Abstract
It is widely agreed that emotion regulation plays an important role in many psychological disorders. We make the case that emotion regulation is in fact a key transdiagnostic factor, using the Research Domain Criteria (RDoC) as an organizing framework. In particular, we first consider how transdiagnostic and RDoC approaches have extended categorical views. Next, we examine links among emotion generation, emotion regulation, and psychopathology, with particular attention to key emotion regulation stages including identification, strategy selection, implementation, and monitoring. We then propose that emotion regulation be viewed as a sixth domain in the RDoC matrix, and provide a brief overview of how the literature has used the RDoC units of analyses to study emotion regulation. Finally, we highlight opportunities for future research and make recommendations for assessing and treating psychopathology.
Efforts to classify psychopathology in the United States date back to the mid-19th century, when the need for information on the prevalence of different forms of psychopathology became salient. By 1880, seven categories of mental illness had been identified (Wines, 1888). In 1952, the American Psychiatric Association published the first Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 1952) and, like its four successors (American Psychiatric Association, 1968, 1980, 1994, 2013), it was based on a categorical conceptualization of psychopathology. More specifically, the DSM in its various incarnations has consistently conceptualized psychopathology as somewhat overlapping, yet distinct, clusters of signs and symptoms; for example, the diagnostic criteria of generalized anxiety disorder (GAD) and major depressive disorder (MDD) share four symptoms (Zbozinek et al., 2012).
This emphasis on categorical distinctions among disorders has meant that assessment, training, research, and treatment have largely been couched within a disorder-specific framework, resulting in many researchers and clinicians identifying as experts in a specific disorder or set of disorders (e.g., an eating disorders researcher focuses on developing better treatments for eating disorders). However, a growing body of evidence has begun to reveal the overlap among disorders, highlighting elements and processes that cut across disorders. For decades, emotion regulation has been explored as an important process in the onset and maintenance of various forms of psychopathology, yet only recently has it has been discussed as a transdiagnostic factor specifically (Aldao, 2012; Kring & Sloan, 2010). In the current article, we build upon this work and propose that emotion regulation be considered as a transdiagnostic factor that can be mapped directly onto the transdiagnostic framework proposed by the National Institutes of Mental Health (NIMH) —the Research Domain Criteria (RDoC).
From Transdiagnostic Theory to the RDoC Framework
Transdiagnostic theory aims to identify transdiagnostic factors, or constructs that play a role in the onset and/or maintenance of several (or many) different disorders. Traditionally, risk factors have been studied within the context of a specific disorder. For example, risk factors that increase the likelihood of developing MDD are studied primarily within individuals who meet diagnostic criteria for MDD. However, consistent with transdiagnostic theory, there is evidence that risk factors for one specific disorder may also confer risk for other disorders—especially those that are highly comorbid or share symptoms. For example, intolerance of uncertainty (i.e., a predisposition to react negatively to uncertain situations) has been posited as a risk factor for a variety of disorders including GAD, MDD, and obsessive-compulsive disorder (OCD; Gentes & Ruscio, 2011). Therefore, it has been suggested that rather than examining risk factors for each specific disorder in turn, a more fruitful approach to understanding psychopathology would be to focus on transdiagnostic factors that can contribute to the development and maintenance of various forms of psychopathology (e.g., Aldao, Nolen-Hoeksema, & Schweizer, 2010; Buckholtz & Meyer-Lindenberg, 2012). A corollary of this suggestion is that treatments that target shared features of multiple disorders should be developed. This approach has been incorporated into several psychosocial treatments, such as the Unified Protocol for the Treatment of Emotional Disorders (Barlow, Allen, & Choate, 2004).
A number of transdiagnostic factors have now been identified, including: negative and positive affect (e.g., Brown, Chorpita, & Barlow, 1998; Clark & Watson, 1991), repetitive negative thinking (e.g., McEvoy, Watson, Watkins, & Nathan, 2013), neuroticism (e.g., Barlow, Sauer-Zavala, Carl, Bullis, & Ellard, 2014; Rosellini & Brown, 2011), experiential avoidance (e.g., Chawla & Ostafin, 2007; Spinhoven, Drost, de Rooij, van Hemert, & Penninx, 2014), and sleep disturbances (e.g., Harvey, Murray, Chandler, & Soehner, 2011). Although the identification of various transdiagnostic factors is a helpful first step in better understanding the transdiagnostic nature of psychopathology, one disadvantage of this divide-and-conquer approach is that the end result is an unorganized list of transdiagnostic factors. Taken together, the above list highlights the need for a unifying framework.
The NIMH, in support of transdiagnostic theory, created the RDoC (Insel et al., 2010), a framework that conceptualizes mechanisms underlying psychopathology in terms of constructs grouped into five overarching domains (negative valence systems, positive valence systems, cognitive systems, systems for social processes, and arousal and regulatory systems) that can be assessed across seven different levels of analysis (see Table 1). The negative valence systems domain (row 1) captures processes related to constructs such as threat and loss, whereas the positive valence systems domain (row 2) captures processes related to constructs such as approach motivation and reward learning. The cognitive systems domain (row 3) contains constructs such as attention, perception, and memory, whereas the systems for social processes domain (row 4) captures constructs such as social communication and perception and understanding of self and others. Finally, the arousal and regulatory systems domain (row 5) contains constructs such as sleep-wake and cardiac activity. The RDoC framework encourages each of these domains to be assessed and measured via several units of analysis, including genes (e.g., DRD2, 5HTR), molecules (e.g., dopamine and serotonin), cells (e.g., neurons and pituitary hormones), circuits (e.g., amygdala), physiology (e.g., heart rate and skin conductance), behavior (e.g., working memory tasks, behavioral assessments), self-report (e.g., questionnaires and interview-based scales), and paradigms (e.g., fear conditioning).
Table 1. Original Five-Domain Research Domain Criteria (RDoC) Matrix.
| Domain | Genes | Molecules | Cells | Circuits | Physiology | Behavior | Self-Report | Paradigms |
|---|---|---|---|---|---|---|---|---|
| Negative Valence Systems | ||||||||
| Positive Valence Systems | ||||||||
| Cognitive Systems | ||||||||
| Social Processes | ||||||||
| Arousal and Regulatory Systems |
Note. See (http://www.nimh.nih.gov/research-priorities/rdoc/constructs/rdoc-matrix.shtml) for full matrix.
The five overarching domains in the RDoC matrix were selected after deliberations among members of an internal NIMH working group, and according to Cutherbert and Insel (2013), “were conceived on empirical grounds from such diverse research areas as temperament, behavior genetics and structural mental models of mental disorders” (p. 4). These authors emphasize that this matrix is meant to develop over time, noting that “the RDoC framework is explicitly intended to be a moving target, and [that] the framework should grow and change with the pace of new research findings” (p. 7). Indeed, these five domains—although an excellent starting point—are unlikely to represent an exhaustive list of all relevant domains. Rather, as the RDoC authors highlight, the five domains serve as core building blocks for future research, especially research focusing on the functional interrelationships among these five domains.
In the sections that follow, we highlight the importance and relevance of emotion regulation to the transdiagnostic literature by discussing a specific framework of emotion regulation that can, in turn, be incorporated into the RDoC matrix. In this article, our specific goals are to: (a) clearly define important terms such as emotion and emotion regulation, (b) discuss the relationships among emotion, emotion regulation, and psychopathology, and (c) begin the discussion of integrating emotion regulation into the RDoC matrix. More specifically, we propose conceptualizing emotion regulation as a new, sixth domain in the RDoC matrix. Throughout, we highlight exciting opportunities for continued research and potential areas for refinement in the assessment and treatment of psychopathology.
Emotion, Emotion Regulation, and Psychopathology
Emotions involve loosely coupled changes in subjective experience, expressive behavior, and physiological responses (Mauss, Levenson, McCarter, Wilhelm, & Gross, 2005). Emotions differ in their intensity, duration, frequency, and type, and the process by which emotions are generated may be usefully described in four steps: (1) encountering an emotionally-relevant situation, (2) directing attention toward the emotionally-relevant situation, (3) evaluating and interpreting the emotionally-relevant situation, and (4) having an emotional response comprised of experiential, behavioral, and physiological components (Gross & Jazaieri, 2014).
Emotion regulation refers to the activation of a goal to influence emotion generation (Gross & Jazaieri, 2014; Gross, Sheppes, & Urry, 2011) and can occur at the intrapersonal level or the interpersonal level; the latter is also termed social regulation (Reeck, Ames, & Ochsner, 2016) or interpersonal emotion regulation (e.g., Zaki & Williams, 2013). Across both intrapersonal and interpersonal levels, emotion regulation can take place at any stage throughout the emotion generative process: upon encountering the emotionally-relevant situation, when directing attention toward the emotionally-relevant situation, when evaluating and interpreting the emotionally-relevant situation, and when having an emotional response.
Emotion dysregulation occurs when such a process has failed to influence emotion generation in the desired way, and can take two forms: emotion-regulation failure (i.e., not engaging in emotion regulation when it would be helpful to do so) or emotion misregulation (i.e., using a form of emotion regulation that is poorly matched to the situation; Gross, 2013). While psychopathology has long been considered to be a moderator of effective emotional responding (e.g., Seeley et al., this issue), it is important to note that difficulties with emotional responding (as characterized by problematic emotion intensity, duration, frequency, and type) do not necessarily signify difficulties with regulating emotion. For example, an individual may report intense negative emotions, such as fear, and yet also employ adaptive regulation of this fear, such that the heightened emotional intensity does not result in any dysfunction or impairment.
One model for conceptualizing how emotion regulation occurs is the extended process model of emotion regulation (Gross, 1998b; Gross, 2015; Sheppes, Suri, & Gross, 2015). This model posits that emotion regulation occurs via a four-stage process that includes: (1) identifying emotions that need regulating, (2) selecting an emotion regulation strategy, (3) implementing the selected strategy, and (4) monitoring the implemented strategy over time to determine if further modification is necessary. In addition to providing a framework for understanding how emotion regulation unfolds in real time, the extended process model allows for the relationship between emotion regulation and psychopathology to be explored in terms of stage-specific difficulties.
Difficulties with Identification
Whether or not emotion regulation will occur is determined in the identification stage (Sheppes et al., 2015). At this stage, the difference (if any) between the current emotional response and the desired emotional response is considered, as the individual determines whether to regulate the current emotional response. Difficulties in the identification stage have been associated with different forms of psychopathology. For example, individuals who meet criteria for Bipolar I disorder, when in a manic state, typically report feelings of euphoria and, as a result, are less likely to be interested in downregulating their emotional state; in other words, their emotion regulation goal would be to increase or maintain feelings of euphoria (rather than decreasing the intensity or duration of the euphoria). It is crucial to note that the goals an individual sets for a particular instance of emotion regulation are paramount in determining the extent of success of employing emotion regulation. Take for example two individuals who experience anxiety: Person A's goal is to avoid the experience of anxiety at all costs, and Person B's goal is to expose himself to anxiety to practice tolerating it. If both of these individuals find themselves in an anxiety-provoking situation, the selection of an emotion regulation strategy will heavily depend on the goal. Person A may wish to utilize suppression to successfully achieve his goal, whereas use of suppression for Person B may result in not achieving his goal. Thus, the goal selected for emotion regulation purposes, coupled with the selected strategy and implementation of the strategy, determine emotion regulation success.
To date, the majority of empirical research within the field of emotion regulation has largely ignored the person's specific goal in a given situation when regulating emotion; generally the assumption has been made that an individual's emotion regulatory goals are simply to downregulate negative emotions and upregulate positive emotions. However, we know that for many people under many circumstances (and from a variety of cultural backgrounds), maintaining or enhancing negative emotions and decreasing positive emotions may be consistent with their regulatory goals. For example, theoretical and empirical research with individuals with borderline personality disorder (BPD) who experience invalidating environments suggest that these individuals sometimes adopt the goal of upregulating negative emotion to meet the longer term goal of communicating their pain to others (Linehan, 1993). In the context of interpersonal emotion regulation within the identification stage, Zaki and Williams (2013) recently proposed a framework for studying interpersonal emotion regulation that differentiates such regulation according to whether an individual is attempting to alter his own or another's emotion.
Difficulties with Strategy Selection
Recent studies have explored the relationship between problematic selection of emotion-regulation strategies and psychopathology (Aldao et al., 2010). For example, Blalock, Kashdan, and Farmer (this issue) found a pattern of maladaptive strategy choice in individuals with social anxiety disorder (SAD) who had higher levels of suppression of positive and negative emotions and lower levels of reappraisal. Naumann and colleagues (this issue) found that in the context of sadness, women with anorexia and bulimia nervosa (vs. controls) had a greater tendency to employ rumination and suppression and lower tendency to employ acceptance. In another study, Van Meter and Youngstrom (this issue) found that depression was more related to the failure to select an appropriate emotion regulation strategy, with a greater tendency to select strategies such as rumination and a reduced tendency to select strategies such as acceptance and positive reappraisal.
The examination of emotion regulation strategy selection as it relates to psychopathology has been extended to child and adolescent samples. For example, Heleniak and colleagues (this issue) found that child maltreatment was significantly and positively associated with rumination and brooding. In another study, Shapero, Abramson, and Alloy (this issue) examined the interaction between emotion regulation strategies (suppression and reappraisal) and emotional reactivity in predicting internalizing symptoms during adolescence. Results indicated that higher levels of trait cognitive reappraisal (but not suppression) were associated with reduced association between higher levels of trait emotional reactivity and depressive (but not anxiety) symptoms.
As with identification, difficulties in the context of interpersonal emotion regulation can occur at the strategy selection stage as well. For example, Dixon-Gordon and colleagues (this issue) examined the main and interactive effects of maternal interpersonal emotion regulation on adolescent girls' BPD symptoms. Using a behavioral study in which girls diagnosed with BPD had a video-recorded (and then observer coded) conflict conversation with their mothers, these authors found that maternal problem-solving in the absence of support/validation in response to adolescent girls' high expressed negative affect was associated with greater BPD severity. One extension of this work is examining how individuals typically use other people to regulate their own emotions. For example, Hofmann, Carpenter, and Curtiss (this issue) developed a new measure to assess how individuals utilize others to regulate their own emotions, the Interpersonal Emotion Regulation Questionnaire (IERQ). They identified four factors underlying interpersonal emotion regulation: enhancing positive affect (seeking out others to increase feelings of joy), perspective taking (using others to be reminded not to worry and that others have it worse), social support (seeking out others for comfort and sympathy), and social modeling (looking to others to see how they might cope with a given situation). They found that individuals who reported more difficulty with regulating negative emotions in general also tended to report greater use of interpersonal emotion regulation strategies, suggesting that they may more frequently look to others to regulate their emotions rather than regulating emotions independently.
Difficulties with Implementation
During the implementation stage of the extended process model of emotion regulation, the specific emotion regulation strategy that has been selected is implemented. As with the identification and selection stages, difficulties with implementation have also been found to relate to psychopathology. For example, there is evidence that depressed individuals have an impaired ability to recall happy memories to repair sad mood (e.g., Joormann & Siemer, 2004; Joormann, Siemer, & Gotlib, 2007). Thus, while these individuals have identified an emotion regulation goal (i.e., to repair sad mood) and have selected a strategy (i.e., to recall happy memories), they experience difficulties with the actual implementation of their selected strategy.
When considering implementation, it is important to consider the role of emotion regulation flexibility (Aldao, Sheppes, & Gross, 2015). The concept of emotion regulation flexibility is important because people vary in the extent to which they use emotion regulation strategies in response to different situations that in turn vary on a variety of dimensions (e.g., intensity, valence, etc.). Aldao and colleagues define emotion regulation flexibility as “the degree of covariation between emotion regulation variability and changes in the environment, where the environment might consist of external events and/or appraisals of emotional reactions to such events” (p. 268). Because psychological disorders are typically characterized by a prioritization of short-term goals (e.g., avoidance) that provide immediate relief (e.g., anxiety reduction) over longer-term goals that might result in greater well-being (e.g., building mastery over difficult situations), it is important to consider the relationship between psychopathology and emotion regulation flexibility, and potentially consider emotion regulation flexibility as an area to target in treatment.
For example, some forms of psychopathology are associated with decreased flexibility in strategy selection; in other words, individuals may exhibit a preference for selecting a particular set of emotion regulation strategies rather than flexibly selecting strategies according to what would be most adaptive in that specific context. An example of decreased flexibility of emotion regulation can be seen in the context of rituals in individuals with OCD: When experiencing an anxiety-provoking trigger, these individuals tend to engage in ritualized behavior to minimize anxiety, and may prefer this particular strategy to other emotion regulation strategies such as reappraisal or engagement with the anxiety-provoking stimulus (e.g., Wang & Bello, 2006).
Difficulties with Monitoring
At the monitoring stage, individuals decide whether to stop regulating, switch their regulation strategy, or adjust some aspect of their selected strategy (Sheppes et al., 2015). It is in the monitoring stage that one can notice that prioritizing short-term goals (e.g., avoidance) over longer-term goals (e.g., gaining skills to manage difficult emotions) is ineffective, a realization that affords the opportunity to modify either the regulation goal or the regulation strategy. Failures to stop a maladaptive strategy or to switch from a maladaptive or inefficient strategy to a more adaptive and efficient one are associated with various forms of psychopathology.
For example, depressed individuals are more likely to employ rumination as an emotion regulation strategy, which is known to negatively affect mood (Nolen-Hoeksema, 2000). Failure to stop rumination once it has started may lead to negative downstream effects, such as increased depressed mood and increased ratings of the self as worthless and incompetent (Nolen-Hoeksema, Morrow, & Fredrickson, 1993; Rimes & Watkins, 2005). Difficulties with monitoring can also occur with other forms of psychopathology, such as substance use disorder. Several studies have investigated the comorbidity between depression and alcohol-related problems (e.g., Holahan, Moos, Holahan, Cronkite, & Randall, 2003), which has led to the proposal of several potential contributors to this relationship, including the drinking to cope explanation, whereby individuals engage in problematic drinking to cope with emotional distress (Abbey, Smith, & Scott, 1993). Viewed within the emotion regulation framework, drinking in an effort to cope with emotional distress specifies that individuals may choose consuming alcohol as their preferred emotion regulation strategy. Taken together with other studies showing that emotion regulation-relevant processes such as impulse control difficulties as well as difficulties engaging in goal-directed behavior are positively associated with number of alcohol-related consequences (e.g., interpersonal problems, blackout drinking; Dvorak et al., 2014), it appears as though individuals who drink to cope may be experiencing difficulties with the monitoring stage of emotion regulation. More specifically, once they have selected their strategy (drinking) and have implemented it and are experiencing some relief (emotion regulatory goal), there is a point during the monitoring stage at which it would be beneficial to stop or switch strategies, as continuing to drink can lead to dangerous outcomes such as blackout drinking and alcohol poisoning, among other negative consequences; failure to do so, whether because of the individual's difficulty with properly monitoring his or her emotion regulation strategy or because alcohol itself may inhibit proper monitoring, can result in the serious negative consequences described above (e.g., Dvorak et al.).
Emotion Regulation as a New RDoC Domain
The five RDoC domains (negative valence systems, positive valence systems, cognitive systems, systems for social processes, and arousal and regulatory systems) are usually discussed as separate systems. However, we believe that the functional relationships among these domains should be explicitly considered, in part because such relationships may give rise to other domains that are inherently more complex than the simple sum of the five more molecular domains. An analogy is that of a car: A car is comprised of many parts, and can be described as the sum of all of these parts stored together in a single, transportable unit. However, the main function of a car—to transport an individual to a desired location—only occurs when these parts interact with each other to create movement. Similarly, the process of emotion regulation cannot be fully appreciated as the simple sum of the five existing RDoC domains, rather it is a unique, affective regulatory process that may be best conceptualized as a new, sixth domain in the RDoC matrix. In other words, emotion regulation is the functional consequence of patterns of interaction among the five existing more molecular RDoC domains—an emergent construct. This idea is illustrated in Figure 1.
Figure 1. Emotion Regulation as a Sixth RDoC Domain.
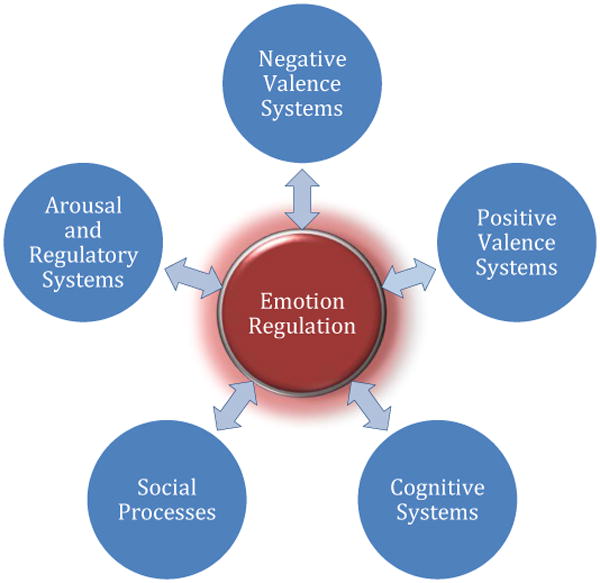
More specifically, we propose that, in the case of intrapersonal emotion regulation, the constructs within the cognitive systems domain regulate the negative valence, positive valence, and arousal systems. In the case of interpersonal emotion regulation, the systems for social processes domain regulates the negative valence, positive valence, cognitive, and arousal systems. Unlike RDoC constructs (Cuthbert & Insel, 2013), to the best of our knowledge, there are no clear criteria for proposing and testing new RDoC domains. However, we believe that new domains should meet several clear, empirically based criteria. From our perspective, these include being: (1) relevant to multiple disorders (i.e., transdiagnostic) as well as to the full range of normal functioning, (2) not reducible to the more basic (already existing) RDoC domains, and (3) empirically grounded across all of the RDoC units of analysis. Emotion regulation satisfies these three criteria and, thus, appears to be a suitable candidate for a sixth RDoC domain.
To illustrate this idea, consider Jay, who is very anxious about public speaking. Today, Jay is delivering an important presentation to a room full of people. Midway through his presentation he notices a lady in the audience giving him a disapproving look. Jay's attention and perception (cognitive systems) are in rapid exchange as he determines whether to keep his gaze fixed on the lady and how to interpret the look on her face. He may even use memory-related systems (cognitive systems) to recall whether he has encountered this lady or a similar situation like this before. At some point in this process, Jay might feel a decrease in his excitement (positive valence systems), and increases in his anxiety (negative valence systems) and sympathetic nervous system activation, such as rapid heartbeat and beads of sweat forming on his forehead (arousal and regulatory systems). Perhaps next, on some level, the disapproving audience member will be identified as either an acute or potential threat (negative valence systems). But Jay is still giving an important presentation, and he must find a way to regulate this cascade of emotions so that he can finish his presentation.
Jay has many options at this point to regulate his emotions in order to finish his presentation. In the selection and implementation stages, Jay may decide to intervene at the level of his attention (cognitive systems), and he may decide to avert his gaze away from the disapproving audience member to a positive or neutral looking audience member. Alternatively, he might remind himself of how supportive his boss has been lately, and how he has encouraged Jay to see each presentation as a learning opportunity (systems for social processes). He may decide to regulate his respiratory rate by inhaling through his nose and exhaling fully through his mouth so that his heart rate will decelerate and so his throat doesn't dry up (arousal and regulatory systems). Jay may decide to intervene at the level of his thoughts, or perception of the situation (cognitive systems), and reappraise the situation and conclude the lady is thinking deeply about the material he is presenting, and not necessarily disapproving of it. He may decide to focus on increasing his positive affect (positive valence systems) and speak more enthusiastically about the material he is presenting, and/or he may decide to suppress his negative emotions (negative valence systems) and continue giving the presentation without making many changes. Should Jay opt to approach the situation from an interpersonal emotion regulation perspective, he may decide to try to change the lady's emotional state to be more positive by making eye contact and smiling directly at her (systems for social processes).
This simple example illustrates how emotion regulation may be analyzed in terms of a series of dynamic interactions among constructs from all five domains. To divide emotion regulation among the five domains would result in a series of pieces that are no longer emotion regulation, but rather parts of the emotion regulation process. In other words, it would be an engine, a tire, and a windshield wiper, but no longer a car. To more specifically consider what it might mean to introduce emotion regulation as a sixth domain in the RDoC matrix, we selectively review emotion regulation research at each of the levels of analysis in the RDoC matrix (see Table 2). It bears noting that Table 2 represents a preliminary version of emotion regulation as an RDoC domain for illustrative purposes only and is not intended to be exhaustive. In the subsections that follow, we highlight key findings for each level of analysis.
Table 2. Sample Depiction of Emotion Regulation as a Sixth RDoC Domain.
| Domain | Genes | Molecules | Cells | Circuits | Physiology | Behavior | Self-report | Paradigms |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Emotion Regulation |
5-HTT1-2 COMT3 Oxytocin receptor gene4 |
Dopamine5 Serotonin6-9 Oxytocin10 Cortisol10-12 |
Microglia13 Cytokines14 |
Amygdala15-17 PFCs18-20,58 ACC21-23 Insula24 |
Skin conductance25,26,
29-30 Respiration26,28-30 Finger pulse amplitude25-26,28-30 Heart rate25-34 Somatic activity25,26,29-30 Blood pressure28-30 Facial EMG31,38 EEG35-38 |
Impromptu speeches39 CO2 challenge40 Behavioral observation/coding systems26,41-42 |
ERQ43 DERS44 CERQ45 ERI46 ERP-R47 EROS48 IERQ49 TAS-2056-57 |
Picture reappraisal50 Film clips26,51-52 Emotional Stroop Tasks53-55 |
Note. 5-HTT=serotonin transporter gene; COMT=catechol-O-methyltransferase gene; PFC=prefrontal cortices; ACC=anterior cingulate cortex; EMG=electromyography; EEG=electroencephalogram; ERQ=Emotion Regulation Questionnaire; DERS = Difficulties in Emotion Regulation Scale; CERQ = Cognitive Emotion Regulation Questionnaire; ERI = Emotion Regulation Interview; ERP-R=Emotion Regulation Profile-Revised; EROS=Emotion Regulation of Others and Self; IERQ=Interpersonal Emotion Regulation Questionnaire;
(Gross, 1998a);
Genes
Within the gene unit of analysis, there has been a growing body of literature testing the relationship between certain genes and emotion regulation (see Canli, Ferri, & Duman, 2009, for a review). For example, Gilman and colleagues (2015) examined variation in the 5-HTTLPR and emotion responses to a task designed to spontaneously induce emotion regulation; they found that for individuals with two copies of the short allele of this gene, there was weakened downregulation of negative emotion, indicating that perhaps these individuals (relative to those without two copies of the short allele) are more vulnerable to affective disorders. In a separate study, Miu and colleagues (2013) found evidence for reappraisal as a mediator of the relationship between the 5-HTTLPR gene and social anxiety symptoms, such that individuals with two copies of the short allele reported increased social anxiety symptoms and decreased use of reappraisal.
Molecules
At the molecular level, several studies have explored the relationship between emotion regulation and molecules such as dopamine (e.g., Salgado-Pineda, Delaveau, Blin, & Nieoullon, 2005), serotonin (e.g., Canli & Lesch, 2007; Hariri & Holmes, 2006; Outhred et al., 2015), oxytocin (e.g., Quirin, Kuhl, & Dusing, 2011), and cortisol (e.g., Lam, Dickerson, Zoccola, & Zaldivar, 2009; Quirin et al., 2011). For example, in terms of serotonin, there is evidence that increasing an individual's amount of serotonin available for absorption via the administration of a selective serotonin reuptake inhibitor facilitates reappraisal of negative stimuli (Outhred et al., 2015), suggesting a close relationship between serotonin and emotion regulation strategies. Similarly, using the ultimatum game, Crockett and colleagues (2008) found that lowering 5-HT levels using acute tryptophan depletion modulated behavioral reactions to unfairness, such that individuals who received acute tryptophan depletion increased their rejection rates to unfair offers; in other words, “temporarily lowering 5-HT levels increased retaliation to perceived unfairness without affecting mood, fairness judgment, basic reward processing, or response inhibition” (p. 1739), providing evidence again for a direct link between serotonin and emotion regulation. Finally, Poon and colleagues (this issue) found that low cortisol reactivity and high emotion regulation difficulties tended to relate to higher substance use and externalizing symptoms, and high cortisol reactivity coupled with higher emotion regulation difficulties tended to relate to depressive (but not anxiety) symptoms.
Cells
Though research on cells specifically relating to emotion regulation is sparse, there is a body of research that sets the stage for investigation the role of cells such as microglia (Walker, Nilsson, & Jones, 2013) and cytokines (Miller, Capuron, & Raison, 2005) in emotion regulation. For example, in studies conducted on rats exposed to chronic stress or anxiety-provoking situations, there is evidence that stress-induced microglial disturbances may play a role in regulating emotional states (Hinwood, Morandini, Day, & Walker, 2012; Wohleb et al., 2011). In terms of cytokines, Miller, Capuron, and Raison (2005) have explored the ways in which psychological and physical stress influence emotion regulation through their association with immune activation of cytokines such as interferon-alpha.
Circuits
A large number of studies have now examined the neural correlates of various aspects of emotion regulation (e.g., Etkin, Büchel, & Gross, 2015; Kim & Hamann, 2007; Rive et al., 2013; Taylor & Liberzon, 2007; Ziv, Goldin, Jazaieri, Hahn, & Gross, 2013). Many circuit-based studies of emotion regulation have focused on brain regions such as the dorsolateral and ventrolateral prefrontal cortices (e.g., Buhle et al., 2014; Kohn et al., 2014; Ochsner, Bunge, Gross, & Gabrieli, 2002), anterior cingulate cortex (e.g., Etkin, Egner, Peraza, Kandel, & Hirsch, 2006a; Etkin, Prater, Hoeft, Menon, & Schatzberg, 2010; Etkin & Wager, 2007), amygdala (e.g., Banks, Eddy, Angstadt, Nathan, & Phan, 2007; Etkin & Schatzberg, 2011; Marusak, Martin, Etkin, & Thomason, 2015), and insula (e.g., Phillips, Drevets, Rauch, & Lane, 2003). Much of this research has focused on the downregulation of emotion-processing regions such as the amygdala by prefrontal systems in the context of negative emotion.
Physiology
The effects of emotion regulation on physiological measures have been studied using many different measures. For example, Gross (1998a) used physiological measures relating to sympathetic activation, somatic activity, and heart rate to assess the effects of the emotion regulation strategies of reappraisal and suppression. Results indicated a lack of elevations in physiological responding when participants reappraised, but increases in multiple indices of sympathetic nervous system activation when participants used suppression. These results are consistent with earlier findings showing suppression related to increased sympathetic nervous system activity, decreased somatic activity, decreased heart rate, and increased blinking (Gross & Levenson, 1993). Other studies have focused on physiological effects of emotion regulation strategies in specific contexts. For example the physiological consequences, measured via several different physiological indices (see the Physiology column of Table 2), of the effects of reappraisal on anger (Mauss, Cook, Cheng, & Gross, 2007), the effects of acceptance and suppression on negative and positive emotion pictures (Dan-Glauser & Gross, 2015), the effects of suppression on disgust (Roberts, Levenson, & Gross, 2008), the effects of reappraisal on amusement (Giuliani, McRae, & Gross, 2008), and the effects of unconscious reappraisal on a frustrating task (Yuan, Ding, Liu, & Yang, 2015), among many others. In terms of late positive potential (LPP), MacNamara, Kotov, and Hajcak (this issue) assessed the impact of emotional intensity on LPP, a neurobiological measure assessing event-related potential that is larger for emotion (vs. neutral) stimuli. They found that greater symptoms of MDD were associated with less emotional modulation of the LPP, and greater GAD symptomatology (controlling for MDD symptoms) was associated with greater negative potentiation of the LPP, suggesting that emotion dysregulation in GAD and MDD may stem from abnormal emotion generation (e.g., abnormal intensities of the emotions generated). Finally, Rosenthal and colleagues (this issue) investigated how individuals diagnosed with BPD reacted emotionally to personally-relevant (vs. standardized) sounds and found that individuals with BPD (vs. healthy controls) reported higher arousal and lower valence, and heightened skin conductance responses in response to personally-relevant unpleasant sounds.
Behavior
Behaviors are typically observed via performances on various tasks designed to elicit emotion and assess how individuals regulate such emotions. Weiss, Thomson, and Chan (2014) recently conducted a systematic literature review of emotion regulation measurement in individuals with autism spectrum disorder, and identified several measures of naturalistic observation of emotion regulation; for example, Jahromi, Meek, and Ober-Reynolds (2012) conducted a study in which coders coded for 12 emotion regulation strategies in 10-second intervals. Results indicated that children with autism employed more avoidance and venting strategies when faced with frustration. In another study, participants were asked to either reappraise, suppress, or accept their emotion experience after giving an impromptu speech; results indicated both reappraising and accepting anxiety were more effective for moderating physiological arousal than suppressing anxiety (Hofmann, Heering, Sawyer, & Asnaani, 2009). Finally, Levitt and colleagues (2004) conducted a study in which participants were exposed to a 5.5% carbon dioxide challenge and asked to either utilize suppression, acceptance, or neither (control). Results support acceptance as a potentially beneficial strategy for reducing both subjective anxiety and avoidance in individuals with panic disorder.
Self-Report
Self-report assessment tools are ubiquitous in the study of emotional regulation. A plethora of self-report questionnaires focusing on specific aspects of emotion regulation have been used, including questionnaires focusing on difficulties identifying emotions (e.g., Toronto Alexithymia Scale-20; Bagby, Parker, & Taylor, 1994; Bagby, Taylor, & Parker, 1994), emotion regulation strategies such as reappraisal and suppression (e.g., Emotion Regulation Questionnaire; Gross & John, 2003), and cognitive strategies such as self-blame, rumination and catastrophizing (e.g., the Cognitive Emotion Regulation Questionnaire; Garnefski & Kraaij, 2007). In addition to self-report, an emotion regulation interview was recently developed (Emotion Regulation Interview; Werner, Goldin, Ball, Heimberg, & Gross, 2011) that assesses the frequency and self-efficacy ratings of five strategies (avoid situations, modify situations, distraction, think about the situation differently, and hide visible signs of anxiety). Though there is a relative dearth of measures assessing interpersonal regulation, the IERQ is a recent example of one such measure (Hofmann et al., this issue). The only other measure assessing specifically interpersonal emotion regulation is the Emotion Regulation of Others and Self (Niven, Totterdell, Stride, & Holman, 2011) scale, which assesses four factors (cognitive improvement, behavioral improvement, cognitive worsening, and behavioral worsening) relating to four types of interpersonal emotion regulation strategies. Consistent with the RDoC approach (Cuthbert & Insel, 2013), emotion regulation has been assessed across the full range of functioning. In addition to studies of clinical samples, emotion regulation has also been studied in many normative, non-clinical samples (e.g., Gross & John, 2003; Manser, Cooper, & Trefusis, 2012).
Paradigms
Finally, the study of emotion regulation has incorporated several paradigms that typically involve an emotion induction component followed by an emotion regulation strategy implementation. For example, Gross (1998a) showed participants a film designed to elicit disgust, and then asked participants to either reappraise the situation, suppress their emotional reactions, or simply watch the film (control). Results indicated that both reappraisal and suppression reduced emotion-expressive behavior, and those who reappraised also had lesser increases in disgust experience while watching the film, whereas those who suppressed did not. In other studies (e.g., Sheppes, Scheibe, Suri, & Gross, 2011), pictures varying in emotion valence and intensity have been used to induce emotional states, including pictures from the International Affective Picture System (IAPS; Lang, Bradley, & Cuthbert, 2008).
Directions for Future Research, Assessment, and Treatment
Aldao (2016) has offered two main recommendations for researchers interested in links between emotion regulation and psychopathology. The first involves conducting studies that include more than one diagnostic group in an effort to identify whether any between group differences are due to psychopathology more generally or due to a specific condition. The second involves analyzing symptoms dimensionally in order to understand the relationship between symptoms and pathological processes. We concur, and in the following subsections, we consider more specific suggestions for future empirical research, assessment, and treatment.
Research
We have proposed that emotion regulation is a sixth domain in the RDoC framework, and we have illustrated how work on emotion regulation naturally populates the units of analysis in the RDoC matrix. However, much more remains to be done to investigate the many clinically relevant emotion regulation constructs at each of these levels of analysis. Several of the constructs we have discussed in this article that bear on each of the four main emotion regulation stages are viable candidates for constructs to populate the emotion regulation domain, but further empirical work is needed. For example, in the identification stage, an individual's ability to notice and label their own emotional states (i.e., emotion awareness) will likely affect his or her ability to identify an emotional goal. In the selection stage, an individual's ability to engage in a specific emotion regulation strategy such as cognitive reappraisal and suppression will likely affect his or her selection of a strategy. In the implementation stage, an individual's ability to tolerate distress—especially if a strategy that requires tolerance of acute, short-term distress is selected—will likely affect his or her ability to properly implement the selected strategy. And finally, in the monitoring stage, an individual's ability to remain mindful of his or her emotional experience will likely affect his or her ability to modify the experience if such modification is deemed necessary. Additionally, given our proposal that emotion regulation be considered as an RDoC domain that inherently incorporates interactions among other domains, a more direct assessment of each of these domains (and relevant constructs within domains) when assessing emotion regulation would facilitate a better understanding of the place of emotion regulation in the RDoC matrix.
We also encourage researchers to consider integrative study designs that utilize multiple units of analysis and multiple diagnostic groups. In terms of the variables under study, we encourage researchers to capture various aspects of emotion regulation (reflecting each of the emotion regulation processes discussed above), assess symptoms dimensionally, assess related transdiagnostic factors (e.g., sleep disturbance) to better understand how emotion regulation is influenced by and influences other factors, and consider incorporating a developmental perspective into theories about emotion regulation to help bridge the divide between the adult and child/adolescent bodies of research within emotion regulation research. We also encourage researchers to continue considering the effects of emotion regulation (and mental health more broadly) on physical health (e.g., Farris, Zvolensky, & Schmidt, this issue); such research would be nicely suited to the RDoC framework, given its inclusion of relevant biological constructs. It is of course highly unlikely that any single research study will achieve all of these goals simultaneously, but our hope is that each of these goals may be met as research in this area accumulates.
Assessment and Treatment
In terms of assessment, we encourage clinicians to consider the role of emotion regulation in an individual's psychopathology. Though a large portion of descriptions of disorders (40.3%) likely contain some form of affective disturbance, affective disturbance is specifically mentioned as part of the diagnostic criteria in far fewer disorders (19.3%; Jazaieri, Urry, & Gross, 2013). Consistent with transdiagnostic approaches to psychopathology, we encourage assessors to avoid overreliance of the diagnostic criteria to understand psychopathology and instead consider transdiagnostic factors that may be maintaining or exacerbating maladaptive behavior. Consistent with Aldao (2016) and the RDoC approach, we encourage researchers to adopt a dimensional and flexible perspective to symptoms. Whether through self-report questionnaires, interview questions specifically designed to assess emotion regulation, or documentation of behaviors and their consequences, consider how the individual's emotion goals, how he or she is attempting to reach such goals via emotion regulation, and whether such attempts are successful.
After assessing emotion regulation, we encourage clinicians to specify the type of emotion regulation difficulty that is occurring. Is the individual able to identify an emotion regulation goal that will lead to more adaptive outcomes (identification)? Is the individual able to select an emotion regulation strategy that is appropriate to the goal (selection)? Once the individual has selected a strategy, is he or she able to implement it effectively (implementation)? And once the individual is implementing a strategy, is he or she able to monitor the implementation and make any necessary modifications, including flexibly altering emotion regulation strategies to achieve a more beneficial long-term goal, rather than a short-term goal (monitoring)? The clinician could then follow-up with a more targeted approach to treatment with explicit skills training modules for the emotion regulatory deficits; for example, specific sections from the Emotion Regulation module in Dialectical Behavior Therapy (DBT; Linehan, 2015) skills training. As with research, obtaining a clear and specific understanding of where in the emotion regulation process the individual is struggling can yield powerful insights into the mechanisms maintaining psychopathology and will pave the way for more targeted, effective interventions and accompanying targeted assessments that can document the efficacy of the newly developed interventions.
Concluding Comment
We are excited to see the tremendous growth of emotion regulation research and its application to psychopathology, and we are particularly gratified to see the recent surge of studies investigating emotion regulation as a transdiagnostic construct. To better understand emotion regulation as a transdiagnostic construct, in this article we explored the links among emotion generation, emotion regulation, and psychopathology. We have argued that emotion regulation is a crucial new domain in the RDoC framework that reflects interactions among the other five domains. By reviewing the RDoC units of analysis, and providing an initial overview of how emotion regulation has been assessed using these units, we have sought to set the stage for future research further grounding the emotion regulation domain within the RDoC matrix. We have also highlighted avenues for future research focusing on ways in which emotion regulation can be more clearly brought into psychopathology research, assessment, and treatment.
Footnotes
Katya C. Fernandez, Ph.D., Hooria Jazaieri, M.A., & James J. Gross, Ph.D. declare that they have no conflict of interest.
Disclosures: Conflict of Interest: Authors declare that they have no conflict of interest.
Informed Consent: All procedures followed were in accordance with the ethical standards of the institutional review boards where the study was approved. Informed consent was obtained from all individual subjects participating in the study.
Animal Rights: No animal studies were carried out by the authors for this paper.
References
- Abbey A, Smith MJ, Scott RO. The relationship between reasons for drinking alcohol and alcohol consumption: An interactional approach. Addictive Behaviors. 1993;18:659–670. doi: 10.1016/0306-4603(93)90019-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao A. Emotion regulation strategies as transdiagnostic processes: A closer look at the invariance of their form and function. Revista de Psicopatologia y Psicologia Clinica. 2012;17:261–277. doi: 10.5944/rppc.vol.17.num.3.2012.11843. [DOI] [Google Scholar]
- Aldao A. Introduction to the special issue: Emotion regulation as a transdiagnostic process. Cognitive Therapy and Research. 2016 doi: 10.1007/s10608-016-9764-2. [DOI] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Aldao A, Sheppes G, Gross JJ. Emotion regulation flexibility. Cognitive Therapy and Research. 2015;39:263–278. doi: 10.1007/s10608-014-9662-4. [DOI] [Google Scholar]
- American Psychiatric Association. Mental Disorders: Diagnostic and Statistical Manual. American Psychiatric Association, Mental Hospital Service; 1952. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (Second Edition) 3rd. Washington, DC: American Psychiatric Association; 1968. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Bagby RM, Parker JDA, Taylor GJ. The twenty-item Toronto Alexithymia Scale: I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Taylor GJ, Parker JDA. The twenty-item Toronto Alexithymia Scale: II. Convergent, discriminant, and concurrent validity. Journal of Psychosomatic Research. 1994;38:33–40. doi: 10.1016/0022-3999(94)90006-X. [DOI] [PubMed] [Google Scholar]
- Banks SJ, Eddy KT, Angstadt M, Nathan PJ, Phan KL. Amygdala–frontal connectivity during emotion regulation. Social Cognitive Affective Neuroscience. 2007;2:303–312. doi: 10.1093/scan/nsm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/S0005-7894(04)80036-4. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, Ellard KK. The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science. 2014;2:344–365. doi: 10.1177/2167702613505532. [DOI] [Google Scholar]
- Baur R, Conzelmann A, Wieser MJ, Pauli P. Spontaneous emotion regulation: Differential effects on evoked brain potentials and facial muscle activity. International Journal of Psychophysiology. 2015;96:38–48. doi: 10.1016/j.ijpsycho.2015.02.022. [DOI] [PubMed] [Google Scholar]
- Blalock DV, Kashdan TB, Farmer AS. Trait and daily emotion regulation in social anxiety disorder. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9739-8. [DOI] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037/0021-843X.107.2.179. [DOI] [PubMed] [Google Scholar]
- Buckholtz JoshuaW, Meyer-Lindenberg A. Psychopathology and the human connectome: Toward a transdiagnostic model of risk for mental illness. Neuron. 2012;74:990–1004. doi: 10.1016/j.neuron.2012.06.002. [DOI] [PubMed] [Google Scholar]
- Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H, et al. Ochsner KN. Cognitive reappraisal of emotion: A meta-analysis of human neuroimaging studies. Cerebral Cortex. 2014;24:2981–2990. doi: 10.1093/cercor/bht154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canli T, Ferri J, Duman EA. Genetics of emotion regulation. Neuroscience. 2009;164:43–54. doi: 10.1016/j.neuroscience.2009.06.049. [DOI] [PubMed] [Google Scholar]
- Canli T, Lesch KP. Long story short: the serotonin transporter in emotion regulation and social cognition. Nature Neuroscience. 2007;10:1103–1109. doi: 10.1038/nn1964. [DOI] [PubMed] [Google Scholar]
- Chawla N, Ostafin B. Experiential avoidance as a functional dimensional approach to psychopathology: An empirical review. Journal of Clinical Psychology. 2007;63:871–890. doi: 10.1002/jclp.20400. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Crockett MJ, Clark L, Tabibnia G, Lieberman MD, Robbins TW. Serotonin modulates behavioral reactions to unfairness. Science. 2008;320(5884):1739. doi: 10.1126/science.1155577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Medicine. 2013;11:1–8. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dan-Glauser ES, Gross JJ. The temporal dynamics of emotional acceptance: Experience, expression, and physiology. Biological Psychology. 2015;108:1–12. doi: 10.1016/j.biopsycho.2015.03.005. [DOI] [PubMed] [Google Scholar]
- Dennis TA, Malone MM, Chen CC. Emotional face processing and emotion regulation in children: An ERP study. Developmental Neuropsychology. 2009;34:85–102. doi: 10.1080/87565640802564887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon-Gordon KL, Whalen DJ, Scott LN, Cummins ND, Stepp SD. The main and interactive effects of maternal interpersonal emotion regulation and negative affect on adolescent girls' borderline personality disorder symptoms. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9706-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorak R, Sargent E, Kilwein T, Stevenson B, Kuvaas N, Williams T. Alcohol use and alcohol-related consequences: Associations with emotion regulation difficulties. The American Journal of Drug and Alcohol Abuse. 2014;40:125–130. doi: 10.3109/00952990.2013.877920. [DOI] [PubMed] [Google Scholar]
- Etkin A, Büchel C, Gross JJ. The neural bases of emotion regulation. Nature Reviews Neuroscience. 2015;16:693–700. doi: 10.1038/nrn4044. [DOI] [PubMed] [Google Scholar]
- Etkin A, Egner T, Peraza DM, Kandel ER, Hirsch J. Resolving emotional conflict: A role for the rostral anterior cingulate cortex in modulating activity in the amygdala. Neuron. 2006a;51:871–882. doi: 10.1016/j.neuron.2006.07.029. [DOI] [PubMed] [Google Scholar]
- Etkin A, Egner T, Peraza DM, Kandel ER, Hirsch J. Resolving emotional conflict: A role for the rostral anterior cingulate cortex in modulating activity in the amygdala. Neuron. 2006b;51:871–882. doi: 10.1016/j.neuron.2006.07.029. [DOI] [PubMed] [Google Scholar]
- Etkin A, Prater KE, Hoeft F, Menon V, Schatzberg AF. Failure of anterior cingulate activation and connectivity with the amygdala during implicit regulation of emotional processing in generalized anxiety disorder. The American Journal of Psychiatry. 2010;167:545–554. doi: 10.1176/appi.ajp.2009.09070931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etkin A, Schatzberg AF. Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders. The American Journal of Psychiatry. 2011;168:968–978. doi: 10.1176/appi.ajp.2011.10091290. [DOI] [PubMed] [Google Scholar]
- Etkin A, Wager TD. Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. American Journal of Psychiatry. 2007;164:1476–1488. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris SG, Zvolensky MJ, Schmidt NB. Difficulties with emotion regulation and psychopathology interact to predict early smoking cessation lapse. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9705-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V. The Cognitive Emotion Regulation Questionnaire: Psychometric features and prospective relationships with depression and anxiety in adults. European Journal of Psychological Assessment. 2007;23:141–149. doi: 10.1027/1015-5759.23.3.141. [DOI] [Google Scholar]
- Gentes EL, Ruscio AM. A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive–compulsive disorder. Clinical Psychology Review. 2011;31:923–933. doi: 10.1016/j.cpr.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Gilman TL, Latsko M, Matt L, Flynn J, de la Cruz Cabrera O, Douglas D, et al. Coifman KG. Variation of 5-HTTLPR and deficits in emotion regulation: A pathway to risk? Psychology & Neuroscience. 2015;8:397–413. doi: 10.1037/pne0000017. [DOI] [Google Scholar]
- Giuliani NR, McRae K, Gross JJ. The up- and down-regulation of amusement: Experiential, behavioral, and autonomic consequences. Emotion. 2008;8:714–719. doi: 10.1037/a0013236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/b:joba.0000007455.08539.94. [DOI] [Google Scholar]
- Gross JJ. Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology. 1998a;74:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998b;2:271. [Google Scholar]
- Gross JJ. Emotion regulation: Taking stock and moving forward. Emotion. 2013;13:359–365. doi: 10.1037/a0032135. [DOI] [PubMed] [Google Scholar]
- Gross JJ. The extended process model of emotion regulation: Elaborations, applications, and future directions. Psychological Inquiry. 2015;26:130–137. doi: 10.1080/1047840X.2015.989751. [DOI] [Google Scholar]
- Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: An affective science perspective. Clinical Psychological Science. 2014;2:387–401. doi: 10.1177/2167702614536164. [DOI] [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Levenson RW. Emotional suppression: Physiology, self-report, and expressive behavior. Journal of Personality and Social Psychology. 1993;64:970–986. doi: 10.1037/0022-3514.64.6.970. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Levenson RW. Emotion elicitation using films. Cognition and Emotion. 1995;9:87–108. doi: 10.1080/02699939508408966. [DOI] [Google Scholar]
- Gross JJ, Sheppes G, Urry HL. Emotion generation and emotion regulation: A distinction we should make (carefully) Cognition and Emotion. 2011;25:765–781. doi: 10.1080/02699931.2011.555753. [DOI] [PubMed] [Google Scholar]
- Hariri AR, Holmes A. Genetics of emotional regulation: the role of the serotonin transporter in neural function. Trends in Cognitive Sciences. 2006;10:182–191. doi: 10.1016/j.tics.2006.02.011. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Murray G, Chandler RA, Soehner A. Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clinical Psychology Review. 2011;31:225–235. doi: 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heleniak C, Jenness JL, Vander Stoep A, McCauley E, McLaughlin KA. Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9735-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinwood M, Morandini J, Day TA, Walker FR. Evidence that microglia mediate the neurobiological effects of chronic psychological stress on the medial prefrontal cortex. Cerebral Cortex. 2012;22:1442–1454. doi: 10.1093/cercor/bhr229. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Carpenter JK, Curtiss J. Interpersonal emotion regulation questionnaire (IERQ): Scale development and psychometric characteristics. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-016-9756-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Heering S, Sawyer AT, Asnaani A. How to handle anxiety: The effects of reappraisal, acceptance, and suppression strategies on anxious arousal. Behaviour Research and Therapy. 2009;47:389–394. doi: 10.1016/j.brat.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope and alcohol use and abuse in unipolar depression: A 10-year model. Journal of Abnormal Psychology. 2003;112:159–165. doi: 10.1037/0021-843X.112.1.159. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Kozak M, Pine DS, et al. Wang P. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167 doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jahromi LB, Meek SE, Ober-Reynolds S. Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2012;53:1250–1258. doi: 10.1111/j.1469-7610.2012.02560.x. [DOI] [PubMed] [Google Scholar]
- Jazaieri H, Urry HL, Gross JJ. Affective disturbance and psychopathology: An emotion regulation perspective. Journal of Experimental Psychopathology. 2013;4:584–599. [Google Scholar]
- Joormann J, Siemer M. Memory accessibility, mood regulation, and dysphoria: Difficulties in repairing sad mood with happy memories? Journal of Abnormal Psychology. 2004;113:179–188. doi: 10.1037/0021-843X.113.2.179. [DOI] [PubMed] [Google Scholar]
- Joormann J, Siemer M, Gotlib IH. Mood regulation in depression: Differential effects of distraction and recall of happy memories on sad mood. Journal of Abnormal Psychology. 2007;116:484–490. doi: 10.1037/0021-843X.116.3.484. [DOI] [PubMed] [Google Scholar]
- Kim HS, Sherman DK, Mojaverian T, Sasaki JY, Park J, Suh EM, Taylor SE. Gene–culture interaction: Oxytocin receptor polymorphism (OXTR) and emotion regulation. Social Psychological and Personality Science. 2011;2:665–672. doi: 10.1177/1948550611405854. [DOI] [Google Scholar]
- Kim SH, Hamann S. Neural correlates of positive and negative emotion regulation. Journal of Cognitive Neuroscience. 2007;19:776–798. doi: 10.1162/jocn.2007.19.5.776. [DOI] [PubMed] [Google Scholar]
- Kohn N, Eickhoff SB, Scheller M, Laird AR, Fox PT, Habel U. Neural network of cognitive emotion regulation: An ALE meta-analysis and MACM analysis. Neuroimage. 2014;87:345–355. doi: 10.1016/j.neuroimage.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Sloan DM. Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. New York, NY: Guilford Press; 2010. [Google Scholar]
- Lam S, Dickerson SS, Zoccola PM, Zaldivar F. Emotion regulation and cortisol reactivity to a social-evaluative speech task. Psychoneuroendocrinology. 2009;34:1355–1362. doi: 10.1016/j.psyneuen.2009.04.006. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Bradley BN, Cuthbert BN. International Affective Picture System (IAPS): Affective ratings of pictures and instruction manual (Technical Report No A-8) Gainesville, FL: University of Florida; 2008. [Google Scholar]
- Levitt JT, Brown TA, Orsillo SM, Barlow DH. The effects of acceptance versus suppression of emotion on subjective and psychophysiological response to carbon dioxide challenge in patients with panic disorder. Behavior Therapy. 2004;35:747–766. doi: 10.1016/S0005-7894(04)80018-2. [DOI] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; New York, NY: 1993. [Google Scholar]
- Linehan MM. DBT® skills training manual. 2nd. Guilford Press; New York, NY: 2015. [Google Scholar]
- MacNamara A, Kotov R, Hajcak G. Diagnostic and symptom-based predictors of emotional processing in generalized anxiety disorder and major depressive disorder: An event-related potential study. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9717-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manser R, Cooper M, Trefusis J. Beliefs about emotions as a metacognitive construct: Initial development of a self - report questionnaire measure and preliminary investigation in relation to emotion regulation. Clinical Psychology & Psychotherapy. 2012;19:235–246. doi: 10.1002/cpp.745. [DOI] [PubMed] [Google Scholar]
- Marusak HA, Martin KR, Etkin A, Thomason ME. Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology. 2015;40:1250–1258. doi: 10.1038/npp.2014.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews A, MacLeod C. Selective processing of threat cues in anxiety states. Behaviour Research and Therapy. 1985;23:563–569. doi: 10.1016/0005-7967(85)90104-4. [DOI] [PubMed] [Google Scholar]
- Mauss IB, Cook CL, Cheng JYJ, Gross JJ. Individual differences in cognitive reappraisal: Experiential and physiological responses to an anger provocation. International Journal of Psychophysiology. 2007;66:116–124. doi: 10.1016/j.ijpsycho.2007.03.017. [DOI] [PubMed] [Google Scholar]
- Mauss IB, Levenson RW, McCarter L, Wilhelm FH, Gross JJ. The tie that binds? Coherence among emotion experience, behavior, and physiology. Emotion. 2005;5:175–190. doi: 10.1037/1528-3542.5.2.175. [DOI] [PubMed] [Google Scholar]
- McEvoy PM, Watson H, Watkins ER, Nathan P. The relationship between worry, rumination, and comorbidity: Evidence for repetitive negative thinking as a transdiagnostic construct. Journal of Affective Disorders. 2013;151:313–320. doi: 10.1016/j.jad.2013.06.014. [DOI] [PubMed] [Google Scholar]
- Miller AH, Capuron L, Raison CL. Immunologic influences on emotion regulation. Clinical Neuroscience Research. 2005;4:325–333. doi: 10.1016/j.cnr.2005.03.010. [DOI] [Google Scholar]
- Miu AC, Vulturar R, Chis A, Ungureanu L, Gross JJ. Reappraisal as a mediator in the link between 5-HTTLPR and social anxiety symptoms. Emotion. 2013;13:1012–1022. doi: 10.1037/a0033383. [DOI] [PubMed] [Google Scholar]
- Naumann E, Tuschen-Caffier B, Voderholzer U, Svaldi J. Spontaneous emotion regulation in anorexia and bulimia nervosa. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9723-3. [DOI] [Google Scholar]
- Nelis D, Quoidbach J, Hansenne M, Mikolajczak M. Measuring individual differences in emotion regulation: The Emotion Regulation Profile-Revised (ERP-R) Psychologica Belgica. 2011;51:49–91. doi: 10.5334/pb-51-1-49. [DOI] [Google Scholar]
- Nikolova YS, Davis EG, Hariri AR. Genetic Contributions to Affect and Emotion. In: Barrett LF, Haviland-Jones M, Lewis M, editors. Handbook of Emotions. 4th. New York: Guildford Press; 2014. [Google Scholar]
- Niven K, Totterdell P, Stride CB, Holman D. Emotion Regulation of Others and Self (EROS): The development and validation of a new individual difference measure. Current Psychology. 2011;30:53–73. doi: 10.1007/s12144-011-9099-9. [DOI] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109:504–511. [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J, Fredrickson BL. Response styles and the duration of episodes of depressed mood. Journal of Abnormal Psychology. 1993;102:20–28. doi: 10.1037//0021-843x.102.1.20. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Bunge SA, Gross JJ, Gabrieli JD. Rethinking feelings: An FMRI study of the cognitive regulation of emotion. Journal of Cognitive Neuroscience. 2002;14:1215–1229. doi: 10.1162/089892902760807212. [DOI] [PubMed] [Google Scholar]
- Outhred T, Das P, Felmingham KL, Bryant RA, Nathan PJ, Malhi GS, Kemp AH. Facilitation of emotion regulation with a single dose of escitalopram: A randomized fMRI study. Psychiatry Research: Neuroimaging. 2015;233:451–457. doi: 10.1016/j.pscychresns.2015.07.018. [DOI] [PubMed] [Google Scholar]
- Phillips ML, Drevets WC, Rauch SL, Lane R. Neurobiology of emotion perception I: The neural basis of normal emotion perception. Biological Psychiatry. 2003;54:504–514. doi: 10.1016/S0006-3223(03)00168-9. [DOI] [PubMed] [Google Scholar]
- Poon JA, Turpyn CC, Hansen A, Jacangelo J, Chaplin TM. dolescent substance use & psychopathology: Interactive effects of cortisol reactivity and emotion regulation. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9729-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quirin M, Kuhl J, Dusing R. Oxytocin buffers cortisol responses to stress in individuals with impaired emotion regulation abilities. Psychoneuroendocrinology. 2011;36:898–904. doi: 10.1016/j.psyneuen.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Reeck C, Ames DR, Ochsner KN. The social regulation of emotion: An integrative, cross-disciplinary model. Trends in Cognitive Sciences. 2016;20:47–63. doi: 10.1016/j.tics.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimes KA, Watkins E. The effects of self-focused rumination on global negative self-judgements in depression. Behaviour Research and Therapy. 2005;43:1673–1681. doi: 10.1016/j.brat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Rive MM, van Rooijen G, Veltman DJ, Phillips ML, Schene AH, Ruhé HG. Neural correlates of dysfunctional emotion regulation in major depressive disorder. A systematic review of neuroimaging studies. Neuroscience and Biobehavioral Reviews. 2013;37:2529–2553. doi: 10.1016/j.neubiorev.2013.07.018. [DOI] [PubMed] [Google Scholar]
- Roberts NA, Levenson RW, Gross JJ. Cardiovascular costs of emotion suppression cross ethnic lines. International Journal of Psychophysiology. 2008;70:82–87. doi: 10.1016/j.ijpsycho.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosellini AJ, Brown TA. The NEO Five-Factor Inventory: Latent structure and relationships with dimensions of anxiety and depressive disorders in a large clinical sample. Assessment. 2011;18:27–38. doi: 10.1177/1073191110382848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal MZ, Neacsiu AD, Geiger PJ, Fang C, Ahn R, Larrauri J. Emotional reactivity to personally-relevant and standardized sounds in borderline personality disorder. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9736-y. [DOI] [Google Scholar]
- Rottenberg J, Ray RD, Gross JJ. Emotion elicitation using films Handbook of Emotion Elicitation and Assessment. New York, NY: Oxford University Press; 2007. pp. 9–28. [Google Scholar]
- Salgado-Pineda P, Delaveau P, Blin O, Nieoullon A. Dopaminergic contribution to the regulation of emotional perception. Clinical Neuropharmacology. 2005;28:228–237. doi: 10.1097/01.wnf.0000185824.57690.f0. [DOI] [PubMed] [Google Scholar]
- Seeley SH, Mennin DS, Aldao A, McLaughlin KA, Rottenberg J, Fresco DM. Impact of comorbid depression on subjective and physiological responses to emotion in generalized anxiety disorder. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9744-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapero BG, Abramson LY, Alloy LB. Emotional reactivity and internalizing symptoms: Moderating role of emotion regulation. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9722-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppes G, Scheibe S, Suri G, Gross JJ. Emotion-regulation choice. Psychological Science. 2011;22:1391–1396. doi: 10.1177/0956797611418350. [DOI] [PubMed] [Google Scholar]
- Sheppes G, Suri G, Gross JJ. Emotion regulation and psychopathology. Annual Review of Clinical Psychology. 2015;11:379–405. doi: 10.1146/annurev-clinpsy-032814-112739. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Drost J, de Rooij M, van Hemert AM, Penninx BW. A longitudinal study of experiential avoidance in emotional disorders. Behavior Therapy. 2014;45:840–850. doi: 10.1016/j.beth.2014.07.001. [DOI] [PubMed] [Google Scholar]
- Taylor SF, Liberzon I. Neural correlates of emotion regulation in psychopathology. Trends in Cognitive Sciences. 2007;11:413–418. doi: 10.1016/j.tics.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Thiruchselvam R, Blechert J, Sheppes G, Rydstrom A, Gross JJ. The temporal dynamics of emotion regulation: An EEG study of distraction and reappraisal. Biological Psychology. 2011;87:84–92. doi: 10.1016/j.biopsycho.2011.02.009. [DOI] [PubMed] [Google Scholar]
- Van Meter AR, Youngstrom EA. Distinct roles of emotion reactivity and regulation in depressive and manic symptoms among euthymic patients. Cognitive Therapy and Research. this issue doi: 10.1007/s10608-015-9738-9. [DOI] [Google Scholar]
- vanOyen Witvliet C, Knoll RW, Hinman NG, DeYoung PA. Compassion-focused reappraisal, benefit-focused reappraisal, and rumination after an interpersonal offense: Emotion-regulation implications for subjective emotion, linguistic responses, and physiology. The Journal of Positive Psychology. 2010;5:226–242. doi: 10.1080/17439761003790997. [DOI] [Google Scholar]
- Walker FR, Nilsson M, Jones K. Acute and chronic stress-induced disturbances of microglial plasticity, phenotype and function. Current Drug Targets. 2013;14:1262–1276. doi: 10.2174/13894501113149990208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Bello P. Ritualized behavior as a domain-general choice of actions. Behavioral and Brain Sciences. 2006;29:633–634. doi: 10.1017/S0140525X06009551. [DOI] [Google Scholar]
- Weiss JA, Thomson K, Chan L. A systematic literature review of emotion regulation measurement in individuals with autism spectrum disorder. Autism Research. 2014;7:629–648. doi: 10.1002/aur.1426. [DOI] [PubMed] [Google Scholar]
- Werner KH, Goldin PR, Ball TM, Heimberg RG, Gross JJ. Assessing emotion regulation in social anxiety disorder: The Emotion Regulation Interview. Journal of Psychopathology and Behavioral Assessment. 2011;33:346–354. doi: 10.1007/s10862-011-9225-x. [DOI] [Google Scholar]
- Williams DP, Cash C, Rankin C, Bernardi A, Koenig J, Thayer JF. Resting heart rate variability predicts self-reported difficulties in emotion regulation: A focus on different facets of emotion regulation. Frontiers in Psychology. 2015;6:261. doi: 10.3389/fpsyg.2015.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Mathews A, MacLeod C. The emotional Stroop task and psychopathology. Psychological Bulletin. 1996;120:3–24. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]
- Wines FH. Report on the defective, dependent, and delinquent classes of the population of the United States as returned at the tenth census (June 1, 1880) Washington, DC: G.P.O; 1888. [Google Scholar]
- Wohleb ES, Hanke ML, Corona AW, Powell ND, Stiner LTM, Bailey MT, et al. Sheridan JF. β-adrenergic receptor antagonism prevents anxiety-like behavior and microglial reactivity induced by repeated social defeat. The Journal of Neuroscience. 2011;31:6277–6288. doi: 10.1523/JNEUROSCI.0450-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J, Ding N, Liu Y, Yang J. Unconscious emotion regulation: Nonconscious reappraisal decreases emotion-related physiological reactivity during frustration. Cognition and Emotion. 2015;29:1042–1053. doi: 10.1080/02699931.2014.965663. [DOI] [PubMed] [Google Scholar]
- Zaki J, Williams WC. Interpersonal emotion regulation. Emotion. 2013;13:803–810. doi: 10.1037/a0033839. [DOI] [PubMed] [Google Scholar]
- Zbozinek TD, Rose RD, Wolitzky-Taylor KB, Sherbourne C, Sullivan G, Stein MB, et al. Craske MG. Diagnostic overlap of generalized anxiety disorder and major depressive disorder in a primary care sample. Depression and Anxiety. 2012;29:1065–1071. doi: 10.1002/da.22026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziv M, Goldin PR, Jazaieri H, Hahn KS, Gross JJ. Emotion regulation in social anxiety disorder: Behavioral and neural responses to three socio-emotional tasks. Biol Mood Anxiety Disord. 2013;3:20. doi: 10.1186/2045-5380-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]


