Abstract
Weight-dependent loading of the skeleton plays an important role in establishing and maintaining bone mass and strength. This review focuses on mechanical signaling induced by body weight as an essential mechanism for maintaining bone health. In addition, the skeletal effects of deviation from normal weight are discussed. The magnitude of mechanical strain experienced by bone during normal activities is remarkably similar among vertebrates, regardless of size, supporting the existence of a conserved regulatory mechanism, or mechanostat, that senses mechanical strain. The mechanostat functions as an adaptive mechanism to optimize bone mass and architecture based on prevailing mechanical strain. Changes in weight, due to altered mass, weightlessness (spaceflight), and hypergravity (modeled by centrifugation), induce an adaptive skeletal response. However, the precise mechanisms governing the skeletal response are incompletely understood. Furthermore, establishing whether the adaptive response maintains the mechanical competence of the skeleton has proven difficult, necessitating development of surrogate measures of bone quality. The mechanostat is influenced by regulatory inputs to facilitate non-mechanical functions of the skeleton, such as mineral homeostasis, as well as hormones and energy/nutrient availability that support bone metabolism. While the skeleton is very capable of adapting to changes in weight, the mechanostat has limits. At the limits, extreme deviations from normal weight and body composition are associated with impaired optimization of bone strength to prevailing body size.
Keywords: Osteoporosis, mechanical strain, fracture risk, weight change, leptin
Introduction
The skeleton is a complex multifunctional organ system which, in adults, is comprised of 206 bones. The acquisition of bone mass occurs primarily during childhood and the decade following puberty with peak bone mass achieved in the 3rd to 4th decade of life (Baxter-Jones, et al. 2011). Bone loss may be an inevitable consequence of aging. However, the rate of loss has been shown to differ greatly among individuals (Cauley, et al. 2009). Low peak bone mass and excessive age-related bone loss predisposes individuals to osteoporosis, an important underlying risk factor for fragility fractures (Chevalley, et al. 2012). Factors influencing skeletal dynamics over the lifecycle are under investigation; the usual suspects, including genetic variation, disturbed mineral homeostasis, gender, reproductive status, diet, physical activity, and body weight have each been shown to be important. However, in spite of major advances, current understanding is inadequate to fully explain all of the variation in fracture risk.
Physical attributes and physiological functions vary among individual bones and among skeletal compartments within a bone. Bone provides a stiff structure required for locomotion, acts as a physical barrier for protection of vital organs, provides a hospitable environment for hematopoietic cell maturation, is an important adipose tissue depot, is an endocrine organ, and a dependable and rapidly mobilizable reservoir for calcium and other minerals. Significant throughout life, the mineral depot in bone is particularly important during catabolic conditions such as late pregnancy, lactation and prolonged fasting. The skeleton influences and is, in turn, influenced by tissues within the bone marrow (hematopoietic, adipose and immune), adjacent tissues (muscle, cartilage, tendons and ligaments), and remote tissues (endocrine, gastrointestinal, kidney, sensory and sympathetic nervous systems). As a consequence of competing responsibilities and regulatory inputs, optimization of bone mass, architecture and turnover for one function could potentially compromise other critical functions (Turner 2001). This can be illustrated by considering the skeletal response to inadequate dietary calcium. Failure to maintain levels of ionic calcium within narrow limits has immediate, potentially life threatening consequences. Although the skeleton nearly always contains mineral reserves sufficient to balance serum calcium requirements, the resulting bone loss associated with chronic suboptimal dietary calcium will likely reduce the mechanical competence of bone and increase fracture risk. Similarly, pathologies such as hemophilia and anemia involving marrow can place demands on the skeleton that can compromise its mechanical function. Specifically, chronic anemia results in reduced BMD and increased fracture risk due to osteoclast-mediated expansion of the bone marrow cavity in response to increased need for hematopoiesis (Almeida and Roberts 2005; Perisano, et al. 2012; Recht, et al. 2013; Vogiatzi, et al. 2005). The high rate of fragility fractures in the aged, with an annual rate of over nine million worldwide, testifies to the inability of the skeleton to always maintain sufficient mechanical competence (Kanis, et al. 2012).
Body weight can influence a multitude of physiological functions. Not surprisingly, there is a close association between bone mass and weight during growth, and preservation of this relationship throughout life is vital to bone health. The direct pathway for weight to influence bone is via mechanical loading. This review focuses on mechanical signaling as an essential mechanism for coupling bone mass to changes in body weight during growth and adulthood. The influence of weight change, ranging from weightlessness to hypergravity, is also considered. Finally, factors that result in disturbances in the relationship between weight and bone mass are discussed. For additional perspectives, please see reviews by Dimitri et al. and Shapses and Sukumar (Dimitri, et al. 2012; Shapses and Sukumar 2012).
Mechanical Loading and Skeletal Adaptation: Mechanostat Theory
The skeleton serves multiple mechanical functions: 1) application of mechanical forces (e.g., jaws, fingers); 2) resisting mechanical forces (e.g., weight bearing bones); 3) providing a scaffold for the attachment of ligaments and tendons required for locomotion (e.g., long bones), and 4) protecting vital organs (e.g., ribs, vertebrae and skull). Body weight exhibits minimal day to day variation. However, static load and the resulting deformation of bone (mechanical strain) generated by weight depend upon posture. For example, standing on one leg places a higher load on weight bearing bones of the lower limb than standing on both legs, while transferring to a sitting or lying prone position alters the direction as well as reduces the magnitude of limb loading. These forms of skeletal loading are static; the loads are ≤ body weight and occur over sustained durations of seconds or longer. The larger mechanical loads applied during physical activities such as walking subject loaded bones to higher peak strain levels. Skeletal loading associated with physical activity is dynamic because loads change rapidly in magnitude and direction and peak strain is maintained for short durations (ms). During walking, the lower limbs are subjected to peak loads equivalent to ~ 1.5 × body weight with the interval between strides being ~1 Hz (1 cycle/s) (Al Nazer, et al. 2008; Fritton, et al. 2000). More intense physical activates, such as those that occur in many sports, place even greater strains on loaded portions of the skeleton.
The maximum mechanical strain levels in bone during activities of normal living are well below levels capable of inducing catastrophic failure. Furthermore, the magnitude of strain during normal activities is remarkably similar among vertebrates, regardless of size, supporting the existence of a conserved regulatory mechanism, or mechanostat, that senses strain (Rubin and Lanyon 1984). When peak strain levels deviate above or below this set point, a compensatory mechanism is initiated which results in addition of bone due to excessive strain or removal of bone due to insufficient strain, maintaining a low risk for catastrophic failure without incurring the metabolic costs associated with forming and maintaining unnecessary bone (Figure 1).
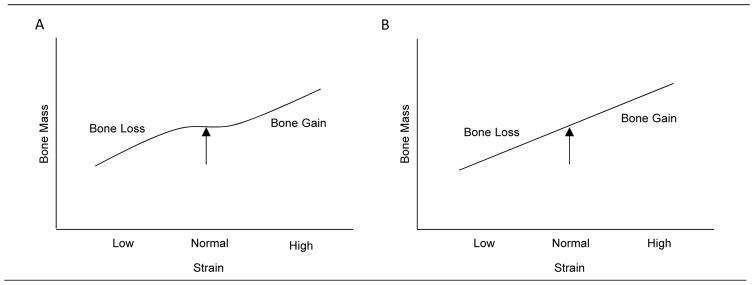
Figure 1.
The mechanostat is hypothesized as a mechanism that regulates bone mass in response to changes in mechanical strain. As originally envisioned (A), strain levels consistently falling below the lower boundary lead to an adaptive response where bone is lost, increasing strain. Strain levels consistently exceeding the upper boundary lead to an adaptive response where bone is gained, decreasing strain. Based on this model there is a zone between upper and lower boundaries where strain differences do not evoke an adaptive response (Frost 1987). An alternative model has been proposed (B) where strain levels below or above a set point that is bone specific evokes an adaptive response (Skerry 2006). While some studies suggest that moderate weight changes need not evoke an adaptive response (see text) other findings are consistent with the alternative model (see Figure 2).
The mechanostat model predicts that incremental overall increases in weight can increase bone mass and alter bone architecture by inducing an adaptive response to increased mechanical loads. Lean mass may have additional importance as a contributor to weight-dependent skeletal loading because muscles are attached to bone via tendons and larger and more powerful muscles can deliver greater mechanical loads directly to bone. We emphasize “can” because mechanostat-mediated adaptations, as originally envisioned, only occur when an upper or lower threshold strain is violated (Frost 1987). However, recent studies performed in mice suggest that the skeleton’s adaptive response to mechanical loading is essentially linear over a wide range of strain (Figure 1) (Sugiyama, et al. 2012). This finding is supported by the strong association between weight and bone mass in mice (Figure 2).
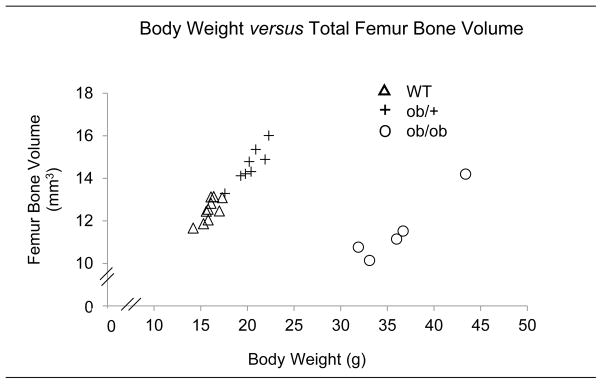
Figure 2.
Leptin alters the sensitivity of the skeleton to body weight changes. Total femur mass is strongly associated with body weight in 7-week-old female WT, partially leptin deficient ob/+, and leptin-deficient ob/ob mice fed a normal diet. ob/+ have near normal leptin levels due to increased fat mass and demonstrate an association between body weight and bone mass nearly identical to WT mice. In contrast, ob/ob mice require a much higher body weight to achieve a bone mass equivalent to WT. Please note that the slope of the regression lines is less than unity (0.49 for WT and ob/+ mice and 0.34 for ob/ob mice); increasing body weight by 50% in a WT mouse would be expected to lead to ~25% increase in bone mass. Reproduced, with permission, from Philbrick KA, Turner RT, Branscum AJ, Wong CP & Iwaniec UT (2015) Paradoxical effects of partial leptin deficiency on bone in growing female mice, The Anatomical Record 298 2018–2029. Copyright 2015 Wiley Periodicals, Inc.
The mechanostat functions to help “optimize” the ability of bone to resist loads conferred by activities of normal living but not the atypical loads often experienced during falls (Silva 2007). This is important because atypical loads are responsible for the majority of low trauma fractures in children and the elderly. In this regard, the highest rates of fractures due to falling occur in prepubertal boys and elderly women, indicating that the skeleton exhibits a low safety factor (failure load/peak load) in these two groups.
Changes in weight necessarily precede skeletal adaptation to changes in mechanical loads. This delay in adaptive response may contribute to the high fracture rate in rapidly growing children. Additionally, the dynamics of bone structure change immediately prior to and during pubertal growth may partially explain the high rate of fractures. During rapid growth, addition of bone to periosteal bone surfaces is slow compared to bone elongation, resulting in inadequate cortical thickness for bone length (Clark, et al. 2006; Rauch 2012). Overweight children appear to be especially prone to fracture (Cole, et al. 2012; Dimitri, et al. 2014). Studies employing high resolution peripheral quantitative computed tomography (HR-pQCT) and finite element analyses suggest that although childhood obesity alters radial and tibial microstructure, these adaptations are inadequate to compensate for the increased loading potential from a fall (Dimitri, et al. 2015; Kim, et al. 2013). While higher body weight can increase mechanical loading on bone and, as a consequence, increase bone mass or alter microarchitecture to improve bone quality, it also has the potential to increase the magnitude of atypical loads that are often responsible for a fracture. Thus, weight-associated increases in mechanical strain would lower the safety factor until skeletal adaptation is completed.
Bones change in size, mass, density and architecture through the processes of growth, modeling and remodeling. Most bones grow in length through endochondral ossification where primary spongiosa created by osteoclast-mediated resorption of calcified cartilage is replaced by bone through osteoblast-mediated deposition of bone matrix. Bones also grow in size due to osteoblasts depositing bone matrix onto the periosteal surface. Modeling refers to changes in bone architecture where bone is added to a preexisting bone surface without a requirement for prior bone resorption or by which bone is resorbed from a bone surface without initiating subsequent bone formation. Remodeling is initiated when osteoclasts are recruited to quiescent bone surfaces where they degrade bone. Osteoblasts are then recruited to the resorption site where they secrete matrix that undergoes mineralization to form bone to complete a remodeling cycle. When bone formation is tightly coupled to bone resorption there is minimal change in bone architecture following completion of bone remodeling. In the process of bone formation during growth, modeling, or remodeling, some osteoblasts become quiescent lining cells while others are incorporated into bone matrix and become osteocytes.
Osteocytes, through their intricate network of lacunae and interconnecting canaliculi, play an essential role in mechanosignal transduction. Osteocytes embedded in a mineralized matrix experience strain-induced interstitial fluid flow and fluid shear stress resulting in activation of signaling pathways that regulate bone turnover (Govey, et al. 2015). Mechanoreceptors on osteocytes fall into 3 general classes; ion channels, G-protein-coupled receptors, and cytoskeletal/integrin complexes (Robling 2012). Mechanoactivation of these receptors on osteocytes results in transduction of signals to cells lining bone surfaces that communicate mechanical strain magnitude and distribution.
Bone lining cells and osteoblasts cover the majority of bone surfaces and are interconnected by gap junctions, allowing intracellular communication via ions and small molecules. Gap junctions and ion channels are also used to communicate signals from osteocytes to osteoblast lineage cells (Lloyd, et al. 2014). Additionally, osteocytes generate soluble factors, including FGF-23, sclerostin, RANKL and DKK-1 that regulate bone turnover (Goldring 2015). Several mechanically regulated intracellular signaling cascades have been described, including activation of kinases (Akt, MAPK, FAK), β-catenin, GTPases, and calcium signaling (Thompson, et al. 2012). Additionally, nitric oxide signaling (Klein-Nulend, et al. 2014) and BMP signaling (Kopf, et al. 2014) play important roles in the skeletal response to mechanical loads.
The signaling pathways mentioned above are not unique to mechanoregulation (Price, et al. 2011) and the state of our knowledge is inadequate to accurately predict the skeletal consequences of manipulating individual pathways. To date, the effects of mechanical signaling on the human skeleton have been studied primarily by altering the applied loads. This is accomplished by increasing physical activity or by evaluating the skeletal response to changes in body weight. Based on extensive observational and intervention studies in humans and animal models, several principles emerge (Skerry 2006): 1) the skeleton responds to mechanical strain stimulus but the strain stimulus is different in different parts of the skeleton; 2) peak strain magnitude, duration, rate of change and frequency are among the important variables that impact mechanosignal transduction; 3) the efficacy of the mechanostat in maintaining bone mass and quality diminishes with age; and 4) mechanical signal transduction can be influenced by systemic factors such as hormones, cytokines and nutritional status.
Peak strain is dependent upon the magnitude of force applied to bone. Force is, in turn, proportional to mass and velocity. Changing either parameter will change strain, which in turn has the potential to influence bone microarchitecture. Increasing mechanical strain has been used as a strategy to develop biomechanical-based interventions to improve bone health (Rittweger 2008). Increasing mechanical strain to increase bone mass has been found to be more effective prior to puberty than in adults (Gunter, et al. 2008). High impact loading during jumping (increased velocity) has proven to be effective in increasing bone mass in children in part by increasing bone size. Importantly, this form of high impact exercise was shown to confer lasting benefit (Gunter et al. 2008). In adults, increasing mechanical loading by wearing weighted vests (increased mass) does not increase bone mass but appears to slow age-related bone loss (Snow, et al. 2000).
Weightlessness
The importance of static and dynamic weight bearing on the skeleton has been investigated in humans and animals subjected to spaceflight or ground-based models for spaceflight. An astronaut in low Earth orbit is essentially weightless due to the astronaut and surroundings being uniformly accelerated towards Earth. Although mass of the astronaut remains constant, static and dynamic loading of the skeleton essentially cease because there is no net external force to induce changes in strain energy within bone tissue. In ground-based models for weightlessness (hindlimb unweighting), dynamic and static loading of portions of the skeleton are reduced (Morey, et al. 1979).
Astronauts typically lose bone during exposure to weightlessness, but the pattern of bone loss shows considerable site-specificity (Orwoll, et al. 2013; Sibonga 2013). In general, bone loss is confined to sites subjected to high levels of dynamic weight bearing. Bone mineral density (BMD) in crewmembers aboard the International Space Station (ISS) showed precipitous declines at weight-bearing sites, including the hip and spine after a typical 6-mo mission but negligible impact at many other skeletal sites (Sibonga, et al. 2015). Forces measured during treadmill walking and running on the ISS, using in-shoe monitors, were reduced by 25% and 46%, respectively, compared to similar activities on Earth. A mean calculated decrease of 25% in the daily load experienced by the lower extremity was associated with BMD decreases of 0.7% and 0.8% per month in the femoral neck and lumbar spine, respectively (Cavanagh, et al. 2010). The rate of bone loss observed in these male astronauts greatly exceeds the rapid bone loss observed in women following menopause. Long-duration bed rest also results in bone loss (Spector, et al. 2009). In addition to bone loss, bed rest results in an increase in marrow adipose tissue (MAT) (Trudel, et al. 2009). MAT has not been investigated in astronauts but has been shown to increase in rats subjected to weightlessness and hindlimb unweighting (Jee, et al. 1983; Keune, et al. 2016; Tian, et al. 2011). The similarity in skeletal response to weightlessness and ground-based models for weightlessness argue that static loads generated by weight have little direct effect on the skeleton whereas dynamic loads have important site-specific effects.
Human spaceflight and long-duration bedrest studies have been performed exclusively in adults. Thus, they provide little insight into the role of weight on bone accrual during growth. On the other hand, animal studies focusing on the skeletal effects of weightlessness have generally been performed in growing rodents, initially rats and more recently mice (Keune, et al. 2015; Turner 2000). Of key importance to this review is the observed reduction of bone accrual onto periosteal surfaces of weight-bearing long bones during weightlessness followed by normalization upon reweighting (Sessions, et al. 1989). Additionally, site-specific reductions in cancellous bone mass have been reported following weightlessness in rodents and astronauts (Keune et al. 2015; Vico, et al. 2000). Furthermore, the deficiency in bone accrual was shown to have a negative effect on bone strength (Sessions et al. 1989). Taken together, studies in humans and animals provide strong evidence that weight-dependent mechanical loading of the skeleton plays an important role in establishing and maintaining bone mass and strength.
Rodent studies provide insight into whether the mechanostat is sufficient to fully account for the tight coupling between bone mass and body weight. Bone length is an important determinant of bone mass but weightlessness had no effect on longitudinal bone growth (Sibonga, et al. 2000). Additionally, a strong interaction between weight and estrogen status was identified (Luo, et al. 2000; Westerlind, et al. 1997). Subsequent ground-based studies in mice further suggest an important role of estrogen receptor signaling in mechanotransduction (Galea, et al. 2013; Melville, et al. 2015). Finally, although weightlessness and reweighting impact bone mass in opposing directions, the kinetics differ; the time course for bone mass changes during unloading is much more rapid than reloading, implying that factors in addition to mechanostat signaling are involved in mediating skeletal adaptation to changes in weight.
Astronauts are healthy and physically active when subjected to weightlessness. They remain physically active yet experience dramatic site-specific bone loss in only 4–6 months. The rate of recovery of BMD following restoration of normal weight bearing is much slower than the rate of loss; recovery approximates an exponential function with 50% restoration of bone requiring ~9 months and complete restoration requiring several years (Sibonga, et al. 2007). This slow recovery occurs in spite of immediate restoration of normal skeletal loading. Similar findings regarding rapid skeletal changes during weightlessness and slow recovery have been reported in rodents (Sessions et al. 1989). These findings suggest that the rate of skeletal adaptation to weight change may depend on the direction as well as magnitude of weight change.
Hypergravity
Weight is the product of mass and acceleration, the latter typically being the net acceleration imparted by gravity. However, an individual located within an isolated compartment cannot distinguish force imparted by the action of gravity from force imparted by a mechanical device. Hypergravity refers to a force that exceeds that of gravity and is modeled in humans and animals using centrifugation. Hypergravity has been used to investigate physiological adaptation to changes in weight. Male mice subjected to a 2-fold increase in weight for 21 days exhibited decreased osteoclast surface and increased osteoblast surface in femur and vertebra, resulting in increased cancellous bone (Gnyubkin, et al. 2015). Also, increasing weight 2.8-fold increased femur density in female rats during a long-duration (810 d) study (Jaekel, et al. 1977). Increasing body weight 3-fold had detrimental effects on the skeleton of mice but these data are more difficult to interpret because body mass increment slowed compared to normally housed controls, suggesting that the adaptive response to weight are antagonized by physiological stress.
The effect of long-duration continuous hypergravity on the human skeleton is unknown. However, the effects of transient increases of 2–6 × body weight in young men during 12 months of training to fly high performance aircraft have been reported. Increases in thoracic spine (11%), pelvis (4.9 %), and total body BMD (3.7%) were observed but no changes were noted in the pilots’ lumbar spine, arms or legs (Naumann, et al. 2001). These findings suggest that large but intermittent increases in ‘weight’ can have dramatic, effects on the human skeleton at sites subjected to increased mechanical loads.
Scaling Bone Mass to Body Weight
Studies performed in microgravity and hypergravity generally support the concept of a gravity continuum where the skeleton continuously adapts to changes in gravitational loading (Wade 2005). Weight generally continues to increase following cessation of linear growth but at a much slower rate, typically ≤0.25 kg/y (Weigle 1990). However, a parallel increase in BMD is not typically observed. A complicating factor in interpreting this apparent discrepancy with the concept of a gravity continuum is that fracture resistance is not solely dependent on BMD. Weight gain in adults is generally accompanied by changes in the relative proportions of lean tissue and fat tissue and changes in fat distribution. An important unanswered question is whether bone mass and quality is appropriate for adult-associated weight gain. Several methods have been used to adjust BMD for differences in body size in children and adults. In children, dual energy absorptiometry data have been adjusted using univariate and multivariate models that include age, weight, height, BMC, bone area, lean mass and fat mass as variables (Dimitri et al. 2012). Similar adjustments have been made in adults and in animal models with the simplest adjustment being dividing bone mass by body mass. None of these methods are completely satisfactory because the adjustments typically assume a uniform effect of weight on bone throughout the skeleton. This assumption is not supported by animal studies where bone mass, density and microarchitecture can be easily determined at multiple locations. Although a strong linear association was shown between body weight and bone mass in young male mice fed a normal diet, the slope of the linear regression was less than unity, indicating that heavier mice normally have less bone/g body weight than lighter mice (Figure 2). Also, the Pearson’s R value ranged from 0.55–0.88, depending upon skeletal site and age (Iwaniec, et al. 2009), indicating considerable variation in the response of individual bones and bone compartments to weight change during normal growth. In addition, BMD adjustments to weight provide little insight into the amount of bone required to provide equivalent mechanical competence in individuals who differ in weight.
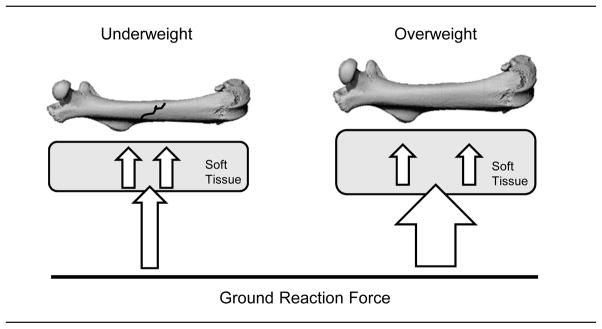
The material and mechanical properties of bone are often determined in animal models as a surrogate measure of fracture resistance. During mechanical testing, load (compression, tension, torsion, or bending) is applied directly to bone. This approach can be exquisitely sensitive. For humans, noninvasive imaging methods are being developed to predict bone strength (Bouxsein and Seeman 2009). However, the methods used in animal models and humans fail to account for the contribution of soft tissue attached to or located immediately adjacent to bone that deforms under mechanical load, thus effectively diminishing the load on bone (Figure 3). To determine fracture risk, it is necessary to account for the contribution of all tissues involved in dissipating loads during falls and other traumatic injury events. The ‘gold standard’ for evaluating skeletal loading in vivo is surgical implantation of strain gages onto bone surfaces (Meakin, et al. 2014). Unfortunately, strain measurements to determine whether skeletal adaptation in response to weight gain is appropriate to maintain mechanical competence have yet to be performed. A far less precise but clinically meaningful alternative is to evaluate the associations between weight, BMD and fracture prevalence.
Figure 3.
The complex relationship between BMI, BMD and fracture risk is illustrated in the schematic. Compared to an underweight individual, an overweight individual experiencing a fall from the same height would generate a proportionately greater load on a limb (ground reaction force). However, the presence of greater amount of soft tissue in the heavier individual should attenuate more of the load and distribute the remaining load over a larger bone surface, reducing peak strain such that the effective load could be greater in the lighter individual. Assuming equivalent bone quality, the higher BMD typical in the heavier individual would be a further advantage in reducing strain below that required for a fracture. However, based on epidemiological studies, further increases in weight may provide a diminishing return because the reductions in load during a fall related to soft tissue and higher BMD may not fully compensate for increased weight.
The prevalence of osteoporosis (defined by low BMD) in older men and women is inversely associated with body mass index (BMI, kg/m2) and this association is observed among diverse ethnicities. The prevalence of osteoporosis has been reported to decrease from 45% in underweight (BMI <18.5) to <1% in obese (BMI >30) women (Nielson, et al. 2012). Hip fracture prevalence was also shown to decrease with increased BMI in men and women. In women, the decrease was progressive; fracture rates decreased from 131 fractures/10,000 person years in underweight women to 50 fractures/10,000 person years in obese women. The relationship was less clear in men. Fracture rates decreased from 56 fractures/10,000 person years in underweight men to 30 fractures/10,000 person years in normal weight men but showed no additional change in the overweight and obese male populations. We interpret these findings as evidence that a higher body weight, at least partially, counteracts age-associated bone loss. It is, however, unlikely the higher BMD values in overweight and obese adults are exclusively due to a reduction in bone loss during aging. Obesity is associated with higher BMD throughout adulthood (Maïmoun, et al. 2015). Reciprocal changes have been observed in prevalence of obesity and hip fracture rates in the United States over several decades (Wright, et al. 2012). Although causality has not been established, weight gain during the same interval may have contributed to reduced hip fracture rates. Reduced fracture risk may not be the only positive benefit of excess weight; if fractures occur, obese and overweight subjects experience lower mortality rate (Prieto-Alhambra, et al. 2014).
Despite the generally positive effects of weight on bone health, excess weight may not always be beneficial. The impact of a higher BMI to reduce prevalence of osteoporosis (as defined by BMD) is greater than the contribution of increased BMI to reduce fracture prevalence. When adjusted for BMD (see previous text for caveats), the advantage of being overweight disappears, implying that the main positive impact of increased weight on fracture prevalence is an increase in BMD. At very high BMI adjusted fracture risk is increased, suggesting a reduction in bone quality (Nielson et al. 2012). Moreover, some obese men and women have unexpectedly low BMD (Greco, et al. 2010) and not all studies have found obesity to be protective against fractures (Compston, et al. 2011). There are several plausible explanations for the discrepant results. Most studies to date have not segregated the contributions of lean tissue and adipose tissue depots to BMI. This may be important because the contribution of muscle to skeletal loading includes the forces generated by muscle as well as weight, whereas the contribution of adipose tissue to skeletal loading is limited to weight. Adipose tissue can also influence bone as a consequence of the tissue’s endocrine function. The potential for dysregulation of bone due to excess adipose tissue will be discussed later.
Increased muscle mass and function is likely to contribute to the positive impact of higher BMI on bone health. Sarcopenic and dynopenic obese individuals appear to be at a greater risk for lower BMD and higher fracture risk than obese individuals with normal muscle mass and strength (Scott, et al. 2016). This interpretation is consistent with studies reporting that obese osteopenic individuals are at a higher fracture risk compared to normal weight osteopenic individuals (Cawsey, et al. 2015). Finally, sarcopenia and dynopenia could result in higher strain levels during a fall or increased fall frequency. Additional research focusing on muscle is required to evaluate these possibilities.
In summary, the full advantage of increasing weight on BMD or fracture rate may not extend to morbid obesity. Also, the precise relationship between weight and fracture rate may depend upon fracture type. Increased weight is generally associated with reduction in osteoporotic fractures (hip and vertebral) but in obese subjects there appears to be an increase in the less common upper arm and ankle fractures (Caffarelli, et al. 2014; Compston et al. 2011; Mpalaris, et al. 2015; Prieto-Alhambra, et al. 2012). In general, if weight gain leads to successful skeletal adaptation, as evidenced by an increase in BMD, fracture risk is reduced.
Weight Loss
Weight fluctuations >0.25 kg/y occur in adults and can impact BMD and bone turnover (Holbrook and Barrett-Connor 1993; Newman, et al. 2005; Von Thun, et al. 2014). Weight loss, particularly rapid weight loss induced by dieting, is generally associated with a decrease in BMD which is not completely restored following a regain in weight. Bariatric surgery is now commonly performed as an alternative to dieting to induce weight loss; in 2013 approximately a half million procedures were performed worldwide (Angrisani, et al. 2015). Not surprising, bone loss is a common negative side effect of bariatric surgery (Scibora 2014). Changes in bone microarchitecture, including reduced trabecular number suggest an accompanying reduction in bone strength (Frederiksen, et al. 2016). The reduction in BMD and strength may not be entirely due to weight loss and the magnitude of change varies with the surgical procedure (Hsin, et al. 2015). In this regard, bariatric surgery can negatively impact bone health due to impaired absorption of critical micronutrients and alterations in bone regulating hormones (Yu 2014).
The bone loss associated with weight loss can involve decreased bone formation and/or increased bone resorption (Rector, et al. 2009; Redman, et al. 2008; Shapses and Riedt 2006). Studies performed in rodents suggest that endocrine status is one of the factors that impact the cellular mechanisms for bone loss associated with skeletal unweighting. Cancellous bone loss in unweighted hindlimbs of normal male and female rats was due to decreased bone formation, but in ovariectomized rats was due to increased bone resorption (Hefferan, et al. 2003). Changes in energy intake are often responsible for changes in weight in adults. In skeletally mature mice, reducing energy to 60% of normal resulted in cortical bone loss in femur with preservation of cancellous bone (Hamrick, et al. 2008). As little as a 5% reduction in body weight in adult female rats induced by caloric restriction was accompanied by decreased bone formation, increased bone resorption and cancellous bone loss (Turner and Iwaniec 2011). These findings contrast with the lack of an effect of a 21% increase in body weight on bone mass, architecture and turnover in skeletally mature rats (Turner and Iwaniec 2010). The rapidity of the bone loss during severe caloric restriction as well as the failure of weight gain resulting from moderately increased energy intake to increase bone mass are not easily explained by mechanostat theory.
Energy Homeostasis
Several hormones are intimately associated with skeletal growth, maturation and turnover. These include pituitary-, gonadal-, thyroid- and adipocyte-derived hormones. Optimal growth is critically dependent upon adequate energy availability and energy insufficiency reduces secretion and/or antagonizes the actions of growth promoting hormones. The adipocyte-derived hormone leptin is of particular interest because there is strong evidence that leptin acts to regulate bone cell differentiation and function at multiple levels; via direct actions on skeletal tissues and indirectly through modulation of bone regulating hormones and energy homeostasis. There is also evidence that leptin plays a role in mechanostat signaling.
Leptin is produced primarily by adipocytes and leptin levels in blood are positively associated with adipose tissue mass (Friedman and Halaas 1998). The hormone crosses the blood brain barrier and acts at the hypothalamus to communicate the size of peripheral energy stores (Harris 2013). Notably, leptin acts to reduce appetite and increase energy expenditure (Ahima and Flier 2000). Leptin deficiency due to inactivation of the leptin (ob) gene results in morbid obesity (Campfield, et al. 1995; Montague, et al. 1997). The excess weight in leptin-deficient ob/ob mice is the result of a combination of hyperphagia and reduced thermogenesis (Hwa, et al. 1996). In addition, leptin deficiency in mice results in hypogonadism (Barkan, et al. 2005), elevated corticosteroid levels (Saito and Bray 1983), impaired thermoregulation (Trayhurn and James 1978) and impaired growth hormone signaling (Luque, et al. 2007). Thus, when leptin levels are very low, signaling low energy availability, key regulatory pathways required for growth and reproduction are suppressed and as a consequence, bone growth, maturation and turnover are impaired.
Obesity due to loss of function mutations in the gene for leptin or its receptor is very rare in humans. However, despite absence of leptin signaling and hypogonadism, bone age was accelerated in a pre-pubertal female child and BMD was increased in an older girl with loss of function mutation in the receptor for leptin (Hannema, et al. 2016). These findings contrast with individuals with low leptin production associated with anorexia or lipodystrophy. In these individuals very low leptin levels are associated with low BMD and leptin treatment was shown to increase bone mass (Mantzoros, et al. 2011; Sienkiewicz, et al. 2011). These divergent observations may be explained if metabolic changes secondary to and/or responsible for leptin deficiency impact bone metabolism. This conclusion is supported by studies performed in leptin-deficient ob/ob and partial leptin-deficient ob/+ mice where weight, adiposity and serum glucose levels were associated with important leptin-independent differences in bone mass, architecture and metabolism (Philbrick, et al. 2015; Turner, et al. 2014).
Leptin and Mechanosignaling
There is a positive association between body weight and bone mass in wildtype (WT) mice which is preserved in mice heterozygous (ob/+) for the obesity gene (Figure 2) (Philbrick et al. 2015). ob/+ mice have a reduced ability to generate leptin but compensate for this deficiency by increasing adipose tissue. Although there is also a positive association between body weight and total femur bone volume in ob/ob mice (Iwaniec et al. 2009), the presence of leptin appears to dramatically sensitize the skeletal response to increased body weight (Philbrick et al. 2015). This conclusion is supported by evidence that leptin modulates mechanosensitivity of the skeleton (Baek and Bloomfield 2009; Kapur, et al. 2010). However, other mechanisms are plausible. Estrogen alters the mechanosensitivity of the skeleton by increasing the set point at which bone responds to mechanical load (Luo et al. 2000). Since ob/ob mice are hypogonadal, low estrogen levels could contribute to the relative insensitivity of ob/ob mice to increased weight. Alternatively, it is possible that one or more cytokines produced by the abundant adipose tissue antagonize the positive effect of weight gain on bone mass in these mice.
Leptin attenuates the negative skeletal effects of unweighting and weight loss. Food restriction lowers serum leptin levels and enhances the negative effects of hindlimb unweighting (Baek, et al. 2008), which in turn are attenuated by leptin treatment (Baek and Bloomfield 2009). The positive effects of leptin appear to be mediated by peripheral leptin signaling because administering high levels of leptin into the hypothalamus not only resulted in weight loss and lower serum leptin levels but exaggerated bone loss in the non-weight bearing limbs of hindlimb unweighted rodents (Martin, et al. 2008). Weight loss typically results in decreased leptin levels (Hamann and Matthaei 1996), reduced bone accrual during growth (Devlin, et al. 2010), and accelerated age-related bone loss (Talbott, et al. 2001; Turner and Iwaniec 2011). Importantly, leptin treatment attenuates the inhibitory effects of caloric restriction on bone growth (Gat-Yablonski, et al. 2004; Goldstone, et al. 2002). Furthermore, leptin administered at supraphysiological levels was reported to maintain BMD despite inducing weight loss (Stunes, et al. 2012). These studies identify leptin as playing a key role in coupling bone metabolism to energy availability. Leptin appears to accomplish this role by a variety of mechanisms, including modulating mechanosignaling.
Dysfunction
The mechanostat is not infallible as witnessed by chronic bone loss in elderly women and men. The dramatic increase in atraumatic fractures, especially notable in women having low and normal BMI, implies that the mechanostat becomes less effective with advancing age in maintaining the biomechanical componence of the skeleton. Several explanations for this failure have been proposed, including a parallel age-associated decrease in muscle mass, reduced levels of physical activity and altered levels of bone regulating hormones (Faulkner, et al. 2007; Ribeiro and Kehayias 2014). Reductions in muscle mass and weight bearing physical activity clearly have the potential to decrease peak mechanical loads on the skeleton. The skeletal adaptation to reduced loading could then lower bone mass to a level that restores strain to pre-muscle loss levels. An age-related decrease in growth hormone secretion (Melmed 2013; Sattler 2013) contributes to muscle atrophy and bone loss in humans (Kuzma, et al. 2013), suggesting that growth hormone facilitates the mechanostat through its anabolic actions on bone. Notably, growth hormone had similar anabolic effects on bone in weight bearing and weightless rats (Turner 1995), a finding that suggests that reduced skeletal loading does not impair the skeletal response to growth hormone.
Gender differences are important to bone accrual during growth and bone loss during aging. Females accumulate more bone at puberty than is required to support the skeleton’s mechanical requirements (Wang, et al. 2015) and lose bone following menopause at a more rapid rate than aging males (Clarke and Khosla 2010). Postmenopausal bone loss is prevented with hormone replacement. There are multiple lines of evidence that estrogen acts physiologically to modulate the sensitivity of the mechanostat to mechanical loads. Bone in excess of the minimum required for mechanical function would be beneficial to provide minerals for bone development and growth during pregnancy and lactation (Clarke and Khosla 2010; Kovacs 2005). Animal studies further support an important role for estrogen in modulating the skeletal response to mechanical loading (Westerlind et al. 1997). Reduced dynamic loading (Turner, et al. 1998), and weightlessness (Keune et al. 2015) result in bone- and bone-compartment specific further bone loss in estrogen-deficient rats. Increased skeletal loading can attenuate estrogen deficiency-associated bone loss whereas increased estrogen levels can attenuate bone loss associated with reduced mechanical loading (Westerlind et al. 1997). Thus, altered endocrine status during aging may contribute to chronic bone loss by multiple mechanisms that are not completely counteracted by the mechanostat. In some cases, hormone action (e.g., growth hormone) on bone appears to be independent of the mechanostat whereas in other cases, the hormone (e.g., estrogen and leptin) is an integral component of the mechanisms mediating mechanosignaling.
High Fat Diet
Based on mechanostat theory, increased body weight should attenuate age-related decline in bone mass by increasing skeletal loading and as described earlier there is evidence that this indeed occurs. However, there is also creditable evidence that underfeeding and overfeeding can impair the ability of the skeleton to fully adapt to mechanical loads. In regard to overfeeding, there has been a great deal of recent interest regarding the impact of specific components of the diet (e.g., fat) on bone health.
Bone compartment-specific increases and decreases in bone mass have been reported in growing mice fed high fat diets but most studies report negative effects. Several mechanisms have been proposed to explain the negative effect of excess fat on rodent bone. Obesity results in chronic mild inflammation and insulin resistance (Xu, et al. 2003), conditions which could negatively impact bone turnover (Hardy and Cooper 2009) and reduce the efficacy of mechanosignaling. While obesity in general may have detrimental effects, fat depots within the skeleton may be particularly damaging because of the proximity to bone cells. An obesity associated increase in MAT has been suggested as an additional mechanism by which excess weight could negatively impact the skeleton. Anorexia, severe weight loss, and weightlessness each result in increased MAT (Bredella, et al. 2009; Duque 2008; Trudel et al. 2009), implicating MAT in bone loss. Bone marrow adipocytes have been implicated in regulating cell differentiation through generation and release of adipokines (Kilroy, et al. 2007). Additionally, osteoblasts and adipocytes are derived from the mesenchymal lineage and share a common bone marrow progenitor cell (Prockop 1997). The reciprocal relationship between MAT and bone mass that is often observed is potentially explained by lower osteoblast number (Akune, et al. 2004). A deficiency in PPARγ, a key mediator of adipocyte differentiation, reduces marrow fat and enhances osteogenesis (Akune et al. 2004). Thus, increased MAT may reflect altered lineage decision where increased adipocyte differentiation occurs at the expense of osteoblast differentiation. However, a causal relationship between differentiation of adipocytes and osteoblasts has not been established and the results obtained in some studies suggest that adipocyte and osteoblast numbers in bone marrow can be regulated independently (Iwaniec and Turner 2013; Menagh, et al. 2010).
When considering diet, species differences need to be considered. Increases in body weight are commonly induced in rodents by feeding energy dense high fat diets, where fat typically contributes 45–60% of total energy. Notably, normal rodent diets typically contribute 10–15% of calories as fat. While the mechanostat has been conserved among vertebrate species their dietary requirements show dramatic divergences. Contemporary hunter gatherers show variability in diet that is related to environmental differences, but in most populations the majority of energy is obtained from animal products (Cordain, et al. 2002). Diet reconstruction using stable isotope analysis supports animal products contributing the majority of energy to the diet in preagricultural populations (Eaton and Eaton III 2000). On the other hand, with the advent of agriculture >10,000 BP humans have successfully adapted to predominantly plant-based diets. Present dietary recommendations for fat vary among countries but are generally between 20–35% of total energy in adults and fat consumption in the United States and Europe is typically at the upper end of the recommended range (Arnett, et al. 2000; Vergnaud, et al. 2013). In spite of increased prevalence of obesity, in the United States there has been a progressive decrease in fat consumption whereas in Europe fat consumption has increased (Vergnaud et al. 2013). In general, excess weight gain in humans is more associated with excess calories rather than excess in a specific macronutrient. Thus, it is not clear whether the high fat diets administered to rodents accurately model any commonly consumed human diet.
In spite of uncertainty regarding the precise role of dietary fat, there is growing evidence that excessive fat accrual due to excess calories can have negative effects on BMD (Zhang, et al. 2015). While lean mass is generally positively associated with BMD, the relationship between fat mass and BMD is more complex. Visceral and subcutaneous fat may have independent effects with the former reported to be negatively associated with BMD (Zhang et al. 2015). Additionally there is evidence for a threshold where the relationship between fat mass and BMD changes from a positive to a negative association (Liu, et al. 2014). Successful mechanical adaptation of the skeleton to changes in weight and body composition should confer a reduction in fracture risk. In this regard, the evidence associating BMI and fracture rate is often contradictory. However, there is strong evidence that low trauma fractures in the obese represent a significant and growing health problem (Greco, et al. 2015; Premaor, et al. 2010).
Hyperleptinemia: Too Much of a Good Thing?
The regulatory actions of leptin to reduce energy intake are mediated through a hypothalamic relay involving activation of leptin receptors on orexigenic NPY and anorexigenic POMC-expressing neurons (Forbes, et al. 2001). In contrast, the physiological actions of leptin to increase bone growth are primarily mediated by systemic actions of the hormone (Turner, et al. 2013). Humans and rodents exhibit age-related weight gain and bone loss in spite of increased leptin levels. The failure of increased serum leptin to prevent further weight gain is generally attributed to leptin resistance (Banks and Farrell 2003; Burguera, et al. 2000). As discussed below, it seems plausible that development of leptin resistance may play a causal role for impaired skeletal adaptation to greatly increased body weight. Thus, low leptin levels in severely underweight and leptin resistance associated with obesity may negatively impact optimization of bone mass to body weight.
There are several mechanisms by which obesity could result in skeletal resistance to the bone anabolic actions of leptin, including receptor saturation, reduced receptor levels and activation of counter regulatory pathways. Based on the affinity of leptin for its receptor in cultured human osteogenic cells (Kd of ~0.4 nM), the bone anabolic effects of the hormone would occur at relatively low circulating levels (Hess, et al. 2005). Overweight and obese individuals have serum leptin levels in great excess of the Kd and would, as a consequence, derive little or no additional benefit of higher hormone levels on bone compared to normal weight individuals (Boden, et al. 1996; Weigle, et al. 1997). Continuous exposure to high levels of leptin have been shown to result in downregulation of leptin receptor mRNA and protein in the hypothalamus (Martin et al. 2008). However, the impact of hyperleptinemia on leptin receptors in skeletal tissues is unknown. Finally, continuous exposure to high levels of leptin have been shown to increase expression of Socs3 in the hypothalamus, which in turn blocked leptin-induced signal transduction (Bjørbæk, et al. 1998). Socs3 is also a potent negative regulator of cytokine signaling in osteoblasts and osteoclasts (Gao and Van Dyke 2013), but its role in leptin signaling in bone has not been investigated.
Summary and Conclusions
Lifelong maintenance of the mechanical competence of the skeleton requires a bone mass appropriate for body size. Skeletal growth and maturation is regulated by several hormones and is dependent upon adequate energy to support growth. The mechanostat functions as an adaptive mechanism to help optimize bone mass and architecture based on prevailing mechanical strain induced by body weight. However, the mechanostat is influenced by regulatory inputs mandating non-mechanical functions of the skeleton, such as mineral homeostasis. While the skeleton is very capable of adapting to changes in weight, the mechanostat has limits related to magnitude and rate of change in bone mass. Both underweight and obesity are associated with impaired optimization of bone strength. The mechanisms for these deficiencies are unknown but may be related; we speculate that leptin deficiency and leptin resistance may be a common factor contributing to decreased mechanical competence noted in anorectic and obese individuals.
Acknowledgments
Funding: This work was supported by NIH (AR 060913) and NASA (NNX12AL24).
Footnotes
Declaration of Conflict of Interest: The authors declare that that there is no conflict of interest.
Bibliography
- Ahima RS, Flier JS. Leptin. Annual Review of Physiology. 2000;62:413–437. doi: 10.1146/annurev.physiol.62.1.413. [DOI] [PubMed] [Google Scholar]
- Akune T, Ohba S, Kamekura S, Yamaguchi M, Chung U-i, Kubota N, Terauchi Y, Harada Y, Azuma Y, Nakamura K. PPAR γ insufficiency enhances osteogenesis through osteoblast formation from bone marrow progenitors. Journal of Clinical Investigation. 2004;113:846–855. doi: 10.1172/JCI19900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Nazer R, Rantalainen T, Heinonen A, Sievanen H, Mikkola A. Flexible multibody simulation approach in the analysis of tibial strain during walking. Journal of Biomechanics. 2008;41:1036–1043. doi: 10.1016/j.jbiomech.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Almeida A, Roberts I. Bone involvement in sickle cell disease. British Journal of Haematology. 2005;129:482–490. doi: 10.1111/j.1365-2141.2005.05476.x. [DOI] [PubMed] [Google Scholar]
- Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric surgery worldwide 2013. Obesity Surgery. 2015;25:1822–1832. doi: 10.1007/s11695-015-1657-z. [DOI] [PubMed] [Google Scholar]
- Arnett DK, Xiong B, McGovern PG, Blackburn H, Luepker RV. Secular trends in dietary macronutrient intake in Minneapolis-St, Paul, Minnesota, 1980–1992. American Journal of Epidemiology. 2000;152:868–873. doi: 10.1093/aje/152.9.868. [DOI] [PubMed] [Google Scholar]
- Baek K, Barlow AA, Allen MR, Bloomfield SA. Food restriction and simulated microgravity: effects on bone and serum leptin. Journal of Applied Physiology (1985) 2008;104:1086–1093. doi: 10.1152/japplphysiol.01209.2007. [DOI] [PubMed] [Google Scholar]
- Baek K, Bloomfield SA. β-adrenergic blockade and leptin replacement effectively mitigate disuse bone loss. Journal of Bone and Mineral Research. 2009;24:792–799. doi: 10.1359/jbmr.081241. [DOI] [PubMed] [Google Scholar]
- Banks WA, Farrell CL. Impaired transport of leptin across the blood-brain barrier in obesity is acquired and reversible. American Journal of Physiology. Endocrinology and Metabolism. 2003;285:E10–15. doi: 10.1152/ajpendo.00468.2002. [DOI] [PubMed] [Google Scholar]
- Barkan D, Hurgin V, Dekel N, Amsterdam A, Rubinstein M. Leptin induces ovulation in GnRH-deficient mice. The FASEB Journal. 2005;19:133–135. doi: 10.1096/fj.04-2271fje. [DOI] [PubMed] [Google Scholar]
- Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. Journal of Bone and Mineral Research. 2011;26:1729–1739. doi: 10.1002/jbmr.412. [DOI] [PubMed] [Google Scholar]
- Bjørbæk C, Elmquist JK, Frantz JD, Shoelson SE, Flier JS. Identification of SOCS-3 as a potential mediator of central leptin resistance. Molecular Cell. 1998;1:619–625. doi: 10.1016/s1097-2765(00)80062-3. [DOI] [PubMed] [Google Scholar]
- Boden G, Chen X, Mozzoli M, Ryan I. Effect of fasting on serum leptin in normal human subjects. Journal of Clinical Endocrinology and Metabolism. 1996;81:3419–3423. doi: 10.1210/jcem.81.9.8784108. [DOI] [PubMed] [Google Scholar]
- Bouxsein ML, Seeman E. Quantifying the material and structural determinants of bone strength. Best Practice and Research Clinical Rheumatology. 2009;23:741–753. doi: 10.1016/j.berh.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Bredella MA, Fazeli PK, Miller KK, Misra M, Torriani M, Thomas BJ, Ghomi RH, Rosen CJ, Klibanski A. Increased bone marrow fat in anorexia nervosa. Journal of Clinical Endocrinology and Metabolism. 2009;94:2129–2136. doi: 10.1210/jc.2008-2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burguera B, Couce ME, Curran GL, Jensen MD, Lloyd RV, Cleary MP, Poduslo JF. Obesity is associated with a decreased leptin transport across the blood-brain barrier in rats. Diabetes. 2000;49:1219–1223. doi: 10.2337/diabetes.49.7.1219. [DOI] [PubMed] [Google Scholar]
- Caffarelli C, Alessi C, Nuti R, Gonnelli S. Divergent effects of obesity on fragility fractures. Clinical Interventions in Aging. 2014;9:1629–1636. doi: 10.2147/CIA.S64625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P. Recombinant mouse OB protein: evidence for a peripheral signal linking adiposity and central neural networks. Science. 1995;269:546–549. doi: 10.1126/science.7624778. [DOI] [PubMed] [Google Scholar]
- Cauley JA, Lui LY, Barnes D, Ensrud KE, Zmuda JM, Hillier TA, Hochberg MC, Schwartz AV, Yaffe K, Cummings SR, et al. Successful skeletal aging: a marker of low fracture risk and longevity. The Study of Osteoporotic Fractures (SOF) Journal of Bone and Mineral Research. 2009;24:134–143. doi: 10.1359/JBMR.080813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh PR, Genc KO, Gopalakrishnan R, Kuklis MM, Maender CC, Rice AJ. Foot forces during typical days on the international space station. Journal of Biomechanics. 2010;43:2182–2188. doi: 10.1016/j.jbiomech.2010.03.044. [DOI] [PubMed] [Google Scholar]
- Cawsey S, Padwal R, Sharma A, Wang X, Li S, Siminoski K. Women with severe obesity and relatively low bone mineral density have increased fracture risk. Osteoporosis International. 2015;26:103–111. doi: 10.1007/s00198-014-2833-z. [DOI] [PubMed] [Google Scholar]
- Chevalley T, Bonjour J-P, Van Rietbergen B, Rizzoli R, Ferrari S. Fractures in healthy females followed from childhood to early adulthood are associated with later menarcheal age and with impaired bone microstructure at peak bone mass. The Journal of Clinical Endocrinology and Metabolism. 2012;97:4174–4181. doi: 10.1210/jc.2012-2561. [DOI] [PubMed] [Google Scholar]
- Clark EM, Ness AR, Bishop NJ, Tobias JH. Association between bone mass and fractures in children: a prospective cohort study. Journal of Bone and Mineral Research. 2006;21:1489–1495. doi: 10.1359/jbmr.060601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke BL, Khosla S. Female reproductive system and bone. Archives of Biochemistry and Biophysics. 2010;503:118–128. doi: 10.1016/j.abb.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole Z, Harvey N, Kim M, Ntani G, Robinson S, Inskip H, Godfrey K, Cooper C, Dennison E Group SWsSS. Increased fat mass is associated with increased bone size but reduced volumetric density in pre pubertal children. Bone. 2012;50:562–567. doi: 10.1016/j.bone.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compston JE, Watts NB, Chapurlat R, Cooper C, Boonen S, Greenspan S, Pfeilschifter J, Silverman S, Diez-Perez A, Lindsay R, et al. Obesity is not protective against fracture in postmenopausal women: GLOW. The American Journal of Medicine. 2011;124:1043–1050. doi: 10.1016/j.amjmed.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordain L, Eaton S, Brand Miller J, Mann N, Hill K. Original Communications-The paradoxical nature of hunter-gatherer diets: Meat-based, yet non-atherogenic. European Journal of Clinical Nutrition. 2002;56:S42. doi: 10.1038/sj.ejcn.1601353. [DOI] [PubMed] [Google Scholar]
- Devlin MJ, Cloutier AM, Thomas NA, Panus DA, Lotinun S, Pinz I, Baron R, Rosen CJ, Bouxsein ML. Caloric restriction leads to high marrow adiposity and low bone mass in growing mice. Journal of Bone and Mineral Research. 2010;25:2078–2088. doi: 10.1002/jbmr.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitri P, Bishop N, Walsh J, Eastell R. Obesity is a risk factor for fracture in children but is protective against fracture in adults: a paradox. Bone. 2012;50:457–466. doi: 10.1016/j.bone.2011.05.011. [DOI] [PubMed] [Google Scholar]
- Dimitri P, Jacques RM, Paggiosi M, King D, Walsh J, Taylor ZA, Frangi AF, Bishop N, Eastell R. Leptin may play a role in bone microstructural alterations in obese children. Journal of Clinical Endocrinology and Metabolism. 2015;100:594–602. doi: 10.1210/jc.2014-3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duque G. Bone and fat connection in aging bone. Current Opinion in Rheumatology. 2008;20:429–434. doi: 10.1097/BOR.0b013e3283025e9c. [DOI] [PubMed] [Google Scholar]
- Eaton SB, Eaton SB., III Paleolithic vs. modern diets–slected pathophysiological implications. European Journal of Nutrition. 2000;39:67–70. doi: 10.1007/s003940070032. [DOI] [PubMed] [Google Scholar]
- Faulkner JA, Larkin LM, Claflin DR, Brooks SV. Age-related changes in the structure and function of skeletal muscles. Clinical and Experimental Pharmacology and Physiology. 2007;34:1091–1096. doi: 10.1111/j.1440-1681.2007.04752.x. [DOI] [PubMed] [Google Scholar]
- Forbes S, Bui S, Robinson BR, Hochgeschwender U, Brennan MB. Integrated control of appetite and fat metabolism by the leptin-proopiomelanocortin pathway. Proceeding of the National Academy of Sciences. 2001;98:4233–4237. doi: 10.1073/pnas.071054298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederiksen KD, Hanson S, Hansen S, Brixen K, Gram J, Jorgensen NR, Stoving RK. Bone Structural Changes and Estimated Strength After Gastric Bypass Surgery Evaluated by HR-pQCT. Calcified Tissue International. 2016;98:253–262. doi: 10.1007/s00223-015-0091-5. [DOI] [PubMed] [Google Scholar]
- Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature. 1998;395:763–770. doi: 10.1038/27376. [DOI] [PubMed] [Google Scholar]
- Fritton SP, McLeod KJ, Rubin CT. Quantifying the strain history of bone: spatial uniformity and self-similarity of low-magnitude strains. Journal of Biomechanics. 2000;33:317–325. doi: 10.1016/s0021-9290(99)00210-9. [DOI] [PubMed] [Google Scholar]
- Frost HM. The mechanostat: a proposed pathogenic mechanism of osteoporoses and the bone mass effects of mechanical and nonmechanical agents. Bone and Mineral. 1987;2:73–85. [PubMed] [Google Scholar]
- Galea GL, Price JS, Lanyon LE. Estrogen receptors’ roles in the control of mechanically adaptive bone (re)modeling. Bonekey Reports. 2013;2:413. doi: 10.1038/bonekey.2013.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao A, Van Dyke TE. Role of suppressors of cytokine signaling 3 in bone inflammatory responses. Frontiers in Immunology. 2013:4. doi: 10.3389/fimmu.2013.00506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gat-Yablonski G, Ben-Ari T, Shtaif B, Potievsky O, Moran O, Eshet R, Maor G, Segev Y, Phillip M. Leptin reverses the inhibitory effect of caloric restriction on longitudinal growth. Endocrinology. 2004;145:343–350. doi: 10.1210/en.2003-0910. [DOI] [PubMed] [Google Scholar]
- Gnyubkin V, Guignandon A, Laroche N, Vanden-Bossche A, Normand M, Lafage-Proust M-H, Vico L. Effects of chronic hypergravity: from adaptive to deleterious responses in growing mouse skeleton. Journal of Applied Physiology. 2015 doi: 10.1152/japplphysiol.00364.2015. 00364.02015. [DOI] [PubMed] [Google Scholar]
- Goldring SR. The osteocyte: key player in regulating bone turnover. RMD Open. 2015;1:e000049. doi: 10.1136/rmdopen-2015-000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstone A, Howard J, Lord G, Ghatei M, Gardiner J, Wang Z, Wang R, Girgis S, Bailey C, Bloom S. Leptin prevents the fall in plasma osteocalcin during starvation in male mice. Biochemical and Biophysical Research Communications. 2002;295:475–481. doi: 10.1016/s0006-291x(02)00697-6. [DOI] [PubMed] [Google Scholar]
- Govey PM, Kawasawa YI, Donahue HJ. Mapping the osteocytic cell response to fluid flow using RNA-Seq. Journal of Biomechanics. 2015;48:4327–4332. doi: 10.1016/j.jbiomech.2015.10.045. [DOI] [PubMed] [Google Scholar]
- Greco EA, Fornari R, Rossi F, Santiemma V, Prossomariti G, Annoscia C, Aversa A, Brama M, Marini M, Donini LM, et al. Is obesity protective for osteoporosis? Evaluation of bone mineral density in individuals with high body mass index. International Journal of Clinical Practice. 2010;64:817–820. doi: 10.1111/j.1742-1241.2009.02301.x. [DOI] [PubMed] [Google Scholar]
- Greco EA, Lenzi A, Migliaccio S. The obesity of bone. Therapeutic Advances in Endocrinology and Metabolism. 2015;6:273–286. doi: 10.1177/2042018815611004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunter K, Baxter-Jones AD, Mirwald RL, Almstedt H, Fuchs RK, Durski S, Snow C. Impact exercise increases BMC during growth: an 8-year longitudinal study. Journal of Bone and Mineral Research. 2008;23:986–993. doi: 10.1359/JBMR.071201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamann A, Matthaei S. Regulation of energy balance by leptin. Experimental and Clinical Endocrinology and Diabetes. 1996;104:293–300. doi: 10.1055/s-0029-1211457. [DOI] [PubMed] [Google Scholar]
- Hamrick MW, Ding KH, Ponnala S, Ferrari SL, Isales CM. Caloric restriction decreases cortical bone mass but spares trabecular bone in the mouse skeleton: implications for the regulation of bone mass by body weight. Journal of Bone and Mineral Research. 2008;23:870–878. doi: 10.1359/jbmr.080213. [DOI] [PubMed] [Google Scholar]
- Hannema SE, Wit JM, Houdijk ME, van Haeringen A, Bik EC, Verkerk AJ, Uitterlinden AG, Kant SG, Oostdijk W, Bakker E, et al. Novel leptin receptor mutations identified in two girls with severe obesity are associated with increased bone mineral density. Hormone Research in Paediatrics. 2016 doi: 10.1159/000444055. [DOI] [PubMed] [Google Scholar]
- Hardy R, Cooper MS. Bone loss in inflammatory disorders. Journal of Endocrinology. 2009;201:309–320. doi: 10.1677/JOE-08-0568. [DOI] [PubMed] [Google Scholar]
- Harris RB. Is leptin the parabiotic “satiety” factor? Past and present interpretations. Appetite. 2013;61:111–118. doi: 10.1016/j.appet.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hefferan TE, Evans GL, Lotinun S, Zhang M, Morey-Holton E, Turner RT. Effect of gender on bone turnover in adult rats during simulated weightlessness. Journal of Applied Physiology (1985) 2003;95:1775–1780. doi: 10.1152/japplphysiol.00455.2002. [DOI] [PubMed] [Google Scholar]
- Hess R, Pino AM, Ríos S, Fernández M, Rodríguez JP. High affinity leptin receptors are present in human mesenchymal stem cells (MSCs) derived from control and osteoporotic donors. Journal of Cellular Biochemistry. 2005;94:50–57. doi: 10.1002/jcb.20330. [DOI] [PubMed] [Google Scholar]
- Holbrook TL, Barrett-Connor E. The association of lifetime weight and weight control patterns with bone mineral density in an adult community. Bone and Mineral. 1993;20:141–149. doi: 10.1016/s0169-6009(08)80023-2. [DOI] [PubMed] [Google Scholar]
- Hsin MC, Huang CK, Tai CM, Yeh LR, Kuo HC, Garg A. A case-matched study of the differences in bone mineral density 1 year after 3 different bariatric procedures. Surgery of Obesity and Related Diseases. 2015;11:181–185. doi: 10.1016/j.soard.2014.07.008. [DOI] [PubMed] [Google Scholar]
- Hwa J, Ghibaudi L, Compton D, Fawzi A, Strader C. Intracerebroventricular injection of leptin increases thermogenesis and mobilizes fat metabolism in ob/ob mice. Hormone and Metabolic Research. 1996;28:659–663. doi: 10.1055/s-2007-979873. [DOI] [PubMed] [Google Scholar]
- Iwaniec U, Dube M, Boghossian S, Song H, Helferich W, Turner R, Kalra S. Body mass influences cortical bone mass independent of leptin signaling. Bone. 2009;44:404–412. doi: 10.1016/j.bone.2008.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwaniec UT, Turner RT. Failure to generate bone marrow adipocytes does not protect mice from ovariectomy-induced osteopenia. Bone. 2013;53:145–153. doi: 10.1016/j.bone.2012.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaekel E, Amtmann E, Oyama J. Effect of chronic centrifugation on bone density of the rat. Anatomy and Embriology. 1977;151:223–232. doi: 10.1007/BF00297483. [DOI] [PubMed] [Google Scholar]
- Jee W, Wronski T, Morey E, Kimmel D. Effects of spaceflight on trabecular bone in rats. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. 1983;244:R310–R314. doi: 10.1152/ajpregu.1983.244.3.R310. [DOI] [PubMed] [Google Scholar]
- Kanis JA, Odén A, McCloskey E, Johansson H, Wahl DA, Cooper C. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporosis International. 2012;23:2239–2256. doi: 10.1007/s00198-012-1964-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapur S, Amoui M, Kesavan C, Wang X, Mohan S, Baylink DJ, Lau K-HW. Leptin receptor (Lepr) is a negative modulator of bone mechanosensitivity and genetic variations in Lepr may contribute to the differential osteogenic response to mechanical stimulation in the C57BL/6J and C3H/HeJ pair of mouse strains. Journal of Biological Chemistry. 2010;285:37607–37618. doi: 10.1074/jbc.M110.169714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keune JA, Branscum AJ, Iwaniec UT, Turner RT. Effects of spaceflight on bone microarchitecture in the axial and appendicular skeleton in growing ovariectomized rats. Scientific Reports. 2015;5:18671. doi: 10.1038/srep18671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keune JA, Philbrick KA, Branscum AJ, Turner RT. Spaceflight-induced vertebral bone loss in ovariectomized rats is assosicated with increased bone marrow adiposity and no change in bone formation. Microgravity. 2016;2:16016. doi: 10.1038/npjmgrav.2016.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilroy GE, Foster SJ, Wu X, Ruiz J, Sherwood S, Heifetz A, Ludlow JW, Stricker DM, Potiny S, Green P. Cytokine profile of human adipose-derived stem cells: Expression of angiogenic, hematopoietic, and pro-inflammatory factors. Journal of Cellular Physiology. 2007;212:702–709. doi: 10.1002/jcp.21068. [DOI] [PubMed] [Google Scholar]
- Kim JE, Hsieh MH, Soni BK, Zayzafoon M, Allison DB. Childhood obesity as a risk factor for bone fracture: a mechanistic study. Obesity. 2013;21:1459–1466. doi: 10.1002/oby.20355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein-Nulend J, van Oers RF, Bakker AD, Bacabac RG. Nitric oxide signaling in mechanical adaptation of bone. Osteoporosis International. 2014;25:1427–1437. doi: 10.1007/s00198-013-2590-4. [DOI] [PubMed] [Google Scholar]
- Kopf J, Paarmann P, Hiepen C, Horbelt D, Knaus P. BMP growth factor signaling in a biomechanical context. Biofactors. 2014;40:171–187. doi: 10.1002/biof.1137. [DOI] [PubMed] [Google Scholar]
- Kovacs CS. Calcium and bone metabolism during pregnancy and lactation. Journal of Mammary Gland Biology and Neoplasia. 2005;10:105–118. doi: 10.1007/s10911-005-5394-0. [DOI] [PubMed] [Google Scholar]
- Kuzma M, Homerova Z, Dlesk A, Koller T, Killinger Z, Vanuga P, Lazurova I, Tomkova S, Payer J. Effect of growth hormone on bone status in growth hormone-deficient adults. Bratislarske Lekarske Listy. 2013;114:689–695. doi: 10.4149/bll_2013_146. [DOI] [PubMed] [Google Scholar]
- Liu PY, Ilich JZ, Brummel-Smith K, Ghosh S. New insight into fat, muscle and bone relationship in women: determining the threshold at which body fat assumes negative relationship with bone mineral density. International Journal of Preventive Medicine. 2014;5:1452–1463. [PMC free article] [PubMed] [Google Scholar]
- Lloyd SA, Loiselle AE, Zhang Y, Donahue HJ. Shifting paradigms on the role of connexin43 in the skeletal response to mechanical load. Journal of Bone and Mineral Research. 2014;29:275–286. doi: 10.1002/jbmr.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo ZP, Zhang L, Turner RT, An KN. Effects of mechanical stress/strain and estrogen on cancellous bone structure predicted by fuzzy decision. IEEE Transections in Biomedical Engineering. 2000;47:344–351. doi: 10.1109/10.827295. [DOI] [PubMed] [Google Scholar]
- Luque RM, Huang ZH, Shah B, Mazzone T, Kineman RD. Effects of leptin replacement on hypothalamic-pituitary growth hormone axis function and circulating ghrelin levels in ob/ob mice. American Journal of Physiology. Endocrinology and Metabolism. 2007;292:E891–899. doi: 10.1152/ajpendo.00258.2006. [DOI] [PubMed] [Google Scholar]
- Maïmoun L, Mura T, Leprieur E, Avignon A, Mariano-Goulart D, Sultan A. Impact of obesity on bone mass throughout adult life: Influence of gender and severity of obesity. Bone. 2015 doi: 10.1016/j.bone.2015.11.020. [DOI] [PubMed] [Google Scholar]
- Mantzoros CS, Magkos F, Brinkoetter M, Sienkiewicz E, Dardeno TA, Kim SY, Hamnvik OP, Koniaris A. Leptin in human physiology and pathophysiology. American Journal of Physiology. Endocrinology and Metabolism. 2011;301:E567–584. doi: 10.1152/ajpendo.00315.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A, David V, Vico L, Thomas T. Impaired energetic metabolism after central leptin signaling leads to massive appendicular bone loss in hindlimb-suspended rats. Journal of Bone and Mineral Research. 2008;23:2040–2047. doi: 10.1359/jbmr.080708. [DOI] [PubMed] [Google Scholar]
- Meakin LB, Price JS, Lanyon LE. The contribution of experimental in vivo models to understanding the mechanisms of Adaptation to mechanical loading in bone. Frontiers in Endocrinology (Lausanne) 2014;5:154. doi: 10.3389/fendo.2014.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melmed S. Idiopathic adult growth hormone deficiency. Journal of Clinical Endocrinology and Metabolism. 2013;98:2187–2197. doi: 10.1210/jc.2012-4012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melville KM, Kelly NH, Surita G, Buchalter DB, Schimenti JC, Main RP, Ross FP, van der Meulen MC. Effects of Deletion of ERalpha in Osteoblast-Lineage Cells on Bone Mass and Adaptation to Mechanical Loading Differ in Female and Male Mice. Journal of Bone and Mineral Research. 2015;30:1468–1480. doi: 10.1002/jbmr.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menagh PJ, Turner RT, Jump DB, Wong CP, Lowry MB, Yakar S, Rosen CJ, Iwaniec UT. Growth hormone regulates the balance between bone formation and bone marrow adiposity. Journal of Bone and Mineral Research. 2010;25:757–768. doi: 10.1359/jbmr.091015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H, Wareham NJ, Sewter CP, Digby JE, Mohammed SN, Hurst JA. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature. 1997;387:903–907. doi: 10.1038/43185. [DOI] [PubMed] [Google Scholar]
- Morey E, Sabelman E, Turner R, Baylink D. A new rat model simulating some aspects of space flight. The Physiologist. 1979;22:S23. [PubMed] [Google Scholar]
- Mpalaris V, Anagnostis P, Goulis D, Iakovou I. Complex association between body weight and fracture risk in postmenopausal women. Obesity Reviews. 2015;16:225–233. doi: 10.1111/obr.12244. [DOI] [PubMed] [Google Scholar]
- Naumann FL, Bennell KL, Wark JD. The effects of +Gz force on the bone mineral density of fighter pilots. Aviation, Space, and Environmental Medicine. 2001;72:177–181. [PubMed] [Google Scholar]
- Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Nevitt M, Harris TB. Weight change and the conservation of lean mass in old age: the Health, Aging and Body Composition Study. American Journal of Clinical Nutrition. 2005;82:872–878. doi: 10.1093/ajcn/82.4.872. quiz 915–876. [DOI] [PubMed] [Google Scholar]
- Nielson CM, Srikanth P, Orwoll ES. Obesity and fracture in men and women: an epidemiologic perspective. Journal of Bone and Mineral Research. 2012;27:1–10. doi: 10.1002/jbmr.1486. [DOI] [PubMed] [Google Scholar]
- Orwoll ES, Adler RA, Amin S, Binkley N, Lewiecki EM, Petak SM, Shapses SA, Sinaki M, Watts NB, Sibonga JD. Skeletal health in long-duration astronauts: Nature, assessment, and management recommendations from the NASA bone summit. Journal of Bone and Mineral Research. 2013;28:1243–1255. doi: 10.1002/jbmr.1948. [DOI] [PubMed] [Google Scholar]
- Perisano C, Marzetti E, Spinelli MS, Calla CA, Graci C, Maccauro G. Physiopathology of bone modifications in beta-thalassemia. Anemia. 2012;2012:320737. doi: 10.1155/2012/320737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philbrick KA, Turner RT, Branscum AJ, Wong CP, Iwaniec UT. Paradoxical effects of partial leptin deficiency on bone in growing female mice. Anatomical Record. 2015;298:2018–2029. doi: 10.1002/ar.23267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Premaor MO, Pilbrow L, Tonkin C, Parker RA, Compston J. Obesity and fractures in postmenopausal women. Journal of Bone and Mineral Research. 2010;25:292–297. doi: 10.1359/jbmr.091004. [DOI] [PubMed] [Google Scholar]
- Price JS, Sugiyama T, Galea GL, Meakin LB, Sunters A, Lanyon LE. Role of endocrine and paracrine factors in the adaptation of bone to mechanical loading. Current Osteoporosis Reports. 2011;9:76–82. doi: 10.1007/s11914-011-0050-7. [DOI] [PubMed] [Google Scholar]
- Prieto-Alhambra D, Premaor MO, Aviles FF, Castro AS, Javaid MK, Nogues X, Arden NK, Cooper C, Compston JE, Diez-Perez A. Relationship between mortality and BMI after fracture: a population-based study of men and women aged >/=40 years. Journal of Bone and Mineral Research. 2014;29:1737–1744. doi: 10.1002/jbmr.2209. [DOI] [PubMed] [Google Scholar]
- Prieto-Alhambra D, Premaor MO, Fina Aviles F, Hermosilla E, Martinez-Laguna D, Carbonell-Abella C, Nogues X, Compston JE, Diez-Perez A. The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. Journal of Bone and Mineral Research. 2012;27:294–300. doi: 10.1002/jbmr.1466. [DOI] [PubMed] [Google Scholar]
- Prockop DJ. Marrow stromal cells as stem cells for nonhematopoietic tissues. Science. 1997;276:71–74. doi: 10.1126/science.276.5309.71. [DOI] [PubMed] [Google Scholar]
- Rauch F. The dynamics of bone structure development during pubertal growth. Journal of Musculoskeletal and Neuronal Interactions. 2012;12:1–6. [PubMed] [Google Scholar]
- Recht M, Liel MS, Turner RT, Klein RF, Taylor JA. The bone disease associated with factor VIII deficiency in mice is secondary to increased bone resorption. Haemophilia. 2013;19:908–912. doi: 10.1111/hae.12195. [DOI] [PubMed] [Google Scholar]
- Rector RS, Loethen J, Ruebel M, Thomas TR, Hinton PS. Serum markers of bone turnover are increased by modest weight loss with or without weight-bearing exercise in overweight premenopausal women. Applied Physiology, Nutrition and Metabolism. 2009;34:933–941. doi: 10.1139/H09-098. [DOI] [PubMed] [Google Scholar]
- Redman LM, Rood J, Anton SD, Champagne C, Smith SR, Ravussin E. Calorie restriction and bone health in young, overweight individuals. Archives of Internal Medicine. 2008;168:1859–1866. doi: 10.1001/archinte.168.17.1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro SM, Kehayias JJ. Sarcopenia and the analysis of body composition. Advances in Nutrtion. 2014;5:260–267. doi: 10.3945/an.113.005256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rittweger J. Ten years muscle-bone hypothesis: what have we learned so far?--almost a festschrift. Journal of Musculoskeletal and Neuronal Interactions. 2008;8:174–178. [PubMed] [Google Scholar]
- Robling AG. The interaction of biological factors with mechanical signals in bone adaptation: recent developments. Current Osteoporosis Reports. 2012;10:126–131. doi: 10.1007/s11914-012-0099-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin CT, Lanyon LE. Dynamic strain similarity in vertebrates; an alternative to allometric limb bone scaling. Journal of Theoretical Biology. 1984;107:321–327. doi: 10.1016/s0022-5193(84)80031-4. [DOI] [PubMed] [Google Scholar]
- Saito M, Bray G. Diurnal Rhythm for Corticosterone in Obese (ob/ob) Diabetes (db/db) and Gold-Thioglucose-Induced Obesity in Mice. Endocrinology. 1983;113:2181–2185. doi: 10.1210/endo-113-6-2181. [DOI] [PubMed] [Google Scholar]
- Sattler FR. Growth hormone in the aging male. Best Practice and Research in Clinical Endocrinololgy and Metabolism. 2013;27:541–555. doi: 10.1016/j.beem.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scibora LM. Skeletal effects of bariatric surgery: examining bone loss, potential mechanisms and clinical relevance. Diabetes, Obesity and Metabolism. 2014;16:1204–1213. doi: 10.1111/dom.12363. [DOI] [PubMed] [Google Scholar]
- Scott D, Chandrasekara SD, Laslett LL, Cicuttini F, Ebeling PR, Jones G. Associations of Sarcopenic Obesity and Dynapenic Obesity with Bone Mineral Density and Incident Fractures Over 5–10 Years in Community-Dwelling Older Adults. Calcified Tissue International. 2016;99:30–42. doi: 10.1007/s00223-016-0123-9. [DOI] [PubMed] [Google Scholar]
- Sessions ND, Halloran BP, Bikle DD, Wronski TJ, Cone CM, Morey-Holton E. Bone response to normal weight bearing after a period of skeletal unloading. American Journal of Physiology. 1989;257:E606–610. doi: 10.1152/ajpendo.1989.257.4.E606. [DOI] [PubMed] [Google Scholar]
- Shapses SA, Riedt CS. Bone, body weight, and weight reduction: what are the concerns? The Journal of Nutrition. 2006;136:1453–1456. doi: 10.1093/jn/136.6.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapses SA, Sukumar D. Bone metabolism in obesity and weight loss. Annual Review of Nutrition. 2012;32:287–309. doi: 10.1146/annurev.nutr.012809.104655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibonga JD. Spaceflight-induced bone loss: is there an osteoporosis risk? Current Osteoporosis Reports. 2013;11:92–98. doi: 10.1007/s11914-013-0136-5. [DOI] [PubMed] [Google Scholar]
- Sibonga JD, Evans HJ, Sung HG, Spector ER, Lang TF, Oganov VS, Bakulin AV, Shackelford LC, LeBlanc AD. Recovery of spaceflight-induced bone loss: bone mineral density after long-duration missions as fitted with an exponential function. Bone. 2007;41:973–978. doi: 10.1016/j.bone.2007.08.022. [DOI] [PubMed] [Google Scholar]
- Sibonga JD, Spector ER, Johnston SL, Tarver WJ. Evaluating bone loss in ISS astronauts. Aerospace Medicine and Human Performance. 2015;86:A38–44. doi: 10.3357/AMHP.EC06.2015. [DOI] [PubMed] [Google Scholar]
- Sibonga JD, Zhang M, Evans GL, Westerlind KC, Cavolina JM, Morey-Holton E, Turner RT. Effects of spaceflight and simulated weightlessness on longitudinal bone growth. Bone. 2000;27:535–540. doi: 10.1016/s8756-3282(00)00352-5. [DOI] [PubMed] [Google Scholar]
- Sienkiewicz E, Magkos F, Aronis KN, Brinkoetter M, Chamberland JP, Chou S, Arampatzi KM, Gao C, Koniaris A, Mantzoros CS. Long-term metreleptin treatment increases bone mineral density and content at the lumbar spine of lean hypoleptinemic women. Metabolism. 2011;60:1211–1221. doi: 10.1016/j.metabol.2011.05.016. [DOI] [PubMed] [Google Scholar]
- Silva MJ. Biomechanics of osteoporotic fractures. Injury. 2007;38(Suppl 3):S69–76. doi: 10.1016/j.injury.2007.08.014. [DOI] [PubMed] [Google Scholar]
- Skerry TM. One mechanostat or many? Modifications of the site-specific response of bone to mechanical loading by nature and nurture. Journal of Musculoskeletal and Neuronal Interactions. 2006;6:122–127. [PubMed] [Google Scholar]
- Snow CM, Shaw JM, Winters KM, Witzke KA. Long-term exercise using weighted vests prevents hip bone loss in postmenopausal women. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2000;55:M489–M491. doi: 10.1093/gerona/55.9.m489. [DOI] [PubMed] [Google Scholar]
- Spector ER, Smith SM, Sibonga JD. Skeletal effects of long-duration head-down bed rest. Aviation, Space, and Environmental Medicine. 2009;80:A23–28. doi: 10.3357/asem.br02.2009. [DOI] [PubMed] [Google Scholar]
- Stunes AK, Westbroek I, Gordeladze JO, Gustafsson BI, Reseland JE, Syversen U. Systemic leptin administration in supraphysiological doses maintains bone mineral density and mechanical strength despite significant weight loss. Endocrinology. 2012;153:2245–2253. doi: 10.1210/en.2011-1848. [DOI] [PubMed] [Google Scholar]
- Sugiyama T, Meakin LB, Browne WJ, Galea GL, Price JS, Lanyon LE. Bones’ adaptive response to mechanical loading is essentially linear between the low strains associated with disuse and the high strains associated with the lamellar/woven bone transition. Journal of Bone and Mineral Research. 2012;27:1784–1793. doi: 10.1002/jbmr.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbott SM, Cifuentes M, Dunn MG, Shapses SA. Energy restriction reduces bone density and biomechanical properties in aged female rats. The Journal of Nutrition. 2001;131:2382–2387. doi: 10.1093/jn/131.9.2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson WR, Rubin CT, Rubin J. Mechanical regulation of signaling pathways in bone. Gene. 2012;503:179–193. doi: 10.1016/j.gene.2012.04.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian X, Jee WS, Li X, Paszty C, Ke HZ. Sclerostin antibody increases bone mass by stimulating bone formation and inhibiting bone resorption in a hindlimb-immobilization rat model. Bone. 2011;48:197–201. doi: 10.1016/j.bone.2010.09.009. [DOI] [PubMed] [Google Scholar]
- Trayhurn P, James W. Thermoregulation and non-shivering thermogenesis in the genetically obese (ob/ob) mouse. Pflugers Archiv - European Journal of Physiology. 1978;373:189–193. doi: 10.1007/BF00584859. [DOI] [PubMed] [Google Scholar]
- Trudel G, Payne M, Mädler B, Ramachandran N, Lecompte M, Wade C, Biolo G, Blanc S, Hughson R, Bear L. Bone marrow fat accumulation after 60 days of bed rest persisted 1 year after activities were resumed along with hemopoietic stimulation: the Women International Space Simulation for Exploration study. Journal of Applied Physiology. 2009;107:540–548. doi: 10.1152/japplphysiol.91530.2008. [DOI] [PubMed] [Google Scholar]
- Turner R, Iwaniec U. Moderate weight gain does not influence bone metabolism in skeletally mature female rats. Bone. 2010;47:631–635. doi: 10.1016/j.bone.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RT. Effects of short-term spaceflight and recombinant human growth hormone (rhGH) on bone growth in young rats. Aviation, Space, and Environmental Medicine. 1995;66:763–769. [PubMed] [Google Scholar]
- Turner RT. Invited review: what do we know about the effects of spaceflight on bone? Journal of Applied Physiology. 2000;89:840–847. doi: 10.1152/jappl.2000.89.2.840. [DOI] [PubMed] [Google Scholar]
- Turner RT. Skeletal adaptation to external loads optimizes mechanical properties: fact or fiction. Current Opinion in Orthopaedics. 2001;12:384–388. doi: 10.1097/00001433-200110000-00004. [DOI] [PubMed] [Google Scholar]
- Turner RT, Evans GL, Cavolina JM, Halloran B, Morey-Holton E. Programmed administration of parathyroid hormone increases bone formation and reduces bone loss in hindlimb-unloaded ovariectomized rats. Endocrinology. 1998;139:4086–4091. doi: 10.1210/endo.139.10.6227. [DOI] [PubMed] [Google Scholar]
- Turner RT, Iwaniec UT. Low dose parathyroid hormone maintains normal bone formation in adult male rats during rapid weight loss. Bone. 2011;48:726–732. doi: 10.1016/j.bone.2010.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RT, Kalra SP, Wong CP, Philbrick KA, Lindenmaier LB, Boghossian S, Iwaniec UT. Peripheral leptin regulates bone formation. Journal of Bone and Mineral Research. 2013;28:22–34. doi: 10.1002/jbmr.1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RT, Philbrick KA, Wong CP, Olson DA, Branscum AJ, Iwaniec UT. Morbid obesity attenuates the skeletal abnormalities associated with leptin deficiency in mice. Journal of Endocrinology. 2014;223:M1–15. doi: 10.1530/JOE-14-0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergnaud AC, Norat T, Mouw T, Romaguera D, May AM, Bueno-de-Mesquita HB, van der AD, Agudo A, Wareham N, Khaw KT, et al. Macronutrient composition of the diet and prospective weight change in participants of the EPIC-PANACEA study. PLoS One. 2013;8:e57300. doi: 10.1371/journal.pone.0057300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vico L, Collet P, Guignandon A, Lafage-Proust MH, Thomas T, Rehaillia M, Alexandre C. Effects of long-term microgravity exposure on cancellous and cortical weight-bearing bones of cosmonauts. Lancet. 2000;355:1607–1611. doi: 10.1016/s0140-6736(00)02217-0. [DOI] [PubMed] [Google Scholar]
- Vogiatzi MG, Autio KA, Mait JE, Schneider R, Lesser M, Giardina PJ. Low bone mineral density in adolescents with beta-thalassemia. Annals of the New York Academy of Sciences. 2005;1054:462–466. doi: 10.1196/annals.1345.063. [DOI] [PubMed] [Google Scholar]
- Von Thun NL, Sukumar D, Heymsfield SB, Shapses SA. Does bone loss begin after weight loss ends? Results 2 years after weight loss or regain in postmenopausal women. Menopause. 2014;21:501–508. doi: 10.1097/GME.0b013e3182a76fd5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade CE. Responses across the gravity continuum: hypergravity to microgravity. Advances in Space Biology and Medicine. 2005;10:225–245. doi: 10.1016/s1569-2574(05)10009-4. [DOI] [PubMed] [Google Scholar]
- Wang Q, Chen D, Cheng SM, Nicholson P, Alen M, Cheng S. Growth and aging of proximal femoral bone: a study with women spanning three generations. Journal of Bone and Mineral Research. 2015;30:528–534. doi: 10.1002/jbmr.2353. [DOI] [PubMed] [Google Scholar]
- Weigle DS. Human obesity. Exploding the myths. Western Journal of Medicine. 1990;153:421–428. [PMC free article] [PubMed] [Google Scholar]
- Weigle DS, Duell PB, Connor WE, Steiner RA, Soules MR, Kuijper JL. Effect of fasting, refeeding, and dietary fat restriction on plasma leptin levels. Journal of Clinical Endocrinology and Metabolism. 1997;82:561–565. doi: 10.1210/jcem.82.2.3757. [DOI] [PubMed] [Google Scholar]
- Westerlind KC, Wronski TJ, Ritman EL, Luo Z-P, An K-N, Bell NH, Turner RT. Estrogen regulates the rate of bone turnover but bone balance in ovariectomized rats is modulated by prevailing mechanical strain. Proceedings of the National Academy of Sciences. 1997;94:4199–4204. doi: 10.1073/pnas.94.8.4199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright NC, Saag KG, Curtis JR, Smith WK, Kilgore ML, Morrisey MA, Yun H, Zhang J, Delzell ES. Recent trends in hip fracture rates by race/ethnicity among older US adults. Journal of Bone and Mineral Research. 2012;27:2325–2332. doi: 10.1002/jbmr.1684. [DOI] [PubMed] [Google Scholar]
- Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. Journal of Clinical Investigation. 2003;112:1821. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu EW. Bone metabolism after bariatric surgery. Journal of Bone and Mineral Research. 2014;29:1507–1518. doi: 10.1002/jbmr.2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P, Peterson M, Su GL, Wang SC. Visceral adiposity is negatively associated with bone density and muscle attenuation. American Journal of Clinical Nutrition. 2015;101:337–343. doi: 10.3945/ajcn.113.081778. [DOI] [PMC free article] [PubMed] [Google Scholar]