was also found to be higher in the 9-month-old HIV-Tg rats not treated with cocaine.
Figure 2.
Hemodynamic measurements and vascular remodeling in 9-month-old HIV-Tg rats in the presence or absence of cocaine. The 9-month-old HIV-Tg rats or WT F334 rats were administered cocaine or saline daily for 21 days, and (A) mPAP and (B) RVSP were measured. Values are mean (±SEM) of n = 5 per group. (C) Heart sections from the respective animals were stained with Masson’s trichrome. Scale bars: 100 μm. (D) Representative images from paraffin-embedded and sectioned lung tissues from each group, stained for VVT, vWF, and α-SMA. Scale bars: 50 μm. Morphometric analysis of the pulmonary vessels from HIV-Tg or WT rats treated or untreated with cocaine (E and F). *P < 0.05, ***P < 0.001 versus WT, #P < 0.001versus WT + Coc, $P < 0.001 versus HIV.
Enhanced Pulmonary Vascular Remodeling in HIV-Tg Rats Treated with Cocaine
As presented in Figure 1D, remarkable thickening in the arterial vessel wall was observed by Verhoeff-Van trichrome staining in HIV-cocaine group rats compared with the other three groups. Blebbing of endothelial cells was also observed in HIV-cocaine group rats. Remarkable thickening of the pulmonary arterial smooth muscle layer was observed in some of the larger vessels (between 50- and 100-μm diameter) in a 4-month-old HIV-cocaine animal, as shown in Figure 1D. We then measured the thickness of vessel diameters ranging from 200 to over 50 μm between the four groups. As seen in Figure 1E, there was an increase in vessel hypertrophy in the cocaine, HIV, and HIV-cocaine rats compared with the WT group in vessels ranging from 50- to 200-μm diameter. This difference was significant in vessels less than 50 μm in the cocaine and HIV-cocaine groups compared with the WT group in the 4-month-old animals. In the 9-month-old group, there appeared to be more smooth muscle hypertrophy and adventitial thickening in the HIV-cocaine group, as highlighted by Verhoeff-Van trichrome staining in Figure 2D. Focal proliferation of endothelial cells and presence of smooth muscle layer in intra-acinar vessels (Figure 2D) were more common in HIV-cocaine group rats compared with other groups. There was a significant increase in the thickness of vessels of 50 μm or less in diameter in the HIV-cocaine group, as seen in Figure 2E. Furthermore, the number of smooth muscle–positive vessels with less than 30 μm diameter was assessed using Aperio after scanning the α-smooth muscle actin (α-SMA)–stained tissue sections. The 4-month-old HIV or cocaine groups had higher number of these α-SMA–positive vessels compared with the WT group. However, the increase was greatest in the HIV-cocaine group, and was significantly higher compared with the WT group (Figure 1F). Interestingly, in the older animals aged 9 months, the cocaine group also demonstrated significantly higher α-SMA–positive vessels less than 30 μm in diameter (Figure 2F) compared with untreated WT rats. Similar to the 4-month-old rats, the maximum number of these small vessels was also in the 9-month-old HIV-cocaine group, which was significantly higher than that of WT or HIV groups. These results suggest that the combination of HIV-1 transgene expression and exposure to cocaine causes greater structural damage to the lung compared with HIV or cocaine alone.
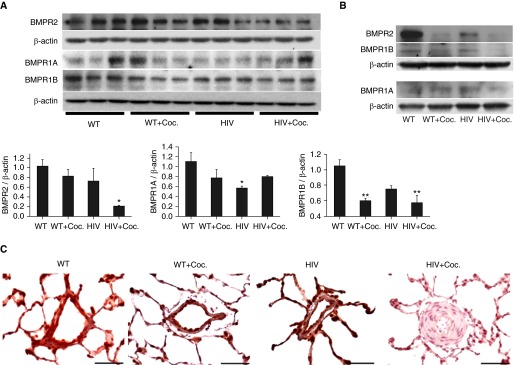
Significant Decrease in the Protein Expression of BMPRs in Lungs from Cocaine-Exposed HIV-Tg Rats
Similar to our earlier report (15), we identified significant reduction in BMPR2 and BMPR1B protein expression in the total lung extract from HIV-Tg rats exposed to cocaine compared with lung homogenates from WT rats. A trend toward decrease was also seen in BMPR1A expression in the HIV-cocaine group compared with WT controls. In contrast, neither HIV nor WT-cocaine group rats showed significant alterations in BMPR2 expression. However, HIV-group rats were found to have significantly lower BMPR1A protein expression, whereas the WT-cocaine group demonstrated significant decreases in BMPR1B levels when compared with WT rats (Figure 3A). In the case of 9-month-old rat lung tissues, we observed a complete knockdown of BMPR2 protein expression in three out of five animals in the HIV-cocaine group, as well as in the cocaine group, by Western blot analysis. However, BMPR2 expression in the lung tissue from two rats from the cocaine group was higher than the expression in two animals from the HIV-cocaine group. Hence, to avoid experimental bias in representation of Western blot images, we pooled the protein samples from all the groups and performed Western blot for BMPR. As seen in the blots in Figure 3B, the minimum BMPR2, BMPR1B, and BMPR1A expression was observed in the HIV-cocaine group compared with either group alone or WT rats. The decrease in BMPR2 protein expression in the HIV-cocaine group was also confirmed by immunohistochemistry. As seen in representative images (Figure 3C), a remarkably low staining intensity was observed in the 4-month-old rats from the HIV-cocaine group compared with lung sections from the age-matched WT group with abundant BMPR2 expression, as indicated by reddish brown coloration.
Figure 3.
Significant decrease in the protein expression of bone morphogenetic protein (BMP) receptors (BMPRs) in the lungs from cocaine-exposed HIV-Tg rats. (A) Total protein was extracted from rat lung tissues (n = 3 per group) from 4-month-old animals using RIPA buffer followed by Western blot for BMPR2, -1A, and -1B. The blot probed with BMPR1A was stripped and reprobed for BMPR1B antibody. The graphs represent the average densitometry of protein expression. Values are means (±SEM). *P < 0.05, **P < 0.01 versus WT. (B) Almost complete loss of BMPR2 expression was observed in the pooled samples from 9-month-old HIV + Coc. rats compared with WT (n = 5/group). (C) Representative images showing BMPR2 expression after immune-histochemical staining of paraffin-embedded rat lung sections. Absence or very low reddish-brown coloration was seen in the thickened smooth muscle layer of pulmonary arteries from the HIV + Coc. Group, as indicated. Scale bars: 50 μm.
Hyperproliferation of PASMCs Isolated from HIV-Tg Rats Exposed to Cocaine
Next, we determined the proliferation status of pulmonary SMCs isolated from rats with HIV with and without cocaine and WT rats with and without cocaine. The purity of isolated cells was confirmed by the positive α-SMA expression and negative von Willebrand factor staining (see Figure E1 in the online supplement). As illustrated in Figure 4A, the (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) cell proliferation assay revealed a significant increase in the proliferation of rat PASMCs (RPASMCs) isolated from HIV group rats when grown in full media. The same trend was observed in serum-starved cells, as shown in Figure 4B. The RPASMCs isolated from cocaine group rats also proliferated at a higher rate compared with controls on 2 days of serum starvation, with the difference becoming significantly higher after 4 days. However, the cells from the HIV-cocaine group rats showed maximum proliferation at all time points tested, both under serum-starved and regular medium conditions. The difference in the cell number from the HIV-cocaine group rats was also significant compared with either the cocaine or HIV groups. A qualitative representation of proliferating cells grown in 0.1% FBS is shown in Figure 4C by crystal violet staining. Here, the difference in cell number between all four groups is clearly apparent by visual comparison, with maximum proliferation seen in cells isolated from the HIV-cocaine group. These findings were further validated by Western blot of protein extract from non–serum-starved RPASMCs for the proliferating cell nuclear antigen (Figure 4D). As seen in the densitometry analysis, significantly higher proliferating cell nuclear antigen expression was observed in HIV-cocaine rats compared with the WT group.
Figure 4.
Hyperproliferation of pulmonary arterial smooth muscle cells (PASMCs) isolated from HIV-Tg rats exposed to cocaine. Rat PASMCs (RPASMCs; 3 × 103) from WT, WT-cocaine, HIV, and HIV-cocaine group rats (passage 3) were plated on 96-well plates. After 48 hours of plating, cells were made quiescent by adding 0.1% FBS containing rat smooth muscle cell medium (RSMCM) for 48 hours, followed by the addition of either (A) complete RSMCM or (B) 0.1% FBS containing RSMCM. (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) cell proliferation assay was later performed after 2, 4, and 6 days. Values are means (±SD) of n = 3 rats/group. *P < 0.05, **P < 0.001 versus WT, #P < 0.001 versus WT+Coc., $P < 0.001 versus HIV. (C) Representative images of crystal violet–stained RPASMCs isolated from various groups are shown. Cells were grown in 0.1% serum containing RSMCM. Magnification, 4×. (D) RPASMCs (passage 3) grown in complete medium were lysed with RIPA buffer followed by protein extraction and Western blot for proliferating cell nuclear antigen (PCNA). Graph represents average densitometry for three rats per group. Values are means (±SEM). *P < 0.05 versus WT.
Development of Apoptosis Resistance in PASMCs Isolated from HIV-Tg Rats Exposed to Cocaine
As expected, cell death ELISA revealed a downward trend of apoptosis in RPASMCs from cocaine, HIV, and HIV-cocaine groups compared with that of WT cells grown in complete (Figure 5A) as well as serum-deprived (Figure 5B) rat smooth muscle cell medium. Although there was significantly lower apoptosis in RPASMCs from HIV group rats, an even lower rate of apoptosis was seen in the HIV-cocaine group compared with the other three groups. This could indicate the development of apoptosis resistance, considering the higher level of proliferation shown in Figure 4. We further confirmed the ELISA results by staining these cells for apoptosis marker, annexin V. As shown in Figure 5C, the maximum number of annexin V–positive cells per field were observed in the WT group compared with the cocaine group, relatively few in the HIV group, and negligible in the HIV-cocaine group–derived RPASMCs. Similarly, Western blot for cleaved poly ADP ribose polymerase (PARP) showed the least protein expression in the RPASMCs from the HIV-cocaine group compared with only cocaine or HIV, which was significantly lower compared with RPASMCs isolated from WT and WT-cocaine group rats (Figure 5D).
Figure 5.
Development of apoptosis resistance in pulmonary SMCs isolated from HIV-Tg rats exposed to cocaine. RPASMCs (1.2 × 104) from three rats per group were plated on 96-well plates followed by changing medium the next day to (A) complete RSMCM or (B) 0.1% FBS containing RSMCM. Apoptosis was measured after 24 hours by oligonucleosome ELISA. Values are means (±SD) of n = 3 rats/group. (C) RPASMCs were grown to 80% confluency on coverslips in 24-well plates followed by Alexa Fluor 488 annexin V binding on live cells and mounting with 4′,6-diamidino-2-phenylindole. Representative fluorescence images were captured at 40×. Scale bars: 50 μm. (D) The blot of RPASMC protein lysate used for probing PCNA was re-probed for cleaved poly ADP ribose polymerase (c-PARP) expression. Graph represents average densitometry for c-PARP expression from three rats per group. Values are means (±SEM). *P < 0.05, **P < 0.01, ***P < 0.001 versus WT, #P < 0.05, ##P < 0.001 versus WT + Coc.
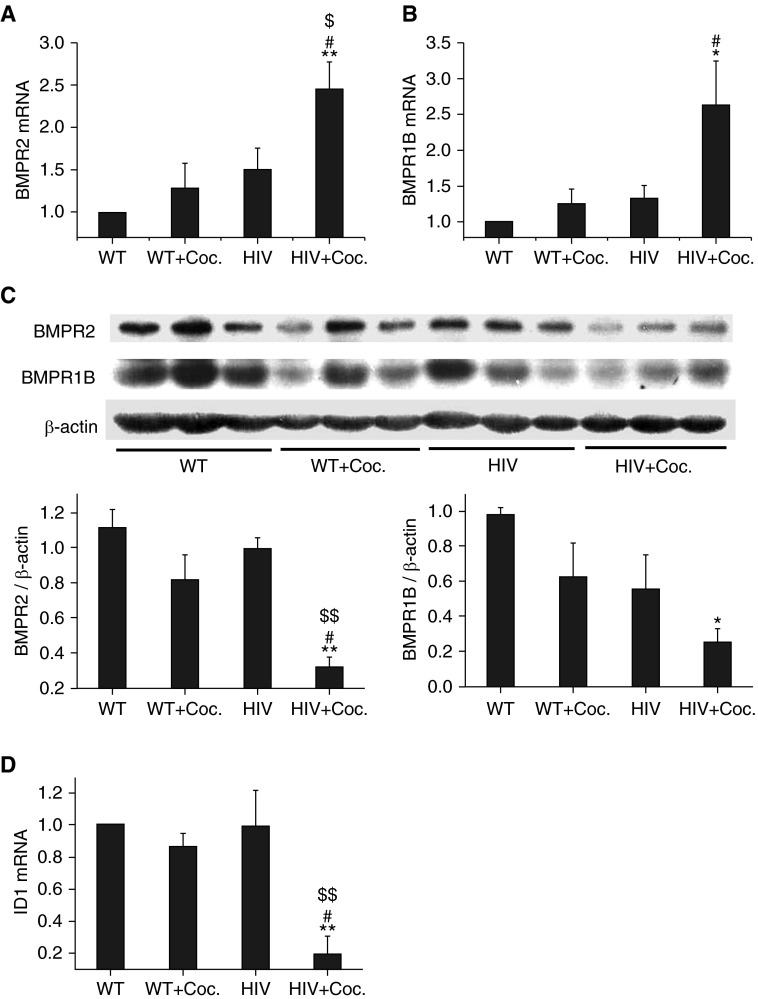
Down-Regulation of BMP Signaling in Pulmonary SMCs Isolated from Cocaine-Treated HIV-Tg Rats
Consistent with our earlier report (15), we found significantly increased mRNA expression of BMPR2 and BMPR1B (Figures 6A and 6B) in RPASMCs from HIV-cocaine rats compared with the WT group. The increase in BMPR2 mRNA in cells from HIV-cocaine rats was also significant compared with either the cocaine or HIV groups. However, as observed in the total lung extract from HIV-cocaine rats, a significant reduction in the protein expression of BMPR2 and BMPR1B was found in RPASMCs from HIV-cocaine rats compared with WT rats (Figure 6C). This reduced BMPR expression in cells from HIV-cocaine rats also correlated with a significant decrease in the mRNA expression of the downstream target gene, ID1 (Figure 6D).
Figure 6.
Down-regulation of BMPR signaling in pulmonary SMCs isolated from cocaine-injected HIV-Tg rats. Total RNA was extracted from RPASMCs using Trizol reagent, followed by quantitative RT-PCR using predesigned primers for (A) BMPR2, (B) BMPR1B, (D) and ID1 from Integrated DNA Technologies (Coralville, Iowa). (C) Protein extracted from RPASMCs was analyzed for BMPR2 and BMPR1B (n = 3 per group) protein expression by Western blot. Graphs represent average densitometry. *P < 0.05, **P < 0.01 versus WT, #P < 0.05 versus WT + Coc., $P < 0.05, $$P < 0.01 versus HIV.
Viral Protein Staining in the Lung Sections from Fischer and Sprague-Dawley Strains of HIV-Tg Rats
As the objective of the study was to characterize the effect of HIV proteins on the pulmonary vasculature, we further evaluated the presence of HIV-Tat and negative regulatory factor (Nef) proteins in the paraffin-embedded lung sections. Notably, the HIV-cocaine group showed a remarkable presence of Nef protein in the endothelial lining of remodeled vessels, as indicated by the dark brown coloration seen in Figure 7A, with negligible positivity for Nef in SMCs. The presence of Nef staining was also observed in the mononuclear cells surrounding the vessels in the HIV-cocaine group (Figure 7A) and the HIV group (Figure 7B), as well as in the epithelial cells. However, we did not observe significant perivascular inflammation in the Fischer strain of HIV-Tg rats, as we saw in our earlier published findings on Sprague-Dawley (SD) HIV-Tg rats (16). We reported significant pulmonary artery medial hypertrophy with RV hypertrophy in the SD strain of HIV-Tg rats, even in the absence of cocaine (16). Here, when we stained paraffin-embedded lung sections from the same SD HIV-Tg rats, we observed intense positivity for Nef protein in the remarkably increased number of inflammatory cells surrounding the remodeled vessels (Figures 7D and 7E). Similar to the Fischer strain, endothelial cells were also found to be positive for Nef, but not SMCs, in SD rats. Importantly, SD HIV rats had notably more vascular remodeling when compared with the Fischer strain in the absence of cocaine. The staining for Tat protein showed a similar pattern as Nef staining in the Fischer as well as SD HIV-Tg rats, with high Tat expression in the inflammatory cells surrounding the remodeled vessels in the SD strain (Figures 7J and 7K). In addition, mild Tat expression was also seen in the arterial SMCs (Figures 7G, 7H, 7J, and 7K), but this could have been a false positive, as one of the Fischer WT rats also showed some background staining (Figure E2). Overall the WT strains of both Fischer and SD rats were negative for HIV proteins (Figures 7C, 7F, 7I, and 7L). In addition, we noted that SD WT rats had increased cellularity to begin with, and relatively slightly more thickened vessels in certain areas when compared with Fischer WT rats.
Figure 7.
Presence of HIV-Negative regulatory factor (Nef) and -Transactivator of transcription (Tat) proteins in the lungs from HIV-Tg rats. Paraffin-embedded lung sections from Fischer HIV-Tg rats (A–C and G–I) and Sparague-Dawley (SD) HIV-Tg rats (D–F and J–L) were immunostained for HIV proteins, Nef and Tat. The WT Fischer (C and I) or SD (F and L) rats did not show positivity for either of the HIV proteins, whereas the HIV-Tg (B and H) and HIV + Coc. (A and G) Fischer rats were positive for Nef (A and B) and Tat (G and H). There were notably elevated numbers of inflammatory cells in the HIV-Tg SD rat lungs with intense positivity for Nef (D and E) and Tat (J and K). Scale bars: 50 μm.
Discussion
In this study, we took a multifaceted approach to support the additive effect of cocaine and HIV infection on pulmonary vascular remodeling using a noninfectious HIV-Tg rat model. From a hemodynamic standpoint, the mPAP and RVSP were significantly elevated in the group exposed to both cocaine and HIV. This was evident in both the 4- and 9-month-old groups. Histologically, significantly increased SMC hypertrophy was evident in both the 4- and 9-month-old groups. There was a significant decrease in BMP expression and down-regulation of BMP signaling in the HIV-cocaine group. In addition, there appeared to be development of hyperproliferation of pulmonary SMCs along with development of apoptosis resistance in the HIV-cocaine group.
Although not all HRPAH is due to intravenous drug abuse, it appears to be one of the major risk factors for the development of the disease (1, 2). Cocaine and other stimulants have also been implicated in the development of PAH without HIV infection (12). We have previously reported enhanced pulmonary vascular remodeling in HIV-infected lung tissues from intravenous heroin and cocaine abusers (14). Simian immunodeficiency virus–infected macaques exposed to morphine developed a severe pulmonary arteriopathy, including the presence of plexiform lesions similar to those found in humans with PAH (10). In addition, we demonstrated that cocaine synergizes with HIV-Tat to promote proliferation in PASMCs (15). The findings we present in this current report further support our previous results showing additive effect of abused drugs and HIV infection on pulmonary vascular dysfunction.
The pathophysiology of the development of HRPAH remains unclear at this time, in part due to limited options in regard to an animal model. Several studies have demonstrated that pulmonary vasculature cells are not directly infectable, and HIV proteins released by the infected lymphocytes and macrophages play a major role in the development of HRPAH (21). Apart from one report suggesting HIV-infection of arterial SMCs with low levels of viral replication in vitro (22), no evidence of the virus or viral DNA in pulmonary endothelial cells or SMCs has been reported (23, 24). HIV proteins, such as Tat, Nef, and envelope glycoprotein-120 (gp120), alone can lead to the development of pulmonary arteriopathy with the ability to directly act on the endothelium/smooth muscle and alter cellular function (25, 26). HIV-envelope gp120, for example, has been shown to directly activate SMCs via the presence of CD4 cells and mitogen-activated protein kinase pathways, leading to enhanced atherosclerosis and arteriogenesis (27). gp120 also appears to have the ability to induce apoptosis in endothelial cells, even in the absence of infection (28). HIV-Tat can act as an angiogenic and oncogenic factor by promoting growth, migration, and production of growth factors in various cell types (29, 30). In our previous findings, we have shown that cocaine synergizes with Tat to promote proliferation of PASMCs (31) through activation of platelet-derived growth factor signaling. It can also induce apoptosis of microvascular endothelial cells via caspase activation (25). In earlier studies, HIV-1–Tg rat lungs have been observed to be under significant oxidative stress, as signified by enhanced expression of hypoxia-inducible factor-1α (16). It is plausible that HIV proteins in conjunction with a second exposure to drugs of abuse enhance these mechanisms, inciting increased oxidative stress, dysregulation of growth factors, and inflammation, resulting in pulmonary arteriopathy.
Using a SD noninfectious HIV-Tg rat model, we previously reported development of pulmonary vascular remodeling in the presence of HIV-1 proteins without an active infection (16). In the present study, we used Fischer HIV-1–Tg rats containing a gag-pol NL4-3 nonreplicative provirus, just like SD rats that express seven of the nine HIV genes throughout the lymphoreticular system, including functional tat and env. This HIV-Tg rat model was developed by Reid and colleagues (32) and has been proven to be an effective tool for investigating pathologies associated with HIV disease, including age-associated alterations in the immune response, T cell abnormalities (33), kidney failure (34), and neuronal changes (32). It was created by microinjecting a noninfectious proviral plasmid into fertilized single-cell SD × Fisher344/NHsd F1 eggs (32). The integration of microinjected plasmid is expected to occur at a single-cell stage, because foreign DNA is present in every cell of the Tg animal, including germ cells (35). This notion has also been supported by various investigators where the expression of viral proteins is shown in various HIV-Tg rat tissues, including the lymph nodes, thymus, liver, lung, kidney, spleen, blood, epidermis, and brain (32, 36, 37). Furthermore, levels of viral protein gp120 in the lung lavage fluid of HIV-Tg female rats were not significantly different from those of HIV-Tg male rats (37). In addition, in our earlier report, we used both female and male SD HIV-Tg rats, and did not find sex-dependent changes in pulmonary vessels or right ventricle (16). The HIV-Tg rat model also appears to be superior to mouse models, as HIV-Tg mice replicate only some of the human pathologies of HIV infection, as the viral promoter does not function normally in mice (38).
Several studies have demonstrated lung parenchymal, hemodynamic, and right ventricular changes in this HIV-Tg rat model as well. Lund and colleagues were among the first to report significantly elevated RVSP as well as RV hypertrophy in 3 and 9 months aged Fischer HIV-Tg rats compared with age-matched controls. In our previous report showing increased smooth muscle remodeling in SD strain of these 4–5 months old HIV-Tg rats, we also demonstrated significantly more RV hypertrophy compared with WT rats using the Fulton index:Right ventricle/left ventricle+septum (RV/LV+S) ratio. However, in this study, using Fischer HIV-Tg rats, we have demonstrated an elevated mPAP and RVSP, as well as increased SMC proliferation in the HIV-Tg rats only after exposure to cocaine in both the 4- and 9-month-old groups. Interestingly, the HIV-Tg rats did not show evidence of pulmonary hypertension in the absence of cocaine. This is in contrast to what we reported earlier in SD HIV-Tg rats and by Lund and colleagues (16, 17). Strain-specific differences in pulmonary vascular remodeling have been reported earlier (39). It may be that the Fischer344 strain is more resistant to pulmonary vascular remodeling, as shown by He and colleagues (39), when compared with SD rats. In addition, studies by Lund and colleagues (17) were conducted at high altitude, which may have led to hypoxic challenge. Studies by Porter and colleagues (40) also demonstrated resistance of Fischer344 to vascular injury while investigating the effect of HIV-1 proteins on pulmonary vascular remodeling in the presence of hypoxia. Similar to our present study, they reported no significant changes in HIV-Tg rats when compared with WT rats; however, increased RVSP, RV hypertrophy, and pulmonary artery smooth muscle thickness was observed on exposure to hypoxia.
Comparison of histological findings in this study suggests remarkably more pulmonary vasculopathy in SD HIV-Tg rats than in Fischer HIV-Tg rats. Furthermore, we observed enormous perivascular inflammation in SD HIV-Tg rats when compared with cocaine-treated or untreated Fischer HIV-Tg rats, and this corresponded with significantly more vascular remodeling in SD rats. In addition, these inflammatory cells were abundantly positive for HIV proteins, as shown by Nef and Tat staining, whereas negligible positivity was observed in SMCs within the remodeled vessels. Nevertheless, it is notable that Tinkle and colleagues (41), although using a different HIV-Tg mouse model, describe a vasculopathy induced by the expression of HIV-1 mRNA in vascular SMCs and the recruitment of inflammatory cells in adventitia. In addition, we report the presence of Nef and Tat proteins in the pulmonary endothelium of both Fischer and SD HIV-Tg rats. Previous studies based on PAH animal models suggest that endothelial injury is the first step in the development of pulmonary arteriopathy, and, upon activation, elicits responses on SMCs leading to the muscularization of vessels (42). Presence of Nef-positive endothelial cells in the remodeled pulmonary vessels in the lungs of simian-HIV-infected macaques has been reported previously by Marecki and colleagues (24). These findings suggest that the perivascular inflammation is associated with more medial hypertrophy in HIV-Tg rats, and underscore the importance of communication between inflammatory cells, endothelial cells, and SMCs during pulmonary arteriopathy.
The lack of significant differences in the Fulton index among Fischer HIV-Tg rats in the presence or absence of cocaine when compared with WT rats may, in part, be due to total weight differences, especially in the 9-month-old group. The HIV-Tg rats exposed to cocaine had significantly less weight gain than the other groups. The HIV-cocaine group mean weight was 311 g versus 417 g for the cocaine group, 404.6 g for the WT group, and 327 g for the HIV group. The exposure of both HIV proteins and cocaine may have caused the HIV-cocaine group to gain less weight over time. We did find an increase in the ratio of RV weight:total body weight in HIV-Tg rats on cocaine exposure, but, likely due to a small sample size, no significant difference was observed. However, increase in RV size was supported by increase in RV fibrosis in these rats on cocaine exposure. Hematocrit was also obtained on all animals, and there was no significant difference. Hematocrit is expected to rise in animals and humans exposed to hypoxia; however, our rats were only exposed to normoxic conditions, and the altitude of our current laboratory is only 265 m above sea level.
Furthermore, as in our previous study using SD HIV-Tg rats (10), pulmonary arteriopathy was associated with medial hypertrophy, smooth muscle hyperproliferation, and some endothelial injury, as seen by blebbing and proliferation of cells in some small vessels, but we did not find significant angio-obliteration or presence of plexiform lesions. Plexiform lesions are the hallmark end-stage lesions found in severe PAH (43). However, in the most frequently studied animal models, including chronic hypoxic and monocrotaline-injected rats, plexiform lesions are rarely found (44). Only recently has a potential rodent model been tested that was subjected to hypoxia/normoxia and injected with the vascular endothelial receptor blocker, semaxinib. Abe and colleagues (45) did find that these animals developed plexiform lesions that appeared similar to those found in human subjects. Lack of advanced-stage plexiform lesions in our HIV-Tg rat model also may be due to the age of the animals; it may be that these lesions develop later than 9 months.
BMPR dysfunction has been found to be one of the key factors in familial and idiopathic PAH (IPAH) (46). BMPs, on binding to heteromeric complexes of BMPR1A or BMPR1B with BMPR2, negatively regulate SMC growth and proliferation (46, 47). Reduction in the BMPR expression has been reported in monocrotaline and hypoxia-induced animal models of PAH (48, 49). Although BMPR2 has been most extensively reported to be mutated in familial and IPAH, there are specific reports on the loss of BMPR1A or BMPR1B causing attenuated SMC hyperproliferation in patients with IPAH (50, 51) as well. In our recent article, we reported a paradoxical decrease in the protein expression of BMPR1A, BMPR1B, and BMPR2 in spite of significant increases in their mRNA expression on exposure of HPASMCs to both Tat and cocaine. These in vitro findings were further corroborated by ex vivo findings demonstrating significant increases in mRNA, but decreases in protein expression of BMPRs in human lung tissues from IVDUs with HIV showing enhanced vascular remodeling compared with lungs from HIV-infected non–drug abusers or uninfected IVDUs (15). Likewise, here, we report significant down-regulation in the protein expression of BMPRs with higher expression of BMPR mRNA in RPASMCs isolated from the HIV-cocaine group compared with cells isolated from all other groups, further suggesting the involvement of post-transcriptional regulation of BMPR2 expression. There have been similar reports of discrepancies in mRNA and corresponding protein expression (52, 53). This may be due to a negative feedback loop generated on enhanced BMPR mRNA expression, triggering an exacerbated expression of microRNAs that may inhibit the translation of BMPRs (54). We are currently focusing on the post-transcriptional regulation of BMPRs, and some of our preliminary findings are published in the form of an abstract (55). Another possible mechanism could be direct tagging of BMPR proteins for ubiquitin-mediated degradation (56).
Finally, although the HIV-Tg rat is likely one of the better small animal models to explore the link between HIV and the development of pulmonary arteriopathy, it is not a replica of true HIV infection in patients, and results may not be completely extrapolated to humans. Also of note is that the RV/LV + S ratio, which has been widely used in similar studies, was not significantly increased in our present study. However, we were able to provide hemodynamics data, including mPAP, which is the definitive diagnostic test in the human population. In addition, it is difficult to compare the amount of cocaine given to rats in a controlled laboratory setting versus people who usually consume in “binge” settings, often in combination with other illicit drugs. This is certainly another limitation of the study; however, a controlled laboratory investigation with an animal model is important to understand the direct effects of cocaine on HIV-associated cardiopulmonary dysfunction.
In summary, we demonstrate evidence of the potentiation of pulmonary vascular remodeling, hemodynamic changes, and development of significant pulmonary arteriopathy in a HIV-Tg rat model exposed to cocaine. Mechanistically, we also provide evidence that these changes were due, in part, to the development of apoptosis resistance as well as down-regulation of BMP signaling in the PASMCs.
Supplementary Material
Footnotes
This work was supported by National Institutes of Health grants R01DAO34542, R56 HL129875, and R03DAO31589, and American Heart Association’s Scientist Development grant 11SDG7500016 (N.K.D.).
Author Contributions: P.D., L.S., A.O’B.-L., and N.K.D. drafted the manuscript for important intellectual content; P.D., J.A., V.G.G., H.S., M.G., and J.M.d.O. performed the experiments; P.D. and N.K.D. analyzed and interpreted the data; N.K.D. designed the study and supervised overall experimental plan.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1165/rcmb.2015-0264OC on January 28, 2016
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Opravil M, Sereni D. Natural history of HIV-associated pulmonary arterial hypertension: trends in the HAART era. AIDS. 2008;22:S35–S40. doi: 10.1097/01.aids.0000327514.60879.47. [DOI] [PubMed] [Google Scholar]
- 2.Quezada M, Martin-Carbonero L, Soriano V, Vispo E, Valencia E, Moreno V, de Isla LP, Lennie V, Almería C, Zamorano JL. Prevalence and risk factors associated with pulmonary hypertension in HIV-infected patients on regular follow-up. AIDS. 2012;26:1387–1392. doi: 10.1097/QAD.0b013e328354f5a1. [DOI] [PubMed] [Google Scholar]
- 3.Michelakis ED, Wilkins MR, Rabinovitch M. Emerging concepts and translational priorities in pulmonary arterial hypertension. Circulation. 2008;118:1486–1495. doi: 10.1161/CIRCULATIONAHA.106.673988. [DOI] [PubMed] [Google Scholar]
- 4.Reinsch N, Buhr C, Krings P, Kaelsch H, Kahlert P, Konorza T, Neumann T, Erbel R Competence Network of Heart Failure. Effect of gender and highly active antiretroviral therapy on HIV-related pulmonary arterial hypertension: results of the HIV-HEART Study. HIV Med. 2008;9:550–556. doi: 10.1111/j.1468-1293.2008.00602.x. [DOI] [PubMed] [Google Scholar]
- 5.Hsue PY, Deeks SG, Farah HH, Palav S, Ahmed SY, Schnell A, Ellman AB, Huang L, Dollard SC, Martin JN. Role of HIV and human herpesvirus-8 infection in pulmonary arterial hypertension. AIDS. 2008;22:825–833. doi: 10.1097/QAD.0b013e3282f7cd42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niakara A, Drabo YJ, Kambire Y, Nebie LV, Kabore NJ, Simon F. Cardiovascular diseases and HIV infection: study of 79 cases at the National Hospital of Ouagadougou (Burkina Faso) [article in French] Bull Soc Pathol Exot. 2002;95:23–26. [PubMed] [Google Scholar]
- 7.Cool CD, Rai PR, Yeager ME, Hernandez-Saavedra D, Serls AE, Bull TM, Geraci MW, Brown KK, Routes JM, Tuder RM, et al. Expression of human herpesvirus 8 in primary pulmonary hypertension. N Engl J Med. 2003;349:1113–1122. doi: 10.1056/NEJMoa035115. [DOI] [PubMed] [Google Scholar]
- 8.Kawut SM, Krowka MJ, Trotter JF, Roberts KE, Benza RL, Badesch DB, Taichman DB, Horn EM, Zacks S, Kaplowitz N, et al. Pulmonary Vascular Complications of Liver Disease Study Group. Clinical risk factors for portopulmonary hypertension. Hepatology. 2008;48:196–203. doi: 10.1002/hep.22275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.George MP, Brower A, Kling H, Shipley T, Kristoff J, Reinhart TA, Murphey-Corb M, Gladwin MT, Champion HC, Morris A, et al. Pulmonary vascular lesions are common in SIV- and SHIV-env–infected macaques. AIDS Res Hum Retroviruses. 2011;27:103–111. doi: 10.1089/aid.2009.0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spikes L, Dalvi P, Tawfik O, Gu H, Voelkel NF, Cheney P, O’Brien-Ladner A, Dhillon NK. Enhanced pulmonary arteriopathy in simian immunodeficiency virus–infected macaques exposed to morphine. Am J Respir Crit Care Med. 2012;185:1235–1243. doi: 10.1164/rccm.201110-1909OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Swain SD, Han S, Harmsen A, Shampeny K, Harmsen AG. Pulmonary hypertension can be a sequela of prior Pneumocystis pneumonia. Am J Pathol. 2007;171:790–799. doi: 10.2353/ajpath.2007.070178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collazos J, Martínez E, Fernández A, Mayo J. Acute, reversible pulmonary hypertension associated with cocaine use. Respir Med. 1996;90:171–174. doi: 10.1016/s0954-6111(96)90160-2. [DOI] [PubMed] [Google Scholar]
- 13.Dhillon NK, Peng F, Bokhari S, Callen S, Shin SH, Zhu X, Kim KJ, Buch SJ. Cocaine-mediated alteration in tight junction protein expression and modulation of CCL2/CCR2 axis across the blood–brain barrier: implications for HIV-dementia. J Neuroimmune Pharmacol. 2008;3:52–56. doi: 10.1007/s11481-007-9091-1. [DOI] [PubMed] [Google Scholar]
- 14.Dhillon NK, Li F, Xue B, Tawfik O, Morgello S, Buch S, Ladner AO. Effect of cocaine on human immunodeficiency virus–mediated pulmonary endothelial and smooth muscle dysfunction. Am J Respir Cell Mol Biol. 2011;45:40–52. doi: 10.1165/rcmb.2010-0097OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dalvi P, O’Brien-Ladner A, Dhillon NK. Downregulation of bone morphogenetic protein receptor axis during HIV-1 and cocaine-mediated pulmonary smooth muscle hyperplasia: implications for HIV-related pulmonary arterial hypertension. Arterioscler Thromb Vasc Biol. 2013;33:2585–2595. doi: 10.1161/ATVBAHA.113.302054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mermis J, Gu H, Xue B, Li F, Tawfik O, Buch S, Bartolome S, O’Brien-Ladner A, Dhillon NK. Hypoxia-inducible factor-1 α/platelet derived growth factor axis in HIV-associated pulmonary vascular remodeling. Respir Res. 2011;12:103. doi: 10.1186/1465-9921-12-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lund AK, Lucero J, Herbert L, Liu Y, Naik JS. Human immunodeficiency virus transgenic rats exhibit pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2011;301:L315–L326. doi: 10.1152/ajplung.00045.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elmer GI, Brockington A, Gorelick DA, Carrol FI, Rice KC, Matecka D, Goldberg SR, Rothman RB. Cocaine cross-sensitization to dopamine uptake inhibitors: unique effects of GBR12909. Pharmacol Biochem Behav. 1996;53:911–918. doi: 10.1016/0091-3057(95)02143-4. [DOI] [PubMed] [Google Scholar]
- 19.Fontana D, Post RM, Weiss SR, Pert A. The role of D1 and D2 dopamine receptors in the acquisition and expression of cocaine-induced conditioned increases in locomotor behavior. Behav Pharmacol. 1993;4:375–387. [PubMed] [Google Scholar]
- 20.York JL, MacKinnon K. Acute and chronic alcohol–cocaine interactions in rats. Alcohol. 1999;17:13–18. doi: 10.1016/s0741-8329(98)00027-5. [DOI] [PubMed] [Google Scholar]
- 21.Voelkel NF, Tuder RM. Cellular and molecular mechanisms in the pathogenesis of severe pulmonary hypertension. Eur Respir J. 1995;8:2129–2138. doi: 10.1183/09031936.95.08122129. [DOI] [PubMed] [Google Scholar]
- 22.Eugenin EA, Morgello S, Klotman ME, Mosoian A, Lento PA, Berman JW, Schecter AD. Human immunodeficiency virus (HIV) infects human arterial smooth muscle cells in vivo and in vitro: implications for the pathogenesis of HIV-mediated vascular disease. Am J Pathol. 2008;172:1100–1111. doi: 10.2353/ajpath.2008.070457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chalifoux LV, Simon MA, Pauley DR, MacKey JJ, Wyand MS, Ringler DJ. Arteriopathy in macaques infected with simian immunodeficiency virus. Lab Invest. 1992;67:338–349. [PubMed] [Google Scholar]
- 24.Marecki JC, Cool CD, Parr JE, Beckey VE, Luciw PA, Tarantal AF, Carville A, Shannon RP, Cota-Gomez A, Tuder RM, et al. HIV-1 Nef is associated with complex pulmonary vascular lesions in SHIV-nef–infected macaques. Am J Respir Crit Care Med. 2006;174:437–445. doi: 10.1164/rccm.200601-005OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Price TO, Ercal N, Nakaoke R, Banks WA. HIV-1 viral proteins gp120 and Tat induce oxidative stress in brain endothelial cells. Brain Res. 2005;1045:57–63. doi: 10.1016/j.brainres.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 26.Albini A, Soldi R, Giunciuglio D, Giraudo E, Benelli R, Primo L, Noonan D, Salio M, Camussi G, Rockl W, et al. The angiogenesis induced by HIV-1 tat protein is mediated by the Flk-1/KDR receptor on vascular endothelial cells. Nat Med. 1996;2:1371–1375. doi: 10.1038/nm1296-1371. [DOI] [PubMed] [Google Scholar]
- 27.Schecter AD, Berman AB, Yi L, Mosoian A, McManus CM, Berman JW, Klotman ME, Taubman MB. HIV envelope gp120 activates human arterial smooth muscle cells. Proc Natl Acad Sci USA. 2001;98:10142–10147. doi: 10.1073/pnas.181328798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ullrich CK, Groopman JE, Ganju RK. HIV-1 gp120– and gp160–induced apoptosis in cultured endothelial cells is mediated by caspases. Blood. 2000;96:1438–1442. [PubMed] [Google Scholar]
- 29.Ensoli B, Buonaguro L, Barillari G, Fiorelli V, Gendelman R, Morgan RA, Wingfield P, Gallo RC. Release, uptake, and effects of extracellular human immunodeficiency virus type 1 Tat protein on cell growth and viral transactivation. J Virol. 1993;67:277–287. doi: 10.1128/jvi.67.1.277-287.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barillari G, Ensoli B. Angiogenic effects of extracellular human immunodeficiency virus type 1 Tat protein and its role in the pathogenesis of AIDS-associated Kaposi’s sarcoma. Clin Microbiol Rev. 2002;15:310–326. doi: 10.1128/CMR.15.2.310-326.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dhillon NK, Li F, Xue B, Tawfik O, Morgello S, Buch S, Ladner AO. Effect of cocaine on human immunodeficiency virus–mediated pulmonary endothelial and smooth muscle dysfunction. Am J Respir Cell Mol Biol. 2011;45:40–52. doi: 10.1165/rcmb.2010-0097OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reid W, Sadowska M, Denaro F, Rao S, Foulke J, Jr, Hayes N, Jones O, Doodnauth D, Davis H, Sill A, et al. An HIV-1 transgenic rat that develops HIV-related pathology and immunologic dysfunction. Proc Natl Acad Sci USA. 2001;98:9271–9276. doi: 10.1073/pnas.161290298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reid W, Abdelwahab S, Sadowska M, Huso D, Neal A, Ahearn A, Bryant J, Gallo RC, Lewis GK, Reitz M. HIV-1 transgenic rats develop T cell abnormalities. Virology. 2004;321:111–119. doi: 10.1016/j.virol.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 34.Ray PE, Liu XH, Robinson LR, Reid W, Xu L, Owens JW, Jones OD, Denaro F, Davis HG, Bryant JL. A novel HIV-1 transgenic rat model of childhood HIV-1–associated nephropathy. Kidney Int. 2003;63:2242–2253. doi: 10.1046/j.1523-1755.2003.00028.x. [DOI] [PubMed] [Google Scholar]
- 35.Massaro EJ. Boca Raton, NY: CRC Press; 1997. Handbook of human toxicology. [Google Scholar]
- 36.Cedeno-Laurent F, Bryant J, Fishelevich R, Jones OD, Deng A, Eng ML, Gaspari AA, Trujillo JR. Inflammatory papillomatous hyperplasia and epidermal necrosis in a transgenic rat for HIV-1. J Dermatol Sci. 2009;53:112–119. doi: 10.1016/j.jdermsci.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joshi PC, Raynor R, Fan X, Guidot DM. HIV-1–transgene expression in rats decreases alveolar macrophage zinc levels and phagocytosis. Am J Respir Cell Mol Biol. 2008;39:218–226. doi: 10.1165/rcmb.2007-0344OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wei P, Garber ME, Fang SM, Fischer WH, Jones KA. A novel CDK9-associated C-type cyclin interacts directly with HIV-1 Tat and mediates its high-affinity, loop-specific binding to TAR RNA. Cell. 1998;92:451–462. doi: 10.1016/s0092-8674(00)80939-3. [DOI] [PubMed] [Google Scholar]
- 39.He LS, Chang SW, Voelkel NF. Pulmonary vascular reactivity in Fischer rats. J Appl Physiol (1985) 1991;70:1861–1866. doi: 10.1152/jappl.1991.70.4.1861. [DOI] [PubMed] [Google Scholar]
- 40.Porter KM, Walp ER, Elms SC, Raynor R, Mitchell PO, Guidot DM, Sutliff RL. Human immunodeficiency virus-1 transgene expression increases pulmonary vascular resistance and exacerbates hypoxia-induced pulmonary hypertension development. Pulm Circ. 2013;3:58–67. doi: 10.4103/2045-8932.109915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tinkle CW, Lipschitz D, Ponnappan U. Decreased association of p56lck with CD4 may account for lowered tyrosine kinase activity in mitogen-activated human T lymphocytes during aging. Cell Immunol. 1998;186:154–160. doi: 10.1006/cimm.1998.1313. [DOI] [PubMed] [Google Scholar]
- 42.Rosenberg HC, Rabinovitch M. Endothelial injury and vascular reactivity in monocrotaline pulmonary hypertension. Am J Physiol. 1988;255:H1484–H1491. doi: 10.1152/ajpheart.1988.255.6.H1484. [DOI] [PubMed] [Google Scholar]
- 43.Tuder RM. Pathology of pulmonary arterial hypertension. Semin Respir Crit Care Med. 2009;30:376–385. doi: 10.1055/s-0029-1233307. [DOI] [PubMed] [Google Scholar]
- 44.Maarman G, Lecour S, Butrous G, Thienemann F, Sliwa K. A comprehensive review: the evolution of animal models in pulmonary hypertension research; are we there yet? Pulm Circ. 2013;3:739–756. doi: 10.1086/674770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abe K, Toba M, Alzoubi A, Ito M, Fagan KA, Cool CD, Voelkel NF, McMurtry IF, Oka M. Formation of plexiform lesions in experimental severe pulmonary arterial hypertension. Circulation. 2010;121:2747–2754. doi: 10.1161/CIRCULATIONAHA.109.927681. [DOI] [PubMed] [Google Scholar]
- 46.Morrell NW, Yang X, Upton PD, Jourdan KB, Morgan N, Sheares KK, Trembath RC. Altered growth responses of pulmonary artery smooth muscle cells from patients with primary pulmonary hypertension to transforming growth factor-β1 and bone morphogenetic proteins. Circulation. 2001;104:790–795. doi: 10.1161/hc3201.094152. [DOI] [PubMed] [Google Scholar]
- 47.Nakaoka T, Gonda K, Ogita T, Otawara-Hamamoto Y, Okabe F, Kira Y, Harii K, Miyazono K, Takuwa Y, Fujita T. Inhibition of rat vascular smooth muscle proliferation in vitro and in vivo by bone morphogenetic protein-2. J Clin Invest. 1997;100:2824–2832. doi: 10.1172/JCI119830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McMurtry IF, Abe K, Ota H, Fagan KA, Oka M. Rho kinase–mediated vasoconstriction in pulmonary hypertension. Adv Exp Med Biol. 2010;661:299–308. doi: 10.1007/978-1-60761-500-2_19. [DOI] [PubMed] [Google Scholar]
- 49.Takahashi H, Goto N, Kojima Y, Tsuda Y, Morio Y, Muramatsu M, Fukuchi Y. Downregulation of type II bone morphogenetic protein receptor in hypoxic pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2006;290:L450–L458. doi: 10.1152/ajplung.00206.2005. [DOI] [PubMed] [Google Scholar]
- 50.Du L, Sullivan CC, Chu D, Cho AJ, Kido M, Wolf PL, Yuan JX, Deutsch R, Jamieson SW, Thistlethwaite PA. Signaling molecules in nonfamilial pulmonary hypertension. N Engl J Med. 2003;348:500–509. doi: 10.1056/NEJMoa021650. [DOI] [PubMed] [Google Scholar]
- 51.Chida A, Shintani M, Nakayama T, Furutani Y, Hayama E, Inai K, Saji T, Nonoyama S, Nakanishi T. Missense mutations of the BMPR1B (ALK6) gene in childhood idiopathic pulmonary arterial hypertension. Circ J. 2012;76:1501–1508. doi: 10.1253/circj.cj-11-1281. [DOI] [PubMed] [Google Scholar]
- 52.Reichrath J, Welter C, Mitschele T, Classen U, Meineke V, Tilgen W, Seifert M. Different expression patterns of calpain isozymes 1 and 2 (CAPN1 and 2) in squamous cell carcinomas (SCC) and basal cell carcinomas (BCC) of human skin. J Pathol. 2003;199:509–516. doi: 10.1002/path.1308. [DOI] [PubMed] [Google Scholar]
- 53.Wei X, Guo W, Wu S, Wang L, Huang P, Liu J, Fang B. Oxidative stress in NSC-741909–induced apoptosis of cancer cells. J Transl Med. 2010;8:37. doi: 10.1186/1479-5876-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Archer SL, Weir EK, Wilkins MR. Basic science of pulmonary arterial hypertension for clinicians: new concepts and experimental therapies. Circulation. 2010;121:2045–2066. doi: 10.1161/CIRCULATIONAHA.108.847707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dalvi P, O'Brien-Ladner A, Dhillon NK. Differential expression of microRNAs during cocaine and HIV-Tat mediated enhanced proliferation of pulmonary smooth muscle cells: probable involvement in the regulation of bone morphogenetic protein receptor expression [abstract] Am J Respir Crit Care Med. 2014;189:A1206. [Google Scholar]
- 56.Durrington HJ, Upton PD, Hoer S, Boname J, Dunmore BJ, Yang J, Crilley TK, Butler LM, Blackbourn DJ, Nash GB, et al. Identification of a lysosomal pathway regulating degradation of the bone morphogenetic protein receptor type II. J Biol Chem. 2010;285:37641–37649. doi: 10.1074/jbc.M110.132415. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.