Abstract
Background
Limited research addresses interventions to increase physical activity among American Indian and Hispanic preschool-aged children living in rural areas. We examined the impact of a Head Start-based intervention (Child Health Initiative for Lifelong Eating and Exercise [CHILE]) on physical activity at home.
Method
Sixteen Head Start centers in predominantly Hispanic or American Indian communities were group randomized to the six-component intervention or a comparison group for 2 years. Structured surveys were administered at four assessment times to a convenience sample of caregivers of 655 children in the study. Multilevel modeling was used to assess the effects of the intervention on physical activity.
Results
The relative change in physical activity in the intervention group compared with the comparison group over the 2-year period was 1.56 (95% confidence interval [1.02, 2.38]; p = .04). Among specific promoted activities (ball playing, dancing, active games, jumping, and walking), dancing increased significantly in the intervention compared with the comparison group (2.9; 95% confidence interval [1.2, 7.1]; p = .02).
Conclusions
The CHILE intervention was effective at increasing physical activity at home in preschool children in priority populations. Future research should focus on increasing family involvement and strengthening messaging about physical activity in these populations.
Keywords: child/adolescent health, chronic disease, community intervention, health disparities, health promotion, Latino, Native American/American Indian, physical activity
INTRODUCTION
Childhood obesity is a major public health concern, and Hispanic and American Indian (AI) children have higher rates of overweight and obesity than White children (Ogden, Carroll, Kit, & Flegal, 2014). Overweight and obese children are more likely to become obese adults, and obesity in adulthood is associated with cardiovascular disease and some cancers (Biro & Wien, 2010). Physical activity can help children maintain a healthy weight (Reilly, 2008). National guidelines call for preschool-aged children to have at least 60 minutes of structured and 60 minutes of unstructured physical activity per day (National Association for Sport and Physical Education, 2009) and 15 minutes of physical activity during each hour of the school day (Birch, Parker, & Burns, 2011), but these guidelines are not being met (Reilly, 2008). Moreover, children living in rural areas have a higher prevalence of sedentary behaviors than those in urban areas (Lutfiyya, Lipsky, Wisdom-Behounek, & Inpanbutr-Martinkus, 2007).
About one quarter of all preschool children are cared for in organized facilities, including Head Start (HS) centers (Laughlin, 2013). Few obesity interventions have focused exclusively on preschool children; in a systematic review, Waters et al. (2011) identified only eight studies that included a comparison group. Waters et al. (2011) conducted a meta-analysis of these studies and observed a trend toward a positive intervention effect. In a comparative effectiveness review and meta-analysis, Wang et al. (2013) found that physical activity interventions that were school-based but had a home component were beneficial for childhood obesity prevention. Although AI and Hispanic pre-school children represent priority populations for obesity prevention, interventions addressing these groups are rare (Tovar, Renzaho, Guerrero, Mena, & Ayala, 2014; Waters et al., 2011). The Child Health Initiative for Lifelong Eating and Exercise (CHILE) was an intervention developed to provide strategies for increasing physical activity in HS centers serving predominately Hispanic and AI children in rural areas of New Mexico.
BACKGROUND
In New Mexico, 59% of children who are 5 years of age or younger are Hispanic and 10% are AI (National Kids Count Data Center, 2015). In 2014, New Mexican Hispanic and AI kindergarten children had overweight/ obesity rates of 26.2% and 37.4%, respectively, whereas the rate in non-Hispanic White kindergarteners was 18.7% (New Mexico Department of Health, 2014a). Surveillance data are not available for preschool-aged children. New Mexico is one of the most rural states, with an average of only 17.2 people per square mile (New Mexico Department of Health, 2014b). Data from the 1996–2006 National Health and Nutrition Examination Survey and 2003 National Survey of Children’s Health showed that among children aged 2 to 5 years, 27.2% of those in rural areas were overweight and 12.2% were obese; the corresponding rates in urban children were 21.8% and 10.7% (Liu, Jones, Sun, & Probst, 2010).
In 2013, more than 7,000 New Mexican children were enrolled in HS centers (U.S. Department of Health and Human Services, 2013). CHILE, which is described in detail elsewhere (Cruz, Davis, FitzGerald, Canaca, & Keane, 2014; Davis et al., 2013), enrolled children attending 16 HS centers in an obesity prevention intervention that used a socioecological model (McLaren & Hawe, 2005). Briefly, CHILE included a nutrition and physical activity curriculum for the HS centers, professional development training for HS teachers and food service staff, an HS food service component, a family component focused on nutrition and physical activity, a local grocery store component, and a health care provider component. The analysis described in this article examined the effects of the CHILE intervention on the physical activity of children in the home environment.
METHOD
Design and Recruitment
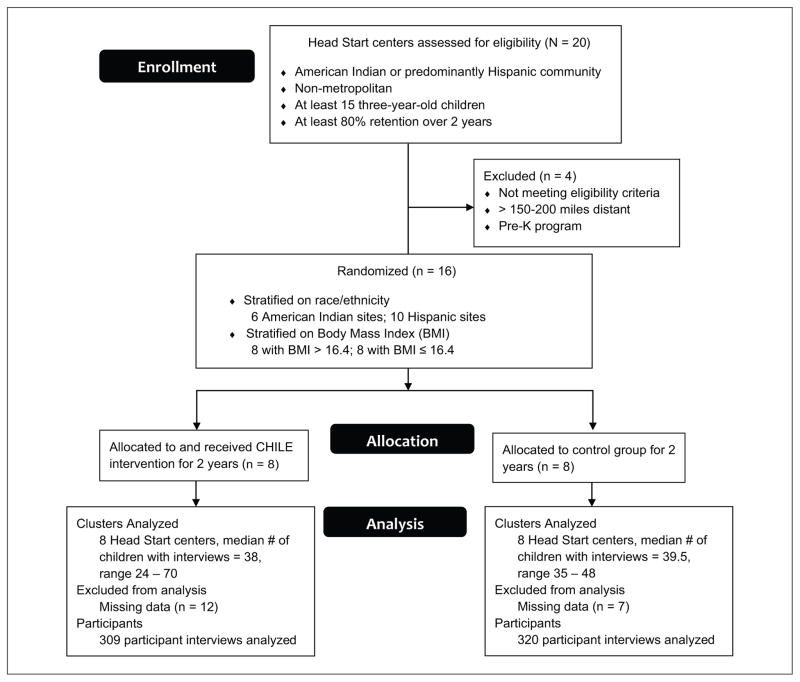
CHILE was a group randomized controlled trial (RCT) with a stratified cluster design (Figure 1). The HS centers were stratified according to body mass index (BMI; high and low) and race/ethnicity (AI or Hispanic), after which half were randomly assigned to the intervention or the comparison group (N = 8 per group). Randomization, intervention, and the intention-to-treat approach were at the group (HS center) level. Informed consent was obtained for all participants in CHILE, which was approved by the Human Research Review Committee of the University of New Mexico Health Sciences Center and conducted in accordance with HS center protocols and tribal processes.
FIGURE 1. Enrollment, allocation, and analysis of Surveys in the CHILE Intervention.
Note. CHILE = Child Health Initiative for Lifelong Eating and Exercise.
Trained research team members collected baseline and follow-up data through structured surveys administered in person at the beginning and end of each of 2 academic years (2008–2009 and 2009–2010). These proxy surveys about the children enrolled in CHILE were conducted with a parent or primary caregiver, usually the child’s mother. A convenience subsample of caregivers was recruited by hired local champions who assisted with coordination at each study site (HS center). The champions used a list of primary caregivers, a recruitment script, and a manual of procedures to recruit respondents and coordinate scheduling of the surveys. The goal was to recruit 20 respondents per study site during each survey period. Respondents who had previously been surveyed were prioritized to be surveyed again; thus, participants who started the study in fall 2008 could be surveyed up to four times during the study. Rolling admission policies and graduation of children to kindergarten after the first year of the intervention limited the opportunity for follow-up surveys.
Intervention
The CHILE intervention promoted physical activity through a classroom curriculum, professional development for HS teachers, family events at HS centers, and take-home materials distributed by teachers. The curriculum was designed to meet HS objectives and learning domains and to fit into the HS center day. Physical activities ranged from 5-minute activity bursts to 30-minute sessions that included a warm-up, two activities, and a cool-down. The teacher training addressed ways to promote developmentally appropriate physical activity for 3- to 5-year-old children and included demonstrations and hands-on practice of new physical activities and games. Quarterly family events included active games and activities for families, as well as physical activity performances by children. Take-home materials described specific activities for families to engage in with their children. Activities that are developmentally appropriate and safe for preschool-aged children, as well as suitable for a rural setting, were emphasized and categorized as ball playing (catching, kicking, rolling, and throwing), dancing, playing active games, jumping, or walking. The HS centers in the comparison group participated in usual physical activity practices.
Surveys
The structured surveys took approximately 1 hour and focused on health behaviors, familial and household factors, and demographic and other characteristics of the children, their parents, and the community. Questions on physical activity were adapted from a questionnaire used in a previous study of AI and Hispanic fourth and fifth graders (Going et al., 2003). A list of activities appropriate for preschool-aged children was obtained from an observational instrument for preschool children (McKenzie, Marshall, Sallis, & Conway, 2000). During the survey, a member of the research team read the list of common play activities and asked how often the child participated in each (“never,” “sometimes,” or “often”).
A total of 988 surveys (77.2% of the targeted number of 1,280 based on 20 surveys per site per time period) were conducted with the parents or primary caregivers of 655 children. Fourteen surveys were excluded because of a child’s medical condition (N = 5) or incomplete data (N = 9). The remaining 974 surveys with parents (88.2%) or caregivers (11.8%) of 648 children were retained for analysis. Most children (62.0%) had one parent or caregiver survey; 28.7% had two; 6.2% had three; and 3.1% had four. For 46 children (18.5%), surveys were obtained both at baseline (fall 2008) and after the intervention (spring 2010).
Original sample sizes were based on a change in BMI for the main cluster-randomized study of 16 HS centers. For a binary physical activity outcome, a comparison between intervention and comparison sites in the final measurement would have approximately 80% statistical power (two-sided α = .05) if the odds for more frequent physical activity were between about 1.9 and 2.8 for a balanced cluster sample size of 20, intra-class correlations between .002 and .01, and control relative frequencies between .5 and .8.
Data Analysis
Descriptive statistics were generated for the demographic, behavioral, and outcome variables. The five promoted physical activity behaviors were dichotomized before analysis on the basis of whether the response was for the most frequent participation (“often” vs. “sometimes” or “never”). Generalized mixed-model regression analyses were used to predict participation in each behavior while accounting for repeated measurements on children that were nested within HS centers. Models included a random HS center effect and fixed effects for HS center race/ethnicity strata, prestudy BMI strata, year of study, second-year baseline, gender, age at enrollment, highest level of education of parents, sampling period, intervention, and period by intervention. The year of study and second-year baseline effects were required to account for rolling recruitment of participants. The primary test of intervention was a contrast of the pre-to-post change (fall 2008 to spring 2010) among intervention sites compared with comparison sites. Four of the HS centers participating in CHILE began offering prekindergarten (pre-K) programs after the study began, and some of the children in the study enrolled in these programs. Data obtained from these children after pre-K program enrollment were excluded from the analyses, and a covariate was added to the analyses to account for the dropouts.
The combined effect of the intervention on the five promoted physical activities was also assessed by using a multivariate, generalized, mixed-model analysis. The analysis mirrored the individual analyses but assessed all five outcomes simultaneously, with parameters to account for differences among mean responses and inclusion of unstructured variances and covariances among the five measures. There were no missing data at the level of the intervention: All HS centers were measured on each occasion. Missing child-level data reduced the power for assessing the center-level intervention. Analyses included an effect for the drop out to pre-K and prestudy BMI strata and covariates for race/ ethnicity, age, gender, highest level of parental education, and year of study. These covariates help justify the missing at-random assumption that is required for unbiased estimates of intervention effects by maximum likelihood (Little & Rubin, 2002).
The magnitude of the intervention effect was summarized as the exponentiated contrast estimate, with 95% confidence intervals (CIs). For reporting purposes, the marginal estimated probability that behaviors were reported as “often” for period-by-intervention combinations and the 95% CIs were scaled.
RESULTS
Characteristics of the 648 children with valid caregiver surveys are shown in Table 1. Approximately 60% of the children were Hispanic and 40% were AI, which is representative of the communities in which the HS centers participating in CHILE were located. The children in the intervention and comparison groups were similar with respect to age, gender, race, ethnicity, and perceived neighborhood safety. Parents of children in the intervention sites were significantly more likely to have more than a high school education (p < .001). Of the 648 children, 629 had valid height and weight measurements and were included in the physical activity analysis. At baseline (fall 2008), of the 284 children with valid height and weight measurements and at least one survey, 83 (29.2%) were overweight or obese (BMI ≥85th percentile for age and gender) and 39 (13.7%) were obese (BMI ≥ 95th percentile for age and gender). There was no significant difference between the intervention and comparison groups in weight status at baseline.
TABLE 1.
Characteristics of all Children, and according to Study group, at the Time of the First Caregiver Surveya
| Characteristic | All Children (N = 648) | Intervention Group (n = 321) | Comparison Group (n = 327) |
|---|---|---|---|
| M (SE) age, years | 4.1 (0.7) | 4.1 (0.7) | 4.1 (0.7) |
| Gender | |||
| Female | 323 (49.8) | 164 (51.0) | 159 (48.6) |
| Male | 325 (50.2) | 157 (49.0) | 168 (51.4) |
| Hispanic ethnicity | 386 (59.5) | 201 (62.6) | 185 (56.5) |
| Race of child | |||
| White | 357 (55.0) | 179 (55.7) | 178 (54.4) |
| American Indian | 243 (37.5) | 118 (36.7) | 125 (38.2) |
| Mixed race | 39 (6.0) | 18 (5.6) | 21 (6.4) |
| Other | 9 (1.3) | 6 (1.8) | 3 (0.9) |
| Head Start center race/ethnicity | |||
| American Indian | 249 (38.4) | 124 (38.6) | 125 (38.2) |
| Hispanic | 399 (61.5) | 197 (61.3) | 202 (61.7) |
| ≥1 Parent with >high school educationb | 329 (51.2) | 185 (58.1) | 144 (44.4)c |
| Neighborhood safe for outdoor play | 559 (87.0) | 283 (88.9) | 276 (85.1) |
Values are number (percentage) unless otherwise indicated.
Education data missing for six surveys.
Significantly different from intervention group (p < .001).
Table 2 shows data on the specific activities that the children in the two study groups were reported to engage in “often” at the four assessment times, as well as information on the change from baseline to the final assessment. Of the five activities assessed, only dancing showed a significant increase in the intervention group compared with the comparison group (p = .02).
TABLE 2.
Children Engaging in Physical activity Behaviors “often” at Baseline and at Three Postintervention assessment Times, according to Study group and With Change analysis
| Activity/Group | Assessment Time, % (SE)
|
Change: Fall 2008 to Spring 2010 | Relative Change: Intervention Versus Comparison (95% CI)a | |||
|---|---|---|---|---|---|---|
| Fall 2008 (Baseline) | Spring 2009 | Fall 2009 | Spring 2010 | |||
| Ball playing | ||||||
| Intervention | 65.9 (6.2) | 62.3 (6.7) | 67.1 (5.7) | 74.1 (3.8) | +8.2 | |
| Comparison | 74.9 (5.3) | 60.6 (6.3) | 67.8 (4.2) | 70.4 (4.0) | −4.5 | 1.9 [0.8, 4.5] |
| Dancing | ||||||
| Intervention | 59.6 (6.9) | 68.4 (6.7) | 75.7 (5.4) | 75.7 (3.9) | +16.1 | |
| Comparison | 66.2 (6.2) | 58.3 (6.7) | 65.3 (4.6) | 55.6 (4.9) | −10.6 | 3.3 [1.4, 8.1]b |
| Playing active games | ||||||
| Intervention | 62.3 (6.3) | 62.5 (6.5) | 56.2 (6.0) | 73.1 (3.8) | +10.8 | |
| Comparison | 61.6 (6.1) | 56.5 (6.3) | 66.1 (4.2) | 67.5 (4.1) | +5.9 | 1.3 [0.6, 2.9] |
| Jumping | ||||||
| Intervention | 69.7 (6.1) | 74.7 (5.9) | 81.2 (4.6) | 81.5 (3.5) | +11.8 | |
| Comparison | 68.2 (6.0) | 66.4 (6.2) | 76.9 (3.7) | 73.6 (3.9) | +5.4 | 1.5 [0.6, 3.6] |
| Walking | ||||||
| Intervention | 53.5 (6.5) | 61.0 (6.6) | 50.0 (5.9) | 55.8 (4.4) | + 2.5 | |
| Comparison | 58.8 (6.1) | 49.5 (6.3) | 56.4 (4.5) | 57.5 (4.4) | −1.3 | 1.2 [0.5, 2.6] |
NOTE: CI = confidence interval.
Adjusted for Head Start center race/ethnicity, prestudy body mass index strata, gender, age at enrollment, late entry into study, parental education, sample period, and drop out to attend a prekindergarten program.
Significant contrast (p < .01).
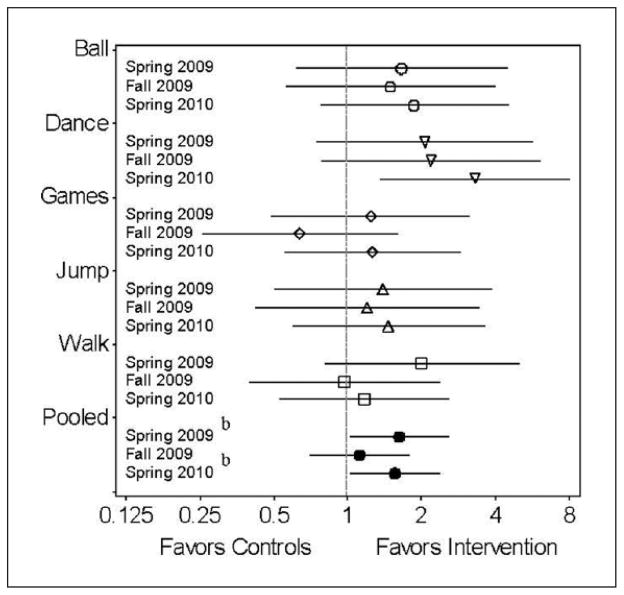
As shown in Figure 2, the pooled physical activity relative change from baseline for the intervention group was increased significantly relative to the comparison group at the spring 2009 (1.63; 95% CI [1.02, 2.59]) and spring 2010 (1.56; 95% CI [1.02, 2.38]) assessments but was not significantly different in fall 2009 (1.12; 95% CI [0.70, 1.79]).
FIGURE 2. Specific activities and Pooled activity relative Changesa (95% Confidence Intervals; Log 2 Scale), according to assessment Time, in the Control Compared with the CHILE Intervention group.
NOTE: CHILE = Child Health Initiative for Lifelong Eating and Exercise.
aRelative changes values were adjusted for Head Start center race/ ethnicity, prestudy body mass index strata, parent education level, sampling period, and drop out to attend another prekindergarten program. bSignificant difference (p < .05)
Frequencies of the five assessed physical activity behaviors were not significantly associated with community race/ethnicity strata, neighborhood safety, parental education, or baseline BMI. Compared with boys, girls were less likely to engage in playing ball “often” (odds ratio [OR] = 0.38; 95% CI [0.27, 0.53]) and more likely to engage in dancing “often” (OR = 4.31; 95% CI [3.03, 6.13]). Analyses conducted to assess whether intervention effects were different for boys and girls did not detect a significant interaction.
DISCUSSION
The aim of this analysis was to describe the effects of CHILE, a preschool-based, transcommunity obesity prevention intervention, on physical activity at home among predominantly Hispanic and AI children. Exposure to the intervention resulted in a significant increase in dancing (one of the promoted activities) among the children. In addition, a pooled analysis of the five promoted activities showed increases over time in the intervention group relative to the comparison group.
There are several possible reasons for the lack of significant increases in the other four physical activity behaviors (ball playing, playing active games, jumping, and walking). Power was calculated on the basis of the main outcome (BMI) and may have been insufficient to detect a difference in each physical activity behavior at home. The intensity and duration of the family component of the intervention may have been inadequate. In 2013, 29.4% of Hispanic and 26.6% of AI adults in New Mexico reported no leisure-time physical activity (New Mexico Department of Health, 2013). Some previous research showed that addressing diet, physical activity, and behavior change among mothers of children aged 1 to 3 years increased physical activity among both the mothers and their children (Klohe-Lehman et al., 2007). Therefore, a more intense focus on physical activity of adults may increase physical activity of young children. On the other hand, Fitzgibbon et al. (2013) found that an HS center– and family-based intervention to prevent obesity in Hispanic preschool children, partly by increasing physical activity among parents, did not produce results that differed significantly from those in a comparison group.
The systematic review by Tovar et al. (2014) included eight interventions to prevent obesity (primarily RCTs) among primarily Hispanic children (51% to 100% of children enrolled; N = 33–401) with a mean age of under 5 years. Five of the eight interventions were based in HS centers or preschools. All five had physical activity components, but only four (Bellows, Davies, Anderson, & Kennedy, 2013; Fitzgibbon et al., 2006; Fitzgibbon et al., 2013; Yin et al., 2012) included physical activity as a primary or secondary outcome. The results were mixed: One study (Yin et al., 2012) showed a significant increase in overall physical activity in the intervention group; the other three (Bellows et al., 2013; Fitzgibbon et al., 2006; Fitzgibbon et al., 2013) did not.
Physical activity interventions among preschool-aged AI and rural children are uncommon. Only one of the studies reviewed by Waters et al. (2011), a pilot RCT conducted more than 15 years ago in northern New York and southern Canada (Harvey-Berino & Rourke, 2003), focused on preschool AI children (N = 43 mother/child pairs). The intervention, a home-visiting program delivered by AI peer educators, had no significant effect on children’s physical activity levels as measured by an accelerometer. A more recent intervention among 454 AI children in kindergarten or the first grade in South Dakota (Story et al., 2012) did not significantly change the duration of physical activity in school.
Our study was unique in that it investigated the effects of an intervention on specific physical activities at home among Hispanic and AI preschool children in HS centers in rural areas. Several of our findings are notable. There was a difference between girls and boys in activities participated in more often (dancing among girls and playing ball among boys), although no gender-specific significant differences in physical activity were observed. The difference between girls and boys with respect to dancing and ball playing may have been due to cultural influences, societal expectations, or other environmental characteristics (Thomas & French, 1985). Of the five physical activities studied, the greatest postintervention increase occurred in dancing. Dancing has been identified as being particularly suited to preschoolers, who are exploring their physical abilities and beginning to understand and follow rules (Feigelman, 2007). Dance-type activities in the HS classroom and at home should therefore provide an excellent vehicle for maintaining physical activity levels, especially among girls. Dancing is easy for teachers and families to encourage in children because it requires minimal equipment and skills and is tied to community and culture.
Limitations of this study included the lack of a direct measure of physical activity. Direct observation plus accelerometer use represents the current standard method for evaluating physical activity in preschool-aged children (Pate, O’Neill, & Mitchell, 2010). However, at the time of pilot testing for CHILE (2006), the formative assessment determined that the accelerometers available were impractical for use in the priority populations in the study. The primary focus on BMI measurement and the larger-than-expected sample size (90% of eligible children enrolled) further limited our ability to employ direct measurement techniques.
Another limitation was that validated questionnaires for caregiver proxy report of physical activity in preschool children were not readily available at the onset of the study. Moreover, a summary of self-report measures by Sternfeld and Goldman-Rosas (2012) did not include any for young children. The instrument used in this research was adapted from one employed in studies of fourth- and fifth-grade students and included activities appropriate for preschool-aged children, as described in the SOPLAY observational instrument (McKenzie et al., 2000). Furthermore, the questions in our survey were developed to address the specific categories of physical activity promoted by CHILE.
The feasibility, reliability, and validity of parental proxy reports on children’s health-related quality of life have been demonstrated (Varni, Limbers, & Burwinkle, 2007). Parental proxy reports of physical activity may be suitable for some studies (Pate et al., 2010), but investigations of these reports are limited, and poor to fair correlation of proxy records with accelerometer data has been observed (Pate et al., 2010). Differences between accelerometer and self-report data may result from social desirability bias, the challenge of remembering and estimating the frequency and duration of physical activity, or problems related to wearing an accelerometer (de Leeuw, Borgers, & Smits 2004).
Other possible limitations of our study include possible selection bias resulting from use of a convenience sample of survey participants, the broad outcome-measure categories (“never,” “sometimes,” and “often”), and the significant difference between the intervention and comparison group in parental education level at baseline.
Strengths of the CHILE intervention and its assessment include a focus on priority populations at high risk of childhood obesity; the group RCT design; the socioecological, transcommunity approach; the use of multilevel modeling to evaluate intervention effects on physical activity; and the commitment to community-engaged research that incorporates age-appropriate and culturally relevant physical activity.
CONCLUSIONS
An HS-based, transcommunity obesity prevention intervention was effective in increasing physical activity at home among Hispanic and AI preschool-aged children. A socioecological model incorporating six components, including family participation, was used to achieve the effects. Dissemination and implementation of the CHILE intervention provides an effective mechanism for increasing physical activity in these priority populations. CHILE has expanded to become CHILE Plus and has reached children through 21 additional HS centers in New Mexico and is being adapted for use in other child care settings. Future research should focus on strategies that increase family involvement and strengthen messaging about the importance of physical activity.
Acknowledgments
We express our deepest appreciation to the teachers, staff, and administration at the participating Head Start centers, as well as families and other community members who assisted in the development, implementation, and evaluation of the CHILE study. We wish to thank members of the CHILE research team who contributed their time and expertise to the work represented here. We would also like to thank Alexandra Borosova, MSc, for her assistance with the literature review and for contributing to and reviewing drafts of the manuscript, and Elizabeth Yakes-Jimenez, PhD, at the University of New Mexico for her critical review of the manuscript. Lastly, we would like to express our gratitude to the National Institute of Diabetes and Digestive and Kidney Diseases for the financial support to carry out this research. This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases Grant No. 1 R01 DK72958-01. This study is registered at Clinicaltrials.gov (No. NCT00428805).
References
- Bellows LL, Davies PL, Anderson J, Kennedy C. Effectiveness of a physical activity intervention for Head Start preschoolers: A randomized intervention study. American Journal of Occupational Therapy. 2013;67:28–36. doi: 10.5014/ajot.2013.005777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Parker L, Burns A, editors. Early childhood obesity prevention policies. Washington, DC: National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biro FM, Wien M. Childhood obesity and adult morbidities. American Journal of Clinical Nutrition. 2010;91(Suppl 5):1499S–1505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz TH, Davis SM, FitzGerald CA, Canaca GF, Keane PC. Engagement, recruitment, and retention in a trans-community, randomized controlled trial for the prevention of obesity in rural American Indian and Hispanic children. Journal of Primary Prevention. 2014;35:135–149. doi: 10.1111/josh.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis SM, Sanders SG, Fitzgerald C, Keane P, Canaca G, Volker-Rector R. CHILE: An evidence-based preschool intervention for obesity prevention in Head Start. Journal of School Health. 2013;83:223–229. doi: 10.1111/josh.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leeuw E, Borgers N, Smits A. Pretesting questionnaires for children and adolescents. In: Presser S, Rothgeb JM, Couper MP, Lessler JT, Martin E, Martin J, Singer E, editors. Methods for testing and evaluating survey questionnaires. Hoboken, NJ: Wiley; 2004. pp. 409–412. [Google Scholar]
- Feigelman S. The preschool years. In: Kliegman R, Behrman RE, Jenson HB, Stanton BM, editors. Nelson textbook of pediatrics. 18. Philadelphia, PA: Saunders; 2007. pp. 54–57. [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Kong A, Braunschweig CL, Gomez-Perez SL, … Dyer AR. Family-based hip-hop to health: Outcome results. Obesity (Silver Spring) 2013;21:274–283. doi: 10.1002/oby.20269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity. 2006;14:1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- Going S, Thompson J, Cano S, Stewart D, Stone E, Harnack L, … Corbin C. The effects of the pathways obesity prevention program on physical activity in American Indian children. Preventive Medicine. 2003;37(6 Pt 1):S62–S69. doi: 10.1016/j.ypmed.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, Rourke J. Obesity prevention in pre-school Native-American children: A pilot study using home visiting. Obesity Research. 2003;11:606–611. doi: 10.1038/oby.2003.87. [DOI] [PubMed] [Google Scholar]
- Klohe-Lehman DM, Freeland-Graves J, Clarke KK, Cai G, Voruganti VS, Milani TJ, … Bohman TM. Low-income, overweight and obese mothers as agents of change to improve food choices, fat habits, and physical activity in their 1-to-3-year-old children. Journal of the American College of Nutrition. 2007;26:196–208. doi: 10.1080/07315724.2007.10719602. [DOI] [PubMed] [Google Scholar]
- Laughlin L. Who’s minding the kids? Child care arrangements: Spring 2011. Washington, DC: U.S. Census Bureau; 2013. Retrieved from https://www.census.gov/prod/2013pubs/p70-135.pdf. [Google Scholar]
- Little R, Rubin D. Statistical analysis with missing data. 2. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- Liu J, Jones SJ, Sun H, Probst JC. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: An urban and rural comparison. Columbia: South Carolina Rural Health Research Center; 2010. Retrieved from http://rhr.sph.sc.edu/report/(9-1)Diet,%20Physical%20Activity%20and%20Sedentary%20Behaviors.pdf. [DOI] [PubMed] [Google Scholar]
- Lutfiyya MN, Lipsky MS, Wisdom-Behounek J, Inpanbutr-Martinkus M. Is rural residency a risk factor for overweight and obesity for U.S. children? Obesity. 2007;15:2348–2356. doi: 10.1038/oby.2007.278. [DOI] [PubMed] [Google Scholar]
- McKenzie TL, Marshall SJ, Sallis JF, Conway TL. Leisure-time physical activity in school environments: An observational study using SOPLAY. Preventive Medicine. 2000;30:70–77. doi: 10.1006/pmed.1999.0591. [DOI] [PubMed] [Google Scholar]
- McLaren L, Hawe P. Ecological perspectives in health research. Journal of Epidemiology & Community Health. 2005;59:6–14. doi: 10.1136/jech.2003.018044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association for Sport and Physical Education. Active Start: A statement of physical activity guidelines for children from birth to age 5. 2. Sewickley, PA: American Alliance for Health, Physical Education, Recreation, and Dance; 2009. [Google Scholar]
- National Kids Count Data Center. Child population by race and age group, 2013. Baltimore, MD: Annie E. Casey Foundation; 2015. Retrieved from http://datacenter.kidscount.org/data/tables/8446-child-population-by-race-and-age-group?loc=1&loct=1#detailed/2/2,33-34/false/36/13,66,67,68,69,70,71,12|/17077,17078. [Google Scholar]
- New Mexico Department of Health. Indicator-based information system for public health: Query results for New Mexico behavioral risk factor surveillance system data. 2013 Retrieved from http://ibis.health.state.nm.us/
- New Mexico Department of Health. Healthy Kids New Mexico, 2014. New Mexico childhood obesity 2014 update. 2014a Retrieved from http://nmhealth.org/data/view/chronic/1585/
- New Mexico Department of Health. New Mexico state health improvement plan. 2014b Retrieved from http://nmhealth.org/publication/view/plan/411/
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. Journal of the American Medical Association. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pate RR, O’Neill JR, Mitchell J. Measurement of physical activity in preschool children. Medicine & Science in Sports&Exercise. 2010;42:508–512. doi: 10.1249/MSS.0b013e3181cea116. [DOI] [PubMed] [Google Scholar]
- Reilly JJ. Physical activity, sedentary behaviour and energy balance in the preschool child: Opportunities for early obesity prevention. Proceedings of the Nutrition Society. 2008;67:317–325. doi: 10.1017/S0029665108008604. [DOI] [PubMed] [Google Scholar]
- Sternfeld B, Goldman-Rosas L. A systematic approach to selecting an appropriate measure of self-reported physical activity or sedentary behavior. Journal of Physical Activity & Health. 2012;9(Suppl 1):S19–S28. doi: 10.1123/jpah.9.s1.s19. [DOI] [PubMed] [Google Scholar]
- Story M, Hannan PJ, Fulkerson JA, Holy Rock B, Smyth M, Arcan C, Himes JA. Bright Start: Description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity. 2012;20:2241–2249. doi: 10.1038/oby.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JR, French KE. Gender differences across age in motor performance a meta-analysis. Psychological Bulletin. 1985;98:260–282. [PubMed] [Google Scholar]
- Tovar A, Renzaho AM, Guerrero AD, Mena N, Ayala GX. A systematic review of obesity prevention intervention studies among immigrant populations in the US. Current Obesity Reports. 2014;3:206–222. doi: 10.1007/s13679-014-0101-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Head Start program facts: fiscal year 2013. 2013 Retrieved from https://eclkc.ohs.acf.hhs.gov/hslc/data/factsheets/docs/hs-program-fact-sheet-2013.pdf.
- Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: An analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 generic core scales. Health and Quality of Life Outcomes. 2007;5:2. doi: 10.1186/1477-7525-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C, … Segal J. Childhood obesity prevention programs: Comparative effectiveness review and meta-analysis. Rockville, MD: Agency for Healthcare Research and Quality; 2013. Comparative Effectiveness Review No. 115. [PubMed] [Google Scholar]
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, Summerbell CD. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews. 2011;(3):CD00187. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- Yin Z, Parra-Medina D, Cordova A, He M, Trummer V, Sosa E, … Ramirez A. Míranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Childhood Obesity. 2012;8:429–439. doi: 10.1089/chi.2012.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]