Abstract
Background:
Depression is one of the mental health problems confronting those with diabetes mellitus and may result from self-defeating thoughts and lifestyles. Therefore, the aim of this study was to investigate the effects of cognitive behavioral coaching (CBC) program on depressive symptoms in a sample of the Type 2 diabetic inpatients in Onitsha metropolis of Anambra State, Nigeria.
Methods:
The design of the study was pretest–post-test randomized control group design. The participants were 80 Type 2 diabetic inpatients randomly assigned to the treatment and control groups. The primary outcome measures were Beck's Depression Inventory-II and a Diabetic Inpatient's Depressive Symptoms Observation Checklist. Mean, standard deviation, repeated measures analysis of covariance, and partial eta squared were used for data analysis.
Results:
The results revealed that the baseline of depressive symptoms was similar between the control and treatment groups of the Type 2 diabetic inpatients. But, exposing the Type 2 diabetic inpatients to a cognitive behavioral coaching program significantly reduced the depressive symptoms in the treatment group compared to those in the control group at the end of the intervention. The effects of cognitive behavioral coaching program on the depressive symptoms of those in the treatment group remained consistent at a 6 month follow-up meetings compared to the control group.
Conclusion:
Given the potential benefits of a cognitive behavioral coaching program, clinicians and mental health professionals are urged to support and implement evidence-based cognitive-behavioral coaching interventions aimed at promoting diabetic inpatients’ wellbeing in the Nigerian hospitals.
Keywords: cognitive behavioral coaching, depression, depressive symptoms, diabetes mellitus, health coaching, inpatients
1. Introduction
Depression is a leading contributor to the overall worldwide burden of disease yet fewer than 10% of those affected in the world receive effective care partly due to inaccurate assessment.[1] In countries of all income levels, individuals who are depressed are often not correctly diagnosed, and others who do not have the disorder are too often misdiagnosed and prescribed antidepressants.[1] Yet, the global burden of depression is still on the rise with a large body of evidence that depression is a prevalent illness that burdens the world's population,[2–5] and those with diabetes mellitus are not exempted.[6–8]
The presence of diabetes mellitus is known to multiply the risk of comorbid depression affecting >1 quarter of the diabetic population, and making its recognition and treatment in diabetic patients clinically relevant.[9] In fact, those patients being treated for Type 2 diabetes mellitus are at a much higher rate for developing depressive symptoms than the general population.[10] Without adequate treatment, the symptoms of depression in individuals [with diabetes] can last for weeks, months, or years but appropriate treatment modality can help such individuals to cope and lead a well-adjusted life.[1,11] As depression also result from self-defeating life patterns besides other underlying factors,[12] it may be possible to surmount it via a cognitive behavioral coaching program.
The Cognitive Behavioral Coaching (CBC) approach premises that individuals may have inadequate problem-solving skills or may not apply skills they have in a contextually appropriate manner, and that their thoughts, emotions, and behaviors are keys to understanding their perception of problems and situations.[13] Furthermore, the cognitive behavioral coaching approach to psychotherapy helps clients to identify, examine, and change self-defeating thoughts and beliefs, develop productive behaviors, become more skilled at emotional management and reach their desired goals in life.[14] Thus, the focus of cognitive behavioral coaching approach is on the client's current concerns and the ultimate goal is for the client to become their own coach, “self-coach” in order to tackle present and future challenges.[13,15]
Though the research on cognitive behavioral coaching seems limited, the approach appears promising as there are evidences showing its consistent positive benefits to clients who are exposed to it. Despite the fact that, all of the studies in that regard demonstrated at least some positive impact of the cognitive behavioral coaching approach, various limitations associated with some of the studies include the lack of a control group,[16–18] lack of a within-subject design,[15] an undue reliance on self-report measures,[19,20] lack of randomization,[19] possible selection bias,[17] and lack of clarity in reporting.[21] Furthermore, when it comes to the cognitive behavioral coaching approach, most therapists typically think about outpatient treatment, and infrequently think about inpatient treatment for their clients. Thus, there is also tendency for these therapists to ask “What is the right treatment for depressive symptoms: outpatient or inpatient?” “Which should the clients attend and why?” “Is the cognitive behavioral coaching approach effective if used in inpatient treatment of depressive symptoms?” These questions and a number of other questions have come to our mind regarding the rationale and justification for initiating a cognitive behavioral coaching approach to assist the diabetic inpatients in dealing with their depressive symptoms in the Nigerian hospitals setting.
Although there are research evidences confirming the presence of depression in the Nigerian population,[22–24] no study, to the best of the researchers’ knowledge, has applied the cognitive behavioral coaching approach despite its potential benefits, to assist the Nigerian clients toward remediating their depressive symptoms. In the current study, the researchers are concerned about the consequences of untreated depression in the Type 2 diabetic inpatients in Nigerian hospitals in that they often go unnoticed by most of the physicians. This study is warranted in that if nothing is done to help them manage their depressive symptoms, the diabetic inpatients’ will likely continue to show symptoms such as feelings of sadness, worthlessness, helplessness, and hopelessness which might even become heightened despite receiving medications, and these symptoms might interfere with their work, mood, thoughts, eating habit, and ability to sleep.[25] Other consequences might include but are not limited to irritability, guilt, and fatigue.[26] These consequences among others might even be exacerbated given that depression is a commonly overlooked comorbidity, and poor quality data limit the interpretation and validity of the burden of depression estimates.[27] Besides, diabetic patients with depression may find it hard to maintain daily diabetes care partly due to the adverse effects associated with overreliance on antidepressant medication, and thus the offering of psychological treatments, such as cognitive behavioral coaching becomes pertinent.
In view of the above, it is possible that the Type 2 diabetic inpatients can be helped to identify, examine, and change self-defeating thoughts and beliefs, develop productive behaviors, maintain daily diabetic care, and become more skilled at emotional management and invariably reduce their depression in accordance with the cognitive behavioral coaching therapy approach. To this end, the purpose of the current study is to investigate the effects of cognitive behavioral coaching on depressive symptoms among the Type 2 diabetic inpatients in public hospitals in Onitsha metropolis of Anambra State, Nigeria. To guide the study, the researchers hypothesized that the depressive symptoms of Type 2 diabetic inpatients will not significantly differ across the treatment and control groups at baseline. Conversely, it was also hypothesized that cognitive behavioral coaching will significantly reduce the depressive symptoms among the Type 2 diabetic inpatients in the treatment group compared to those in control group over time and that the reduction in depressive symptoms would be consistent.
2. Methods
2.1. Ethical approval
The researchers obtained approval to conduct this study from the Research Ethics/Grants Committee of the Department of Educational Foundations, University of Nigeria, Nsukka, Enugu State, and the Hospitals’ Management Board where the current study took place. Participants’ written informed consent was appropriately obtained.
2.2. Participants
The researchers accessed 250 diabetic inpatients by using the Becks Depression Inventory-II (BDI-II) to identify those with severe depression in public hospitals in Onitsha metropolis of Anambra State, Nigeria. More so, eligible participants were determined using the Diabetic Inpatients’ Depressive Symptoms’ Observation Checklist (DIDSOC) developed by the researchers. Besides being depressed, the study's eligibility criteria also included being a Type 2 diabetic patient (see Fig. 1). From the accessible population, the researchers identified eighty (80) Type 2 diabetic inpatients who met the inclusion criteria and were then randomly assigned to treatment and control groups. The mean age of the participants was 52.79 ± 21.89 years. Table 1 shows the demographic characteristics of the study's participants.
Figure 1.
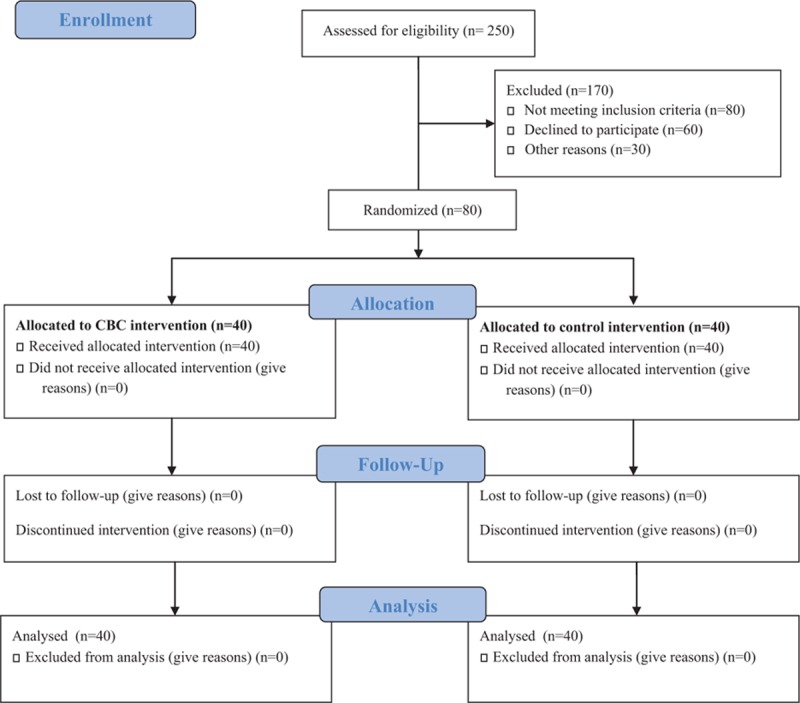
Flow diagram of participant's eligibility criteria.
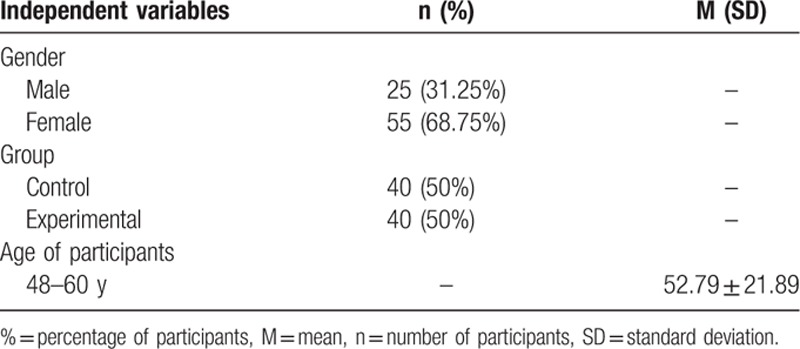
Table 1.
Summary statistics for demographic information of the study's participants.
2.3. Procedure
Only the Type 2 diabetic inpatients who met the inclusion criteria were selected as participants. The criterion was based on their scores in the BDI-II and DIDSOC, which indicates the severity of depression. Overall, a pretest was given to participants in both groups before the intervention (Time 1). Participants with severe depression were purposively selected and randomized into control and treatment groups. However, in order to avoid selection and expectation bias, the researchers concealed the assignment sequence until the moment before group assignment. This allocation concealment prevented the study's participants and caregivers from predicting and manipulating the assignment sequence. The allocation concealment was also combined with blinding. Using the blinding technique enabled the researchers to ensure that the group assignment remains concealed after assignment and not deliberately disclosed until after the study is completed.
The treatment process for mitigating the depressive symptoms of the Type 2 diabetic inpatients was guided by the cognitive behavioral coaching manual for depression adapted from David et al.[11] Conversely, the control intervention was based on conventional counseling approach (one not anchored on any theoretical orientation). By counseling not based on any theoretical orientation, the researchers mean just giving advice and instruction about managing depression in order to guide the judgment of the individual participants to make decision independently about health behavior change. Thus, in the control intervention, the researchers merely gave advice and instruction about managing depression to the participants in the control group to guide their judgment to make autonomous decisions about dealing with depression arising from their diabetic condition.
Furthermore, the participants in the treatment group took part in the cognitive behavioral coaching program for 18 sessions (sessions were held twice per week) for 9 consecutive weeks that lasted 50 minutes each. However, participants in the control group took part in a conventional counseling for 18 sessions (sessions were held twice per week) for 9 consecutive weeks that lasted 50 minutes each. After the end of the intervention, a post-test was administered (Time 2). However, a third assessment was done after 6-month follow-up meetings with the participants (Time 3). Twenty (20) professional caregivers with adequate background in the administration and interpretation of the depression measures assisted in the data collection throughout the study using the Diabetic Inpatients’ Depressive Symptoms’ Observation Checklist (DIDSOC) developed by the researchers.
2.4. Measure
2.4.1. Beck's Depression Inventory-II (BDI-II)
The BDI-II is a widely validated and an internally consistent self-report inventory which contains 21 items that assess the occurrence and severity of the symptoms of depression.[28–30] The BDI-II has 2 subscales, namely, affective (8 items) and somatic (13 items). The BDI-II is scored on a 4-point scale of 0–3 arranged in increasing severity about a particular symptom of depression, bringing the BDI–II in tandem with DSM–IV criteria. Each of the 21 items corresponding to a symptom of depression is summed to give a single score. The cutoffs used in the interpretation of scores in the BDI-II ranges from: 0 to 13= minimal depression; 14 to 19= mild depression; 20 to 28=moderate depression; and 29 to 63=severe depression. Thus, higher total scores indicate more severe depressive symptoms. The internal reliability consistency of the BDI-II in the current study is 0.89 alpha.
2.4.2. Diabetic Inpatients’ Depressive Symptoms’ Observation Checklist (DIDSOC)
The DIDSOC is a 21 items checklist used by the professional caregivers of the inpatients with Type 2 diabetes mellitus to rate the severity of depression in the patients. The DIDSOC was adapted by the researchers from the Hamilton Rating Scale for Depression (HAM-D).[31] In the DIDSOC, the higher the score, the more severe the depression experienced by the diabetic inpatients as in: 0 to 7 = minimal depression, 8 to 13 = mild depression, 14 to 18 = moderate depression, 19 to 22 = severe depression, >23 = very severe depression. The construct validity of the items in the DIDSOC was determined using Principal Component Analysis.
2.5. Intervention package
2.5.1. Cognitive Behavioral Coaching for Depression Manual (CBCDM)
The CBCDM is based on the framework of rational-emotive and cognitive-behavioral therapy manual for treatment of depression, which is an evidence-based manual that has been tested in a randomized clinical trial.[11] Thus, with the cognitive behavioral coaching for depression manual, the researchers ensured that after creating rapport and explaining the basic rules of therapy, such as scheduling and confidentiality, the rationale of the cognitive behavioral coaching program and the goals of the program are discussed with the participants. Nevertheless, in the current study, the overall cognitive behavioral coaching treatment focused on the problematic beliefs mediating depressive symptoms, namely, demandingness, self-downing, awfulizing, and low frustration tolerance. Furthermore, cognitive, behavioral, and emotive techniques were used to change the target problematic beliefs of the participants.
Worth noting is that the cognitive behavioral coaching program as contained in this manual is a group-focused face-to-face psychological treatment for managing depression. Furthermore, the cognitive behavioral coaching program as used by the researchers is a health coaching intervention underpinned by cognitive and behavioral principles and aimed at engaging and motivating the individual participants towards managing their depressive symptoms. Thus, during the CBC intervention, several cognitive and behavioral coaching strategies and techniques (such as goal setting, motivational interviewing, cognitive restructuring, and coping imagery) were used to tackle psychological blocks to diabetes health goal achievement and reducing unhelpful emotions by examining the individual participant's health inhibiting thinking and then assisting them to develop health enhancing behaviors as suggested by coaching experts.[32–34]
Overall, the cognitive-behavioral coaching program of this study partly followed similar steps and implementation guidelines for CBC intervention as used by Karas and Spada[17] and thus the researchers focused on 6 major areas of intervention, namely, enhancing participants’ motivation to change; goal setting; monitoring progress; dietary management; disputing unrealistic beliefs; and relapse prevention. In fact, these areas of intervention were considered vital in that there is a growing number of evidence in the psychological literature supporting the usefulness of dealing with these areas in therapeutic work,[35–41] and they are also seen as key target areas in the cognitive-behavioral therapy approach.[42] Each of the 6 key areas was implemented in 3 sessions respectively, making up a total of the 18 sessions of the CBC program for managing depression in the Type 2 diabetic inpatients. The intervention was delivered by the first, second, third, and seventh authors of this manuscript given their background in the CBC approach.
2.5.2. Design and data analyses
The design of this study was pretest-post-test randomized control group design. The repeated measures analysis of covariance (ANCOVA) was used to show the significant effects of cognitive behavioral coaching program on depressive symptoms in the treatment group compared to the control group at different time interval. The univariate analysis of variance (ANOVA) was also employed. The researchers further reported partial eta squared
 |
for this design. Prior to analyses, screening for missing values and violation of assumptions was done with the aid of SPSS 16.
3. Results
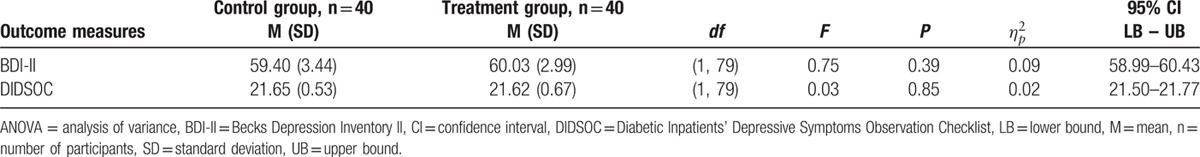
First, the researchers sought to examine whether the depressive symptoms of Type 2 diabetic inpatients will not significantly differ across the treatment and control groups at baseline. Results in Table 2 shows that at baseline (Time 1), the control group's mean depression was 59.40 ± 3.44, whereas that of the treatment group was 60.03 ± 2.99 as measured by the BDI-II. On the other hand, the control group's mean depression was 21.65 ± 0.53, whereas that of the treatment group was 21.62 ± 0.67 as measured by the DIDSOC. From Table 2, it can be seen that the depressive symptoms of the Type 2 diabetic inpatients was severe and did not differ significantly across the treatment and control groups at baseline, BDI-II [F(1, 79)=; P > 0.05; 95% CI: 58.99–60.43], and DIDSOC [F(1, 79)=; P > 0.05; 95% CI: 21.50–21.77].
Table 2.
Summary of univariate ANOVA showing depressive symptoms of the Type 2 diabetic inpatients at baseline (Time 1).
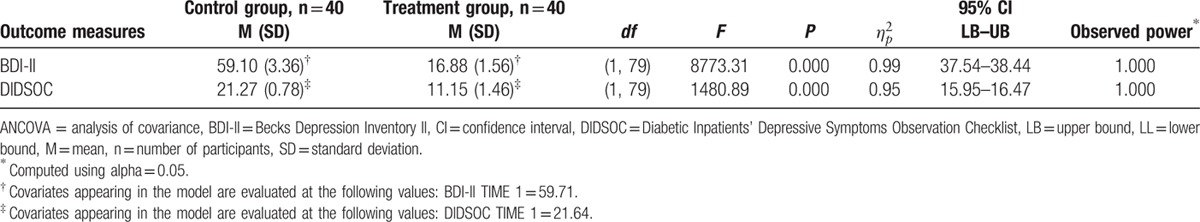
Second, the researchers examined whether cognitive behavioral coaching will significantly reduce the depressive symptoms among the Type 2 diabetic inpatients in the treatment group compared to those in the control group over time. Results in Table 3 show an exact probability value of 0.00 which is less than the “a priori” probability value of 0.05 as measured by the BDI-II and DIDSOC at Time 2. This implies that the cognitive behavioral coaching program significantly reduced depressive symptoms of the Type 2 diabetic inpatients in the treatment group compared to those in the control group, BDI-II [F (1, 79)=8773.31; P < 0.0001; CI: 37.54–38.44], and DIDSOC [F (1,97)=1480.89; P < 0.0001; CI: 15.95–16.47]. Furthermore, the
 |
values of 0.99 and 0.95 obtained with the BDI-II and DIDSOC respectively is an indication that the cognitive behavioral coaching program was strongly effective in helping Type 2 diabetic inpatients in the treatment group reduce depressive symptoms compared to those in control group.
Table 3.
Summary of repeated measures ANCOVA showing the significant effect of cognitive-behavioral coaching on depressive symptom of the Type 2 diabetic inpatients at post-test (Time 2).
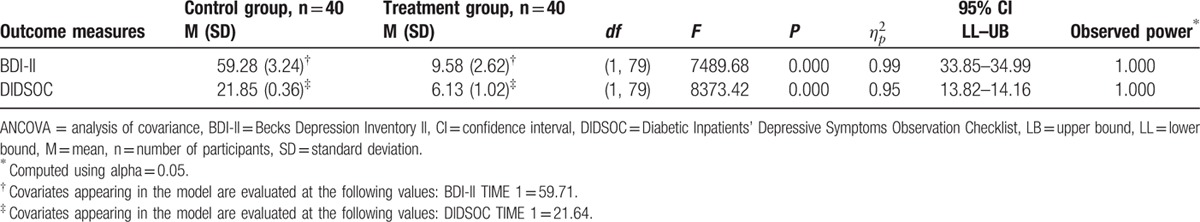
Third, the researchers sought to ascertain whether the reduction in depressive symptoms due to cognitive behavioral coaching among the Type 2 diabetic inpatients in the treatment group would be maintained. Results in Table 4 show an exact probability value of 0.000 which is less than the “a priori” probability value of 0.05 as measured by the BDI-II and DIDSOC at Time 3. This implies that the effects of the cognitive behavioral coaching program on depressive symptoms’ reduction in the Type 2 diabetic inpatients in the treatment group remained consistent compared to those in the control group, BDI-II [F (1, 79)=7489.68; P < 0.0001; CI: 33.85–34.99], and DIDSOC [F (1, 79)=8373.42; P < 0.0001, CI: 13.82–14.16]. The
 |
values of 0.99 and 0.95 from the BDI-II and DIDSOC, respectively, is an indication that the cognitive behavioral coaching program was strongly effective and consistent in helping the Type 2 diabetic inpatients in the treatment group deal with their depressive symptoms compared to those in the control group.
Table 4.
Summary of repeated measures ANCOVA showing the significant effect of cognitive-behavioral coaching on depressive symptom of the Type 2 diabetic inpatients at a 6-month follow-up (Time 3).
Overall, Fig. 2 shows how the cognitive behavioral coaching program significantly reduced depressive symptoms in the Type 2 diabetic inpatients in the treatment group compared to those in the control group over time and how this gain was maintained at 6 months follow-up meetings. The covariates appearing in the model are evaluated at the following values: BDI-II TIME 1 = 59.71 and DIDSOC TIME 1 = 21.64. Thus, Fig. 2 indicates that the reduction in depression experienced by the treatment group persisted over time.
Figure 2.
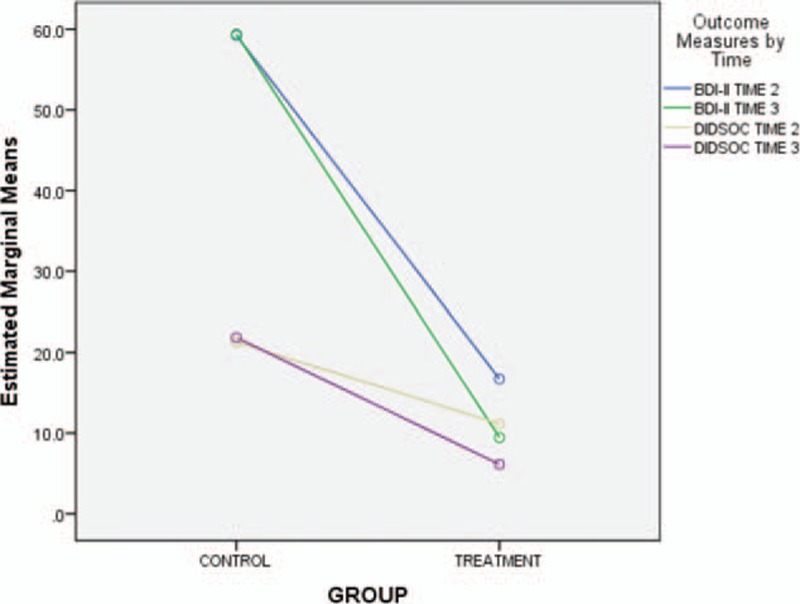
Effects of cognitive behavioral coaching program on depressive symptoms among diabetic inpatients.
4. Discussion
The purpose of this study was to investigate the effects of cognitive behavioral coaching program on depressive symptoms among inpatients in Onitsha metropolis of Anambra State, Nigeria. The study found that the level of depressive symptoms in the diabetic inpatients was severe and this did not differ significantly across the treatment and control groups at baseline. This finding supports research evidences which indicate the presence of depression in the Nigerian population,[22–24] and those with diabetes.[6–8] However, the cognitive behavioral coaching significantly reduced the depressive symptoms in the Type 2 diabetic inpatients in the treatment group compared to those in control group at end of the intervention. The effects of the cognitive behavioral coaching remained consistent for the treatment group at 6-month follow-up meetings. The findings demonstrates how the diabetic inpatients, having been exposed to cognitive behavioral coaching were able to identify, examine and change their self-defeating thoughts and beliefs, develop productive behaviors and become more skilled at emotional management and thus supports Gladeana.[14] They were enabled to learn that their thoughts, emotions, and behaviors are keys to understanding their perception of problems and situations. This was unlike their counterparts in the control group who did not have the opportunity of gaining such insights. The finding of this study lend credence to previous studies[16,17,19] which showed that cognitive behavioral coaching is effective in managing depression among individuals. The findings also support Palmer and Gyllensten[34] who argued that psychological coaching could be used to prevent the development of depression or help a coaching client to intervene at a very initial stage.
However, certain limitations might be associated with the current study in view of the inpatient versus outpatient treatment divergence. Therefore, the researchers acknowledge that there might be important differences in utilizing cognitive behavioral coaching as inpatient treatment versus cognitive behavioral coaching as outpatient treatment for the Type 2 diabetic patients. Therefore, future researchers may need to compare inpatient CBC treatment with outpatient treatment by implementing at least 10 CBC outpatient sessions and 10 CBC inpatient sessions. Such research endeavor would also have to articulate the major differences between inpatient depressiveness and outpatient depressiveness. Additionally, the researchers suggest that future research would have to use much larger samples, carryout a cross-sectional and/or an in-depth longitudinal studies on the efficacy of cognitive behavioral coaching approach in assisting the Nigerian diabetic inpatients’ population.
Overall, the researchers hope that more rigorous methodologies, when applied by future researches, will help to further confirm the efficacy of a cognitive-behavioral coaching program, and also spur researchers to conduct comparative investigations with other psychotherapies in terms of cost-effectiveness and effectiveness in Nigeria. Therefore, cognitive behavioral coaching researchers who might want to implement this program should follow the similar step and techniques adopted in this study to generate positive outcomes. But cognizance must be taken not to conduct the follow-up assessment so close to the end of the intervention, as it might be more important to know whether this reduction in depression experienced by the treatment group persists over a much longer time. In that regard, a third assessment 9 to 12 month later might be helpful in future intervention in Nigeria.
5. Conclusion
Evidently, depression can impede the Type 2 diabetic inpatients’ ability to cope with the disease condition and lifestyle changes but psychological treatments, such as cognitive behavioral coaching can be effective in helping them to cope with daily life. In fact, cognitive behavioral coaching program offered to the Type 2 diabetic inpatients had significant effects on their depressive symptoms reduction over time. Before the commencement of the intervention program by the researchers, the diabetic inpatients’ depressive symptoms remained considerably severe, but after the intervention, they were able to adjust their thoughts and feelings which resulted in reduction of their depressive symptoms. Thus, the outcome of the current study seems beneficial to different groups of people including the guidance counselors and other mental health professionals. In that regard, the Nigerian guidance counselors would need to conduct follow-up studies with the diabetic inpatients to assess the efficacy of cognitive-behavioral coaching using mixed method designs. The researchers feel that the Nigerian therapists are in better position to support cognitive-behavioral coaching programs aimed at improving diabetic inpatients’ wellbeing in the Nigerian setting. In the light of the present study's outcome, the researchers also urge clinicians and mental health professionals in Nigeria to support and implement evidence-based cognitive behavioral coaching interventions to assist the diabetic patients in dealing with their day-to-day psychosocial burdens, such as depression. In addition, medical psychologists are urged to support cognitive-behavioral coaching interventions designed to assist the Nigerian inpatients towards achieving wellness.
Acknowledgments
The researchers would like to appreciate all the professional caregivers that assisted in the data collection process. The researchers are also very much grateful to the Editor-In-Chief and the 3 Anonymous Reviewers whose expertise helped to improve the standard of reporting of this manuscript. Finally, the researchers would like to thank staff and management of Otusum Consult, Training and Services, Nigeria, for advice on the statistical method employed in the study.
Footnotes
Abbreviations: ANCOVA = analysis of covariance, BDI-II = Beck's Depression Inventory version n, CBC = Cognitive Behavioral Therapy, CBCDM = Cognitive Behavioral Coaching for Depression Manual, DIDSOC = Diabetic Inpatients’ Depressive Symptoms’ Observation Checklist, HAM-D = Hamilton Rating Scale for Depression.
The authors have no conflicts of interest to disclose.
References
- 1.World Health Organization. Depression. Updated April, 2016. Fact sheet No. 369. Available from: http://www.who.int/mediacentre/factsheets/fs369/en/ Accessed May 1, 2016. [Google Scholar]
- 2.Ferrari AJ, Somerville AJ, Baxter AJ, et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol Med 2013; 43:471–481. [DOI] [PubMed] [Google Scholar]
- 3.Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007; 370:851–858. [DOI] [PubMed] [Google Scholar]
- 4.Reddy MS. Depression: the disorder and the burden. Indian J Psychol Med 2010; 32:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. The Global Burden of Disease—2004. Geneva, Switzerland: WHO Press; 2008. [Google Scholar]
- 6.American Diabetes Association. Depression. Updated May 14, 2014. Available from: http://www.diabetes.org/living-with-diabetes/complications/mentalhealth/depression.html Accessed May 1, 2016. [Google Scholar]
- 7.Diabetes Australia. Depression and mental health. 2015. Available from: https://www.diabetesaustralia.com.au/depression-and-mental-health Accessed April 25, 2016. [Google Scholar]
- 8.National Institute of Mental Health at National Institutes of Health, United States. Chronic illness and mental health: recognizing and treating depression. 2015. Available from: http://www.nimh.nih.gov/health/publications/chronic-illness-mental-health-2015/nih-15-mh-8015_151898.pdf Accessed June 26, 2015. [Google Scholar]
- 9.Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications 2005; 19:113–122. [DOI] [PubMed] [Google Scholar]
- 10.Jovinelly J. Diabetes and Depression: Mental Health Concerns for Type 2 Diabetes Patients. May 14, 2014. [medically reviewed by Baker J.]. Available from: http://www.healthline.com/health/type-2-diabetes/depression Accessed June 26, 2015. [Google Scholar]
- 11.David D, Kangas M, Schnur JB, et al. REBT Depression Manual: Managing Depression Using Rational Emotive Behavior Therapy. Romania: Babes-Bolyai University; 2004. [Google Scholar]
- 12.Keeran D. Counseling in a book: help for common life problems. 2012. Available from: http://www.ctihalifax.com/images/CounselingInABook.pdf Accessed July 20, 2016. [Google Scholar]
- 13.Palmer S, Szymanska K. Palmer S, Whybrow A. Cognitive behavioral coaching: an integrative approach. Handbook of Coaching Psychology: A Guide for Practitioners. New York, NY: Routledge/Taylor & Francis Group; 2008. 86–117. [Google Scholar]
- 14.Gladeana M. Cognitive Behavioral Coaching Works! 2016. Available from: http://www.cognitivebehaviouralcoachingworks.com/ Accessed June 26, 2016. [Google Scholar]
- 15.Neenan M. From cognitive behaviour therapy (CBT) to cognitive behaviour coaching (CBC). J Rat-Emo Cog-Behav Ther 2008; 26:3–15. [Google Scholar]
- 16.Grant AM. Personal life coaching for coaches-in-training enhances goal attainment, insight and learning. Coaching Int J Theor Res Pract 2008; 1:54–70. [Google Scholar]
- 17.Karas D, Spada MM. Brief cognitive-behavioural coaching for procrastination: a case series. Coaching Int J Theor Res Pract 2009; 2:44–53. [Google Scholar]
- 18.Kearns H, Forbes A, Gardiner M. A cognitive behavioral coaching intervention for the treatment of perfectionism and self-handicapping in a non-clinical population. Behav Change 2007; 24:157–172. [Google Scholar]
- 19.Green S, Grant AM, Rynsaardt J. Evidence-based life coaching for senior high schools: building hardiness and hope. Int Coaching Psychol Rev 2007; 2:24–32. [Google Scholar]
- 20.Green LS, Oades LG, Grant AM. Cognitive-behavioral, solution-focused life coaching: enhancing goal striving, well-being and hope. J Positive Psychol 2006; 1:142–149. [Google Scholar]
- 21.Jefferson V, Jaser SS, Lindemann E, et al. Coping skills training in a telephone health coaching program for youth at risk for type 2 diabetes. J Pediatr Health Care 2011; 25:153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balogun AG, Olawoye PA. Correlates of depression among prison inmates in South-Western Nigeria. Nig J Appl Behav Sci 2013; 1:43–55. [Google Scholar]
- 23.Nwaopara U, Stanley P. Prevalence of depression in Port Harcourt Prison. J Psychiatry 2015; 18:340. [Google Scholar]
- 24.Nwaopara U, Stanley P. Clinical factors as predictors of depression in a Nigerian Prison Population. J Psychiatry 2015; 18:345. [Google Scholar]
- 25.Mental Health Foundation, England. Depression. 2016. Available from: https://www.mentalhealth.org.uk/a-to-z/d/depression Accessed June 29, 2016. [Google Scholar]
- 26.Chan JEC, reviewer. Beck depression inventory (BDI). February 01, 2013. Available from: http://www.scireproject.com/outcome-measures-new/beck-depression-inventory-bdi Accessed June 13, 2015. [Google Scholar]
- 27.Brhlikova P, Pollock AM, Manners R. Global burden of disease estimates of depression—how reliable is the epidemiological evidence? J R Soc Med 2011; 104:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory II (BDI-II). 2nd edSan Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 29.Beck AT, Steer RA, Ball R, et al. Comparison of Beck depression inventories-IA and-II in psychiatric outpatients. J Pers Assess 1996; 67:588–597. [DOI] [PubMed] [Google Scholar]
- 30.Steer RA, Rissmiller DJ, Beck AT. Use of the Beck depression inventory with depressed geriatric patients. Behav Res Ther 2000; 38:311–318. [DOI] [PubMed] [Google Scholar]
- 31.Hamilton MA. Rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palmer S. Health coaching: a developing field within health education. Health Educ J 2004; 63:189–191. [Google Scholar]
- 33.Palmer S. Health coaching to facilitate the promotion of healthy behavior and achievement of health-related goals. Int J Health Promot Educ 2003; 41:91–93. [Google Scholar]
- 34.Palmer S, Gyllensten K. How cognitive behavioral, rational emotive behavioral or multimodal coaching could prevent mental health problems, enhance performance and reduce work related stress. J Rat-Emo Cog-Behav Ther 2008; 26:38–52. [Google Scholar]
- 35.Ariely D, Wertenbroch K. Procrastination, deadlines and performance: self-control by precommitment. Psychol Sci 2002; 13:219–224. [DOI] [PubMed] [Google Scholar]
- 36.Austin JT, Vancouver JB. Goal constructs in psychology: structure, process and content. Psychol Bull 1996; 120:338–375. [Google Scholar]
- 37.Beck AT. The current state of cognitive therapy: a 40-year retrospective. Arch General Psychiatry 2005; 62:953–959. [DOI] [PubMed] [Google Scholar]
- 38.DiClemente CC, Prochaska JO, Fairhurst SK, et al. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consulting Clin Psychol 1991; 59:295–304. [DOI] [PubMed] [Google Scholar]
- 39.Gotlib IH, Hammen CL. Handbook of Depression. New York: Guilford Press; 2002. [Google Scholar]
- 40.Prochaska JO, Velicier WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol 1994; 13:39–46. [DOI] [PubMed] [Google Scholar]
- 41.Sheldon KM, Kasser T, Smith K, et al. Personal goals and psychological growth: testing an intervention to enhance goal attainment and personality integration. J Pers 2002; 70:5–31. [DOI] [PubMed] [Google Scholar]
- 42.Beck AT, Wright FD, Newman CF, et al. Cognitive Therapy of Substance Abuse. New York: Guilford Press; 1993. [PubMed] [Google Scholar]


