Abstract
Melanoma claims approximately 80% of skin cancer-related deaths. Its life-threatening nature is primarily due to a propensity to metastasize. The prognosis for melanoma patients with distal metastasis is bleak, with median survival of six months even with the latest available treatments. The most commonly mutated oncogenes in melanoma are BRAF and NRAS accounting approximately 60% and 20% of cases, respectively. In malignant melanoma, accumulating evidence suggests that multiple signaling pathways are constitutively activated and play an important role in cell proliferation, cell survival, epithelial to mesenchymal transition, metastasis and resistance to therapeutic regimens. Phytochemicals are gaining considerable attention because of their low toxicity, low cost, and public acceptance as dietary supplements. Cell culture and animals studies have elucidated several cellular and molecular mechanisms by which phytochemicals act in the prevention and treatment of metastatic melanoma. Several promising phytochemicals, such as, fisetin, epigallocatechin-3-gallate, resveratrol, curcumin, proanthocyanidins, silymarin, apigenin, capsaicin, genistein, indole-3-carbinol, and luteolin are gaining considerable attention and found in a variety of fresh fruits, vegetables, roots, and herbs. In this review, we will discuss the preventive potential, therapeutic effects, bioavailability and structure activity relationship of these selected phytochemicals for the management of melanoma.
Keywords: Apoptosis, Cell proliferation, Invasion, Metastasis, Melanoma, Phytochemicals, Signaling pathways
1. INTRODUCTION
Skin cancer is the most common malignancy worldwide with particularly high incidence among fair-skinned populations [1]. Skin cancer poses a major threat to public health as incidence and mortality rates of skin cancers are dramatically increasing [2–4]. Skin cancers are divided into two major groups according to cellular origin as either melanoma (melanocytic) or non-melanoma (epithelial) skin cancers (NMSCs) [5]. The NMSCs are comprised of basal cell carcinomas (BCCs) and squamous cell carcinomas (SSCs) and accounts for 80 and 16 percent of all skin cancer cases respectively. Although both BCCs and SCCs arise from the epidermal basal layer, they have different characteristics [5]. Though BCCs exhibit slow growth and rarely metastasize, their SCCs counterparts metastasize 2 to 5 of the time and carry a poor prognosis if metastasis has occurred [6]. Melanoma, which accounts for only 4 percent of all skin cancers, is a potentially life-threatening skin cancer due to its propensity to metastasize. It claims approximately 80 percent of skin cancer related deaths. The prognosis for melanoma patients with distal metastasis is minimal, with median survival of only six months [7, 8]. Moreover, the incidence of melanoma is rapidly increasing worldwide. The majority of melanoma cancers occur in developed countries such as Europe, Australia, New Zealand and the United States [8, 9]. The World Health Organization reports the annual incidence of melanoma to be approximately 160,000 with an associated 48,000 deaths worldwide each year [10–12]. In recent years, melanoma is the only common cancer with an increasing incidence and death rate. More importantly, the incidence of melanoma in children is also increasing rapidly. Reports estimate that 1 in 50 Americans will be diagnosed with melanoma during their lifetime. According to an estimate from the American Cancer Society, one person dies every hour from melanoma [13, 14]. Furthermore, about 9,940 melanoma-related deaths are projected to occur in the United States in 2015 [15, 16]. A gender-based analysis predicted that approximately 42,670 men and 31,200 women are expected to be diagnosed with melanoma and about 6,640 men and 3,300 women will die from melanoma in the United States in 2015.
Melanoma develops when melanocytes proliferate abnormally and become unresponsive to the regulatory signals from fibroblasts and keratinocytes. The signaling pathways that regulate melanocyte proliferation become aberrantly activated, and thus these cells divide to develop melanoma [17–20]. Melanoma development is characterized by two distinct growth phases. The radial growth phase (RGP) is characterized by the growth of single cells or small clusters of cells confined to the epidermis and extend to the papillary dermis. Alternatively, the invasion of melanoma cells into the dermis and development of tumor-like-nodules or plaques is referred to as vertical growth phase (VGP) [17, 18, 21, 22]. Depending upon the frequency and location, melanoma of the skin can be divided into various types according to clinical and histological growth patterns. However, they all pose the same risk according to their tumor depth, mitotic index (dividing melanoma cells), ulceration and, more importantly, level of spread in the regional lymph nodes [23–25].
Depending upon the clinical and pathological growth patterns melanoma can be divided into four major subtypes [26, 27]. Superficial spreading melanoma is the most common type that accounts for approximately half to three-quarters of all diagnosed melanoma and is most common in fair skinned persons of all ages. Superficial spreading melanoma usually derived from a preexisting benign melanocytic nevus and remain confined to the epidermis (RGP) for an extended time before beginning to VGP [28]. Areas of the skin with the highest nevus density (most commonly found on the back and trunk in men and on the back and legs in women) and with intermittent sun exposure are at high risk for superficial spreading melanoma. Nodular melanoma is the second most common type that accounts for approximately 15 to 35% of all diagnosed melanomas and is notoriously rapidly-growing and invasive. It usually develops as uniform dark blue-black, blue-red or sometimes colorless bump at the trunk, head and neck areas [29, 30]. Lentigo malignant melanoma is less common subtype of melanoma that accounts approximately 5 to 15% of cases. It occurs on sun-exposed skin of faces of middle aged to elderly adults with a history of photodamage. Lentigo maligna melanoma is slow growing and has a prolonged RGP and is less invasive [31, 32]. Acral lentiginous melanoma is the least common form that accounts for approximately 5 to 10% of all diagnosed melanomas. It develops most commonly in dark-skinned individuals such as in people of Japanese, African American, Latin American, and Native American descents [33]. The most common sites for occurrence of acryl lentiginous melanoma are the soles of the feet, palms and beneath the nail plates [34, 35]. Acryl lentiginous melanomas appear clinically as tan to brown-black, macules and patches with irregular borders and an average size of 3 centimeters [36]. Melanoma can develop anywhere in the body, including the internal organs. Some less common types of melanoma include ocular and mucosal melanoma. Ocular melanoma, which represents 3–5% of all melanoma cases, occurs inside the eyes when melanocytes of the iris or choroid layer begin to proliferate abnormally. Uveal melanoma is the most common form of ocular melanoma and primarily affects light-skinned populations [37]. Mucosal melanoma represents less than 2% of all cases of melanoma and can develop in the nose, mouth, throat, and in the genital areas [38]. This review begins with a review of the gene mutations and dysregulated signaling pathways in melanoma. Beyond this, we explain the preventative and therapeutic effects of key phytochemicals for the management of melanoma in the context of their bioavailability and structure-activity relationship.
2. GENE MUTATIONS AND SIGNALING PATHWAYS ACTIVATED IN MELANOMA
The use of advanced technology in the analysis of the human genome has helped to shed light on specific gene mutations that occur frequently in melanomas and the impact of these mutations on the regulation of signaling pathways. More importantly, studies have confirmed that these mutations control the progression and malignancy of melanomas. Some of the most frequently mutated genes found in in melanoma are described below.
2.1. BRAF Mutations
BRAF, a serine/threonine protein kinase of RAF family (ARAF, BRAF and CRAF), is generally expressed in neuronal tissues and melanocytes [39–41]. It is encoded on chromosome 7q34 and is a component of the mitogen-activated protein kinase (MAPK) pathway. MAPK a pro-growth signaling pathway is activated by cell surface growth factors receptors [42]. BRAF signaling is mutated in approximately 60% of melanomas resulting in induction of genomic instability, driving the proliferation of melanoma cells. The Sanger Institute first described activating mutations in BRAF signaling in 2002 [43]. The most common BRAF mutation (> 90% of known BRAF mutations) results from substitution of glutamic acid (E) in place of valine (V) at codon 600 (a single nucleotide mutation resulting in BRAFV600E, nucleotide 1799 T>A; codon GTG>GAG). Mutated BRAFV600E leads to hyper-activation of MAPK signaling. Another common BRAF mutation (BRAFV600K) is the substitution of lysine (K) for valine (V) at position 600, which has been reported more common in some populations [44]. Activating mutation BRAFV600E has been implicated in melanoma progression by activating the downstream MEK/ERK signaling pathway and thus enhancing replicative potential, reducing senescence and apoptosis, and promoting angiogenesis [45, 46]. Activation of this pathway also stimulates cell invasion and metastasis by upregulating proteins involved in migration, cell contractility, as well as evasion of the immune response [47, 48].
2.2. NRAS Mutations
NRAS, another crucial signaling molecule of RAS family (HRAS, KRAS and NRAS), is located upstream of the BRAF/MEK/ERK (MAPK) and PI3K/AKT pathways [49–51]. After BRAF, NRAS is the second most commonly activated oncogene found mutated in 15–25% of all melanomas. Although KRAS mutations are the most common among all human malignancies, NRAS mutations are most frequently found in melanoma [52]. The substitution of an arginine (R) for a glutamine (Q) at position 61 within the NRAS protein is NRASQ61R. The NRAS protein is a small GTP binding proteins (guanosine-5-triphosphate; GTPase) that cleaves bound GTP and thus regulates cellular responses to many extracellular stimuli, including soluble growth factors [49]. Signal transduction through this pathway begins when extracellular growth factors interact with cell surface receptors [53]. This creates intracellular docking sites that then interact with specific adaptor molecules and signal transducing proteins leading to activation of guanine nucleotide-exchange factors (GNEFs). GNEFs remove guanine nucleotides from NRAS and allow passive binding to GTP, which is abundantly present in the cytosol. GTP bound NRAS then interacts with downstream effector molecules including BRAF, PI3K and others to regulate proliferation, survival and differentiation. Although NRAS mutations are distinct from BRAF, they both cause the constitutive activation of MAPK and PI3K/AKT signaling pathways [54, 55]. Melanomas with NRAS mutations develop higher-grade tumors with higher mitotic and invasive potentials than the BRAF mutated melanomas [56, 57]. BRAF and NRAS mutations can be detected at early stages of melanoma progression and remains activated throughout the progression of disease [58, 59]. It is well established that these mutations are almost never simultaneously present and, alone, are insufficient to initiate melanoma development [60].
2.3. PTEN Mutations
PTEN (phosphatase and tensin homologue), a tumor suppressor gene located at 10q23–24, is mutated in 30–50% of melanoma cell lines and in 5–20% primary melanomas [61–63]. PTEN functions as a dual specificity phosphatase with the ability to dephosphorylate both proteins and lipids. It can dephosphorylate phosphoserine and phosphotyrosine residues in proteins, and convert the lipid phosphatidylinositol 3,4,5-trisphosphate (PIP3) to phosphatidylinositol 4,5-biphosphate (PIP2) via dephosphorylation. As a protein phosphatase, PTEN suppress MAPK signaling through dephosphorylation of focal adhesion kinase (FAK), and regulates cell-to-cell adhesion and thus inhibits cell survival, proliferation, migration and invasion [64–66]. PTEN’s lipid phosphatase activity is considered as its primary and major function. PTEN converts PIP3 to PIP2 and thus negatively regulates the PI3K/AKT signaling pathway that is important for cell proliferation, survival, and apoptosis [67–69].
2.4. p53 Mutations
The tumor suppressor, p53, is regarded as the guardian of the genome. It responds to variety of stress stimuli, including DNA damage and hypoxia [70, 71]. p53 acts as a transcription factor for a variety of genes related to DNA repair, cell cycle progression, apoptosis and the maintenance of cellular homeostasis [72]. Mutations in the p53 gene are associated with more aggressive phenotypes in various human cancers. p53 gene mutation analysis in melanoma established that approximately 10% of all melanomas harbor p53 mutations [73, 74]. Most of these mutations are ultraviolet radiation-induced mutations [75–77]. Furthermore, higher frequency of p53 inactivation in wild type BRAF and NRAS melanoma exhibited low ERK activity, suggesting MAPK independent melanoma progression [78, 79]. Although the frequency of p53 mutations in melanomas is low, various studies have demonstrated p53’s major role in the suppression of progression from nevus to melanoma [80, 81]. Several studies of superficial spreading melanoma have also found a longer relapse-free-survival rate among patients whose tumors expressed wild type p53 [82, 83].
2.5. CDKN2A/p16 Mutations
CDKN2A/p16 (also known as CDK4I or INK4a), a tumor suppressor gene associated with red hair and freckles, encodes a cyclin-dependent kinase (CDK) inhibitor p16. CDKN2A/p16 is responsible for cell cycle arrest at G1 checkpoint prior to the DNA synthesis (S) phase [84–86]. The CDKN2A/p16 protein inhibits phosphorylation and activation of retinoblastoma (Rb) proteins by CDK4 and CDK6. Since non-functional or inactivated CDKN2A/p16 shows reduced binding with CDK4, phosphorylation and activation of Rb occurs, resulting in abnormal cell proliferation [87, 88]. Cytogenetic, linkage and molecular analyses of the 9p21 region in familial and sporadic melanoma with multiple primary lesions has implicated CDKN2A/p16 as melanoma susceptibility gene [89]. CDKN2A/p16 mutations have been detected in variety of tumors including melanomas, providing evidence for CDKN2A/p16 involvement in the development of these malignancies [90, 91]. A study of 60 melanoma cell lines demonstrated that 92% of melanoma cell lines had aberrantly activated CDKN2A/p16 or CDK4. In the same study, 80% cell lines carried either non-function p16 or absent in p16 [92]. More importantly, the presence of CDKN2A/p16 germline mutations are not only associated with melanoma but also increase the risk of other malignancies such as pancreatic and breast cancer [54]. According to an estimate 5–10% of melanomas are known to be hereditary, and among those only 20–40% are associated with a pathogenic mutation in CDKN2A/p16 [93]. Frequency of CDKN2A/p16 mutation in familial melanoma ranged from 8–50% established after screening of 230 melanoma families worldwide for germline mutation in CDKN2A/p16 [94]. Furthermore, Americans who carry a CDKN2A/p16 mutation have an estimated 76% lifetime risk of developing melanoma [95]. Due to the exceptionally high probability of developing melanoma in the CDKN2A/p16 mutated population with poor prognosis of late-stage disease, it may be useful to institute a screening process to identify and warn CDKN2A/p16 mutation carriers of their high-risk status before the development of melanoma [96–98]. Recent studies have implicated that CDKN2B mutation is also involved in the promotion and progression of benign melanocytic nevi to melanoma [99].
3. PHYTOCHEMICALS FOR THE PREVENTION/TREATMENT OF MELANOMA
The role of diet and nutrition in the prevention of disease has gained public attention recently. A growing body of scientific evidence has established the protective effect of dietary manipulation, especially the use of dietary supplements to protect the skin from various diseases such as cancer. Epidemiologic studies have also addressed the role of dietary factors in melanoma prevention. Since these dietary phytochemicals are safe and carry minimal toxicity, they hold promising potential as complementary therapies for the treatment of melanoma as well [100–103]. In the present review, we have explored the protective and therapeutic potential of dietary phytochemicals against cell proliferation, apoptosis, invasion and metastasis by targeting signal transduction pathways (Table 1 and Fig. 1). These phytochemicals includes fisetin, epigallocatechin-3-gallate, resveratrol, curcumin, proanthocyanidin, silymarin, apigenin, capsaicin, genistein, indole-3-carbinol, and luteolin.
Table 1.
Phytochemicals and their cellular targets
| Name | Sources | Targets | References |
|---|---|---|---|
| Fisetin | Onion, cucumber, apple, persimmon, strawberry |
|
[106, 108, 110–112] |
| EGCG | Green tea |
|
[124–127, 129, 130] |
| Resveratrol | Peanut, grape skin, mulberry |
|
[152,153,155–163,171] |
| Curcumin | Turmeric |
|
[185–203] |
| Proanthocyanidins | Cocoa, grape, apple, tea, red wine |
|
[220–222] |
| Silymarin | Milk thistle |
|
[102,243,244] |
| Apigenin | Chicory, clove, apple, cherry, grape, beans, broccoli, celery, leeks, onion, barley, parsley, tomato, tea |
|
[154,252–256] |
| Capsaicin | Chili pepper |
|
[268, 270–273] |
| Genistein | Soybean |
|
[289–302] |
| Indole-3-carbinol | Broccoli, cauliflower, Brussels sprouts |
|
[325–327] |
| Luteolin | Carrot, pepper, celery, olive, peppermint, thyme, rosemary, oregano |
|
[343–350] |
Fig. 1.
Signal transduction pathways altered by selected phytochemicals. Fis inhibits PI3K, AKT, mTOR, NFκB, MEK, ERK, Wnt, β-catenin, MITF; EGCG inhibits NFκB; Res inhibits AKT, mTOR, NFκB, MEK, ERK, β-catenin, MITF, STAT3, c-kit, c-Jun, α-MSH; Sil inhibits NFκB, MEK, ERK, β-catenin, STAT3; Cur inhibits PI3K, AKT, NFκB, ERK, STAT3; Pro inhibits NFκB, ERK; Cap inhibits PI3K, AKT, mTOR, NFκB; Gen inhibits AKT, p38; I3C inhibits AKT, MITF; Lut inhibits α-MSH; Api inhibits PI3K, AKT, ERK, MITF, p38. p53 is upregulated by Res, Cur, Gen, Api.
Abbreviations: Fis=Fisetin, EGCG=Epigallocatechin gallate, Res=Resveratrol, Sil=Silymarin, Cur=Curcumin, Pro=Proanthocyanidin, Cap=Capsaicin, Gen=Genistein, I3C=Indole-3-carbinol, Lut=Luteolin, Api=Apigenin
3.1. Fisetin
Fisetin (3,3′,4′,7-Tetrahydroxyflavone) (Fig. 2A), a naturally occurring flavonoid, is commonly found in various fruits and vegetables such as strawberries, mangoes, kiwis, apples, grapes, persimmons, cucumbers and onions [104, 105]. Fisetin has shown to possess antioxidant, anti-inflammatory, and anti-proliferative properties against various cancers including melanoma and non-melanoma skin cancers [106–110]. Treatment of various malignant melanoma cell lines carrying different genetic characteristics (BRAF-mutant, NRAS-mutant, BRAF-NRAS wild type) with fisetin inhibited their invasion. Strengthening this finding, fisetin also decreased the invasive potential of melanoma cells in experiments using three-dimensional human skin equivalents. The anti-invasive effects of fisetin were associated with a decrease in the phosphorylation of MEK1/2 and ERK1/2 as well as inhibition of nuclear factor kappaB (NFκB) signaling pathway. Fisetin treatment also promoted mesenchymal to epithelial transition (MET) by decreasing mesenchymal marker proteins and increasing epithelial marker proteins [108]. Syed et al. [111, 112] observed downregulation of Wnt/β-catenin, PI3K/AKT, mTOR, and microphthalmia-associated transcription factor (MITF) signaling proteins in melanoma cell lines and in a three-dimensional human skin equivalent melanoma model. These findings show that fisetin is a phytochemical with promising anti-melanoma activities.
Fig. 2.
Fisetin and its structural analogs.
3.1.1. Bioavailability of Fisetin
Murine investigations have not been able to demonstrate any measurable toxicity of the phytochemical, fisetin [113, 114]. Bioavailability studies have demonstrated that fisetin was readily absorbed with detectable levels in the serum of mice [113, 115–117]. Pharmacokinetics studies involved conversion of fisetin-loaded dimyristoylphosphatidylcholine liposomal vesicles into nanocochleates by the action of Ca2+ ions. Analysis following intraperitoneal injection of nanocochleates showed a 141-fold higher relative bioavailability in mice [115]. In another study, liposomal encapsulation of fisetin increased bioavailability by 47-fold and enhanced the anti-tumor potential when compared to free fisetin [116]. Furthermore, intraperitoneal administration of the fisetin nano-emulsion resulted in a 24-fold increase of relative fisetin bioavailability [113].
3.1.2. Structure Activity Relationship of Fisetin
The basic flavonoid structure is two benzene rings (A- and B-ring) linked through a central heterocyclic pyrane (also known as pyrone or C-ring). The 2-position of the pyrone ring is generally with B-ring. The presence of an oxy group at position 4, a double bond between carbon atoms 2 and 3 (C2=C3 double bond), and a hydroxyl group at position 3 (3-OH) of the C-ring determine the type of flavonoid compound. Flavonols (e.g., quercetin, myricetin, quercetagetin, fisetin) all have an oxygen group at position 4, a C2=C3 double bond, and a 3-hydroxyl (3-OH) group and are known to possess anti-cancer properties [118]. Furthermore, fisetin, has 3′ - and 4' -OH on the B-ring, and elimination of 3' -OH on the B-ring, 4',5,7 trihydroxyflavone (THF) (Fig. 2B), has been shown to reduce the anti-cancer potency of fisetin. The important structural features of flavonoids (3'- and 4' -OH on the B-ring, 3-OH on the C-ring, the C2=C3 double bond in the C-ring and the phenylchromone C6–C5–C6) promote inhibition of epidermal growth factor (EGF)-induced cell transformation [118]. In another study, the structure activity relationship of fisetin was examined using different derivatives of the flavonoid. Sagara et al. [119] evaluated four trihydroxyflavones (THF), lacking one hydroxyl group, and three dihydroxyflavones (DHF), lacking two hydroxyl groups. All the derivatives tested promoted nerve cell differentiation and protected nerve cells from oxidative stress induced death, although there was a significant difference in both potency and efficacy. The 3,3',4' THF (Fig. 2C) most effectively induced differentiation, accomplishing this in >80% cells. Furthermore, Akaishi et al. [120] recently reported that the 3',4'-dihydroxyl (Fig. 2D) group is essential for the inhibitory effect of fisetin on amyloid beta protein fibril formation.
3.2. Epigallocatechin Gallate (EGCG)
Green tea (Camellia sinensis) leaves contain many polyphenols such as flavanols (catechins), flavandiols, and phenolic acid. Among them, the four main catechins present in green tea leaves are (−)-epigallocatechin gallate (EGCG), (−)-epicatechin gallate (ECG), (−)-epigallocatechin (EGC) and (−)-epicatechin (EC) (Fig. 3A–D). Epidemiological studies suggested that regular consumption of green tea attenuates the risk of many cancers. Green tea polyphenols and EGCG are known to have antioxidant, anti-mutagenic, anti-inflammatory, and anti-carcinogenic activities. [121–123]. Evidence shows that EGCG is more potent than other catechins in reducing the human melanoma cell growth [124]. Most importantly, neither EGCG nor other catechins have any effect on growth of normal melanocytes [125]. EGCG inhibits growth, promotes cell cycle arrest, and induces apoptosis of melanoma cells by modulating cyclin-dependent kinase network and Bcl-2 family proteins [125, 126]. In addition, combining EGCG with interferon/vorinostat therapy enhanced its efficacy against melanoma by targeting NFκB signaling pathways. Combination of EGCG/vorinostat significantly inhibited melanoma cell proliferation and increased apoptosis through activation of cell cycle inhibitory proteins, modulation of Bcl-2 family proteins, and NFκB signaling pathway. A recent study established that treatment of melanoma cells with EGCG at physiological dose reduced melanoma growth by inhibiting NFκB activity [127]. This was correlated with decreased IL-1β secretion. In addition, numerous investigations have demonstrated that EGCG inhibited many pro-inflammatory enzymes and cytokines such as iNOS, COX-2, MMPs, IL-6, IL-8, IL-12 and TNFα [128, 129]. EGCG-induced IL-1β suppression was mediated by downregulation of the inflammasome, decreased nuclear localization leucine-rich-repeat protein 1 (NLRP1), and reduced caspase-1 activation.
Fig. 3.
EGCG and its structural analogs.
In a recent study, Singh and Katiyar [130] demonstrated the anti-invasive potential of various green tea catechins on human melanoma cell invasion. They showed that EGCG carried the greatest inhibitory effect of the green tea catechins, with lesser effects from EGC > ECG, GC and EC. EGCG was found to inhibit melanoma cell invasion by decreasing EMT through reduced COX-2 expression, PGE2, and PGE2 receptors in melanoma cells [130]. Overall these findings revealed signaling pathways by which EGCG may inhibit invasion of melanoma cells. Thus this non-toxic, dietary component of green tea, EGCG, possesses antioxidant, anti-inflammatory, anti-carcinogenic potential, which makes it a logical candidate molecule for melanoma prevention and therapeutics.
3.2.1. Bioavailability of EGCG
Centuries of tea consumption provide evidence of EGCG’s safety in humans. Phase I clinical investigations have demonstrated that catechins and polyphenon E in doses ranging from 200 to 1200 mg were well-tolerated. Murine investigations found a broad range of bioavailability from 26.5% in mice to 1.6% in rats [131–133]. HPLC studies have revealed levels ranging from 5 to 150 ng/ml of EGCG, EC, and ECG in serum after oral tea consumption [134, 135]. Some bioavailability investigations have postulated that the low bioavailability may be because of the large size of the compounds [136]. The bioavailability of tea catechins in humans is relatively low at a range of only 0.2 to 2% [133, 137–139]. Oral administration of 1.5 mM of EGC, ECG and EGCG resulted in an average plasma concentration of 5 µM, 3.1 µM, and 1.3 µM respectively [140]. Oral consumption of 100 to 1600 mg of pure EGCG resulted in 0.26 to 6.35 µM of EGCG detectable in plasma after 2 to 3 hrs [141]. These studies show that tea catechins reach human plasma at the micromolar level (less than 1–2%) while the metabolites are present to a greater extent in human plasma after oral consumption of green tea [136, 142].
3.2.2. Structure Activity Relationship of EGCG
The catechins are the major components of green tea. These catechins contain a benzopyran skeleton with a hydroxyl or ester moiety at the 3-position and a phenyl group substituted at the 2-position. Catechins are classified by 2,3 subsituents and by the number of hydroxyl groups in the B- and D-ring [143]. In a recent study, using 10 different polyphenols demonstrated that anti-cancer potential of polyphenols such as catechin and epicatechin increases significantly if they were esterified with gallic acid to produce catechin gallate and ECG [144]. Among the 10 polyphenols, EGCG was most potent in inhibiting cell growth and inducing apoptosis. Although epicatechin has not demonstrated anti-proliferative effects, the catechin and epicatechin were found to significantly inhibit proliferation after esterification with gallic acid to form gallate and ECG. Similarly, gallic acid group of EGCG significantly enhanced catechin's anti-cancer potential. This property may be used to synthesize flavonoid derivatives to develop novel anti-cancer agents in the future [144]. Khandelwal et al. established that EGCG functions as an Hsp90 inhibitor [145]. They found that the prenyl-substituted aryl ester of 3,5-dihydroxychroman-3-ol ring system act as a novel scaffold that exhibits greater Hsp90 inhibition than EGCG. The abilities of various green tea polyphenols to inhibit cell growth, RAS signaling, and activator protein-1 (AP-1) activity were compared. With the exception of epicatechin, all of the tea polyphenols showed strong inhibition of cell growth and AP-1 activity. Among these compounds, both the galloyl structure on the B-ring and the gallate moiety inhibited growth and AP-1 signaling with the galloyl structure contributing the strongest effects. Catechin epimers such as theaflavin-3,3'-digallate, inhibited the phosphorylation of p38. EGCG decreased levels of c-Jun, while theaflavin-3,3'-digallate decreased the level of fra-1. Based on the results they suggested that catechins and theaflavins inhibited AP-1 activity and the MAPK pathway through different mechanisms [146]. EGCG inhibited the chymotrypsin-like activity of the proteasome organelle both in vitro and in vivo at concentrations equivalent to that found in the serum of green tea drinkers. Atomic orbital energy analyses and HPLC demonstrated that the carbon of the polyphenol ester bond is necessary for inhibition of proteasome activity in cancer cells [147, 148]. In an effort to discover more stable polyphenol proteasome inhibitors, Landis-Piwowar et al. [149] synthesized several novel EGCG analogs and observed that elimination of hydroxyl groups from either the B- or D-ring decreased proteasome inhibition in vitro. Another group developed alkyl gallate and gallamide derivatives with strong anti-proliferative and apoptotic activity against human cancer cells by using the EGCG-derived galloyl group as a core structure [150]. Dodo et al. [150] the pioneers of the aforementioned technique, subsequently added a galloyl group into alkyl gallates and gallamides to synthesize various bisgallate and bisgallamide derivatives. This enhanced the anti-proliferative effects of gallamides but not alkyl gallates.
3.3. Resveratrol
It is a polyphenolic phytoalexin stilbenoid derivative of stilbene (Fig. 4A), produced naturally by a wide variety of plants such as grapes, peanuts, mulberries, cranberries, and eucalyptus. Resveratrol is known to possess cardio-protective, antioxidant, neuroprotective, immunomodulatory, anti-inflammatory, metabolism-regulating, and anti-cancer effects [151]. An accumulating body of evidence has shown that resveratrol inhibits cell growth and induces apoptosis in various melanoma cells by S-phase cell cycle arrest and down-regulation of cyclins [152, 153]. In addition, Caltagirone et al. [154] found that intraperitoneal administration of resveratrol delayed the tumor growth in mice. Fang et al. [155] recently found that resveratrol enhances the sensitivity of melanoma cells to radiation by inhibiting proliferation and inducing apoptosis. The anti-proliferative effects of resveratrol following radiation were associated with decreased expression of the proliferative molecules. Decreased expression of the anti-apoptotic molecules cFLIP, Bcl-2 and survivin correlated with the apoptotic effects of resveratrol after radiation. In a recent study, Gatouillat et al. [156] showed that resveratrol inhibited the growth of a doxorubicin-resistant B16 melanoma cells through inhibition of the G1/S phase transition, down-regulation of cyclin D1/cdk4, and increased expression of p53, which ultimately induced apoptosis. Furthermore, resveratrol reduced the growth of doxorubicin-resistant B16 melanoma cells in mice and prolonged survival of mice compared to untreated controls. In studies of DR5-positive melanoma cells, Ivanov et al. [157] found that resveratrol decreased signal transducer and activator of transcription 3 (STAT3) and NFκB activation, suppressed Bcl-xL and cFLIP proteins, and enhanced cellular sensitivity to exogenous TRAIL. Furthermore, upregulation of the α-melanocyte-stimulating hormone (α-MSH) signal transduction pathway involving Wnt/β-catenin, c-kit, and MITF were suppressed by resveratrol [158]. These signaling pathways have well-established roles in the immortality, viability, and invasiveness of melanoma cells [159]. In addition, Lee et al. [160] found that resveratrol inhibited STAT3 acetylation, which is markedly increased in melanoma cells when compared to normal melanocytes. Inactivation of the estrogen receptor alpha (ERα) gene via methylation strongly correlates with poor prognosis as well as an aggressive phenotype of melanoma [159]. Resveratrol reactivates gene expression in tumors by reducing STAT3 acetylation [158]. In addition, it triggers protective autophagy by increasing signaling through the ceramide/AKT/mTOR pathway in B16 melanoma cells [161]. In a recent study, Trapp et al. [162] found that resveratrol stimulated isolated human umbilical vein cell (HUVEC) proliferation, however it resulted in growth inhibition of HUVECs grown with melanoma cells in three-dimensional co-culture and in three-dimensional spheroids. This selective effect of the compound on melanoma cells was associated with increased p53 expression and matrix protein thrombospondin-1. Resveratrol inhibited vascular endothelial growth factor (VEGF) production through enhanced expression of hypoxia inducible factor-1α. Furthermore, resveratrol reduced hepatic metastatic invasion of B16M melanoma cells inoculated intra-splenically by decreasing vascular adhesion molecule 1 expression in the hepatic sinusoidal endothelium. This consequently decreased B16M cell adhesion to endothelial cells through late activation of antigen 4. Resveratrol was found to inhibit the nuclear translocation and transcriptional activity of NFκBp65, an important inducer of EMT. This lead to significantly prolonged animal survival time and reduced melanoma tumor sizes in vivo. This was associated with inhibition of lipopolysaccharide induced tumor migration and decreased markers of EMT [159, 163]. These data support a potential use of mono or combination resveratrol therapy for the management of melanoma.
Fig. 4.
Resveratrol and its structural analogs.
3.3.1. Bioavailability of Resveratrol
The bioavailability and pharmacological activity of resveratrol in rabbits, rats, and mice models have been reported after intravenous and oral administration [151]. Oral treatment of mice with 20 mg/kg resveratrol yielded the highest plasma concentration (2.6 ±1.0µM) after 5 min. In another study, Asensi et al. [164] reported that intravenous administration of resveratrol (20 mg/kg) to rabbits yielded its maximum concentration in plasma (42.8 ± 4.4 µM) 5 min after administration, but reduced rapidly to 0.9 ± 0.2 µM (0.2 mg/l) at 1 hr. More importantly, when the same quantity of resveratrol is administered orally, the maximum concentration reached in plasma (2–3 µM in mice and about 1 µM in rabbits or rats) within the first 5 min after administration followed by a decrease in its level to less than 0.1 µM at 1 hr [165–167]. Compounds such as glucuronides or sulfates are the most common resveratrol metabolites found in human plasma or urine following oral consumption [168, 169]. In another studies, administration of single dose of 0.5 g to 5 g resveratrol in 40 healthy volunteers showed that free resveratrol is rapidly absorbed with a comparatively low mean plasma concentration from 73 ng/mL (50.3 mmol/L) to 539 ng/mL (52.4 mmol/L) respectively [168–170]. After 5–6 hrs, the concentration of resveratrol metabolites [resveratrol-3-O-sulfate (with a maximum concentration of 1135–4294 ng/mL (3.7–14 mmol/L) and monoglucuronides] was 20 fold high than the free resveratrol with plasma half-life of 2.9 – 11.5 hrs.
3.3.2. Structure Activity Relationship of Resveratrol
Resveratrol has demonstrated its potential to inhibit melanoma growth by targeting various signaling pathways [153–157, 159, 171]. Murias et al. [172, 173] synthesized resveratrol derivatives by increasing the number of hydroxyl groups on the phenol rings of the stilbene structure and evaluated their anti-tumor potential against human cancer cell lines. The cytostatic activity exhibited by hydroxystilbenes with ortho-hydroxyl groups was three-fold higher as compared to hydroxystilbenes with other moieties. Hydroxylated resveratrol analogs exhibited COX-2 inhibition, while methoxylated resveratrol did not exhibit these effects. In addition, resveratrol derivatives such as 3’,4′,3,5-tetrahydroxy-trans-stilbene (piceatannol), 3,4,4′,5-tetrahydroxy-transstilbene and 3,4,5,3′,4′,5′-hexahydroxy-trans-stilbene (Fig. 4B,C,E) demonstrated a 6,600-fold anti-radical activity above resveratrol. In another study, Lee et al. [174] found that the hydroxyl group at the meta position of the B-ring is crucial for MEK/ERK inhibition in the resveratrol analogue, 3,5,3′,4′,5′-pentahydroxy-trans-stilbene (Fig. 4D), which acts by inhibiting cell transformation. An accumulating body of evidence has demonstrated that increasing the number of hydroxyl groups on the ring-structure further enhances the cytotoxic and free-radical-scavenging effects of resveratrol [172–175]. Furthermore, Murias et al. [172, 173] reported that hexahydroxystilbene (M8) (Fig. 4E) was the most effective resveratrol analogue against various cancer cell lines including melanoma through inhibition of deoxynucleosidetriphosphate formation (dATP and dTTP) by inhibition of enzyme ribonucleotide reductase. Moreover, hexahydroxystilbene (M8) was active in inhibiting the melanoma growth in two different melanoma animal models. Wachek et al. [176] demonstrated that hexahydroxystilbene (M8) was effective in sensitizing malignant melanoma in vivo as a single compound and in combination with dacarbacine. In this study, animals that were treated with a combination of hexahydroxystilbene (M8) and decarbacine were found to be tumor free due to synergistic action of these compounds. Furthermore, hexahydroxystilbene (M8) inhibited cell migration in matrigel assays. In addition, hexahydroxystilbene (M8) inhibited melanoma tumor growth and prevented metastasis of melanoma cells to distant lymph nodes in the SCID mouse model [177–179]. Monohydroxylated resveratrol (also, piceatannol) possesses better anti-tumor activity than resveratrol itself and is a potent COX-2 inhibitor. Piceatannol has also been found to induce apoptosis of SK-MEL-28 melanoma cells by downregulating cyclins A, E and B1 (causing cell cycle arrest at the G2 phase) and by inhibiting NFκB signaling [152]. In fact, Ashikawa et al. [180] demonstrated that the hydroxyl groups of stilbenes are critical for suppression of NFκB activation. Studies using human melanoma cells demonstrated that 3,4,5,4′-tetramethoxystilbene (DMU-212) (Fig. 4F) exerts it anti-mitotic effect by ERK1/2 activation [181]. Moreover studies have demonstrated that methylation at key positions of the cis-resveratrol (Fig. 4G) form results in more potent methylated analogs of cis-resveratrol (cis-3,5,4′-trimethoxystilbene) (Fig. 4H) with enhanced anti-cancer properties [182].
3.4. Curcumin
Curcumin (Fig. 5A) is a hydrophobic, polyphenolic, bioactive compound extracted from the rhizome of the dietary spice turmeric (Curcuma longa). Turmeric, commonly found in curry powder, has been used for centuries in indigenous medicine as it possesses wide-range of anti-inflammatory, antioxidant, and anti-cancer properties [183]. The chemotherapeutic potential of curcumin is evident by its known abilities to induce apoptosis and cell adhesion as well as inhibit angiogenesis in cancer cells. Phase I and phase II clinical trials have established its safety and therapeutic efficacy in cancer patients [184]. The compound was found to exert its anti-cancer effects by targeting AKT [185], NFκB [186], AP-1 [187], and c-Jun N-terminal kinase [188].
Fig. 5.
Curcumin and its structural analogs.
In melanoma cells, curcumin has been found to induce apoptosis through several mechanisms including upregulation of p53, p21(Cip1), p27(Kip1), and checkpoint kinase 2. It also decreases cancer cell survival by downregulating NFκB, iNOS, and DNA-dependent protein kinase catalytic subunit expression [189]. Furthermore, curcumin treatment of melanoma cells attenuated NFκB binding activity without suppressing the BRAF kinase pathway or AKT phosphorylation. Evidence suggests that curcumin decreases tumor growth by inhibiting glutathione S-transferase, inducing apoptosis through the Fas receptor/caspase-8 pathway, inhibiting COX enzymes, and by downregulating NFκB signaling [190–192]. Endoplasmic reticulum (ER) stress triggers curcumin to activate death pathways through p23 cleavage and downregulation of the anti-apoptotic Mcl-1 protein in melanoma cells [193]. Furthermore, the anti-metastatic potential of curcumin worked by downregulating collagenase activity, FAK expression, and MMP-2 function. It also modulated integrin receptors and upregulated the expression of E-cadherin [194]. Curcumin also has the potential to reverse melanoma cell multi-drug resistance by inhibiting glutathione-S-transferases [195, 196]. Elevated expression of the phosphatase of regenerating liver 3 (PRL-3), a member of tyrosine phosphatase family, has been found in highly metastatic melanomas. PRL-3, an oncogene that promotes tumor cell motility and invasion [197, 198], was downregulated by curcumin [199], thus raising its profile as a possible anti-cancer agent.
Curcumin suppresses osteopontin (OPN)-induced IκBα phosphorylation and degradation by inhibiting the IKK activity in B16F10 murine melanoma cells. Furthermore, curcumin inhibited the OPN-induced translocation of NFκBp65, NFκB-DNA binding, and NFκB transcriptional activity along with reduction of MMP activities. As a consequence of reduction in the NFκB signaling pathway, it synergistically induced apoptosis by inhibiting OPN-induced cell proliferation, migration and invasion. More importantly, curcumin suppressed the OPN-induced tumor growth in nude mice [200, 201]. Oral administration of curcumin in melanoma-tumor-bearing mice has been found to inhibit the lung metastasis of melanoma by as much as 80%, thus lengthening the survival of mice by 144% [202, 203].
3.4.1. Bioavailability of Curcumin
Pharmacological studies have shown that curcumin is non-toxic and effective in the treatment and prevention of many diseases. Epidemiological and scientific evidence have shown its beneficial health effects as antioxidant, anti-inflammatory and anti-cancer agent [204]. In one study, oral administration of curcumin 2g/kg in experimental rats resulted in 1.35±0.23 µg/ml peak serum concentration after 0.83 hr, though the same dose in humans resulted in very low serum levels (0.006±0.005 µg/ml) after 1 hr [205]. In another study, Cheng et al. [206] reported that 4–8 g/kg oral administration of curcumin to humans resulted in 0.41–1.75µM/ml peak plasma concentration after 1 hr. Clinical trials demonstrated a 11.1 nmol/L plasma concentration in participants one hour after 3.6 g/kg oral administration of curcumin [207]. However, intravenous administration of curcumin in rats showed a 50-fold higher serum concentration when compared to oral administration [208].
3.4.2. Structure Activity Relationship of Curcumin
Curcumin, a natural diaryl heptanoid, can be obtained from substituted aryl aldehydes and acetylacetone, which enables the synthesis of a diverse set of curcumin analogs. Numerous analogs have been synthesized and are being tested against known biological targets to improve upon the pharmacological, absorption, distribution, metabolism and secretion profile by modifying substitutions on its aromatic rings, the β-diketone moiety, and the two flanking double bonds that are conjugated to the β-diketone moiety. This has led the way for researchers to further study the structure-activity relationship of curcumin in medicinal chemistry [209, 210]. Interestingly, Pisano et al. [211] recently showed that a new curcumin analog alpha,beta-unsaturated ketone D6 [(3E,3'E)-4,4'-(5,5',6,6'-tetramethoxy-[1,1'-biphenyl]-3,3'-diyl)bis(but-3-en-2-one)] (Fig. 5E) was more effective at inhibiting melanoma cell growth and inducing apoptosis in vitro and in vivo when compared to curcumin [211, 212]. Other curcumin analogs (FLLL32 and FLLL62) (Fig. 5C–D) reduced STAT3 phosphorylation resulting in apoptosis induction at micromolar concentrations in human melanoma cell lines. Furthermore, treatment with these analogs inhibited STAT3 target genes expression, uncoupled mitochondrial membrane potential and induced caspase-mediated apoptosis [213, 214]. The DM-1 compound (Sodium 4-[5-(4-hydroxy-3-methoxyphenyl)-3- oxo-penta-1,4-dienyl]-2-methoxy-phenolate) (Fig. 5B) is a curcumin analog that possesses curcumin’s anti-proliferative, anti-tumor, and anti-metastatic characteristics [215]. A recent study by Zhang et al. [216] demonstrated that EF24 (diphenyl difluoroketone) (Fig. 5F) suppressed melanoma cell migration and EMT by targeting HMGA2.
3.5. Proanthocyanidins
Proanthocyanidins, the secondary metabolites of plants are present in various fruits and plant-derived beverages such as cocoa, grapes, apple, tea and red wine [183, 217, 218]. Proanthocyanidins belong to a class of condensed tannins made of (+)-catechin, (−)-epicatechin and other flavonoid oligomers and polymers. Linkages between these oligomers and polymers typically consist of B type (C4→C6 or C8) or A-type bonds (C2→O7). Grape seed extract proanthocyanidins (GSPs), the most common proanthocyanidin consumed by humans, contain B-type linkages. Grape seeds are considered as a good source of polyphenolic proanthocyanidins and procyanidins. GSPs exhibit antioxidant and anti-inflammatory properties [183, 219, 220]. GSPs are predominantly composed of proanthocyanidin, catechin or epicatechin oligomers [219]. Although GSPs have been shown to have antioxidant, photo-protective, and anti-tumor effects, their chemotherapeutic/preventive effects on melanoma are yet to be explored. In a recent study, Vaid et al. [221] demonstrated the effect of GSPs on melanoma cell invasion and delineated the molecular mechanism underlying these effects. GSPs inhibited melanoma cell invasion through decreased COX-2 expression and PGE2 production. It also decreased cellular migration and phosphorylation of ERK1/2 induced by 12-O-tetradecanoylphorbol-13-acetate. GSPs also inhibited the activation of NFκBp65. Inhibition of melanoma cell invasion by GSPs increased the levels of epithelial biomarkers with a concomitant loss of mesenchymal biomarkers in melanoma cells, indicating that inhibition of invasion was related with reversal of the EMT process [221]. In addition, a murine study found grape seed extract administration to be associated with significantly fewer metastatic pulmonary melanoma nodules (a 26% decrease) when compared to controls [222].
3.5.1. Bioavailability of Proanthocyanidins
In the United States, the average dietary intake of proanthocyanidins has been estimated to be 58 mg/day [223, 224]. Absorption of monomeric flavonoids including (+)-catechin and (−)-epicatechin following the consumption of dietary proanthocyanidins has been reported in humans and animals, either as parent compounds or conjugated metabolites. There have been limited and conflicting bioavailability studies of larger proanthocyanidins to-date [225, 226]. In a study, Deprez et al. [227] demonstrated that human microbiota degrade proanthocyanidins to low molecular weight phenolic compounds. Moreover, appearance of simpler compounds such as benzoic acids, phenylpropionic acids, phenylacetic acids, phenylvaleric acids, phenylpropionic acids, and phenylacetic acids in the plasma and urine have been reported after proanthocyanidin melabolism [228, 229]. Animal and human studies have demonstrated the detection of unconjugated procyanidin B2 in plasma 30 min following consumption of proanthocyanidin extracts or proanthocyanidin-rich seeds. Levels of unconjugated procyanidin B2 were found to peak approximately 2 hrs after high-dose oral proanthocyanidin administration with an associated 63% excreted in the urine within 4 days of administration [224–226]. However, the bioavailability of larger proanthocyanidins is still unclear [226, 230].
3.5.2. Structure Activity Relationship of Proanthocyanidins
Structural analogs of proanthocynidins have been synthesized and evaluated for anti-cancer potential due to their unique structures and significant biological activities. Kashiwada et al. [231] reported on the cytotoxic potential of proanthocyanidins in an analysis of 57 tannin-related compounds such as gallotannins, ellagitannins and condensed/complex tannins. These compounds exhibited weak cytotoxicity against RPMI-7951 human melanoma cells while being less active against several other cell lines [231, 232]. Synthesis and evaluation of anti-tumor activity of proanthocynidin was first reported by Kozikowski et al. [233]. Numerous compounds were synthesized and their efficacy was tested against various human cancer cell lines. Kozikowski et al. [234] synthesized procyanidin epicatechin oligomers and evaluated for anti-tumor potential. Cytotoxic effects were observed based on the induction of cell cycle arrest in the G0/G1 phase was associated with high degree of oligomerization and activity was observed for the epicatechin dimer, trimer and tetramer. Prodelphinidin B1, B2 and B4 showed significantly better cytotoxic activity than EGCG and prodelphinidin B3 (Fig. 6A–D). Prodelphinidin B3 and C2 were almost the same as EGCG (Fig. 6D,E) [235].
Fig. 6.
Proanthocyanidin and its structural analogs.
3.6. Silymarin
Silymarin, a flavanolignan extracted from the milk thistle plant (Silybum marianum L. Gaertn) [236, 237], possesses important therapeutic potential. Silymarin exists as a mixture of three flavonolignans, silybin, silydianin and silychristin with silybin serving as the most abundant (70–80%) and most biologically active component [238]. Pharmacological studies have shown that silymarin is safe even at higher physiological doses, which may translate to safety for human use. Silymarin possesses antioxidant, anti-inflammatory, cytoprotective, and anti-carcinogenic properties [239, 240]. An accumulating evidence suggests that both silymarin and silybin exhibit similar chemopreventive properties [241, 242].
Silymarin has been found to inhibit migration and invasion of melanoma cells by targeting the β-catenin signaling pathway. It inhibited nuclear translocation of β-catenin, increased levels of casein kinase 1α, upregulated glycogen synthase kinase-3β (GSK-3β), enhanced β-catenin phosphorylation and thus increased binding of phosphorylated β-catenin with β-transducin repeat-containing proteins (β-TrCP) [102]. Furthermore, silymarin reduced MMP-2 and MMP-9 levels, which are down-stream effectors of β-catenin signaling pathway. In another study, Lee et al. [243] reported that silybin induces cell cycle arrest at G1 phase and inhibits MEK1/2, ribosomal S6 Kinase 2 signaling and phosphorylation of ERK1/2 in melanoma cells. Furthermore, it reduced NFκB, AP-1 and STAT3 activation in melanoma cells in vitro and in vivo. In addition, silymarin increased apoptosis of melanoma cells by upregulating Fas-associated proteins with death domain (FADD) expression and enhancing procaspase-8 cleavage [244].
3.6.1. Bioavailability of Silymarin
In a study Schandalik et al. [245] demonstrated that, after single dose of oral administration of 120 mg silybin in 14 patients demonstrated that it was quickly absorbed from the gastrointestinal tract and levels of free drug peaked within 3 hrs. Total (free + conjugated) silybin levels (≥400 ng/ml) reached a peak at about 3 to 4 hrs were >40 fold higher than the free silybin and maintained up to 24 hrs. After reaching peak concentration at about 3 to 4 hrs, free silybin levels were declined and at 12 hrs reaches to limit of quantification (2 ng/ml). Administration of single dose of silipide and silymarin (120 mg, as silybin) demonstrated a several-fold higher serum concentration of silipide after 4 hrs versus silymarin. Forty-eight hours after oral silipide and silymarin administration, 11% and 3% silybin was observed in bile, respectively [246]. This study confirmed that silybin (derived from silipide) has superior bioavalability as compared to silymarin. Furthermore, Weyhenmeyer et al. [247] demonstrated a linear dose-response relationship in a human investigation of oral silybin administration. Approximately 10% of total silybin in plasma was found to be unconjugated within 4–6 hrs. Moreover, elimination half-life for total silybin was ~6 hrs and about 5% of the silybin administered was excreted into the urine indicating the good renal clearance. More importantly, silymarin is very well tolerated in humans without any adverse health effects [247, 248].
3.6.2. Structure Activity Relationship of Silymarin
Since silymarin is a mixture of three isomers with silybin (Fig. 7A) acting as the most active as hepato-protective agent, Ahmed et al. [249] synthesized different analogous and evaluated them for structure activity relationship. The most hepato-protective analog contained a hydroxymethyl group at position 2 of the dioxanes ring. In a recent study, Agarwal et al. [250] synthesized and characterized a series of silybin derivatives namely 2,3-dehydrosilybin (DHS), 7-O-methylsilybin (7OM), 7-Ogalloylsilybin (7OG), 7,23-disulphatesilybin (DSS), 7-O-palmitoylsilybin (7OP), and 23-O-palmitoylsilybin (23OP). In an investigation of the anti-cancer activity of these compounds, 2,3-dehydrosilybin (DHS), 7-O-methylsilybin (7OM), 7-Ogalloylsilybin (7OG) (Fig. 7B–D) exhibited improved growth inhibitory effects compared to silybin. Results from their study clearly suggest that structural modifications can improved the anti-cancer efficacy of silybin. Furthermore, many water-soluble semi-synthetic analogs of silybin were prepared by various laboratories but increased in water solubility led to decrease in the activity.
Fig. 7.
Silybin and its structural analogs.
3.7. Apigenin
Apigenin (4',5,7-trihydroxyflavone) (Fig. 8A), a flavonoid belonging to the flavone structural class, is found in plants such as parsley, celery, artichokes and chamomile. A growing body of evidence has shown that apigenin possess antioxidant, anti-mutagenic, anti-carcinogenic, anti-inflammatory, and anti-proliferative properties [251]. In addition, preparations from chamomile have been historically used to treat cutaneous inflammation and other dermatological diseases [251]. Apigenin has been identified as a cancer chemopreventive agent owing to its potent antioxidant, anti-melanoma and anti-inflammatory activities with low toxicities [252, 253]. In two separate studies, Caltagirone et al. [154] and Piantelli et al. [254] found that apigenin inhibited melanoma tumor growth (B16-BL6 melanoma cells) in vivo and inhibited VEGF secretion by downregulating ERK1/2 and PI3K/AKT signaling in vitro [252]. Moreover, apigenin significantly decreased the invasion of melanoma cells in vitro and inhibited lung metastasis in vivo by reducing lung colonization of B16-BL6 cells in mice [154, 254]. In a recent study, Das et al. [255] observed that apigenin inhibits cell growth and induced apoptosis in A375 melanoma cells with no concomitant toxicity to peripheral blood mononuclear cells. Further, apigenin’s therapeutic efficacy was enhanced by the poly-lactic-co-glycolide formulation, since this vehicle readily enters cancer cells, intercalates with dsDNA, and induces conformational change [256].
Fig. 8.
Apigenin and its structural analogs.
3.7.1. Bioavailability of Apigenin
Apigenin’s low intrinsic toxicity and anti-cancer potential have gained attention in recent years. The pure form of apigenin is unstable and least soluble in water and organic solvents. In nature, apigenin exists in the form of water-soluble glycoside conjugates and acylated derivatives [257, 258]. The absorption and bioavailability of apigenin is determined by conjugated moiety, since the compound undergoes enzymatic cleavage by mammalian or microbial glucosidases before absorption. It has been found that apigenin remains bound to β-galactoside in its natural form, which provides its best bioavailability [259–261]. In the gut, apigenin is metabolized via uridine 5'-diphospho-glucuronosyltransferase UGT1A1 as glucoroside and sulfate conjugates, which are more easily excreted in bile or urine. Gradolatto et al. [259] have shown that apigenin appeared in the blood 24 hrs after oral intake of a single dose of radio labeled apigenin. In rats, oral intake after a single dose of radio-labeled apigenin resulted in 51% detection of 51, 12, 1.2, 0.4, 9.4, 1.2, and 25% of the radioactive compound in urine, feces, blood, kidneys, intestine, liver, and the remaining tissues, respectively, within 10 days. Furthermore, kinetics of apigenin in blood exhibited a relatively high elimination half-life of 91.8 hrs (slow excretion) compared to other dietary flavonoids [258, 261]. These results clearly demonstrated the limited bioavailability of apigenin, though slow pharmacokinetics may lead to possible accumulation of this flavonoid in the tissues to effectively impart its chemopreventive effects [259–262].
3.7.2. Structure Activity Relationship of Apigenin
Protoapigenone, a natural apigenin derivative, has demonstrated a 10-fold greater anti-tumor activity than apigenin in vitro and in vivo [143, 263, 264]. Several apigenin derivatives have been synthesized and studied for their anti-cancer potential [265, 266]. Derivatives such as 1'-O-alkyl-protoapigenone and protoapigenone 1'-O-butyl ether (Fig. 8B,C) exerted significantly stronger activity than the non-substituted analog protoapigenone. On the contrary, β-naphthoflavone derivatives containing same pharmacophore when substituted with an O-alkyl side-chain at position 1 showed decreased cytotoxic activities. Furthermore, Liu et al. [267] demonstrated that nitrogen-containing apigenin analogs (R= ethylamino, propylamino, isopropylamino etc.) showed better anti-cancer and antioxidant potential (Fig. 8D).
3.8. Capsaicin
Capsaicin (Fig. 9A), a pungent component of chili peppers, is one of the most commonly used spices in the world [268]. Though capsaicin has historically been used for its anti-inflammatory and analgesic abilities [268], it is receiving increasing attention for its anti-tumor properties [269]. Evidence suggests that capsaicin induces A375 melanoma cell apoptosis by activating caspases 3, 8, and 9, which is accelerated by its downregulation of Bcl-2 [270]. It also reduces melanoma cell survival by decreasing NFκB activity [271, 272]. The compound was found to inhibit growth and increase apoptosis of A375 and SK-MEL-28 melanoma cells by inhibiting plasma membrane NADH oxidase activity [273]. It also inhibited the migration of B16-F10 melanoma cells through inhibition of the PI3K/AKT/Rac-1 pathway [268]. The compound’s effects on VEGF are currently under debate, however. While Patel et al. [271, 272] found that capsaicin decreased cell proliferation through enhanced VEGF production in A375 melanoma cells. Min and colleagues [274] observed its ability to decrease angiogenesis in cultured human endothelial cells. Despite the current uncertainty of capsaicin’s effects on VEGF production, the body of evidence suggests that capsaicin promotes apoptosis, decreases survival, and inhibits migration of melanoma cells.
Fig. 9.
Capsaicin and its structural analogs.
3.8.1. Bioavailability of Capsaicin
Capsaicin is a lipophilic compound that has demonstrated fast absorption and a short half-life in humans. In addition, the compound resists diffusion and in vitro studies have shown that it exhibits a slow cutaneous biotransformation in humans [275, 276]. After intragastric administration of 15 mg/kg body weight capsaicin in rats, the plasma concentrations peaked to approximately 10 ng/ml after the first hr and then declined rapidly, with an absolute bioavailability of orally administered capsaicin to be 0.106% [277, 278]. According to Chaiyasit et al. [279] oral administration of capsaicin (26.6 mg) in humans resulted in maximum plasma concentration of 47.1 (2.0) min with T1/2 of 24.9 (5.0) min, and 2.5 (0.1) ng ml−1 of Cmax. In another study conducted by Suresh and Srinivasan [280], oral administration of 30 mg/kg body weight capsaicin in rats demonstrated 94% bioavailability. In a recent study, Rollyson et al. [281] demonstrated that orally administered capsaicin resulted in detectable levels in the liver, lungs, kidney and serum of the mice within 15 min after oral administration. The maximum concentration was observed at 60 min and the lungs exhibited the greatest absorption.
3.8.2. Structure Activity Relationship of Capsaicin
The cytotoxic potential of vanilloid compounds was evaluated by modifying vanilloid ring pharmacophores and nonivamide analogs of capsaicin versus the transient receptor potential vanilloid-1 (TRPV1). Specific regions of the compound including the aromatic “A-ring”, the hydrogen bond-donating group in the “B-region” and the hydrophobic hydrocarbon “C-region” tail are required for maximum potency at TRPV1 [282–285]. Analogs with “A-ring” modification such as 6-iodo-nordihydrocapsaicin (Fig. 9B) and 3-methoxy-4-hydroxybenzyl have been identified as the most potent. Removal of the 4-OH or 3-MeO moieties or modification of positions 2, 5 and 6 of the “A-ring” has been found to significantly reduce its activity [277, 286, 287].
3.9. Genistein
Genistein (4',5,7-trihydroxyisoflavone) (Fig. 10A), a phytoestrogen and isoflavone found in soybeans with structural and functional similarities to estrogen, has anti-inflammatory and antioxidant effects with ongoing investigation into its ability to prevent and treat cancer, metabolic syndrome, diabetes, and chronic inflammatory diseases. Genistein has been found to inhibit angiogenesis, promote apoptosis, reduce tumor metastasis, and decrease proliferation in various malignancies ranging from neuroblastoma to breast cancer [100, 288, 289]. It has been found, however, to promote melanoma cell differentiation through stabilization of protein-linked DNA strand breakage in SK-MEL-131 cells [290, 291]. Genistein has been shown to have beneficial effects against various melanoma cells by inhibiting cell cycle progression and inducing apoptosis while inhibiting tumor growth and metastasis potential of B164A5 melanoma cells in C57BL/6J mouse model [289, 292, 293]. Genistein inhibited cell cycle progression in melanoma cells by targeting cellular p53, p21, checkpoint kinase 2 (Chk2) [294–297]. Furthermore, it inhibited invasion, cell adhesion and lung metastasis of melanoma cells in mice [298–300]. It also inhibited angiogenesis in mouse model of melanoma [288, 301]. Moreover, it induced differentiation of mouse and human melanoma cells [302–304].
Fig. 10.
Genistein and its structural analogs.
3.9.1. Bioavailability of Genistein
Genistein’s high lipid solubility, significant first-pass metabolism and fast gut transit time strongly limit its bioavailability [305, 306]. However, Coldham et al. [307] observed a peak serum concentration 30 min after an oral administration of 4 mg/kg. In another study, Steensma et al. [308] were able to detect serum genistein 15 min after portal vein administration. Oral treatment yielded a 5.49 µM maximum concentration after 15 min. In another study, Kwon et al. [309] found that 4, 20 and 40 mg/kg genistein oral administration resulted in 39, 24 and 31% bioavailabilities, respectively. Oral genistein treatment (40 mg/kg) yielded a Tmax, Cmax and AUC(0−∞) of 2 hrs, 4880 ng/ml and 0.03 mg hr/ml, respectively. It is suggested that in infants, consumption of 4–7 mg/kg per day of total genistein will result in 1–5 µM of total circulating genistein. Adults can safely consume 1mg/kg of genistein per day resulting in ~0.5 µM serum concentration. An accumulating body of evidence has shown that genistein is safe and very well tolerated in humans [310–312].
3.9.2. Structure Activity Relationship of Genistein
Several synthetic analogs of genistein have been developed to explore its potential beneficial effects [313]. Ullah et al. [314] found that genistein possessed greater antioxidant and DNA-protective effects than its methylated structural analogue biochanin A (Fig. 10B). Genistein derivatives with substitutions at the C7 hydroxyl group of the A-ring exhibited anti-mitotic activity while analogs substituted at the 4′-position of the B-ring (Fig. 10C) induced p53-independent G1 cell-cycle arrest and autophagy [315]. In addition, genistein derivatives have been found to be non-genotoxic [316]. Several studies have shown that genistein glycoconjugates (Fig. 10D) exhibit anti-proliferative potential [313, 317, 318] and even induce cell cycle arrest [319, 320]. Interestingly, some of these analogs also inhibited microtubule assembly [318, 319, 321].
3.10. Indole-3-Carbinol
Indole-3-carbinol (I3C) (Fig. 11A) is a bioactive metabolite of glucosinolate glucobrassicin, a substance found at high concentrations in vegetables from the family Cruciferae including broccoli, cauliflower, and Brussels sprouts [322, 323]. The compound has been found to inhibit proliferation through various mechanisms in various cancer cell lines [322]. Animal models have also demonstrated the promise of I3C in the prevention of chemical-induced tumorigenesis of breast, liver, lung, cervical, and gastrointestinal tract tissues [324]. Thus far, I3C has only been found to promote apoptosis in melanoma cell lines. In addition, I3C sensitized G361 melanoma cells to UVB radiation through decreased anti-apoptotic Bcl-2 expression [325]. Another study found that I3C induces apoptosis in SK-MEL-5 melanoma cells by down-regulation of MITF [326]. Furthermore, I3C-mediated anti-proliferative effect was through interaction with neuronal precursor cell-expressed developmentally down regulated 4 and wild-type PTEN degradation in human melanoma cells [327]. I3C consumption was also associated with increased sensitivity to chemotherapy in a study of mice with B16 melanoma [328]. I3C is a promising compound that may be effective in melanoma therapy, especially since evidence suggests that it decreases the expression of MITF, a signaling molecule known to be over-activated in resistant cases of melanoma [326].
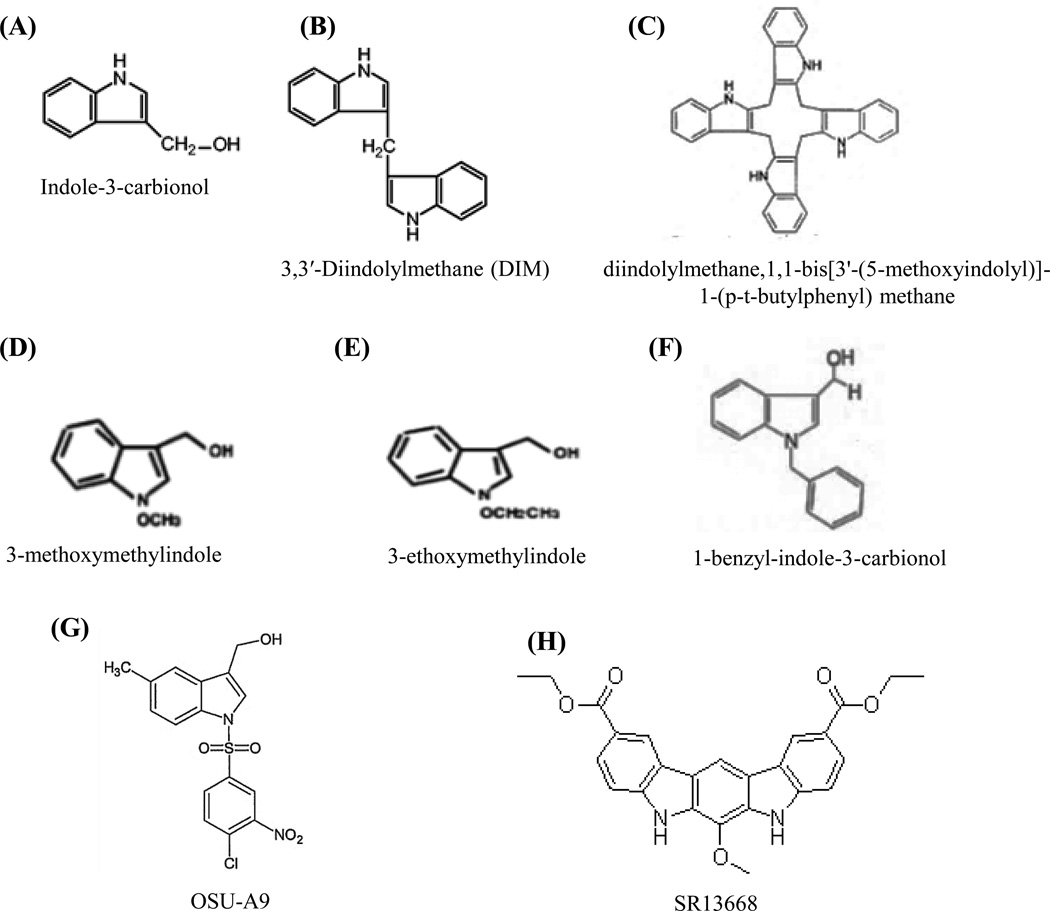
Fig. 11.
Indol-3-carbionol and its structural analogs.
3.10.1 Bioavailability of Indole-3-Carbinol
Consumption of vegetables from the cruciferous family serves as a good source of the I3C precursor, glucobrassicin. Mechanical damage to cells from these plants (e.g., during chewing or chopping) results in the formation of I3C from the interaction between myrosinase and glucobrassicin [186, 323]. After oral ingestion, I3C combines with gastric HCl to form a complex mixture of biologically active compounds such as a 3,3'-diindolylmethane dimer and a cyclic trimer. However, acid condensation products are less likely to form in the more alkaline environment of the intestine. To date, there have been few animal studies investigating the bioavailability of I3C [329, 330]. A phase 1 clinical trial demonstrated undetectable plasma concentrations of I3C in women who received 400 to 1200 mg oral doses. However, DIM levels (Fig. 11B) were detectable with a Cmax of 61 ng/mL and 607 ng/mL after 400 and 1000 mg doses, respectively [329, 330].
3.10.2. Structure Activity Relationship of Indole-3-Carbinol
Due to its significant anti-cancer potential but weak acid stability, several successful attempts have been made to synthesize structural analogs of I3C such as (p-substituted phenyl)-diindoylmethanes peroxisome proliferator-activated receptor γ agonists [331–335], SR13668 (Fig.11H) as an AKT inhibitor [336, 337], and an I3C tetrameric derivative (Fig. 11C) as a CDK6 inhibitor [338]. Acid-catalyzed condensation resistant analog OSU-A9 ([1-(4-chloro-3-nitrobenzenesulfonyl)- 1H-indol-3-yl]-methanol) (Fig. 11G) exhibited significantly improved pro-apoptotic (100-fold higher) and anti-tumor properties than I3C in vitro and in vivo [324, 339]. In addition, I3C-based N-alkoxy derivatives produced a marked increase in cell cycle arrest and apoptosis. Furthermore, the inhibitory potential of 3-methoxymethylindole and 3-ethoxymethylindole (Fig. 11D–E) was similar to I3C. The hydroxymethyl group at the C-3 position of the indole ring is likely important in I3C’s ability to induce cell cycle arrest since substitutions at that position was found to inactivate the compound [340]. Another I3C analog, 1-benzyl-I3C (Fig. 11F), displayed an approximate 1000-fold stronger abilities to inhibit proliferation, induce cell cycle arrest and down-regulate the production of ERα protein in estrogen responsive cancer cells [341].
3.11. Luteolin
Luteolin (Fig. 12A) is a flavanoid found in a wide variety of dietary sources such as carrots, peppers, celery, olives, peppermint, thyme, rosemary, and oregano with known antioxidant, anti-inflammatory, and anti-tumor activities. It has been found to inhibit angiogenesis, promote apoptosis, and sensitize cells to anti-cancer therapy in a variety of malignancies [342]. The compound was found to induce melanogenesis and reduce invasive potential of B16F10 melanoma cells by decreasing EMT through inhibition of the β3 integrin/FAK signal pathway [343–345]. Luteolin protected DNA, inhibited cell cycle progression and promoted apoptosis in A375 melanoma cells in a different investigation [346–348]. In addition, the compound was found to inhibit cell growth and increase apoptosis (B16 and 4A5 melanoma cells) via Bcl-2 downregulation and Bax upregulation [349]. An in vitro study of B16 melanoma cells showed that the flavanoid decreased ERK1/2 signaling [350]. This compound exhibits promising preliminary activity against melanoma, though further investigation will be necessary to confirm its efficacy in the management of the disease.
Fig. 12.
Luteolin and its structural analogs.
3.11.1. Bioavailability of Luteolin
Shimoi et al. [351] observed free luteolin and its conjugates present in plasma after administration of the compound to rats and humans. Plasma concentrations of luteolin and its conjugates peaked between 15 and 30 min after treatment with luteolin. Luteolin was absorbed more rapidly when administered with propyleneglycol versus 0.5% carboxymethyl cellulose. Furthermore, Zohu et al. [306] reported that the absorption rate constant of pure luteolin (5.0 microg/mL) was markedly higher in the duodenum and jejunum than the colon and ileum. Luteolin was likely passively absorbed given that it was taken up in an ATP-independent manner. Furthermore, oral administration in rats resulted a peak concentration and AUC of 1.97 ± 0.15 microg/mL and 10.7 ± 2.2 microg/mL/hr, respectively [306].
3.11.2. Structure Activity Relationship of Luteolin
Though luteolin is known for its antioxidant, anti-inflammatory, and anti-tumor activities, limited studies on its structure-activity relationship have been conducted. In one study, Cheng et al. [352] synthesized luteolin analogs by replacing hydroxy groups at C-3' and C-4' with alkynyl groups using neutral, electron-deficient, electron-rich and heteroaromatic (4-pyridine, imidazole alkynes) at the C-4' position. This luteolin analog LA-12 (Fig. 12B), more efficiently sensitized cells to TNFα-induced cell death than did luteolin.
4. CONCLUSIONS AND FUTURE DIRECTIONS
Melanoma, with its unique ability to metastasize early, is the most deadly skin cancer affecting humans. Patients with metastatic melanoma face a median survival time of only six months and have very few targeted chemotherapies available to them. Although personalized chemotherapies targeting common mutations such as BRAF and MEK have been developed recently, these drugs have only been found to extend progression free survival by a few months. Patients who attempt these treatments frequently develop resistance and succumb to their disease. Recent studies of combination chemotherapies for the prevention and treatment of melanoma give us hope that achieving a cure is indeed possible. If ongoing investigations continue their current trajectory, the anti-cancer properties of phytochemicals may yield complimentary chemotherapies to augment today’s treatments. Accumulating evidence has recently begun to illuminate the various pathways by which these bioactive molecules promote apoptosis, inhibit proliferation and suppress EMT of melanoma cells. By targeting multiple disrupted signaling molecules critical to the pathogenesis of melanoma, phytochemicals such as fisetin, EGCG, silymarin, proanthocyanidin, resveratrol, curcumin, apigenin, capsaicin, lupeol, genistein, indole-3-carbinol and luteolin may one-day serve as necessary adjuvant chemotherapies to successfully treat metastatic melanoma with minimal toxicity. This review highlights the largely untapped anti-cancer potential that phytochemicals possess. The obvious need for effective combination therapies to combat melanoma and the therapeutic promise that phytochemicals offer grant us a glimpse at a cure for melanoma. Ongoing studies are needed to evaluate various combinations of phytochemicals with existing drugs such as BRAF and MEK inhibitors. Numerous combinations of phytochemicals and targeted chemotherapies will need to be evaluated to determine which pairings yield the greatest synergy so that translational studies may then be attempted.
Acknowledgments
This work was supported by NIH Grant 1R21CA173043-01A1 to FA.
LIST OF ABBREVIATIONS
- AP-1
Activator protein-1
- CDKN2A
Cyclin-dependent kinase inhibitor 2A
- COX
Cyclooxygenase
- EMT
Epithelial-mesenchymal transition
- FAK
Focal adhesion kinase
- FLIP
Cellular FLICE-like inhibitory protein
- GSK-3β
Glycogen synthase kinase-3β
- GTP
Guanosine-5-triphosphate
- MAPK
Mitogen-activated protein kinase
- MITF
Microphthalmia-associated transcription factor
- MMP
Matrix metallopeptidase
- mTOR
Mammalian target of rapamycin
- NFκB
Nuclear factor kappa B
- NLRP1
Nuclear localization leucine-rich-repeat protein 1
- PGE2
Prostaglandin E2
- PI3K
Phosphatidylinositol 3-kinase
- PTEN
Phosphatase and tensin homolog
- Rb
Retinoblastoma
- RGP
Radial growth phase
- STAT3
Signal transducer and activator of transcription 3
- VGP
Vertical growth phase
- α-MSH
Alpha-melanocyte-stimulating hormone
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
REFERENCES
- 1.Parra EJ. Human pigmentation variation: evolution, genetic basis, and implications for public health. Am J Phys Anthropol. 2007;(Suppl 45):85–105. doi: 10.1002/ajpa.20727. [DOI] [PubMed] [Google Scholar]
- 2.Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, Coldiron BM. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146(3):283–287. doi: 10.1001/archdermatol.2010.19. [DOI] [PubMed] [Google Scholar]
- 3.Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146(3):279–282. doi: 10.1001/archdermatol.2010.4. [DOI] [PubMed] [Google Scholar]
- 4.Rogers HW, Coldiron BM. Analysis of skin cancer treatment and costs in the United States Medicare population, 1996–2008. Dermatol Surg. 2013;39(1 Pt 1):35–42. doi: 10.1111/dsu.12024. [DOI] [PubMed] [Google Scholar]
- 5.Khavari PA. Modelling cancer in human skin tissue. Nat Rev Cancer. 2006;6(4):270–280. doi: 10.1038/nrc1838. [DOI] [PubMed] [Google Scholar]
- 6.Darr OA, Colacino JA, Tang AL, McHugh JB, Bellile EL, Bradford CR, Prince MP, Chepeha DB, Rozek LS, Moyer JS. Epigenetic alterations in metastatic cutaneous carcinoma. Head Neck. 2014 doi: 10.1002/hed.23701. 10.1002/hed.23701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Houghton AN, Polsky D. Focus on melanoma. Cancer Cell. 2002;2(4):275–278. doi: 10.1016/s1535-6108(02)00161-7. [DOI] [PubMed] [Google Scholar]
- 8.Erdei E, Torres SM. A new understanding in the epidemiology of melanoma. Expert Rev Anticancer Ther. 2010;10(11):1811–1823. doi: 10.1586/era.10.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erdmann F, Lortet-Tieulent J, Schuz J, Zeeb H, Greinert R, Breitbart EW, Bray F. International trends in the incidence of malignant melanoma 1953–2008--are recent generations at higher or lower risk? Int J Cancer. 2013;132(2):385–400. doi: 10.1002/ijc.27616. [DOI] [PubMed] [Google Scholar]
- 10.Ries LAG KM, MD, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, ltekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M. SEER Cancer Statistics Review,1975–2005. [cited 2014];2007 Available from: http://seer.cancer.gov/archive/csr/1975_2005/.
- 11.R L. World Health Organization; 2006. Global Burden of Disease of Solar Ultraviolet Radiation. No. 13. [Google Scholar]
- 12.Ferlay J, S I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman DB. F GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. [cited 2013];2013 [Google Scholar]
- 13.Institute, N.C. SEER Stat Fact Sheets: Melanoma of the Skin. [cited 2014];2014 Available from: http://seer.cancer.gov/statfacts/html/melan.html.
- 14.Society, A.C. Cancer Facts & Figures. [cited 2014];2013 Available from: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf. [Google Scholar]
- 15.DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, Alteri R, Robbins AS, Jemal A. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64(4):252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 16.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 17.Clark WH. Tumour progression and the nature of cancer. Br J Cancer. 1991;64(4):631–644. doi: 10.1038/bjc.1991.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark WH., Jr Human cutaneous malignant melanoma as a model for cancer. Cancer Metastasis Rev. 1991;10(2):83–88. doi: 10.1007/BF00049406. [DOI] [PubMed] [Google Scholar]
- 19.D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV Radiation and the Skin. Int J Mol Sci. 2013;14(6):12222–12248. doi: 10.3390/ijms140612222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoerter JD, Bradley P, Casillas A, Chambers D, Denholm C, Johnson K, Weiswasser B. Extrafollicular dermal melanocyte stem cells and melanoma. Stem Cells Int. 2012;2012:407079. doi: 10.1155/2012/407079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bohm M, Schulte U, Funk JO, Raghunath M, Behrmann I, Kortylewski M, Heinrich PC, Kues T, Luger TA, Schwarz T. Interleukin-6-resistant melanoma cells exhibit reduced activation of STAT3 and lack of inhibition of cyclin E-associated kinase activity. J Invest Dermatol. 2001;117(1):132–140. doi: 10.1046/j.0022-202x.2001.01372.x. [DOI] [PubMed] [Google Scholar]
- 22.Holzel M, Bovier A, Tuting T. Plasticity of tumour and immune cells: a source of heterogeneity and a cause for therapy resistance? Nat Rev Cancer. 2013;13(5):365–376. doi: 10.1038/nrc3498. [DOI] [PubMed] [Google Scholar]
- 23.Briggs JC. Histological diagnosis and prognosis of malignant melanoma. J Clin Pathol. 1980;33(7):702. doi: 10.1136/jcp.33.7.702-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levene A. On the histological diagnosis and prognosis of malignant melanoma. J Clin Pathol. 1980;33(2):101–124. doi: 10.1136/jcp.33.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGovern VJ. The nature of melanoma. A critical review. J Cutan Pathol. 1982;9(2):61–81. doi: 10.1111/j.1600-0560.1982.tb01044.x. [DOI] [PubMed] [Google Scholar]
- 26.Metcalf JS. Melanoma: criteria for histological diagnosis and its reporting. Semin Oncol. 1996;23(6):688–692. [PubMed] [Google Scholar]
- 27.Smoller BR. Histologic criteria for diagnosing primary cutaneous malignant melanoma. Mod Pathol. 2006;19(Suppl 2):S34–S40. doi: 10.1038/modpathol.3800508. [DOI] [PubMed] [Google Scholar]
- 28.Taran JM, Heenan PJ. Clinical and histologic features of level 2 cutaneous malignant melanoma associated with metastasis. Cancer. 2001;91(9):1822–1825. doi: 10.1002/1097-0142(20010501)91:9<1822::aid-cncr1202>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 29.Kiene P, Petres-Dunsche C, Folster-Holst R. Pigmented pedunculated malignant melanoma. A rare variant of nodular melanoma. Br J Dermatol. 1995;133(2):300–302. doi: 10.1111/j.1365-2133.1995.tb02633.x. [DOI] [PubMed] [Google Scholar]
- 30.Plotnick H, Rachmaninoff N, VandenBerg HJ., Jr Polypoid melanoma: a virulent variant of nodular melanoma. Report of three cases and literature review. J Am Acad Dermatol. 1990;23(5 Pt 1):880–884. doi: 10.1016/0190-9622(90)70309-6. [DOI] [PubMed] [Google Scholar]
- 31.Cohen LM. Lentigo maligna and lentigo maligna melanoma. J Am Acad Dermatol. 1997;36(6 Pt 1):913. [PubMed] [Google Scholar]
- 32.Kroumpouzos G, Frank EW, Albertini JG, Krivo JM, Ramsey ML, Tyler WB, Cohen LM. Lentigo maligna with spread onto oral mucosa. Arch Dermatol. 2002;138(9):1216–1220. doi: 10.1001/archderm.138.9.1216. [DOI] [PubMed] [Google Scholar]
- 33.Chen YJ, Wu CY, Chen JT, Shen JL, Chen CC, Wang HC. Clinicopathologic analysis of malignant melanoma in Taiwan. J Am Acad Dermatol. 1999;41(6):945–949. doi: 10.1016/s0190-9622(99)70251-3. [DOI] [PubMed] [Google Scholar]
- 34.King R. Lentiginous melanoma. Arch Pathol Lab Med. 2011;135(3):337–341. doi: 10.5858/2009-0538-RA.1. [DOI] [PubMed] [Google Scholar]
- 35.King R, Page RN, Googe PB, Mihm MC., Jr Lentiginous melanoma: a histologic pattern of melanoma to be distinguished from lentiginous nevus. Mod Pathol. 2005;18(10):1397–1401. doi: 10.1038/modpathol.3800454. [DOI] [PubMed] [Google Scholar]
- 36.Keir J. Dermatoscopic features of cutaneous non-facial non-acral lentiginous growth pattern melanomas. Dermatol Pract Concept. 2014;4(1):77–82. doi: 10.5826/dpc.0401a13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yonekawa Y, Kim IK, Gragoudas ES, Njauw CN, Tsao H, Jakobiec FA, Stacy RC. Aggressive skull base metastasis from uveal melanoma: a clinicopathologic study. Eur J Ophthalmol. 2014;24(5):811–813. doi: 10.5301/ejo.5000468. [DOI] [PubMed] [Google Scholar]
- 38.Seetharamu N, Ott PA, Pavlick AC. Mucosal melanomas: a case-based review of the literature. Oncologist. 2010;15(7):772–781. doi: 10.1634/theoncologist.2010-0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dhomen N, Reis-Filho JS, da Rocha Dias S, Hayward R, Savage K, Delmas V, Larue L, Pritchard C, Marais R. Oncogenic Braf induces melanocyte senescence and melanoma in mice. Cancer Cell. 2009;15(4):294–303. doi: 10.1016/j.ccr.2009.02.022. [DOI] [PubMed] [Google Scholar]
- 40.Holderfield M, Deuker MM, McCormick F, McMahon M. Targeting RAF kinases for cancer therapy: BRAF-mutated melanoma and beyond. Nat Rev Cancer. 2014;14(7):455–467. doi: 10.1038/nrc3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wellbrock C, Karasarides M, Marais R. The RAF proteins take centre stage. Nat Rev Mol Cell Biol. 2004;5(11):875–885. doi: 10.1038/nrm1498. [DOI] [PubMed] [Google Scholar]
- 42.Dumaz N, Hayward R, Martin J, Ogilvie L, Hedley D, Curtin JA, Bastian BC, Springer C, Marais R. In melanoma, RAS mutations are accompanied by switching signaling from BRAF to CRAF and disrupted cyclic AMP signaling. Cancer Res. 2006;66(19):9483–9491. doi: 10.1158/0008-5472.CAN-05-4227. [DOI] [PubMed] [Google Scholar]
- 43.Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, Davis N, Dicks E, Ewing R, Floyd Y, Gray K, Hall S, Hawes R, Hughes J, Kosmidou V, Menzies A, Mould C, Parker A, Stevens C, Watt S, Hooper S, Wilson R, Jayatilake H, Gusterson BA, Cooper C, Shipley J, Hargrave D, Pritchard-Jones K, Maitland N, Chenevix-Trench G, Riggins GJ, Bigner DD, Palmieri G, Cossu A, Flanagan A, Nicholson A, Ho JW, Leung SY, Yuen ST, Weber BL, Seigler HF, Darrow TL, Paterson H, Marais R, Marshall CJ, Wooster R, Stratton MR, Futreal PA. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–954. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 44.Long GV, Menzies AM, Nagrial AM, Haydu LE, Hamilton AL, Mann GJ, Hughes TM, Thompson JF, Scolyer RA, Kefford RF. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29(10):1239–1246. doi: 10.1200/JCO.2010.32.4327. [DOI] [PubMed] [Google Scholar]
- 45.Gray-Schopfer V, Wellbrock C, Marais R. Melanoma biology and new targeted therapy. Nature. 2007;445(7130):851–857. doi: 10.1038/nature05661. [DOI] [PubMed] [Google Scholar]
- 46.Wan PT, Garnett MJ, Roe SM, Lee S, Niculescu-Duvaz D, Good VM, Jones CM, Marshall CJ, Springer CJ, Barford D, Marais R. Mechanism of activation of the RAF-ERK signaling pathway by oncogenic mutations of B-RAF. Cell. 2004;116(6):855–867. doi: 10.1016/s0092-8674(04)00215-6. [DOI] [PubMed] [Google Scholar]
- 47.Dhomen N, Marais R. New insight into BRAF mutations in cancer. Curr Opin Genet Dev. 2007;17(1):31–39. doi: 10.1016/j.gde.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 48.Sumimoto H, Imabayashi F, Iwata T, Kawakami Y. The BRAF-MAPK signaling pathway is essential for cancer-immune evasion in human melanoma cells. J Exp Med. 2006;203(7):1651–1656. doi: 10.1084/jem.20051848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ackermann J, Frutschi M, Kaloulis K, McKee T, Trumpp A, Beermann F. Metastasizing melanoma formation caused by expression of activated N-RasQ61K on an INK4a-deficient background. Cancer Res. 2005;65(10):4005–4011. doi: 10.1158/0008-5472.CAN-04-2970. [DOI] [PubMed] [Google Scholar]
- 50.Rebecca VW, Alicea GM, Paraiso KH, Lawrence H, Gibney GT, Smalley KS. Vertical inhibition of the MAPK pathway enhances therapeutic responses in NRAS-mutant melanoma. Pigment Cell Melanoma Res. 2014 doi: 10.1111/pcmr.12303. 10.1111/pcmr.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sensi M, Nicolini G, Petti C, Bersani I, Lozupone F, Molla A, Vegetti C, Nonaka D, Mortarini R, Parmiani G, Fais S, Anichini A. Mutually exclusive NRASQ61R and BRAFV600E mutations at the single-cell level in the same human melanoma. Oncogene. 2006;25(24):3357–3364. doi: 10.1038/sj.onc.1209379. [DOI] [PubMed] [Google Scholar]
- 52.Greene VR, Johnson MM, Grimm EA, Ellerhorst JA. Frequencies of NRAS and BRAF mutations increase from the radial to the vertical growth phase in cutaneous melanoma. J Invest Dermatol. 2009;129(6):1483–1488. doi: 10.1038/jid.2008.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Burotto M, Chiou VL, Lee JM, Kohn EC. The MAPK pathway across different malignancies: A new perspective. Cancer. 2014 doi: 10.1002/cncr.28864. 10.1002/cncr.28864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Platz A, Egyhazi S, Ringborg U, Hansson J. Human cutaneous melanoma; a review of NRAS and BRAF mutation frequencies in relation to histogenetic subclass and body site. Mol Oncol. 2008;1(4):395–405. doi: 10.1016/j.molonc.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Posch C, Moslehi H, Feeney L, Green GA, Ebaee A, Feichtenschlager V, Chong K, Peng L, Dimon MT, Phillips T, Daud AI, McCalmont TH, LeBoit PE, Ortiz-Urda S. Combined targeting of MEK and PI3K/mTOR effector pathways is necessary to effectively inhibit NRAS mutant melanoma in vitro and in vivo. Proc Natl Acad Sci U S A. 2013;110(10):4015–4020. doi: 10.1073/pnas.1216013110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hatzivassiliou G, Song K, Yen I, Brandhuber BJ, Anderson DJ, Alvarado R, Ludlam MJ, Stokoe D, Gloor SL, Vigers G, Morales T, Aliagas I, Liu B, Sideris S, Hoeflich KP, Jaiswal BS, Seshagiri S, Koeppen H, Belvin M, Friedman LS, Malek S. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature. 2010;464(7287):431–435. doi: 10.1038/nature08833. [DOI] [PubMed] [Google Scholar]
- 57.Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, Chen Z, Lee MK, Attar N, Sazegar H, Chodon T, Nelson SF, McArthur G, Sosman JA, Ribas A, Lo RS. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 2010;468(7326):973–977. doi: 10.1038/nature09626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lidsky M, Antoun G, Speicher P, Adams B, Turley R, Augustine C, Tyler D, Ali-Osman F. MAP kinase hyper-activation and enhanced NRAS expression drive acquired vemurafenib resistance in V600E BRAF melanoma cells. J Biol Chem. 2014 doi: 10.1074/jbc.M113.532432. 10.1074/jbc.M113.532432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Omholt K, Platz A, Kanter L, Ringborg U, Hansson J. NRAS and BRAF mutations arise early during melanoma pathogenesis and are preserved throughout tumor progression. Clin Cancer Res. 2003;9(17):6483–6488. [PubMed] [Google Scholar]
- 60.Wong AK, Chin L. An inducible melanoma model implicates a role for RAS in tumor maintenance and angiogenesis. Cancer Metastasis Rev. 2000;19(1–2):121–129. doi: 10.1023/a:1026537423753. [DOI] [PubMed] [Google Scholar]
- 61.Masaki T, Wang Y, DiGiovanna JJ, Khan SG, Raffeld M, Beltaifa S, Hornyak TJ, Darling TN, Lee CC, Kraemer KH. High frequency of PTEN mutations in nevi and melanomas from xeroderma pigmentosum patients. Pigment Cell Melanoma Res. 2014;27(3):454–464. doi: 10.1111/pcmr.12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shull AY, Latham-Schwark A, Ramasamy P, Leskoske K, Oroian D, Birtwistle MR, Buckhaults PJ. Novel somatic mutations to PI3K pathway genes in metastatic melanoma. PLoS One. 2012;7(8):e43369. doi: 10.1371/journal.pone.0043369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tsao H, Chin L, Garraway LA, Fisher DE. Melanoma: from mutations to medicine. Genes Dev. 2012;26(11):1131–1155. doi: 10.1101/gad.191999.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dankort D, Curley DP, Cartlidge RA, Nelson B, Karnezis AN, Damsky WE, Jr, You MJ, DePinho RA, McMahon M, Bosenberg M. Braf(V600E) cooperates with Pten loss to induce metastatic melanoma. Nat Genet. 2009;41(5):544–552. doi: 10.1038/ng.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goel VK, Lazar AJ, Warneke CL, Redston MS, Haluska FG. Examination of mutations in BRAF, NRAS, and PTEN in primary cutaneous melanoma. J Invest Dermatol. 2006;126(1):154–160. doi: 10.1038/sj.jid.5700026. [DOI] [PubMed] [Google Scholar]
- 66.Nogueira C, Kim KH, Sung H, Paraiso KH, Dannenberg JH, Bosenberg M, Chin L, Kim M. Cooperative interactions of PTEN deficiency and RAS activation in melanoma metastasis. Oncogene. 2010;29(47):6222–6232. doi: 10.1038/onc.2010.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Marsh Durban V, Deuker MM, Bosenberg MW, Phillips W, McMahon M. Differential AKT dependency displayed by mouse models of BRAFV600E-initiated melanoma. J Clin Invest. 2013;123(12):5104–5118. doi: 10.1172/JCI69619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Silva JM, Bulman C, McMahon M. BRAFV600E cooperates with PI3K signaling, independent of AKT, to regulate melanoma cell proliferation. Mol Cancer Res. 2014;12(3):447–463. doi: 10.1158/1541-7786.MCR-13-0224-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vredeveld LC, Possik PA, Smit MA, Meissl K, Michaloglou C, Horlings HM, Ajouaou A, Kortman PC, Dankort D, McMahon M, Mooi WJ, Peeper DS. Abrogation of BRAFV600E-induced senescence by PI3K pathway activation contributes to melanomagenesis. Genes Dev. 2012;26(10):1055–1069. doi: 10.1101/gad.187252.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Benjamin CL, Melnikova VO, Ananthaswamy HN. P53 protein and pathogenesis of melanoma and nonmelanoma skin cancer. Adv Exp Med Biol. 2008;624:265–282. doi: 10.1007/978-0-387-77574-6_21. [DOI] [PubMed] [Google Scholar]
- 71.Sarasin A, Dessen P. DNA repair pathways and human metastatic malignant melanoma. Curr Mol Med. 2010;10(4):413–418. doi: 10.2174/156652410791317011. [DOI] [PubMed] [Google Scholar]
- 72.Jochemsen AG. Reactivation of p53 as therapeutic intervention for malignant melanoma. Curr Opin Oncol. 2014;26(1):114–119. doi: 10.1097/CCO.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 73.Ji Z, Njauw CN, Taylor M, Neel V, Flaherty KT, Tsao H. p53 rescue through HDM2 antagonism suppresses melanoma growth and potentiates MEK inhibition. J Invest Dermatol. 2012;132(2):356–364. doi: 10.1038/jid.2011.313. [DOI] [PubMed] [Google Scholar]
- 74.Lu M, Miller P, Lu X. Restoring the tumour suppressive function of p53 as a parallel strategy in melanoma therapy. FEBS Lett. 2014;588(16):2616–2621. doi: 10.1016/j.febslet.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 75.Hocker T, Tsao H. Ultraviolet radiation and melanoma: a systematic review and analysis of reported sequence variants. Hum Mutat. 2007;28(6):578–588. doi: 10.1002/humu.20481. [DOI] [PubMed] [Google Scholar]
- 76.Rass K, Reichrath J. UV damage and DNA repair in malignant melanoma and nonmelanoma skin cancer. Adv Exp Med Biol. 2008;624:162–178. doi: 10.1007/978-0-387-77574-6_13. [DOI] [PubMed] [Google Scholar]
- 77.von Thaler AK, Kamenisch Y, Berneburg M. The role of ultraviolet radiation in melanomagenesis. Exp Dermatol. 2010;19(2):81–88. doi: 10.1111/j.1600-0625.2009.01025.x. [DOI] [PubMed] [Google Scholar]
- 78.Dovey M, White RM, Zon LI. Oncogenic NRAS cooperates with p53 loss to generate melanoma in zebrafish. Zebrafish. 2009;6(4):397–404. doi: 10.1089/zeb.2009.0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shields JM, Thomas NE, Cregger M, Berger AJ, Leslie M, Torrice C, Hao H, Penland S, Arbiser J, Scott G, Zhou T, Bar-Eli M, Bear JE, Der CJ, Kaufmann WK, Rimm DL, Sharpless NE. Lack of extracellular signal-regulated kinase mitogen-activated protein kinase signaling shows a new type of melanoma. Cancer Res. 2007;67(4):1502–1512. doi: 10.1158/0008-5472.CAN-06-3311. [DOI] [PubMed] [Google Scholar]
- 80.Box NF, Terzian T. The role of p53 in pigmentation, tanning and melanoma. Pigment Cell Melanoma Res. 2008;21(5):525–533. doi: 10.1111/j.1755-148X.2008.00495.x. [DOI] [PubMed] [Google Scholar]
- 81.Yu H, McDaid R, Lee J, Possik P, Li L, Kumar SM, Elder DE, Van Belle P, Gimotty P, Guerra M, Hammond R, Nathanson KL, Dalla Palma M, Herlyn M, Xu X. The role of BRAF mutation and p53 inactivation during transformation of a subpopulation of primary human melanocytes. Am J Pathol. 2009;174(6):2367–2377. doi: 10.2353/ajpath.2009.081057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Anwar A, Norris DA, Fujita M. Ubiquitin proteasomal pathway mediated degradation of p53 in melanoma. Arch Biochem Biophys. 2011;508(2):198–203. doi: 10.1016/j.abb.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Avery-Kiejda KA, Bowden NA, Croft AJ, Scurr LL, Kairupan CF, Ashton KA, Talseth-Palmer BA, Rizos H, Zhang XD, Scott RJ, Hersey P. P53 in human melanoma fails to regulate target genes associated with apoptosis and the cell cycle and may contribute to proliferation. BMC Cancer. 2011;11:203. doi: 10.1186/1471-2407-11-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Castellano M, Parmiani G. Genes involved in melanoma: an overview of INK4a and other loci. Melanoma Res. 1999;9(5):421–432. [PubMed] [Google Scholar]
- 85.Tsao H, Benoit E, Sober AJ, Thiele C, Haluska FG. Novel mutations in the p16/CDKN2A binding region of the cyclin-dependent kinase-4 gene. Cancer Res. 1998;58(1):109–113. [PubMed] [Google Scholar]
- 86.Law MH, Macgregor S, Hayward NK. Melanoma genetics: recent findings take us beyond well-traveled pathways. J Invest Dermatol. 2012;132(7):1763–1774. doi: 10.1038/jid.2012.75. [DOI] [PubMed] [Google Scholar]
- 87.Ha L, Merlino G, Sviderskaya EV. Melanomagenesis: overcoming the barrier of melanocyte senescence. Cell Cycle. 2008;7(13):1944–1948. doi: 10.4161/cc.7.13.6230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sharpless E, Chin L. The INK4a/ARF locus and melanoma. Oncogene. 2003;22(20):3092–3098. doi: 10.1038/sj.onc.1206461. [DOI] [PubMed] [Google Scholar]
- 89.Ward KA, Lazovich D, Hordinsky MK. Germline melanoma susceptibility and prognostic genes: a review of the literature. J Am Acad Dermatol. 2012;67(5):1055–1067. doi: 10.1016/j.jaad.2012.02.042. [DOI] [PubMed] [Google Scholar]
- 90.Hodis E, Watson IR, Kryukov GV, Arold ST, Imielinski M, Theurillat JP, Nickerson E, Auclair D, Li L, Place C, Dicara D, Ramos AH, Lawrence MS, Cibulskis K, Sivachenko A, Voet D, Saksena G, Stransky N, Onofrio RC, Winckler W, Ardlie K, Wagle N, Wargo J, Chong K, Morton DL, Stemke-Hale K, Chen G, Noble M, Meyerson M, Ladbury JE, Davies MA, Gershenwald JE, Wagner SN, Hoon DS, Schadendorf D, Lander ES, Gabriel SB, Getz G, Garraway LA, Chin L. A landscape of driver mutations in melanoma. Cell. 2012;150(2):251–263. doi: 10.1016/j.cell.2012.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jovanovic B, Egyhazi S, Eskandarpour M, Ghiorzo P, Palmer JM, Bianchi Scarra G, Hayward NK, Hansson J. Coexisting NRAS and BRAF mutations in primary familial melanomas with specific CDKN2A germline alterations. J Invest Dermatol. 2010;130(2):618–620. doi: 10.1038/jid.2009.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Walker GJ, Flores JF, Glendening JM, Lin AH, Markl ID, Fountain JW. Virtually 100% of melanoma cell lines harbor alterations at the DNA level within CDKN2A, CDKN2B, or one of their downstream targets. Genes Chromosomes Cancer. 1998;22(2):157–163. doi: 10.1002/(sici)1098-2264(199806)22:2<157::aid-gcc11>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 93.Hansson J. Familial cutaneous melanoma. Adv Exp Med Biol. 2010;685:134–145. doi: 10.1007/978-1-4419-6448-9_13. [DOI] [PubMed] [Google Scholar]
- 94.Yakobson E, Shemesh P, Azizi E, Winkler E, Lassam N, Hogg D, Brookes S, Peters G, Lotem M, Zlotogorski A, Landau M, Safro M, Shafir R, Friedman E, Peretz H. Two p16 (CDKN2A) germline mutations in 30 Israeli melanoma families. Eur J Hum Genet. 2000;8(8):590–596. doi: 10.1038/sj.ejhg.5200505. [DOI] [PubMed] [Google Scholar]
- 95.Taber JM, Aspinwall LG, Kohlmann W, Dow R, Leachman SA. Parental preferences for CDKN2A/p16 testing of minors. Genet Med. 2010;12(12):823–838. doi: 10.1097/GIM.0b013e3181f87278. [DOI] [PubMed] [Google Scholar]
- 96.Aspinwall LG, Leaf SL, Dola ER, Kohlmann W, Leachman SA. CDKN2A/p16 genetic test reporting improves early detection intentions and practices in high-risk melanoma families. Cancer Epidemiol Biomarkers Prev. 2008;17(6):1510–1519. doi: 10.1158/1055-9965.EPI-08-0010. [DOI] [PubMed] [Google Scholar]
- 97.Mehnert JM, Kluger HM. Driver mutations in melanoma: lessons learned from bench-to-bedside studies. Curr Oncol Rep. 2012;14(5):449–457. doi: 10.1007/s11912-012-0249-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sheppard KE, McArthur GA. The cell-cycle regulator CDK4: an emerging therapeutic target in melanoma. Clin Cancer Res. 2013;19(19):5320–5328. doi: 10.1158/1078-0432.CCR-13-0259. [DOI] [PubMed] [Google Scholar]
- 99.McNeal AS, Liu K, Nakhate V, Natale CA, Duperret EK, Capell BC, Dentchev T, Berger SL, Herlyn M, Seykora JT, Ridky TW. CDKN2B Loss Promotes Progression from Benign Melanocytic Nevus to Melanoma. Cancer Discov. 2015;5(10):1072–1085. doi: 10.1158/2159-8290.CD-15-0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Afaq F, Katiyar SK. Polyphenols: skin photoprotection and inhibition of photocarcinogenesis. Mini Rev Med Chem. 2011;11(14):1200–1215. doi: 10.2174/13895575111091200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sun Q, Prasad R, Rosenthal E, Katiyar SK. Grape seed proanthocyanidins inhibit the invasive potential of head and neck cutaneous squamous cell carcinoma cells by targeting EGFR expression and epithelial-to-mesenchymal transition. BMC Complement Altern Med. 2011;11:134. doi: 10.1186/1472-6882-11-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vaid M, Prasad R, Sun Q, Katiyar SK. Silymarin targets beta-catenin signaling in blocking migration/invasion of human melanoma cells. PLoS One. 2011;6(7):e23000. doi: 10.1371/journal.pone.0023000. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 103.Strickland LR, Pal HC, Elmets CA, Afaq F. Targeting drivers of melanoma with synthetic small molecules and phytochemicals. Cancer Lett. 2015;359(1):20–35. doi: 10.1016/j.canlet.2015.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Arai Y, Watanabe S, Kimira M, Shimoi K, Mochizuki R, Kinae N. Dietary intakes of flavonols, flavones and isoflavones by Japanese women and the inverse correlation between quercetin intake and plasma LDL cholesterol concentration. J Nutr. 2000;130(9):2243–2250. doi: 10.1093/jn/130.9.2243. [DOI] [PubMed] [Google Scholar]
- 105.Kimira M, Arai Y, Shimoi K, Watanabe S. Japanese intake of flavonoids and isoflavonoids from foods. J Epidemiol. 1998;8(3):168–175. doi: 10.2188/jea.8.168. [DOI] [PubMed] [Google Scholar]
- 106.Pal HC, Baxter RD, Hunt KM, Agarwal J, Elmets CA, Athar M, Afaq F. Fisetin, a phytochemical, potentiates sorafenib-induced apoptosis and abrogates tumor growth in athymic nude mice implanted with BRAF-mutated melanoma cells. Oncotarget. 2015;6(29):28296–28311. doi: 10.18632/oncotarget.5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pal HC, Sharma S, Elmets CA, Athar M, Afaq F. Fisetin inhibits growth, induces G(2) /M arrest and apoptosis of human epidermoid carcinoma A431 cells: role of mitochondrial membrane potential disruption and consequent caspases activation. Exp Dermatol. 2013;22(7):470–475. doi: 10.1111/exd.12181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pal HC, Sharma S, Strickland LR, Katiyar SK, Ballestas ME, Athar M, Elmets CA, Afaq F. Fisetin inhibits human melanoma cell invasion through promotion of mesenchymal to epithelial transition and by targeting MAPK and NFkappaB signaling pathways. PLoS One. 2014;9(1):e86338. doi: 10.1371/journal.pone.0086338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pal HC, Athar M, Elmets CA, Afaq F. Fisetin inhibits UVB-induced cutaneous inflammation and activation of PI3K/AKT/ NFkappaB signaling pathways in SKH-1 hairless mice. Photochem Photobiol. 2014 doi: 10.1111/php.12337. 10.1111/php.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pal HC, Diamond AC, Strickland LR, Kappes JC, Katiyar SK, Elmets CA, Athar M, Afaq F. Fisetin, a dietary flavonoid, augments the anti-invasive and anti-metastatic potential of sorafenib in melanoma. Oncotarget. 2016;7(2):1227–1241. doi: 10.18632/oncotarget.6237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Syed DN, Afaq F, Maddodi N, Johnson JJ, Sarfaraz S, Ahmad A, Setaluri V, Mukhtar H. Inhibition of human melanoma cell growth by the dietary flavonoid fisetin is associated with disruption of Wnt/beta-catenin signaling and decreased Mitf levels. J Invest Dermatol. 2011;131(6):1291–1299. doi: 10.1038/jid.2011.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Syed DN, Chamcheu JC, Khan MI, Sechi M, Lall RK, Adhami VM, Mukhtar H. Fisetin inhibits human melanoma cell growth through direct binding to p70S6K and mTOR: findings from 3-D melanoma skin equivalents and computational modeling. Biochem Pharmacol. 2014;89(3):349–360. doi: 10.1016/j.bcp.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ragelle H, Crauste-Manciet S, Seguin J, Brossard D, Scherman D, Arnaud P, Chabot GG. Nanoemulsion formulation of fisetin improves bioavailability and antitumour activity in mice. Int J Pharm. 2012;427(2):452–459. doi: 10.1016/j.ijpharm.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 114.Touil YS, Seguin J, Scherman D, Chabot GG. Improved antiangiogenic and antitumour activity of the combination of the natural flavonoid fisetin and cyclophosphamide in Lewis lung carcinoma-bearing mice. Cancer Chemother Pharmacol. 2011;68(2):445–455. doi: 10.1007/s00280-010-1505-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bothiraja C, Yojana BD, Pawar AP, Shaikh KS, Thorat UH. Fisetin-loaded nanocochleates: formulation, characterisation, in vitro anticancer testing, bioavailability and biodistribution study. Expert Opin Drug Deliv. 2014;11(1):17–29. doi: 10.1517/17425247.2013.860131. [DOI] [PubMed] [Google Scholar]
- 116.Seguin J, Brulle L, Boyer R, Lu YM, Ramos Romano M, Touil YS, Scherman D, Bessodes M, Mignet N, Chabot GG. Liposomal encapsulation of the natural flavonoid fisetin improves bioavailability and antitumor efficacy. Int J Pharm. 2013;444(1–2):146–154. doi: 10.1016/j.ijpharm.2013.01.050. [DOI] [PubMed] [Google Scholar]
- 117.Shia CS, Tsai SY, Kuo SC, Hou YC, Chao PD. Metabolism and pharmacokinetics of 3,3',4',7-tetrahydroxyflavone (fisetin), 5-hydroxyflavone, and 7-hydroxyflavone and antihemolysis effects of fisetin and its serum metabolites. J Agric Food Chem. 2009;57(1):83–89. doi: 10.1021/jf802378q. [DOI] [PubMed] [Google Scholar]
- 118.Ichimatsu D, Nomura M, Nakamura S, Moritani S, Yokogawa K, Kobayashi S, Nishioka T, Miyamoto K. Structure-activity relationship of flavonoids for inhibition of epidermal growth factor-induced transformation of JB6 Cl 41 cells. Mol Carcinog. 2007;46(6):436–445. doi: 10.1002/mc.20292. [DOI] [PubMed] [Google Scholar]
- 119.Sagara Y, Vanhnasy J, Maher P. Induction of PC12 cell differentiation by flavonoids is dependent upon extracellular signal-regulated kinase activation. J Neurochem. 2004;90(5):1144–1155. doi: 10.1111/j.1471-4159.2004.02563.x. [DOI] [PubMed] [Google Scholar]
- 120.Akaishi T, Morimoto T, Shibao M, Watanabe S, Sakai-Kato K, Utsunomiya-Tate N, Abe K. Structural requirements for the flavonoid fisetin in inhibiting fibril formation of amyloid beta protein. Neurosci Lett. 2008;444(3):280–285. doi: 10.1016/j.neulet.2008.08.052. [DOI] [PubMed] [Google Scholar]
- 121.Katiyar S, Elmets CA, Katiyar SK. Green tea and skin cancer: photoimmunology, angiogenesis and DNA repair. J Nutr Biochem. 2007;18(5):287–296. doi: 10.1016/j.jnutbio.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 122.Katiyar SK, Afaq F, Perez A, Mukhtar H. Green tea polyphenol (−)-epigallocatechin-3-gallate treatment of human skin inhibits ultraviolet radiation-induced oxidative stress. Carcinogenesis. 2001;22(2):287–294. doi: 10.1093/carcin/22.2.287. [DOI] [PubMed] [Google Scholar]
- 123.Nandakumar V, Vaid M, Katiyar SK. (−)-Epigallocatechin-3-gallate reactivates silenced tumor suppressor genes, Cip1/p21 and p16INK4a, by reducing DNA methylation and increasing histones acetylation in human skin cancer cells. Carcinogenesis. 2011;32(4):537–544. doi: 10.1093/carcin/bgq285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ravindranath MH, Ramasamy V, Moon S, Ruiz C, Muthugounder S. Differential growth suppression of human melanoma cells by tea (Camellia sinensis) epicatechins (ECG, EGC and EGCG) Evid Based Complement Alternat Med. 2009;6(4):523–530. doi: 10.1093/ecam/nem140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nihal M, Ahsan H, Siddiqui IA, Mukhtar H, Ahmad N, Wood GS. (−)-Epigallocatechin-3-gallate (EGCG) sensitizes melanoma cells to interferon induced growth inhibition in a mouse model of human melanoma. Cell Cycle. 2009;8(13):2057–2063. doi: 10.4161/cc.8.13.8862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Nihal M, Roelke CT, Wood GS. Anti-melanoma effects of vorinostat in combination with polyphenolic antioxidant (−)-epigallocatechin-3-gallate (EGCG) Pharm Res. 2010;27(6):1103–1114. doi: 10.1007/s11095-010-0054-5. [DOI] [PubMed] [Google Scholar]
- 127.Ellis LZ, Liu W, Luo Y, Okamoto M, Qu D, Dunn JH, Fujita M. Green tea polyphenol epigallocatechin-3-gallate suppresses melanoma growth by inhibiting inflammasome and IL-1beta secretion. Biochem Biophys Res Commun. 2011;414(3):551–556. doi: 10.1016/j.bbrc.2011.09.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ahmed S, Rahman A, Hasnain A, Lalonde M, Goldberg VM, Haqqi TM. Green tea polyphenol epigallocatechin-3-gallate inhibits the IL-1 beta-induced activity and expression of cyclooxygenase-2 and nitric oxide synthase-2 in human chondrocytes. Free Radic Biol Med. 2002;33(8):1097–1105. doi: 10.1016/s0891-5849(02)01004-3. [DOI] [PubMed] [Google Scholar]
- 129.Shin HY, Kim SH, Jeong HJ, Kim SY, Shin TY, Um JY, Hong SH, Kim HM. Epigallocatechin-3-gallate inhibits secretion of TNF-alpha, IL-6 and IL-8 through the attenuation of ERK and NF-kappaB in HMC-1 cells. Int Arch Allergy Immunol. 2007;142(4):335–344. doi: 10.1159/000097503. [DOI] [PubMed] [Google Scholar]
- 130.Singh T, Katiyar SK. Green tea catechins reduce invasive potential of human melanoma cells by targeting COX-2, PGE2 receptors and epithelial-to-mesenchymal transition. PLoS One. 2011;6(10):e25224. doi: 10.1371/journal.pone.0025224. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 131.Chen L, Lee MJ, Li H, Yang CS. Absorption, distribution, elimination of tea polyphenols in rats. Drug Metab Dispos. 1997;25(9):1045–1050. [PubMed] [Google Scholar]
- 132.Langley-Evans SC. Consumption of black tea elicits an increase in plasma antioxidant potential in humans. Int J Food Sci Nutr. 2000;51(5):309–315. doi: 10.1080/096374800426902. [DOI] [PubMed] [Google Scholar]
- 133.Yashin A, N B, Yashin Y. Bioavailability of Tea Components. Journal of Food Research. 2012;1(2):281–290. [Google Scholar]
- 134.Lambert JD, Lee MJ, Lu H, Meng X, Hong JJ, Seril DN, Sturgill MG, Yang CS. Epigallocatechin-3-gallate is absorbed but extensively glucuronidated following oral administration to mice. J Nutr. 2003;133(12):4172–4177. doi: 10.1093/jn/133.12.4172. [DOI] [PubMed] [Google Scholar]
- 135.Lee MJ, Maliakal P, Chen L, Meng X, Bondoc FY, Prabhu S, Lambert G, Mohr S, Yang CS. Pharmacokinetics of tea catechins after ingestion of green tea and (−)-epigallocatechin-3-gallate by humans: formation of different metabolites and individual variability. Cancer Epidemiol Biomarkers Prev. 2002;11(10 Pt 1):1025–1032. [PubMed] [Google Scholar]
- 136.Kale A, Gawande S, Kotwal S, Netke S, Roomi W, Ivanov V, Niedzwiecki A, Rath M. Studies on the effects of oral administration of nutrient mixture, quercetin and red onions on the bioavailability of epigallocatechin gallate from green tea extract. Phytother Res. 2010;24(Suppl 1):S48–S55. doi: 10.1002/ptr.2899. [DOI] [PubMed] [Google Scholar]
- 137.Li C, Lee MJ, Sheng S, Meng X, Prabhu S, Winnik B, Huang B, Chung JY, Yan S, Ho CT, Yang CS. Structural identification of two metabolites of catechins and their kinetics in human urine and blood after tea ingestion. Chem Res Toxicol. 2000;13(3):177–184. doi: 10.1021/tx9901837. [DOI] [PubMed] [Google Scholar]
- 138.Wiseman S, Mulder T, Rietveld A. Tea flavonoids: bioavailability in vivo and effects on cell signaling pathways in vitro. Antioxid Redox Signal. 2001;3(6):1009–1021. doi: 10.1089/152308601317203549. [DOI] [PubMed] [Google Scholar]
- 139.Yang CS, Chen L, Lee MJ, Balentine D, Kuo MC, Schantz SP. Blood and urine levels of tea catechins after ingestion of different amounts of green tea by human volunteers. Cancer Epidemiol Biomarkers Prev. 1998;7(4):351–354. [PubMed] [Google Scholar]
- 140.van het Hof KH, de Boer HS, Wiseman SA, Lien N, Westrate JA, Tijburg LB. Consumption of green or black tea does not increase resistance of low-density lipoprotein to oxidation in humans. Am J Clin Nutr. 1997;66(5):1125–1132. doi: 10.1093/ajcn/66.5.1125. [DOI] [PubMed] [Google Scholar]
- 141.Sun T, H C-T, Shahidi F. Tea and Tea Products. Chemistry and Health – Promoting Properties. Boca Raton, London, New York: CRC Press. Taylor and Francis Group; 2009. Bioavailability and metabolism of tea catechins in human subjects. [Google Scholar]
- 142.Dryden GW, Lam A, Beatty K, Qazzaz HH, McClain CJ. A pilot study to evaluate the safety and efficacy of an oral dose of (−)-epigallocatechin-3-gallate-rich polyphenon E in patients with mild to moderate ulcerative colitis. Inflamm Bowel Dis. 2013;19(9):1904–1912. doi: 10.1097/MIB.0b013e31828f5198. [DOI] [PubMed] [Google Scholar]
- 143.Chen WY, Hsieh YA, Tsai CI, Kang YF, Chang FR, Wu YC, Wu CC. Protoapigenone, a natural derivative of apigenin, induces mitogen-activated protein kinase-dependent apoptosis in human breast cancer cells associated with induction of oxidative stress and inhibition of glutathione S-transferase pi. Invest New Drugs. 2011;29(6):1347–1359. doi: 10.1007/s10637-010-9497-0. [DOI] [PubMed] [Google Scholar]
- 144.Du GJ, Zhang Z, Wen XD, Yu C, Calway T, Yuan CS, Wang CZ. Epigallocatechin Gallate (EGCG) is the most effective cancer chemopreventive polyphenol in green tea. Nutrients. 2012;4(11):1679–1691. doi: 10.3390/nu4111679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Khandelwal A, Hall JA, Blagg BS. Synthesis and structure-activity relationships of EGCG analogues, a recently identified Hsp90 inhibitor. J Org Chem. 2013;78(16):7859–7884. doi: 10.1021/jo401027r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chung JY, Huang C, Meng X, Dong Z, Yang CS. Inhibition of activator protein 1 activity and cell growth by purified green tea and black tea polyphenols in H-ras-transformed cells: structure-activity relationship and mechanisms involved. Cancer Res. 1999;59(18):4610–4617. [PubMed] [Google Scholar]
- 147.Nam S, Smith DM, Dou QP. Ester bond-containing tea polyphenols potently inhibit proteasome activity in vitro and in vivo. J Biol Chem. 2001;276(16):13322–13330. doi: 10.1074/jbc.M004209200. [DOI] [PubMed] [Google Scholar]
- 148.Wan SB, Landis-Piwowar KR, Kuhn DJ, Chen D, Dou QP, Chan TH. Structure-activity study of epi-gallocatechin gallate (EGCG) analogs as proteasome inhibitors. Bioorg Med Chem. 2005;13(6):2177–2185. doi: 10.1016/j.bmc.2004.12.056. [DOI] [PubMed] [Google Scholar]
- 149.Landis-Piwowar KR, Kuhn DJ, Wan SB, Chen D, Chan TH, Dou QP. Evaluation of proteasome-inhibitory and apoptosis-inducing potencies of novel (−)-EGCG analogs and their prodrugs. Int J Mol Med. 2005;15(4):735–742. [PubMed] [Google Scholar]
- 150.Dodo K, Minato T, Hashimoto Y. Structure-activity relationship of bis-galloyl derivatives related to (−)-epigallocatechin gallate. Chem Pharm Bull (Tokyo) 2009;57(2):190–194. doi: 10.1248/cpb.57.190. [DOI] [PubMed] [Google Scholar]
- 151.Aggarwal BB, Bhardwaj A, Aggarwal RS, Seeram NP, Shishodia S, Takada Y. Role of resveratrol in prevention and therapy of cancer: preclinical and clinical studies. Anticancer Res. 2004;24(5a):2783–2840. [PubMed] [Google Scholar]
- 152.Larrosa M, Tomas-Barberan FA, Espin JC. The grape and wine polyphenol piceatannol is a potent inducer of apoptosis in human SK-Mel-28 melanoma cells. Eur J Nutr. 2004;43(5):275–284. doi: 10.1007/s00394-004-0471-5. [DOI] [PubMed] [Google Scholar]
- 153.Niles RM, McFarland M, Weimer MB, Redkar A, Fu YM, Meadows GG. Resveratrol is a potent inducer of apoptosis in human melanoma cells. Cancer Lett. 2003;190(2):157–163. doi: 10.1016/s0304-3835(02)00676-6. [DOI] [PubMed] [Google Scholar]
- 154.Caltagirone S, Rossi C, Poggi A, Ranelletti FO, Natali PG, Brunetti M, Aiello FB, Piantelli M. Flavonoids apigenin and quercetin inhibit melanoma growth and metastatic potential. Int J Cancer. 2000;87(4):595–600. doi: 10.1002/1097-0215(20000815)87:4<595::aid-ijc21>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 155.Fang Y, Bradley MJ, Cook KM, Herrick EJ, Nicholl MB. A potential role for resveratrol as a radiation sensitizer for melanoma treatment. J Surg Res. 2013;183(2):645–653. doi: 10.1016/j.jss.2013.02.037. [DOI] [PubMed] [Google Scholar]
- 156.Gatouillat G, Balasse E, Joseph-Pietras D, Morjani H, Madoulet C. Resveratrol induces cell-cycle disruption and apoptosis in chemoresistant B16 melanoma. J Cell Biochem. 2010;110(4):893–902. doi: 10.1002/jcb.22601. [DOI] [PubMed] [Google Scholar]
- 157.Ivanov VN, Partridge MA, Johnson GE, Huang SX, Zhou H, Hei TK. Resveratrol sensitizes melanomas to TRAIL through modulation of antiapoptotic gene expression. Exp Cell Res. 2008;314(5):1163–1176. doi: 10.1016/j.yexcr.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Habibie, Yokoyama S, Abdelhamed S, Awale S, Sakurai H, Hayakawa Y, Saiki I. Survivin suppression through STAT3/beta-catenin is essential for resveratrol-induced melanoma apoptosis. Int J Oncol. 2014;45(2):895–901. doi: 10.3892/ijo.2014.2480. [DOI] [PubMed] [Google Scholar]
- 159.Chen YJ, Chen YY, Lin YF, Hu HY, Liao HF. Resveratrol inhibits alpha-melanocyte-stimulating hormone signaling, viability, and invasiveness in melanoma cells. Evid Based Complement Alternat Med. 2013;2013:632121. doi: 10.1155/2013/632121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lee H, Zhang P, Herrmann A, Yang C, Xin H, Wang Z, Hoon DS, Forman SJ, Jove R, Riggs AD, Yu H. Acetylated STAT3 is crucial for methylation of tumor-suppressor gene promoters and inhibition by resveratrol results in demethylation. Proc Natl Acad Sci U S A. 2012;109(20):7765–7769. doi: 10.1073/pnas.1205132109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Wang M, Yu T, Zhu C, Sun H, Qiu Y, Zhu X, Li J. Resveratrol triggers protective autophagy through the ceramide/Akt/mTOR pathway in melanoma B16 cells. Nutr Cancer. 2014;66(3):435–440. doi: 10.1080/01635581.2013.878738. [DOI] [PubMed] [Google Scholar]
- 162.Trapp V, Parmakhtiar B, Papazian V, Willmott L, Fruehauf JP. Anti-angiogenic effects of resveratrol mediated by decreased VEGF and increased TSP1 expression in melanoma-endothelial cell co-culture. Angiogenesis. 2010;13(4):305–315. doi: 10.1007/s10456-010-9187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chen MC, Chang WW, Kuan YD, Lin ST, Hsu HC, Lee CH. Resveratrol inhibits LPS-induced epithelial-mesenchymal transition in mouse melanoma model. Innate Immun. 2012;18(5):685–693. doi: 10.1177/1753425912436589. [DOI] [PubMed] [Google Scholar]
- 164.Asensi M, Medina I, Ortega A, Carretero J, Bano MC, Obrador E, Estrela JM. Inhibition of cancer growth by resveratrol is related to its low bioavailability. Free Radic Biol Med. 2002;33(3):387–398. doi: 10.1016/s0891-5849(02)00911-5. [DOI] [PubMed] [Google Scholar]
- 165.Almeida L, Vaz-da-Silva M, Falcao A, Soares E, Costa R, Loureiro AI, Fernandes-Lopes C, Rocha JF, Nunes T, Wright L, Soares-da-Silva P. Pharmacokinetic and safety profile of trans-resveratrol in a rising multiple-dose study in healthy volunteers. Mol Nutr Food Res. 2009;53(Suppl 1):S7–S15. doi: 10.1002/mnfr.200800177. [DOI] [PubMed] [Google Scholar]
- 166.Goldberg DM, Yan J, Soleas GJ. Absorption of three wine-related polyphenols in three different matrices by healthy subjects. Clin Biochem. 2003;36(1):79–87. doi: 10.1016/s0009-9120(02)00397-1. [DOI] [PubMed] [Google Scholar]
- 167.Walle T, Hsieh F, DeLegge MH, Oatis JE, Jr, Walle UK. High absorption but very low bioavailability of oral resveratrol in humans. Drug Metab Dispos. 2004;32(12):1377–1382. doi: 10.1124/dmd.104.000885. [DOI] [PubMed] [Google Scholar]
- 168.Boocock DJ, Faust GE, Patel KR, Schinas AM, Brown VA, Ducharme MP, Booth TD, Crowell JA, Perloff M, Gescher AJ, Steward WP, Brenner DE. Phase I dose escalation pharmacokinetic study in healthy volunteers of resveratrol, a potential cancer chemopreventive agent. Cancer Epidemiol Biomarkers Prev. 2007;16(6):1246–1252. doi: 10.1158/1055-9965.EPI-07-0022. [DOI] [PubMed] [Google Scholar]
- 169.Burkon A, Somoza V. Quantification of free and protein-bound trans-resveratrol metabolites and identification of trans-resveratrol-C/O-conjugated diglucuronides - two novel resveratrol metabolites in human plasma. Mol Nutr Food Res. 2008;52(5):549–557. doi: 10.1002/mnfr.200700290. [DOI] [PubMed] [Google Scholar]
- 170.Boocock DJ, Patel KR, Faust GE, Normolle DP, Marczylo TH, Crowell JA, Brenner DE, Booth TD, Gescher A, Steward WP. Quantitation of trans-resveratrol and detection of its metabolites in human plasma and urine by high performance liquid chromatography. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;848(2):182–187. doi: 10.1016/j.jchromb.2006.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Larrosa M, Tomas-Barberan FA, Espin JC. Grape polyphenol resveratrol and the related molecule 4-hydroxystilbene induce growth inhibition, apoptosis, S-phase arrest, and upregulation of cyclins A, E, and B1 in human SK-Mel-28 melanoma cells. J Agric Food Chem. 2003;51(16):4576–4584. doi: 10.1021/jf030073c. [DOI] [PubMed] [Google Scholar]
- 172.Murias M, Handler N, Erker T, Pleban K, Ecker G, Saiko P, Szekeres T, Jager W. Resveratrol analogues as selective cyclooxygenase-2 inhibitors: synthesis and structure-activity relationship. Bioorg Med Chem. 2004;12(21):5571–5578. doi: 10.1016/j.bmc.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 173.Murias M, Jager W, Handler N, Erker T, Horvath Z, Szekeres T, Nohl H, Gille L. Antioxidant, prooxidant and cytotoxic activity of hydroxylated resveratrol analogues: structure-activity relationship. Biochem Pharmacol. 2005;69(6):903–912. doi: 10.1016/j.bcp.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 174.Lee KW, Kang NJ, Rogozin EA, Oh SM, Heo YS, Pugliese A, Bode AM, Lee HJ, Dong Z. The resveratrol analogue 3,5,3',4',5'-pentahydroxy-trans-stilbene inhibits cell transformation via MEK. Int J Cancer. 2008;123(11):2487–2496. doi: 10.1002/ijc.23830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ruweler M, Gulden M, Maser E, Murias M, Seibert H. Cytotoxic, cytoprotective and antioxidant activities of resveratrol and analogues in C6 astroglioma cells in vitro. Chem Biol Interact. 2009;182(2–3):128–135. doi: 10.1016/j.cbi.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 176.Wachek VHZ, Strommer S, Fuereder T, Szekeres T. Resveratrol analogue M8 chemosensitizes malignant melanoma to dacarbacin in vivo. Clin Cancer Res. 2005;(Part 2 Supply S(11)):8971S. [Google Scholar]
- 177.Paulitschke V, Schicher N, Szekeres T, Jager W, Elbling L, Riemer AB, Scheiner O, Trimurtulu G, Venkateswarlu S, Mikula M, Swoboda A, Fiebiger E, Gerner C, Pehamberger H, Kunstfeld R. 3,3',4,4',5,5'-hexahydroxystilbene impairs melanoma progression in a metastatic mouse model. J Invest Dermatol. 2010;130(6):1668–1679. doi: 10.1038/jid.2009.376. [DOI] [PubMed] [Google Scholar]
- 178.Szekeres T, Fritzer-Szekeres M, Saiko P, Jager W. Resveratrol and resveratrol analogues--structure-activity relationship. Pharm Res. 2010;27(6):1042–1048. doi: 10.1007/s11095-010-0090-1. [DOI] [PubMed] [Google Scholar]
- 179.Szekeres T, Saiko P, Fritzer-Szekeres M, Djavan B, Jager W. Chemopreventive effects of resveratrol and resveratrol derivatives. Ann N Y Acad Sci. 2011;1215:89–95. doi: 10.1111/j.1749-6632.2010.05864.x. [DOI] [PubMed] [Google Scholar]
- 180.Ashikawa K, Majumdar S, Banerjee S, Bharti AC, Shishodia S, Aggarwal BB. Piceatannol inhibits TNF-induced NF-kappaB activation and NF-kappaB-mediated gene expression through suppression of IkappaBalpha kinase and p65 phosphorylation. J Immunol. 2002;169(11):6490–6497. doi: 10.4049/jimmunol.169.11.6490. [DOI] [PubMed] [Google Scholar]
- 181.Androutsopoulos VP, Fragiadaki I, Tosca A. Activation of ERK1/2 is required for the antimitotic activity of the resveratrol analogue 3,4,5,4'-tetramethoxystilbene (DMU-212) in human melanoma cells. Exp Dermatol. 2015;24(8):632–644. doi: 10.1111/exd.12721. [DOI] [PubMed] [Google Scholar]
- 182.Morris VL, Toseef T, Nazumudeen FB, Rivoira C, Spatafora C, Tringali C, Rotenberg SA. Anti-tumor properties of cis-resveratrol methylated analogs in metastatic mouse melanoma cells. Mol Cell Biochem. 2015;402(1–2):83–91. doi: 10.1007/s11010-014-2316-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Sharma RA, Gescher AJ, Steward WP. Curcumin: the story so far. Eur J Cancer. 2005;41(13):1955–1968. doi: 10.1016/j.ejca.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 184.Dhillon N, Aggarwal BB, Newman RA, Wolff RA, Kunnumakkara AB, Abbruzzese JL, Ng CS, Badmaev V, Kurzrock R. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res. 2008;14(14):4491–4499. doi: 10.1158/1078-0432.CCR-08-0024. [DOI] [PubMed] [Google Scholar]
- 185.Woo JH, Kim YH, Choi YJ, Kim DG, Lee KS, Bae JH, Min DS, Chang JS, Jeong YJ, Lee YH, Park JW, Kwon TK. Molecular mechanisms of curcumin-induced cytotoxicity: induction of apoptosis through generation of reactive oxygen species, down-regulation of Bcl-XL and IAP, the release of cytochrome c and inhibition of Akt. Carcinogenesis. 2003;24(7):1199–1208. doi: 10.1093/carcin/bgg082. [DOI] [PubMed] [Google Scholar]
- 186.Aggarwal S, Ichikawa H, Takada Y, Sandur SK, Shishodia S, Aggarwal BB. Curcumin (diferuloylmethane) down-regulates expression of cell proliferation and antiapoptotic and metastatic gene products through suppression of IkappaBalpha kinase and Akt activation. Mol Pharmacol. 2006;69(1):195–206. doi: 10.1124/mol.105.017400. [DOI] [PubMed] [Google Scholar]
- 187.Balasubramanian S, Eckert RL. Curcumin suppresses AP1 transcription factor-dependent differentiation and activates apoptosis in human epidermal keratinocytes. J Biol Chem. 2007;282(9):6707–6715. doi: 10.1074/jbc.M606003200. [DOI] [PubMed] [Google Scholar]
- 188.Chen YR, Tan TH. Inhibition of the c-Jun N-terminal kinase (JNK) signaling pathway by curcumin. Oncogene. 1998;17(2):173–178. doi: 10.1038/sj.onc.1201941. [DOI] [PubMed] [Google Scholar]
- 189.Zheng M, Ekmekcioglu S, Walch ET, Tang CH, Grimm EA. Inhibition of nuclear factor-kappaB and nitric oxide by curcumin induces G2/M cell cycle arrest and apoptosis in human melanoma cells. Melanoma Res. 2004;14(3):165–171. doi: 10.1097/01.cmr.0000129374.76399.19. [DOI] [PubMed] [Google Scholar]
- 190.Iersel ML, Ploemen JP, Struik I, van Amersfoort C, Keyzer AE, Schefferlie JG, van Bladeren PJ. Inhibition of glutathione S-transferase activity in human melanoma cells by alpha, beta-unsaturated carbonyl derivatives. Effects of acrolein, cinnamaldehyde, citral, crotonaldehyde, curcumin, ethacrynic acid, and trans-2-hexenal. Chem Biol Interact. 1996;102(2):117–132. doi: 10.1016/s0009-2797(96)03739-8. [DOI] [PubMed] [Google Scholar]
- 191.Siwak DR, Shishodia S, Aggarwal BB, Kurzrock R. Curcumin-induced antiproliferative and proapoptotic effects in melanoma cells are associated with suppression of IkappaB kinase and nuclear factor kappaB activity and are independent of the B-Raf/mitogen-activated/extracellular signal-regulated protein kinase pathway and the Akt pathway. Cancer. 2005;104(4):879–890. doi: 10.1002/cncr.21216. [DOI] [PubMed] [Google Scholar]
- 192.Bush JA, Cheung KJ, Jr, Li G. Curcumin induces apoptosis in human melanoma cells through a Fas receptor/caspase-8 pathway independent of p53. Exp Cell Res. 2001;271(2):305–314. doi: 10.1006/excr.2001.5381. [DOI] [PubMed] [Google Scholar]
- 193.Bakhshi J, Weinstein L, Poksay KS, Nishinaga B, Bredesen DE, Rao RV. Coupling endoplasmic reticulum stress to the cell death program in mouse melanoma cells: effect of curcumin. Apoptosis. 2008;13(7):904–914. doi: 10.1007/s10495-008-0221-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ray S, Chattopadhyay N, Mitra A, Siddiqi M, Chatterjee A. Curcumin exhibits antimetastatic properties by modulating integrin receptors, collagenase activity, and expression of Nm23 and E-cadherin. J Environ Pathol Toxicol Oncol. 2003;22(1):49–58. [PubMed] [Google Scholar]
- 195.Banerji A, Chakrabarti J, Mitra A, Chatterjee A. Effect of curcumin on gelatinase A (MMP-2) activity in B16F10 melanoma cells. Cancer Lett. 2004;211(2):235–242. doi: 10.1016/j.canlet.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 196.Depeille P, Cuq P, Passagne I, Evrard A, Vian L. Combined effects of GSTP1 and MRP1 in melanoma drug resistance. Br J Cancer. 2005;93(2):216–223. doi: 10.1038/sj.bjc.6602681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wu X, Zeng H, Zhang X, Zhao Y, Sha H, Ge X, Zhang M, Gao X, Xu Q. Phosphatase of regenerating liver-3 promotes motility and metastasis of mouse melanoma cells. Am J Pathol. 2004;164(6):2039–2054. doi: 10.1016/S0002-9440(10)63763-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zeng Q, Dong JM, Guo K, Li J, Tan HX, Koh V, Pallen CJ, Manser E, Hong W. PRL-3 and PRL-1 promote cell migration, invasion, and metastasis. Cancer Res. 2003;63(11):2716–2722. [PubMed] [Google Scholar]
- 199.Wang L, Shen Y, Song R, Sun Y, Xu J, Xu Q. An anticancer effect of curcumin mediated by down-regulating phosphatase of regenerating liver-3 expression on highly metastatic melanoma cells. Mol Pharmacol. 2009;76(6):1238–1245. doi: 10.1124/mol.109.059105. [DOI] [PubMed] [Google Scholar]
- 200.Philip S, Bulbule A, Kundu GC. Osteopontin stimulates tumor growth and activation of promatrix metalloproteinase-2 through nuclear factor-kappa B-mediated induction of membrane type 1 matrix metalloproteinase in murine melanoma cells. J Biol Chem. 2001;276(48):44926–44935. doi: 10.1074/jbc.M103334200. [DOI] [PubMed] [Google Scholar]
- 201.Philip S, Kundu GC. Osteopontin induces nuclear factor kappa B-mediated promatrix metalloproteinase-2 activation through I kappa B alpha /IKK signaling pathways, and curcumin (diferulolylmethane) down-regulates these pathways. J Biol Chem. 2003;278(16):14487–14497. doi: 10.1074/jbc.M207309200. [DOI] [PubMed] [Google Scholar]
- 202.Marin YE, Wall BA, Wang S, Namkoong J, Martino JJ, Suh J, Lee HJ, Rabson AB, Yang CS, Chen S, Ryu JH. Curcumin downregulates the constitutive activity of NF-kappaB and induces apoptosis in novel mouse melanoma cells. Melanoma Res. 2007;17(5):274–283. doi: 10.1097/CMR.0b013e3282ed3d0e. [DOI] [PubMed] [Google Scholar]
- 203.Odot J, Albert P, Carlier A, Tarpin M, Devy J, Madoulet C. In vitro and in vivo anti-tumoral effect of curcumin against melanoma cells. Int J Cancer. 2004;111(3):381–387. doi: 10.1002/ijc.20160. [DOI] [PubMed] [Google Scholar]
- 204.Prasad S, Tyagi AK, Aggarwal BB. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: the golden pigment from golden spice. Cancer Res Treat. 2014;46(1):2–18. doi: 10.4143/crt.2014.46.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Shoba G, Joy D, Joseph T, Majeed M, Rajendran R, Srinivas PS. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998;64(4):353–356. doi: 10.1055/s-2006-957450. [DOI] [PubMed] [Google Scholar]
- 206.Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, Ko JY, Lin JT, Lin BR, Ming-Shiang W, Yu HS, Jee SH, Chen GS, Chen TM, Chen CA, Lai MK, Pu YS, Pan MH, Wang YJ, Tsai CC, Hsieh CY. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001;21(4b):2895–2900. [PubMed] [Google Scholar]
- 207.Sharma RA, Euden SA, Platton SL, Cooke DN, Shafayat A, Hewitt HR, Marczylo TH, Morgan B, Hemingway D, Plummer SM, Pirmohamed M, Gescher AJ, Steward WP. Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res. 2004;10(20):6847–6854. doi: 10.1158/1078-0432.CCR-04-0744. [DOI] [PubMed] [Google Scholar]
- 208.Sun J, Bi C, Chan HM, Sun S, Zhang Q, Zheng Y. Curcumin-loaded solid lipid nanoparticles have prolonged in vitro antitumour activity, cellular uptake and improved in vivo bioavailability. Colloids Surf B Biointerfaces. 2013;111c:367–375. doi: 10.1016/j.colsurfb.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 209.Reddy AR, Dinesh P, Prabhakar AS, Umasankar K, Shireesha B, Raju MB. A comprehensive review on SAR of curcumin. Mini Rev Med Chem. 2013;13(12):1769–1777. doi: 10.2174/1389557511313120007. [DOI] [PubMed] [Google Scholar]
- 210.Vyas A, Dandawate P, Padhye S, Ahmad A, Sarkar F. Perspectives on new synthetic curcumin analogs and their potential anticancer properties. Curr Pharm Des. 2013;19(11):2047–2069. [PMC free article] [PubMed] [Google Scholar]
- 211.Pisano M, Pagnan G, Dettori MA, Cossu S, Caffa I, Sassu I, Emionite L, Fabbri D, Cilli M, Pastorino F, Palmieri G, Delogu G, Ponzoni M, Rozzo C. Enhanced anti-tumor activity of a new curcumin-related compound against melanoma and neuroblastoma cells. Mol Cancer. 2010;9:137. doi: 10.1186/1476-4598-9-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Rozzo C, Fanciulli M, Fraumene C, Corrias A, Cubeddu T, Sassu I, Cossu S, Nieddu V, Galleri G, Azara E, Dettori MA, Fabbri D, Palmieri G, Pisano M. Molecular changes induced by the curcumin analogue D6 in human melanoma cells. Mol Cancer. 2013;12:37. doi: 10.1186/1476-4598-12-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Bill MA, Fuchs JR, Li C, Yui J, Bakan C, Benson DM, Jr, Schwartz EB, Abdelhamid D, Lin J, Hoyt DG, Fossey SL, Young GS, Carson WE, 3rd, Li PK, Lesinski GB. The small molecule curcumin analog FLLL32 induces apoptosis in melanoma cells via STAT3 inhibition and retains the cellular response to cytokines with anti-tumor activity. Mol Cancer. 2010;9:165. doi: 10.1186/1476-4598-9-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Bill MA, Nicholas C, Mace TA, Etter JP, Li C, Schwartz EB, Fuchs JR, Young GS, Lin L, Lin J, He L, Phelps M, Li PK, Lesinski GB. Structurally modified curcumin analogs inhibit STAT3 phosphorylation and promote apoptosis of human renal cell carcinoma and melanoma cell lines. PLoS One. 2012;7(8):e40724. doi: 10.1371/journal.pone.0040724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Faiao-Flores F, Suarez JA, Soto-Cerrato V, Espona-Fiedler M, Perez-Tomas R, Maria DA. Bcl-2 family proteins and cytoskeleton changes involved in DM-1 cytotoxic effect on melanoma cells. Tumour Biol. 2013;34(2):1235–1243. doi: 10.1007/s13277-013-0666-6. [DOI] [PubMed] [Google Scholar]
- 216.Zhang P, Bai H, Liu G, Wang H, Chen F, Zhang B, Zeng P, Wu C, Peng C, Huang C, Song Y, Song E. MicroRNA-33b, upregulated by EF24, a curcumin analog, suppresses the epithelial-to-mesenchymal transition (EMT) and migratory potential of melanoma cells by targeting HMGA2. Toxicol Lett. 2015;234(3):151–161. doi: 10.1016/j.toxlet.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 217.Li WG, Zhang XY, Wu YJ, Tian X. Anti-inflammatory effect and mechanism of proanthocyanidins from grape seeds. Acta Pharmacol Sin. 2001;22(12):1117–1120. [PubMed] [Google Scholar]
- 218.Martinez C, Vicente V, Yanez J, Alcaraz M, Castells MT, Canteras M, Benavente-Garcia O, Castillo J. The effect of the flavonoid diosmin, grape seed extract and red wine on the pulmonary metastatic B16F10 melanoma. Histol Histopathol. 2005;20(4):1121–1129. doi: 10.14670/HH-20.1121. [DOI] [PubMed] [Google Scholar]
- 219.Mittal A, Elmets CA, Katiyar SK. Dietary feeding of proanthocyanidins from grape seeds prevents photocarcinogenesis in SKH-1 hairless mice: relationship to decreased fat and lipid peroxidation. Carcinogenesis. 2003;24(8):1379–1388. doi: 10.1093/carcin/bgg095. [DOI] [PubMed] [Google Scholar]
- 220.Tatsuno T, Jinno M, Arima Y, Kawabata T, Hasegawa T, Yahagi N, Takano F, Ohta T. Anti-inflammatory and anti-melanogenic proanthocyanidin oligomers from peanut skin. Biol Pharm Bull. 2012;35(6):909–916. doi: 10.1248/bpb.35.909. [DOI] [PubMed] [Google Scholar]
- 221.Vaid M, Singh T, Katiyar SK. Grape seed proanthocyanidins inhibit melanoma cell invasiveness by reduction of PGE2 synthesis and reversal of epithelial-to-mesenchymal transition. PLoS One. 2011;6(6):e21539. doi: 10.1371/journal.pone.0021539. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 222.Martinez Conesa C, Vicente Ortega V, Yanez Gascon MJ, Garcia Reverte JM, Canteras Jordana M, Alcaraz Banos M. Experimental model for treating pulmonary metastatic melanoma using grape-seed extract, red wine and ethanol. Clin Transl Oncol. 2005;7(3):115–121. doi: 10.1007/BF02708744. [DOI] [PubMed] [Google Scholar]
- 223.Gu L, Kelm MA, Hammerstone JF, Beecher G, Holden J, Haytowitz D, Gebhardt S, Prior RL. Concentrations of proanthocyanidins in common foods and estimations of normal consumption. J Nutr. 2004;134(3):613–617. doi: 10.1093/jn/134.3.613. [DOI] [PubMed] [Google Scholar]
- 224.Stoupi S, Williamson G, Viton F, Barron D, King LJ, Brown JE, Clifford MN. In vivo bioavailability, absorption, excretion, and pharmacokinetics of [14C]procyanidin B2 in male rats. Drug Metab Dispos. 2010;38(2):287–291. doi: 10.1124/dmd.109.030304. [DOI] [PubMed] [Google Scholar]
- 225.Choy YY, Jaggers GK, Oteiza PI, Waterhouse AL. Bioavailability of intact proanthocyanidins in the rat colon after ingestion of grape seed extract. J Agric Food Chem. 2013;61(1):121–127. doi: 10.1021/jf301939e. [DOI] [PubMed] [Google Scholar]
- 226.Shoji T, Masumoto S, Moriichi N, Akiyama H, Kanda T, Ohtake Y, Goda Y. Apple procyanidin oligomers absorption in rats after oral administration: analysis of procyanidins in plasma using the porter method and high-performance liquid chromatography/tandem mass spectrometry. J Agric Food Chem. 2006;54(3):884–892. doi: 10.1021/jf052260b. [DOI] [PubMed] [Google Scholar]
- 227.Deprez S, Brezillon C, Rabot S, Philippe C, Mila I, Lapierre C, Scalbert A. Polymeric proanthocyanidins are catabolized by human colonic microflora into low-molecular-weight phenolic acids. J Nutr. 2000;130(11):2733–2738. doi: 10.1093/jn/130.11.2733. [DOI] [PubMed] [Google Scholar]
- 228.Appeldoorn MM, Vincken JP, Aura AM, Hollman PC, Gruppen H. Procyanidin dimers are metabolized by human microbiota with 2-(3,4-dihydroxyphenyl)acetic acid and 5-(3,4-dihydroxyphenyl)-gamma-valerolactone as the major metabolites. J Agric Food Chem. 2009;57(3):1084–1092. doi: 10.1021/jf803059z. [DOI] [PubMed] [Google Scholar]
- 229.Manach C, Williamson G, Morand C, Scalbert A, Remesy C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am J Clin Nutr. 2005;81(1 Suppl):230s–242s. doi: 10.1093/ajcn/81.1.230S. [DOI] [PubMed] [Google Scholar]
- 230.Tsang C, Auger C, Mullen W, Bornet A, Rouanet JM, Crozier A, Teissedre PL. The absorption, metabolism and excretion of flavan-3-ols and procyanidins following the ingestion of a grape seed extract by rats. Br J Nutr. 2005;94(2):170–181. doi: 10.1079/bjn20051480. [DOI] [PubMed] [Google Scholar]
- 231.Kashiwada Y, Nonaka G, Nishioka I, Chang JJ, Lee KH. Antitumor agents 129. Tannins and related compounds as selective cytotoxic agents. J Nat Prod. 1992;55(8):1033–1043. doi: 10.1021/np50086a002. [DOI] [PubMed] [Google Scholar]
- 232.Kolodziej HHC, Woerdenbag HJ. Konings, AWT Moderate cytotoxicity of proanthocyanidins to human tumour cell lines. Phytotherapy Research. 1995;(9):410–415. [Google Scholar]
- 233.Kozikowski AP, Tuckmantel W, George C. Studies in polyphenol chemistry and bioactivity. 2. Establishment of interflavan linkage regio- and stereochemistry by oxidative degradation of an O-alkylated derivative of procyanidin B2 to (R)-(−)-2,4-diphenylbutyric acid. J Org Chem. 2000;65(17):5371–5381. doi: 10.1021/jo000485+. [DOI] [PubMed] [Google Scholar]
- 234.Kozikowski AP, Tuckmantel W, Bottcher G, Romanczyk LJ., Jr Studies in polyphenol chemistry and bioactivity. 4.(1) Synthesis of trimeric, tetrameric, pentameric, and higher oligomeric epicatechin-derived procyanidins having all-4beta,8-interflavan connectivity and their inhibition of cancer cell growth through cell cycle arrest. J Org Chem. 2003;68(5):1641–1658. doi: 10.1021/jo020393f. [DOI] [PubMed] [Google Scholar]
- 235.Fujii W, Toda K, Kawaguchi K, Kawahara SI, Katoh M, Hattori Y, Fujii H, Makabe H. Syntheses of prodelphinidin B3 and C2, and their antitumor activities through cell cycle arrest and caspase-3 activation. Tetrahedron. 2013;(69):3543–3550. [Google Scholar]
- 236.Duan L, Carrier DJ, Clausen EC. Silymarin extraction from milk thistle using hot water. Appl Biochem Biotechnol. 2004;113–116:559–568. doi: 10.1385/abab:114:1-3:559. [DOI] [PubMed] [Google Scholar]
- 237.Wallace SN, Carrier DJ, Clausen E. Extraction of nutraceuticals from milk thistle: part II. Extraction with organic solvents. Appl Biochem Biotechnol. 2003;105–108:891–903. doi: 10.1385/abab:108:1-3:891. [DOI] [PubMed] [Google Scholar]
- 238.Wagner H, Horhammer L, Munster R. On the chemistry of silymarin (silybin), the active principle of the fruits from Silybum marianum (L.) Gaertn. (Carduus marianus L.) Arzneimittelforschung. 1968;18(6):688–696. [PubMed] [Google Scholar]
- 239.Katiyar SK. Silymarin and skin cancer prevention: anti-inflammatory, antioxidant and immunomodulatory effects (Review) Int J Oncol. 2005;26(1):169–176. [PubMed] [Google Scholar]
- 240.Katiyar SK, Korman NJ, Mukhtar H, Agarwal R. Protective effects of silymarin against photocarcinogenesis in a mouse skin model. J Natl Cancer Inst. 1997;89(8):556–566. doi: 10.1093/jnci/89.8.556. [DOI] [PubMed] [Google Scholar]
- 241.Agarwal R, Agarwal C, Ichikawa H, Singh RP, Aggarwal BB. Anticancer potential of silymarin: from bench to bed side. Anticancer Res. 2006;26(6b):4457–4498. [PubMed] [Google Scholar]
- 242.Singh RP, Agarwal R. Flavonoid antioxidant silymarin and skin cancer. Antioxid Redox Signal. 2002;4(4):655–663. doi: 10.1089/15230860260220166. [DOI] [PubMed] [Google Scholar]
- 243.Lee MH, Huang Z, Kim DJ, Kim SH, Kim MO, Lee SY, Xie H, Park SJ, Kim JY, Kundu JK, Bode AM, Surh YJ, Dong Z. Direct targeting of MEK1/2 and RSK2 by silybin induces cell-cycle arrest and inhibits melanoma cell growth. Cancer Prev Res (Phila) 2013;6(5):455–465. doi: 10.1158/1940-6207.CAPR-12-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Li LH, Wu LJ, Jiang YY, Tashiro S, Onodera S, Uchiumi F, Ikejima T. Silymarin enhanced cytotoxic effect of anti-Fas agonistic antibody CH11 on A375-S2 cells. J Asian Nat Prod Res. 2007;9(6–8):593–602. doi: 10.1080/10286020600882502. [DOI] [PubMed] [Google Scholar]
- 245.Schandalik R, Perucca E. Pharmacokinetics of silybin following oral administration of silipide in patients with extrahepatic biliary obstruction. Drugs Exp Clin Res. 1994;20(1):37–42. [PubMed] [Google Scholar]
- 246.Schandalik R, Gatti G, Perucca E. Pharmacokinetics of silybin in bile following administration of silipide and silymarin in cholecystectomy patients. Arzneimittelforschung. 1992;42(7):964–968. [PubMed] [Google Scholar]
- 247.Weyhenmeyer R, Mascher H, Birkmayer J. Study on dose-linearity of the pharmacokinetics of silibinin diastereomers using a new stereospecific assay. Int J Clin Pharmacol Ther Toxicol. 1992;30(4):134–138. [PubMed] [Google Scholar]
- 248.Lorenz D, Lucker PW, Mennicke WH, Wetzelsberger N. Pharmacokinetic studies with silymarin in human serum and bile. Methods Find Exp Clin Pharmacol. 1984;6(10):655–661. [PubMed] [Google Scholar]
- 249.Ahmed B, Khan SA, Alam T. Synthesis and antihepatotoxic activity of some heterocyclic compounds containing the 1,4-dioxane ring system. Pharmazie. 2003;58(3):173–176. [PubMed] [Google Scholar]
- 250.Agarwal C, Wadhwa R, Deep G, Biedermann D, Gazak R, Kren V, Agarwal R. Anti-cancer efficacy of silybin derivatives -- a structure-activity relationship. PLoS One. 2013;8(3):e60074. doi: 10.1371/journal.pone.0060074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Patel D, Shukla S, Gupta S. Apigenin and cancer chemoprevention: progress, potential and promise (review) Int J Oncol. 2007;30(1):233–245. [PubMed] [Google Scholar]
- 252.Chao SC, Huang SC, Hu DN, Lin HY. Subtoxic Levels of Apigenin Inhibit Expression and Secretion of VEGF by Uveal Melanoma Cells via Suppression of ERK1/2 and PI3K/Akt Pathways. Evid Based Complement Alternat Med. 2013;2013:817674. doi: 10.1155/2013/817674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Ye Y, Chou GX, Wang H, Chu JH, Yu ZL. Flavonoids, apigenin and icariin exert potent melanogenic activities in murine B16 melanoma cells. Phytomedicine. 2010;18(1):32–35. doi: 10.1016/j.phymed.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 254.Piantelli M, Rossi C, Iezzi M, La Sorda R, Iacobelli S, Alberti S, Natali PG. Flavonoids inhibit melanoma lung metastasis by impairing tumor cells endothelium interactions. J Cell Physiol. 2006;207(1):23–29. doi: 10.1002/jcp.20510. [DOI] [PubMed] [Google Scholar]
- 255.Das S, Das J, Samadder A, Boujedaini N, Khuda-Bukhsh AR. Apigenin-induced apoptosis in A375 and A549 cells through selective action and dysfunction of mitochondria. Exp Biol Med (Maywood) 2012;237(12):1433–1448. doi: 10.1258/ebm.2012.012148. [DOI] [PubMed] [Google Scholar]
- 256.Das S, Das J, Samadder A, Paul A, Khuda-Bukhsh AR. Strategic formulation of apigenin-loaded PLGA nanoparticles for intracellular trafficking, DNA targeting and improved therapeutic effects in skin melanoma in vitro. Toxicol Lett. 2013;223(2):124–138. doi: 10.1016/j.toxlet.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 257.Ross JA, Kasum CM. Dietary flavonoids: bioavailability, metabolic effects, and safety. Annu Rev Nutr. 2002;22:19–34. doi: 10.1146/annurev.nutr.22.111401.144957. [DOI] [PubMed] [Google Scholar]
- 258.Zhang J, Liu D, Huang Y, Gao Y, Qian S. Biopharmaceutics classification and intestinal absorption study of apigenin. Int J Pharm. 2012;436(1–2):311–317. doi: 10.1016/j.ijpharm.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 259.Gradolatto A, Basly JP, Berges R, Teyssier C, Chagnon MC, Siess MH, Canivenc-Lavier MC. Pharmacokinetics and metabolism of apigenin in female and male rats after a single oral administration. Drug Metab Dispos. 2005;33(1):49–54. doi: 10.1124/dmd.104.000893. [DOI] [PubMed] [Google Scholar]
- 260.Hanske L, Loh G, Sczesny S, Blaut M, Braune A. The bioavailability of apigenin-7-glucoside is influenced by human intestinal microbiota in rats. J Nutr. 2009;139(6):1095–1102. doi: 10.3945/jn.108.102814. [DOI] [PubMed] [Google Scholar]
- 261.Meyer H, Bolarinwa A, Wolfram G, Linseisen J. Bioavailability of apigenin from apiin-rich parsley in humans. Ann Nutr Metab. 2006;50(3):167–172. doi: 10.1159/000090736. [DOI] [PubMed] [Google Scholar]
- 262.Ding SM, Zhang ZH, Song J, Cheng XD, Jiang J, Jia XB. Enhanced bioavailability of apigenin via preparation of a carbon nanopowder solid dispersion. Int J Nanomedicine. 2014;9:2327–2333. doi: 10.2147/IJN.S60938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Chang HL, Su JH, Yeh YT, Lee YC, Chen HM, Wu YC, Yuan SS. Protoapigenone, a novel flavonoid, inhibits ovarian cancer cell growth in vitro and in vivo. Cancer Lett. 2008;267(1):85–95. doi: 10.1016/j.canlet.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 264.Chang HL, Wu YC, Su JH, Yeh YT, Yuan SS. Protoapigenone, a novel flavonoid, induces apoptosis in human prostate cancer cells through activation of p38 mitogen-activated protein kinase and c-Jun NH2-terminal kinase 1/2. J Pharmacol Exp Ther. 2008;325(3):841–849. doi: 10.1124/jpet.107.135442. [DOI] [PubMed] [Google Scholar]
- 265.Hunyadi A, Chuang DW, Danko B, Chiang MY, Lee CL, Wang HC, Wu CC, Chang FR, Wu YC. Direct semi-synthesis of the anticancer lead-drug protoapigenone from apigenin, and synthesis of further new cytotoxic protoflavone derivatives. PLoS One. 2011;6(8):e23922. doi: 10.1371/journal.pone.0023922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Zheng X, Yu L, Yang J, Yao X, Yan W, Bo S, Liu Y, Wei Y, Wu Z, Wang G. Synthesis and Anti-cancer Activities of Apigenin Derivatives. Med Chem. 2014 doi: 10.2174/1573406410666140307152557. [DOI] [PubMed] [Google Scholar]
- 267.Liu R, Zhao B, Wang DE, Yao T, Pang L, Tu Q, Ahmed SM, Liu JJ, Wang J. Nitrogen-containing apigenin analogs: preparation and biological activity. Molecules. 2012;17(12):14748–14764. doi: 10.3390/molecules171214748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Shin DH, Kim OH, Jun HS, Kang MK. Inhibitory effect of capsaicin on B16-F10 melanoma cell migration via the phosphatidylinositol 3-kinase/Akt/Rac1 signal pathway. Exp Mol Med. 2008;40(5):486–494. doi: 10.3858/emm.2008.40.5.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Surh YJ, Lee E, Lee JM. Chemoprotective properties of some pungent ingredients present in red pepper and ginger. Mutat Res. 1998;402(1–2):259–267. doi: 10.1016/s0027-5107(97)00305-9. [DOI] [PubMed] [Google Scholar]
- 270.Kim MY. Nitric oxide triggers apoptosis in A375 human melanoma cells treated with capsaicin and resveratrol. Mol Med Rep. 2012;5(2):585–591. doi: 10.3892/mmr.2011.688. [DOI] [PubMed] [Google Scholar]
- 271.Patel PS, Varney ML, Dave BJ, Singh RK. Regulation of constitutive and induced NF-kappaB activation in malignant melanoma cells by capsaicin modulates interleukin-8 production and cell proliferation. J Interferon Cytokine Res. 2002;22(4):427–435. doi: 10.1089/10799900252952217. [DOI] [PubMed] [Google Scholar]
- 272.Patel PS, Yang S, Li A, Varney ML, Singh RK. Capsaicin regulates vascular endothelial cell growth factor expression by modulation of hypoxia inducing factor-1alpha in human malignant melanoma cells. J Cancer Res Clin Oncol. 2002;128(9):461–468. doi: 10.1007/s00432-002-0368-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Morre DJ, Sun E, Geilen C, Wu LY, de Cabo R, Krasagakis K, Orfanos CE, Morre DM. Capsaicin inhibits plasma membrane NADH oxidase and growth of human and mouse melanoma lines. Eur J Cancer. 1996;32a(11):1995–2003. doi: 10.1016/0959-8049(96)00234-1. [DOI] [PubMed] [Google Scholar]
- 274.Min JK, Han KY, Kim EC, Kim YM, Lee SW, Kim OH, Kim KW, Gho YS, Kwon YG. Capsaicin inhibits in vitro and in vivo angiogenesis. Cancer Res. 2004;64(2):644–651. doi: 10.1158/0008-5472.can-03-3250. [DOI] [PubMed] [Google Scholar]
- 275.Beaudry F, Vachon P. Quantitative determination of capsaicin, a transient receptor potential channel vanilloid 1 agonist, by liquid chromatography quadrupole ion trap mass spectrometry: evaluation of in vitro metabolic stability. Biomed Chromatogr. 2009;23(2):204–211. doi: 10.1002/bmc.1107. [DOI] [PubMed] [Google Scholar]
- 276.Chanda S, Bashir M, Babbar S, Koganti A, Bley K. In vitro hepatic and skin metabolism of capsaicin. Drug Metab Dispos. 2008;36(4):670–675. doi: 10.1124/dmd.107.019240. [DOI] [PubMed] [Google Scholar]
- 277.Appendino G, Harrison S, De Petrocellis L, Daddario N, Bianchi F, Schiano Moriello A, Trevisani M, Benvenuti F, Geppetti P, Di Marzo V. Halogenation of a capsaicin analogue leads to novel vanilloid TRPV1 receptor antagonists. Br J Pharmacol. 2003;139(8):1417–1424. doi: 10.1038/sj.bjp.0705387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Yang D, Luo Z, Ma S, Wong WT, Ma L, Zhong J, He H, Zhao Z, Cao T, Yan Z, Liu D, Arendshorst WJ, Huang Y, Tepel M, Zhu Z. Activation of TRPV1 by dietary capsaicin improves endothelium-dependent vasorelaxation and prevents hypertension. Cell Metab. 2010;12(2):130–141. doi: 10.1016/j.cmet.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Chaiyasit K, Khovidhunkit W, Wittayalertpanya S. Pharmacokinetic and the effect of capsaicin in Capsicum frutescens on decreasing plasma glucose level. J Med Assoc Thai. 2009;92(1):108–113. [PubMed] [Google Scholar]
- 280.Suresh D, Srinivasan K. Tissue distribution & elimination of capsaicin, piperine & curcumin following oral intake in rats. Indian J Med Res. 2010;131:682–691. [PubMed] [Google Scholar]
- 281.William Rollyson CS. Kathleen Brown, Haley Perry, Cathryn Stevenson, Clayton Crabtree, Aaron Dom, Jamie Lau, Theodore Witte, W Hardman, Piyali Dasgupta, The anti-cancer dietary compound capsaicin shows higher bioavailability in the lung than other organs. The FASEB Journal. 2014;1(28):S644.2. [Google Scholar]
- 282.Walpole CS, Bevan S, Bovermann G, Boelsterli JJ, Breckenridge R, Davies JW, Hughes GA, James I, Oberer L, Winter J, et al. The discovery of capsazepine, the first competitive antagonist of the sensory neuron excitants capsaicin and resiniferatoxin. J Med Chem. 1994;37(13):1942–1954. doi: 10.1021/jm00039a006. [DOI] [PubMed] [Google Scholar]
- 283.Walpole CS, Wrigglesworth R, Bevan S, Campbell EA, Dray A, James IF, Masdin KJ, Perkins MN, Winter J. Analogues of capsaicin with agonist activity as novel analgesic agents; structure-activity studies. 3. The hydrophobic side-chain "C-region". J Med Chem. 1993;36(16):2381–2389. doi: 10.1021/jm00068a016. [DOI] [PubMed] [Google Scholar]
- 284.Walpole CS, Wrigglesworth R, Bevan S, Campbell EA, Dray A, James IF, Masdin KJ, Perkins MN, Winter J. Analogues of capsaicin with agonist activity as novel analgesic agents; structure-activity studies. 2. The amide bond "B-region". J Med Chem. 1993;36(16):2373–2380. doi: 10.1021/jm00068a015. [DOI] [PubMed] [Google Scholar]
- 285.Walpole CS, Wrigglesworth R, Bevan S, Campbell EA, Dray A, James IF, Perkins MN, Reid DJ, Winter J. Analogues of capsaicin with agonist activity as novel analgesic agents; structure-activity studies. 1. The aromatic "A-region". J Med Chem. 1993;36(16):2362–2372. doi: 10.1021/jm00068a014. [DOI] [PubMed] [Google Scholar]
- 286.Huang XF, Xue JY, Jiang AQ, Zhu HL. Capsaicin and its analogues: structure-activity relationship study. Curr Med Chem. 2013;20(21):2661–2672. doi: 10.2174/0929867311320210004. [DOI] [PubMed] [Google Scholar]
- 287.Thomas KC, Ethirajan M, Shahrokh K, Sun H, Lee J, Cheatham TE, 3rd, Yost GS, Reilly CA. Structure-activity relationship of capsaicin analogs and transient receptor potential vanilloid 1-mediated human lung epithelial cell toxicity. J Pharmacol Exp Ther. 2011;337(2):400–410. doi: 10.1124/jpet.110.178491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Cong R, Sun Q, Yang L, Gu H, Zeng Y, Wang B. Effect of Genistein on vasculogenic mimicry formation by human uveal melanoma cells. J Exp Clin Cancer Res. 2009;28:124. doi: 10.1186/1756-9966-28-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Danciu C, Borcan F, Bojin F, Zupko I, Dehelean C. Effect of the isoflavone genistein on tumor size, metastasis potential and melanization in a B16 mouse model of murine melanoma. Nat Prod Commun. 2013;8(3):343–346. [PubMed] [Google Scholar]
- 290.Kiguchi K, Constantinou AI, Huberman E. Genistein-induced cell differentiation and protein-linked DNA strand breakage in human melanoma cells. Cancer Commun. 1990;2(8):271–277. doi: 10.3727/095535490820874218. [DOI] [PubMed] [Google Scholar]
- 291.Sjoberg ER, Chammas R, Ozawa H, Kawashima I, Khoo KH, Morris HR, Dell A, Tai T, Varki A. Expression of de-N-acetyl-gangliosides in human melanoma cells is induced by genistein or nocodazole. J Biol Chem. 1995;270(7):2921–2930. doi: 10.1074/jbc.270.7.2921. [DOI] [PubMed] [Google Scholar]
- 292.Ji C, Yang YL, He L, Gu B, Xia JP, Sun WL, Su ZL, Chen B, Bi ZG. Increasing ceramides sensitizes genistein-induced melanoma cell apoptosis and growth inhibition. Biochem Biophys Res Commun. 2012;421(3):462–467. doi: 10.1016/j.bbrc.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 293.Yang Y, Wang H, Wang J, Li X, Ma M, Yang W. Effect of livin gene suppression by genistein on apoptosis, cell cycle and proliferation of malignant melanoma LiBr cells. Nan Fang Yi Ke Da Xue Xue Bao. 2012;32(8):1163–1167. [PubMed] [Google Scholar]
- 294.Casagrande F, Darbon JM. p21CIP1 is dispensable for the G2 arrest caused by genistein in human melanoma cells. Exp Cell Res. 2000;258(1):101–108. doi: 10.1006/excr.2000.4914. [DOI] [PubMed] [Google Scholar]
- 295.Darbon JM, Penary M, Escalas N, Casagrande F, Goubin-Gramatica F, Baudouin C, Ducommun B. Distinct Chk2 activation pathways are triggered by genistein and DNA-damaging agents in human melanoma cells. J Biol Chem. 2000;275(20):15363–15369. doi: 10.1074/jbc.275.20.15363. [DOI] [PubMed] [Google Scholar]
- 296.Kuzumaki T, Kobayashi T, Ishikawa K. Genistein induces p21(Cip1/WAF1) expression and blocks the G1 to S phase transition in mouse fibroblast and melanoma cells. Biochem Biophys Res Commun. 1998;251(1):291–295. doi: 10.1006/bbrc.1998.9462. [DOI] [PubMed] [Google Scholar]
- 297.Rauth S, Kichina J, Green A. Inhibition of growth and induction of differentiation of metastatic melanoma cells in vitro by genistein: chemosensitivity is regulated by cellular p53. Br J Cancer. 1997;75(11):1559–1566. doi: 10.1038/bjc.1997.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Menon LG, Kuttan R, Nair MG, Chang YC, Kuttan G. Effect of isoflavones genistein and daidzein in the inhibition of lung metastasis in mice induced by B16F-10 melanoma cells. Nutr Cancer. 1998;30(1):74–77. doi: 10.1080/01635589809514644. [DOI] [PubMed] [Google Scholar]
- 299.Yan C, Han R. Suppression of adhesion-induced protein tyrosine phosphorylation decreases invasive and metastatic potentials of B16-BL6 melanoma cells by protein tyrosine kinase inhibitor genistein. Invasion Metastasis. 1997;17(4):189–198. [PubMed] [Google Scholar]
- 300.Yan C, Han R. Genistein suppresses adhesion-induced protein tyrosine phosphorylation and invasion of B16-BL6 melanoma cells. Cancer Lett. 1998;129(1):117–124. doi: 10.1016/s0304-3835(98)00093-7. [DOI] [PubMed] [Google Scholar]
- 301.Farina HG, Pomies M, Alonso DF, Gomez DE. Antitumor and antiangiogenic activity of soy isoflavone genistein in mouse models of melanoma and breast cancer. Oncol Rep. 2006;16(4):885–891. [PubMed] [Google Scholar]
- 302.Record IR, Broadbent JL, King RA, Dreosti IE, Head RJ, Tonkin AL. Genistein inhibits growth of B16 melanoma cells in vivo and in vitro and promotes differentiation in vitro. Int J Cancer. 1997;72(5):860–864. doi: 10.1002/(sici)1097-0215(19970904)72:5<860::aid-ijc24>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 303.Wang Y, Catana F, Yang Y, Roderick R, van Breemen RB. An LC-MS method for analyzing total resveratrol in grape juice, cranberry juice, and in wine. J Agric Food Chem. 2002;50(3):431–435. doi: 10.1021/jf010812u. [DOI] [PubMed] [Google Scholar]
- 304.Yan CH, Chen XG, Li Y, Han R. Effects of genistein, a soybean-derived isoflavone, on proliferation and differentiation of B16-BL6 mouse melanoma cells. J Asian Nat Prod Res. 1999;1(4):285–299. doi: 10.1080/10286029908039877. [DOI] [PubMed] [Google Scholar]
- 305.Cohen R, Schwartz B, Peri I, Shimoni E. Improving bioavailability and stability of genistein by complexation with high-amylose corn starch. J Agric Food Chem. 2011;59(14):7932–7938. doi: 10.1021/jf2013277. [DOI] [PubMed] [Google Scholar]
- 306.Zhou P, Li LP, Luo SQ, Jiang HD, Zeng S. Intestinal absorption of luteolin from peanut hull extract is more efficient than that from individual pure luteolin. J Agric Food Chem. 2008;56(1):296–300. doi: 10.1021/jf072612+. [DOI] [PubMed] [Google Scholar]
- 307.Coldham NG, Zhang AQ, Key P, Sauer MJ. Absolute bioavailability of [14C] genistein in the rat; plasma pharmacokinetics of parent compound, genistein glucuronide and total radioactivity. Eur J Drug Metab Pharmacokinet. 2002;27(4):249–258. doi: 10.1007/BF03192335. [DOI] [PubMed] [Google Scholar]
- 308.Steensma A, Faassen-Peters MA, Noteborn HP, Rietjens IM. Bioavailability of genistein and its glycoside genistin as measured in the portal vein of freely moving unanesthetized rats. J Agric Food Chem. 2006;54(21):8006–8012. doi: 10.1021/jf060783t. [DOI] [PubMed] [Google Scholar]
- 309.Kwon SH, Kang MJ, Huh JS, Ha KW, Lee JR, Lee SK, Lee BS, Han IH, Lee MS, Lee MW, Lee J, Choi YW. Comparison of oral bioavailability of genistein and genistin in rats. Int J Pharm. 2007;337(1–2):148–154. doi: 10.1016/j.ijpharm.2006.12.046. [DOI] [PubMed] [Google Scholar]
- 310.Kim KH, Dodsworth C, Paras A, Burton BK. High dose genistein aglycone therapy is safe in patients with mucopolysaccharidoses involving the central nervous system. Mol Genet Metab. 2013;109(4):382–385. doi: 10.1016/j.ymgme.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 311.Setchell KD, Brown NM, Desai P, Zimmer-Nechemias L, Wolfe BE, Brashear WT, Kirschner AS, Cassidy A, Heubi JE. Bioavailability of pure isoflavones in healthy humans and analysis of commercial soy isoflavone supplements. J Nutr. 2001;131(4 Suppl):1362s–1375s. doi: 10.1093/jn/131.4.1362S. [DOI] [PubMed] [Google Scholar]
- 312.Ullmann U, Oberwittle H, Grossmann M, Riegger C. Repeated oral once daily intake of increasing doses of the novel synthetic genistein product Bonistein in healthy volunteers. Planta Med. 2005;71(10):891–896. doi: 10.1055/s-2005-864186. [DOI] [PubMed] [Google Scholar]
- 313.Rusin A, Krawczyk Z, Grynkiewicz G, Gogler A, Zawisza-Puchalka J, Szeja W. Synthetic derivatives of genistein, their properties and possible applications. Acta Biochim Pol. 2010;57(1):23–34. [PubMed] [Google Scholar]
- 314.Ullah MF, Shamim U, Hanif S, Azmi AS, Hadi SM. Cellular DNA breakage by soy isoflavone genistein and its methylated structural analogue biochanin A. Mol Nutr Food Res. 2009;53(11):1376–1385. doi: 10.1002/mnfr.200800547. [DOI] [PubMed] [Google Scholar]
- 315.Byczek A, Gruca JZ-PA, Papaj K, Grynkiewicz G, Rusin M, Szeja W, Rusin A. Genistein Derivatives Regioisomerically Substituted at 7-O- and 4'-O- Have Different Effect on the Cell Cycle. Journal of Chemistry. 2013 [Google Scholar]
- 316.Li QS, Li CY, Li ZL, Zhu HL. Genistein and its synthetic analogs as anticancer agents. Anticancer Agents Med Chem. 2012;12(3):271–281. doi: 10.2174/187152012800228788. [DOI] [PubMed] [Google Scholar]
- 317.Polkowski K, Popiolkiewicz J, Krzeczynski P, Ramza J, Pucko W, Zegrocka-Stendel O, Boryski J, Skierski JS, Mazurek AP, Grynkiewicz G. Cytostatic and cytotoxic activity of synthetic genistein glycosides against human cancer cell lines. Cancer Lett. 2004;203(1):59–69. doi: 10.1016/j.canlet.2003.08.023. [DOI] [PubMed] [Google Scholar]
- 318.Rusin A, Gogler A, Glowala-Kosinska M, Bochenek D, Gruca A, Grynkiewicz G, Zawisza J, Szeja W, Krawczyk Z. Unsaturated genistein disaccharide glycoside as a novel agent affecting microtubules. Bioorg Med Chem Lett. 2009;19(17):4939–4943. doi: 10.1016/j.bmcl.2009.07.089. [DOI] [PubMed] [Google Scholar]
- 319.Rusin A, Zawisza-Puchalka J, Kujawa K, Gogler-Piglowska A, Wietrzyk J, Switalska M, Glowala-Kosinska M, Gruca A, Szeja W, Krawczyk Z, Grynkiewicz G. Synthetic conjugates of genistein affecting proliferation and mitosis of cancer cells. Bioorg Med Chem. 2011;19(1):295–305. doi: 10.1016/j.bmc.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 320.Rusin A, C M, Papaj K, Grynkiewicz G, Szeja W. C-Glycosidic genistein conjugates and their antiproliferative activity. Journal of Chemistry. 2013;14 [Google Scholar]
- 321.Gogler-Piglowska A, Rusin A, Bochenek D, Krawczyk Z. Aneugenic effects of the genistein glycosidic derivative substituted at C7 with the unsaturated disaccharide. Cell Biol Toxicol. 2012;28(5):331–342. doi: 10.1007/s10565-012-9227-9. [DOI] [PubMed] [Google Scholar]
- 322.Aggarwal BB, Ichikawa H. Molecular targets and anticancer potential of indole-3-carbinol and its derivatives. Cell Cycle. 2005;4(9):1201–1215. doi: 10.4161/cc.4.9.1993. [DOI] [PubMed] [Google Scholar]
- 323.Safe S, Papineni S, Chintharlapalli S. Cancer chemotherapy with indole-3-carbinol, bis(3'-indolyl)methane and synthetic analogs. Cancer Lett. 2008;269(2):326–338. doi: 10.1016/j.canlet.2008.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Weng JR, Tsai CH, Kulp SK, Wang D, Lin CH, Yang HC, Ma Y, Sargeant A, Chiu CF, Tsai MH, Chen CS. A potent indole-3-carbinol derived antitumor agent with pleiotropic effects on multiple signaling pathways in prostate cancer cells. Cancer Res. 2007;67(16):7815–7824. doi: 10.1158/0008-5472.CAN-07-0794. [DOI] [PubMed] [Google Scholar]
- 325.Kim DS, Jeong YM, Moon SI, Kim SY, Kwon SB, Park ES, Youn SW, Park KC. Indole-3-carbinol enhances ultraviolet B-induced apoptosis by sensitizing human melanoma cells. Cell Mol Life Sci. 2006;63(22):2661–2668. doi: 10.1007/s00018-006-6306-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Kim SY, Kima DS, Jeong YM, Moon SI, Kwon SB, Park KC. Indole-3-carbinol and ultraviolet B induce apoptosis of human melanoma cells via down-regulation of MITF. Pharmazie. 2011;66(12):982–987. [PubMed] [Google Scholar]
- 327.Aronchik I, Kundu A, Quirit JG, Firestone GL. The Anti-proliferative Response of Indole-3-carbinol in human melanoma cells is Triggered by an Interaction with NEDD4-1 and Disruption of Wild-type PTEN Degradation. Mol Cancer Res. 2014 doi: 10.1158/1541-7786.MCR-14-0018. 10.1158/1541-7786.mcr-14-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Christensen JG, LeBlanc GA. Reversal of multidrug resistance in vivo by dietary administration of the phytochemical indole-3-carbinol. Cancer Res. 1996;56(3):574–581. [PubMed] [Google Scholar]
- 329.Leibelt DA, Hedstrom OR, Fischer KA, Pereira CB, Williams DE. Evaluation of chronic dietary exposure to indole-3-carbinol and absorption-enhanced 3,3'-diindolylmethane in sprague-dawley rats. Toxicol Sci. 2003;74(1):10–21. doi: 10.1093/toxsci/kfg103. [DOI] [PubMed] [Google Scholar]
- 330.Reed GA, Arneson DW, Putnam WC, Smith HJ, Gray JC, Sullivan DK, Mayo MS, Crowell JA, Hurwitz A. Single-dose and multiple-dose administration of indole-3-carbinol to women: pharmacokinetics based on 3,3'-diindolylmethane. Cancer Epidemiol Biomarkers Prev. 2006;15(12):2477–2481. doi: 10.1158/1055-9965.EPI-06-0396. [DOI] [PubMed] [Google Scholar]
- 331.Chintharlapalli S, Papineni S, Baek SJ, Liu S, Safe S. 1,1-Bis(3'-indolyl)-1-(p-substitutedphenyl)methanes are peroxisome proliferator-activated receptor gamma agonists but decrease HCT-116 colon cancer cell survival through receptor-independent activation of early growth response-1 and nonsteroidal anti-inflammatory drug-activated gene-1. Mol Pharmacol. 2005;68(6):1782–1792. doi: 10.1124/mol.105.017046. [DOI] [PubMed] [Google Scholar]
- 332.Chintharlapalli S, Smith R, 3rd, Samudio I, Zhang W, Safe S. 1,1-Bis(3'-indolyl)-1-(p-substitutedphenyl)methanes induce peroxisome proliferator-activated receptor gamma-mediated growth inhibition, transactivation, and differentiation markers in colon cancer cells. Cancer Res. 2004;64(17):5994–6001. doi: 10.1158/0008-5472.CAN-04-0399. [DOI] [PubMed] [Google Scholar]
- 333.Contractor R, Samudio IJ, Estrov Z, Harris D, McCubrey JA, Safe SH, Andreeff M, Konopleva M. A novel ring-substituted diindolylmethane,1,1-bis[3'-(5-methoxyindolyl)]-1-(p-t-butylphenyl) methane, inhibits extracellular signal-regulated kinase activation and induces apoptosis in acute myelogenous leukemia. Cancer Res. 2005;65(7):2890–2898. doi: 10.1158/0008-5472.CAN-04-3781. [DOI] [PubMed] [Google Scholar]
- 334.Kassouf W, Chintharlapalli S, Abdelrahim M, Nelkin G, Safe S, Kamat AM. Inhibition of bladder tumor growth by 1,1-bis(3'-indolyl)-1-(p-substitutedphenyl)methanes: a new class of peroxisome proliferator-activated receptor gamma agonists. Cancer Res. 2006;66(1):412–418. doi: 10.1158/0008-5472.CAN-05-2755. [DOI] [PubMed] [Google Scholar]
- 335.Qin C, Morrow D, Stewart J, Spencer K, Porter W, Smith R, 3rd, Phillips T, Abdelrahim M, Samudio I, Safe S. A new class of peroxisome proliferator-activated receptor gamma (PPARgamma) agonists that inhibit growth of breast cancer cells: 1,1-Bis(3'-indolyl)-1-(p-substituted phenyl)methanes. Mol Cancer Ther. 2004;3(3):247–260. [PubMed] [Google Scholar]
- 336.Jong L, C W. In: Analogs of indole-3-carbinol metabolites as chemotherapeutic and chemopreventive agents. U S, editor. 2004. [Google Scholar]
- 337.Jong L, C W. In: Analogs of indole-3-carbinol metabolites as chemotherapeutic and chemopreventive agents. U S, editor. 2006. [Google Scholar]
- 338.Brandi G, Paiardini M, Cervasi B, Fiorucci C, Filippone P, De Marco C, Zaffaroni N, Magnani M. A new indole-3-carbinol tetrameric derivative inhibits cyclin-dependent kinase 6 expression, and induces G1 cell cycle arrest in both estrogen-dependent and estrogen-independent breast cancer cell lines. Cancer Res. 2003;63(14):4028–4036. [PubMed] [Google Scholar]
- 339.Weng JR, Omar HA, Kulp SK, Chen CS. Pharmacological exploitation of indole-3-carbinol to develop potent antitumor agents. Mini Rev Med Chem. 2010;10(5):398–404. doi: 10.2174/138955710791330945. [DOI] [PubMed] [Google Scholar]
- 340.Jump SM, Kung J, Staub R, Kinseth MA, Cram EJ, Yudina LN, Preobrazhenskaya MN, Bjeldanes LF, Firestone GL. N-Alkoxy derivatization of indole-3-carbinol increases the efficacy of the G1 cell cycle arrest and of I3C-specific regulation of cell cycle gene transcription and activity in human breast cancer cells. Biochem Pharmacol. 2008;75(3):713–724. doi: 10.1016/j.bcp.2007.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Nguyen HH, Lavrenov SN, Sundar SN, Nguyen DH, Tseng M, Marconett CN, Kung J, Staub RE, Preobrazhenskaya MN, Bjeldanes LF, Firestone GL. 1-Benzyl-indole-3-carbinol is a novel indole-3-carbinol derivative with significantly enhanced potency of anti-proliferative and anti-estrogenic properties in human breast cancer cells. Chem Biol Interact. 2010;186(3):255–266. doi: 10.1016/j.cbi.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Lopez-Lazaro M. Distribution and biological activities of the flavonoid luteolin. Mini Rev Med Chem. 2009;9(1):31–59. doi: 10.2174/138955709787001712. [DOI] [PubMed] [Google Scholar]
- 343.Horibe I, Satoh Y, Shiota Y, Kumagai A, Horike N, Takemori H, Uesato S, Sugie S, Obata K, Kawahara H, Nagaoka Y. Induction of melanogenesis by 4'-O-methylated flavonoids in B16F10 melanoma cells. J Nat Med. 2013;67(4):705–710. doi: 10.1007/s11418-012-0727-y. [DOI] [PubMed] [Google Scholar]
- 344.Choi MY, Song HS, Hur HS, Sim SS. Whitening activity of luteolin related to the inhibition of cAMP pathway in alpha-MSH-stimulated B16 melanoma cells. Arch Pharm Res. 2008;31(9):1166–1171. doi: 10.1007/s12272-001-1284-4. [DOI] [PubMed] [Google Scholar]
- 345.Ruan JS, Liu YP, Zhang L, Yan LG, Fan FT, Shen CS, Wang AY, Zheng SZ, Wang SM, Lu Y. Luteolin reduces the invasive potential of malignant melanoma cells by targeting beta3 integrin and the epithelial-mesenchymal transition. Acta Pharmacol Sin. 2012;33(10):1325–1331. doi: 10.1038/aps.2012.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Casagrande F, Darbon JM. Effects of structurally related flavonoids on cell cycle progression of human melanoma cells: regulation of cyclin-dependent kinases CDK2 and CDK1. Biochem Pharmacol. 2001;61(10):1205–1215. doi: 10.1016/s0006-2952(01)00583-4. [DOI] [PubMed] [Google Scholar]
- 347.George VC, Naveen Kumar DR, Suresh PK, Kumar S, Kumar RA. Comparative studies to evaluate relative in vitro potency of luteolin in inducing cell cycle arrest and apoptosis in HaCaT and A375 cells. Asian Pac J Cancer Prev. 2013;14(2):631–637. doi: 10.7314/apjcp.2013.14.2.631. [DOI] [PubMed] [Google Scholar]
- 348.Horvathova K, Chalupa I, Sebova L, Tothova D, Vachalkova A. Protective effect of quercetin and luteolin in human melanoma HMB-2 cells. Mutat Res. 2005;565(2):105–112. doi: 10.1016/j.mrgentox.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 349.Iwashita K, Kobori M, Yamaki K, Tsushida T. Flavonoids inhibit cell growth and induce apoptosis in B16 melanoma 4A5 cells. Biosci Biotechnol Biochem. 2000;64(9):1813–1820. doi: 10.1271/bbb.64.1813. [DOI] [PubMed] [Google Scholar]
- 350.Nakashima S, Matsuda H, Oda Y, Nakamura S, Xu F, Yoshikawa M. Melanogenesis inhibitors from the desert plant Anastatica hierochuntica in B16 melanoma cells. Bioorg Med Chem. 2010;18(6):2337–2345. doi: 10.1016/j.bmc.2010.01.046. [DOI] [PubMed] [Google Scholar]
- 351.Shimoi K, Okada H, Furugori M, Goda T, Takase S, Suzuki M, Hara Y, Yamamoto H, Kinae N. Intestinal absorption of luteolin and luteolin 7-O-beta-glucoside in rats and humans. FEBS Lett. 1998;438(3):220–224. doi: 10.1016/s0014-5793(98)01304-0. [DOI] [PubMed] [Google Scholar]
- 352.Cheng L, Tan H, Wu X, Hu R, Aw C, Zhao M, Shen HM, Lu Y. Novel synthetic luteolin analogue-caused sensitization of tumor necrosis factor-alpha-induced apoptosis in human tumor cells. Org Biomol Chem. 2008;6(22):4102–4104. doi: 10.1039/b813904k. [DOI] [PubMed] [Google Scholar]