Abstract
Background:
Despite significant advances in pharmacological and psychological therapies for bipolar disorder, many people continue to have less than optimal outcomes, which are associated with significant disability and poor quality of life (QOL). This study aimed to assess the disability and QOL and factors associated with such suboptimal outcomes in subjects with bipolar disorder in remission.
Methods:
Consecutive patients diagnosed to have bipolar disorder in remission attending the Department of Psychiatry, MOSC Medical College, Kerala, India were recruited for the study. They were assessed using the International Classification of Diseases Diagnostic Criteria for Research-10, Hamilton Scale for Depression, Young's Mania Rating Scale, World Health Organization-QOL (WHO QOL-BREF), WHO-Disability Assessment Scale (WHO-DAS), and Kuppuswamy's scale for socioeconomic status assessment.
Results:
Eighty-four patients were evaluated. The mean total WHO-DAS score was 19.2 ± 2.09, the maximum disability in domain 4 (getting along) followed by domain 2 (mobility). The mean total WHO-QOL BREF score was 54.26 ± 2.85, the lowest subscore in domain 3 (social interactions). Disability scores were significantly associated with increasing age, female gender, not being an earning member of the family, and lower QOL scores. Poorer QOL scores were significantly associated with increasing age and higher disability score.
Conclusions:
Many bipolar patients in remission have significant disability and poorer QOL. There is a need for longitudinal studies to explore such associations and develop interventions to reduce the disability thereby enhancing the QOL.
Key words: Bipolar disorder, disability, quality of life
INTRODUCTION
Bipolar disorder (bipolar affective disorder [BPAD]) is one of the most complex psychiatric conditions characterized by recurrent mood episodes and longitudinally varied course. It affects at least 1% of the population[1] and according to the World Health Organization (WHO), BPAD is the sixth leading cause of disability among illnesses worldwide.[2] The traditionally accepted clinical conception of the course of BPAD is that it is marked by time-limited acute episodes of mania and major depression, with occasional hypomanic and mixed episodes, with recovery back to euthymia. The classical concept also suggests favorable functional adaptation between episodes, with a marked decrease in acute morbidity with effective mood-stabilizing treatments.[3] However, a number of recent studies have indicated that several patients with BPAD, who no longer met the syndromal or symptomatic criteria following recovery from an acute affective episode, nevertheless continue to display functional impairment.[4]
Quality of life (QOL) and mental health have a mutual correlation in the sense that QOL is a direct consequence of mental health. A study done by Xiang et al.[5] in 2010 concluded that social functioning is the main predictor of QOL in psychiatric patients. Several QOL studies on bipolar patients revealed that they experience lower functioning and well-being even in the euthymic phase of the disorder.[6,7,8,9,10]
Functional impairment in vocational and social adjustment is commonly encountered among patients diagnosed with BPAD. The link between BPAD and the important outcome measure of social disability is under-researched in India.[11]
This study attempted to assess the level of disability and QOL in outpatients with BPAD in remission and to identify the sociodemographic, clinical, illness, and treatment-related characteristics associated with poor outcome.
METHODS
Consecutive patients, who satisfied the inclusion criteria, and attending the Psychiatry Outpatient Department at MOSC Medical College, Kolenchery, between August 2014 and August 2015 were contacted for participation.
Inclusion criteria
Patients between 20 and 60 years belonging to either sex who agreed to give an informed consent, with a diagnosis of BPAD – currently in remission as per The International Classification of Diseases – Diagnostic Criteria for Research (ICD-10 DCR) were recruited. To ensure remission, they required scores of <8 and <12 on the Hamilton Depression Rating Scale (HAM-D) and the Young's Mania Rating Scale (YMRS), respectively. Also, episodes of mood disturbance should not be present over the past 2 months.
Exclusion criteria
Organic mood (affective) disorders, seizure disorder, mental retardation, persistent neurological deficits, and other chronic debilitating medical illnesses such as chronic obstructive pulmonary disease, coronary artery disease, valvular heart disease, chronic liver disease, chronic kidney disease, and arthritis were exclusion criteria. The presence of any other psychiatric comorbidity or psychoactive substance use other than nicotine, amounting to harmful use/dependence was also considered exclusion criteria.
Assessment
The following rating scales were used.
The International Classification of Diseases-10 Diagnostic Criteria for Research,[12] derived from Chapter V (F) of ICD-10 was used to diagnose BPAD. The criteria being deliberately restrictive were intended to maximize homogeneity of study groups and comparability of findings in various studies.
The Hamilton Rating Scale for Depression-21 item[13] developed by Max Hamilton in 1960, is the most widely used assessment scale for depression. The strengths include its excellent validation/ research base and ease of administration. Total scores range from 0 to 53 (the sum of the first 17 items).
Young's Mania Rating Scale (YMRS)[14] is a clinician-rated scale to assess the severity of manic symptoms. Information for assigning scores is gained from subjectively reported symptoms over the past 48 hours and observation during the interview. YMRS is appropriate for assessing baseline severity and response to treatment. Total score is 60 and a score of ≤12 indicates remission of symptoms.
World Health Organization Quality of Life Scale – BREF Malayalam version (WHO QOL-BREF)[15] is based on four domains – physical, psychological, social relationship, and environmental. There are also two items about individual's overall perception of QOL and his/her health. This scale contains a total of 26 items. Higher scores denote higher QOL.
World Health Organization Disability Assessment Schedule 2.0 (WHO DAS)[16] is constructed on the conceptual framework of the International Classification of Functioning, Disability, and Health. It assesses the level of functioning in the six major life domains: (i) Cognition, (ii) mobility, (iii) self-care, (iv) getting along, (v) life activities, and (vi) participation in society. For ease of administration in the outpatient setting, the 12-item interviewer version was used.
Kuppuswamy's Socio-economic Status Scale[17] is the most widely accepted scale in India to assess the socio-economic status of the study group. Education, occupation and family income were the three measurements. Individuals were classified as belonging to lower, upper lower, lower middle, upper middle, or upper socio-economic status.
A specially designed semi-structured proforma was used to collect sociodemographic, illness related, and treatment-related variables.
Procedure
Consecutive patients who met the inclusion and exclusion criteria were recruited. The socio-demographic, illness–related, and treatment-related variables were collected from the patients and/or the family members. The QOL and disability were assessed using the respective scales.
Statistical analysis
Mean and standard deviation were used to describe continuous variables, whereas frequencies and percentages were obtained for categorical data. Pearson's correlation coefficient and Student's t-test were employed to assess the statistical significance. Multiple linear regression was done after adjusting for age and gender. Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS for Windows, SPSS Inc., Version 20, Chicago, IL, USA).
RESULTS
Eighty-four patients were recruited for the study. The socio-demographic and clinical characteristics are recorded in Table 1. Majority of patients were males, and were middle-aged, married, educated, employed, hailing from nuclear families in rural habitat, and belonging to lower socio-economic class. They had early age of onset of illness, with multiple affective episodes, with psychotic symptoms during these episodes. They were on psychotropic medications and reported certain adverse drug reactions.
Table 1.
Socio-demographic and clinical characteristics
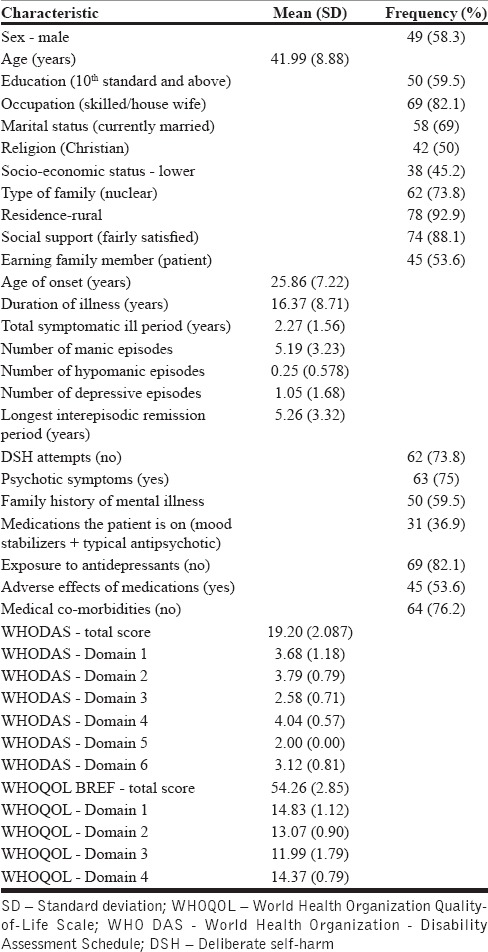
The patients had a mean total WHO-Disability Assessment Scale score of 19.2 ± 2.09. The maximum subscore was in domain 4 (4.04 ± 0.57), i.e. domain of getting along (ability to interact with other people) followed by domain 2 (mobility, i.e., ability to move and get around). Disability was least in the domain 5, i.e., life activities (mean total score of 2).
The subjects had a poor QOL with a mean total WHO-QOL BREF score of 54.26 ± 2.85. The QOL was worst in the domain 3, i.e., social interactions (11.99 ± 1.79) and was better was in the domain 1 (physical, 14.83 ± 1.12).
Table 2 documents the factors associated with disability. The following variables were statistically significantly related to disability on bivariate analysis: gender, age, marital status, not an earning member, age of onset of illness, duration of illness, number of depressive and hypomanic episodes, history of deliberate self–harm, and QOL score. Negative earning member status, and QOL scores were the predictive variables as per multiple linear regression done after adjusting for age and gender. Disability scores increased with increasing age, among females and in those who were not the bread-winners of their family, while it was inversely related to QOL scores.
Table 2.
Factors associated with World Health Organization disability assessment schedule II score
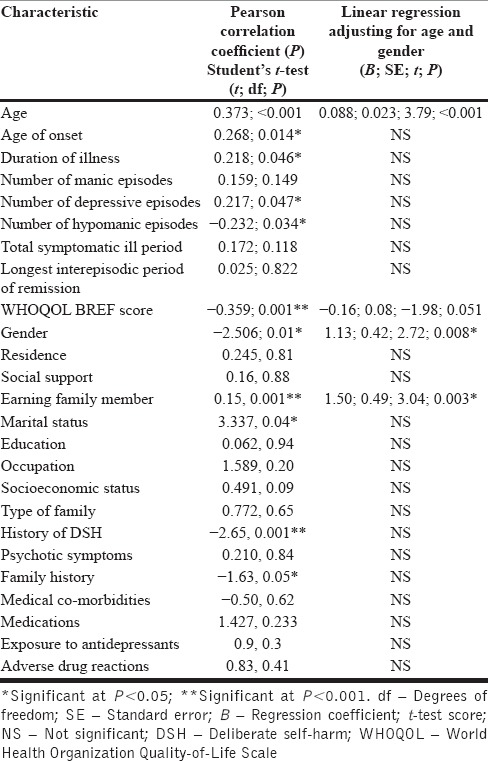
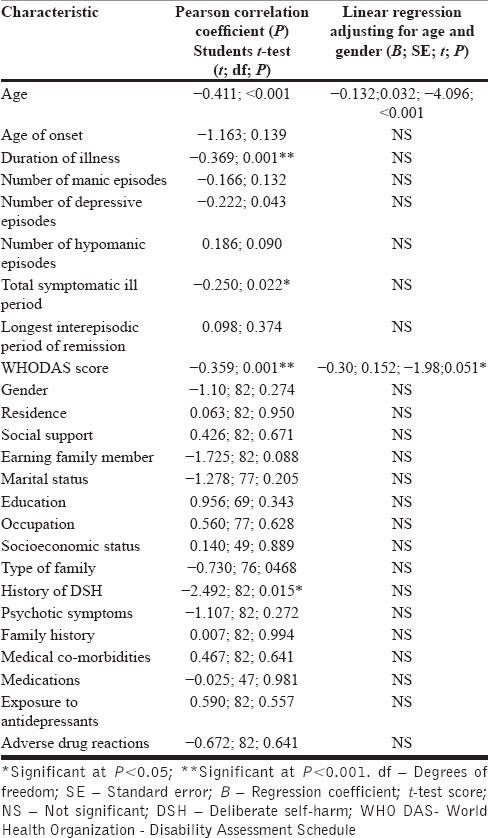
Table 3 includes the factors associated with QOL score. The following variables were significantly related to QOL on bivariate analysis: age, duration of illness, total duration of ill period, history of deliberate self-harm, and WHO DAS score. However, only age and WHO DAS scores remained statistically significant after adjustment using multiple linear regression. QOL was inversely related to age and disability score.
Table 3.
Factors associated with World Health Organization Quality of Life-BREF score
Therefore, disability worsened with increasing age, among females and in those who were not bread-winners of their family, while it was inversely related to QOL scores. QOL was inversely correlated with age and disability score.
DISCUSSION
A significant proportion of patients with bipolar disorder in remission had disability and poor QOL. This is consistent with reports from other studies.[18,19,20,21]
Disability was significantly associated with poorer QOL score. This has been demonstrated in previous studies[22] which suggested the need to identify disability and QOL issues among bipolar patients who are in remission and are asymptomatic. Interventions should focus on reducing disability and improving QOL.
Contrary to a previous study,[20] increasing age was associated with increased disability and low QOL. Disability was also associated with gender and not being an earning member of the family.[7] Social pressures based on gender and livelihood issues form important stress for people with mental illness. Women living within patriarchal societies are prone to extreme stress and need help and support in addition to attempts at changing social norms. Livelihood issues, particularly in countries without welfare measures, are sources of severe stress. Examining and evaluating interventions to reduce disability and to improve QOL are crucial in the successful management of people with bipolar illness. While much has been achieved in reducing symptoms using psychotropic medications, a lot more is needed to be done to reduce disability and to improve QOL in people with mental illness. The strengths of the study are the inclusion of consecutive cases and a relatively larger number of people with bipolar disorder in remission. The cross-sectional study design is one of the limitations.
CONCLUSION
Increasing age remains an irreversible factor associated with poor outcome in BPAD. However, being a male who could earn for himself and family was found to be associated with lower disability level and better QOL. Planning and implementing measures to empower bipolar patients to meet the demands of day to day living and identifying the reversible physical and psychological causes of poor outcome in females may help to improve the outcome. Health insurances and policies should be adopted to meet the treatment expenses, and opportunities for better education and employment of the BPAD population as well as the 'at-risk' group are areas that need to be worked upon. To conclude, the authors identify the need for more longitudinal studies to generalize these findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We wish to acknowledge with deep gratitude, the guidance, and help offered by Dr. K. S. Jacob, Professor of Psychiatry, CMC, Vellore, and for his valuable suggestions and constructive criticisms. The authors also wish to thank Mrs. Renju Susan Baby, Associate Professor, College of Nursing, MOSC Medical College, Kolenchery for her assistance in statistical analysis. We express our heartfelt gratitude toward our colleagues and all those who participated in this study for their kind cooperation and goodwill.
REFERENCES
- 1.Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:293–9. [PubMed] [Google Scholar]
- 2.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global burden of disease study. Lancet. 1997;349:1436–42. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 3.Huxley N, Baldessarini RJ. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9:183–96. doi: 10.1111/j.1399-5618.2007.00430.x. [DOI] [PubMed] [Google Scholar]
- 4.Arnold LM, Witzeman KA, Swank ML, McElroy SL, Keck PE., Jr Health-related quality of life using the SF-36 in patients with bipolar disorder compared with patients with chronic back pain and the general population. J Affect Disord. 2000;57:235–9. doi: 10.1016/s0165-0327(99)00042-7. [DOI] [PubMed] [Google Scholar]
- 5.Xiang YT, Wang CY, Wang Y, Chiu HFK, Zhao J-P, Chen Q, et al. Socio-demographic and clinical determinants of quality of life in Chinese patients with schizophrenia: a prospective study. Qual Life Res. 2010;19:317–22. doi: 10.1007/s11136-010-9593-9. [DOI] [PubMed] [Google Scholar]
- 6.Solomon J, editor. Alcoholism and Clinical Psychiatry. US: Springer; 1982. [Last cited on 2015 Nov 11]. Alcoholism and Clinical Psychiatry; pp. 57–67. Available from: http://www.link.springer.com/chapter/10.1007/978.1-4684-4028-7_5 . [Google Scholar]
- 7.Robb JC, Young LT, Cooke RG, Joffe RT. Gender differences in patients with bipolar disorder influence outcome in the medical outcomes survey (SF-20) subscale scores. J Affect Disord. 1998;49:189–93. doi: 10.1016/s0165-0327(98)00003-2. [DOI] [PubMed] [Google Scholar]
- 8.Leidy NK, Palmer C, Murray M, Robb J, Revicki DA. Health-related quality of life assessment in euthymic and depressed patients with bipolar disorder. Psychometric performance of four self-report measures. J Affect Disord. 1998;48:207–14. doi: 10.1016/s0165-0327(97)00147-x. [DOI] [PubMed] [Google Scholar]
- 9.Namjoshi MA, Buesching DP. A review of the health-related quality of life literature in bipolar disorder. Qual Life Res. 2001;10:105–15. doi: 10.1023/a:1016662018075. [DOI] [PubMed] [Google Scholar]
- 10.Harvey PD, Wingo AP, Burdick KE, Baldessarini RJ. Cognition and disability in bipolar disorder: Lessons from schizophrenia research. Bipolar Disord. 2010;12:364–75. doi: 10.1111/j.1399-5618.2010.00831.x. [DOI] [PubMed] [Google Scholar]
- 11.Goswami U, Sharma A, Khastigir U, Ferrier IN, Young AH, Gallagher P, et al. Neuropsychological dysfunction, soft neurological signs and social disability in euthymic patients with bipolar disorder. Br J Psychiatry. 2006;188:366–73. doi: 10.1192/bjp.188.4.366. [DOI] [PubMed] [Google Scholar]
- 12.ICD-10. Geneva: [Last cited on 2015 Nov 09]. Available from: http://www.apps.who.int/iris/bitstream/10665/37958/8/9241544228_eng.pdf . [Google Scholar]
- 13.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 15.Health WHOD of M. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment: Field Trial Version, December, 1996. [Last cited on 2015 Nov 09]. Available from: http://www.who.int/iris/handle/10665/63529 .
- 16.WHO | WHO Disability Assessment Schedule 2.0 (WHODAS 2.0). WHO. [Last cited on 2015 Nov 09]. Available from: http://www.who.int/classifications/icf/whodasii/en/
- 17.Oberoi SS. Updating income ranges for Kuppuswamy's socio-economic status scale for the year 2014. Indian J Public Health. 2015;59:156–7. doi: 10.4103/0019-557X.157540. [DOI] [PubMed] [Google Scholar]
- 18.Tharoor H, Chauhan A, Sharma PS. A cross-sectional comparison of disability and quality of life in euthymic patients with bipolar affective or recurrent depressive disorder with and without comorbid chronic medical illness. Indian J Psychiatry. 2008;50:24–9. doi: 10.4103/0019-5545.39755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chand PK, Mattoo SK, Sharan P. Quality of life and its correlates in patients with bipolar disorder stabilized on lithium prophylaxis. Psychiatry Clin Neurosci. 2004;58:311–8. doi: 10.1111/j.1440-1819.2004.01237.x. [DOI] [PubMed] [Google Scholar]
- 20.Chacko D, Narayan KT, Prabhavathy KS. Disability in patients with bipolar and recurrent depressive disorder in remission: A comparative study. Indian J Psychol Med. 2011;33:49–53. doi: 10.4103/0253-7176.85395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar D, Basu D, Kulhara P, Sharan P. Psychosocial correlates of subsyndromal symptoms and functioning of bipolar patients stabilized on prophylactic lithium. Indian J Psychiatry. 2001;43:199–205. [PMC free article] [PubMed] [Google Scholar]
- 22.Tharoor H, NarasimhanaSharma PS, Chauhan A. Disability and quality of life in euthymic patients with bipolar affective or recurrent depressive disorder. Ger J Psychiatry. 2007;10:111–6. doi: 10.4103/0019-5545.39755. [DOI] [PMC free article] [PubMed] [Google Scholar]


