Abstract
Functional outcomes, length of stay (LOS), and discharge disposition have become frequent outcome measures among stroke patients after rehabilitation programs. To examine the trends of changes in functional outcomes, LOS, and discharge disposition in stroke patients discharged from an inpatient rehabilitation facility.
All patients (n = 432) were admitted to a tertiary inpatient rehabilitation hospital in Riyadh, Saudi Arabia with stroke diagnoses from November 2008 to December 2014. The functional independence measure (FIM) instrument used to assess the patient's functional status. The LOS was measured as the number of days the patients spent in the hospital from the day of admission to the day of discharge. The FIM efficiency was used to measure the patient's rehabilitation progress. All of the variables of the prospectively collected data were retrospectively analyzed.
There were significant changes by years in the total FIM ranging from 23 to 29 (P < 0.001) and subscores: FIM motor ranging from 20 to 26 (P < 0.001); FIM cognitive ranging from 1.8 to 3 (P < 0.001). The mean LOS remained constant, from 52 days in 2011 to 40 days in 2013. The FIM efficiency was stable between years and ranged from 0.52 to 0.72. The rates of discharge (to home) were significantly unstable and ranged from 100% in 2010 and 2011 to 92% in 2013.
Our results suggest that functional outcomes in patients with stroke have improved after an inpatient stroke rehabilitation program between 2008 and 2014 even with a constant LOS. Discharge disposition has remained unstable over this period. To improve the efficiency of the stroke rehabilitation program in Saudi Arabia, there is a need to decrease the LOS and emphasize a comprehensive interdisciplinary approach.
Keywords: physical therapy, rehabilitation, rehabilitation facilities, Saudi Arabia, stroke
1. Introduction
Functional outcomes, length of stay (LOS), and discharge disposition have become frequent outcome measures among stroke patients in inpatient rehabilitation facilities.[1] Recovery of function is often observed in patients with stroke over the 1st few months in an inpatient rehabilitation program (IRP).[2] Although the duration of this recovery is less certain, it is common at certain points to show variable functional improvements that lead to near-complete recovery.[3–5] Ottenbacher et al[6] and Chiou-Tan et al[7] found that stroke patients experienced functional status gains during the IRP.
Rehabilitation interventions are one method for managing stroke patients. These interventions seek to promote recovery and independence through neurofacilitative, functional, and compensatory training strategies.[2] If the stroke patient is medically stable, rehabilitation can begin in the acute care facility within approximately 72 hours.[2] Such interventions in a stroke unit can prevent or minimize the impact of deconditioning and the risk of secondary impairments.[8] Evidence shows that patients involved in an IRP have significantly improved functional outcomes compared with patients who do not receive such care.[9–11] According to recent studies, there is a deficit in the level of stroke awareness in the general population in Saudi Arabia.[12,13] Not surprizingly, many studies have indicated the need for more health care services for stroke patients, including rehabilitation services.[14,15]
Recent evidence suggests that patients’ LOSs in the IRP have decreased dramatically.[16] From another rehabilitation outcome angle, there is some disagreement in the literature regarding the impact of the LOS on the recovery outcome.[17] The average LOS in the United States varies from 17 to 25 days, whereas the LOSs in Canada, Australia, and New Zealand are 23 to 49, 28, and 30 days, respectively.[18] Tan et al[19] found that a patient's socioeconomic status and family structure are more likely to influence LOS and motor function at admission. Another study published in 2004 found that the LOS is likely to be longer for female patients and that patients residing in rural areas had shorter LOSs.[20]
Previous studies have reported that the majority of stroke patients are discharged to home after the IRP.[21,22] An objective of this study was to examine the trends of changes in functional outcomes, LOS, and discharge disposition in stroke patients discharged from an inpatient rehabilitation facility in Riyadh, Saudi Arabia. To date, no reliable evidence reports have examined our study objective in Saudi Arabia.
2. Materials and methods
2.1. Study design
This study was a single-center, hospital-based, retrospective cohort study conducted at a King Fahad Medical City-Rehabilitation Hospital (KFMC-RH) in Riyadh, Saudi Arabia.
2.2. Setting
The KFMC-RH is largest tertiary inpatient rehabilitation hospital in Riyadh, Saudi Arabia. KFMC-RH follows the Uniform Data System for Medical Rehabilitation protocol in administering the functional independence measure (FIM) instrument. Since 1987, the Uniform Data System for Medical Rehabilitation, a not-for-profit organization affiliated with University at Buffalo Foundation Activities, Inc., at the State University of New York at Buffalo, has maintained the largest nongovernmental national registry of standardized information on medical rehabilitation inpatients in the world.[23]
2.3. Participants
Between November 2008 and December 2014, admission and discharge data were reviewed for 432 patients with a primary diagnosis of stroke (International Classification of Diseases, Ninth Revision codes 348–438 and 799.3) who received inpatient rehabilitation services at KFMC-RH and were considered for inclusion in the study. We classified the patients, according to the inpatient rehabilitation discharge by year (2008–2009, 2010, 2011, 2012, 2013, and 2014) from the total stroke patients. The patients, who discharged from inpatient rehabilitation in 2008 and 2009, were combined for consistency. We refined the sample by including patients from the 4 impairment groups with the greatest number of patients: right hemisphere (49%), left hemisphere (36%), bilateral hemisphere (4%), and another stroke (11%). The Committee on Human Research, the Institutional Review Board at King Fahd Medical City, Riyadh, approved the study (approval numbers: 14-273).
2.4. Variables
The dependent variables were change in the total FIM score, motor and cognitive FIM subscores, LOS, FIM efficiency (change in the FIM total score/LOS [median]), and discharge disposition (to home vs not to home).
2.5. Measurements
We used the FIM instrument to measure the patient's functional status throughout their IRP.[24] The FIM measures the patient's functional status and indicates how much assistance is required for the individual to conduct activities of daily living. It comprises 18 items composed of 13 motor tasks and 5 cognitive tasks: eating, grooming, bathing, upper body dressing, lower body dressing, toileting, bladder management, bowel management, bed-to-chair transfer, toilet transfer, shower transfer, locomotion (ambulation or wheelchair use), stairs, cognitive comprehension, expression, social interaction, problem solving, and memory. All of the tasks are graded on a 7-point ordinal scale that begins with total assistance (or complete dependence, in which patients perform <25% of the task) and finishes with complete independence. The final total FIM scores range from 18 (lowest) to 126 (highest), which indicates the level of assistance required. The motor score ranges from 13 to 91 and a cognitive FIM score ranges from 5 to 35. The validity and reliability of the FIM instrument for stroke patients is well established.[25–27]
The LOS was measured as the number of days the patients spent in the hospital from the day of admission to the day of discharge. The FIM efficiency was defined as the change in functional status from admission to discharge and was divided by the LOS (median) as defined by Ottenbacher et al.[16] The FIM efficiency was used to measure the patient's rehabilitation progress. An accepted measure of an adequate rehabilitation progress is a gain of 1 FIM point per day.[28]
2.6. Statistical analysis
All of the variables of the prospectively collected data were retrospectively analyzed. The statistical analysis compared the functional status, that is, the independent variable, to all of the dependent variables (the change in the FIM total score, the change in the motor and cognitive FIM subscores, LOS, FIM efficiency, and discharge disposition [home versus not-to-home]). The IRP effectiveness was obtained by subtracting admission mean score on the total FIM as well as motor and cognitive FIM subscale mean scores from discharge score; paired t test was used to compute the mean difference and its significance by year.[29] The analyses of variance test was used to examine the change in LOS and efficiency trends, while Chi-square test was used to compute the discharge disposition trends. All of the analyses were performed using the statistical analysis software system for Windows version 9.2 (SAS Institute, Inc., Cary, NC) with a significance level of .05.
3. Results
The total samples included 432 records from the KFMC-RH facility that hosted the IRP from 2008 to 2014. The patients’ mean age was 57.5 ± 16 years, and just over half of the sample was male (57%). The mean time to admission was 71 days from the onset of stroke, and the mean LOS was 47.5 days from admission to discharge. The majority of the patients were significantly affected by a right-hemisphere stroke (49%). The descriptive characteristics of all of the patients, stratified by year, are shown in Table 1.
Table 1.
Demographic characteristics of all patients, stratified by year, from 2008 to 2014.
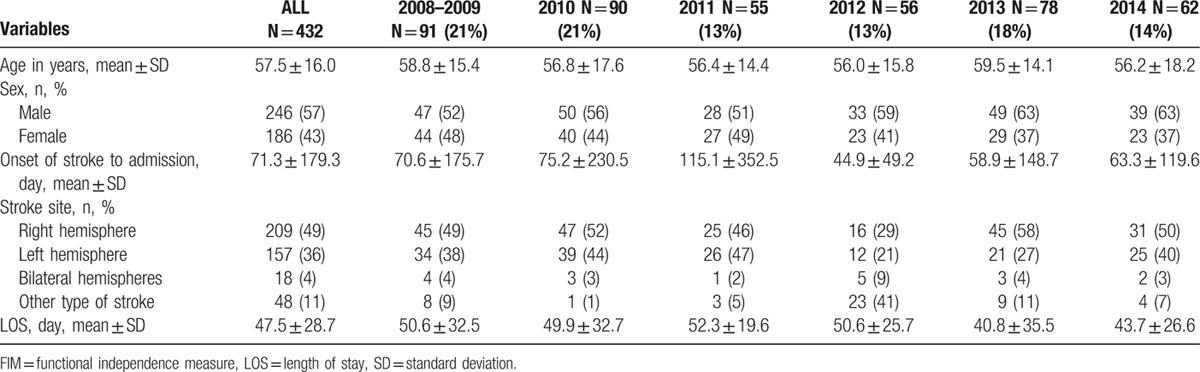
Table 2 shows the outcome measures for total FIM, the motor and cognitive FIM subscores, LOS, efficiency scores, and discharge disposition by year from 2008 to 2014. There were substantial changes by years in the total FIM, FIM motor, and FIM cognitive subscores, which ranged from 23 to 29 (changes in the total FIM [P < 0.001]), 20 to 26 (changes in the FIM motor subscore [P < 0.001]), and from 1.8 to 3 (changes in the FIM cognitive subscore [P < 0.001]), respectively. The largest improvement in total FIM (29.5 ± 16.0) and FIM motor (26.5 ± 16.1) occurred in 2014 (Fig. 1). The total LOS by year decreased from a median of 51 days in 2011 to 2012 to 41 days in 2014 (F = 1.65, P = 0.14). The mean LOS remained constant from 40 days in 2013 to 52 days in 2011. The reduction in median LOS was greatest for the patients discharged in 2014 (41 days). The FIM efficiency was stable between years and ranged from 0.52 to 0.72 (P = 0.17). There was a significant change in the percentage of patients discharged to home after inpatient rehabilitation between 2008 and 2014. The rates of discharge to home were unstable and ranged from 92% in 2013 to 100% between 2010 and 2011. Overall, there was a higher probability of patient discharge to home in 2010 and 2011 (100%) compared with other years.
Table 2.
Trends of effectiveness of inpatient rehabilitation program on functional outcome, LOS, and discharge disposition, stratified by year, from 2008 to 2014∗.
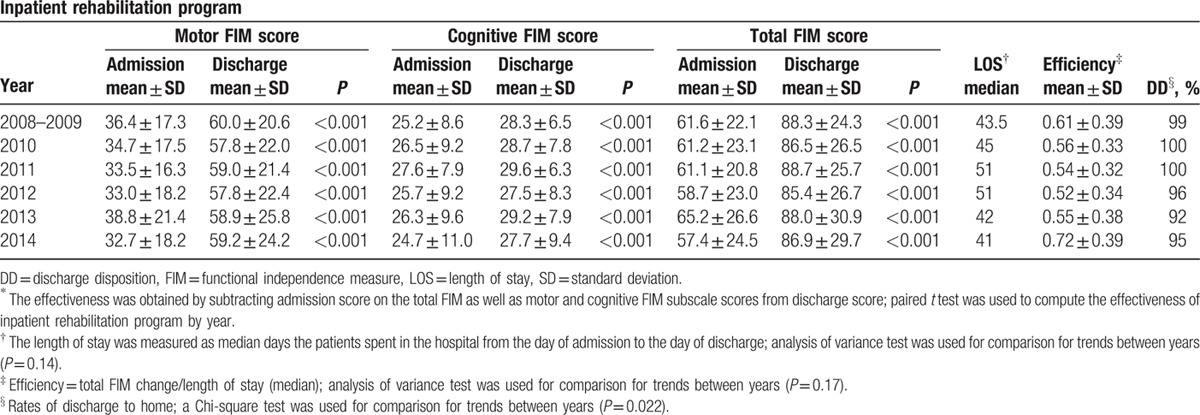
Figure 1.
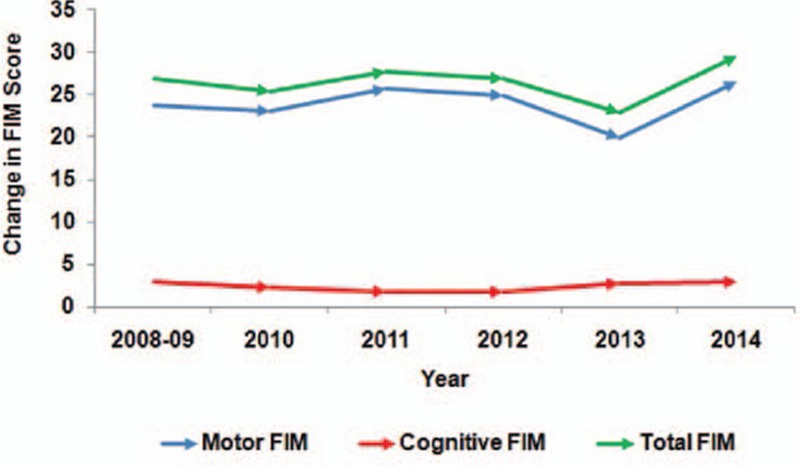
Trends of changes in functional independence measure score after inpatient rehabilitation program, stratified by year.
4. Discussion
The results of this study show that there was statistically significant change in total FIM, FIM motor, and FIM cognitive scores after IRP among patients who attended the program from 2008 to 2014. The most important clinically relevant finding was that the changes in total FIM, FIM motor, and FIM cognitive scores were clinically significant. One interesting finding was that the LOS for the IRP decreased from 2008 to 2014. Surprizingly, no difference was found in the rehabilitation efficiency from 2008 to 2014. Another important finding was that there has been a significant alteration in the percentage of patients discharged to home following IRP from 2008 to 2014.
This finding suggests that the change in the total FIM, FIM motor, and FIM cognitive scores had a minimal clinically important difference (MCID). A prospective case series study by Beninato et al[30] of 113 stroke patients suggested that changes in FIM scores were associated with MCID; they reported total FIM, FIM motor, and FIM cognitive score changes of 22, 17, and 3, respectively. In Saudi Arabia, Abdul-Sattar and Godab[31] found that the change in total FIM was not clinically significant (the MCID was 20). It also indicated that stroke severity, stroke recurrence, cognitive impairment, and depression influenced the functional outcome of stroke patients in the IRP. The retrospective observational cohort study by Meiner et al[32] showed that the mean FIM values at admission and at discharge and the FIM efficiency were significantly higher in stroke patients following IRP. Our study differs from this study's finding in that the total FIM, FIM motor, and FIM cognitive scores were clinically significant, and FIM efficiency was stable between years. These findings from our study can help physicians interpret FIM change scores in terms of their clinical importance.
It is interesting to note that in our study, the LOS for IRP decreased from 2008 to 2014. This finding is similar to that of the retrospective cohort study from 1994 to 2001 by Ottenbacher et al,[16] which found that the LOS decreased substantially from 1994 to 2001. Al-Jadid and Robert[33] findings in Riyadh, Saudi Arabia, support our findings that the mean LOS for stroke patients in an IRP was 45 days. This study also found that the LOSs of Saudi patients were higher than those of non-Saudis.
Our findings are rather disappointing in that FIM efficiency was stable between years, and no difference was found in the rehabilitation efficiency from 2008 to 2014. Another important finding was the significant alteration in the number of the patients discharged to home following the IRP from 2008 to 2014. Our study results regarding discharge disposition are similar and were consistent with the retrospective studies of Bottemiller et al[21] as well as Nguyen et al,[22] which found that more than 75% of stroke patients were discharged to home following an IRP.
This finding has important implications for developing rehabilitation services in Saudi Arabia to achieve better functional outcomes for stroke patients. Al Khathaami et al[34] found that stroke care in Saudi Arabia lags behind that of developed countries. Out of more than 350 hospitals nationwide, Saudi Arabia has only 1 active stroke center and 7 centers providing thrombolysis; only 2 hospitals have a stroke team. Ayoola et al[35] case–control study that evaluated the epidemiological characteristics of stroke in different geographical regions of Saudi Arabia has not been fully investigated. Reports from some areas indicate that stroke is a major cause of morbidity and mortality in the population of Gizan, a largely rural area with a lower stroke incidence than the reported rates for urban areas of Saudi Arabia.[36] In addition, Alaqeel et al[13] suggested that there is an alarming deficit in the level of stroke awareness in the Saudi population. Prompt public health measures to correct this deficiency are urgently needed.
One limitation of this study is its small sample size; large studies produce narrow intervals and therefore more precise results. The possibility of coding and reporting errors exists, but the consistency of the information collection process has been extensively examined.[37] Another limitation is the lack of information regarding health covariables (e.g., comorbidity, depressive symptoms, and body mass index) and some sociodemographic information (e.g., marital status, education, living status, and race). The other sociodemographic information (age and gender) in KFMC-RH database was obtained from existing medical records and self-reports. The strength of our study is that KFMC-RH is a large tertiary inpatient rehabilitation hospital in Riyadh, Saudi Arabia, and is licensed to use the FIM scale.
5. Conclusion
Our results suggest that functional outcomes in patients with stroke have improved after an inpatient stroke rehabilitation program between 2008 and 2014 even with a constant LOS. Discharge disposition has remained unstable over this period. In an effort to improve the efficiency of the stroke rehabilitation program in Saudi Arabia, there is a need to decrease LOSs and emphasize comprehensive, interdisciplinary approach. On a national level, larger-scale studies are needed to confirm our findings, and long-term follow-up analyses should be used to standardize the outcome measures.
Acknowledgements
The authors thank the General Directorate for Research Grants (GDRG) at King Abdulaziz City for Science and Technology (KACST) (Grant No: AT 343-34) for the support.
Footnotes
Abbreviations: FIM = functional independence measure, IRP = inpatient rehabilitation program, KFMC-RH = King Fahad Medical City-Rehabilitation Hospital, LOS = length of stay, MCID = minimal clinically important difference.
This study was presented at the 92nd American Congress of Rehabilitation Medicine Annual Conference on Progress in Rehabilitation Research (PIRR), Dallas, TX, October 25 to 30, 2015.
Authorship: B-SM contributed to the conception and design of the study, the analysis and interpretation of the data, prepared the initial draft of the manuscript, and edited and critically revised the manuscript. VV acquired the data, contributed to the analysis, interpretation of the data, and the initial drafting of the manuscript. MH contributed to the conception and design of the study, edited, and critically revised the manuscript. AH contributed to the acquired the data, analysis, and interpretation of the data, prepared the initial draft of the manuscript.
Funding/support: This work was supported by a grant from the General Directorate for Research Grants (GDRG) at King Abdulaziz City for Science and Technology (KACST) (Grant No: AT 343-34).
The authors have no conflicts of interest to disclose.
References
- 1.Galski T, Bruno RL, Zorowitz R, et al. Predicting length of stay, functional outcome, and aftercare in the rehabilitation of stroke patients. The dominant role of higher-order cognition. Stroke 1993; 24:1794–1800. [DOI] [PubMed] [Google Scholar]
- 2.Chollet F, DiPiero V, Wise RJ, et al. The functional anatomy of motor recovery after stroke in humans: a study with positron emission tomography. Ann Neurol 1991; 29:63–71. [DOI] [PubMed] [Google Scholar]
- 3.Andrews K, Brocklehurst JC, Richards B, et al. The rate of recovery from stroke – and its measurement. Int Rehabil Med 1981; 3:155–161. [DOI] [PubMed] [Google Scholar]
- 4.Wade DT, Wood VA, Hewer RL. Recovery after stroke – the first 3 months. J Neurol Neurosurg Psychiatry 1985; 48:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berges IM, Kuo YF, Ottenbacher KJ, et al. Recovery of functional status after stroke in a tri-ethnic population. PM R 2012; 4:290–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ottenbacher KJ, Campbell J, Kuo YF, et al. Racial and ethnic differences in postacute rehabilitation outcomes after stroke in the United States. Stroke 2008; 39:1514–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chiou-Tan FY, Keng MJ, Jr, Graves DE, et al. Racial/ethnic differences in FIM scores and length of stay for underinsured patients undergoing stroke inpatient rehabilitation. Am J Phys Med Rehabil 2006; 85:415–423. [DOI] [PubMed] [Google Scholar]
- 8.Gordon NF, Gulanick M, Costa F, et al. Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention; the Council on Cardiovascular Nursing; the Council on Nutrition, Physical Activity, and Metabolism; and the Stroke Council. Stroke 2004; 35:1230–1240. [DOI] [PubMed] [Google Scholar]
- 9.Hakkennes SJ, Brock K, Hill KD. Selection for inpatient rehabilitation after acute stroke: a systematic review of the literature. Arch Phys Med Rehabil 2011; 92:2057–2070. [DOI] [PubMed] [Google Scholar]
- 10.Barnes M, Dobkin B, Bogousslavsky J. Recovery After Stroke. New York: Cambridge University Press; 2009. [Google Scholar]
- 11.Teasell R, Foley N, Salter K, et al. Evidence-based review of stroke rehabilitation: executive summary, 12th edition. Top Stroke Rehabil 2009; 16:463–488. [DOI] [PubMed] [Google Scholar]
- 12.Kamran S, Bener AB, Deleu D, et al. The level of awareness of stroke risk factors and symptoms in the Gulf Cooperation Council countries: Gulf Cooperation Council stroke awareness study. Neuroepidemiology 2007; 29:235–242. [DOI] [PubMed] [Google Scholar]
- 13.Alaqeel A, AlAmmari A, AlSyefi N, et al. Stroke awareness in the Saudi community living in Riyadh: prompt public health measures must be implemented. J Stroke Cerebrovasc Dis 2014; 23:500–504. [DOI] [PubMed] [Google Scholar]
- 14.Tummers JF, Schrijvers AJ, Visser-Meily JM. Economic evidence on integrated care for stroke patients; a systematic review. Int J Integr Care 2012; 12:e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Modeer MA, Hassanien NS, Jabloun CM. Profile of morbidity among elderly at home health care service in Southern Saudi Arabia. J Family Community Med 2013; 20:53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ottenbacher KJ, Smith PM, Illig SB, et al. Trends in length of stay, living setting, functional outcome, and mortality following medical rehabilitation. JAMA 2004; 292:1687–1695. [DOI] [PubMed] [Google Scholar]
- 17.Maulden SA, Gassaway J, Horn SD, et al. Timing of initiation of rehabilitation after stroke. Arch Phys Med Rehabil 2005; 86 (12 Suppl 2):S34–S40. [DOI] [PubMed] [Google Scholar]
- 18.Grant C, Goldsmith CH, Anton HA. Inpatient stroke rehabilitation lengths of stay in Canada derived from the National Rehabilitation Reporting System, 2008 and 2009. Arch Phys Med Rehabil 2014; 95:74–78. [DOI] [PubMed] [Google Scholar]
- 19.Tan WS, Heng BH, Chua KS, et al. Factors predicting inpatient rehabilitation length of stay of acute stroke patients in Singapore. Arch Phys Med Rehabil 2009; 90:1202–1207. [DOI] [PubMed] [Google Scholar]
- 20.Somerford PJ, Lee AH, Yau KK. Ischemic stroke hospital stay and discharge destination. Ann Epidemiol 2004; 14:773–777. [DOI] [PubMed] [Google Scholar]
- 21.Bottemiller KL, Bieber PL, Basford JR, et al. FIM score, FIM efficiency, and discharge disposition following inpatient stroke rehabilitation. Rehabil Nurs 2006; 31:22–25. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen VQ, PrvuBettger J, Guerrier T, et al. Factors associated with discharge to home versus discharge to institutional care after inpatient stroke rehabilitation. Arch Phys Med Rehabil 2015; 96:1297–1303. [DOI] [PubMed] [Google Scholar]
- 23.Graham JE, Granger CV, Karmarkar AM, et al. The Uniform Data System for Medical Rehabilitation: report of follow-up information on patients discharged from inpatient rehabilitation programs in 2002–2010. Am J Phys Med Rehabil 2014; 93:231–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Granger CV. The emerging science of functional assessment: our tool for outcomes analysis. Arch Phys Med Rehabil 1998; 79:235–240. [DOI] [PubMed] [Google Scholar]
- 25.Dickson HG, Kohler F. Interrater reliability of the 7-level functional independence measure (FIM). Scand J Rehabil Med 1995; 27:253–256. [PubMed] [Google Scholar]
- 26.Ottenbacher KJ, Hsu Y, Granger CV, et al. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil 1996; 77:1226–1232. [DOI] [PubMed] [Google Scholar]
- 27.Dodds TA, Martin DP, Stolov WC, et al. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil 1993; 74:531–536. [DOI] [PubMed] [Google Scholar]
- 28.Keith RA, Wilson DB, Gutierrez P. Acute and subacute rehabilitation for stroke: a comparison. Arch Phys Med Rehabil 1995; 76:495–500. [DOI] [PubMed] [Google Scholar]
- 29.Frey LR, Botan CH, Kreps GL. Investigating Communication: An Introduction to Research Methods. 2nd ed. Boston: Allyn and Bacon; 2000. [Google Scholar]
- 30.Beninato M, Gill-Body KM, Salles S, et al. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Arch Phys Med Rehabil 2006; 87:32–39. [DOI] [PubMed] [Google Scholar]
- 31.Abdul-Sattar AB, Godab T. Predictors of functional outcome in Saudi Arabian patients with stroke after inpatient rehabilitation. NeuroRehabilitation 2013; 33:209–216. [DOI] [PubMed] [Google Scholar]
- 32.Meiner Z, Sajin A, Feintuch U, et al. Rehabilitation outcomes of patients with stroke: effect of age on functional outcome and discharge destination. Top Geriatr Rehabil 2015; 31:138–144. [Google Scholar]
- 33.Al-Jadid MS, Robert AA. Determinants of length of stay in an inpatient stroke rehabilitation unit in Saudi Arabia. Saudi Med J 2010; 31:189–192. [PubMed] [Google Scholar]
- 34.Al Khathaami AM, Algahtani H, Alwabel A, et al. The status of acute stroke care in Saudi Arabia: an urgent call for action!. Int J Stroke 2011; 6:75–76. [DOI] [PubMed] [Google Scholar]
- 35.Ayoola AE, Banzal SS, Elamin AK, et al. Profile of stroke in Gizan, Kingdom of Saudi Arabia. Neurosciences (Riyadh) 2003; 8:229–232. [PubMed] [Google Scholar]
- 36.al Tahan A, Buchur J, el Khwsky F, et al. Risk factors of stroke at high and low altitude areas in Saudi Arabia. Arch Med Res 1998; 29:173–177. [PubMed] [Google Scholar]
- 37.Stineman MG, Hamilton BB, Granger CV, et al. Four methods for characterizing disability in the formation of function related groups. Arch Phys Med Rehabil 1994; 75:1277–1283. [PubMed] [Google Scholar]


