Abstract
Dedifferentiated endometrial carcinoma is an aggressive type of endometrial cancer that contains a mix of low grade endometrioid and undifferentiated carcinoma components. We performed targeted sequencing of 8 dedifferentiated endometrial carcinomas and identified somatic frameshift/nonsense mutations in SMARCA4, a core member of the switch/sucrose non-fermenting (SWI/SNF) complex, in the undifferentiated components of 4 tumors. Immunohistochemical analysis confirmed the loss of SMARCA4 in the undifferentiated component of these 4 SMARCA4-mutated cases while the corresponding low grade endometrioid component showed retained SMARCA4 expression. An expanded survey of another member of the SWI/SNF complex showed SMARCB1 loss in the undifferentiated component of 2 SMARCA4-intact tumors. Subsequent immunohistochemical analysis of SMARCA4 and SMARCB1 was done in an additional set of 22 centrally reviewed dedifferentiated endometrial carcinomas and 31 grade 3 endometrioid carcinomas. Combining the results from the index and the expansion set, 15 of 30 (50%) of the dedifferentiated endometrial carcinomas examined showed either SMARCA4 loss (37%) or SMARCB1 loss (13%). The loss of SMARCA4 or SMARCB1 was mutually exclusive and occurred only in the undifferentiated component. All 31 grade 3 endometrioid carcinomas showed intact SMARCA4/SMARCB1 expression. The majority (73%) of the SMARCA4-deficient and half of SMARCB1-deficient undifferentiated component developed in a mismatch repair protein (MMR)-deficient molecular context. The observed spatial association between SMARCA4/SMARCB1 loss and histologic dedifferentiation suggests that loss of these SWI/SNF complex proteins may contribute to the development of dedifferentiated endometrial carcinoma.
Keywords: Endometrial cancer, dedifferentiated carcinoma, undifferentiated carcinoma, dedifferentiation, SMARCA4, SMARCB1, BRG1, INI1, SWI/SNF
Introduction
Dedifferentiated endometrial carcinoma is a subtype of endometrial cancer in which an endometrioid carcinoma occurs in association with an undifferentiated carcinoma. In the initial series described by Silva et al,1, 2 the endometrioid component displayed either FIGO (The International Federation of Gynecology and Obstetrics) grade 1 or 2 morphology. In contrast to the differentiated component, the undifferentiated component was composed of monotonous medium to large round/polygonal cells growing in solid discohesive sheets, without any evidence of glandular formation. The undifferentiated component showed a high mitotic rate with the majority showing tumor necrosis. Some of the undifferentiated components also exhibited focal rhabdoid cytologic features, focal marked nuclear pleomorphism or abrupt keratinization. It was postulated that the undifferentiated carcinoma represented a form of tumor progression termed “dedifferentiation” from the pre-existing low-grade endometrioid carcinoma, and that this phenomenon of dedifferentiation was associated with a highly aggressive clinical course, even in cases where the undifferentiated carcinoma constituted a minor component of the overall tumor.1
Since the original report by Silva et al, dedifferentiated endometrial carcinoma has become increasingly recognized by pathologists.3-6 An association between dedifferentiated histology and mismatch repair (MMR) protein deficiency/Lynch syndrome was subsequently recognized,7, 8 with 58% of the dedifferentiated endometrial carcinomas reported to show MMR deficiency by immunohistochemistry5. In these MMR-deficient cases, the differentiated endometrioid component and undifferentiated component both showed an identical pattern of MMR deficiency. Most recently, Kuhn et al compared the mutation profiles between the endometrioid component and undifferentiated component of a series of dedifferentiated endometrial carcinomas.4 They identified the same somatic mutations in the corresponding endometrioid and undifferentiated components in all cases. While these findings support a clonal origin between the differentiated endometrioid and undifferentiated component of dedifferentiated endometrial carcinoma, the precise molecular mechanism underlying this postulated progression from low-grade endometrioid carcinoma to undifferentiated carcinoma (dedifferentiation) remains poorly understood.
In this study, we performed targeted sequencing and immunohistochemical analysis comparing the endometrioid and the undifferentiated component of a series of dedifferentiated endometrial carcinomas. We identified frequent inactivation of SMARCA4 or SMARCB1 in the undifferentiated component of these tumors, indicating that a loss of expression of these switch/sucrose non-fermenting (SWI/SNF) complex proteins may contribute to the process of dedifferentiation in endometrial carcinoma.
Materials and methods
Study samples
The study included 8 dedifferentiated endometrial carcinomas in the index series and 22 dedifferentiated endometrial carcinomas in the validation series. All cases were centrally reviewed, fulfilling the morphologic features described by Silva et al.1, 2 We excluded cases that were inadequately fixed such that histologic evaluation could not be properly performed. Tumors showing focal glandular differentiation (away from apparent interface between differentiated and undifferentiated components), well-demarcated cohesive lobules and/or cellular spindling (spindled epithelial component) were excluded. A series of 31 FIGO grade 3 endometrioid carcinomas that were initially diagnosed as dedifferentiated endometrial carcinomas but subsequently revised to FIGO grade 3 endometrioid carcinomas upon histologic review were included for comparison. All of the endometrial carcinomas included in this study were from hysterectomy specimens. The cases were identified and obtained from the pathology archives at Vancouver General Hospital (Vancouver, Canada), Calgary Laboratory Services (Calgary, Canada), Royal Alexandra Hospital (Edmonton, Canada), The Ottawa Hospital (Ottawa, Canada) and Memorial Sloan Kettering Cancer Center (New York, United States). The study was approved by the Institutional Review Board.
DNA extraction
For each case, tissue cores (0.6 mm) of different histological components (endometrioid and undifferentiated) and the corresponding normal tissues were obtained from formalin fixed paraffin embedded (FFPE) blocks. The tumor cores were obtained from areas showing the most histologically viable tumor with the least amount of stromal tissue. To ensure that each tissue core contained only the histological component that it was supposed to represent, each individual tumor FFPE block was flipped over and re-embedded to produce a H&E slide from the opposite side of the block, and tissue cores that were contaminated by a different component were excluded from further analysis. Normal tissue (i.e. uterine cervix, fallopian tube and ovary) that was distant from and uninvolved by endometrial carcinoma was used for comparison. DNA was extracted from the tissue cores using the Qiagen FFPE DNA extraction kit based on the manufacturer's protocols.
Targeted gene panel sequencing analysis and validations
We performed sequencing analysis to detect mutations in 26 genes that have been previously found to be recurrently mutated in carcinomas of the gynecologic tract. These included the full coding regions of AKT1, ARID1A, FBXW7, FGFR2, JAK1, KRAS, MLH1, MSH2, MSH6, NRAS, PIK3CA, PIK3R1, PIK3R2, PMS2, POLE, PPP2R1A, PTEN, RNF43, RPL22, SMARCA4, STK11, SPOP, TP53, and in selected exons in FOXL2 (exon 1), CTNNB1 (exon 3) and BRAF (exon 15).9 The Illumina custom TruSeq amplicon panel was designed using Illumina's DesignStudio and included 1173 amplicons (175bp) that covers 98% of the exons and untranslated regions (UTR) of these 26 genes. Custom amplicon libraries were prepared starting with 250ng of FFPE DNA as per Ilumina's Custom TruSeq Library Preparation protocol. Before pooling, normalization was performed by quantifying individual libraries using the Qubit fluorometer, then pooled based on equal concentrations. Library pools were then quantitated for amplifiable libraries using the Kapa Biosystems FAST qPCR SYBR quantification kit based on manufacturer's protocols. Pooled TruSeq libraries were sequenced using the Illumina MiSeq using 300 cycle V2 kits. Analysis was performed using the MiSeq Reporter and somatic variant caller 3.2.3.0. Only non-synonymous mutations passing quality filter with at least 10% variant allele frequency were further evaluated. These mutations were manually checked in bam files using Integrated Genome Viewer. Selected mutations (such as those involving SMARCA4) were validated orthogonally by direct Sanger sequencing using primer sets that target the regions containing the mutations; comparisons were made to the corresponding genomic sequences from normal tissue to determine the somatic/germline status of these mutations.
Tissue microarray (TMA) construction
Two 0.6 mm cores from each histologic component (endometrioid and undifferentiated) of dedifferentiated endometrial carcinoma were arrayed and placed on a single tissue microarray.
Immunohistochemistry and interpretation
SMARCA4 (BRG1) immunohistochemical analysis was performed on representative whole tissue sections from the hysterectomy specimens, while SMARCB1 (INI1), MLH1, MSH2, MSH6 and PMS2 immunohistochemical analyses were initially performed on tissue microarrays, followed by subsequent whole section analysis in cases with abnormal or equivocal results. For mismatch repair proteins (MLH1, MSH2, MSH6 and PMS2), the primary antibodies used and the staining methods are the same as that reported previously.9, 10 The slides were incubated with MLH1 (DAKO clone ES05 1:100), MSH2 (NCL clone 25D12 prediluted), MSH6 (BD Bioscience 44/MSH6 1:2000), PMS2 (BD Bioscience A16-4 1:100) and processed using the Leica Bond Max platform (Leica Microsystems, Wetzlar, Germany) as per manufacturer's protocol with proprietary reagents. The detection system used was the Bond polymer refine. For SMARCA4 and SMARCB1, the slides were incubated with SMARCA4 (1:25, clone EPNCIR111A, ab110641, Abcam, Toronto, ON) and SMARCB1/BAF47/INI1 (1:50, 25/BAF47, 612110, BD Biosciences, Mississauga, ON) and processed using the Ventana Discovery XT, and the Ventana Benchmark XT and Benchmark Ultra automated systems (Ventana Medical Systems, Tucson, AZ, USA).
All whole sections and TMAs were scored by two pathologists (A.N.K. and C.H.L). The differentiated and undifferentiated components of all dedifferentiated carcinomas were scored separately. For SMARCA4 and SMARCB1, tumors were scored as SMARCA4/SMARCB1-intact if any tumor cell nuclei showed staining; tumors scored as positive usually showed diffuse, moderate to strong staining (Anthony J Path paper in press). Tumors were scored as SMARCA4/SMARCB1-deficient if tumor nuclei showed no staining in the presence of internal positive control (nuclear staining of the stromal fibroblasts, endothelial cells and inflammatory cells). For MLH1, MSH2, MSH6 and PMS2, staining was considered abnormal (MMR-deficient) when there was loss of nuclear expression by the tumor cells compared to internal positive control (nuclear staining of the stromal fibroblasts, endothelial cells and inflammatory cells).9
Results
Targeted sequencing identifies somatic inactivating SMARCA4 mutations in the undifferentiated component
We performed targeted next generation sequencing analysis on an index series of 8 dedifferentiated endometrial carcinomas, with both the endometrioid and undifferentiated components analyzed in 4 cases and only the undifferentiated component analyzed in the remaining 4 cases due to limited material in the available blocks. All 8 dedifferentiated endometrial carcinomas contained a mix of low-grade (FIGO grade 1 or 2) endometrioid carcinoma and undifferentiated carcinoma (Table 1 and Figure 1). The undifferentiated component displayed a sheet-like proliferation of monotonous oval to round cells in all 10 cases and constituted between 10-95 % of the overall tumor. The undifferentiated component all displayed prominent mitotic activity with tumor necrosis. Cellular discohesion was noted in all cases, and rhabdoid cytologic features were seen in 7 cases (Figure 1). Six of the 8 tumors were MMR-deficient, showing the same pattern of MMR deficiency in the corresponding endometrioid and undifferentiated components.
Table 1. Summary of the clinicopathologic and molecular features - index series of 8 dedifferentiated endometrial carcinomas.
| Case | Age | Histology | Stage | MMR IHC | Mutations in EC | Mutations in UC | SMARCA4 IHC | SMARCB1 IHC |
|---|---|---|---|---|---|---|---|---|
| 1 | 54 | 90% EC1, 10% UC | 1A | MMR-intact | MSH6 (A25S), PIK3R1 (K567E, R461X), PIK3R2 (R574Q), POLE (M1L, S459F), PTEN (R130L, S59X), SPOP (D140N) | EC: Intact, UC: intact | EC: Intact, UC: deficient | |
| 2 | 55 | 20% EC2, 80% UC | 3B | MLH1 and PMS2 loss | ARID1A (f.s. x 3, R1749K), CTNNB1 (S33A), FBXW7 (A423T), JAK1 (f.s.), PIK3CA (E545K), POLE (S2231N), PTEN (deletion, f.s.), RPL22 (f.s.) | ARID1A (f.s. x 3, R1749K), CTNNB1 (S33A), FBXW7 (A423T), JAK1 (f.s.), PIK3CA (E545K), POLE (S2231N), PTEN (deletion, f.s.), RPL22 (f.s.) | EC: Intact, UC: intact | EC: Intact, UC: intact |
| 3 | 70 | 10% EC1, 90% UC | 3C1 | PMS2 loss | ARID1A (f.s. x 2), FBXW7 (R399Q), KRAS (A146T), PIK3CA (E545A), POLE (R573L), PTEN (f.s.x 2, L139X), SMARCA4 (f.s. C1046R) | EC: Intact, UC: deficient | EC: Intact, UC: intact | |
| 4 | 73 | 10% EC1, 90% UC | 1A | MLH1 and PMS2 loss | ARID1A (W1498X), KRAS (G12A), PIK3CA (E545K, V344M), PTEN (K128N), SMARCA4 (f.s., Q756X), SPOP (E50K) | EC: Intact, UC: deficient | EC: Intact, UC: intact | |
| 5 | 66 | 70% EC1, 30% UC | 1B | PMS2 loss | ARID1A (f.s., N102S), CTNNB1 (T41A), JAK1 (f.s. x 2), MSH2 (f.s.), PIK3R1 (f.s.), PTEN (f.s.), RPL22 (f.s.), SMARCA4 (P327S) | ARID1A (f.s.), JAK1 (f.s. x 2), KRAS (G12D), MSH2 (f.s.), PTEN (f.s.), RPL22 (f.s.), SMARCA4 (f.s.x 2, R1203C) | EC: Intact, UC: deficient | EC: Intact, UC: intact |
| 6 | 73 | 30% EC1, 70% UC | 1B | MLH1 and PMS2 loss | FBXW7 (deletion), HRAS (R68W), JAK1 (f.s., Y412X), PIK3CA (N575K, H1047L), PTEN (Y68X, f.s.), PPP2R1A (R418Q) | FBXW7 (R49P), JAK1 (f.s., Y412X), PIK3CA (N575K, H1047L), PTEN (Y68X, f.s.), PPP2R1A (R418Q) | EC: Intact, UC: intact | EC: Intact, UC: intact |
| 7 | 51 | 60% EC1, 40% UC | 3C2 | MLH1 and PMS2 loss | ARID1A (f.s.), JAK1 (f.s.), KRAS (G12V), PIK3R1 (deletion), PTEN (f.s.), RNF43 (f.s.), RPL22 (f.s.) | ARID1A (f.s.), JAK1 (f.s.), KRAS (G12V), PIK3R1 (deletion), POLE (R1284Q), PTEN (f.s.), RNF43 (f.s.), RPL22 (f.s.), SMARCA4 (f.s.), TP53 (R26C) | EC: Intact, UC: deficient | EC: Intact, UC: intact |
| 8 | 46 | 5% EC2, 95% UC | 1A | MMR-intact | ARID1A (Q1172X), FGFR2 (E413D), MSH2 (E580X, K918N), PIK3CA (R93W, T1025A), PIK3R1 (E217K), PMS2 (R563X, E172A), POLE (V411L), PTEN (E299X), SPOP (K101T), SMARCA4 (R549C) | EC: Intact, UC: intact | EC: Intact, UC: deficient |
Stage: based on 2009 FIGO staging; MMR: mismatch repair protein; EC: endometrioid carcinoma; UC: undifferentiated carcinoma; f.s.: frameshift mutation.
Figure 1. Representative images of dedifferentiated endometrial carcinomas.
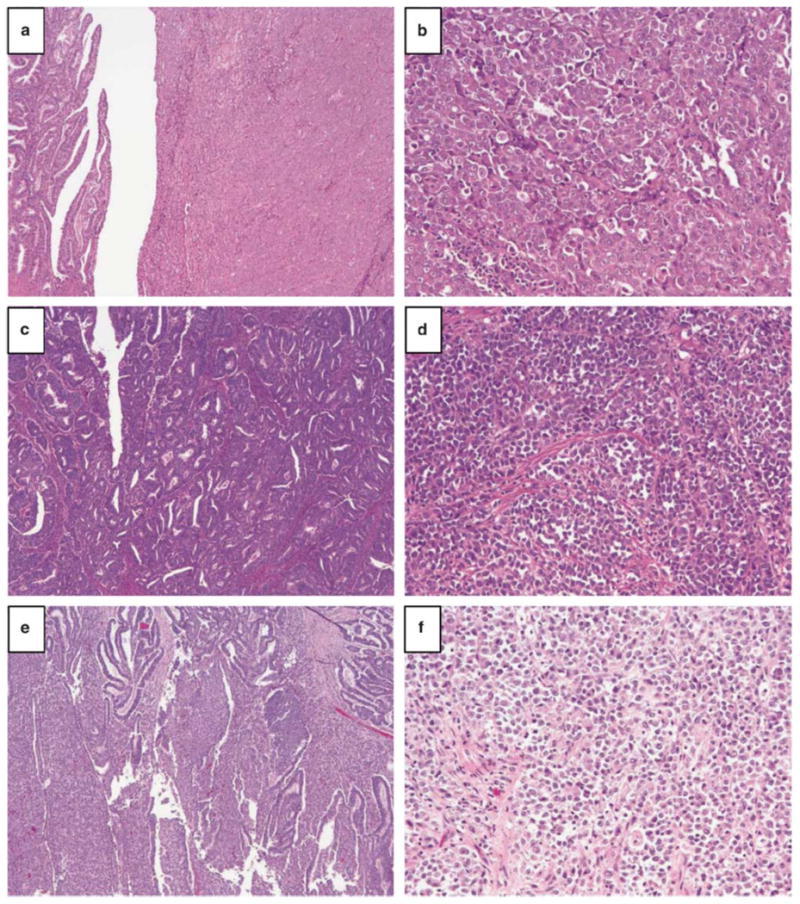
A-B) case 3 showing both the FIGO grade 1 endometrioid and the undifferentiated component in A with a higher magnification of the undifferentiated component in B. C-D) case 5 showing the FIGO grade 1 endometrioid component in C and the undifferentiated component in D. E-F) case 7 showing both the FIGO grade 1 endometrioid and the undifferentiated component in E with a higher magnification of the undifferentiated component in F.
The mutation profiles of the undifferentiated component in this index series are shown in Table 1. We identified recurrent mutations involving PTEN (8/8), ARID1A (6/8), PIK3CA (5/8), SMARCA4 (5/8, with frameshift/nonsense mutations in 4 cases and a missense mutation in 1 case), JAK1 (4/8), KRAS (4/8), PIK3R1 (4/8), POLE (4/8, only 1 involving exonuclease domain), RPL22 (3/8), FBXW7 (3/8), SPOP (3/8) and CTNNB1 (2/8). In the 4 cases where the endometrioid and the undifferentiated components were both analyzed, 67% of the mutations identified were shared between the two histologic components. One of the two MMR-intact tumors harbored a V411L POLE exonuclease domain mutation. While the overall mutation profiles are in keeping with the endometrioid histotype 11, the findings of frequent frameshift and/or nonsense SMARCA4 mutations solely in the undifferentiated component warranted further investigation. Four tumors (case 3, 4, 5 and 7) harbored inactivating SMARCA4 mutations (frameshift and/or nonsense) and all 4 tumors were MMR-deficient. Subsequent Sanger sequencing confirmed the somatic nature of these frameshift/nonsense SMARCA4 mutations.
Immunohistochemical analysis of SMARCA4 (BRG1) and SMARCB1 (INI1)
Based on the mutation findings, we examined the expression of SMARCA4 (BRG1) as well as another member of SWI/SNF complex SMARCB1 (INI1) by immunohistochemistry in the index series. All four MMR-deficient tumors harboring inactivating SMARCA4 mutations showed a complete loss of SMARCA4 expression in the undifferentiated component but intact SMARCA4 expression in the corresponding endometrioid component (Figure 2). SMARCB1 expression was intact in these 4 SMARCA4-deficient tumors. The 3 tumors (case 1, 2 and 6) with wild-type SMARCA4 and the POLE (V411L)-mutated tumor (case 8) with a missense mutation (R549C) in SMARCA4 mutation all showed intact SMARCA4 expression in both the endometrioid and the undifferentiated components. Two of these SMARCA4-intact tumors (case 1 and 8) showed a complete loss of SMARCB1 expression in the undifferentiated component but intact SMARCB1 expression in the corresponding endometrioid component (Figure 3) while 2 SMARCA4-intact tumors showed intact SMARCB1 expression throughout the tumor (Figure 4).
Figure 2. SMARCA4 (BRG1) and SMARCB1 (INI1) immunostaining in SMARCA4-deficient dedifferentiated endometrial carcinomas.
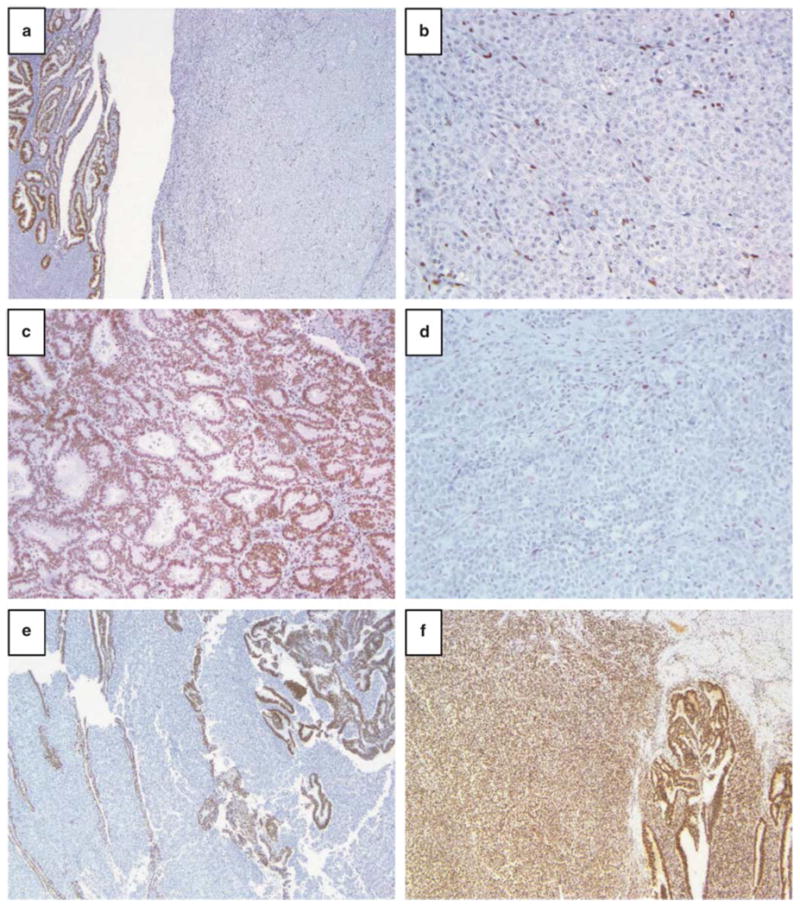
A-B) case 3 showing a complete loss of SMARCA4 nuclear staining in the undifferentiated component (with internal stromal positive control) and intact SMARCA4 nuclear staining in the differentiated endometrioid component. C-D) case 3 showing a complete loss of SMARCA4 nuclear staining in the undifferentiated component (with internal stromal positive control) and intact SMARCA4 nuclear staining in the differentiated endometrioid component. E) case 7 showing a complete loss of SMARCA4 nuclear staining in the undifferentiated component and intact SMARCA4 nuclear staining in the differentiated endometrioid component. F) case 7 showing intact SMARCB1 nuclear staining in both the differentiated endometrioid component and the undifferentiated component.
Figure 3. SMARCB1 (INI1) immunostaining in SMARCB1-deficient dedifferentiated endometrial carcinomas.
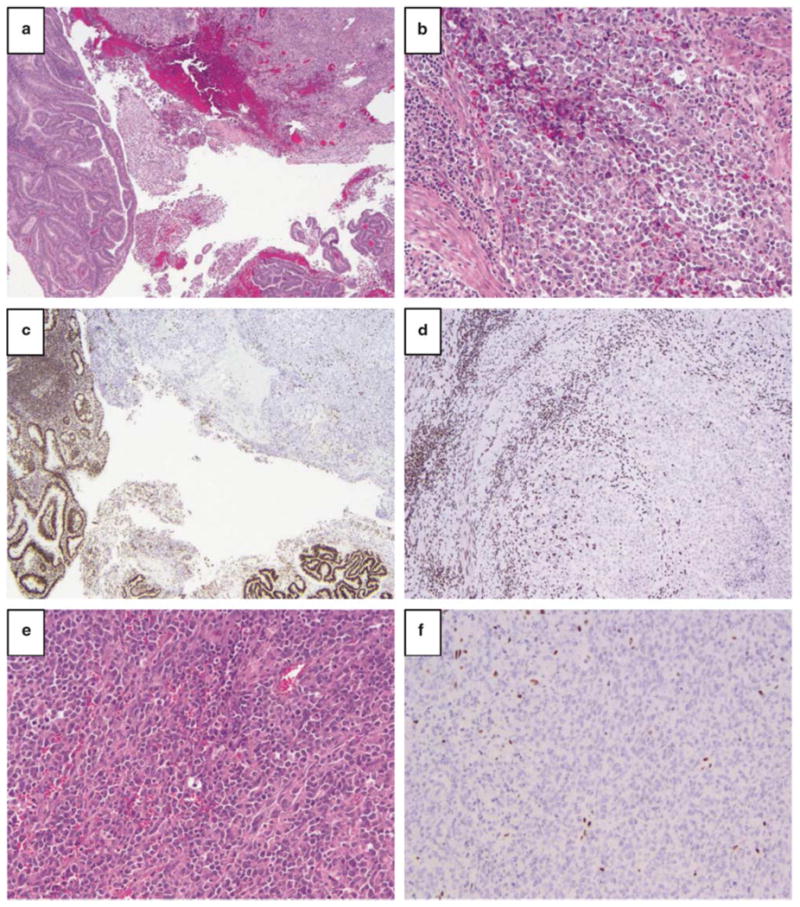
A-B) case 1 showing FIGO grade 1 endometrioid component and undifferentiated component in A with a higher magnification of the undifferentiated component in B. C-D) case 1 showing a complete loss of SMARCB1 nuclear staining in the undifferentiated component (with internal stromal positive control) and intact SMARCB1 nuclear staining in the differentiated endometrioid component. E-F) case 8 showing SMARCB1-deficient undifferentiated component.
Figure 4. SMARCA4 and SMARCB1-intact dedifferentiated endometrial carcinoma.
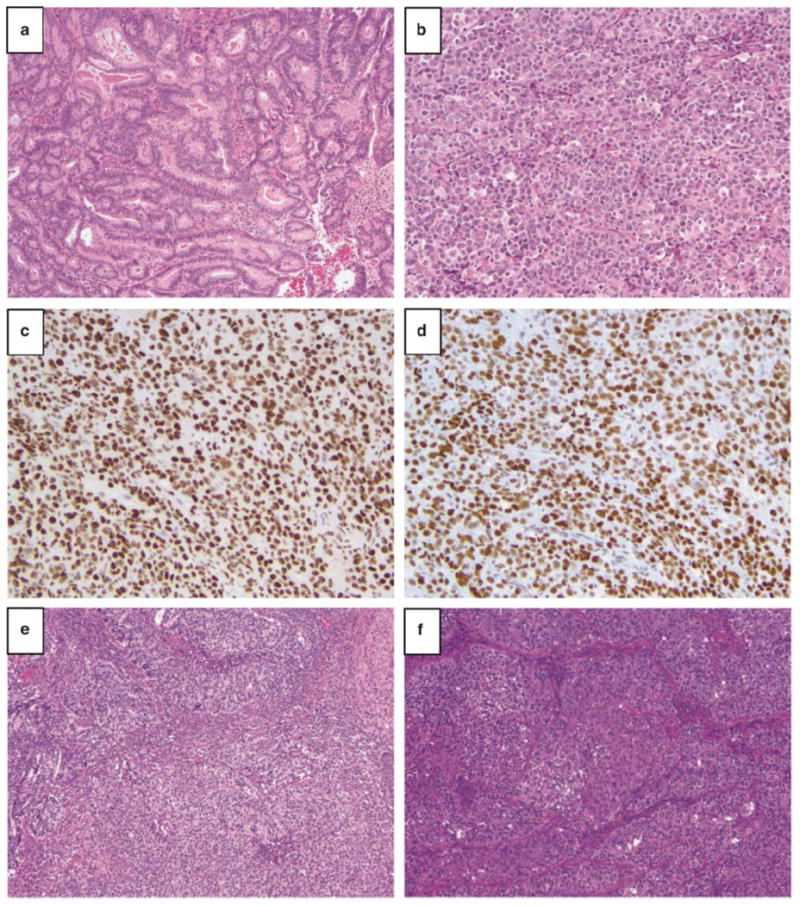
Case 2 showing the low-grade endometrioid component (A) and undifferentiated component (B), with intact SMARCA4 (C) and SMARCB1 (D) expression.
To further validate these results and determine the frequency of SMARCA4/SMARCB1 loss in dedifferentiated endometrial carcinoma, we surveyed their expression in an additional series of 22 centrally reviewed dedifferentiated endometrial carcinomas. The undifferentiated component constituted on average 60% of the overall tumor (ranging from 5 to 95%). 70% of the tumors were MMR-deficient, with the corresponding endometrioid and undifferentiated components in these MMR-deficient tumors showing the same pattern of MMR protein loss. We also included a series of 32 FIGO grade 3 endometrioid carcinomas for comparison; these 32 cases were all initially diagnosed as dedifferentiated endometrial carcinomas but were reassigned to FIGO grade 3 endometrioid carcinomas upon centralized review. The reason for the histologic reassignment was the presence of focal glandular differentiation and/or the presence of well demarcated cohesive lobules - features that are inconsistent with the diagnosis of dedifferentiated endometrial carcinoma. In comparison, 63% (19 of 30 cases with interpretable results) of the tumors reclassified as FIGO grade 3 endometrioid carcinomas were MMR-deficient.
In the validation cohort, 7 of the 22 dedifferentiated carcinomas showed a complete loss of SMARCA4 in the undifferentiated component while the corresponding endometrioid component showed intact expression. SMARCB1 expression was intact in these SMARCA4-deficient tumors. Of the remaining 13 SMARCA4-intact tumors, 2 showed a complete loss of INI1 in the undifferentiated component and intact INI1 expression in the corresponding endometrioid component. These findings confirm the frequent loss of SMARCA4/SMARCB1 in the undifferentiated component of dedifferentiated endometrial carcinomas. In comparison, none of the 31 FIGO grade 3 endometrioid carcinomas examined showed SMARCA4 and/or SMARCB1 loss.
Clinicopathologic of SMARCA4/SMARCB1-deficient dedifferentiated endometrial carcinomas
Combining our findings in the index series and the validation series (Table 2), SMARCA4 deficiency in the undifferentiated component was present in 11/30 dedifferentiated carcinomas (37%) and SMARCB1 deficiency in 4/30 (13%). The loss of SMARCA4 or SMARCB1 was mutually exclusive, so loss of either protein was observed in 15/30 (50%) dedifferentiated carcinomas. Eight of eleven (73%) SMARCA4-deficient tumors were MMR-deficient, while 2 of 4 (50%) SMARCB1-deficient tumors and 11 of 15 (73%) of SMARCA4/SMARCB1-intact tumors were MMR-deficient. Histologically, the undifferentiated component of SMARCA4/SMARCB1-deficient DDEC was the predominant component in 67% of the cases (ranging from 5 to 95%). The differentiated component in all 15 SMARCA4/SMARCB1-deficient DDEC exhibited typical FIGO grade 1 or 2 endometrioid morphology. The undifferentiated components all showed sheet-like proliferation of monomorphic round to polygonal shaped cells with a vascular stroma (fine capillary network). There were patchy foci (readily identified by low power examination) of cellular discohesion and focal rhabdoid cytologic features in all cases. Tumor necrosis was present in all cases. Mitotic activity was high in the undifferentiated component, with an average mitotic rate of 49 MF/10 HPF (1.5 mm2) that ranged from 35 to 65 MF/10 HPF.
Table 2. Summary of SMARCA4, SMARCB1 and MMR protein immunohistochemistry findings in the entire study cohort.
| SMARCA4/SMARCB1 status | Frequency of MMR-deficiency | |
|---|---|---|
| Dedifferentiated endometrial carcinoma (n=30) | 21 (70%) | |
|
| ||
| SMARCA4-deficient*/SMARCB1-intact | 11 (37%) | 8 (73%) |
| SMARCA4-intact/SMARCB1-deficient* | 4 (13%) | 2 (50%) |
| SMARCA4-intact/SMARCB1-intact | 15 (50%) | 11 (73%) |
|
| ||
| FIGO grade 3 endometrioid carcinoma (n=31) | 19 (63%)** | |
|
| ||
| SMARCA4-deficient*/SMARCB1-intact | 0 (0%) | |
| SMARCA4-intact/SMARCB1-deficient* | 0 (0%) | |
| SMARCA4-intact/SMARCB1-intact | 31 (100%) | 19 (63%)** |
loss of SMARCA4 or SMARCB1 in only the undifferentiated component with intact expression in the corresponding endometrioid component;
out of 30 cases with interpretable MMR staining results
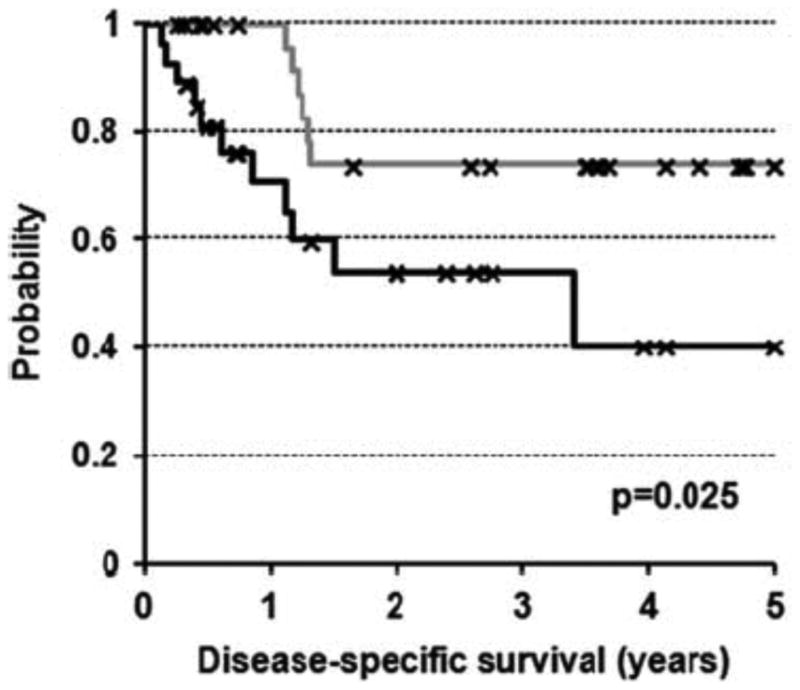
Clinically, the average age at the time of disease diagnosis is 61 years (ranging from 46 to 75 years) for patients with SMARCA4/SMARCB1-deficient dedifferentiated carcinoma, 62 years (ranging from 39 to 93 years) for patients with SMARCA4/SMARCB1-intact dedifferentiated carcinoma and 61 years (ranging from 34 to 86 years) for patients with grade 3 endometrioid carcinomas. In terms of FIGO stage, 47% of the patients with SMARCA4/SMARCB1-deficient dedifferentiated carcinoma had stage 2-4 disease, compared to 33% of the patients with SMARCA4/SMARCB1-intact dedifferentiated carcinoma and 23% of patients with grade 3 endometrioid carcinoma. In terms of adjuvant treatment, 70% of the patients with dedifferentiated carcinoma received adjuvant therapy (radiation therapy and/or chemotherapy) while 22% of the patients declined adjuvant therapy, compared to 83% of the patients with grade 3 endometrioid carcinoma that received and 7% that declined adjuvant therapy. With respect to patient outcome, dedifferentiated carcinoma as a group had a worse disease-specific survival compared to FIGO grade 3 endometrioid carcinoma (p=0.025) (Figure 5). There was no significant difference with respect to disease-specific survival between SMARCA4/SMARCB1-deficient dedifferentiated carcinomas and SMARCA4/SMARCB1-intact dedifferentiated carcinomas (p=0.92) based on Kaplan-Meier survival analysis (data not shown).
Figure 5. Kaplan-Meier survival analysis showing decreased disease-specific survival in review-confirmed dedifferentiated endometrial carcinomas (n=30) compared to FIGO grade 3 endometrioid carcinomas (n=31) that were initially diagnosed as dedifferentiated carcinoma.
Discussion
Dedifferentiated endometrial carcinoma is a morphologically distinct subtype of endometrial carcinoma. As demonstrated by previous and present findings,4, 5 the undifferentiated component shares the same molecular aberrations as the corresponding endometrioid component. In contrast to the differentiated endometrioid component that displays clear evidence of epithelial differentiation (in the form of glandular or villoglandular structures), the undifferentiated component lacks any histologic evidence of glandular/villoglandular differentiation. This corresponds to the absence or markedly reduced expression of epithelial markers (i.e. cytokeratins and epithelial membrane antigen) in the undifferentiated component compared to the endometrioid component.2
In this study, we identified through targeted sequencing and subsequent immunohistochemical validation that the loss of SMARCA4 or SMARCB1 expression is associated with histologic dedifferentiation in half of dedifferentiated endometrial carcinomas. The findings of SMARCA4 inactivating mutations (frameshift and/or nonsense) in the undifferentiated component but not in the differentiated endometrioid component further support the hypothesis that undifferentiated component represents a distinct form of tumor progression from the pre-existing low-grade endometrioid carcinoma. Our immunohistochemical findings corroborate the recent reports by Strehl et al and Stewart et al that demonstrated the loss of SMARCA4/SMARCB1 expression in the undifferentiated component of a subset of dedifferentiated endometrial carcinoma.12, 13 Strehl et al described a single case of SMARCA4-deficient dedifferentiated endometrial carcinoma composed of endometrioid component and an undifferentiated component with prominent rhabdoid cytologic features.13 This case showed loss of SMARCA4 expression by immunohistochemistry in the undifferentiated component with intact SMARCA4 expression in the endometrioid component. SMARCB1 and MMR protein expression were intact in both components in this case. Strehl et al also surveyed the expression of SMARCA4 and SMARCB1 in 24 FIGO grade 3 endometrioid carcinomas and identified no loss of expression in these tumors, similar to our findings here. Stewart and Crook examined the expression of SMARCA4, SMARCB1 and MMR proteins in 17 dedifferentiated endometrial carcinomas.12 They observed a loss of SMARCA4 that is limited only to the undifferentiated component in 3 of 17 (18%) tumors and a loss of SMARCB1 in both the endometrioid and undifferentiated components in 1 of 17 (6%) tumors. In the present study, we observed a higher frequency of SMARCA4 loss at 37% and SMARCB1 loss at 13% in our cohort. Even though there is a difference in the sample size between the two studies, we speculate that our histologic inclusion criteria that are based on the original description may account for at least some of the differences here. We closely adhered to the original histological description in our centralized histologic review, in which we reclassified about half of the cases originally diagnosed as dedifferentiated endometrial carcinomas to FIGO grade 3 endometrioid carcinomas. For instance, we did not include tumors that displayed spindled epithelial component or cohesive solid architecture in the undifferentiated component. The importance of this centralized review is further underscored by our findings that review-confirmed dedifferentiated endometrial carcinomas showed worse disease specific survival than tumors reclassified FIGO grade 3 endometrioid carcinomas. This raises an important diagnostic issue with regards to the subjectivity in the diagnosis of dedifferentiated endometrial carcinoma and the need for more objective criteria through better molecular understanding. While SMARCA4 or SMARCB1 deficiency as demonstrated by immunohistochemistry may help to confirm the diagnosis of dedifferentiated endometrial carcinoma in the appropriate histologic context, intact expression of SMARCA4 and SMARCB1 does not exclude the possibility of dedifferentiated endometrial carcinoma. Furthermore, it is important to note that an abnormal MMR immunostaining result does not necessarily support the diagnosis of dedifferentiated endometrial carcinomas, as we observed frequent (63%) MMR deficiency in FIGO grade 3 endometrioid carcinomas that were initially diagnosed as dedifferentiated endometrial carcinomas, slightly higher than the 45% recently reported for typical FIGO grade 3 endometrioid carcinomas.14
SMARCA4 and SMARCB1 are both components of an evolutionarily conserved multi-subunit SWI/SNF chromatin remodeling complex. SWI/SNF complex plays an important role in several cellular processes such as transcription, cell differentiation and DNA repair. Mutations in the SWI/SNF chromatin remodeling complex have been reported in up to 20% of human cancers,15, 16 including several rare tumor types such as rhabdoid tumors of the brain, kidney and extrarenal sites,17 epithelioid sarcoma,18, 19 small cell carcinoma of the ovary - hypercalcemic type,20-23 (Karnezis et al, Orphanet Rare Diseases 2015.in press) as well as a subset of pancreatic undifferentiated carcinoma and a subset of poorly-differentiated carcinomas of the sinonasal tract. 24, 25 The function of the SWI/SNF complex in transcriptional regulation suggests that the principle mechanism of oncogenesis upon mutation of its components is epigenetic dysregulation. The common pathological features among several tumours lacking either SMARCA4 or SMARCB1 – sheet-like growth of undifferentiated, highly proliferative cells with cytology ranging from small round cell to rhabdoid – suggest that the principal defect involves the failure to activate genes that promote terminal differentiation and cell-cell adhesion. Consistent with this hypothesis, the undifferentiated component of dedifferentiated endometrial carcinoma show absent or reduced expression of markers that are present in the well differentiated areas.2, 5, 12, 13 Similarly, renal cell carcinoma with rhabdoid morphology, a tumor that also shows dual SWI/SNF protein deficiency (SMARCA4/BRG1 and SMARCB1/INI1) has also been proposed to be a dedifferentiated tumor.26 In lung cancer, loss of SMARCA4 and the related SMARCA2 protein is associated with poorly differentiated morphology (solid-predominant), reduced bronchial epithelial immunophenotype and more aggressive disease behavior.27, 28 It therefore appears that deficiency in core members of the SWI/SNF complex (i.e. SMARCA4 or SMARCB1) predisposes to cellular dedifferentiation (in either a susceptible normal cell or a pre-existing low-grade tumor cell) into an aggressive, monomorphic, high-grade tumor with undifferentiated morphology. Therapeutically, the loss of these core SWI/SNF components such as SMARCA4 and SMARCB1 in dedifferentiated endometrial carcinoma may predict their response to classes of drugs that regulate epigenetic modifications.29, 30
We observed a high frequency of MMR deficiency in our present series of dedifferentiated endometrial carcinomas, including cases showing SMARCA4 deficiency. It therefore appears that a hypermutating molecular context predisposes to molecular event(s) such as SMARCA4 inactivation that induce dedifferentiation. We also identified in our index series a case of dedifferentiated endometrial carcinoma that harbored a hotspot POLE exonuclease domain mutation. This POLE-mutated tumor showed intact MMR protein expression and a loss of SMARCB1 in the undifferentiated component of the tumor. Given that the great majority of POLE exonuclease domain mutated endometrial carcinomas are associated with a favorable clinical course,11, 31, 32 it is unclear whether the apparent histologic progression that is accompanied by the loss of a SWI/SNF component would confer more aggressive biology and clinical behavior or whether the ultramutated POLE exonuclease domain mutated molecular context dominates.
In summary, we found that SMARCA4 inactivating mutation with the consequent loss of SMARCA4 and the loss of SMARCAB1 are associated with histologic dedifferentiation in half of dedifferentiated endometrial carcinoma. These findings implicate the inactivation of SMARCA4 or SMARCB1 as a potential oncogenic mechanism for the development of undifferentiated carcinoma from an underlying low-grade endometrioid carcinoma. Further studies are needed to determine the effects of SMARCA4/SMARCB1 inactivation in the context of endometrioid carcinoma and the potential for targeting SWI/SNF deficiency in patients with dedifferentiated endometrial carcinoma.
Acknowledgments
Sources of support/funding: This study is supported by a research funds from Royal Alexandra Hospital foundation, Calgary Laboratory Services Internal Research Competition (RS10-536) and Alberta Cancer Foundation.
Footnotes
Disclosure/conflict of interest: The authors declare no conflicts of interest.
References
- 1.Silva EG, Deavers MT, Bodurka DC, et al. Association of low-grade endometrioid carcinoma of the uterus and ovary with undifferentiated carcinoma: a new type of dedifferentiated carcinoma? Int J Gynecol Pathol. 2006;25:52–58. doi: 10.1097/01.pgp.0000183048.22588.18. [DOI] [PubMed] [Google Scholar]
- 2.Silva EG, Deavers MT, Malpica A. Undifferentiated carcinoma of the endometrium: a review. Pathology. 2007;39:134–138. doi: 10.1080/00313020601159494. [DOI] [PubMed] [Google Scholar]
- 3.Giordano G, D'Adda T, Bottarelli L, et al. Two cases of low-grade endometriod carcinoma associated with undifferentiated carcinoma of the uterus (dedifferentiated carcinoma): a molecular study. Pathol Oncol Res. 2012;18:523–528. doi: 10.1007/s12253-011-9386-7. [DOI] [PubMed] [Google Scholar]
- 4.Kuhn E, Ayhan A, Bahadirli-Talbott A, et al. Molecular characterization of undifferentiated carcinoma associated with endometrioid carcinoma. Am J Surg Pathol. 2014;38:660–665. doi: 10.1097/PAS.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 5.Tafe LJ, Garg K, Chew I, et al. Endometrial and ovarian carcinomas with undifferentiated components: clinically aggressive and frequently underrecognized neoplasms. Mod Pathol. 2010;23:781–789. doi: 10.1038/modpathol.2010.41. [DOI] [PubMed] [Google Scholar]
- 6.Vita G, Borgia L, Di Giovannantonio L, et al. Dedifferentiated endometrioid adenocarcinoma of the uterus: a clinicopathologic study of a case. Int J Surg Pathol. 2011;19:649–652. doi: 10.1177/1066896911405987. [DOI] [PubMed] [Google Scholar]
- 7.Garg K, Leitao MM, Jr, Kauff ND, et al. Selection of endometrial carcinomas for DNA mismatch repair protein immunohistochemistry using patient age and tumor morphology enhances detection of mismatch repair abnormalities. Am J Surg Pathol. 2009;33:925–933. doi: 10.1097/PAS.0b013e318197a046. [DOI] [PubMed] [Google Scholar]
- 8.Garg K, Shih K, Barakat R, et al. Endometrial carcinomas in women aged 40 years and younger: tumors associated with loss of DNA mismatch repair proteins comprise a distinct clinicopathologic subset. Am J Surg Pathol. 2009;33:1869–1877. doi: 10.1097/PAS.0b013e3181bc9866. [DOI] [PubMed] [Google Scholar]
- 9.Hoang LN, McConechy MK, Meng B, et al. Targeted mutation analysis of endometrial clear cell carcinoma. Histopathology. 2015;66:664–674. doi: 10.1111/his.12581. [DOI] [PubMed] [Google Scholar]
- 10.Hoang LN, Han G, McConechy M, et al. Immunohistochemical characterization of prototypical endometrial clear cell carcinoma--diagnostic utility of HNF-1beta and oestrogen receptor. Histopathology. 2014;64:585–596. doi: 10.1111/his.12286. [DOI] [PubMed] [Google Scholar]
- 11.Kandoth C, Schultz N, Cherniack AD, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67–73. doi: 10.1038/nature12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stewart CJ, Crook ML. SWI/SNF complex deficiency and mismatch repair protein expression in undifferentiated and dedifferentiated endometrial carcinoma. Pathology. 2015;47:439–445. doi: 10.1097/PAT.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 13.Strehl JD, Wachter DL, Fiedler J, et al. Pattern of SMARCB1 (INI1) and SMARCA4 (BRG1) in poorly differentiated endometrioid adenocarcinoma of the uterus: analysis of a series with emphasis on a novel SMARCA4-deficient dedifferentiated rhabdoid variant. Ann Diagn Pathol. 2015;19:198–202. doi: 10.1016/j.anndiagpath.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Nelson GS, Pink A, Lee S, et al. MMR deficiency is common in high-grade endometrioid carcinomas and is associated with an unfavorable outcome. Gynecol Oncol. 2013;131:309–314. doi: 10.1016/j.ygyno.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Kadoch C, Hargreaves DC, Hodges C, et al. Proteomic and bioinformatic analysis of mammalian SWI/SNF complexes identifies extensive roles in human malignancy. Nat Genet. 2013;45:592–601. doi: 10.1038/ng.2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masliah-Planchon J, Bieche I, Guinebretiere JM, et al. SWI/SNF chromatin remodeling and human malignancies. Annu Rev Pathol. 2015;10:145–171. doi: 10.1146/annurev-pathol-012414-040445. [DOI] [PubMed] [Google Scholar]
- 17.Agaimy A. The expanding family of SMARCB1(INI1)-deficient neoplasia: implications of phenotypic, biological, and molecular heterogeneity. Adv Anat Pathol. 2014;21:394–410. doi: 10.1097/PAP.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 18.Hornick JL, Dal Cin P, Fletcher CD. Loss of INI1 expression is characteristic of both conventional and proximal-type epithelioid sarcoma. Am J Surg Pathol. 2009;33:542–550. doi: 10.1097/PAS.0b013e3181882c54. [DOI] [PubMed] [Google Scholar]
- 19.Modena P, Lualdi E, Facchinetti F, et al. SMARCB1/INI1 tumor suppressor gene is frequently inactivated in epithelioid sarcomas. Cancer Res. 2005;65:4012–4019. doi: 10.1158/0008-5472.CAN-04-3050. [DOI] [PubMed] [Google Scholar]
- 20.Foulkes WD, Clarke BA, Hasselblatt M, et al. No small surprise - small cell carcinoma of the ovary, hypercalcaemic type, is a malignant rhabdoid tumour. J Pathol. 2014;233:209–214. doi: 10.1002/path.4362. [DOI] [PubMed] [Google Scholar]
- 21.Jelinic P, Mueller JJ, Olvera N, et al. Recurrent SMARCA4 mutations in small cell carcinoma of the ovary. Nat Genet. 2014;46:424–426. doi: 10.1038/ng.2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ramos P, Karnezis AN, Craig DW, et al. Small cell carcinoma of the ovary, hypercalcemic type, displays frequent inactivating germline and somatic mutations in SMARCA4. Nat Genet. 2014;46:427–429. doi: 10.1038/ng.2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Witkowski L, Carrot-Zhang J, Albrecht S, et al. Germline and somatic SMARCA4 mutations characterize small cell carcinoma of the ovary, hypercalcemic type. Nat Genet. 2014;46:438–443. doi: 10.1038/ng.2931. [DOI] [PubMed] [Google Scholar]
- 24.Agaimy A, Haller F, Frohnauer J, et al. Pancreatic undifferentiated rhabdoid carcinoma: KRAS alterations and SMARCB1 expression status define two subtypes. Mod Pathol. 2015;28:248–260. doi: 10.1038/modpathol.2014.100. [DOI] [PubMed] [Google Scholar]
- 25.Bishop JA, Antonescu CR, Westra WH. SMARCB1 (INI-1)-deficient carcinomas of the sinonasal tract. Am J Surg Pathol. 2014;38:1282–1289. doi: 10.1097/PAS.0000000000000285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rao Q, Xia QY, Shen Q, et al. Coexistent loss of INI1 and BRG1 expression in a rhabdoid renal cell carcinoma (RCC): implications for a possible role of SWI/SNF complex in the pathogenesis of RCC. Int J Clin Exp Pathol. 2014;7:1782–1787. [PMC free article] [PubMed] [Google Scholar]
- 27.Matsubara D, Kishaba Y, Ishikawa S, et al. Lung cancer with loss of BRG1/BRM, shows epithelial mesenchymal transition phenotype and distinct histologic and genetic features. Cancer Sci. 2013;104:266–273. doi: 10.1111/cas.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Orvis T, Hepperla A, Walter V, et al. BRG1/SMARCA4 inactivation promotes non-small cell lung cancer aggressiveness by altering chromatin organization. Cancer Res. 2014;74:6486–6498. doi: 10.1158/0008-5472.CAN-14-0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fillmore CM, Xu C, Desai PT, et al. EZH2 inhibition sensitizes BRG1 and EGFR mutant lung tumours to TopoII inhibitors. Nature. 2015;520:239–242. doi: 10.1038/nature14122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oike T, Ogiwara H, Tominaga Y, et al. A synthetic lethality-based strategy to treat cancers harboring a genetic deficiency in the chromatin remodeling factor BRG1. Cancer Res. 2013;73:5508–5518. doi: 10.1158/0008-5472.CAN-12-4593. [DOI] [PubMed] [Google Scholar]
- 31.Church DN, Stelloo E, Nout RA, et al. Prognostic significance of POLE proofreading mutations in endometrial cancer. J Natl Cancer Inst. 2014;107:402. doi: 10.1093/jnci/dju402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meng B, Hoang LN, McIntyre JB, et al. POLE exonuclease domain mutation predicts long progression-free survival in grade 3 endometrioid carcinoma of the endometrium. Gynecol Oncol. 2014;134:15–19. doi: 10.1016/j.ygyno.2014.05.006. [DOI] [PubMed] [Google Scholar]


