Abstract
Background
There is considerable movement in the U.S. to legalize use of cannabis for medicinal purposes. Twenty-three U.S. states and the D.C. have laws that decriminalize use of marijuana for medicinal purposes. Most prior studies of state medical marijuana laws and their association with overall marijuana use, adolescent use, crime rates, and alcohol traffic fatalities, have used a binary coding of whether the state had a medical marijuana law or not. Mixed results from these studies raise the question of whether this method for measuring policy characteristics is adequate.
Objectives
Our objective was to develop a validated taxonomy of medical marijuana laws that will allow researchers to measure variation in aspects of medical marijuana statutes as well as their overall restrictiveness.
Methods/Results
We used a modified Delphi technique using detailed and validated data about each state's medical marijuana law. Three senior researchers coded elements of the state laws in initiation of use, quantity allowed, regulations around distribution, and overall restrictiveness. We used 2013 NSDUH data to assess validity of the taxonomy. Results indicate substantial state-level variation in medical marijuana policies. Validation analysis supported the taxonomy's validity for all four dimensions with the largest effect sizes for the quantity allowed in the state's medical marijuana policy.
Conclusions/Importance
This analysis demonstrates the potential importance of non-dichotomous measurement of medical marijuana laws in studies of their impact. These findings may also be useful to states that are considering medical marijuana laws, to understand the potential impact of characteristics of those laws.
Keywords: Marijuana, medical marijuana, marijuana laws, drug policy, qualitative methods
INTRODUCTION
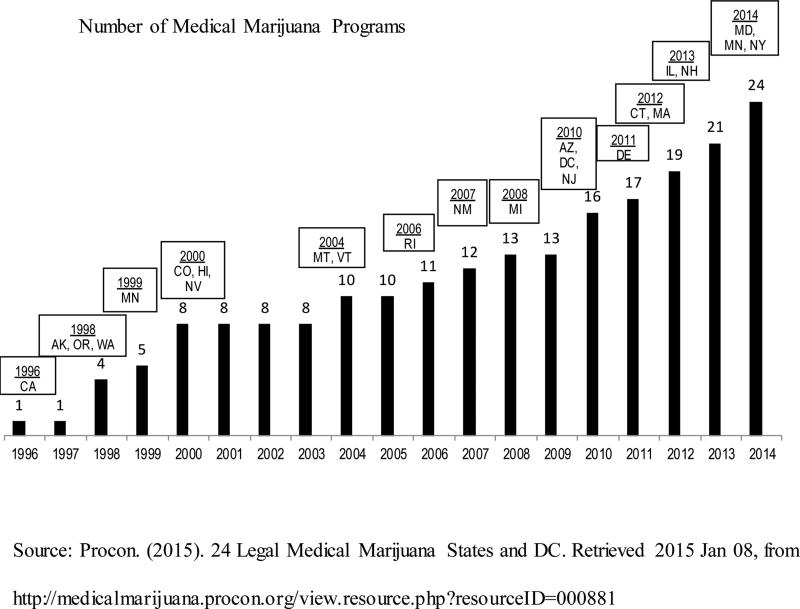
There is considerable momentum to legally permit use of cannabis for medicinal purposes, making this a topic of growing interest among drug policy researchers in the U.S. and abroad. Twenty-three U.S. states and the District of Columbia now have laws that decriminalize use of marijuana for medicinal purposes (Procon, 2015). As Figure 1 shows, the trend is accelerating. Prior to the year 2000, only four states had passed a law permitting medical marijuana; in contrast, during the next decade a total of eight new state laws were enacted. Eighteen additional states have recently introduced medical marijuana legislation, with one of those states still pending action in 2015 (Procon, 2015; Marijuana Policy Project (MPP), 2013). It is estimated that 40 percent of the U.S. population has access to cannabis for medical purposes (Benac, 2013).
FIGURE 1.
Medical marijuana states by year of implementation
Only a small fraction of any given state's population will be directly affected by a medical marijuana statute, in the sense of actually registering as a user under the law (Ogborne et al., 2000). Nonetheless, understanding medical marijuana regulatory regimes is of broad significance due to their potential to bring unintended consequences upon the population at large. Some policy analysts speculate that medical marijuana laws are both a cause and consequence of the growing liberalization of attitudes—or “wettening”—of American public opinion towards cannabis (Pedersen et al., 2013; Khatapoush & Hallfors, 2004). Others suggest that these laws are implicated in the national trend toward increased cannabis consumption via the diversion of medical marijuana products into illegal markets, thereby reducing price (Dawson et al., 2006; Drummer et al., 2004). Further consequences may include increased access to cannabis by youth, possible increases in drugged driving, and the wider availability of more concentrated forms of cannabis (Levy, 2013; Thurstone et al., 2011). There is some, albeit limited, evidence that rates of cannabis consumption and related problems are indeed higher in states with medical marijuana laws (Cerdá et al., 2012). However, thus far the causal pathways are unclear, and some studies suggest these laws have positive unintended consequences, not just negative ones (Anderson et al., 2013; Bachhuber et al., 2014; Kepple and Freisthler, 2012).
An important precondition for studying the impacts of medical marijuana laws is being able to measure their scope and nature as regulatory instruments. Studies that delve into the specific details of marijuana statutes across states are few (Freisthler et al., 2013; Pacula et al., 2001), and the challenges inherent in doing so have been noted in the literature (Pacula & Sevigny, 2014). Pacula and colleagues (2015) provided detailed descriptions of characteristics of medical marijuana state statues and concluded that treating all laws as the same across states is misleading. The heterogeneity in state medical marijuana statutes makes it difficult to measure the overall restrictiveness of one state's law compared to the next and, therefore, to gauge its impacts on the population (Wall et al., 2012). Some statutes, for example, require that patients register with state officials, which can affect the capacity to monitor legal cannabis use. Most states, but not all, charge registration fees, but the fees range from $25 to $300, potentially erecting different barriers to entry into medical marijuana programs. State laws also vary in the amount of marijuana that may be possessed, whether the drug can be cultivated at home, the specific medical conditions warranting medicinal use, and whether and how the drug can be legally dispensed. Some states protect patients from conviction, but not arrest, while others do not. In some states, patients can grow their own plants, while other states restrict cultivation but have established dispensaries or “compassion centers” as the only place where legal cannabis can be accessed (Benac, 2013).
The objective of this study was to develop a validated taxonomy that could allow researchers to systematically measure variation in specific aspects of medical marijuana statutes, as well as to measure their overall restrictiveness. Drawing on publicly available sources and key informant interviews with state officials, we collected detailed data on seventeen different aspects of medical marijuana policy regimes in all states with such laws through 2014. Using a modified Delphi technique, we identified three specific domains that characterize different aspects of medical marijuana laws as well as a summary measure of overall restrictiveness. This report presents the taxonomy, assesses its external validity, and uses it to describe current variation across U.S. states with medical marijuana laws.
Prior Research
Because U.S. states vary significantly in their policies toward cannabis, America offers an ideal context for studying how the specific characteristics of medical marijuana policies impact consumption and drug-related harms. There have been several studies of state medical marijuana laws and their association with overall marijuana use, adolescent use, crime rates, alcohol-related traffic fatalities, and other public health issues. However, most have used a rather crude formula for capturing the policy regime—one limited to the binary coding of whether or not a given state has a medical marijuana statute on the books.
So far, these studies have yielded mixed results, raising questions about whether the predominant methodology for measuring policy is adequate for the task. For example, Cerdá and colleagues (2012) studied the relationship between medical marijuana and marijuana use, abuse and dependence, finding that the residents of states with medical marijuana laws had a greater likelihood of having used marijuana and experiencing cannabis dependence. However, a study by Harper et al. (2012), reported that adolescent use of marijuana decreased after the passage of medical marijuana laws. Chu (2012) found increased arrests for illicit marijuana and a 10 percent increase in referrals for marijuana treatment in states with medical marijuana laws, while Bachhuber and colleagues (2014) found decreases in opioid analgesic overdose mortality rates in medical marijuana states.
The literature underscores the potential value of a medical marijuana law taxonomy for studies examining whether these regulatory regimes produce negative impacts on population health and, if so, which specific aspects of the laws matter most. Several recent papers have concluded with calls for more careful analysis of the heterogeneity in medical marijuana laws (Hunt et al., 2013; Pacula et al., 2015; Pacula and Sevigny, 2014) and two recent studies hint that such a strategy could shed light on why current studies find mixed results. A study by Hunt and colleagues (2013) used latent class analysis to predict which states were likely to pass a medical marijuana statute on the basis of public perceptions about the acceptability of cannabis use, its use as a home remedy and/or as a pharmaceutical. This study demonstrated the potential to find common components across heterogeneous policy regimes. More compelling is Pacula and colleagues’(2015) study documenting that the impact of these laws on cannabis consumption, problems, and treatment admissions varied by whether or not the laws included specific provisions allowing home cultivation and purchasing through dispensaries. Notably, Pacula et al. (2015) found that the impacts of medical marijuana laws were masked when states were simply coded on the basis of whether they did or did not have a medical marijuana law. It was only when researchers took account of specific aspects of medical marijuana policies that it was possible to measure the effects of medical marijuana policies on population health.
METHODS
A taxonomy is a system for classifying multifaceted complex phenomena according to conceptual domains and dimensions (Bradley et al., 2007). In health services research this method is useful in the study of policies and programs, such as state legislation and public initiatives. Developing a taxonomy involves specifying the dimensions of variables and the relationships between variables, and then coding them into concepts or categories (Bradley et al., 2007). Related concepts form a taxonomy when those concepts are linked together. There is a modest tradition of using taxonomies to understand variation in policy regimes in the substance abuse field. One of the most useful has been Karlsson and Österberg's (2007) taxonomy of alcohol control policies across Europe. Here, the final taxonomy included domains pertaining alcohol taxation, control of distribution, social and environmental scores, and age limits (Karlsson & Österberg, 2001).
In keeping with Karlsson and Österberg's research strategy, we used a qualitative, modified Delphi technique involving expert panel assessments. The Delphi process has been used in research, program planning, and policy determination. It was developed at the RAND Corporation in the 1950s (Dalkey & Helmer, 1963), and is a widely used and accepted technique for achieving a convergence and consensus of opinion from a panel of experts (Hsu & Sandford, 2007). The method is noted as being particularly useful for policy investigation or predicting the occurrence of future events (Gupta & Clarke, 1996; Hsu & Sandford, 2007; Landeta, 2006). The feasibility and usefulness of the modified Delphi approach has been established in prior research of state-level policies and other issues in health care (Michtalik et al., 2013; Seago et al., 2004).
Data Collection and Management
We collected and validated data pertaining to the details of medical marijuana laws from the 23 U.S. states and the D.C. that had passed such laws by 2014. Data sources included websites such as Procon (Procon, 2015) and the Marijuana Policy Project (MPP) (Marijuana Policy Project, 2013), public records of state laws, web sites from state medical marijuana programs, published papers, state government reports, and direct communications with state policy officials. The research team developed spreadsheets including data for each state law, for each year the law had been in existence since it was first passed. This allowed us to account for regulatory changes in medical marijuana programs, such as adding covered conditions or allowing dispensaries. These elements of the state laws, and subsequent additions or changes, were entered into a spreadsheet for each year since the state's law/initiative was enacted. We validated the information for each state by cross-checking on the websites Procon and MPP, and also used detailed text in the state laws and initiatives as references. We coded each variable as binary, continuous, or categorical depending on the type of data. For example, each medical condition for which medical marijuana was allowed was coded as binary if the condition was specified in the state's law, while the number of plants that can be cultivated for personal medical use was a continuous variable.
Other aspects of the legislation coded as binary variables included dispensaries allowed, registration required, registration fees, cultivation allowed by patient and caregiver, caregivers allowed, and required terms of the relationship with the authorizing physician. Continuous data included the amount of medical marijuana that could be possessed, in ounces, the number of plants that could be cultivated, the number of caregivers permitted per patient, and the number of patients permitted per caregiver. Table 1 includes a summary of the variables collected and used to code specific aspects of medical marijuana policies.
TABLE 1.
State-level policy characteristics used in taxonomy development
| Variable | Definition |
|---|---|
| Caregivers per patient | The number of caregivers allowed per patient |
| Dispensary in law | Whether medical marijuana dispensaries are allowed to operate in the law |
| Cultivation allowed | Whether cultivation of marijuana plants is allowed by patient or caregiver |
| In-state license required | Whether an in-state license is required for registration |
| Number of approved conditions | Total number of medical conditions approved for medical marijuana prescription |
| Number of dispensaries | Total number of operating dispensaries |
| Number of plants allowed | Total number of mature and immature marijuana plants allowed for cultivation |
| Other conditions approved | Whether other medical conditions, not specified in the law, can be approved for medical marijuana recommendation from physician |
| Other states’ medical marijuana cards | Whether states’ programs will accept other states’ medical marijuana cards |
| Out-of-state licenses allowed | Whether states’ programs will allow out-of-state is allowed for registration |
| Patients per caregiver | The number of patients allowed per caregiver |
| Possession allowed | The number of ounces of usable marijuana allowed in possession |
| Physician statement | Whether a physician statement is mandatory to register for medical marijuana registration |
| Rate of registration | The rate of registered medical marijuana patients per state population |
| Registration | Whether registration is mandatory, voluntary, or non-existent in the law |
| Required length of physician-patient relationship | Whether a physician-patient relationship has to be established for the physician to recommend medical marijuana for a patient and if specified, length of relationship |
| Total initial costs for patient | The total cost to register for a medical marijuana program, assuming no caregiver, no growing fees, and no low income options |
Data Coding and Consensus Process
Three senior researchers from our study team (co-authors SC, JS and LS), from varied disciplinary backgrounds, participated in the rating process and analysis for taxonomy development. Based on their knowledge of the drug policy literature and a review of the characteristics of medical marijuana laws in each state, they identified three distinct dimensions for coding: 1) “initiation,” or the ease with which state policies made it possible to become a medical marijuana user, 2) “quantity,” or how liberal state policies were with respect to the amounts of cannabis that users could legally access, and 3) “distribution,” pertaining to the extent to which the state policy regime was likely to have the capacity to monitor, regulate, and control the supply of marijuana being diverted into illegal markets. The specific state-level policy characteristics used to code each state law are included in Table 1.
After the three dimensions were agreed upon, the researchers spent several weeks independently reviewing the detailed information on each state's medical marijuana law and rating each state on the dimensions of those laws. Each dimension was scored on a 1 to 5 scale. For initiation, a score of 1 indicated that it was difficult to become an approved medical marijuana user, and 5 indicated that it was relatively easy to initiate use. For quantity, a score of 1 was defined as not permitting a large quantity of product for each user, and a score of 5 indicated that a relatively large quantity was permitted. For distribution, a score of 1 indicated that the distribution system was tightly controlled, and a score of 5 was assigned to states with little control over distribution. Table 2 describes the three analytic domains--initiation, quantity, and distribution--and the variables from Table 1 used to determine the score in each domain. A summary domain of overall restrictiveness was a sum of the scores for each of the three domains.
TABLE 2.
Policy domains pertaining to medical marijuana laws
| Policy Domains | Modal Score, Range N=23 States+ DC | Variables used to calculate score |
|---|---|---|
| Initiation (i.e., the degree to which the state's law imposes barriers to becoming a registered medical marijuana user) | 3.0 (1-5) | Physician statement |
| In-state license required | ||
| Out-of-state licenses allowed | ||
| Required length of physician-patient relationship | ||
| Other states’ MMP cards | ||
| Registration | ||
| Rate of registration | ||
| Total initial costs for patient | ||
| Number of approved conditions | ||
| Other conditions approved | ||
| Quantity (i.e., the total amount of cannabis that the state's law allows a user to possess) | 2.0 (1-5) | Possession allowed |
| 3.0 (1-5) | Cultivation allowed | |
| Number of plants | ||
| Patients per caregiver | ||
| Distribution Regulation (i.e., the extent to which the state's law regulates and constrains access to medical marijuana) | 1.0 (1-5) | Cultivation allowed |
| Patients per caregiver | ||
| Caregivers per patient | ||
| Dispensary in law | ||
| Number of dispensaries | ||
| Overall Restrictiveness | 12.0 (4-14) | Sum of Initiation, Overall Quantity, Distribution Regulation |
The independent ratings of each researcher were submitted to a research analyst to create tables of each rater's scores for each dimension. The three researchers then reviewed and discussed the ratings to reach a consensus. If there was agreement among all three raters, the scores were accepted. If two of the raters agreed and one rater was only 1 point different, the score of the 2 raters was accepted. In all other cases with more than a one point difference or three different ratings, the team discussed the discrepancies until a consensus could be reached. Upon completion of the consensus exercise, each rater re-reviewed the final information to ensure internal consistency. Table 3 includes the four consensus scores for each medical marijuana state and changes over time in the laws that were considered in the scoring. Most changes occurred in dispensary regulations added or changed after the original law was passed.
TABLE 3.
Consensus Scores by State
| State | Initiation | Quantity | Distribution | Overall Restrictiveness | Changes Over Time |
|---|---|---|---|---|---|
| Alaska | 1 | 3 | 5 | 9 | |
| Arizona | 3 | 3 | 3 | 9 | |
| California | 5 | 4 | 4 | 13 | |
| Colorado | 4 | 3 | 3 | 10 | Distribution changed from 4 to 3 in 2010 due to the addition of dispensaries. |
| Connecticut | 3 | 1 | 1 | 5 | |
| DC | 3 | 1 | 1 | 5 | |
| Delaware | 3 | 2 | 1 | 6 | |
| Hawaii | 4 | 3 | 5 | 12 | |
| Illinois | 4 | 2 | 2 | 8 | |
| Maine | 5 | 3 | 4 | 12 | |
| Maryland | 3 | 2 | 1 | 6 | |
| Massachusetts | 4 | 4 | 4 | 12 | |
| Michigan | 4 | 3 | 5 | 12 | |
| Minnesota | 2 | 1 | 1 | 4 | |
| Montana | 4 | 4 | 5 | 13 | |
| Nevada | 3 | 2 | 3 | 8 | Distribution changed from 5 to 3 in 2013 due to added dispensaries. |
| New Hampshire | 3 | 2 | 2 | 7 | |
| New Jersey | 2 | 1 | 1 | 4 | |
| New Mexico | 4 | 4 | 2 | 10 | |
| New York | 2 | 1 | 1 | 4 | |
| Oregon | 3 | 5 | 3 | 11 | Distribution changed from 5 to 3 in 2013 due to added dispensaries |
| Rhode Island | 4 | 4 | 3 | 11 | Distribution changed from 4 to 3 in 2009 due to the addition of dispensaries |
| Vermont | 3 | 2 | 2 | 7 | Initiation changed from 2 to 3 in 2006 due to newly approved conditions. Distribution changed from 4 to 2 in 2011 due to the addition of dispensaries |
| Washington | 5 | 5 | 4 | 14 |
Validation Methodology
Once the taxonomy was developed, we used pooled state-level data from the U.S. National Survey on Drug Use and Health (NSDUH) to assess its validity. The NSDUH is an annual survey of the civilian, non-institutionalized population of the United States aged 12 years or older to measure the prevalence and correlates of licit and illicit substance use, and substance abuse and dependence. The survey uses a 50-state sampling approach that generates an independent, multi-stage area probability sample for each of the 50 states and the District of Columbia. The survey includes residents of households, non-institutional group quarters (e.g., shelters, rooming houses, dormitories), and civilians living on military bases. Homeless persons not in public shelters, individuals in active military duties, and residents of institutional group quarters (e.g., prisons and hospitals) are not included in the sampling frame. The hypothesis driving the validation analysis was that, if our measures of specific aspects of medical marijuana laws and their overall restrictiveness were valid, populations in states with less restrictive laws would have “wetter” attitudes towards cannabis and higher levels of consumption.
The 2013 NSDUH is the most recent wave of data that is publicly-available. We extracted state-level data for adults over 25, all that is currently available due to subject confidentiality restrictions. The dependent variables in the validation analysis were the proportion of adults who used marijuana in the past year, the proportion who viewed marijuana use on a monthly basis or more often as a “great risk,” as well as marijuana use on a weekly basis or more often. In a series of ordinary least squares regression analyses, we subjected each medical marijuana policy variable to repeated tests, using population estimates drawn from non-medical marijuana states as a comparison group. These analyses controlled for relevant demographics and characteristics of the state's economic and political environment, including state-level unemployment rate, education level, poverty rate, ethnic diversity, age distribution, percent residing in urban areas, immigrant percentage, and rates of active church-going and political conservatism. All analyses were weighted to control for design effects. In the public use file, the sample weight represents the total number of persons in the target population that each record in the file represents.
RESULTS
State-Level Variation in Medical Marijuana Statutes
The collection of detailed information on all 24 medical marijuana laws passed through 2014 revealed a pronounced degree of state-level variation. Five states (AK, AZ, NH, NJ, VT) and the District of Columbia were reported to have explicit criteria about the length of the relationship required with the authorizing physician. This provision of medical marijuana laws has gained importance as states begin to examine which providers are authorizing medical marijuana and how many providers are active in medical marijuana programs. For example, data from the Arizona medical marijuana program indicated that the majority of medical marijuana certifications (73%) came from 24 professionals in the state (Dyer, 2013). Most of those were from naturopaths, of whom a handful has written most of the certifications. Six physicians wrote 61% of all medical marijuana certifications written in Arizona. Mandatory registration is another important determinant of initiation. California, offered voluntary registration but does not mandate it, whereas in New Jersey registration was required and charged a fee of $200 ($400 with a caregiver).
The quantity of medical marijuana allowed via possession and cultivation varied substantially across states. Total ounces of medical marijuana that may be possessed at a time ranged from 1 ounce in Alaska, Montana, and Nevada to 1½ pounds in Oregon and Washington. Some states allow users to grow their own medical marijuana, and those states specify the number of plants that can be grown, as well as the maturity of those plants. In the 15 states that allow home cultivation, the number of plants allowed ranges from 6 plants (CO, AK, ME) to 24 plants (OR) (Procon, 2015).
Controls over the distribution of medical marijuana are also quite varied across states. State control will be affected by whether cultivation is allowed, whether medical marijuana patients can identify caregivers to obtain it for them, how many patients any given caregiver can have, and whether the state allows dispensaries. The majority of state medical marijuana laws now allow for dispensaries. However, the dispensary elements appear to be actively changing as governments gain experience with implementing these laws. Nevada and Oregon just added dispensaries to their medical marijuana programs in 2013 (Crombie, 2013). California has a history of being rather lax about the proliferation of dispensaries. However, we generally observed a trend whereby states are becoming stricter and allowing more local control over whether and where dispensaries are located (Hicks & Ziegler, 2013).
Capturing Variation in a Taxonomy of Medical Marijuana Policies
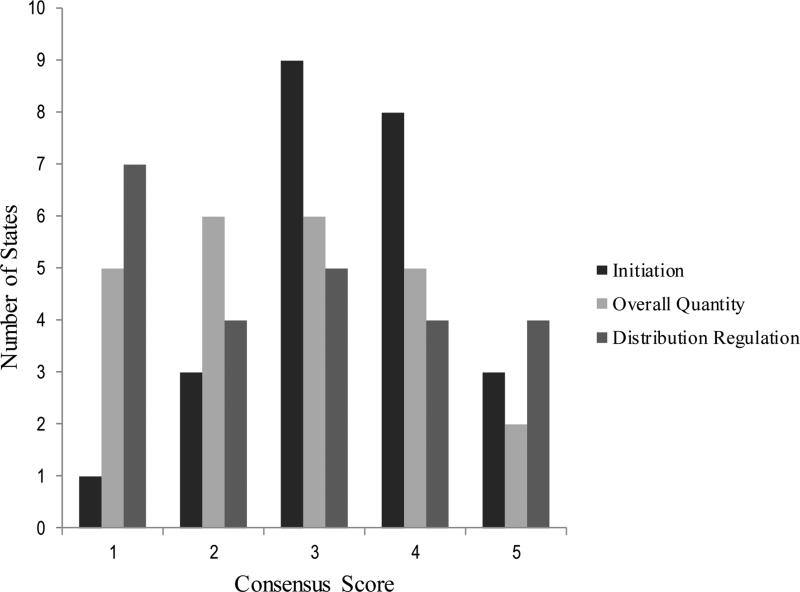
Despite the wide degree of variation across states in medical marijuana laws, it was possible to identify three common threads, or policy domains, that capture specific dimensions of their potential influence. Figure 2 displays the summary variable scores for each of the three domains incorporated into the analysis. The modal score for the initiation dimension was 3 (9 states); one state had an initiation rating of 1 (very hard to become a user), 3 had a score of 2, 8 had a score of 4, and 3 had a score of 5. The modal value of the quantity variable was 2 and 3 (6 states), with scores of 1 and 4 for 5 states each, and a score of 5 for 2 states. The distribution variable had a modal score of 1 (7 states); 4 states had a score of 2, 5 states has a score of 3, 4 states had a score of 4, and 4 states has a score of 5.
FIGURE 2.
Distribution of consensus scores for three policy domains
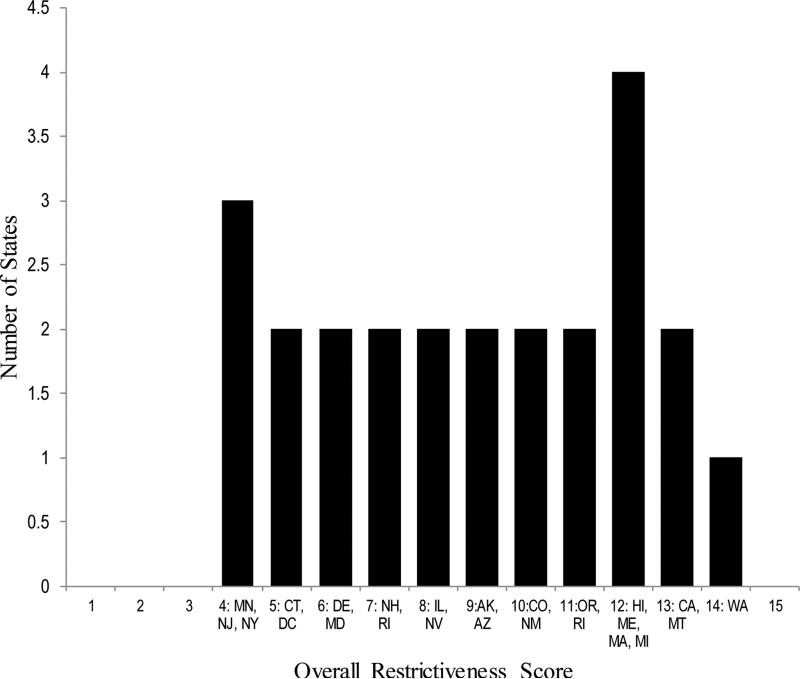
We also created a summary variable, which is the sum of the three separate dimensions of state laws (Figure 3). This variable provided a composite picture of variation across state medical marijuana regimes, one that captures the overall restrictiveness of the state's policy. This variable had a range from 4 to 14, with the modal value being 12. Looking across summary scores, it is interesting to compare states that are on the lower and upper ranges of the summary score. In states like New Jersey, New York, and Minnesota, it is difficult to initiate medical marijuana use: the quantity allowed is limited, and distribution is highly regulated. In contrast, in states such as California, Montana, and Washington, initiation is relatively easy: a greater quantity of medical marijuana is allowed, and there is not much government control over distribution.
FIGURE 3.
Summary measure of overall restrictiveness of state medical marijuana laws
Validating the Taxonomy
As Table 4 illustrates, the regression analysis supports the taxonomy's validity for all four dimensions of medical marijuana policy, using a range of population-based outcome measures. The proportion of the population that used marijuana in the past year is positively associated with all three policy measures, as well as the Overall Restrictiveness score (β=0.365, p<0.001). The relationships for both outcomes are stronger for Quantity (β=1.241) and Distribution Regulation (β=0.980) as compared with Initiation (β=0.693). The shares of the population that views it as a great risk to use marijuana monthly or to use it weekly are negatively associated with all three domains, as well as the Overall Restrictiveness measure; the relationships are largest for Quantity (β=−1.828 for monthly; β=−2.362 for past weekly).
TABLE 4.
Validation of state policy taxonomy using the 2013 National Survey on Drug Use and Health (N = 51 states)
| Initiation β | Quantity β | Distribution Regulation β | Overall Restrictiveness β | |
|---|---|---|---|---|
| Proportion of state's population that: | ||||
| Used marijuana in past year | 0.693** | 1.241*** | 0.980*** | 0.365*** |
| Views it a “great risk” to use marijuana monthly | −1.113* | −1.828*** | −1.276** | −0.527** |
| Views it a “great risk” to use marijuana weekly | −1.339* | −2.362*** | −1.946*** | −0.709*** |
Note: Results represent ordinary least squares regression coefficients run in separate models controlling on state-level unemployment rate, education level, poverty rate, ethnic diversity, age distribution, percent residing in urban areas, immigrant percentage, and rates of active church-going and political conservatism.
p < .05
p < .01
p< .001
DISCUSSION
There is an accelerating trend in the U.S. and abroad to make cannabis more accessible to individuals suffering from chronic pain and other health conditions. The U.S. provides a unique context for studying the impacts of these laws on population health because there is substantial heterogeneity in legal statutes pertaining to medical marijuana across states. However, thus far, most researchers studying the impact of medical marijuana have used crude binary measures that simply identify whether or not a state has a medical marijuana law. Results pertaining to the impacts of these laws on population health have produced mixed findings. To the limited extent that researchers have measured variation in specific aspects of these laws, they have shown larger effects, suggesting the need for more nuanced measures of how these laws are actually being implemented.
When we collected data on the characteristics of medical marijuana laws for 23 U.S. states and the District of Columbia, we observed a notable degree of heterogeneity in the statutory specifics. We identified 17 different variables upon which state laws could vary, and states ranged substantially in the extent to which their laws took these possibilities into account. Using a modified Delphi procedure, we were able to arrive upon three specific areas in which state laws varied, and these characteristics could differentially impact population health. It was possible to accurately code states on the basis of these characteristics with minimal disagreement amongst three expert raters. In a validity analysis, we found robust evidence that the taxonomy of medical marijuana laws corresponds well to population-based outcomes pertaining to cannabis consumption and public attitudes about cannabis.
Limitations
We had three researchers involved in rating the state medical marijuana items and developing the consensus scores. The Delphi method may be less useful if some of the raters have less in-depth knowledge of the topic (Hsu and Sandford, 2007). However, each of our three raters were equally familiar with the laws and the definitions of the elements used in the ratings. Researcher bias is also a concern in qualitative methodology (Pope and Nicholas, 2009). Having three raters from different disciplines working independently to develop initial ratings helped to address potential bias. As far as we know this is the first attempt to create a taxonomy of the facets of medical marijuana laws using a qualitative, consensus building approach. Further research to validate these taxonomies is needed. A further limitation is that we are unable to assess the fidelity of states to the exact language and policies included in the laws. An assessment of how closely states adhere to the statutory content of the laws was not within the scope of this paper.
Implications for Future Research
This analysis adds to recent work that has highlighted the potential importance of measuring medical marijuana regulations as non-dichotomous variables in studies of the impact of medical marijuana on cannabis use, abuse, supply, price, substitution, and other outcomes. An emerging body of research indicates that the characteristics of medical marijuana laws could have substantial influence over whether medical marijuana laws are associated with increased recreational use of marijuana, increased supply of illicit marijuana, changing perceptions of the risk of marijuana use, and the substitution of marijuana for other illicit substances.
Future research should examine the overall and differential impacts of medical marijuana law characteristics. We hypothesize that the initiation dimension of medical marijuana laws could be associated with illicit marijuana use in several ways. First, the ease with which people can become approved medical marijuana users could reflect social norms about the acceptability of marijuana. Second, the ease of approval could signal that marijuana is not very risky, and in fact that it may be beneficial. Third, a large number of approved users may increase the number of people who could potentially divert medical marijuana to illicit markets.
The quantity of medical marijuana permitted might directly affect the amount of marijuana product that is available for potential diversion to illicit use, and may be related to the price of marijuana in the market. Similarly, a loosely controlled distribution system could increase likelihood of diversion, and also might reflect libertarian social norms.
Use of the typology to measure policy impacts on population health will require sophisticated research designs. Such attempts are fraught with challenges, involving the need to take other marijuana policies into consideration (e.g., penalties for possession and sales), how media and public debates around marijuana shape attitudes and use, problems with the time-ordering of events or endogeneity, and the changing potency of cannabis projects over time (Pacula & Sevigny, 2014).
As states have passed medical marijuana laws and voter initiatives, the attributes of the laws have varied in important aspects related to the initiation of use, quantity allowed, and distribution. Those facets of the laws could have different impacts on the illicit use of marijuana. Research on such impacts would be useful to states that are debating, but have not yet passed, medical marijuana laws in considering the components of those laws and potential effects. Future research should include the variation in state laws in analyses of the impacts of medical marijuana.
ACKNOWLEDGMENT
A previous version of this article was delivered to the American Society of Health Economists, Los Angeles, California, in June 2014.
FUNDING
This study was supported by a grant from the National Institute on Drug Abuse (R01 DA034091-01).
GLOSSARY
- Compassion centers
Places for patients who have qualifying conditions to obtain medical marijuana as allowed by state law
- Cultivation
The planting and harvesting of medical marijuana plants
- Delphi technique/process
Technique for achieving a convergence and consensus of opinion from a panel of experts
- Dispensary
Facility that prepares and sells medical marijuana
- Heterogeneity
Assortment or variety
- Latent class analysis
Subset of structural equation modeling, used to find groups or subtypes of cases in multivariate categorical data
- Marijuana Policy Project (MPP)
Organization founded in January 1995 focused on ending marijuana prohibition. MPP monitors and analyzes all marijuana-related bills in all 50 states and the District of Columbia
- Medical marijuana
Medical cannabis, or medical marijuana, refers to the use of cannabis and its cannabinoids to treat disease or improve symptoms
- National Survey on Drug Use And Health (NSDUH)
The NSDUH provides national and state-level data on the use of tobacco, alcohol, illicit drugs (including non-medical use of prescription drugs) and mental health in the United States. NSDUH is sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA) an agency in the U.S. Department of Health and Human Services (DHHS).
- Procon
ProCon.org is a nonpartisan, nonprofit website that presents research, studies, and pro and con statements on questions related to whether or not marijuana should be a medical option.
- Taxonomy
The practice and science of the classification of concepts
Footnotes
DECLARATION OF INTEREST
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the article.
Contributor Information
Susan A. Chapman, Department of Social and Behavioral Sciences, University of California, San Francisco, California, USA
Joanne Spetz, Department of Social and Behavioral Sciences, University of California, San Francisco, California, USA.
Jessica Lin, School of Public Health, University of Michigan, Ann Arbor, Michigan, USA.
Krista Chan, University of California, San Francisco, California, USA.
Laura A. Schmidt, Department of Anthropology, University of California, San Francisco, California, USA
REFERENCES
- Anderson D, Hansen B, Rees DI. Medical marijuana laws, traffic fatalities, and alcohol consumption. Journal of Law and Economics. 2013;56(2):333–369. [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the united states, 1999-2010. JAMA Internal Medicine. 2014;174(10):1668–1673. doi: 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benac N. Us becoming more accepting of medical marijuana. Canadian Medical Association Journal. 2013;185(16):E745–746. doi: 10.1503/cmaj.109-4612. doi: 10.1503/cmaj.109-4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug and Alcohol Dependence. 2012;120(1):22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu YW. Medical marijuana laws and illegal marijuana use. Economics Michigan State University; Michigan: 2012. SSRN 2164478 Working Paper. [DOI] [PubMed] [Google Scholar]
- Crombie N. Medical marijuana bill passes Oregon house, now goes to governor. The Oregonian. 2013 Jul 6; Retrieved from http://www.oregonlive.com/politics/index.ssf/2013/07/medical_marijuana_bill.html.
- Dalkey N, Helmer O. An experimental application of the delphi method to the use of experts. Management Science. 1963;9(3):458–467. [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Maturing out of alcohol dependence: The impact of transitional life events. J Stud Alcohol. 2006;67(2):195–203. doi: 10.15288/jsa.2006.67.195. [DOI] [PubMed] [Google Scholar]
- Drummer OH, Gerostamoulos J, Batziris H, Chu M, Caplehorn J, Robertson MD, Swann P. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239–248. doi: 10.1016/s0001-4575(02)00153-7. [DOI] [PubMed] [Google Scholar]
- Dyer O. The growth of medical marijuana. BMJ. 2013;347:f4755. doi: 10.1136/bmj.f4755. doi: 10.1136/bmj.f4755. [DOI] [PubMed] [Google Scholar]
- Freisthler B, Kepple NJ, Sims R, Martin SE. Evaluating medical marijuana dispensary policies: Spatial methods for the study of environmentally-based interventions. American Journal of Community Psychology. 2013;51(1-2):278–288. doi: 10.1007/s10464-012-9542-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta UG, Clarke RE. Theory and applications of the delphi technique: A bibliography (1975–1994). Technological Forecasting and Social Change. 1996;53(2):185–211. doi: http://dx.doi.org/10.1016/S0040-1625(96)00094-7. [Google Scholar]
- Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(3):207–212. doi: 10.1016/j.annepidem.2011.12.002. doi: 10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Hicks K, Ziegler RG. Developing trends in medical marijuana regulations. Public Law Journal. 2013;36(3):15–21. [Google Scholar]
- Hsu CC, Sandford BA. The delphi technique: Making sense of consensus. Practical Assessment, Research, and Evaluation. 2007;12(10):1–8. [Google Scholar]
- Hunt P, Miles JNV, Boustead A. Understanding patterns in medical marijuana laws: A latent class and transition analysis. RAND Corporation; Santa Monica, CA: 2013. [Google Scholar]
- Karlsson T, Österberg E. A scale of formal alcohol control policy in 15 european countries. Nordic Studies on Alcohol and Drugs. 2001;18(English Supplement):117–131. [Google Scholar]
- Karlsson T, Österberg E. Scaling alcohol control policies across europe. Drugs: Education, Prevention, and Policy. 2007;14(6):499–511. [Google Scholar]
- Kepple NJ, Freisthler B. Exploring the ecological association between crime and medical marijuana dispensaries. Journal of Studies on Alcohol and Drugs. 2012;73(4):523. doi: 10.15288/jsad.2012.73.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatapoush S, Hallfors D. “Sending the wrong message”: Did medical marijuana legalization in California change attitudes about and use of marijuana? Journal of Drug Issues. 2004;34(4):751–770. doi: 10.1177/002204260403400402. [Google Scholar]
- Landeta J. Current validity of the delphi method in social sciences. Technological Forecasting and Social change. 2006;73(5):467–482. [Google Scholar]
- Levy S. Effects of marijuana policy on children and adolescents. JAMA Pediatrics. 2013;167(7):600–602. doi: 10.1001/jamapediatrics.2013.2270. [DOI] [PubMed] [Google Scholar]
- Marijuana Policy Project (MPP) [2014, April 17];State by state medical marjiuana laws. 2013 2013, from https://www.mpp.org/issues/medical-marijuana/state-by-state-medical-marijuana-laws/state-by-state-medical-marijuana-laws-report/
- Michtalik HJ, Pronovost PJ, Marsteller JA, Spetz J, Brotman DJ. Developing a model for attending physician workload and outcomes. JAMA Internal Medicine. 2013;173(11):1026–1028. doi: 10.1001/jamainternmed.2013.405. [DOI] [PubMed] [Google Scholar]
- Ogborne AC, Smart RG, Adlaf EM. Self-reported medical use of marijuana: A survey of the general population. Canadian Medical Association Journal. 2000;162(12):1685–1686. [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Grossman M, Chaloupka FJ, O'Malley PM, Johnston L, Farrelly MC. Marijuana and youth. In: Gruber J, editor. Risky Behavior Among Youths: An Economic Analysis. University of Chicago Press; Chicago: 2001. pp. 271–326. [Google Scholar]
- Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: The devil is in the details. Journal of Policy Analysis and Management. 2015;34(1):7–31. doi: 10.1002/pam.21804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Sevigny EL. Marijuana liberalization policies: Why we can't learn much from policy still in motion. Journal of Policy Analysis and Management. 2014;33(1):212–221. doi: 10.1002/pam.21726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Miles JNV, Ewing BA, Shih RA, Tucker JS, D’Amico EJ. A longitudinal examination of alcohol, marijuana, and cigarette perceived norms among middle school adolescents. Drug and Alcohol Dependence. 2013;133(2):647–653. doi: 10.1016/j.drugalcdep.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C, Nicholas M. Critical reflections on the rise of qualitative research. BMJ. 2009;339 doi: 10.1136/bmj.b3425. [Google Scholar]
- Procon [2014 Apr 17];21 legal medical marijuana states and DC. 2015 from http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881.
- Seago JA, Spetz J, Chapman S, Dyer W, Grumbach K. Supply, demand and use of licensed practical nurses. Center for California Health Workforce Studies, University of California; San Francisco: 2004. [Google Scholar]
- Thurstone C, Lieberman SA, Schmiege SJ. Medical marijuana diversion and associated problems in adolescent substance treatment. Drug and Alcohol Dependence. 2011;118(2):489–492. doi: 10.1016/j.drugalcdep.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall MM, Poh E, Cerda M, Keyes KM, Galea S, Hasin DS. Commentary on Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(7):536–537. doi: 10.1016/j.annepidem.2012.03.003. doi: 10.1016/j.annepidem.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]