Abstract
Isolated sinus of Valsalva aneurysm is a rare occurrence, with an incidence of <1.5% among congenital heart disease repairs in the world. We recount the case of a 64-year-old man who presented with right-sided heart failure symptoms caused by a severely dilated right coronary sinus of Valsalva aneurysm that substantially obstructed the right ventricular outflow tract. Successful surgical repair involved right ventricular outflow tract resection and subcoronary patch repair.
Keywords: Aortic aneurysm/congenital/surgery/ultrasonography, right ventricular outflow tract, sinus of Valsalva/abnormalities/surgery
Aortic sinus of Valsalva aneurysm (SVA) is very rare, comprising <1.5% of congenital heart disease repairs.1 This type of aneurysm is usually congenital, in which instance it results from an absence of muscular and elastic tissue in the aortic wall of the sinus of Valsalva and might be associated with other heart defects.2 Recent improvements in diagnostic techniques have increased the numbers of patients who undergo surgical repair of SVA. In this report, we recount the repair of a rare unruptured large aneurysm of the right SVA that presented as right ventricular (RV) failure arising from narrowing of the RV outflow tract (RVOT).
Case Report
In April 2014, a 64-year-old man presented at our hospital with signs of RV heart failure. His history revealed multiple episodes of dyspnea during the previous month. Further investigations—starting with transthoracic echocardiography and followed by cardiac magnetic resonance imaging (CMR) and computed tomographic (CT) angiography—confirmed RVOT obstruction caused by a large aortic root aneurysm (7.6 × 5.5 cm) (Figs. 1–3).
Fig. 1.
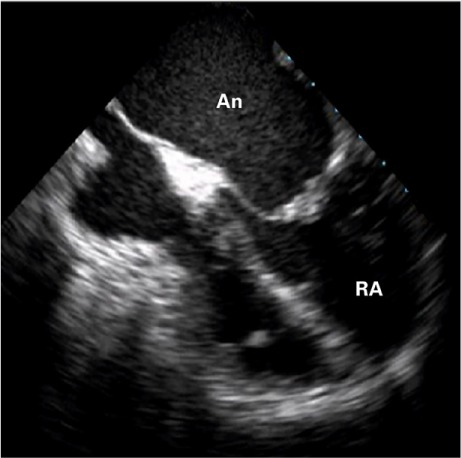
Two-dimensional transthoracic echocardiogram (apical 4-chamber view) shows a large aneurysmal vascular structure protruding into the right ventricle.
An = aneurysm; RA = right atrium
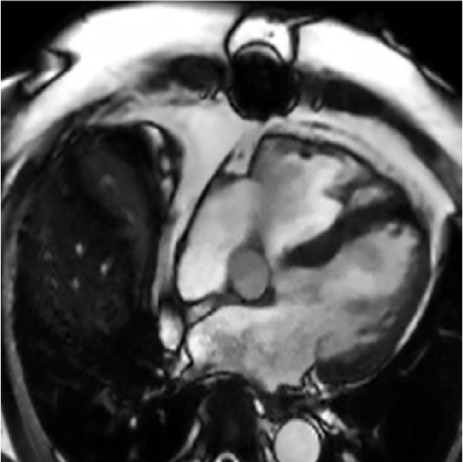
Fig. 3.
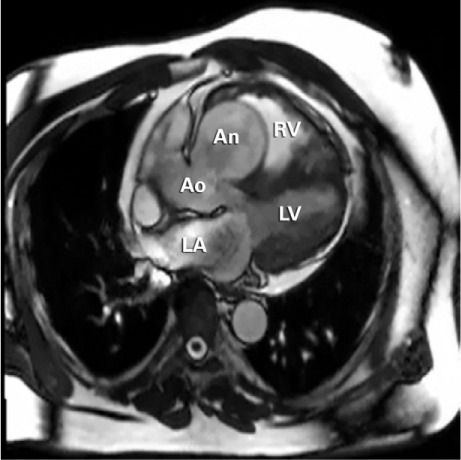
Cardiac magnetic resonance image (3-chamber long-axis view) shows a giant, unruptured sinus of Valsalva aneurysm (approximately 7.6 × 5.5 × 5.7 cm).
An = aneurysm; Ao = aorta; LA = left atrium; LV = left ventricle; RV = right ventricle
Fig. 2.
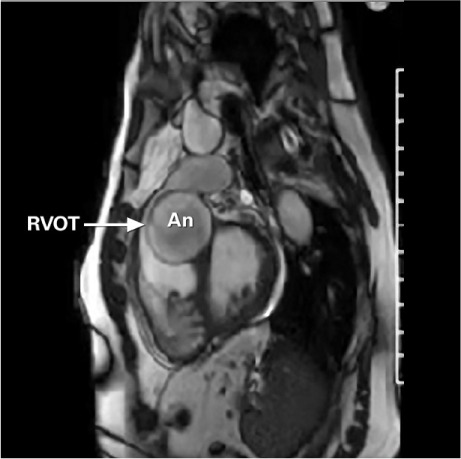
Cardiac magnetic resonance image shows the sinus of Valsalva aneurysm (An) substantially obstructing the right ventricular outflow tract (RVOT).
The surgical technique involved a midline sternotomy, cardiopulmonary bypass with ascending aortic and bicaval cannulation, and cardioplegic arrest. The defect was approached from the aortic root via both a transverse aortotomy and a right ventriculotomy (through the RVOT). The RV itself was seen to be substantially enlarged. The RVOT obstruction was evident: it took the form of a compression by the aortic sinus of Valsalva aneurysm (Fig. 4).
Fig. 4.
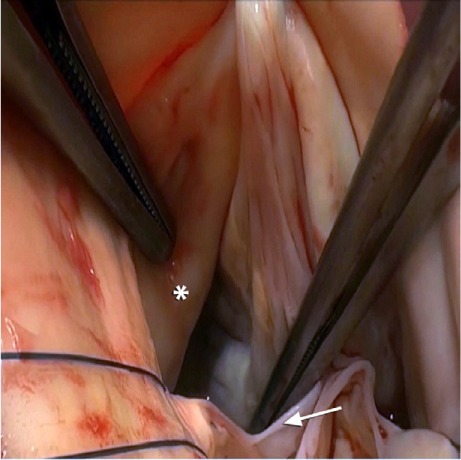
Intraoperative photograph of the open aortotomy shows the unruptured sinus of Valsalva aneurysm (asterisk) and the right cusp of the aortic valve (arrow).
We proceeded to open the ascending aorta and to expose the aortic valve. Inspection revealed a healthy tricuspid aortic valve with a large defect underneath the right coronary ostium, as had been seen upon imaging. The defect within the right sinus of Valsalva was approximately 3.0 × 5.0 cm in diameter. The view of the aneurysm through a right atriotomy and tricuspid valve was not satisfactory, however. Resection of the aneurysm was carried out through the subpulmonic RVOT incision, and this was followed by oversewing with pledgeted 4-0 Prolene sutures, in a continuous fashion. We enlarged the RVOT with bovine pericardium. After inspecting the aorta, we used a circular bovine pericardial patch and running 5-0 Prolene suture to close the SVA in a subcoronary manner. The postoperative period was uneventful, and the patient was discharged from the hospital on postoperative day 9.
As part of our postoperative analysis, we performed a follow-up imaging study that included CMR 6 months after the surgical resection. There was no evidence of the right SVA, and RV systolic function had substantially improved (Fig. 5).
Fig. 5.
At 6 postoperative months, this cardiac magnetic resonance image (3-chamber long-axis view) reveals no residual right sinus of Valsalva aneurysm.
Discussion
Aneurysm of the sinus of Valsalva is a congenital heart disease that constitutes 0.14% to 1.5% of congenital heart disease repairs in the world.1 Because the aortic valve occupies a central position in the base of the heart, an SVA can rupture into any of the 4 heart chambers, most often the right atrium or RV.3 When an SVA ruptures into the RVOT, a coexisting subarterial ventricular septal defect (VSD) is likely.4 Aortic regurgitation is a commonly associated lesion, next in frequency to VSD.
Our patient presented with right-sided heart failure and shortness of breath. Appropriate CT angiography and CMR were performed to determine the location of the aneurysm and cardiac functional status. Through patch repair of the subcoronary sinus, resection of the aneurysm from the RVOT, and patch enlargement of the RVOT, we successfully repaired this aneurysm.
Sinus of Valsalva aneurysms can present with the symptoms of right-sided heart failure. Once the RV pressure overload has been corrected, primary surgical repair is feasible, with good short-term outcomes and delayed RV remodeling.
Footnotes
From: Department of Cardiovascular Surgery, Houston Methodist DeBakey Heart & Vascular Center, Houston Methodist Hospital, Houston, Texas 77030
Dr. Abu Saleh is now at the Department of Surgery, University of Texas Health Science Center, San Antonio, Texas.
Dr. Ramlawi is now at the Department of Cardiothoracic Surgery, Valley Health System, Winchester, Virginia.
Presented at the 95th Annual Meeting of the American Association for Thoracic Surgery, Seattle, Washington; 25–29 April 2015.
References
- 1.Lisowski P, Hirnie T, Adamczuk A, Lisowska A, Sobkowicz B, Nadlewski S, Gorny J. Rupture of the sinus of Valsalva aneurysm complicated by infective endocarditis -- diagnosis difficulties [in Polish] Kardiol Pol. 2006;64(1):77–9. [PubMed] [Google Scholar]
- 2.Lin CY, Hong GJ, Lee KC, Tsai YT, Tsai CS. Ruptured congenital sinus of Valsalva aneurysms. J Card Surg. 2004;19(2):99–102. doi: 10.1111/j.0886-0440.2004.04022.x. [DOI] [PubMed] [Google Scholar]
- 3.Fazio G, Zito R, Dioco DD, Mussagy C, Loredana S, Damasceno A, Novo S. Rupture of a left sinus of Valsalva aneurysm into the pulmonary artery. Eur J Echocardiogr. 2006;7(3):230–2. doi: 10.1016/j.euje.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Choudhary SK, Bhan A, Sharma R, Airan B, Kumar AS, Venugopal P. Sinus of Valsalva aneurysms: 20 years' experience. J Card Surg. 1997;12(5):300–8. doi: 10.1111/j.1540-8191.1997.tb00143.x. [DOI] [PubMed] [Google Scholar]


