Abstract
AIM
To evaluate the technical success, diagnostic yield (DY) and therapeutic potential of retrograde single balloon enteroscopy (rSBE).
METHODS
A retrospective review of 136 rSBE procedures performed at a tertiary academic referral center from January 2006 and September 2013 was completed. Patient characteristics including age, gender and inpatient status were collected. The indication for the procedure was categorized into one of three groups: Obscure gastrointestinal bleeding (GIB), evaluation for Crohn’s disease and abnormal imaging. Procedural characteristics including insertion depth (ID), procedure time, concordance with pre-procedural imaging and complications were also recorded. Lastly, DY, defined as the percentage of cases producing either a definitive diagnosis or findings that could explain clinical symptoms and therapeutic yield (TY), defined as the percentage of cases in which a definitive intervention was performed, were determined. Mucosal tattooing and biopsy alone were not included in the TY.
RESULTS
A total of 136 rSBE procedures were identified. Mean patient age was 57.5 (± 16.2) years, 67 (49.2%) were male, and 110 (80.9%) procedures were performed on an outpatient basis. Indications for rSBE included GIB in 55 (40.4%), evaluation of inflammatory bowel disease (IBD) in 29 (21.3%), and imaging suggestive of pathology other than GIB or IBD in 43 (31.6%). Nine (6.6%) rSBEs were performed for other indications. Mean ID was 68.3 (± 39.3) cm proximal to the ileocecal valve and mean time to completion was 41.7 (± 15.5) min. Overall, 73 (53.7%) cases were diagnostic and 25 (18.4%) cases were therapeutic in which interventions (argon plasma coagulation, stricture dilatation, polypectomy, etc.) were performed. Pre-procedural imaging was performed in 88 (64.7%) patients. Endoscopic concordance of positive imaging findings was seen in 31 (35.2%) cases. Follow up data was available in 93 (68.4%) patients; 2 (2.2%) reported post-procedural abdominal pain within 30 d following rSBE. There were no other reported complications.
CONCLUSION
rSBE exhibits an acceptable diagnostic and TY, rendering it a safe and effective procedure for the evaluation and treatment of small bowel diseases.
Keywords: Retrograde, Single-balloon, Enteroscopy, Endoscopy
Core tip: Disorders of the small intestine account for an increasing number of hospital discharges and aggregate healthcare cost. Single-balloon enteroscopy (SBE) represents a novel approach to diagnose and treat small bowel disease and can be performed via the antegrade or retrograde approach. SBE has different performance characteristics depending upon the route chosen, but most studies combine the information. Little data exists on the retrograde approach alone, a notoriously difficult procedure. This study constitutes the largest published cohort to date of retrograde SBE, with a focus on patient and procedural characteristics, diagnostic and therapeutic yield.
INTRODUCTION
Since its release in 2006, single-balloon endoscopy (SBE) has emerged as a therapeutic option for small bowel lesions visualized by noninvasive tests such as wireless capsule endoscopy. The small bowel can be deeply intubated via the antegrade (mouth) or retrograde approach (anus) depending on the probable location of the suspected lesion. The retrograde approach to SBE has been described as more technically challenging than the antegrade approach for multiple reasons, including: The length and tortuosity of the colon, difficulty traversing the ileocecal valve (ICV) and potential for colonic contents to interfere with the function of the overtube[1]. Limited data is available on performance metrics of retrograde single-balloon endoscopy (rSBE), such as success, complications, diagnostic yield (DY) and therapeutic yield (TY).
In cases where lesions are diffuse or the exact location of a lesion is not clear, many endoscopists will initially perform antegrade enteroscopy, largely because it is technically easier to perform. The retrograde approach is typically chosen when imaging suggests a very distal small bowel lesion. Other indications for retrograde procedures include a non-diagnostic antegrade examination, or as a complimentary procedure to an antegrade examination when complete enteroscopy (CE) is desired[2]. In addition to its more challenging nature, there may also be a longer learning curve[1]. Average insertion depths proximal to the ICV via the retrograde approach have been reported from 73 to 199 cm, but these studies are limited by a relatively small sample size of retrograde cases[2-4]. The purpose of this report is to describe our center’s experience with rSBE, the largest published cohort to date.
MATERIALS AND METHODS
We performed a retrospective analysis of all rSBEs performed at the University of Maryland Medical Center from January 2006 to April 2015. All cases of rSBE were performed by one of three therapeutic endoscopists, who began performing the procedure in 2006 without any formal training. Patient and procedural data were obtained from electronic medical records and the electronic endoscopy reporting system, ProVation MD® (MN). The study was approved by the University of Maryland Medical Center Institutional Review Board.
All patients underwent SBE for accepted indications after signed informed consent was obtained. All patients underwent bowel cleansing prior to the procedure with standard preparations, most receiving four liters of polyethylene glycol. Most cases were performed with monitored anesthesia care, although some were performed under conscious sedation. Few cases were conducted under general anesthesia. The anesthesiologist determined the type of sedation utilized. Fluoroscopy was utilized in select cases, most often in the context of retrieval of a retained capsule.
The indication for rSBE was categorized into one of three groups: Obscure gastrointestinal bleeding (OGIB), abnormal imaging or evaluation of Crohn’s disease. OGIB was defined as persistent or recurrent bleeding whose source was not identified by conventional studies, such as colonoscopy or esophagogastroduodenoscopy (EGD). Abnormal imaging was defined as any abnormality detected via video capsule endoscopy (VCE) or noninvasive radiological study. rSBEs performed for the evaluation of Crohn’s included both cases of previously established disease and suspected, but yet undiagnosed, Crohn’s disease.
Insertion depth (ID) was determined quantitatively, in terms of centimeters (cm) beyond the ICV in some cases, and qualitatively, in terms of the anatomic extent reached, in others. Quantitatively determined ID was estimated during withdrawal of the scope by adding 5 cm increments, similar to the technique described by Efthymiou et al[5]. Procedure time was determined by the time at which the enteroscope was passed through the anus to the time at which it was completely withdrawn. Technical failure was defined as the inability to advance the enteroscope beyond 20 cm proximal to the ICV. Positive findings were defined as any abnormality that explained the patient’s presentation or that required therapeutic intervention. Cases in which positive findings were not observed were categorized as normal exams or technically difficult studies (due either to poor bowel preparation or technical failure). For rSBEs performed due to abnormal imaging, endoscopic concordance was defined as ability of enteroscopy to corroborate the abnormality seen on imaging. DY was defined by the percentage of cases producing either a definitive diagnosis or findings that could explain clinical symptoms. TY was defined as the percentage of cases in which a definitive intervention was performed. Excluded from this definition were cases in which only tissue specimens or mucosal tattooing were achieved. Post-procedure complications were defined as any symptomatic complaint or hospital re-admission within 30 d following rSBE.
Single-balloon system
The Olympus SIF-Q180® (Olympus, Center Valley, Pennsylvania, USA) is a 200-cm high-resolution enteroscope with a 2.8 mm working channel that uses a 140-cm long × 13.2-mm outer diameter flexible overtube. The silicone balloon at the tip of the over tube can be inflated and deflated via an external balloon control module, conventionally within a pressure range of 6-16 kPa. The technique of rSBE has been described previously and is widely recognized[6].
Biostatistics
The statistical methods of this study were reviewed only by the authors listed above and no one else.
RESULTS
Patient demographics and pre-procedural characteristics are presented in Table 1. A total of 136 rSBEs were performed. Mean age was 57.5 years. Sixty-nine (50.7%) patients were female, and 110 (80.9%) cases were on outpatients. Eighteen (13.2%) cases were conducted in patients with post-surgical anatomy due to prior intestinal surgery. Procedural data is presented in Table 2. Fluoroscopy was utilized in only 5 (3.7%) cases. Monitored anesthesia with propofol was the anesthetic strategy in 103 (75.7%) cases. Conscious sedation and generalized anesthesia were utilized in 28 (20.6%) and 5 (3.7%) cases, respectively.
Table 1.
Patient characteristics and pre-procedural characteristics n (%)
| Factor | Value |
| Age (yr) | 57.5 |
| Female | 69 (50.7) |
| Outpatient | 110 (80.9) |
| Pre-procedural imaging | 88 (64.7) |
| Indication | |
| Gastrointestinal bleeding | 55 (40.4) |
| Suspected or known CD | 29 (21.3) |
| Abnormal imaging | 43 (31.6) |
| Other | 9 (6.6) |
| ASA classification | |
| Class I | 8 (5.9) |
| Class II | 109 (80.1) |
| Class III | 19 (14.0) |
CD: Crohn’s disease; ASA: American Society for Anesthesiologists.
Table 2.
Procedural characteristics and findings
| Factor | Value |
| Anesthesia | |
| Monitored anesthesia care | 103 (75.7) |
| Conscious sedation | 28 (20.6) |
| General anesthesia | 5 (3.7) |
| Fluoroscopy | 5 (3.7) |
| Time to completion (min) | 41.7 (15.5) |
| Insertion depth | |
| Quantitative (cm)1 | 68.3 (39.3) |
| Qualitative | |
| Distal ileum | 29 (51.8) |
| Mid ileum | 17 (30.4) |
| Proximal ileum | 5 (8.9) |
| Distal jejunum | 4 (7.1) |
| Mid jejunum | 1 (1.8) |
| Findings | |
| Ulcer | 22 (31.9) |
| Angioectasia | 8 (11.6) |
| Erosion | 3 (4.3) |
| Stricture | 12 (17.4) |
| Polyp | 14 (20.3) |
| Inflammation | 9 (13.0) |
| Other | 6 (8.7) |
As measured from the ileocecal valve. Values presented as mean (SD) for time and quantitative depth, and n (%) otherwise.
Primary indications for rSBE were 55 (40.4%) cases for OGIB, 29 (21.3%) for evaluation of Crohn’s disease and 43 (31.6%) for abnormal radiographic or endoscopic findings observed during the workup of GI complaints unrelated to OGIB or suspected Crohn’s, such as a possible small bowel mass. Another 9 (6.6%) procedures were conducted in patients varied symptoms unrelated to the above three categories, such as diarrhea (Table 1). Imaging data was available in 88 (64.7%) patients. Among them, 69 (78.4%) underwent VCE, 9 (10.22%) computed tomography (CT), 5 (5.7%) magnetic resonance enterography (MRE), 4 (4.5%) small bowel series (SBS) and 1 (1.1%) Meckel’s scan.
ID was estimated quantitatively in 67 (49.3%) cases. Mean ID in these cases was 68.3 ± 39.3 cm. Sixty-three (94.0%) of the cases met criteria for technical success with ID at least 20 cm beyond the ICV. Fifty (74.6%) cases reached at least 50 cm beyond the ICV, and 20 (29.9%), at least 80 cm (Figure 1). Among 56 (41.2%) cases in which ID was qualitatively described on the basis of anatomic extent reached, 29 (51.8%) cases reached the distal ileum, 17 (30.4%) cases reached the mid-ileum and 5 (8.9%) reached the proximal ileum. The jejunum was reached in 5 (8.9%) cases.
Figure 1.
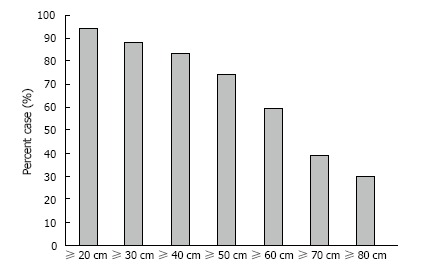
Insertion depth beyond the ileocecal valve.
Overall, 73 cases were diagnostic, producing a DY of 53.7%. The 63 non-diagnostic cases were due to a normal examination in 45 (71.4%) cases, technical failure in 11 (17.5%), and poor preparation or fresh blood in the intestinal lumen in 7 (11.1%). Concordance between abnormalities detected on imaging and rSBE was seen in 31 of the 88 (35.2%) cases in which prior imaging was available. Positive endoscopic findings were present in 69 (50.7%) of all cases, including 22 (31.9%) ulcers, 14 (20.3%) polyps, 12 (17.4%) strictures, 8 (11.6%) arteriovenous malformations (AVMs), and 9 (13.0%) cases with chronic inflammatory changes. One (1.4%) Dieulafoy lesion, 3 (4.3%) diverticuli, 3 (4.3%) erosions and 2 (2.9%) mass lesions accounted for the remaining 6 (13.0%) cases.
There were 25 (18.4 %) therapeutic cases. Argon plasma coagulation (APC) was utilized in 6 (24.0%), stricture dilatation in 8 (32.0%), hemoclipping in 2 (8.0%), polypectomy and removal in 9 (36.0%). Tissue specimens and/or mucosal tattooing were obtained in 48 (35.3%) cases, but these were not included in the overall TY. Eighteen (13.2%) cases were technical failures. However, in one such case, an ileal stricture was diagnosed within 20 cm of the ICV, and in four, a colonic source was identified as the most probable etiology, despite inability to intubate the ICV.
DY per indication for rSBE was 16 of 55 (29.1%) cases for OGIB, 12 of 43 (27.9%) cases for abnormal imaging and 1 of 9 (11.1%) rSBEs indicated due to other reasons. Twelve new diagnoses of Crohn’s disease were established. Similarly, TY per indication was 8 (14.5%) cases for OGIB, 5 (17.2%) for Crohn’s, 10 (23.3%) for abnormal imaging and 2 (22.2%) for rSBE indicated due to other reasons. Post-procedural symptomatic complaints were observed only in 2 among 93 (2.2%) cases in which this data was available. Both of these patients had self-limiting pain and neither required medical intervention or were readmitted to the hospital within 30 d of the procedure. There were no major adverse events. Finally, procedural characteristics were analyzed according to year in which the procedure was conducted, with no significant trends noted in terms of ID, procedure time, diagnostic or TY or failure rates from 2006 to 2013.
DISCUSSION
Disorders of the small intestine account for an increasing number of hospital discharges and aggregate healthcare cost[7]. Continuing to develop the expertise and technical proficiency to safely and effectively visualize and treat disorders of the small bowel remains a challenge. Deep enteroscopy techniques have helped to open what has long been considered the endoscopist’s “black box”[5]. SBE has emerged as a feasible alternative to double-balloon endoscopy in the evaluation of these disorders, due to its increased ease of setup[8], wider availability[1,9], and similar DY[2,5]. A less studied topic has been route selection. The antegrade approach is preferred in cases of suspected small bowel pathology with no localizing evidence, because diagnostic and TYs have been shown to be superior[10-12]. This is likely the result of the proximal (i.e., jejunal) location of most small bowel pathology[13]. The technical challenges of the retrograde approach, in both single and double-balloon platforms, is also well documented[1,11,14]. However, because CE is seldom achieved via one route alone[13], and because capsule endoscopy’s ability to accurately localize lesions is notoriously poor[15,16], facility with the retrograde approach is important. Our study evaluated the efficacy and safety of retrograde enteroscopy in 136 patients, the largest case series of rSBE reported to date.
The primary indications for rSBE in our population were similar to those in other studies[2,3,17], and included OGIB (40.4%), abnormal imaging (31.6%), and evaluation of Crohn’s disease (21.3%). Our concordance rate between abnormalities detected on imaging and enteroscopy was 35.2%, slightly lower than 2 prior studies[3,17]. One explanation for our overall low concordance rate is that erosions and ulcers on capsule studies can be transient and false positives are common[3]. Since ulcers were the most prevalent finding in our population, a lower concordance was expected.
There are multiple methods to determine ID, including fold counting and the 40 cm push-pull cycles described by May et al[8]. Our endoscopists routinely determine ID by addition of 5 cm increments upon withdrawal of the scope. Prior studies have reported a range of IDs from 73-199 cm for rSBE[2-4,18,19]. In our population, 26 (38.8%) retrograde exams were at least 70 cm beyond the ICV. Although no strict correlation exists between ID and DY[20,21], reproducible IDs support the technical feasibility of rSBE.
Average procedure time in our population was 41.7 ± 15.5 min. Previous studies report a range of 48-78 min for rSBE and 38-82 min for the antegrade approach[2-4,17-19,22]. Our observed mean procedure time also compares favorably to previously reported procedure times for retrograde double-balloon endoscopy, which ranges from 59 to 90 min[11,23]. To our knowledge, no studies have demonstrated a relationship between procedure time and DY. Operator experience and patient anatomy are among several factors that may affect procedure time. Shorter procedure time may lend itself to increased cost-effectiveness, and should be a topic for future study.
A definitive diagnosis was established in 73 (53.7%) cases. One prior study of 34 rSBE cases reported a similar DY of 47.0%[17]. The DY of SBE ranges from 41% to 65%[2-4,8,18,19,22,24-26]. In our study, pathology limited to the colon was included in the overall DY, and in all 13 (9.6%) such cases, patients’ symptoms were deemed attributable to a colonic source. DYs were 29.1% and 27.9% in cases of OGIB and abnormal imaging, respectively. For those cases in which Crohn’s disease was suspected, rSBE established that diagnosis in 41.4% of cases. Prior studies predominantly examining the antegrade approach have reported yields of 42.9%-60.0% for OGIB and 25.0%-65.0% for abnormal imaging[4,17].
Twenty-five (18.4%) cases were therapeutic. APC was performed in 6 (24.0%), stricture dilatation in 8 (32.0%), hemoclipping in 2 (8.0%), and polypectomy in 9 (36.0%). TY has never been reported in the isolated context of rSBE, but overall TY for SBE is highly variable ranging from 7%-50%[2-4,8,18,19,22,24-26]. Tissue specimens were obtained where appropriate in 48 (35.3%) cases, but were not considered in the overall TY.
Technical failure, defined in this study as inability to traverse at least 20 cm beyond the ICV, occurred in 18 (13.2%) cases. However, six such cases remained diagnostic either because pathology was found within 20 cm of the ICV or symptoms were attributed to a colonic source. Most technical failures were caused by inability to deeply intubate the ICV. Previous studies have reported failure rates for rSBE ranging from 10%-16%[3,4]. Failure rates in retrograde DBE are more highly variable, occurring in up to 30% of cases[11,23,24,27].
The types of endoscopic findings in our study also merit discussion. Specifically, only 8 (11.6%) had vascular lesions, whereas 22 (31.9%) had ulcers, 12 (17.4%) had strictures and 14 (20.3%) had polyps. One study reported a similar distribution of endoscopic lesions[17], whereas two others reported vascular lesions as the most common[3,22]. The relatively high prevalence of Crohn’s disease in our population may explain this finding. These findings are also consistent with the categorization proposed by one author of typically “jejunal” processes (including obscure overt GIB presenting as melena, among others) vs typically “ileal” processes (including ileal Crohn’s disease, among others)[13].
The limitations of this study include the absence of long-term follow-up data and the retrospective single-center setting. Furthermore, imaging and endoscopy reports that lead to the decision to pursue rSBE were not available in all patients, and so it is possible that our concordance rate may be skewed. Additionally, ID was not quantitatively determined in all cases. Larger prospective studies of rSBE with specific emphasis on long term outcomes and cost-effectiveness are needed to fully define its role in daily clinical gastroenterology.
The niche for SBE in the evaluation of disorders of the small bowel continues to develop. In the correct clinical context and with radiographic or capsule findings to suggest distal pathology, the retrograde approach is appropriate. Therefore, facility with this procedure is important for endoscopists involved in the care of these patients. Inherently, this approach poses a technical challenge because the tortuosity of the colon induces significant looping of the enteroscopy and ICV is often retroverted. To date, studies describing experience with rSBE have dealt with relatively few cases. Our study demonstrates that rSBE is a technically feasible, safe and effective procedure with acceptable diagnostic and TYs.
COMMENTS
Background
Single-balloon enteroscopy (SBE) represents a novel approach to diagnose and treat small bowel disease. The small bowel can be deeply intubated via the anterograde (mouth) or retrograde (anus) approach depending on the probable location of the suspected lesion. SBE has different performance characteristics depending upon the route chosen, but most studies combine the information. This study constitutes the largest published cohort to date of retrograde single-balloon enteroscopy (rSBE).
Research frontiers
Limited data is available on performance metrics of rSBE, such as success, complications, diagnostic yield (DY) and therapeutic yield (TY). Many studies include both and antegrade and retrograde approach for SBE in the study sample, which typically is of a small size. Regarding double vs single-balloon technique, there is evidence to suggest that there is no difference between the two in terms of DY, TY, insertion depth and procedure time.
Innovations and breakthroughs
As previously mentioned, this study adds to the small body of literature on rSBE. Results demonstrate that rSBE is a technically feasible, safe and effective procedure with acceptable diagnostic and TYs.
Applications
Developing the expertise and technical proficiency to safely and effectively visualize and treat disorders of the small bowel remains a challenge, but deep enteroscopy techniques have helped to open what has long been considered the endoscopist’s “black box”. Given that disorders of the small intestine account for an increasing number of hospital discharges and aggregate healthcare cost, research into the most beneficial type of procedure with the appropriate route selection is important. Larger prospective studies of rSBE with specific emphasis on long term outcomes and cost-effectiveness are needed to fully define its role in daily clinical gastroenterology.
Terminology
Antegrade: Approach into the small bowel via the mouth; Retrograde: Approach into the small bowel via the anus; Enteroscopy: Procedure with an enteroscope to directly visualize the small bowel.
Peer-review
rSBE is a very useful interventional procedure of notorious difficulty though. Authors are presenting their experience that is quite impressive for both numbers and results. Manuscript, written in fluent and understandable English is very concise and explanatory.
Footnotes
Institutional review board statement: This study was reviewed and approved by the University of Maryland Medical Center Institutional Review Board. Please see the attached document.
Informed consent statement: All study participants, or their legal guardian, provided informed consent (written or verbal, as appropriate) prior to undergoing the procedures retrospectively described in this study.
Conflict-of-interest statement: Christian, KE and Kapoor K have no conflicts of interest to report. Goldberg EM has served as a consultant for both Olympus and Boston Scientific. Please see the attached signed document.
Data sharing statement: No additional data are available. Please see the attached signed document.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: October 3, 2015
First decision: December 28, 2015
Article in press: May 9, 2016
P- Reviewer: Giannopoulos GA, Skok P, Sharma SS S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
References
- 1.Manno M, Barbera C, Bertani H, Manta R, Mirante VG, Dabizzi E, Caruso A, Pigo F, Olivetti G, Conigliaro R. Single balloon enteroscopy: Technical aspects and clinical applications. World J Gastrointest Endosc. 2012;4:28–32. doi: 10.4253/wjge.v4.i2.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Domagk D, Mensink P, Aktas H, Lenz P, Meister T, Luegering A, Ullerich H, Aabakken L, Heinecke A, Domschke W, et al. Single- vs. double-balloon enteroscopy in small-bowel diagnostics: a randomized multicenter trial. Endoscopy. 2011;43:472–476. doi: 10.1055/s-0030-1256247. [DOI] [PubMed] [Google Scholar]
- 3.Upchurch BR, Sanaka MR, Lopez AR, Vargo JJ. The clinical utility of single-balloon enteroscopy: a single-center experience of 172 procedures. Gastrointest Endosc. 2010;71:1218–1223. doi: 10.1016/j.gie.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Ramchandani M, Reddy DN, Gupta R, Lakhtakia S, Tandan M, Rao GV, Darisetty S. Diagnostic yield and therapeutic impact of single-balloon enteroscopy: series of 106 cases. J Gastroenterol Hepatol. 2009;24:1631–1638. doi: 10.1111/j.1440-1746.2009.05936.x. [DOI] [PubMed] [Google Scholar]
- 5.Efthymiou M, Desmond PV, Brown G, La Nauze R, Kaffes A, Chua TJ, Taylor AC. SINGLE-01: a randomized, controlled trial comparing the efficacy and depth of insertion of single- and double-balloon enteroscopy by using a novel method to determine insertion depth. Gastrointest Endosc. 2012;76:972–980. doi: 10.1016/j.gie.2012.06.033. [DOI] [PubMed] [Google Scholar]
- 6.Buscaglia JM, Okolo PI. Deep enteroscopy: training, indications, and the endoscopic technique. Gastrointest Endosc. 2011;73:1023–1028. doi: 10.1016/j.gie.2011.01.026. [DOI] [PubMed] [Google Scholar]
- 7.Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, Gangarosa LM, Thiny MT, Stizenberg K, Morgan DR, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187.e1-3. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.May A, Färber M, Aschmoneit I, Pohl J, Manner H, Lotterer E, Möschler O, Kunz J, Gossner L, Mönkemüller K, et al. Prospective multicenter trial comparing push-and-pull enteroscopy with the single- and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol. 2010;105:575–581. doi: 10.1038/ajg.2009.712. [DOI] [PubMed] [Google Scholar]
- 9.Upchurch BR, Vargo JJ. Single-balloon enteroscopy. Gastrointest Endosc Clin N Am. 2009;19:335–347. doi: 10.1016/j.giec.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Akyüz Ü, Pata C, Kalayci M, Özdıl K, Altun H, Karıp B, Akyüz F. Route selection for double balloon enteroscopy in patients with obscure gastrointestinal bleeding: experience from a single center. Turk J Gastroenterol. 2012;23:670–675. [PubMed] [Google Scholar]
- 11.Sanaka MR, Navaneethan U, Kosuru B, Yerneni H, Lopez R, Vargo JJ. Antegrade is more effective than retrograde enteroscopy for evaluation and management of suspected small-bowel disease. Clin Gastroenterol Hepatol. 2012;10:910–916. doi: 10.1016/j.cgh.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Dutta AK, Sajith KG, Joseph AJ, Simon EG, Chacko A. Learning curve, diagnostic yield and safety of single balloon enteroscopy. Trop Gastroenterol. 2012;33:179–184. doi: 10.7869/tg.2012.45. [DOI] [PubMed] [Google Scholar]
- 13.Mönkemüller K. Should we illuminate the black box of the small bowel mucosa from above or below? Clin Gastroenterol Hepatol. 2012;10:917–919. doi: 10.1016/j.cgh.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 14.Bourreille A, Ignjatovic A, Aabakken L, Loftus EV, Eliakim R, Pennazio M, Bouhnik Y, Seidman E, Keuchel M, Albert JG, et al. Role of small-bowel endoscopy in the management of patients with inflammatory bowel disease: an international OMED-ECCO consensus. Endoscopy. 2009;41:618–637. doi: 10.1055/s-0029-1214790. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad NA, Iqbal N, Joyce A. Clinical impact of capsule endoscopy on management of gastrointestinal disorders. Clin Gastroenterol Hepatol. 2008;6:433–437. doi: 10.1016/j.cgh.2007.12.035. [DOI] [PubMed] [Google Scholar]
- 16.Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010;71:280–286. doi: 10.1016/j.gie.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 17.Prachayakul V, Deesomsak M, Aswakul P, Leelakusolvong S. The utility of single-balloon enteroscopy for the diagnosis and management of small bowel disorders according to their clinical manifestations: a retrospective review. BMC Gastroenterol. 2013;13:103. doi: 10.1186/1471-230X-13-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsujikawa T, Saitoh Y, Andoh A, Imaeda H, Hata K, Minematsu H, Senoh K, Hayafuji K, Ogawa A, Nakahara T, et al. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: preliminary experiences. Endoscopy. 2008;40:11–15. doi: 10.1055/s-2007-966976. [DOI] [PubMed] [Google Scholar]
- 19.Khashab MA, Lennon AM, Dunbar KB, Singh VK, Chandrasekhara V, Giday S, Canto MI, Buscaglia JM, Kapoor S, Shin EJ, et al. A comparative evaluation of single-balloon enteroscopy and spiral enteroscopy for patients with mid-gut disorders. Gastrointest Endosc. 2010;72:766–772. doi: 10.1016/j.gie.2010.04.043. [DOI] [PubMed] [Google Scholar]
- 20.Albert JG. Interventional balloon-enteroscopy. J Interv Gastroenterol. 2012;2:42–50. doi: 10.4161/jig.20134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xin L, Gao Y, Liao Z, Li ZS. The reasonable calculation of complete enteroscopy rate for balloon-assisted enteroscopy. Endoscopy. 2011;43:832; author reply 832. doi: 10.1055/s-0030-1256569. [DOI] [PubMed] [Google Scholar]
- 22.Frantz DJ, Dellon ES, Grimm IS, Morgan DR. Single-balloon enteroscopy: results from an initial experience at a U.S. tertiary-care center. Gastrointest Endosc. 2010;72:422–426. doi: 10.1016/j.gie.2010.03.1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Caro S, May A, Heine DG, Fini L, Landi B, Petruzziello L, Cellier C, Mulder CJ, Costamagna G, Ell C, et al. The European experience with double-balloon enteroscopy: indications, methodology, safety, and clinical impact. Gastrointest Endosc. 2005;62:545–550. doi: 10.1016/j.gie.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 24.Aktas H, de Ridder L, Haringsma J, Kuipers EJ, Mensink PB. Complications of single-balloon enteroscopy: a prospective evaluation of 166 procedures. Endoscopy. 2010;42:365–368. doi: 10.1055/s-0029-1243931. [DOI] [PubMed] [Google Scholar]
- 25.Kawamura T, Yasuda K, Tanaka K, Uno K, Ueda M, Sanada K, Nakajima M. Clinical evaluation of a newly developed single-balloon enteroscope. Gastrointest Endosc. 2008;68:1112–1116. doi: 10.1016/j.gie.2008.03.1063. [DOI] [PubMed] [Google Scholar]
- 26.Takano N, Yamada A, Watabe H, Togo G, Yamaji Y, Yoshida H, Kawabe T, Omata M, Koike K. Single-balloon versus double-balloon endoscopy for achieving total enteroscopy: a randomized, controlled trial. Gastrointest Endosc. 2011;73:734–739. doi: 10.1016/j.gie.2010.10.047. [DOI] [PubMed] [Google Scholar]
- 27.Mehdizadeh S, Ross A, Gerson L, Leighton J, Chen A, Schembre D, Chen G, Semrad C, Kamal A, Harrison EM, et al. What is the learning curve associated with double-balloon enteroscopy? Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc. 2006;64:740–750. doi: 10.1016/j.gie.2006.05.022. [DOI] [PubMed] [Google Scholar]


