Abstract
The prevalence of diabetes mellitus has been increasing both globally and locally. Primary care physicians (PCPs) are in a privileged position to provide first contact and continuing care for diabetic patients. A territory-wide Reference Framework for Diabetes Care for Adults has been released by the Hong Kong Primary Care Office in 2010, with the aim to further enhance evidence-based and high quality care for diabetes in the primary care setting through wide adoption of the Reference Framework.
A valid questionnaire survey was conducted among PCPs to evaluate the levels of, and the factors associated with, their adoption of the Reference Framework.
A total of 414 completed surveys were received with the response rate of 13.0%. The average adoption score was 3.29 (SD 0.51) out of 4. Approximately 70% of PCPs highly adopted the Reference Framework in their routine practice. Binary logistic regression analysis showed that the PCPs perceptions on the inclusion of sufficient local information (adjusted odds ratio [aOR] = 4.748, 95%CI 1.597–14.115, P = 0.005) and reduction of professional autonomy of PCPs (aOR = 1.859, 95%CI 1.013–3.411, P = 0.045) were more likely to influence their adoption level of the Reference Framework for diabetes care in daily practices.
The overall level of guideline adoption was found to be relatively high among PCPs for adult diabetes in primary care settings. The adoption barriers identified in this study should be addressed in the continuous updating of the Reference Framework. Strategies need to be considered to enhance the guideline adoption and implementation capacity.
Keywords: adoption, diabetes, primary care physicians, primary care settings, Reference Framework
1. Introduction
1.1. Rising prevalence of diabetes
Diabetes mellitus (DM) is a serious global disease burden. The International Diabetes Federation has estimated that the number of people with diabetes will increase from 382 million in 2013 to 592 million in 2035 worldwide.[1] In Hong Kong, up to 10% of the population are suffering from diabetes, 2% of which were aged <35 and 20% were aged >65 years.[2,3] However, these figures do not fully address nonreported figures and the undiagnosed.[3] By 2025, it was projected that at least 12.8% of the HK population, that is, 1 million people, would be affected by diabetes.[4] Proper management and control of diabetes on a regular basis is critical since the suboptimal control of blood glucose profiles can result in various complications, including cardiovascular diseases, stroke, blindness, kidney failure, and leg amputation.[5,6]
1.2. Suboptimal management of diabetes in primary care settings
Primary care physicians (PCPs) play an important role for managing diabetes patients, but the quality of diabetes management has been substandard in many primary care settings.[7,8] A cross-sectional study with 1970 patients in 3 general out-patient clinics in Hong Kong found that only 58.0%, 38.2%, and 36.4% of patients achieved optimal glycemic, blood pressure, and cholesterol targets, respectively. The rates for recording body mass index, nephropathy, and retinopathy screening were 47.9%, 69.0%, and 38.0%, respectively. These figures were far from satisfactory, implying that there is substantial room for improving the clinical services in settings where diabetic care is offered.[9]
1.3. The Reference Framework of the primary care office on diabetes care
The implementation of clinical practice guidelines can positively enhance the quality of care and improve health-related outcomes.[10,11] The Hong Kong Working Group on Primary Care of the Food and Health Bureau set up 3 Task Forces in 2010, one of which was charged with producing the Conceptual Model and Preventive Protocols with the provision of evidence-based recommendations for use in primary care settings.[12] The Reference Framework for diabetes care among adults in primary care setting was produced. This framework adopts a life-course, comprehensive, and continuous approach which is patient-oriented, based on best evidence from global literature and reference by clinical advice panel. It includes primary prevention, lifestyle changes, assessment of high risk groups, and early detection and management of diseases.[13] The guideline on diabetes care was released in 2010 and since then, it was available to PCPs, specialists, healthcare staff, and the general public via different media, including websites, seminars, and medical journals. The Primary Care Office has developed various strategies to promote the adoption of the guideline. It is expected that implementing the guideline will provide more standard and comprehensive care to diabetic patients in the primary care sector.
1.4. Study objectives
This study aims to evaluate the awareness and adoption levels of the Hong Kong Reference Framework for Diabetes Care for Adults in Primary Care Settings among local PCPs, and to identify the factors associated with the adoption of the Reference Framework. We hypothesized that the adoption level of the Reference Framework for diabetes care is low in Hong Kong given previous studies reporting low degrees of guideline adherence, and there are factors related to the adoption of the Reference Framework, such as patient-, physician-, and healthcare system-related factors.
2. Methods
2.1. Survey instruments
Based on the findings obtained from the focus group interviews in our previous study, a questionnaire was created with reference to literature, and it was tailored-made to the local context of primary healthcare in Hong Kong. The face validation was performed by a panel consisting of family medicine specialists (MCSW, SMG), public health professionals (HHXW, MWMK), and researchers in epidemiology (WMC, CKMF). The questionnaire was then pilot-tested among 10 PCPs randomly selected from honorary teaching fellows of the Faculty of Medicine, The Chinese University of Hong Kong in the central registry list. Subsequent amendments were made according to their recommendations. The adoption level was measured by questions on common practice for diabetes patients using a Likert Scale of “1 = never,” “2 = sometimes,” “3 = often,” and “4 = always” as the adoption score. Three questions were used to ask the participants about the recommended drug treatment options for type 2 diabetes patients. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. This study was approved by the Survey and Behavioural Research Ethics Committee of the Chinese University of Hong Kong.
2.2. The sampling frame and methodology
The target group consisted of all registered physicians working in primary care settings in HK, where one of their clinical duties involves the routine management of patients with diabetes. Surveys were also sent to doctors working in the public healthcare sector, namely General Out-patient Clinics, Family Medicine Specialist Clinics, and Staff Clinics in the study period. In the private healthcare sector, we based on the following sources to trace the contact information of private practitioners: the Hong Kong Doctors’ website of the HK Medical Association (www.hkdoctors.org) (n = 2464); a list of clinical teachers working in the private sector, carrying honorary teaching appointment in the Division of Family Medicine and Primary Care, Chinese University of Hong Kong (n = 149); a research database containing the contact details of previous collaborating private practitioners who consented to disclose their contact information for future research (n = 247); private doctors’ list from medical insurance company and association of private medical specialist (n = 760); Hong Kong Doctors’ networks in different districts (n = 86); and members of the Hong Kong College of Family Physicians, including doctors working in the primary care setting (excluding those who worked in the public sector, n = 1500). We established a central registry consisting of all registered physicians currently practicing in the private sector from the above sources (N = 2297 including omission of double counting due to overlaps).
We assumed that 50% of PCPs highly adopted the Reference Framework with a desired precision level of 5%. Using a standard formula.
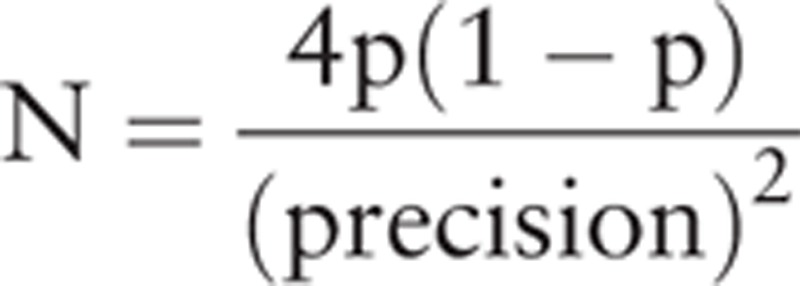 |
where p is the proportion of PCPs highly adopt the Reference Framework, the minimum sample size was estimated as 400. Given the relatively low response rate experienced in a territory-wide physician survey in the primary care sector (11.4%), survey invitations were sent to all PCPs in both the public and private sectors in the central registry to ensure the adequate recruitment of survey participants. Continuous Medical Education (CME) points were available to increase response rate.
Survey invitations to the primary care clinics in the public sector were sent via the logistic arrangements of clinics-in-charge. Invitations sent to PCPs working in the private sector were made through: posts with self-stamped envelopes, emails, faxlines, and visits to CME seminars. All surveys were self-administered. Survey invitations were conducted through all these contact channels for each registered doctor identified in our central registry. For those who had their e-mail addressed registered in the University's databases (1170 PCPs), an electronic web-based copy of the questionnaire was disseminated. This e-survey was technically supported by the Information and Technology Department of the administering University (originally disseminated on December 6th, 2013; 1st reminder on December 16th, 2013; 2nd reminder on January 6th, 2014; and 3rd reminder on January 23rd, 2014). The remaining PCPs from the databases (which amounted to 2014) were invited to complete a mailed copy of the survey to the prelisted addresses (distributed on December 23rd, 2013; 1st reminder on January 17th, 2014; 2nd reminder on February 20th, 2014; and 3rd reminder on March 10th, 2014).
A total of 3184 invitations to PCPs were sent, and informed consent was sought for each survey. PCPs may receive multiple invitations to the surveys and checks for duplications were made. For each survey returned via any means, 2 research assistants independently checked the presence of consent signature, full name of the PCP as appeared in the 1st page of the invitation letter, as well as the completeness of the questionnaires. Each survey received was checked to ensure that all compulsory fields were completed in addition to identity verification. Incentives in the form of shopping coupons were provided to encourage participation, and they were provided to the PCPs upon survey completion. Confidentiality and anonymity was assured by replacing the doctors’ identity with a unique identification number by a researcher prior management of results by the other.
2.3. Statistical analysis
The Statistical Package for Social Sciences 18.0 (Chicago, IL) was used for all data entry and analyses. Adoption level of each recommendation in the Reference Framework was studied and the overall adoption score was calculated. The PCPs with an overall adoption score of ≥3 out of 4 (“3 = often,” “4 = always” of the Likert scale) were considered to have highly adopted the Reference Framework. The outcome was highly dependent on the relative framework adoption levels in relation to the different demographic and practice characteristics. To determine the differences between high adoption and low adoption groups, independent t test was applied on the continuous variables, and Chi-square test was used for categorical data. Individual variables significantly associated with the adoption level of Reference Framework were included into a multivariate logistic regression model to identify independent predictors of adoption level. All P values ≤0.05 were regarded as statistically significant.
3. Results
3.1. Characteristics of participants
A total of 414 completed surveys were received via fax, e-mails, postal returns, the electronic web-based answering system, and on-site collection in CME seminar venues, giving a response rate of 13.0%. The mean age of the study participants was 53.1 years (standard deviation [SD] 13.6). A total of 71.8% were male physicians. The majority of primary care doctors had practice experience of more than 30 years (35.9%), and was in private sector (83.1%). Most were engaged in solo practice (48.0%). Slightly more than 1 in 10 (11.8%) of all participants were family physicians.
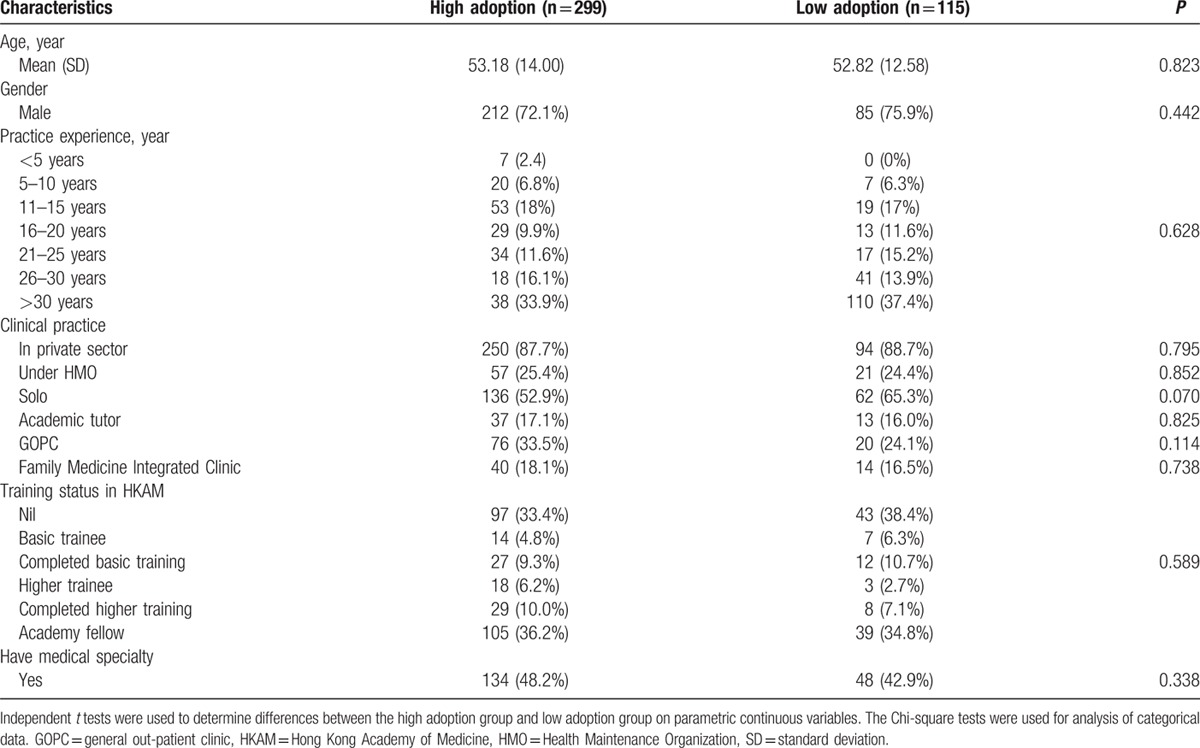
3.2. Difference in physicians by adoption level of Reference Framework for diabetes
With an assumption that practitioners have practiced the recommendation presented in the Reference Framework, the adoption levels of recommendations in the Reference Framework (overall adoption score ≥3 out of 4) were listed in Table 1. The average adoption score of the Reference Framework was calculated as 3.29 (SD = 0.51), and 72.2% of PCPs highly adopted the Reference Framework as their routine practice on diabetes patients. Measuring blood pressure for all diabetes patients at every routine DM visit was considered as the most frequent recommendation given to diabetes patients (73.3%) by practitioners, followed by advising all diabetes patients against smoking (70.5%) and promote “increasing [their] level of physical activity and doing regular exercise” (62.7%). It was found that the participants were less likely to perform additional eye examinations if glycemic and BP control were suboptimal (27.4%). The least practiced recommendations performed daily were fostering foot care education as part of a multidisciplinary approach in all DM patients (29.3%); and performing eye examinations annually on type II DM patients shortly after the diagnosis of diabetes (32.9%). No significant difference was found in the characteristics between PCPs with high and low adoption rates (Table 2).
Table 1.
Adoption levels of recommendations from the Reference Framework for diabetes care.
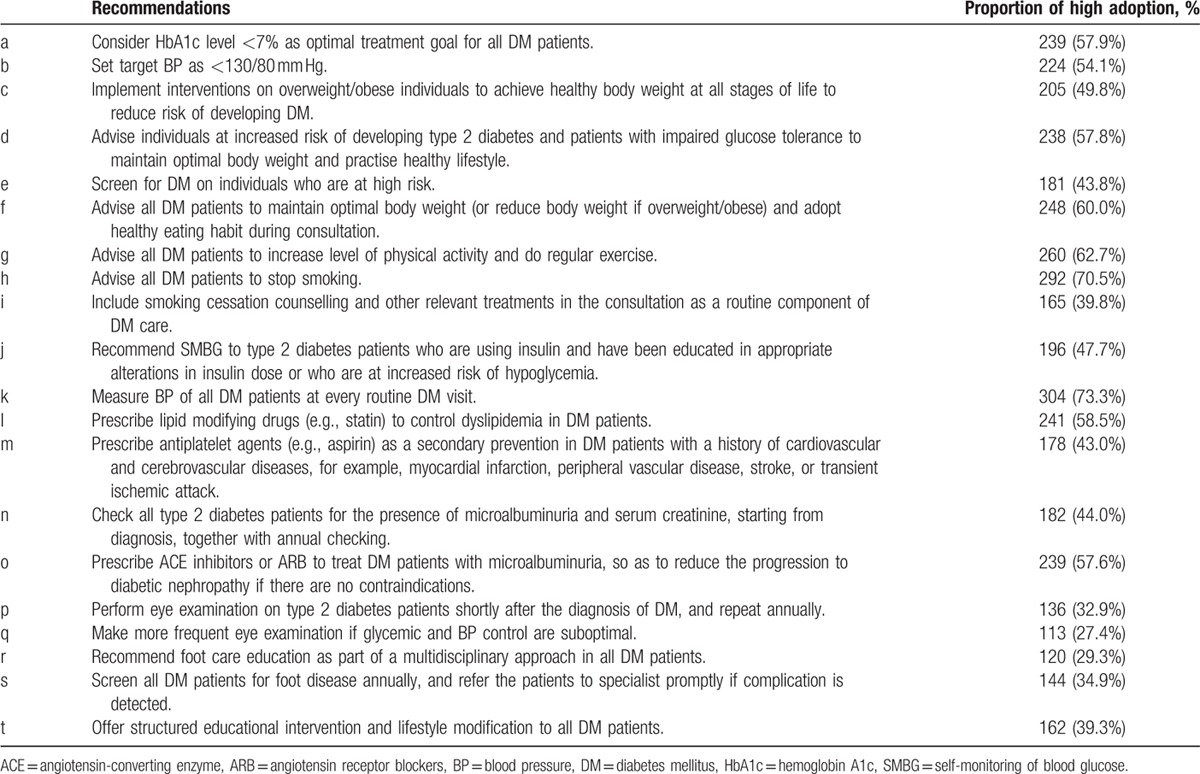
Table 2.
Physicians’ characteristics stratified by adoption of Reference Framework.
Most of the participant PCPs agreed (51.1%) or strongly agreed (43.0%) with the treatment flow for type 2 diabetes patients presented in the framework (Fig. 1). A total of 93.2% of participants agreed or strongly agreed to initiate drug treatment when the HbA1c level of the diabetes patient ≥7.5% despite 6 months of lifestyle modification. Approximately 93.4% of participants considered insulin therapy or additional oral glycemic agents were required if patient's HbA1c level reached >9% or the patient became symptomatic.
Figure 1.
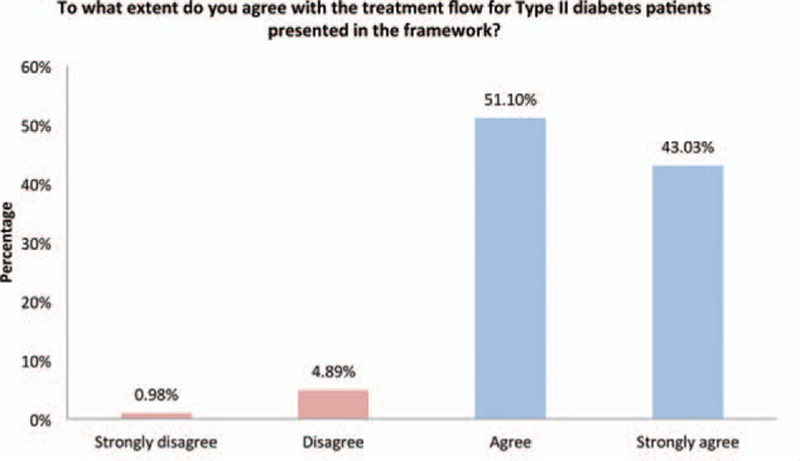
The extent of agreement with the treatment flow for type II diabetes patients presented in the framework.
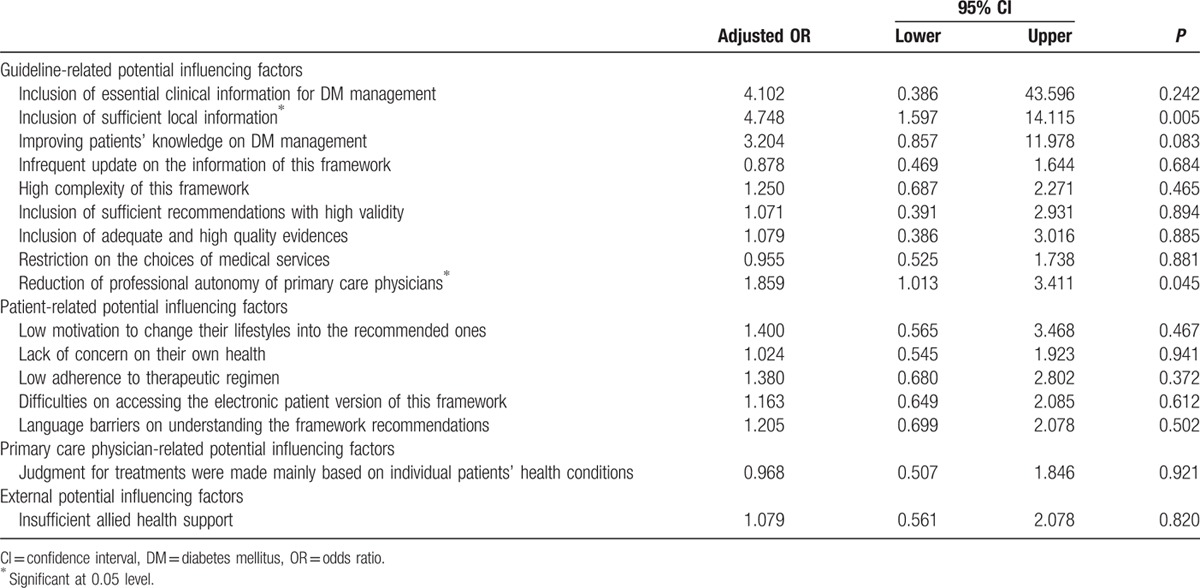
3.3. Factors affecting the adoption of Reference Framework
Potential factors were further categorized into 4 types: guideline-related, patient-related, PCP-related, and external factors. Differences in factors affecting adoption by adoption level were reported in Table 3. Most participants agreed or strongly agreed (95.6%) (P < 0.001) that there was essential clinical information on diabetes management in the Reference Framework. Around 93.7% (P < 0.001) of the participants believed that the framework could improve patients’ knowledge on diabetes management. One hindering factor about the implementation of the guideline was that more than half of the participants (56.4%) (P = 0.038) thought there was a restriction on the choices of medical services. As for patient-related factors, a majority of the participants (90.1%) (P = 0.021) believed that patients had little motivation and discipline needed to convert from their unhealthy lifestyles into the recommended ones. Many of the participants (69.1%) had low awareness of the Reference Framework before the survey, the difference was not statistically significant between high and low adoption group (P = 0.684). Other than insufficient allied health support (80%) (P = 0.021), limited consultation time (68.4%) (P = 0.742), and a lack of resources (70.4%) (P = 0.212), more than half of the participants (56.3%) (P = 0.575) thought that the framework could not be integrated into their current clinical setting.
Table 3.
Potential influencing factors on adoption.
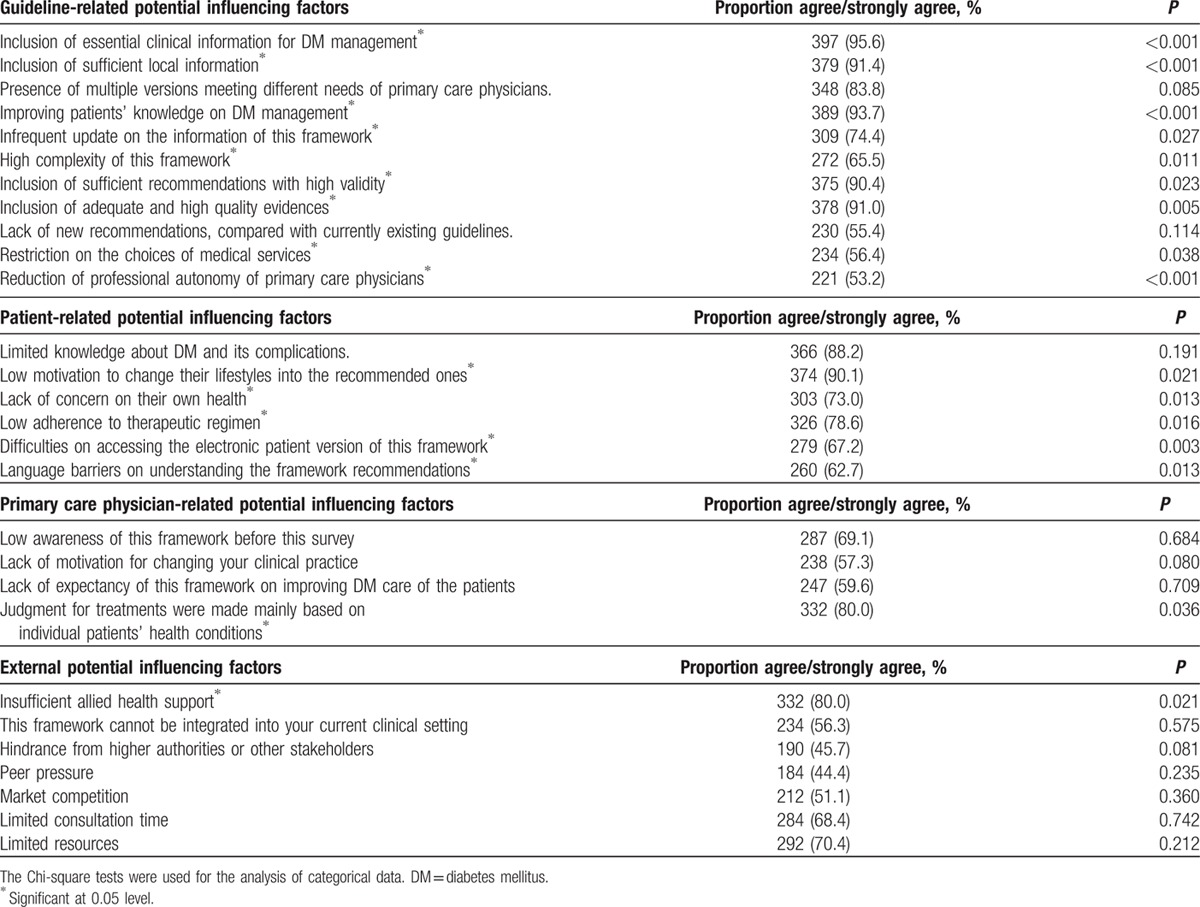
Table 4 shows the results of the multivariate logistic regression model. Independent factors associated with high adoption level included inclusion of sufficient local information (P = 0.005) and reduction of professional autonomy of PCP (P = 0.045).
Table 4.
Summary of the binary logistic regression analysis for potential factors.
4. Discussion
We examined guideline adoption by measuring rates of compliance with recommendations to identify PCP concerns, obstacles, and problems with specific items in the Reference Framework. Previous literature reported that unsatisfactory adherences to the guideline recommendations were prevalent in many clinical settings.[14] Potential barriers to adopting the guideline recommendations in managing individual diabetic patient may include the low awareness of diabetes, poor motivation to change unhealthy lifestyle habits, and suboptimal compliance to medical regimens.[10] Inadequate educational materials for diabetes patients and insufficient organizational support often served as other health care system-related factors associated with the greater adoption of the guideline.
In our study, the average adoption score of the Reference Framework was high (3.29 out of 4.00), implying that physicians’ daily practice in primary care closely matched with the recommendations from the Reference Framework. Low adoption rate was found for practices which required additional allied health support, that is, performing additional eye examinations if glycemic and BP control are suboptimal; recommending foot care education as part of a multidisciplinary approach for all patients; and performing eye examinations on type 2 diabetes patients shortly after its diagnosis, as well as repeating annual assessment. A combination of these factors indicated that there was inadequate support for physicians to follow these recommendations, in addition to 80% of participants having agreed or highly agreed that there was insufficient allied health support. Further cost-effective analyses may be needed to address the gap between needs and resources. In addition, the integration of the Reference Framework into PCPs’ current clinical practice while maintaining their autonomy was crucial.
To achieve a successful implementation of diabetes care management, PCPs are expected to provide health care services in accordance with the Reference Framework. In both the public and private sectors, the PCPs who participated in the study provided a relatively rich body of opinions. The existence of the Reference Framework itself may not be enough to ensure that the essential information contained could be consistently applied by the PCPs through passive dissemination of information in isolation. Present challenges may include the approaches to motivate and support more PCPs. Our study findings suggested a need for policy-makers and public health practitioners to further improve the framework by making the guideline more practical for both PCPs and patients to follow. This could lead to higher quality of patient care in the primary care setting. Strategies to address the hindering factors that affected the adoption rate should be further explored.
Some limitations of this study should be addressed. The sampling frame of the quantitative study only considered practitioners from several databases with contact details of PCPs, and the fact that we could not send survey invitations to all PCPs in Hong Kong could reduce the generalizability of the findings. Furthermore, the response rate was only 13%, and 83% of which worked in private healthcare. In addition to the low response rate, and the inability to reach other PCPs, one might argue that the representativeness of the questionnaires could be limited. Measures to improve response rate should be taken in the future, where an incentive scheme could be incorporated to attain a more representative sample of PCPs. Moreover, the collected data from the surveys were self-reported by the PCPs, and this might lead to response bias; it is unknown whether practitioners might have been practicing what they reported in the surveys due to potentially inaccurate recall. The high adoption rate of the recommendations suggested by the Reference Framework could have been coincidental; their methods of practice on a daily basis could have already been similar to what the framework recommends – and a cause-and-effect relationship between adoptions of the guideline and translating recommendations into practice might not be established. The lower than anticipated response rate might also induce a sampling bias since the ones who completed the surveys might have already adhering to the Reference Framework and were relatively more willing to share their opinions.
5. Conclusions
The recommendations in the Hong Kong Reference Framework for Diabetes Care for Adults in Primary Care Settings were widely adopted in their daily practice as reported by PCPs who participated in this study. The identified hindering factors should be considered in future efforts to streamline and enhance the implementation capacity of the Reference Framework. The development of multiple tailor-made versions of the Reference Framework may be another option to improve the adoption levels among PCPs.
Acknowledgments
The authors thank the Health and Medical Research Fund, Food and Health Bureau, Hong Kong Government for the full funding of this study. The authors also thank all the participants who contributed to this study.
Footnotes
Abbreviations: CME = continuous medical education, DM = diabetes mellitus, PCP = primary care physician.
Funding/support: This study was funded by Health and Medical Research Fund, Food and Health Bureau, Hong Kong Government.
The authors have no conflicts of interest to disclose.
References
- 1.International Diabetes Federation. Diabetes atlas. Epidemiology and morbidity. International Diabetes Federation; 2014. http://www.diabetesatlas.org/content/epidemiology-and-morbidity [Accessed October 1, 2014]. [Google Scholar]
- 2.Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009; 301:2129–2140. [DOI] [PubMed] [Google Scholar]
- 3.Janus ED, Wat NM, Lam KS, et al. The prevalence of diabetes, association with cardiovascular risk factors and implications of diagnostic criteria (ADA 1997 and WHO 1998) in a 1996 community-based population study in Hong Kong Chinese. Diabet Med 2000; 17:741–745. [DOI] [PubMed] [Google Scholar]
- 4.Diabetes Hong Kong. Response to the “Your Health, Your Life”. Healthcare Reform Consultation. Diabetes Hong Kong; 2008. http://www.fhb.gov.hk/beStrong/files/organizations/O017.pdf [Accessed October 1, 2011]. [Google Scholar]
- 5.Wong MC, Sin CK, Lee JP. The reference framework for diabetes care in primary care settings. Hong Kong Med J 2012; 18:238–246. [PubMed] [Google Scholar]
- 6.Roglic G, Unwin N, Bennett PH, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care 2005; 28:2130–2135. [DOI] [PubMed] [Google Scholar]
- 7.Balaji A. Quality of care among type 2 diabetes mellitus patients residing in an urban slum of Chennai Corporation – a community-based cross-sectional study. J Indian Med Assoc 2011; 109:462–464. [PubMed] [Google Scholar]
- 8.Braga MF, Casanova A, Teoh H, et al. Diabetes Registry to Improve Vascular Events [DRIVE] Investigators. Poor Int J Clin Pract 2012; 66:457–464. [DOI] [PubMed] [Google Scholar]
- 9.Wong KW, Ho SY, Chao DV. Quality of diabetes care in public primary care clinics in Hong Kong. Fam Pract 2012; 29:196–202. [DOI] [PubMed] [Google Scholar]
- 10.Rätsep A, Oja I, Kalda R, et al. Family doctors’ assessment of patient- and health care system-related factors contributing to non-adherence to diabetes mellitus guidelines. Prim Care Diabetes 2007; 93–97. [DOI] [PubMed] [Google Scholar]
- 11.Oh SW, Lee HJ, Chin HJ, et al. Adherence to clinical practice guidelines and outcomes in diabetic patients. Int J Qual Health Care 2011; 23:413–419. [DOI] [PubMed] [Google Scholar]
- 12.Primary Care Office. Primary Care Initiatives. Reference Frameworks. Department of Health (HK); 2012. http://www.pco.gov.hk/english/initiatives/frameworks.html [Accessed October 5, 2011]. [Google Scholar]
- 13.Primary Care Office. Hong Kong Reference Framework for Diabetes Care for Adults in Primary Care Settings. Primary Care Office (HK); 2013. http://www.pco.gov.hk/english/resource/files/RF_DM_full.pdf [Accessed October 5, 2011]. [Google Scholar]
- 14.Kirkman MS, Williams SR, Caffrey HH, et al. Impact of a program to improve adherence to diabetes guidelines by primary care physicians. Diabetes Care 2002; 25:1946–1951. [DOI] [PubMed] [Google Scholar]


