SUMMARY
We document the recent profile of health insurance and health care among mid-aged and older Chinese using data from the China Health and Retirement Longitudinal Study conducted in 2011. Overall health insurance coverage is about 93%. Multivariate regressions show that respondents with lower income as measured by per capita expenditure have a lower chance of being insured, as do the less-educated, older, and divorced/widowed women and rural-registered people. Premiums and reimbursement rates of health insurance vary significantly by schemes. Inpatient reimbursement rates for urban people increase with total cost to a plateau of 60%; rural people receive much less. Demographic characteristics such as age, education, marriage status, per capita expenditure, and self-reported health status are not significantly associated with share of out-of-pocket cost after controlling community effects. For health service use, we find large gaps that vary across health insurance plans, especially for inpatient service. People with access to urban health insurance plans are more likely to use health services. In general, Chinese people have easy access to median low-level medical facilities. It is also not difficult to access general hospitals or specialized hospitals, but there exists better access to healthcare facilities in urban areas.
Keywords: health insurance, health care, CHARLS
1. INTRODUCTION
China has conducted a series of health reforms during the past two decades, including expanding its health insurance coverage and reforming its health service system, with the ultimate goal of affordable and equitable health care for all. The reform employed the strategy of universal coverage with shallow benefits at the beginning and progressed with expanded benefits (Yip et al., 2012). The two new programs, the New Rural Cooperative Medical Scheme (NCMS) and the Urban Resident Medical Insurance (URMI), expanded rapidly since their introduction in 2003 and 2007, respectively. These two programs, together with the existing Urban Employee Medical Insurance (UEMI), covered nearly 95% of the population by the end of 2011, that is, almost reaching the goal of universal coverage.1 However, the detailed terms of coverage in China are still very unequal across different sub-populations, and so, China’s rapid health reform has not reached a universal level of generosity compared with other countries and regions such as the UK and Taiwan.
China started with a highly segmented health insurance system with eligibility and benefits conditional on occupation and urban/rural registration. Taiwan is an example, which had similarly segmented insurance coverage, but has greatly reduced these disparities when a universal social insurance program replaced a patchwork of separate social health insurance funds in 1995 (Cheng, 2003). China has experienced extremely rapid economic growth accompanied by an unprecedented mobility of population. As a result, boundaries between rural-registered and urban-registered population have become increasingly blurred, and occupational mobility is on the rise. In the area of health insurance, great strides have been made to expand coverage to the rural population (Strauss et al., 2012), and benefits have also been converging (Barber and Yao, 2010). But significant gaps in benefits still exist, which poses barriers to eventual unification of health insurance programs. Over time, we expect benefits to continue to converge, perhaps in the long run similar to Taiwan.
In this paper, we document the extent of differences between programs. China now has more than four social insurance programs targeting different groups of population with quite different levels of reimbursement rates. For instance, the median of reimbursement rate of the UEMI for inpatient cost is about 66%, while that of NCMS is only 25%. Differences in reimbursement rates may then result in inequalities in utilization of health services, at the moment strongly favoring a subset of urban hukou holders.
So after a large set of health reforms, what is the profile of health insurance coverage and that of healthcare burden given both rising health insurance generosity and rising healthcare cost? How large are the differences in health insurance programs targeting different groups, and what are the implications of such difference on health service utilization?
In this paper, using a national representative survey data collected during 2011–2012, we document the key parameters of various health insurance programs in China and the profile of health service utilization among mid-aged and older Chinese. We also examine the disparity of availability of health insurance and health service among people with different socioeconomic status (SES). Estimates using China Health and Retirement Longitudinal Study (CHARLS) data show that overall health insurance coverage of the mid-aged and older Chinese is about 93%, with more than 95% of the insured covered by one of the three main insurance schemes: NCMS, UEMI, and URMI. That is, the health insurance coverage is near universal among the mid-aged and older Chinese. However, discrepancy exists across population, and benefits vary across insurance programs. We also find large differences in accessibility of healthcare facilities between those with and without health insurance and between rural and urban residents. These results indicate that although China has made great progress in the past decades, it is, to some extent, still at the beginning of the journey towards affordable and equitable health care to all.
The rest of this paper is laid out as follows: We briefly review the literature in Section 2, describe the data in Section 3, and then display empirical results in Section 4. Section 5 concludes the paper.
2. LITERATURE REVIEW
There is a growing literature analyzing China’s health reforms in recent years (see, for instance, a recent issue of Health Economics devoted to this topic, Wagstaff et al., 2009). Some papers focus on health insurance, while others focus on health service usage. Most papers focus only on the urban or only the rural population at one time. Strauss et al. (2012) use the CHARLS Pilot data from Gansu and Zhejiang provinces to explore many of the same issues discussed in this paper. This paper extends it by using representative national data. The national survey data with a much larger sample size allow us to draw conclusions for the whole nation and examine relevant issues in detailed ways (like examining correlates of health insurance access by schemes).
As the most important and also the only medical insurance scheme targeting rural people, the NCMS has attracted numerous studies (see You and Kobayashi, 2009, for a review of early studies). Most recent studies focus on the impact of access to NCMS on health service use and show mixed results. Wagstaff et al. (2009) employ a difference-in-difference strategy to estimate the effect of NCMS on health service utilization and health service costs, and they find that access to NCMS increases healthcare utilization but has no effects on out-of-pocket (OOP) expenditures. Similar results were found by Lei and Lin (2009). On the contrary, using survey data from two provinces, Yu et al. (2010) find no significant correlation between NCMS membership and outpatient service utilization. Using survey data from 25 rural counties, Babiarz et al. (2010) estimate the effects of NCMS on healthcare utilization and healthcare expenditure and find NCMS is associated with a significant increase in village clinic use, but no changes in overall care use; they also find OOP medical spending decreases with access to NCMS. Zhang et al. (2014), using data from the rural area of Jiangsu Province, show that increase in the yearly maximum reimbursement amount of NCMS is associated with an increase in yearly total expenses for patients with type 2 diabetes mellitus, but not with the utilization of different types of health institutions. Discrepancies in findings of previous studies may come from the fact that most of them are using data from one or two provinces, or merely focus on specific groups like those with diabetes in Zhang et al. (2014).
Various studies have been carried out on the URMI, focusing on its targeting urban people without access to the UEMI program. Lin et al. (2009) examine who participates and who benefits using survey data from 79 pilot cities. They find a U-shaped relationship between URMI participation rate and income; that is, the extremely rich or poor are the most likely to participate. They also find that those participants in the bottom 20% of family incomes are happier with URMI than are their more affluent counterparts. Liu and Zhao (2012) show that the introduction of the URMI is significantly associated with increased utilization of formal medical services but not with OOP expenditure.
Other papers focus on health service utilization. Eggleston et al. (2008) provide a review on health service delivery in China, in which they pay special attention on how well China’s healthcare providers perform and what determines their performance. They conclude that China’s current health service delivery leaves room for improvement in terms of quality, responsiveness to patients, efficiency, cost escalation, and equity. They suggest that these problems will not be solved by simply shifting ownership to the private sector or by encouraging providers to compete with one another. Qian et al. (2009) estimate the determinants of healthcare demand using survey data from rural area in Gansu Province and find price and distance play significant roles in choice of healthcare provider. They also find access to health insurance, age, and attributes of illness are significantly related to healthcare demand. Hu et al. (2008) discuss the challenges and opportunities of reform of how health care is paid for in China. They argue that the problems include high levels of OOP payments, stalled progress in providing adequate insurance for all, widespread inefficiencies in health facilities, uneven quality, extensive inequality, and perverse incentives for hospitals and doctors. By reviewing experience of other countries, they claim that the prospects that China will complete the health system transformation successfully in the next two decades are good.
Some studies also discuss the disparities in health and health care across regions in China. Tang et al. (2008) and Zhang and Kanbur (2005) investigate the spatial inequality in health and health care in China, respectively. Besides variation across regions, distinctive attributes of urban and rural settings are more prominent in China (Hu et al., 2008). Even though the implementation of the NCMS since 2003 has covered more than 90% of rural residents, there are evident disparities both across counties and compared with urban plans in reimbursement rate and health service access. On the one hand, urban–rural differences in China are similar to other countries as urban–rural status is closely related to occupational status.2 Occupational differences in health insurance and health service utilization have been explicitly discussed by Frenk et al. (2006), Knaul and Frenk (2005) for Mexico, and Ellis et al. (2000) and Yip and Mahal (2008) for India. On the other hand, the urban–rural differences are more complicated than the occupational/regional differences in China, because of the strict regulation of its hukou system. Private-sector workers with rural hukou are still not eligible for health insurance funded through payroll contributions. Besides the registration status, China’s hukou system also creates spatial segregation, deterring high-level pooling of the health insurance funding. Some studies have discussed the urban–rural disparities in health care in China before the near-universal coverage of health insurance and have consistently documented significant disparities between rural and urban residents in health service utilization (Shi, 1993; Liu et al., 1999; Liu et al., 2007; Yip and Mahal, 2008; Yip, 2010). In general, these studies show that rural residents are disadvantaged in access to health care and are less likely to use inpatient services. More recently, using national survey data from both 2003 and 2008, Jian et al. (2010) show that at the national level, the urban–rural gap in use of inpatient service and OOP medical spending had significantly narrowed from 2003 to 2008, but the gains were uneven across regions.
3. DATA AND EMPIRICAL SPECIFICATIONS
We use data from a newly completed nationwide household survey in China: the CHARLS. CHARLS is a biennial survey conducted by the National School of Development at Peking University, aiming to be representative of the Chinese residents aged 45 years and older and their spouses. CHARLS is part of a set of longitudinal aging surveys that include the Health and Retirement Study in the USA, the English Longitudinal Study of Aging, the Survey of Health, Ageing and Retirement in Europe, the Korean Longitudinal Study of Aging, the Japanese Study of Aging and Retirement, and the Longitudinal Aging Study in India.
Data used here come from the national baseline survey of CHARLS conducted during 2011–2012 (see Zhao et al., 2013, for a complete discussion). The sample was drawn in four stages. County-level units (counties or urban districts) were sampled directly. All county-level units in all provinces except for Tibet were stratified by eight regions, by whether they were urban districts (qu) or rural counties (xian), and by county gross domestic product. They were sorted based on this stratification, and 150 were randomly chosen proportional to population size.3 These counties cover 28 out of 30 provinces in mainland China, other than Tibet.
After the county units were chosen, the National Bureau of Statistics helped us to sample villages and communities within county units using recently updated village-level population data. Our sample used administrative villages (cun) in rural areas and neighborhoods (shequ), which comprise one or more formal resident committees (juweihui), in urban areas as primary sampling units (PSUs). We selected three PSUs within each county-level unit, using probability proportional to size (PPS) sampling, for a total of 450 PSUs.
In each PSU, we constructed our own sampling frame using Google Earth base maps, and a computer-assisted personal interview program was then used to sample households and to conduct the interviews using laptops.4 We interviewed all age-eligible sample households who were willing to participate in the survey, ultimately interviewing 10,257 households containing 17,587 respondents aged 45 years and over and their spouses. In this paper, we exclude the spouses who are younger than 45 years old and have 17,343 observations for the analysis.5
China Health and Retirement Longitudinal Study baseline data include detailed information of respondents and their living spouses. The main questionnaire includes information on basic demographics, family, health status, health care and health insurance, employment, and household economy (income, consumption, and wealth). Module E ‘Health Care and Health Insurance’ provides the most important information for this study. Respondents are asked what types of health insurance they have and if they do the specifics of each insurance type including premium, copayment, and benefit. They are also asked about their healthcare service usage, including outpatient service in the past month and inpatient service in the past year. For those who used any service, more details are followed including cost of care and who paid the care.
We examine four sets of outcomes: health insurance, healthcare cost, healthcare utilization, and hospital types. For each outcome, we first give a general view by providing descriptive statistics and then investigate more deeply with regression results. Linear probability models are employed for all the regressions but one, the estimation on hospital types, in which multinomial logistic regression is used.6 In all the regressions, the dependent variables are aforementioned outcomes, while the key explanatory variables of interest are the SES variables. The two major SES variables considered are the education categories and the log of per capita expenditure (log PCE).7 Education is a commonly used measure of SES, while PCE is less so. We use PCE as it is a better measure of long-run resources than is current income, particularly so in low-income rural settings, where incomes can vary so much year to year because of variation in weather, pests, plant diseases, and so on. PCE includes the value of food production, which is self-consumed, which ought to be included in income, but may not be in all measures of income. PCE also tends to be measured with less error than income (Deaton, 1997; Lee, 2009). We take the log form to capture the nonlinear property of the association and because in logs, PCE is closer to Gaussian. In each regression, basic demographic variables like age, gender, and marital status are also included.
4. EMPIRICAL RESULTS
4.1. Health insurance
Thanks to the establishment of the NCMS (2003) and the URMI (2007), the Chinese government successfully expanded its social health insurance system to nearly all people. As shown in Table I, overall, 92.8% of our study sample have some insurance. NCMS contributes the most to China’s universal coverage, covering more than 66% of the Chinese mid-aged and older people. Among the population with urban hukou, the two important insurance schemes are the UEMI, targeting urban employees, and the URMI for non-employees, covering 15.6% and 5.8% of our overall sample or 50.7% and 17.6% of those with urban hukou. The government medical insurance (GMI) also covers a nontrivial share (8.5%) of people with urban hukou. The GMI provides health insurance for government officials and requires no insurance premiums and has no restrictions on deductible levels and payment ceilings. It has a copayment rate of 10%, which is lower than all other social health insurance schemes. The preferential treatment for government officials has been criticized by the public for a long time. It is expected that the Chinese government will combine the GMI and the UEMI, and such a reform for old-age insurance is already ongoing.
Table I.
Mean coverage of different types of health insurance schemes
| Total | Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Urban hukou | Rural hukou | Total | Urban hukou | Rural hukou | Total | Urban hukou | Rural hukou | |
| New Rural Cooperative Medical Scheme | 66.4 (0.61) | 9.0 (0.55) | 90.0 (0.41) | 64.9 (0.89) | 8.5 (0.67) | 89.8 (0.50) | 67.9 (0.85) | 9.5 (0.87) | 90.3 (0.63) |
| Urban Employee Medical Insurance | 15.6 (0.54) | 50.7 (1.33) | 1.3 (0.29) | 17.9 (0.81) | 54.9 (1.86) | 1.6 (0.25) | 13.5 (0.73) | 46.3 (1.87) | 0.9 (0.51) |
| Urban Resident Medical Insurance | 5.8 (0.33) | 17.6 (1.02) | 1.0 (0.12) | 5.3 (0.52) | 14.8 (1.56) | 1.1 (0.16) | 6.3 (0.41) | 20.4 (1.35) | 0.8 (0.18) |
| Urban and rural resident medical insurance | 1.4 (0.11) | 2.1 (0.28) | 1.1 (0.10) | 1.3 (0.14) | 1.8 (0.31) | 1.1 (0.15) | 1.5 (0.18) | 2.4 (0.47) | 1.0 (0.15) |
| Government medical insurance (gong fei) | 2.6 (0.25) | 8.5 (0.82) | 0.2 (0.04) | 3.3 (0.23) | 9.9 (0.76) | 0.4 (0.09) | 2.0 (0.43) | 7.1 (1.49) | 0.0 (0.01) |
| Medical aid | 0.1 (0.04) | 0.3 (0.11) | 0.0 (0.02) | 0.1 (0.05) | 0.3 (0.14) | 0.1 (0.03) | 0.1 (0.05) | 0.3 (0.17) | 0.0 (0.02) |
| Private medical insurance | 3.0 (0.27) | 5.9 (0.75) | 1.8 (0.21) | 3.3 (0.48) | 5.8 (1.24) | 2.2 (0.40) | 2.7 (0.26) | 6.1 (0.83) | 1.4 (0.15) |
| Other insurance | 0.7 (0.07) | 1.1 (0.20) | 0.5 (0.06) | 0.7 (0.10) | 1.1 (0.27) | 0.5 (0.08) | 0.7 (0.10) | 1.2 (0.28) | 0.6 (0.09) |
| Without insurance | 7.2 (0.32) | 9.6 (0.70) | 6.1 (0.35) | 6.6 (0.41) | 8.6 (1.06) | 5.8 (0.36) | 7.7 (0.49) | 10.6 (0.93) | 6.5 (0.58) |
Estimates are weighted using individual sampling weights with household and individual response adjusted. Standard errors are in parentheses.
Although the health insurance is nearly universal among all the population examined, there are still differences. While the NCMS is designed to cover rural people, there is still 9% of our urban sample who have NCMS. On the contrary, 90% of our study sample with rural hukou are covered by the NCMS, while only less than 4% are covered by other health insurance schemes. One striking fact is that the insurance rate for rural people is even higher than that for urban people, either by hukou status or residency. Looking only at the insurance rate, it looks as if rural people are better insured, but as it will be shown later, the health insurance coverage for rural people is quite shallow. There are no large gender differences in insurance coverage. If anything, the proportion of men covered by the UEMI is a little higher than that of women, which may reflect that men are more likely to work in formal sectors than women.
Table II reports regression results of access to health insurance by hukou status. Each column shows results from one linear probability model. We control for community (PSU) fixed effects to focus on SES gradients at the individual level. The dependent variables are binary measures of either having any health insurance or having a specific type of health insurance.8 For urban people, we categorize health insurance into four groups: the UEMI, URMI, NCMS, and other types of health insurance; for rural people, we separate health insurance into two groups: NCMS and others.
Table II.
Regressions for having health insurance by schemes
| Urban hukou | Rural hukou | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| UEMI | URMI | NCMS | Any others |
Any insurance |
NCMS | Any others |
Any insurance |
|||
| Log(PCE) | 0.063*** (0.012) |
−0.035*** (0.012) |
−0.025*** (0.006) |
0.015 (0.011) |
0.024** (0.011) |
0.005 (0.004) |
0.006 (0.004) |
0.012** (0.005) |
||
| Can read and write | 0.065* (0.036) |
−0.028 (0.030) |
−0.040* (0.024) |
0.028 (0.022) |
0.040 (0.031) |
0.007 (0.008) |
−0.003 (0.005) |
0.004 (0.007) |
||
| Elementary school | 0.092*** (0.024) |
−0.030 (0.027) |
−0.031 (0.021) |
0.051* (0.030) |
0.082** (0.041) |
0.020** (0.009) |
−0.004 (0.005) |
0.015* (0.009) |
||
| Middle school and above | 0.193*** (0.028) |
−0.099** (0.039) |
−0.098*** (0.025) |
0.091** (0.039) |
0.099** (0.042) |
0.008 (0.008) |
0.012 (0.009) |
0.020* (0.010) |
||
| Age 55–64 | 0.036 (0.022) |
−0.018 (0.017) |
−0.034** (0.014) |
0.039*** (0.013) |
0.029* (0.016) |
0.012 (0.007) |
0.004 (0.003) |
0.016** (0.008) |
||
| Age 65–74 | 0.055** (0.026) |
−0.058** (0.026) |
−0.057** (0.023) |
0.122*** (0.038) |
0.062** (0.027) |
0.003 (0.009) |
0.008* (0.005) |
0.012 (0.008) |
||
| Age 75+ | 0.006 (0.040) |
−0.065* (0.034) |
−0.093*** (0.024) |
0.185*** (0.048) |
0.039 (0.027) |
−0.026* (0.013) |
0.024* (0.013) |
−0.001 (0.011) |
||
| Male | 0.076*** (0.017) |
−0.053*** (0.015) |
−0.006 (0.019) |
0.025** (0.012) |
0.005 (0.010) |
−0.016*** (0.005) |
0.010 (0.006) |
−0.006 (0.004) |
||
| Never married/divorced/separated | −0.022 (0.038) |
0.010 (0.028) |
0.002 (0.031) |
−0.012 (0.029) |
−0.037 (0.031) |
−0.027** (0.014) |
0.002 (0.006) |
−0.025* (0.014) |
||
| Widowed | −0.034 (0.023) |
0.047** (0.022) |
−0.010 (0.016) |
−0.028 (0.019) |
−0.036 (0.022) |
−0.038*** (0.012) |
−0.008 (0.005) |
−0.046*** (0.016) |
||
| Constant | −0.310*** (0.114) |
0.609*** (0.141) |
0.468*** (0.073) |
−0.134 (0.130) |
0.574*** (0.130) |
0.874*** (0.038) |
−0.033 (0.042) |
0.840*** (0.049) |
||
| Observations | 3839 | 3839 | 3839 | 3839 | 3839 | 13,306 | 13,306 | 13,306 | ||
| R2 | 0.316 | 0.201 | 0.384 | 0.202 | 0.177 | 0.135 | 0.175 | 0.110 | ||
| p-value of F-test for all age dummies | 0.087 | 0.166 | 0.000 | 0.002 | 0.117 | 0.048 | 0.240 | 0.230 | ||
| p-value of F-test for all education dummies | 0.000 | 0.049 | 0.000 | 0.102 | 0.061 | 0.184 | 0.541 | 0.222 | ||
| p-value of F-test for community fixed effects | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||
Robust standard errors (clustered at the community level) are in parentheses. Reference group for education is illiterate; reference for marriage status is married and living with spouse. Missing values of log(PCE) are imputed by sample mean of log(PCE), and a dummy variable indicating whether log(PCE) is missing is included as control. All regressions control for community fixed effects. Linear probability model, dependent variable: whether having health insurance (=1, Yes; = 0, No).
p < 0.01,
p < 0.05,
p < 0.1.
In general, the associations between insurance holding and SES variables are stronger among urban than rural people, reflecting the fact that the major health insurance in the rural areas is heavily subsidized by the government and thus more equally distributed among the rich and the poor. The only SES gradient among rural people is on marital status, with married people more likely to have access to the NCMS. Within urban hukou holders, people with higher log PCE and higher levels of education are more likely to have any insurance. However, the associations of log PCE and schooling are quite different across the different insurance types. For the UEMI plan, the associations are strongly positive. This is reasonable as employees are more likely to have higher education and income. And people with higher SES are more likely to work with employers who are more likely to abide by the labor law. For the URMI and NCMS, it is the reverse; that is, higher log PCE or education is associated with a lower probability of having these types of insurance. This reflects the fact that URMI and NCMS are targeted at the more disadvantaged groups, in the case of URMI at urban residents who do not have insurance from an employer.
4.2. Healthcare cost
Insurance status determines the actual financial burden that people have for health care. In the previous sections, we generally find health insurance rate is higher and more equally distributed in rural areas than in urban areas. However, insurance is only useful when it actually benefits the insured and relieves their healthcare burden. In this part, therefore, we examine what fraction of healthcare cost is paid by the insurance, what faction is out of pocket of the individuals themselves, and what the differences are of these fractions across different populations.
Table III describes the total medical cost, OOP cost, and the corresponding reimbursement rate for people with different types of health insurance. To capture distributional differences, we show the median amount and the amounts at the 25 and 75 percentiles. In general, people with insurance have higher medical care costs. This is partly because those people with insurance are able to afford more medical care use and partly because those people with higher incentive to use medical care are more likely to join an insurance plan. We also see people with urban insurance schemes have higher total medical care cost. To further understand whether this is due to the difference in respondents’ resources or in the generosity of the plans, it is necessary to examine OOP costs and the reimbursement rate. Most insurance plans only cover inpatient care cost or set a high deductible level for outpatient care cost, partly because the amount of outpatient care cost is much lower than that of inpatient care. We see that the median amount of the reimbursement for outpatient care cost is zero; only some generous urban plans cover some outpatient care cost. In particular, the NCMS does not cover outpatient care cost at all, while the UEMI and the URMI only cover some outpatient care cost for less than half the visits. We thus focus on the inpatient care cost.
Table III.
Cost of health care and reimbursement rate for insured people: by schemes
| Total | Out of pocket | Reimbursement rate | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Median | 25% | 75% | N | Median | 25% | 75% | N | Median | 25% | 75% | |
| A: Outpatient cost of last visit | ||||||||||||
| Urban Employee Medical Insurance | 305 | 300 | 100 | 600 | 304 | 170 | 30 | 500 | 302 | 0.00 | 0.00 | 0.77 |
| Urban residents medical insurance | 120 | 200 | 100 | 600 | 119 | 200 | 11 | 500 | 119 | 0.00 | 0.00 | 0.63 |
| NCMS | 2374 | 100 | 33 | 300 | 2369 | 100 | 28 | 300 | 2367 | 0.00 | 0.00 | 0.00 |
| UEMI|URMI|NCMS | 2799 | 139 | 45 | 400 | 2792 | 100 | 30 | 300 | 2788 | 0.00 | 0.00 | 0.00 |
| Without insurance | 146 | 100 | 40 | 300 | ||||||||
| B: Inpatient cost of last visit | ||||||||||||
| Urban Employee Medical Insurance | 226 | 7800 | 4000 | 11,000 | 223 | 2000 | 1100 | 4000 | 220 | 0.66 | 0.50 | 0.77 |
| Urban residents medical insurance | 76 | 4000 | 2000 | 10,000 | 74 | 2000 | 1000 | 4000 | 74 | 0.33 | 0.00 | 0.63 |
| NCMS | 1064 | 3000 | 1400 | 7500 | 1040 | 2000 | 750 | 5000 | 1027 | 0.25 | 0.00 | 0.50 |
| UEMI|URMI|NCMS | 1366 | 4000 | 2000 | 9000 | 1337 | 2000 | 900 | 5000 | 1321 | 0.33 | 0.00 | 0.64 |
| Without insurance | 55 | 3000 | 1700 | 6000 | ||||||||
Weighted using individual sampling weights with household and individual response adjusted. 2, 1, 1, 2 outliers for total outpatient cost, self-paid outpatient cost, total inpatient cost, and self-paid inpatient cost are deleted, respectively. Respondents without health insurance are also excluded.
NCMS, New Rural Cooperative Medical Scheme; UEMI, Urban Employee Medical Insurance; URMI, Urban Resident Medical Insurance.
Across insurance plans, the difference in OOP cost is smaller than that of total medical cost; as a result, the urban insurance plans (UEMI and URMI) have higher reimbursement rates than that of the rural plan (NCMS). For instance, the reimbursement rate at the 25 percentile of UEMI is 50%, while those of the URMI and the NCMS are both zero. The variation across UEMI, URMI, and NCMS is quite clear at the median amount, as their reimbursement rates are 66%, 33%, and 25%, respectively. In addition, it seems the difference in reimbursement rates across different percentiles is smaller for UEMI than that of URMI and NCMS, indicating that not only the urban employee insurance plan covers more of the cost; the coverage is more equally distributed. In other words, the degree of benefits of the insurance plans for the disadvantaged non-employee urban residents and rural residents varies more, which means the two plans may be less reliable in dealing with healthcare shocks.
In Table IV, we estimate the correlates of total medical cost and the share of cost reimbursed for the last outpatient visit (in the last 1 month) and the last inpatient visit (in the last 1 year), respectively, with special attention paid to health insurance schemes. As shown in columns 1 and 3, the insurance type dummies and their interactions with log PCE are not jointly significantly associated with total cost for either inpatient or outpatient service. This can be interpreted as evidence of no moral hazard. However, log PCE and its interactions with health insurance scheme dummies are jointly significant for regressions on total cost, although the interactions with insurance schemes are not significant. This suggests that higher income respondents do spend more on health care, although this impact does not differ by insurance scheme.
Table IV.
Regression for total medical cost of the last visit and share of cost reimbursed
| Outpatient visit | Inpatient visit | |||
|---|---|---|---|---|
| Log of total cost | Share reimbursed | Log of total cost | Share reimbursed | |
| UEMI | 0.193 (0.240) | 0.186*** (0.041) | 0.237 (0.281) | 0.445*** (0.076) |
| URMI | 0.268 (0.242) | 0.060 (0.039) | 0.180 (0.300) | 0.344*** (0.075) |
| NCMS | 0.046 (0.140) | 0.075*** (0.017) | 0.143 (0.197) | 0.296*** (0.049) |
| Other health insurance | 0.309 (0.247) | 0.132*** (0.045) | 0.350 (0.300) | 0.479*** (0.090) |
| Multiple health insurance | 0.029 (0.228) | 0.057 (0.041) | −0.205 (0.307) | 0.082 (0.077) |
| Log(PCE) | 0.121 (0.144) | 0.014 (0.018) | 0.144 (0.195) | 0.101 (0.072) |
| UEMI * demeaned Log(PCE) | 0.131 (0.232) | 0.030 (0.043) | 0.291 (0.237) | −0.082 (0.084) |
| URMI * demeaned Log(PCE) | 0.291 (0.248) | 0.017 (0.042) | 0.124 (0.265) | −0.176* (0.095) |
| NCMS * demeaned Log(PCE) | 0.075 (0.149) | −0.016 (0.019) | 0.178 (0.207) | −0.103 (0.074) |
| Other HI * demeaned Log(PCE) | 0.041 (0.245) | 0.056 (0.050) | 0.149 (0.273) | −0.137 (0.095) |
| Multiple HI * demeaned Log(PCE) | 0.125 (0.228) | 0.017 (0.046) | 0.143 (0.377) | −0.057 (0.090) |
| Can read and write | −0.049 (0.097) | 0.001 (0.013) | 0.093 (0.129) | −0.014 (0.033) |
| Elementary school | 0.098 (0.110) | −0.001 (0.016) | 0.061 (0.124) | 0.001 (0.034) |
| Middle school and above | 0.060 (0.106) | 0.014 (0.017) | −0.030 (0.128) | −0.016 (0.034) |
| Age 55–64 | 0.001 (0.085) | 0.015 (0.013) | 0.032 (0.116) | 0.029 (0.030) |
| Age 65–74 | 0.041 (0.103) | 0.039** (0.016) | −0.057 (0.127) | 0.051 (0.034) |
| Age 75+ | 0.152 (0.151) | 0.057** (0.025) | −0.190 (0.165) | 0.047 (0.042) |
| Male | 0.071 (0.069) | 0.005 (0.011) | 0.151* (0.086) | −0.004 (0.024) |
| Never married/divorced/separated | −0.285* (0.151) | −0.005 (0.022) | −0.456** (0.205) | −0.003 (0.053) |
| Widowed | 0.210** (0.095) | −0.012 (0.017) | −0.231* (0.134) | −0.020 (0.037) |
| Self-reported poor health | 0.431*** (0.066) | 0.008 (0.011) | 0.131 (0.085) | −0.018 (0.022) |
| Any major chronic conditions | 0.272*** (0.089) | −0.003 (0.013) | 0.175* (0.093) | 0.017 (0.024) |
| Any minor chronic conditions | −0.039 (0.090) | 0.008 (0.014) | −0.133 (0.121) | 0.022 (0.029) |
| Any ADL/IADL | 0.170** (0.081) | 0.006 (0.012) | 0.115 (0.082) | 0.001 (0.024) |
| Constant | 3.410*** (1.252) | −0.128 (0.153) | 6.562*** (1.660) | −0.896 (0.619) |
| Observations | 3049 | 3049 | 1493 | 1449 |
| R2 | 0.335 | 0.355 | 0.464 | 0.445 |
| p-value of F-test for all age dummies | 0.707 | 0.042 | 0.412 | 0.483 |
| p-value of F-test for all education dummies | 0.485 | 0.817 | 0.744 | 0.935 |
| p-value of F-test for insurance schemes and interaction terms | 0.846 | 0.000 | 0.860 | 0.000 |
| p-value of F-test for PCE and its interaction terms | 0.002 | 0.659 | 0.000 | 0.586 |
| p-value of F-test for interaction terms between PCE and insurance schemes | 0.818 | 0.578 | 0.822 | 0.458 |
| p-value of F-test for all health variables | 0.000 | 0.834 | 0.010 | 0.837 |
Robust standard errors (clustered at the community level) are in parentheses. 2 outliers for total outpatient cost are deleted; 1 outliers for total inpatient cost are deleted. Reference group of health insurance dummies are people having no health insurance. All regressions control community fixed effects. As the health status variables are possibly endogenous, we also run regressions without them but obtain similar results.
NCMS, New Rural Cooperative Medical Scheme; UEMI, Urban Employee Medical Insurance; URMI, Urban Resident Medical Insurance; HI, health insurance.
p < 0.01,
p < 0.05,
p < 0.1.
Reimbursement, however, varies widely across health insurance schemes. Patients having UEMI have an 18.6% higher total outpatient cost reimbursed compared with respondents with no health insurance, and 44.5% higher for the last inpatient visit at the sample mean level of log PCE. Patients having URMI and NCMS have smaller fractions of total cost reimbursed compared with UEMI covered respondents, particularly for outpatient visits. Log PCE and education are not significantly related to the share reimbursed, conditional on the type of insurance. This implies an absence of socioeconomic inequality within schemes.
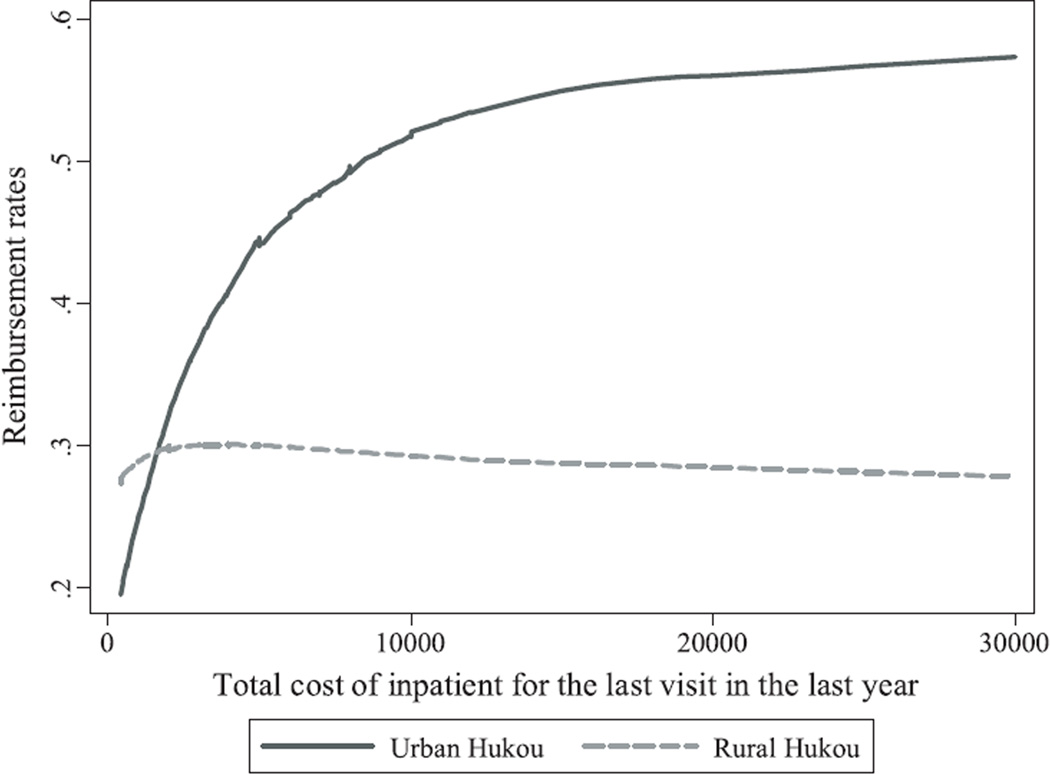
It is important to see whether the reimbursement rate increases with total cost because affordability is a bigger problem at high levels of medical cost. Figure 1 shows nonparametric bivariate relationships between total medical cost of the last inpatient visit and reimbursement rates.9 The reimbursement rate increases with total medical cost among urban people but flattens out at just less than 60%. Reimbursement rates for inpatient care are flat at about 30% for rural people. This result implies that for people with higher medical cost, the actual burden falling on them will be large and that more insurance coverage on catastrophic medical expense is necessary.
Figure 1.
Reimbursement rates for inpatients with any insurance for the last visit in the last year, by total cost
Notes: Bandwidth=0.8. Sample restricted to these having positive inpatient cost. 10% extreme observations (5% at each end) based on values of total cost are excluded in plotting the figure. We run the lowess using whole sample.
Table V presents the correlates of share of reimbursement across counties. For last outpatient visit, the share of reimbursement is significantly higher in wealthy and more urbanized counties. Specifically, a RMB10,000 increase of gross domestic product per capita is associated with about two percentage points higher of the share of reimbursement, while a one percentage point increase of the urbanization rate is associated with about a 17 percentage point higher of the share of reimbursement. For the last inpatient visit, the share of reimbursement is higher in counties having a higher urbanization rate. Meanwhile, Table V shows no differences in share of reimbursement across regions. Therefore, the results in this table show that the disparity of health insurance generosity at the macro-level is mainly between urban and rural rather than across regions.
Table V.
Regression for the share of reimbursement at the county level
| Last outpatient visit | Last inpatient visit | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| GDP per capita | 0.017** (0.007) | 0.017** (0.007) | −0.002 (0.007) | 0.000 (0.007) |
| Urban | 0.168*** (0.047) | 0.170*** (0.047) | 0.240*** (0.044) | 0.243*** (0.043) |
| Middle region | −0.001 (0.020) | 0.018 (0.030) | ||
| Eastern region | −0.006 (0.022) | −0.011 (0.032) | ||
| Constant | 0.056*** (0.019) | 0.057** (0.022) | 0.268*** (0.023) | 0.262*** (0.030) |
| Observations | 149 | 149 | 150 | 150 |
| R2 | 0.233 | 0.234 | 0.168 | 0.173 |
Reimbursement data are from China Health and Retirement Longitudinal Study household survey. Data for explanatory variables are from County Statistic Yearbook 2009. Gross domestic product (GDP) per capita is measured in RMB10,000.
Robust standard errors are in parentheses.
p < 0.01,
p < 0.05,
p < 0.1.
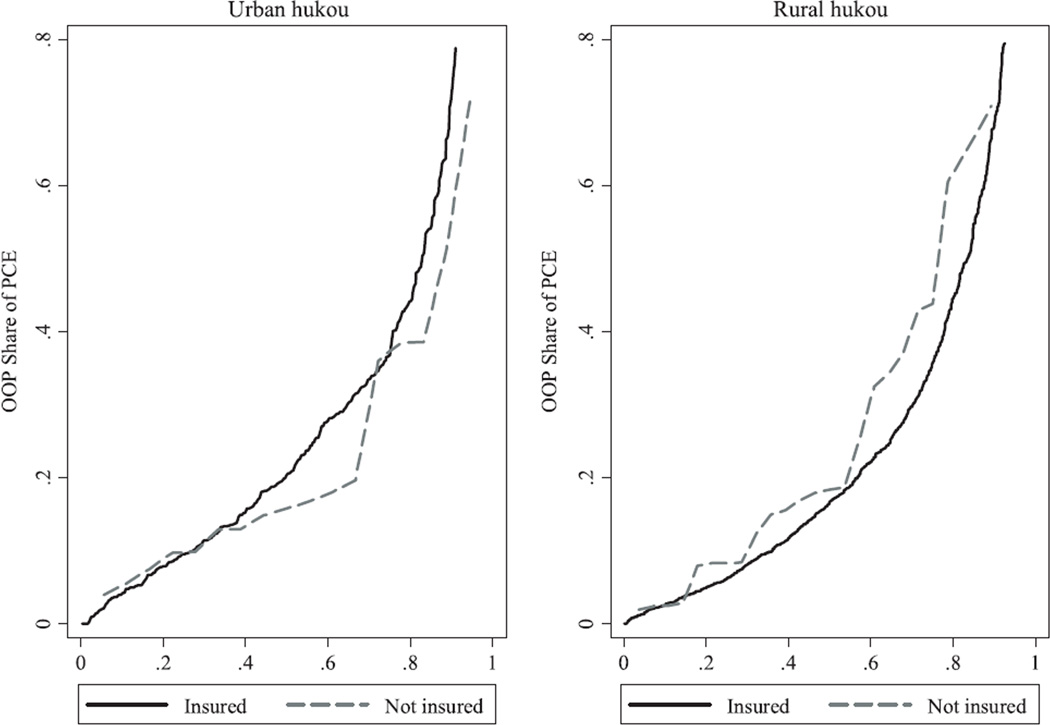
In Figure 2, we directly examine the economic burdens of inpatient health services by looking at the share of OOP expenditures relative to household PCEs. As the amount for outpatient is relatively small, we focus only on the inpatient care payment. We plot the cumulative distributions for respondents with and without insurance, respectively (although we invert the axes compared with how they are normally plotted). We see OOP expenditures of about half the respondents comprise about 20% of PCE. About 20% of the respondents have OOP expenditures greater than 40% of their PCE, an obviously heavy burden to them. The difference between those with and without insurance is not large but presents an opposite pattern for urban and rural people. For the urban people, those without insurance paid a slightly smaller share out of their pocket than the insured, while for rural people, the uninsured paid slightly more.
Figure 2.
Cumulative percentage of share of out-of-pocket (OOP) expenditure of per capita expenditure (PCE): inpatient service
Notes: Weighted using individual sampling weights with household and individual response adjusted. Observations with share of OOP expenditure of PCE larger then 1 are trimmed.
4.3. Healthcare utilization
In this section, we examine how healthcare utilization varies among different populations. Table VI gives a full picture of healthcare utilization. About 20% of the Chinese people older than 45 years report using outpatient service during the last month. There are no apparent differences in outpatient service usage by hukou status, but the difference by gender is quite clear. About 22% of women report using outpatient service during the last month, while only 17% of men do. Taking a look at healthcare utilization by health insurance status, we see insurance holding is related to higher likelihood of using outpatient service, but no large differences exist across health insurance schemes among those insured. Once we separate men and women, however, the variation in outpatient service utilization across health insurance schemes is large. Men having URMI have the largest likelihood of using outpatient services during the last month, while women having UEMI have the largest likelihood. Also, the variation across health insurance schemes is larger for women than that for men.
Table VI.
Mean healthcare utilization: by gender, hukou, and insurance scheme
| Total | Men | Women | ||||
|---|---|---|---|---|---|---|
| % | N | % | N | % | N | |
| A: Outpatient service during the last month | ||||||
| By hukou | ||||||
| Urban | 18.8 | 3836 | 15.8 | 1998 | 22.0 | 1837 |
| Rural | 19.9 | 13,222 | 17.5 | 6298 | 22.0 | 6921 |
| Total | 19.6 | 17,072 | 17.0 | 8300 | 22.1 | 8767 |
| By HI schemes | ||||||
| UEMI | 21.4 | 1893 | 16.3 | 1079 | 27.7 | 813 |
| URMI | 20.0 | 769 | 20.2 | 327 | 19.9 | 442 |
| NCMS | 20.0 | 12,541 | 17.6 | 5960 | 22.2 | 6570 |
| Other HI | 17.7 | 789 | 15.6 | 445 | 20.0 | 344 |
| No insurance | 15.2 | 1137 | 11.4 | 521 | 18.2 | 615 |
| B: Inpatient service during the last year | ||||||
| By hukou | ||||||
| Urban | 10.7 | 3839 | 11.7 | 2000 | 9.7 | 1838 |
| Rural | 8.5 | 13,304 | 8.7 | 6347 | 8.4 | 6954 |
| Total | 9.1 | 17,158 | 9.6 | 8351 | 8.7 | 8802 |
| By HI schemes | ||||||
| UEMI | 11.6 | 1893 | 12.4 | 1080 | 10.6 | 812 |
| URMI | 9.9 | 770 | 9.7 | 326 | 10.0 | 444 |
| NCMS | 8.7 | 12,614 | 8.9 | 6004 | 8.5 | 6599 |
| Other HI | 11.0 | 795 | 12.4 | 448 | 9.5 | 347 |
| No insurance | 5.3 | 1144 | 5.5 | 525 | 5.3 | 618 |
Calculations are weighted using individual sampling weights with household and individual response adjusted.
NCMS, New Rural Cooperative Medical Scheme; UEMI, Urban Employee Medical Insurance; URMI, Urban Resident Medical Insurance; HI, Health Insurance.
Approximately 9% of Chinese people older than 45 years report using inpatient services during the last year. This means that there are at least 40.4 million mid-aged and older Chinese people hospitalized each year,10 while, in 2011, the total number of hospital beds in China is about 3.7 million.11 The difference in inpatient service usage by hukou status is larger than that in outpatient service, suggesting people with urban hukou have higher likelihood of usage. Different from outpatient service, the gender gap in inpatient service usage is quite small. The difference in inpatient service utilization across health insurance status is more striking than that in outpatient service, especially for men. People without any health insurance are less likely to use inpatient service than those with any insurance. People with UEMI are more likely to use inpatient service than those with URMI or NCMS. Overall, Table VI suggests that disparities exist in healthcare utilization between people with and without health insurance, and also between people with different types of health insurance. The gradient across health insurance schemes is also consistent with the generosity of these schemes: UEMI has the highest copayment rate, followed by the URMI and then the NCMS.
Table VII reports results for regressions on healthcare utilization. Access to health insurance is significantly related to healthcare utilization, but only for inpatient service. A joint significant test of PCE and its interactions with health insurance schemes suggests it is generally positively associated with the usage of both outpatient and inpatient services. The relationship between usage of health service and education is nonlinear, with higher usage among respondents with some schooling, but less than primary school. There is a strong positive age gradient for usage of inpatient services, suggesting the deterioration of health status with age. Respondents not living with a spouse and those who are unmarried, divorced, separated, or widowed are less likely to use health services, but the relationship is only statistically significant for inpatient service.
Table VII.
Regression for healthcare usage
| Dependent variable | ||
|---|---|---|
| Having outpatient visit | Having inpatient visit | |
| UEMI | 0.021 (0.017) | 0.039*** (0.014) |
| URMI | 0.013 (0.020) | 0.022* (0.013) |
| NCMS | 0.017 (0.013) | 0.032*** (0.009) |
| Other health insurance | −0.006 (0.020) | 0.036** (0.015) |
| Multiple health insurance | 0.023 (0.019) | 0.003 (0.017) |
| Log(PCE) | 0.024** (0.011) | 0.012 (0.008) |
| UEMI * demeaned Log(PCE) | −0.005 (0.016) | 0.021 (0.013) |
| URMI * demeaned Log(PCE) | 0.013 (0.019) | 0.014 (0.014) |
| NCMS * demeaned Log(PCE) | −0.012 (0.012) | 0.023*** (0.009) |
| Other HI * demeaned Log(PCE) | 0.019 (0.018) | 0.006 (0.013) |
| Multiple HI * demeaned Log(PCE) | −0.013 (0.021) | −0.016 (0.014) |
| Can read and write | 0.024** (0.010) | 0.014* (0.008) |
| Elementary school | 0.021** (0.010) | −0.001 (0.007) |
| Middle school and above | 0.014 (0.010) | 0.002 (0.008) |
| Age 55–64 | −0.003 (0.007) | 0.013** (0.005) |
| Age 65–74 | −0.001 (0.010) | 0.036*** (0.008) |
| Age 75+ | −0.005 (0.014) | 0.059*** (0.012) |
| Male | −0.036*** (0.006) | 0.013*** (0.005) |
| Never married/divorced/separated | −0.015 (0.012) | −0.025*** (0.008) |
| Widowed | −0.001 (0.011) | −0.026*** (0.008) |
| Self-reported poor health | 0.145*** (0.009) | 0.079*** (0.008) |
| Any major chronic conditions | 0.047*** (0.010) | 0.080*** (0.009) |
| Any minor chronic conditions | 0.079*** (0.007) | 0.020*** (0.005) |
| Any ADL/IADL | 0.027*** (0.009) | 0.044*** (0.007) |
| Constant | −0.132 (0.094) | −0.128* (0.068) |
| Observations | 17,014 | 17,100 |
| R2 | 0.130 | 0.106 |
| p-value of F-test for all age dummies | 0.969 | 0.000 |
| p-value of F-test for all education dummies | 0.081 | 0.194 |
| p-value of F-test for insurance schemes and interaction terms | 0.216 | 0.011 |
| p-value of F-test for PCE and its interaction terms | 0.000 | 0.000 |
| p-value of F-test for interaction terms between PCE and insurance schemes | 0.169 | 0.125 |
| p-value of F-test for all health variables | 0.000 | 0.000 |
Robust standard errors (clustered at the community level) are in parentheses. Reference group of health insurance dummies are people with no health insurance. All regressions control community fixed effects. As the health status variables are possibly endogenous, we also run regressions without them but obtain similar results.
NCMS, New Rural Cooperative Medical Scheme; UEMI, Urban Employee Medical Insurance; URMI, Urban Resident Medical Insurance; ADL, activities of daily living; IADL, Instrumental activities of daily living; HI, Health insurance.
p < 0.01,
p < 0.05,
p < 0.1.
4.4. Hospital types
In China, the quality of health care varies across different types of hospitals. In general, large general hospitals have higher quality, while those small township hospitals and community or village healthcare centers have the lowest quality. People prefer general hospitals even for minor sickness, which is not cost-effective. To reduce cost as well as the burden of the large hospitals, some insurance programs, for example, NCMS, require screening first in the lower-level hospitals and design a payment schedule that tends to encourage treatment at lower levels. In this section, we present the distribution of hospital types used among people with various insurance schemes.
Table VIII shows which type of medical facilities the respondents visited, separately for people with access to different types of health insurance. For outpatient services, about 30% of visits occur in general hospitals, about 32% in village clinics/private clinics. Taking a look across health insurance schemes, people with UEMI are more likely to visit general hospitals than those with URMI or NCMS. This may reflect the closer availability of general hospitals for people with urban hukou, the generosity of UEMI, and the greater resources of respondents who have UEMI. Among people with NCMS, about 40% of outpatient visits occur in a village clinic or in a private clinic. This is quite different from those with UEMI or URMI. In parallel, we may expect most outpatient visits for people having UEMI or URMI to occur in community healthcare centers, but in fact, only 16.3% of outpatient visits occur in a community healthcare center for people having UEMI, and 9.6% for people having URMI. Such a high fraction of visiting general hospitals among those with UEMI or URMI may not be necessarily socially optimal, if their illnesses are relatively minor, because usually social efficiency is higher if people start with facilities at lower levels and if necessary get referred up to higher-level facilities. This also explains why it is always crowded in hospitals in municipalities such as Beijing and Shanghai. Nevertheless, the significant differences in types of hospitals visited across health insurance schemes suggest an unequal distribution of public health resources.
Table VIII.
Means of hospital types visited
| Share visited (%) | |||||||
|---|---|---|---|---|---|---|---|
| Types of hospital | Total | UEMI | URMI | NCMS | Other HI | No HI | p-value |
| A: The last outpatient visit | |||||||
| General hospital | 30.2 | 53.7 | 46.0 | 22.6 | 40.7 | 38.0 | 0.000 |
| Specialized hospital | 3.1 | 3.1 | 2.2 | 3.1 | 4.9 | 2.6 | 0.000 |
| Chinese medicine hospital | 5.5 | 10.1 | 9.2 | 3.9 | 8.9 | 2.8 | 0.000 |
| Community healthcare center | 6.1 | 16.3 | 9.6 | 2.6 | 15.5 | 5.7 | 0.000 |
| Township hospital | 15.7 | 4.2 | 7.2 | 19.8 | 8.5 | 14.5 | 0.000 |
| Healthcare post | 4.7 | 0.8 | 0.8 | 6.2 | 2.2 | 2.4 | 0.000 |
| Village clinic/private clinic | 32.5 | 10.4 | 14.4 | 40.1 | 18.3 | 32.1 | 0.000 |
| Others | 1.1 | 0.9 | 0.0 | 1.3 | 1.2 | 0.9 | 0.000 |
| B: The last inpatient visit | |||||||
| General hospital | 62.7 | 80.3 | 91.7 | 55.6 | 62.8 | 54.6 | 0.000 |
| Specialized hospital | 6.4 | 5.6 | 1.0 | 6.8 | 10.1 | 6.2 | 0.000 |
| Chinese medicine hospital | 8.9 | 10.1 | 1.8 | 8.2 | 8.7 | 21.5 | 0.000 |
| Community healthcare center | 1.0 | 0.5 | 0.6 | 1.3 | 0.0 | 0.0 | 0.000 |
| Township hospital | 17.9 | 2.4 | 2.5 | 24.2 | 14.0 | 17.6 | 0.000 |
| Healthcare post | 1.9 | 0.0 | 1.8 | 2.5 | 2.5 | 0.0 | 0.000 |
| Others | 1.3 | 1.2 | 0.6 | 1.3 | 2.0 | 0.0 | 0.000 |
Estimates are weighted using individual sampling weights with household and individual response adjusted. p-values are from joint F-test of equality of values across different health insurance schemes (including having no insurance).
A higher proportion of inpatient visits occur in general hospitals, than for outpatient visits. This is reasonable as inpatient visits are mainly for more complicated illnesses. Again, people with urban insurance have higher fraction of going to general hospitals. Of people having UEMI and URMI, more than 80% and 91% inpatient visits occur in general hospitals, respectively, and the number for those with NCMS is only 56%. Of people without any health insurance, only 54.6% visit general hospitals for their last inpatient visit. The differences across health insurance schemes are statistically significant.
Table IX presents multinomial logit regression results on usage of hospital types. For people with urban hukou, differences exist in correlations between insurance type and hospital type for inpatient services. The relative risk ratios are smaller than 1, indicating that urban people with those insurance plans are less likely to choose type 2 and type 3 hospitals for inpatient care compared with type 4 hospitals. For rural people, the difference exists for outpatient care only. People with any insurance are more likely to use type 1 through type 3 hospitals rather than type 4. For outpatient services among urban people, compared with type 4 facilities, better-educated people are more likely to visit type 1 hospitals and less likely to visit type 3 hospitals; married people are more likely to use type 1 hospitals. For outpatient services among rural people, there are strong gradients of education and also of PCE. Respondents having higher levels of education and higher PCE are more likely to visit type 1 and type 2 hospitals. The results are similar for inpatient services.
Table IX.
Multinomial logistic regressions on hospitals visited
| Outpatient visit | ||||||
|---|---|---|---|---|---|---|
| Urban hukou | Rural hukou | |||||
| Variables | Type 1 | Type 2 | Type 3 | Type 1 | Type 2 | Type 3 |
| Log(PCE) | 1.188 (0.158) |
1.235 (0.249) |
1.234 (0.404) |
1.368*** (0.123) |
1.468*** (0.160) |
1.077 (0.083) |
| Can read and write | 0.931 (0.362) |
1.165 (0.752) |
0.421 (0.277) |
1.098 (0.154) |
1.073 (0.273) |
0.896 (0.135) |
| Elementary school | 1.261 (0.418) |
2.023 (1.083) |
0.564 (0.289) |
1.538*** (0.255) |
1.197 (0.298) |
1.280 (0.199) |
| Middle school and above | 1.875* (0.639) |
2.121 (1.109) |
0.421 (0.224) |
1.449** (0.248) |
1.683** (0.402) |
1.720*** (0.301) |
| Age 55–64 | 1.000 (0.263) |
1.177 (0.370) |
0.888 (0.396) |
0.757** (0.103) |
0.846 (0.168) |
0.952 (0.147) |
| Age 65–74 | 1.593 (0.477) |
1.899* (0.738) |
0.926 (0.476) |
0.562*** (0.093) |
0.512** (0.149) |
1.149 (0.188) |
| Age 75+ | 1.978* (0.787) |
2.802** (1.281) |
0.333 (0.242) |
0.716 (0.182) |
0.240** (0.145) |
0.876 (0.206) |
| Male | 0.908 (0.170) |
0.823 (0.203) |
1.516 (0.585) |
1.125 (0.129) |
1.077 (0.206) |
0.956 (0.105) |
| Never married/divorced/separated | 0.300** (0.145) |
0.804 (0.540) |
0.000*** (0.000) |
0.663** (0.136) |
0.441** (0.162) |
0.852 (0.159) |
| Widowed | 0.528** (0.142) |
0.227*** (0.108) |
0.250 (0.220) |
0.862 (0.167) |
1.087 (0.313) |
1.180 (0.172) |
| UEMI | 1.428 (0.544) |
2.022 (1.251) |
0.612 (0.409) |
3.050* (1.859) |
4.428* (3.658) |
3.196* (1.902) |
| URMI | 1.977 (0.848) |
2.287 (1.513) |
0.925 (0.607) |
3.870** (2.230) |
3.694 (4.572) |
2.694 (2.099) |
| NCMS | 1.477 (0.632) |
1.848 (1.270) |
2.249 (1.413) |
1.200 (0.332) |
2.372* (1.220) |
0.877 (0.223) |
| Other health insurance | 1.496 (0.596) |
1.806 (1.266) |
1.683 (1.293) |
2.213 (1.326) |
1.130 (1.376) |
1.177 (0.707) |
| Multiple health insurance | 2.492 (1.620) |
1.313 (0.737) |
5.237** (4.396) |
1.321 (0.452) |
0.743 (0.375) |
0.711 (0.299) |
| Constant | 0.137 (0.175) |
0.019** (0.037) |
0.061 (0.176) |
0.022*** (0.018) |
0.002*** (0.002) |
0.200** (0.148) |
| Observations | 652 | 652 | 652 | 2632 | 2632 | 2632 |
| Inpatient visit | ||||||
|---|---|---|---|---|---|---|
| Urban hukou | Rural hukou | |||||
| Variables | Type 1 | Type 2 | Type 3 | Type 1 | Type 2 | Type 3 |
| Log(PCE) | 1.804* (0.579) |
2.919*** (1.114) |
1.117 (0.494) |
1.825*** (0.264) |
2.129*** (0.370) |
1.316** (0.180) |
| Can read and write | 0.739 (0.636) |
1.022 (1.031) |
0.232 (0.336) |
0.930 (0.387) |
0.746 (0.346) |
0.990 (0.439) |
| Elementary school | 2.559 (2.546) |
1.025 (0.858) |
1.351 (1.733) |
1.564 (0.667) |
1.367 (0.652) |
1.502 (0.658) |
| Middle school and above | 2.473 (2.129) |
1.401 (1.299) |
2.015 (2.753) |
3.169** (1.727) |
3.113* (1.852) |
3.171** (1.819) |
| Age 55–64 | 0.231** (0.165) |
0.130** (0.109) |
0.250 (0.228) |
2.033** (0.727) |
2.236** (0.871) |
2.412** (0.916) |
| Age 65–74 | 1.898 (0.823) |
2.185 (1.074) |
2.502** (1.088) |
|||
| Age 75+ | 0.375 (0.400) |
0.352 (0.396) |
0.058* (0.086) |
1.475 (0.882) |
0.984 (0.680) |
2.011 (1.215) |
| Male | 0.533 (0.617) |
0.426 (0.519) |
0.238 (0.297) |
0.865 (0.253) |
0.849 (0.275) |
0.739 (0.220) |
| Never married/divorced/separated | 0.085** (0.105) |
0.122 (0.201) |
1.111 (1.842) |
0.287*** (0.138) |
0.452 (0.227) |
0.278** (0.138) |
| Widowed | 2.944 (4.479) |
2.648 (4.137) |
6.003 (9.001) |
0.446** (0.181) |
0.427* (0.201) |
0.635 (0.270) |
| UEMI | 0.547 (0.507) |
0.168* (0.167) |
0.162 (0.201) |
|||
| URMI | 0.222 (0.207) |
0.007*** (0.010) |
0.031** (0.047) |
|||
| NCMS | 0.840 (1.440) |
0.678 (1.236) |
1.676 (3.236) |
0.404 (0.293) |
0.476 (0.379) |
0.532 (0.395) |
| Other health insurance | 0.357 (0.294) |
0.106** (0.103) |
0.081* (0.117) |
|||
| Multiple health insurance | 0.042* (0.069) |
0.271 (0.450) |
0.000*** (0.000) |
|||
| Constant | 0.555 (1.852) |
0.008 (0.030) |
12.410 (55.943) |
0.083* (0.110) |
0.005*** (0.009) |
0.487 (0.618) |
| Observations | 350 | 350 | 350 | 968 | 968 | 968 |
Reported are relative risk ratios. Robust standard errors (clustered at the community level) are in parentheses. Samples are restricted to those visited hospitals for outpatient or inpatient service, respectively. For outpatient visit, there are four categories of hospitals: Type 1 includes ‘general hospital’. Type 2 includes ‘specialized hospital’ and ‘Chinese medicine hospital’. Type 3 includes ‘township hospital’. Type 4 includes ‘community healthcare center’, ‘healthcare post’, ‘village clinic/private clinic’, and ‘others’. Type 4 is the base outcome. For inpatient visit, there are also four categories of hospitals with the first three types the same as those for outpatient and type 4 including ‘community healthcare center’, ‘health care post’, and ‘others’. Again, type 4 is the base outcome. ‘Age 65–74’ is dropped because of multicolinearity problems, the same for health insurance dummies in the last three columns.
NCMS, New Rural Cooperative Medical Scheme; UEMI, Urban Employee Medical Insurance; URMI, Urban Resident Medical Insurance.
p < 0.01,
p < 0.05,
p < 0.1.
5. DISCUSSION AND CONCLUSIONS
For the past two decades, China has conducted a series of ambitious health reforms, and the insurance coverage has quickly reached near universality, both in urban and rural areas. However, with this rapid expansion, questions remain regarding whether insurance benefit is also universal across population sub-types.
In this paper, using a nationally representative survey dataset collected during 2011–2012, we document the key parameters of various health insurance programs in China and the profile of health service utilization among mid-aged and older Chinese.
We show that overall health insurance coverage of the mid-aged and older Chinese is about 93%, with more than 95% of the insured covered by one of the three main insurance schemes: NCMS, UEMI, and URMI. That is, the insurance in China is almost universal among the mid-aged and older Chinese just like that in other countries and regions pursuing universal health insurance (e.g., the UK and Taiwan).
The generosity of health insurance and the burden of healthcare are far from being universal across the country. The healthcare burden falls largely on rural people and those with lower SES. Respondents with lower income as measured by PCE have a lower chance of being insured, as do the less-educated, older, and divorced/widowed women, and rural-registered people living in urban areas.
Our study improves on existing studies by examining correlates and impacts of different health insurance schemes in a unified framework, allowing us to make comparisons across schemes. Different health insurance programs target different groups with the differences being quite large, and we see that these differences have substantial implications on healthcare burden and health service utilization.
In general, the associations between insurance holding and SES variables are stronger among urban than rural people, reflecting the fact that the major health insurance in the rural areas is heavily subsidized by the government and thus more equally distributed among the rich and the poor.
Reimbursement rates of health insurance vary significantly by schemes, with UEMI having the highest level, followed by URMI and NCMS. Inpatient reimbursement rates increase with total medical cost to a plateau of about 60% for urban people but do not increase with total medical cost and are at much lower levels for rural people. A system of major medical insurance still does not exist in China.
While a large number of studies evaluate the impacts of NCMS, few examine the correlates of enrollment. We fill this void by examining the correlation between membership of various health insurance schemes and SES variables. For those with rural hukou, there are no strong associations between membership in types of schemes and SES covariates; however, there is for those with urban hukou. Higher levels of schooling and higher PCE are associated with being a member of the employer-based urban insurance scheme, which has much higher levels of generosity.
The difference in accessibility of healthcare facilities is large between those with and without health insurance and between rural and urban residents. Our findings are consistent with Yu (2009) in that the correlation between NCMS membership and outpatient service utilization is not statistically significant. Our findings are also consistent with Wagstaff et al. (2009), that access to NCMS is positively related to inpatient service utilization, which is also positively related to both types of urban insurance. Similar to Zhang et al. (2014), we also find no significant relationships between NCMS membership and utilization of different types of health institutions. However, people with urban health insurance are more likely to utilize facilities with higher quality.
While previous studies examine the pros and cons of China’s health service delivery and the profile of health service utilization, few have provided a complete picture across different groups of Chinese people. Also, inadequate attention has been paid to the role of health insurance status in health service utilization. Employing nationally representative survey data with a large sample size, this paper fills these gaps by documenting a more detailed profile for health insurance and healthcare utilization among different groups of mid-aged and older Chinese and examining the factors associated with health insurance schemes and healthcare utilization. For outpatient service use among rural people, there are still strong gradients of education and also of PCE. Respondents having higher levels of education and higher PCE are more likely to visit higher-quality type 1 and type 2 hospitals. The results are similar for inpatient services.
Similar to Yip et al. (2012), we conclude that despite the big achievement of expanding health insurance coverage, China still has a long way to transform such coverage into cost-effective services. The results indicate that although the expansion of health insurance coverage has improved the availability of health services and released healthcare burdens of the Chinese people to some extent, challenges still remain. Rural people are in a disadvantaged situation in that their health insurance is less generous, their care burden is higher, and their access to medical facilities with good quality is still not enough. This is largely due to the historical urban–rural disparity in all aspects of life, and the two-step strategy of the health reform also plays an important role. Now that the first step of universal coverage with shallow benefits has been reached, the next steps of health reform should target more on reducing the imbalance between people with different health schemes, particularly between urban and rural schemes. Further evaluation is needed regarding how effective the policy is in equalizing the imbalance between urban and rural areas and between people with different SES, which will be possible with more waves of CHARLS data.
Acknowledgments
The data used in this paper are from China Health and Retirement Longitudinal Study (CHARLS), funded by the National Institute on Aging (NIA) in the USA (grant no. R01-AG037031-01), the World Bank (grant no. 7159234), and the National Natural Science Foundation of China (grant no. 71130002). Financial support from the National Natural Science Foundation of China (grants nos. 71503282 and 71490732) is also acknowledged. The authors thank participants at the 2015 PAA conference for their helpful comments and suggestions. The authors also gratefully acknowledge the valuable comments of the anonymous referee. The findings, interpretations, and conclusions expressed in this paper are, however, entirely those of the authors and do not necessarily represent the views of their affiliations or the countries they represent.
Footnotes
See China Reform Daily on June 19, 2012 http://www.crd.net.cn/2012-06/19/content_5151062.htm; also see http://www.wpro.who.int/china/mediacentre/releases/2013/20130605/en/.
For instance, Larson and Hill (2006) show that rural residents are disproportionately represented among the uninsured in the USA. Telfair et al. (2003), Goins et al. (2006), and Johnson et al. (2006) show significant rural–urban disparities in health service utilization in the USA; Salinas et al. (2010) discuss the rural–urban disparities in health service utilization in Mexico; Casas et al. (2001) discuss the regional and rural–urban disparities in health and health service utilization for countries in Latin America and the Caribbean.
A random number was drawn for the first county selected and then every N-th county thereafter, where N was determined in order to sample 150 counties.
These special PSU sample frames were designed in part to maximize our chances of sampling recent urban migrants, which most other surveys in China fail to do adequately.
We have 7057 couples among these individuals. We cluster standard errors at the community level for all regressions to take into account the correlations between outcome variables. We have also clustered standard errors at the household level, and the results are robust; the standard errors are slightly larger using the community level for clustering, so we report those.
We employ the linear probability model (LPM) for easy interpretation of the estimates. The main drawbacks of the LPM are twofold: the presence of heteroscedasticity and the predicted values of the outcomes need not fall in the unit interval. We compute robust standard errors for all regressions to address the first problem. For the second problem, as our binary outcome variables neither have extreme large share of zeros nor have extreme large share of ones, few predicted values lie outside the unit interval.
Sixteen out of 17,343 respondents have zero expenditure. To deal with zeros, we calculate the variable LogPCE as log(PCE + 1).
Because people may have access to multiple types of insurance, we do not use multinomial models.
We do not draw the figure for outpatient visits as most of the insurance plans do not cover outpatient care.
We use the population size of Chinese people older than 45 in the census year of 2010 (443,254,638) as a proxy for that in the CHARLS survey year, 2011.
Data comes from the yearly statistics reported by the National Bureau of Statistics (NBS) in China.
REFERENCES
- Babiarz K, Miller G, Yi H, Zhang L, Rozelle S. New evidence on the impact of China’s new rural cooperative medical scheme and its implications for rural primary healthcare: multivariate difference-in-difference analysis. BMJ. 2010;341:C5617. doi: 10.1136/bmj.c5617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber S, Yao L. World Health Report, Background Paper. Vol. 37. World Health Organization; 2010. Health insurance systems in China: a briefing note. [Google Scholar]
- Casas J, Dachs J, Bambas A. Health disparities in Latin America and the Caribbean: the role of social and economic determinants. Equity and health. 2001;8:22–49. [Google Scholar]
- Cheng T. Taiwan’s new national health insurance program: genesis and experience so far. Health Affairs. 2003;22(3):61–76. doi: 10.1377/hlthaff.22.3.61. [DOI] [PubMed] [Google Scholar]
- Eggleston K, Li L, Meng Q, Lindelow M, Wagstaff A. Health service delivery in China: a literature review. Health Economics. 2008;17:149–165. doi: 10.1002/hec.1306. [DOI] [PubMed] [Google Scholar]
- Ellis R, Alam M, Gupta I. Health insurance in India: prognosis and prospectus. Economic and Political Weekly. 2000;35:207–217. [Google Scholar]
- Frenk J, González-Pier E, Gómez-Dantés O, Lezana M, Knaul F. Comprehensive reform to improve health system performance in Mexico. The Lancet. 2006;368(9546):1524–1534. doi: 10.1016/S0140-6736(06)69564-0. [DOI] [PubMed] [Google Scholar]
- Goins R, Williams K, Carter M, Spencer S, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. The Journal of Rural Health. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- Hu S, Tang S, Liu Y, Zhao Y, Escobar M, de Ferranti D. Reform of how health care is paid for in China: challenges and opportunities. Lancet. 2008;372(9652):1846–1853. doi: 10.1016/S0140-6736(08)61368-9. [DOI] [PubMed] [Google Scholar]
- Jian W, Chan K, Reidpath D, Xu L. China’s rural–urban care gap shrank for chronic disease patients, but inequities persist. Health Affairs. 2010;29(12):2189–2196. doi: 10.1377/hlthaff.2009.0989. [DOI] [PubMed] [Google Scholar]
- Johnson M, Brems C, Warner T, Roberts L. Rural–urban health care provider disparities in Alaska and New Mexico. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33(4):504–507. doi: 10.1007/s10488-005-0001-7. [DOI] [PubMed] [Google Scholar]
- Knaul F, Frenk J. Health insurance in Mexico: achieving universal coverage through structural reform. Health Affairs. 2005;24(6):1467–1476. doi: 10.1377/hlthaff.24.6.1467. [DOI] [PubMed] [Google Scholar]
- Larson S, Hill S. Rural–urban differences in employment-related health insurance. The Journal of Rural Health. 2006;21(1):21–30. doi: 10.1111/j.1748-0361.2005.tb00058.x. [DOI] [PubMed] [Google Scholar]
- Lei X, Lin W. The new cooperative medical scheme in rural China: does more coverage mean more service and better health? Health Economics. 2009;18(S2):S25–S46. doi: 10.1002/hec.1501. [DOI] [PubMed] [Google Scholar]
- Lin W, Liu G, Chen G. The urban resident basic medical insurance: a landmark reform towards universal coverage in China. Health Economics. 2009;18:S83–S96. doi: 10.1002/hec.1500. [DOI] [PubMed] [Google Scholar]
- Liu H, Zhao Z. Impact of China’s urban resident basic medical insurance on health care utilization and expenditure. IZA Discussion Paper, No. 6768. 2012 [Google Scholar]
- Liu M, et al. Rural and urban disparity in health services utilization in China. Medical Care. 2007;45(8):767–774. doi: 10.1097/MLR.0b013e3180618b9a. [DOI] [PubMed] [Google Scholar]
- Liu Y, Hsiao W, Eggleston K. Equity in health and health care: the Chinese experience. Social Science & Medicine. 1999;49(10):1349–1356. doi: 10.1016/s0277-9536(99)00207-5. [DOI] [PubMed] [Google Scholar]
- Qian D, Pong R, Yin A, Nagarajan K, Meng Q. Determinants of health care demand in poor, rural China: the case of Gansu Province. Health Policy and Planning. 2009;24:324–334. doi: 10.1093/heapol/czp016. [DOI] [PubMed] [Google Scholar]
- Salinas JJ, et al. The rural–urban divide: health services utilization among older Mexicans in Mexico. The Journal of Rural Health. 2010;26(4):333–341. doi: 10.1111/j.1748-0361.2010.00297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L. Health care in China: a rural–urban comparison after the socioeconomic reforms. Bulletin of the World Health Organization. 1993;71(6):723. [PMC free article] [PubMed] [Google Scholar]
- Strauss J, Hong H, Lei X, Li L, Park A, Yang L, Zhao Y-H. Health care and insurance among the elderly in China: evidence from the CHARLS Pilot. In: Majmundar M, Smith JP, editors. Aging in Asia: Findings from New and Emerging Data Initiatives, Committee on Policy Research and Data Needs to Meet the Challenge of Aging in Asia, National Research Council. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008;372(9648):1493–1501. doi: 10.1016/S0140-6736(08)61364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telfair J, et al. Rural/urban differences in access to and utilization of services among people in Alabama with sickle cell disease. Public Health Reports. 2003;118(1):27. doi: 10.1093/phr/118.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagstaff A, Lindelow M, Jun G, Xu L, Qian J. Extending health insurance to rural population: an impact evaluation of China’s new cooperative medical scheme. Health Economics. 2009;28(1):1–19. doi: 10.1016/j.jhealeco.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Wagstaff A, Yip W, Lindelow M, Hsiao W. China’s health systems and its reform: a review of recent studies. Health Economics. 2009;18(0):S7–S23. doi: 10.1002/hec.1518. [DOI] [PubMed] [Google Scholar]
- Yip W. Disparities in health care and health status: the rural–urban gap and beyond. In: Whyte MK, editor. One Country. Two Societies: Harvard University Press; 2010. pp. 147–165. Rural–Urban Inequality in Contemporary China. [Google Scholar]
- Yip W, Hsiao W, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China’s huge and complex health-care reforms. Lancet. 2012;379(9818):833–842. doi: 10.1016/S0140-6736(11)61880-1. [DOI] [PubMed] [Google Scholar]
- Yip W, Mahal A. The health care system of China and India: performance and future challenges. Health Affairs. 2008;27(4):921–932. doi: 10.1377/hlthaff.27.4.921. [DOI] [PubMed] [Google Scholar]
- You X, Kobayashi Y. The new cooperative medical scheme in China. Health Policy. 2009;91(1):1–9. doi: 10.1016/j.healthpol.2008.11.012. [DOI] [PubMed] [Google Scholar]
- Yu B, Meng Q, Collins C, Tolhurs R, Tang S, Yan F, Bogg L, Liu X. How does the new cooperative medical scheme influence health service utilization? A study in two provinces in rural China. BMC Health Services Research. 2010;10:116. doi: 10.1186/1472-6963-10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Wang Z, Qian D, Ni J. Effects of changes in health insurance reimbursement level on outpatient service utilization of rural diabetics: evidence from Jiangsu Province, China. BMC Health Services Research. 2014;14:185. doi: 10.1186/1472-6963-14-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Kanbur R. Spatial inequality in education and health care in China. China Economic Review. 2005;16:189–204. [Google Scholar]
- Zhao Y, Strauss J, Yang G, Giles J, Hu P, Hu Y, Lei X, Liu M, Park A, Smith J, Wang Y. China Health and Retirement Longitudinal Study-2011–2012 National Baseline User’s Guide. School of National Development, Peking University; 2013. http://charls.ccer.edu.cn/en/page/documentation/2011_national_baseline. [Google Scholar]