Abstract
Human exposure to environmental chemicals as persistent organic pollutants (POPs) is usually assessed considering each pollutant individually, with little attention to concentrations of mixtures in individuals or social groups. Yet, it may be relatively common for humans to have low and high concentrations of numerous POPs. The study objectives were to analyze the number of POPs detected per person at high concentrations in the U.S. population, and the associations between such type of indicators and socioeconomic factors as gender, race / ethnicity, education, and poverty level. From 91 POPs analyzed in serum samples of 4,739 individuals in three subsamples of the National Health and Nutrition Examination Survey (NHANES) 2003–2004 (the last period with valid updated individual data for the compounds considered in the present study), we computed the number of POPs whose serum concentrations were above selected cutoff points. POPs included were 13 organochlorine compounds (OCs), 10 polybrominated diphenyl ethers (PBDEs), the polybrominated biphenyl (PBB) 153, 38 polychlorinated biphenyls (PCBs), 17 polychlorinated dibenzo-p-dioxins and dibenzofurans (PCDDs/Fs), and 12 perfluorinated compounds (PFCs). Over 13% of participants had ≥10 of the 37 most detected POPs each at a concentration in the top decile (P90). Over 30% of subjects with total toxic equivalency (TEQ) ≥P75, had ≥10 of 24 POPs not included in TEQ calculations at concentrations ≥P90. Compared to non-Hispanic whites, the adjusted odds ratio of having ≥10 of the 37 POPs at P90 was 9.2 for non-Hispanic blacks and 0.18 for Mexican Americans. Poverty, body mass index, age, and gender were also independently associated with having ≥10 POPs in the top decile. More than one tenth of the US population may have ≥10 POPs each at concentrations in the top decile. Such pattern is nine times more frequent in Non-Hispanic blacks and four times less frequent in Mexican Americans than in non-Hispanic whites.
Introduction
There is abundant evidence worldwide on lifelong human contamination from mixtures of environmental chemicals as persistent organic pollutants (POPs) [1–7]; yet, the vast majority of studies report each pollutant individually, with little attention to concentrations of mixtures in individual persons or social groups. Thus, the complex features of such internal, body contamination remain unsatisfactorily characterized. Biomonitoring surveys, for instance, do not integrate the number of compounds detected per person and the concentration of each compound [1,4–6,8–12]. Possible health effects of POPs include a variety of developmental, metabolic, neurodegenerative, and neoplastic disorders [5,8,9,10,12–24]. Reasonable concerns exist about such effects at low concentrations; such issues can be integrated with the fact that it is common for humans to have mixtures of POPs at low and high concentrations [6,8,12].
Approaches to these issues include ‘Environment-Wide Association Studies’ (EWAS), and analyses of concentrations of POPs combined, using estimates of total body burden, or different sums of concentrations [24–27]. Efforts to improve exposure assessment must continue: not only to advance etiologic studies and risk assessment, but also to foster knowledge on the characteristics of human chemical contamination itself. Such knowledge is a recognized right of citizens in democratic societies; it is also essential to evaluate the impacts of health, industrial, and related policies [1,5,8,10,28,29]. Indeed, the sources and pathways of exposure to pollutants are socioeconomic and cultural. Thus, strong relationships exist between concentrations of individual POPs and social factors, including income, education, and race / ethnicity [1,30–39]. Unfortunately, such relationships have seldom been analyzed integrating several compounds and their concentrations.
Recently, a set of indicators that integrate the number of compounds detected per person and their corresponding concentrations was proposed, including the number of compounds detected at high concentrations. The analyses were based on the general population of Catalonia, Spain [12]. Because studies in the U.S. on combinations of POPs and other chemicals raised relevant questions about the levels and effects of such mixtures [8,9,16,40–44], and because of the relatively large size of the U.S. population, we aimed at applying the methodology [8] to the U.S. general population.
Therefore, the objectives of the present study were to analyze the number of POPs detected per person at high concentrations (nPhc) in the U.S. National Health and Nutrition Examination Survey (NHANES), and to analyze the associations between such indicator and main socioeconomic factors. Our main hypotheses were that most of the U.S. population would have POPs at low and high concentrations, and that sociodemographic factors (such as age, gender, body mass index (BMI), parity, or income) that are often related with POP concentrations when each compound is analyzed individually [2,12,13,30,34,35] would continue to show similar relationships when the POPs are jointly analyzed [12].
Materials and Methods
Data
Conducted by the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS), the National Health and Nutrition Examination Survey (NHANES) collects nationally representative environmental biomonitoring data from about 5,000 annual participants in each two-year cycle [2,45–48]. NHANES is a publicly available data set, and all participants provide written informed consent, consistent with approval by the NCHS Institutional Review Board. Ethical approval for use of NHANES data is not required as it is anonymized. We examined data from NHANES laboratory and demographic files corresponding to 2003–2004, which is the last period with valid updated individual data for compounds considered in the present study [45,47]. Except for perfluorinated compounds (PFCs), in NHANES 2005–2006 and 2007–2008 serum concentrations of POPs were measured using weighted pooled-samples, and no data for POPs have been published for NHANES 2009–2010 and 2011–2012 [47]. Therefore, it is not possible to calculate the number of POPs detected per person at high concentrations in more recent periods.
In each NHANES, most chemicals or their metabolites were measured in serum samples from random subsamples of about 2,500 participants aged 12 years and older. The chemicals’ concentrations were analyzed by CDC’s Environmental Health Laboratory using mass spectrometry and related methods [2,46]. Data for 91 POPs were analyzed, including: 13 organochlorine compounds (OCs) and their respective metabolites; 10 polybrominated diphenyl ethers (PBDEs); the polybrominated biphenyl (PBB) 153; 29 non-dioxin-like polychlorinated biphenyls (PCBs); 3 dioxin-like coplanar PCBs; 6 dioxin-like mono-ortho-substituted PCBs; 10 polychlorinated dibenzofurans (PCDFs); 7 polychlorinated dibenzo-p-dioxins (PCDDs); and 12 PFCs [46] (S1 Table). Thus, serum concentrations of lipophilic chemicals (e.g., dioxins and PCBs) are presented per gram of total lipid (better reflecting the amount stored in body fat) [1,2,12,31,46]; results of analyses per whole weight of serum were similar and are not presented. Concentrations of PFCs, non-lipophilic POPs, are shown per liter of serum. Limits of detection (LOD) for whole weight POP concentrations were different for each serum sample of each person [45,46], while LODs for lipid-adjusted concentrations were the same values for all samples and individuals (values ranged from 3.8 pg/g of lipid and 7.8 ng/g of lipid) [2,45,46]. Finally, LODs for PFCs ranged from 0.1 to 1.0 μg/L [46].
We considered important covariates as age, sex, race/ethnicity (non-Hispanic white, henceforth ‘White’; Mexican American; non-Hispanic black, henceforth ‘Black’; other Hispanic; and other), education (categorized to less than high school diploma, high school diploma, and greater than high school diploma), and body mass index (BMI) in kg/m2. To estimate the participants' income we used the family’s total income divided by the family size-specific poverty threshold income ratio (PIR), with two categories: “Low” income (PIR < 2), and “High” income (PIR ≥ 2) [43,45]. In women, we also considered the number of pregnancies resulting in live births, and the number of children breastfed ≥1 month (henceforth, ‘breastfeeding’) [45].
Statistical analyses
The present study included 4,739 participants ≥20 years old (for all adults 85 years and older, age was coded at 85 years to reduce the risk of disclosure) [45]. They came from three subsamples (S2 Table). There were no significant differences between the 1,610, 1,585 and 1,544 participants of each subsample in a broad range of sociodemographic variables (including sex, race/ethnicity, educational level, PIR, BMI, number of pregnancies or breastfeeding) (S2 Table).
We imputed the unmeasured POP values by the median serum concentration of each POP according to age, sex, race/ethnicity, PIR, BMI, and, in women, number of pregnancies [49,50]. In 79 POPs the imputation was performed using concentrations adjusted by lipids, and in 12 PFCs, in μg/L. We calculated the total toxic equivalency (TEQ) [51,52] for 26 POPs: 3 dioxin-like coplanar PCBs, 6 dioxin-like mono-ortho-substituted PCBs, 10 PCDFs, and 7 PCDDs [45,46]. To compare POP concentrations in the present study and pooled concentrations in NHANES 2005–2006 and 2007–2008 we computed concentrations of POPs by sex, race/ethnicity and age groups [46,47]. We also compared PFC serum concentrations in the present study and concentrations in NHANES of 2005–2006, 2007–2008, 2009–2010 and 2011–2012 [46,47]. Descriptive values for POP concentrations imputed are summarized in S1 Table, sorted from the highest to the lowest percentage of detection.
Based on previous work by Porta et al. (2012) [12], we calculated the number of POPs detected in each person at high concentrations (nPhc) as follows: for each subject we added the number of POPs whose serum concentrations were equal to or greater than a selected cutoff point [12]. To be conservative, in the main analyses we included only 37 POPs that had been detected (each) in >85% of the study subjects (henceforth called the most prevalent POPs). Such 37 POPs were: 2 OCs, 3 PBDEs, PBB 153, 23 non-dioxin-like PCBs, 3 dioxin-like PCBs, one PCDD [1,2,3,4,6,7,8-Heptachlorodibenzo-p-dioxin (HpCDD)], and 4 PFCs (S1 Table). Ancillary analyses included 50 compounds detected in >50% of subjects. Finally, other analyses included all 91 POPs, with quartiles, quintiles and deciles defined after the imputation of concentrations (S1 Table) [12]. As usual, serum concentrations of POPs did not follow a normal distribution [31], and the increment of concentrations in the highest percentiles was very strong (e.g., for p,p’-DDE the increment of concentrations between P75 and P90 was of 2.14 times, and between P90 and the maximum it was 14.5 times; for PCB 153 the corresponding figures were 53% and 12.36 times, respectively) (S1 Table).
We defined ‘high concentrations’ using compound- and population-specific percentiles, based on actual POP distributions, as cutoff points [12,43,44]. In the main statistical analyses the cutoff point used was percentile 90 (P90), the upper decile (S1 Table).
Univariate statistics were computed as customary [53,54]. The highest correlations were observed between PCB congeners 170 and 180, 138 and 153, 146 and 153 (all Spearman’s ρ >0.982 and p’s <0.001). Fisher’s exact test for homogeneity was applied to assess the relationship between two categorical variables. For comparisons between continuous variables ANOVA, Kruskal-Wallis, and Mann-Whitney’s U tests were used. When a tendency was observed, Mantel–Haenszel’s χ2 test and Jonckheere-Terpstra test for linear trend were used.
To estimate the magnitude of associations between the socioeconomic factors and the number of most prevalent POPs with concentrations in the upper decile, multivariate-adjusted odds ratios (ORs) and their corresponding 95% confidence intervals (CI) were calculated by unconditional logistic regression with progressive degrees of adjustment [55]. The main effects of all predictors were independently explored in the base models, and final models were adjusted for age, gender, BMI, race/ethnicity and poverty income, in accordance with the nature of the variables and the study objectives. The number of POPs with concentrations in the upper decile was tested in different regression models using 3 different categorizations (all dichotomous): ≥1 POP (vs. no Phc), ≥6 POPs (vs. <6 POPs) and ≥10 POPs (vs. <10 POPs). Categorical ordinal variables were analyzed for a linear dose–response relation through the multivariate analogue of Mantel’s extension test; when a linear trend was not apparent, the probability test was used. Analyses were conducted using SPSS version 18 (SPSS, Armonk, NY, USA, 2009).
Results
Over 67% of the 4,739 participants (73.8% of men and 61.1% of women) had one or more of the 37 most prevalent POPs at concentrations equal to or greater than the 90th percentile (≥P90), while 38.0% had ≥3 POPs, and over 13% had ≥10 POPs each in such top decile (Table 1 and Table 2). Over 37% of subjects had ≥10 compounds each at concentrations in the top quartile (≥P75) (S3 Table). The number of POPs detected per person ranged between 23 and 74, with an average of 49.7. Over 57% of participants had ≥50 POPs detected (S1 Fig).
Table 1. Characteristics of subjects with and without ten or more POPs with concentrations in the upper decile.
| ≥10 POPs with concentrations in the upper decile | |||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Total | Yes | No | ||||
| N (%) | N (%) | N (%) | p-value | ||||
| Total | 4,739 | (100) | 619 | (13.1) | 4,120 | (86.9) | |
| Gender | <0.001 | ||||||
| Women | 2,467 | (52.1) | 271 | (11.0) | 2,196 | (89.0) | |
| Men | 2,272 | (47.9) | 348 | (15.3) | 1,924 | (84.7) | |
| Age (years) | 49.0 | 70.0 | 45.0 | <0.001a | |||
| Race/ethnicity | <0.001 | ||||||
| Non-Hispanic white | 2,539 | (53.6) | 282 | (11.1) | 2,257 | (88.9) | |
| Mexican American | 951 | (20.1) | 21 | (2.2) | 930 | (97.8) | |
| Non-Hispanic black | 948 | (20.0) | 277 | (29.2) | 671 | (70.8) | |
| Other Hispanic | 140 | (3.0) | 19 | (13.6) | 121 | (86.4) | |
| Other | 161 | (3.4) | 20 | (12.4) | 141 | (87.6) | |
| Educational level | <0.001 | ||||||
| College or above | 2,138 | (45.2) | 243 | (11.4) | 1,895 | (88.6) | |
| High school | 1,193 | (25.2) | 140 | (11.7) | 1,053 | (88.3) | |
| < High school | 1,399 | (29.6) | 232 | (16.6) | 1,167 | (83.4) | |
| Poverty income ratio | 0.036 | ||||||
| >2 | 2,394 | (53.6) | 289 | (12.1) | 2,105 | (87.9) | |
| ≤2 | 2,075 | (46.4) | 295 | (14.2) | 1,780 | (85.8) | |
| Body mass index (kg/m2) | 27.4 | 26.7 | 27.6 | 0.004a | |||
| Underweight (<18.5) | 70 | (1.5) | 10 | (14.3) | 60 | (85.7) | <0.001b |
| Normal weight (18.5–24.9) | 1,406 | (30.3) | 193 | (13.7) | 1,213 | (86.3) | |
| Overweight (25.0–29.9) | 1,630 | (35.1) | 248 | (15.2) | 1,382 | (84.8) | |
| Obese (≥30) | 1,538 | (33.1) | 154 | (10.0) | 1,384 | (90.0) | |
| Pregnancyc | 0.741 | ||||||
| No | 93 | (5.0) | 12 | (12.9) | 81 | (87.1) | |
| Yes | 1,768 | (95.0) | 208 | (11.8) | 1,560 | (88.2) | |
| No. of pregnancies resulting in live birthsc | 2.00 | 3.00 | 2.00 | <0.001a | |||
| Breastfeedingd,e | 0.450 | ||||||
| No | 78 | (7.4) | 6 | (7.7) | 72 | (92.3) | |
| Yes | 975 | (92.6) | 106 | (10.9) | 869 | (89.1) | |
| No. of children breastfedd,e | 2.00 | 2.00 | 2.00 | 0.144a | |||
Values for age, body mass index, number of pregnancies resulting in live births and number of children breastfed are median.
Unless otherwise specified, p-Value derived from Fisher’s exact test (two-tail).
a Mann-Whitney’s U test.
b Without participants <18.5 kg/m2 of body mass index.
c Women only.
d Only women with ≥1 pregnancies resulting in live births.
e Breastfed ≥1 month.
Table 2. Characteristics of the individuals with one or more POPs with concentrations in the upper decile.
| No. of POPs with concentrations in the upper decile | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Total | ≥10 | 6 to 9 | 3 to 5 | 2 | 1 | |||||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | p-value | |||||||
| Total | 3,184 | (67.2) | 619 | (19.4) | 375 | (11.8) | 807 | (25.3) | 560 | (17.6) | 823 | (25.8) | |
| (Cumulative %) | (19.4) | (31.2) | (56.6) | (74.2) | (100) | ||||||||
| Gender | <0.001 | ||||||||||||
| Women | 1,507 | (47.3) | 271 | (18.0) | 135 | (9.0) | 406 | (26.9) | 272 | (18.0) | 423 | (28.1) | |
| Men | 1,677 | (52.7) | 348 | (20.8) | 240 | (14.3) | 401 | (23.9) | 288 | (17.2) | 400 | (23.9) | |
| Age (years) | 57.0 | 70.0 | 60.0 | 64.0 | 46.0 | 43.0 | <0.001a | ||||||
| Race/ethnicity | <0.001b | ||||||||||||
| Non-Hispanic white | 1,780 | (55.9) | 282 | (15.8) | 233 | (13.1) | 530 | (29.8) | 270 | (15.2) | 465 | (26.1) | |
| Mexican American | 581 | (18.2) | 21 | (3.6) | 76 | (13.1) | 159 | (27.4) | 154 | (26.5) | 171 | (29.4) | |
| Non-Hispanic black | 629 | (19.8) | 277 | (44.0) | 40 | (6.4) | 76 | (12.1) | 93 | (14.8) | 143 | (22.7) | |
| Other Hispanic | 79 | (2.5) | 19 | (24.1) | 11 | (13.9) | 17 | (21.5) | 16 | (20.3) | 16 | (20.3) | |
| Other | 115 | (3.6) | 20 | (17.4) | 15 | (13.0) | 25 | (21.7) | 27 | (23.5) | 28 | (24.3) | |
| Educational level | <0.001 | ||||||||||||
| College or above | 1,403 | (44.2) | 243 | (17.3) | 168 | (12.0) | 339 | (24.2) | 248 | (17.7) | 405 | (28.9) | |
| High school | 790 | (24.9) | 140 | (17.7) | 103 | (13.0) | 210 | (26.6) | 144 | (18.2) | 193 | (24.4) | |
| < High school | 984 | (31.0) | 232 | (23.6) | 103 | (10.5) | 256 | (26.0) | 168 | (17.1) | 225 | (22.9) | |
| Poverty income ratio | 0.002 | ||||||||||||
| >2 | 1,608 | (53.4) | 289 | (18.0) | 189 | (11.8) | 389 | (24.2) | 295 | (18.3) | 446 | (27.7) | |
| ≤2 | 1,406 | (46.6) | 295 | (21.0) | 175 | (12.4) | 365 | (26.0) | 240 | (17.1) | 331 | (23.5) | |
| Body mass index (kg/m2) | 27.2 | 26.7 | 28.1 | 26.8 | 27.6 | 27.8 | 0.084a | ||||||
| Pregnancyc | 0.447b | ||||||||||||
| No | 51 | (4.4) | 12 | (23.5) | 4 | (7.8) | 9 | (17.6) | 8 | (15.7) | 18 | (35.3) | |
| Yes | 1,106 | (95.6) | 208 | (18.8) | 97 | (8.8) | 306 | (27.7) | 193 | (17.5) | 302 | (27.3) | |
| No. of pregnancies resulting in live birthsc | 3.00 | 3.00 | 2.00 | 3.00 | 3.00 | 2.00 | <0.001a | ||||||
| Breastfeedingd,e | 0.067 | ||||||||||||
| No | 47 | (7.4) | 6 | (12.8) | 3 | (6.4) | 11 | (23.4) | 7 | (14.9) | 20 | (42.6) | |
| Yes | 592 | (92.6) | 106 | (17.9) | 42 | (7.1) | 180 | (30.4) | 104 | (17.6) | 160 | (27.0) | |
| No. of children breastfedd,e | 2.00 | 2.00 | 2.00 | 2.00 | 2.00 | 2.00 | 0.001a | ||||||
Values for age, body mass index, number of pregnancies resulting in live births and number of children breastfed are median.
Unless otherwise specified, p-Value derived from Mantel–Haenszel’s χ2 test for linear trend.
a Jonckheere-Terpstra test for linear trend.
b Fisher’s exact test (two-tail).
c Women only.
d Only women with ≥1 pregnancies resulting in live births.
e Breastfed ≥1 month.
In over 45% of participants who had only one POP at high concentrations (Phc) (≥P90), this chemical was an OC, a PBDE or PBB 153. By contrast, among subjects with numerous Phc, the majority of such compounds were PCBs. For instance, when the nPhc was ≥3, more than 40% of these compounds were PCBs and HpCDD.
The median age of participants with ≥10 POPs at high concentrations (Phc) was 70 years, while for participants with <10 Phc it was 45 years, and for participants without any Phc, 39 years. Over 11% of Whites, 2.2% of Mexican Americans, and 29.2% of Blacks had ≥10 Phc (p <0.001) (Table 1). Subjects with ≥10 Phc had a slightly lower median BMI than subjects with <10 Phc (26.7 Kg/m2 and 27.6 Kg/m2, respectively, p for trend = 0.004) (Table 1). Women with ≥10 Phc had a higher number of pregnancies resulting in live births than women with <10 Phc (age-unadjusted medians: 3.0 and 2.0, respectively, p for trend <0.001). There were significant differences in the nPhc by sex, age, BMI, race/ethnicity, educational level, PIR, and, in women, by number of pregnancies, and breastfeeding (Table 2).
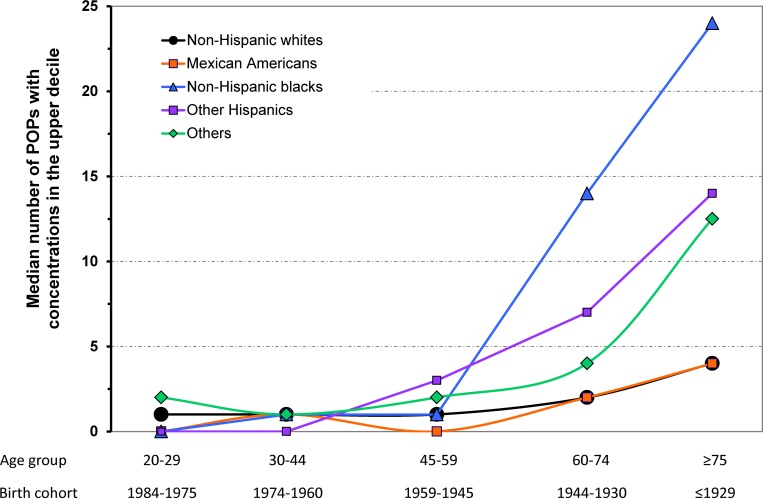
Multivariate analyses adjusted by age, gender and BMI showed that, as compared to Whites, Blacks had an odds ratio (OR) = 10.1 of having ≥10 Phc, whilst for Mexican Americans the OR was 0.2 (both p’s <0.001) (Table 3). When further adjusted by poverty income the OR for Blacks decreased to 9.2, and for Mexican Americans to 0.18 (both p’s <0.001). Differences between Blacks and Whites were larger in the older age groups / birth cohorts, and null in the younger ones (p for interaction <0.001) (Fig 1).
Table 3. Associations between sociodemographic characteristics and having ten or more POPs with concentrations in the upper decile.
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | ORa | (95% CI) | ORa | (95% CI) | ORa | (95% CI) | |||
| Gender | |||||||||
| Women | 1.00 | 1.00 | 1.00 | ||||||
| Men | 1.54*** | (1.28, | 1.85) | 1.74*** | (1.42, | 2.13) | 1.73*** | (1.40, | 2.13) |
| Age (years) | 1.06*** | (1.05, | 1.07) | 1.08*** | (1.07, | 1.09) | 1.08*** | (1.07, | 1.09) |
| Race/ethnicity | |||||||||
| Non-Hispanic white | 1.00 | — | 1.00 | ||||||
| Mexican American | 0.22*** | (0.14, | 0.35) | 0.18*** | (0.11, | 0.30) | |||
| Non-Hispanic black | 10.11*** | (7.82, | 13.1) | 9.18*** | (7.05, | 12.0) | |||
| Other Hispanic | 3.17*** | (1.78, | 5.63) | 2.64** | (1.43, | 4.85) | |||
| Other | 1.94* | (1.11, | 3.37) | 1.55 | (0.84, | 2.88) | |||
| Educational level | |||||||||
| College or above | 1.00 | 1.00 | 1.00 | ||||||
| High school | 0.91 | (0.72, | 1.15) | 0.96 | (0.75, | 1.24) | 0.96 | (0.74, | 1.25) |
| < High school | 1.04 | (0.84, | 1.28) | 1.22 | (0.95, | 1.55) | 1.14 | (0.88, | 1.49) |
| Poverty income ratio | |||||||||
| >2 | 1.00 | 1.00 | — | ||||||
| ≤2 | 1.13 | (0.94, | 1.37) | 1.24* | (1.00, | 1.53) | |||
| Body mass index (kg/m2) | |||||||||
| Normal weight | 1.00 | 1.00 | 1.00 | ||||||
| Overweight | 0.96 | (0.77, | 1.20) | 0.96 | (0.75, | 1.22) | 1.02 | (0.79, | 1.30) |
| Obese | 0.74* | (0.58, | 0.94) | 0.57*** | (0.44, | 0.75) | 0.58*** | (0.44, | 0.77) |
| Pregnancyb | |||||||||
| No | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 0.48* | (0.24, | 0.99) | 0.57 | (0.24, | 1.38) | 0.60 | (0.25, | 1.46) |
| No. of pregnancies resulting in live birthsb | 0.99 | (0.92, | 1.06) | 0.97 | (0.89, | 1.06) | 0.97 | (0.88, | 1.06) |
| Breastfeedingc,d | |||||||||
| No | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 1.15 | (0.46, | 2.87) | 1.36 | (0.48, | 3.84) | 1.30 | (0.46, | 3.68) |
| No. of children breastfedc,d | 0.88 | (0.76, | 1.01) | 0.97 | (0.82, | 1.14) | 0.96 | (0.81, | 1.13) |
Model 1: adjusted by age, gender and body mass index.
Model 2: adjusted by age, gender, body mass index and race/ethnicity.
Model 3: adjusted by age, gender, body mass index, race/ethnicity and poverty income.
a p-Value derived from Wald’s test.
b Women only.
c Only among women with ≥1 pregnancies resulting in live births and, in the three models, further adjusted by such number of pregnancies.
d Breastfed ≥1 month.
* p ≤0.05
** p ≤0.01
*** p ≤0.001.
Fig 1. Median number of POPs with concentrations in the upper decile by age/birth cohort and race/ethnicity.
For PIR ≤2, or “Low” income (vs. PIR>2 or “High” income) the OR of having ≥10 Phc was 1.13 (p >0.05) when the model was adjusted by age, gender and BMI, and 1.24 (p = 0.045) when further adjusted by race/ethnicity. The OR for obesity (vs. normal weight) was 0.74 (p for trend = 0.015) in the model adjusted by age and gender, and, when further adjusting by race/ethnicity and poverty income, it was 0.58 (p for trend <0.001) (Table 3). In women, pregnancy halved the probability of having ≥10 Phc when adjusting by age and body mass index (OR = 0.48, p = 0.048) (Table 3).
In models assessing the relationship between sociodemographic factors and the probability of having ≥1 POPs at concentrations ≥P90 (vs. not having POPs with concentrations ≥P90), adjusted by age, gender and BMI, the OR for Blacks (vs. Whites) was 1.10 (p = 0.266) and for Mexican Americans, 0.74 (p <0.001). When further adjusted by race/ethnicity, the OR for PIR≤2 (vs. PIR>2) was 1.17 (p = 0.026); and for obesity (vs. normal weight), 0.73 (p for trend <0.001 for BMI) (S4A Table). The corresponding figures for the probability of having ≥6 POPs at concentrations ≥P90 were 3.37 for Blacks and 0.51 for Mexican Americans (both p <0.001), 1.24 for PIR≤2 (p <0.01), and 0.91 for obesity (vs. normal weight) (p for trend = 0.353).
Because of the influence of PCBs in the previous results, we also analyzed associations among sociodemographic factors and the likelihood of having ≥1 of 6 POPs other than PCBs (i.e., OCs, PBDEs, and PBB 153 detected ≥85% of subjects) at high concentrations (S4B Table). Contrary to what was observed when all compound families were considered, for Blacks (vs. Whites) the OR of having ≥1 of such POPs was 0.76, and for Mexican Americans, 1.41, adjusting by age, gender and BMI (both p’s <0.01). The corresponding OR for PIR≤2 was 1.19 (p = 0.011), and for obesity, 0.82 (p for trend = 0.013). When further adjusting by race/ethnicity, the OR for PIR≤2 was 1.15 (p = 0.038), and for obesity, 0.80 (p for trend = 0.006) (S4B Table).
The geometric mean (GM) of nPhc doubled when the cutoff P75 was used instead of P90 (see S3 Table). For the cutoff P75 the percentage of subjects with ≥10 Phc was 37.5 for POPs detected in ≥85% of participants, and 45.2 for POPs detected in ≥50% of participants. However, the percentage of subjects without any Phc decreased slightly when the number of POPs included in the analyses increased.
In the 1,183 participants with the highest total TEQ concentrations (≥P75 of the distribution of total TEQ concentrations [i.e., ≥26.68 pg WHO-TEQ/g of lipid]), the percentage of subjects with ≥10 Phc was about twice the corresponding figure observed when all 4,739 participants were considered. Over 90% of the 1,183 subjects had ≥1 POPs a) not included in TEQ calculations, and b) with concentrations ≥P90. Over 30% had ≥10 such POPs, and almost 7% had ≥20 such POPs. Spearman’s ρ coefficient between the total TEQ concentration and nPhc (considering the 24 POPs not included in TEQ calculations, and the P90 in all participants for high concentrations) was 0.475 (p <0.001).
Over 43% of participants had TEQ concentrations ≥21 pg WHO-TEQ/g of lipid, a biomonitoring equivalent value (see Discussion). Taking into account health-based guidelines for other compounds, less than 1% of participants had concentrations of hexachlorobenzene ≥47 ng/g of lipid, and concentrations for the sum of p,p’-DDT and p,p’-DDE ≥5,000 ng/g of lipid. Two subjects had concentrations of BDE 99 ≥520 ng/g of lipid; 2 participants (aged <40 years) had concentrations ≥700 ng/g of lipid for the sum of 35 PCBs (without dioxin-like coplanar PCBs), and 6 participants (aged ≥40 years) had concentrations ≥1,800 ng/g of lipid. 10% of participants had concentrations for the sum of PCBs 138, 153 and 180 ≥216 ng/g of lipid. Only 4 participants had concentrations for the sum of these three PCBs ≥900 ng/g of lipid.
We also compared the concentrations of POPs detected in ≥85% of the participants in the present study (2003–2004), and their respective pooled concentrations for the NHANES periods 2005–2006 and 2007–2008. The concentrations of some POPs in the present study were only slightly higher than in subsequent periods; they were not higher or not statistically significant in the case of p,p’-DDE, PBB 153 and some PBDEs compounds (S5A Table). For 3 PFCs, concentrations in 2003–2004 were similar to concentrations in 2005–2010, and slightly higher than concentrations in 2011–2012 (S5B Table).
Discussion
More than half of the study population had concentrations in the top decile of ≥1 of the most commonly detected POPs, 38% had ≥3, and over 13% had ≥10 POPs each in their respective top decile. Findings are thus partly in contrast with the notion that human POP concentrations are low in the vast majority of the population [5,12]: such view holds only when each individual compound is looked at separately, but not when the individual human is of concern.
Median age of participants with ≥10 of most prevalent POPs at high concentrations was 70 years, while median age of participants without any Phc was 39 years. This could be due to biological aging effects or to birth cohort effects. Furthermore, the median age of participants without any Phc was near the median age of participants with 1 or 2 Phc. There were also significant differences in the nPhc by gender, race/ethnicity, educational level, PIR, BMI, parity, and breastfeeding. These results are in accordance with our main hypotheses (most of the U.S. population had POPs at low and high concentrations; sociodemographic factors related with each POP concentration showed similar relationships for the joint analysis of POPs).
Race/ethnicity was the sociodemographic factor most associated with a higher nPhc: Blacks had 9 times a greater chance of having ≥10 Phc than Whites, and Mexican Americans over 4 times a lower chance. The nPhc indicator not only shows that Blacks have higher body concentrations of POPs than Whites (or Mexican Americans lower concentrations), but it also quantifies how many POPs are in a specific high concentration range. The NHANES questionnaires had a large number of sociodemographic items; in this study, we used the sociodemographic factors that were available and related with body concentrations of POPs [12,32,35,39,45,46].
Results of unconditional logistic regression models for ≥1 Phc, ≥6 Phc, and ≥10 Phc (vs. no Phc, <6 Phc, and <10 Phc, respectively) in the subsample without imputations and PCBs, PCDDs/Fs analyzed by the sociodemographic factors (to assess the possible biases of imputations), were similar to results of models with imputations, except in some models for gender, which was not statistically significant, although ORs were similar.
Most studies found an inverse association between PCB levels in blood and BMI [56–58], as in the present analyses for all participants and 37 POPs.
Also rarely if ever noted before: high percentages of subjects with TEQ ≥P75 (≥26.68 pg WHO-TEQ/g of lipid) had numerous POPs not included in TEQ calculations, at high concentrations. Findings suggest that studies using TEQ measures could be even more relevant if they additionally assessed subgroups with high nPhc. Results do not imply that nPhc and related exposure indicators are preferable to other indicators to evaluate associations between POP mixtures and clinical outcomes; nPhc indicators just provide a different and complementary approach to indicators such as the sum of concentrations of PCBs [48,59–64], or the sum of orders of POPs [65].
Our goal was not to evaluate whether individuals have increased health risks due to multiple compounds at high concentrations, nor to assess the role of modes and mechanisms of action, but to propose a new and useful approach for exposure assessment. However, severe adverse health effects have been reported for concentrations similar to or lower than P90 in the present study [5,9,11,15,16,66–69]; e.g., in an NHANES study the OR of having diabetes for a concentration of ≥60.2 ng/g lipid of PCB 153 was 5.9 (95% CI = 3.0–11.9) [66]; in the present study the P90 for PCB 153 was 79.8 ng/g lipid. P90 of concentrations of individual PCBs in NHANES is as high or higher than in other countries with population-based surveys as Canada and Australia [6,70]. For p,p’-DDE and β-hexachlorocyclohexane (β-HCH), it is also as high or higher than in Canada, Australia and Germany [6,70].
In this study, over 43% of participants had TEQ concentrations ≥21 pg WHO-TEQ/g of lipid, which is the biomonitoring equivalent value published for dioxin TEQ, a health-risk based screening guideline [71]. Also, in the present study 10% of participants had concentrations for the sum of PCBs 138, 153 and 180 equal to or greater than the Human Biomonitoring level-I (HBM-I), which is 3 μg/L plasma or, when accounting for lipids, 216 ng/g lipid for the present study. HBM-I is a health-related exposure limit recommended for PCBs by the German Human Biomonitoring Commission [59–62]. For compounds considered in the present study, other biomonitoring equivalents values are only available for hexachlorobenzene, the arithmetic sum of p,p’-DDT and p,p’-DDE, the sum of 35 PCBs, and BDE 99 [59,71,72]; for these compounds very few subjects had concentrations above the corresponding biomonitoring equivalents in this study. To our knowledge, no current health-related limit values are available for the rest of PBDEs or for PFCs [59–61,71,72]. Although there are regulations and guidelines for other pollutants (e.g. lead, mercury, cadmium and other metals) and for POPs in air, soil, water and food (e.g., tolerable daily intakes), there are hardly any other guidelines for human POP concentrations to define levels of concern than the ones mentioned above [59–62,71].
Beyond findings on concentrations of individual compounds, the indicators illuminate a crucial–and usually overlooked–feature of human contamination by POPs: the frequency of mixtures of POPs at high concentrations. The approach could naturally be developed to integrate other pollutants of concern.
Importantly, 2003–2004 is the last period of NHANES in which the individual concentration of each compound is available for each individual subject. In 2005–2006 and 2007–2008 serum concentrations of POPs (except PFCs) were measured in weighted pooled-samples (not in individual samples); no data were published for 2009–2010 and 2011–2012. Therefore, data to calculate the number of POPs detected per person at high concentrations in more recent periods are not available.
Concentrations of most POPs in 2003–2004 were only slightly higher than in more recent periods (Tables in S5 File). Virtually all major contemporary health effects of POPs will be influenced by concentrations experienced by human cohorts during several decades, not just by recent exposures. Furthermore, the nPhc can be fruitfully applied to analyze data from many periods and settings.
Different POPs were analyzed in participants of the three NHANES 2003–2004 subsamples; even in two of the three subsamples all selected POPs were not analyzed in all participants. Each sample, however, is valid; and it is efficient not to analyze all POPs in all participants [2,46]. For PFCs, the LODs were constant for each sample analyzed [46]. For the other 55 compounds, the LOD for the whole weight concentrations was different for each serum sample of each person [2]. When PCDD/Fs, PCBs, OCs, PBDEs, and PBB 153 concentrations were measured in serum lipid, LOD calculations were performed using the chemical concentration expressed per amount of lipid, and the LOD concentration expressed per amount of lipid was the highest LOD among all the individual samples analyzed [2,46]. LODs for lipid adjusted concentrations were highest compared to the LODs for the whole weight concentrations, and rates of detection were lower, than for whole weight concentrations; as a consequence, lipid adjusted results are more conservative (e.g., because there were less compounds detected in ≥85% of participants).
In the present study, some associations between nPhc and sociodemographic factors are quite influenced by the predominance of PCBs and HpCDD at high concentrations among subjects with ≥3 nPhc. The cutoff point for nPhc should be chosen with this issue in mind, while also avoiding a too high nPhc (e.g., because of lower detection rates of some POPs) [12].
Serum concentrations of POPs do not follow a normal distribution [31]. Values for P90 can be much higher than the P75 (e.g., for p,p’-DDE the P90 value was 2.14 times greater than P75, and for PCB 153 it was 53%). Such differences between highest concentrations minimize a possible misclassification of concentrations in ≥P90 or <P90 due to laboratory measurement errors [46]. The minimum percentage of participants with concentrations in the top decile of ≥1 POPs will be 10%, but such percentage will not necessarily, linearly, or indefinitely increase (nor approach 100%) as the number of compounds considered increases: the percentage of participants with concentrations of ≥1 POPs in the top decile is only partly positively influenced by the number of compounds considered; it is also inversely influenced by the magnitude of the correlations between the pairs of compounds, being highest when POPs are completely uncorrelated (for details see Suppl. Material of Porta et al., 2012) [12]. Therefore, the nPhc follows a distribution that is influenced by all the correlations between the pairs of compounds, and results may not be due to chance. Figure 1 of Supplemental Material of Porta et al., 2012 [12] shows different values for ≥1 by the number of POPs considered, and the values when the POPs were completely uncorrelated. For ≥10 POPs at high concentrations (rather than ≥1 POP) this situation is even more restrictive; when we focused on ≥10 POPs at high concentrations, it was statistically possible for the minimum percentage of participants with ≥10 POPs at high concentrations to be 0% (i.e., it was not statistically inevitable for that percentage to be 10%), since it is possible that highly-correlated sets of POPs comprise 9 or less POPs. Furthermore, such minimum percentage also depends on the number of POPs analyzed, the number of POPs in the top decile, and the number of participants included.
Conclusion
In summary, more than 13% of the US population may have ≥10 POPs each at concentrations in the top decile. This finding is not to be expected just on statistical grounds. High percentages of subjects with TEQ ≥P75 have numerous POPs not included in TEQ calculations, at high concentrations. The nPhc is related to race/ethnicity, age, and BMI. It is also likely to be related to other relevant social, environmental, and individual factors. The study findings foster knowledge on previously unknown characteristics of human chemical contamination in the US population. Such knowledge is a right of citizens, and could also be considered when evaluating the impacts of relevant public and private policies.
Supporting Information
(91 POPs analyzed, n = 4,739)
(PDF)
(DOCX)
(DOCX)
(DOCX)
S4ATable. Associations between sociodemographic characteristics and having one or more POPs with concentrations in the upper decile. S4B Table. Associations between sociodemographic characteristics and having one or more OCs, PBDEs and PBB 153 with concentrations in the upper decile.
(DOCX)
S5A Table. Serum pooled concentrations of POPs most detected for the three most recent NHANES Surveys periods analyzed. S5B Table. Serum concentrations of four perfluorinated compounds (μg/L) most detected for the most recent NHANES Surveys periods analyzed.
(DOCX)
Acknowledgments
The authors gratefully acknowledge technical and scientific assistance provided by Natàlia Pallarès, David J. MacFarlane, Manuel Pastor, Yolanda Rovira and Ferran Sanz.
Abbreviations
- β-HCH
β-hexachlorocyclohexane
- BMI
body mass index
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- GM
geometric mean
- HBM
Human Biomonitoring
- LOD
limit of detection
- NHANES
National Health and Nutrition Examination Survey
- nPhc
number of POPs detected per person at high concentrations
- PBBs
polybrominated biphenyls
- PBDEs
polybrominated diphenyl ethers
- PCBs
polychlorinated biphenyls
- PCDDs
polychlorinated dibenzo-p-dioxins
- PCDFs
polychlorinated dibenzofurans
- PFCs
perfluorinated compounds
- Phc
POPs at high concentrations
- PIR
family’s total income divided by the family size-specific poverty threshold income
- POP
persistent organic pollutant
- OCs
organochlorine compounds
- OR
odds ratio
- TEQ
total toxic equivalency
Data Availability
All NHANES data files are available from: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
Funding Statement
The work was supported in part by research grants from Instituto de Salud Carlos III – FEDER (FIS PI13/00020 and CIBER de Epidemiología y Salud Pública − CIBERESP), Government of Spain; Fundació La Marató de TV3 (20132910); and Government of Catalonia (2014 SGR 1012). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Porta M, Puigdomènech E, Ballester F, Selva J, Ribas-Fitó N, Llop S, et al. Monitoring concentrations of persistent organic pollutants in the general population: the international experience. Environ Int. 2008;34:546–561. [DOI] [PubMed] [Google Scholar]
- 2.Patterson DG Jr, Wong LY, Turner WE, Caudill SP, Dipietro ES, McClure PC, et al. Levels in the U.S. population of those persistent organic pollutants (2003–2004) included in the Stockholm Convention or in other long range transboundary air pollution agreements. Environ Sci Technol. 2009;43:1211–1218. [DOI] [PubMed] [Google Scholar]
- 3.Thornton JW, McCally M, Houlihan J. Biomonitoring of industrial pollutants: health and policy implications of the chemical body burden. Public Health Rep. 2002;117:315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Porta M. Human contamination by environmental chemical pollutants: can we assess it more properly? Prev Med. 2012;55:560–562. 10.1016/j.ypmed.2012.09.020 [DOI] [PubMed] [Google Scholar]
- 5.Bergman A, Jobling S, Kidd KA, Zoeller RT, editors. State of the science of endocrine disrupting chemicals—2012 World Health Organization & United Nations Environment Programme (WHO-UNEP) 2013. Available: http://unep.org/pdf/9789241505031_eng.pdf. Accessed 14 January 2016. [Google Scholar]
- 6.Aylward LL, Green E, Porta M, Toms LM, Den Hond E, Schulz C, et al. Population variation in biomonitoring data for persistent organic pollutants (POPs): An examination of multiple population-based datasets for application to Australian pooled biomonitoring data. Environ Int. 2014;68:127–138. 10.1016/j.envint.2014.03.026 [DOI] [PubMed] [Google Scholar]
- 7.Den Hond E, Govarts E, Willems H, Smolders R, Casteleyn L, Kolossa-Gehring M, et al. First steps toward harmonized human biomonitoring in Europe: demonstration project to perform human biomonitoring on a European scale. Environ Health Perspect. 2015;123:255–263. 10.1289/ehp.1408616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Research Council. Committee on Human Biomonitoring for Environmental Toxicants. Human Biomonitoring for Environmental Chemicals. Washington, DC: The National Academies Press; 2006. Available: http://www.nap.edu/catalog/11700.html. Accessed 14 January 2016. [Google Scholar]
- 9.National Research Council. Committee on the Health Risks of Phthalates. Phthalates and Cumulative Risk Assessment. The tasks ahead. Washington, DC: The National Academies Press; 2008. Available: http://www.nap.edu/catalog/12528.html. Accessed 14 January 2016. [Google Scholar]
- 10.Kolossa-Gehring M. Human biomonitoring: political benefits–scientific challenges. September 26–28, 2010. Int J Hyg Environ Health. 2012;215:247–252. 10.1016/j.ijheh.2011.10.019 [DOI] [PubMed] [Google Scholar]
- 11.Barouki R, Gluckman PD, Grandjean P, Hanson M, Heindel JJ. Developmental origins of non-communicable disease: implications for research and public health. Environ Health. 2012;11:42 10.1186/1476-069X-11-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Porta M, Pumarega J, Gasull M. Number of persistent organic pollutants detected at high concentrations in a general population. Environ Int. 2012;44:106–111. 10.1016/j.envint.2012.02.005 [DOI] [PubMed] [Google Scholar]
- 13.Lee DH, Porta M, Jacobs DR, Vandenberg LN. Chlorinated persistent organic pollutants, obesity, and type 2 diabetes. Endocr Rev. 2014;35:557–601. 10.1210/er.2013-1084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Engel SM, Wolff MS. Causal inference considerations for endocrine disruptor research in children's health. Annu Rev Public Health. 2013;34:139–158. 10.1146/annurev-publhealth-031811-124556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs DR Jr, Lee DH, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic doses responses. Endocr Rev. 2012;33:378–455. 10.1210/er.2011-1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor KW, Novak RF, Anderson HA, Birnbaum LS, Blystone C, Devito M. et al. Evaluation of the association between Persistent Organic Pollutants (POPs) and diabetes in epidemiological studies: A National Toxicology Program workshop review. Environ Health Perspect. 2013;121:774–783. 10.1289/ehp.1205502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casals-Casas C, Desvergne B. Endocrine disruptors: from endocrine to metabolic disruption. Annu Rev Physiol. 2011;73:135–162. 10.1146/annurev-physiol-012110-142200 [DOI] [PubMed] [Google Scholar]
- 18.Henkler F, Luch A. Adverse health effects of environmental chemical agents through non-genotoxic mechanisms. J Epidemiol Community Health 2011;65:1–3. 10.1136/jech.2008.083881 [DOI] [PubMed] [Google Scholar]
- 19.Hernández L, van Steeg H, Luijten M, van Benthem J. Mechanisms of non-genotoxic carcinogens and importance of a weight of evidence approach. Mutat Res. 2009;682:94–109. 10.1016/j.mrrev.2009.07.002 [DOI] [PubMed] [Google Scholar]
- 20.Hou L, Zhang X, Wang D, Baccarelli A. Environmental chemical exposures and human epigenetics. Int J Epidemiol. 2012;41:79–105. 10.1093/ije/dyr154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manikkam M, Guerrero-Bosagna C, Tracey R, Haque MM, Skinner MK. Transgenerational actions of environmental compounds on reproductive disease and identification of epigenetic biomarkers of ancestral exposures. PLoS One. 2012;7:e31901 10.1371/journal.pone.0031901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soto A, Sonnenschein C. Environmental causes of cancer: endocrine disruptors as carcinogens. Nat Rev Endocrinol. 2011;6:363–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stein RA. Epigenetics and environmental exposures. J Epidemiol Community Health. 2012;66:8–13. 10.1136/jech.2010.130690 [DOI] [PubMed] [Google Scholar]
- 24.Lee DH, Steffes MW, Sjodin A, Jones RS, Needham LL, Jacobs DR Jr. Low dose of some persistent organic pollutants predicts type 2 diabetes: a nested case–control study. Environ Health Perspect. 2010;118:1235–1242. 10.1289/ehp.0901480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lind PM, Risérus U, Salihovic S, van Bavel B, Lind L. An environmental wide association study (EWAS) approach to the metabolic syndrome. Environ Int. 2013;55:1–8. 10.1016/j.envint.2013.01.017 [DOI] [PubMed] [Google Scholar]
- 26.Patel CJ, Bhattacharya J, Butte AJ. An Environment-Wide Association Study (EWAS) on type 2 diabetes mellitus. PLoS One. 2010;5:e10746 10.1371/journal.pone.0010746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paul DS, Beck S. Advances in epigenome-wide association studies for common diseases. Trends Mol Med. 2014;20:541–543. 10.1016/j.molmed.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trasande L, Zoeller RT, Hass U, Kortenkamp A, Grandjean P, Myers JP, DiGangi J, Hunt PM, et al. Burden of disease and costs of exposure to endocrine disrupting chemicals in the European Union: an updated analysis. Andrology. 2016. 10.1111/andr.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prüss-Ustün A, Wolf J, C Corvalán C, Bos R, Neira M. Preventing disease through healthy environments: a global assessment of the burden of disease from environmental risks World Health Organization; 2016. Available: http://apps.who.int/iris/bitstream/10665/204585/1/9789241565196_eng.pdf?ua=1. Accessed 12 April 2016. [Google Scholar]
- 30.Gasull M, Pumarega J, Rovira G, López T, Alguacil J, Porta M. Relative effects of educational level and occupational social class on body concentrations of persistent organic pollutants in a representative sample of the general population of Catalonia, Spain. Environ Int. 2013;60:190–201. 10.1016/j.envint.2013.08.001 [DOI] [PubMed] [Google Scholar]
- 31.Porta M, Gasull M, Puigdomènech E, Garí M, Bosch de Basea M, Guillén M, et al. Distribution of blood concentrations of persistent organic pollutants in a representative sample of the population of Catalonia. Environ Int. 2010;36:655–664. 10.1016/j.envint.2010.04.013 [DOI] [PubMed] [Google Scholar]
- 32.Wolff MS, Deych E, Ojo F, Berkowitz GS. Predictors of organochlorines in New York City pregnant women, 1998–2001. Environ Res. 2005;97:170–177. [DOI] [PubMed] [Google Scholar]
- 33.Quinn CL, Wania F. Understanding differences in the body burden-age relationships of bioaccumulating contaminants based on population cross sections versus individuals. Environ Health Perspect. 2012;120:554–559. 10.1289/ehp.1104236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freire C., Amaya E., Fernández M, González-Galarzo MC, Ramos R, Molina-Molina JM, et al. Relationship between occupational social class and exposure to organochlorine pesticides during pregnancy. Chemosphere. 2011;83:831–838. 10.1016/j.chemosphere.2011.02.076 [DOI] [PubMed] [Google Scholar]
- 35.Vrijheid M, Martinez D, Aguilera I, Ballester F, Basterrechea M, Esplugues A, et al. Socioeconomic status and exposure to multiple environmental pollutants during pregnancy: evidence for environmental inequity? J Epidemiol Community Health. 2012;66:106–113. 10.1136/jech.2010.117408 [DOI] [PubMed] [Google Scholar]
- 36.Adamkiewicz G, Spengler JD, Harley AE, Stoddard A, Yang M, Alvarez-Reeves M, et al. Environmental conditions in low-income urban housing: clustering and associations with self-reported health. Am J Public Health. 2014;104:1650–1656. 10.2105/AJPH.2013.301253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jacobs DE. Environmental health disparities in housing. Am J Public Health. 2011;101:S115–S122. 10.2105/AJPH.2010.300058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burger J, Gochfeld M. Conceptual environmental justice model for evaluating chemical pathways of exposure in low-income, minority, native American, and other unique exposure populations. Am J Public Health. 2011;101:S64–S73. 10.2105/AJPH.2010.300077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morrens B, Bruckers L, Hond ED, Nelen V, Schoeters G, Baeyens W, et al. Social distribution of internal exposure to environmental pollution in Flemish adolescents. Int J Hyg Environ Health. 2012;215:474–481. 10.1016/j.ijheh.2011.10.008 [DOI] [PubMed] [Google Scholar]
- 40.Park SK, Tao Y, Meeker JD, Harlow SD, Mukherjee B. Environmental risk score as a new tool to examine multi-pollutants in epidemiologic research: An example from the NHANES study using serum lipid levels. PLoS One. 2014;9:e98632 10.1371/journal.pone.0098632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patel CJ, Cullen MR, Ioannidis JP, Butte AJ. Systematic evaluation of environmental factors: persistent pollutants and nutrients correlated with serum lipid levels. Int J Epidemiol. 2012;41:828–843. 10.1093/ije/dys003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel CJ, Rehkopf DH, Leppert JT, Bortz WM, Cullen MR, Chertow GM, et al. Systematic evaluation of environmental and behavioural factors associated with all-cause mortality in the United States National Health and Nutrition Examination Survey. Int J Epidemiol. 2013;42:1795–1810. 10.1093/ije/dyt208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Belova A, Greco SL, Riederer AM, Olsho LE, Corrales MA. A method to screen U.S. environmental biomonitoring data for race/ethnicity and income-related disparity. Environ Health. 2013;12:114 10.1186/1476-069X-12-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woodruff TJ, Zota AR, Schwartz JM. Environmental chemicals in pregnant women in the United States: NHANES 2003–2004. Environ Health Perspect. 2011;119:878–885. 10.1289/ehp.1002727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention. National Center for Health Statistics (NCHS): National Health and Nutrition Examination Survey Data. Atlanta, GA. 2003–2004. Available: http://wwwn.cdc.gov/nchs/nhanes/search/nhanes03_04.aspx. Accessed 14 January 2016.
- 46.Centers for Disease Control and Prevention. National Center for Environmental Health, Division of Laboratory Sciences: Fourth National Report on Human Exposure to Environmental Chemicals. Atlanta, GA. 2009. Available: http://www.cdc.gov/exposurereport/pdf/FourthReport.pdf. Accessed 14 January 2016.
- 47.Centers for Disease Control and Prevention. National Center for Environmental Health, Division of Laboratory Sciences: Fourth National Report on Human Exposure to Environmental Chemicals. Atlanta, GA. 2015. Available: http://www.cdc.gov/biomonitoring/pdf/FourthReport_UpdatedTables_Feb2015.pdf. Accessed 14 January 2016.
- 48.LaKind JS, Hays SM, Aylward LL, Naiman DQ. Perspective on serum dioxin levels in the United States: an evaluation of the NHANES data. J Expo Sci Environ Epidemiol. 2009;19:435–441. 10.1038/jes.2008.63 [DOI] [PubMed] [Google Scholar]
- 49.Rosner B. Fundamentals of Biostatistics. 7th ed. Boston, MA: Cengage Learning; 2010. [Google Scholar]
- 50.Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2nd ed. Hoboken; New Jersey: Wiley; 2002. [Google Scholar]
- 51.Van den Berg M, Birnbaum LS, Denison M, De Vito M, Farland W, Feeley M, et al. The 2005 World Health Organization reevaluation of human and Mammalian toxic equivalency factors for dioxins and dioxin-like compounds. Toxicol Sci. 2006;93:223–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patterson DG Jr, Turner WE, Caudill SP, Needham LL. Total TEQ reference range (PCDDs, PCDFs, cPCBs, mono-PCBs) for the US population 2001–2002. Chemosphere. 2008;73:S261–S277. 10.1016/j.chemosphere.2007.08.074 [DOI] [PubMed] [Google Scholar]
- 53.Armitage P, Berry G, Matthews JNS. Statistical methods in medical research 4th edition Oxford, Blackwell; 2002. [Google Scholar]
- 54.Kleinbaum DG, Kupper LL, Muller KE, Nizam A. Applied regression analysis and other multivariable methods 3rd ed. Duxbury, CA: Pacific Grove; 1998. [Google Scholar]
- 55.Rothman KJ, Greenland S, Lash TL, eds. Modern Epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 56.Wolff MS, Anderson HA, Britton JA, Rothman N. Pharmacokinetic variability and modern epidemiology–the example of dichlorodiphenyltrichloroethane, body mass index, and birth cohort. Cancer Epidemiol. Biomarkers Prev. 2007;16:1925–1930. [DOI] [PubMed] [Google Scholar]
- 57.Glynn AW, Granath F, Aune M, Atuma S, Darnerud PO, e R, et al. Organochlorines in Swedish women: determinants of serum concentrations. Environ Health Perspect. 2003;111:349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lind PM, Lee DH, Jacobs DR, Salihovic S, van Bavel B, Wolff MS, et al. Circulating levels of persistent organic pollutants are related to retrospective assessment of life-time weight change. Chemosphere. 2013;90:998–1004. 10.1016/j.chemosphere.2012.07.051 [DOI] [PubMed] [Google Scholar]
- 59.Angerer J, Aylward LL, Hays SM, Heinzow B, Wilhelm M. Human biomonitoring assessment values: approaches and data requirements. Int J Hyg Environ Health. 2011;214:348–360. 10.1016/j.ijheh.2011.06.002 [DOI] [PubMed] [Google Scholar]
- 60.Human Biomonitoring Commission. German Federal Environment Agency. Human-Biomonitoring(HBM) values for blood and/or urine. Available: http://www.umweltbundesamt.de/sites/default/files/medien/378/bilder/dateien/tabelle_fuer_hbm-werte_englisch_09_09_2015.pdf. Accessed 14 January 2016.
- 61.Schulz C, Wilhelm M, Heudorf U, Kolossa-Gehring M. Reprint of "Update of the reference and HBM values derived by the German Human Biomonitoring Commission". Int J Hyg Environ Health. 2012;215:150–158. 10.1016/j.ijheh.2012.01.003 [DOI] [PubMed] [Google Scholar]
- 62.Schettgen T, Alt A, Esser A, Kraus T. Current data on the background burden to the persistent organochlorine pollutants HCB, p,p'-DDE as well as PCB 138, PCB 153 and PCB 180 in plasma of the general population in Germany. Int J Hyg Environ Health. 2015;218:380–385. 10.1016/j.ijheh.2015.02.006 [DOI] [PubMed] [Google Scholar]
- 63.Grandjean P, Henriksen JE, Choi AL, Petersen MS, Dalgård C, Nielsen F, et al. Marine food pollutants as a risk factor for hypoinsulinemia and type 2 diabetes. Epidemiology. 2011;22:410–417. 10.1097/EDE.0b013e318212fab9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee DH, Lind PM, Jacobs DR Jr, Salihovic S, van Bavel B, Lind L. Polychlorinated biphenyls and organochlorine pesticides in plasma predict development of type 2 diabetes in the elderly: The prospective investigation of the vasculature in Uppsala Seniors (PIVUS) study. Diabetes Care. 2011;34:1778–1784. 10.2337/dc10-2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee DH, Lee IK, Song K, Steffes M, Toscano W, Baker BA, et al. A strong dose-response relation between serum concentrations of persistent organic pollutants and diabetes: Results from the National Health and Examination Survey 1999−2002. Diabetes Care. 2006;29:1638–1644. [DOI] [PubMed] [Google Scholar]
- 66.De Roos AJ, Hartge P, Lubin JH, Colt JS, Davis S, Cerhan JR, et al. Persistent organochlorine chemicals in plasma and risk of non-Hodgkin's lymphoma. Cancer Res. 2005;65:11214–11226. [DOI] [PubMed] [Google Scholar]
- 67.Freeman MD, Kohles SS. Plasma levels of polychlorinated biphenyls, non-Hodgkin lymphoma, and causation. J Environ Public Health. 2012;2012:258981 10.1155/2012/258981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gascón M, Vrijheid M, Martínez D, Ballester F, Basterrechea M, Blarduni E, et al. Pre-natal exposure to dichlorodiphenyl-dichloroethylene and infant lower respiratory tract infections and wheeze. Eur Respir J. 2012;39:1188–1196. 10.1183/09031936.00011711 [DOI] [PubMed] [Google Scholar]
- 69.McGlynn KA, Quraishi SM, Graubard BI, Weber JP, Rubertone MV, Erickson RL. Persistent organochlorine pesticides and risk of testicular germ cell tumors. J Natl Cancer Inst. 2008;100:663–671. 10.1093/jnci/djn101 [DOI] [PubMed] [Google Scholar]
- 70.Health Canada. Report on human biomonitoring of environmental chemicals in Canada. Results of the Canadian Health Measures Survey Cycle 1 (2007–2009) Ottawa, Ontario: Health Canada; 2010. Available: http://www.healthcanada.gc.ca. Accessed 14 January 2016. [Google Scholar]
- 71.Aylward LL, Kirman CR, Schoeny R, Portier CJ, Hays SM. Evaluation of biomonitoring data from the CDC National Exposure Report in a risk assessment context: perspectives across chemicals. Environ Health Perspect. 2013;121:287–294. 10.1289/ehp.1205740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.AMAP (Arctic Monitoring and Assessment Programme), 1998. AMAP Assessment Report: Arctic Pollution Issues. Oslo, AMAP; Available: http://www.amap.no/documents/doc/amap-assessment-report-arctic-pollution-issues/68. Accessed 14 January 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(91 POPs analyzed, n = 4,739)
(PDF)
(DOCX)
(DOCX)
(DOCX)
S4ATable. Associations between sociodemographic characteristics and having one or more POPs with concentrations in the upper decile. S4B Table. Associations between sociodemographic characteristics and having one or more OCs, PBDEs and PBB 153 with concentrations in the upper decile.
(DOCX)
S5A Table. Serum pooled concentrations of POPs most detected for the three most recent NHANES Surveys periods analyzed. S5B Table. Serum concentrations of four perfluorinated compounds (μg/L) most detected for the most recent NHANES Surveys periods analyzed.
(DOCX)
Data Availability Statement
All NHANES data files are available from: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.