Abstract
Hashimoto's encephalopathy is usually underdiagnosed and untreated because of complex neuropsychiatric manifestation. We report a case of an adolescent female with Hashimoto's encephalopathy who responded well to a combination of aspirin and levothyroxine. A 16-year-old girl presented at psychiatric emergency services with a depressive episode, menstrual irregularities, and a 5-month past history of thyroid swelling. On clinical examination, she was in a euthyroid state with insignificant neurological history. However, her previous investigation revealed a hypothyroid state. Her magnetic resonance imaging findings demonstrated infarcts in the bilateral gangliocapsular region and left frontal periventricular deep white matter lesion. Ultrasonography of the thyroid and fine needle aspiration cytology confirmed lymphocytic thyroiditis. Anti-thyroid peroxidase (289 IU/ml) antibody titer was elevated (289 IU/mL). Her depressive symptoms responded well to antidepressants, mood stabilizers, nonsteroidal anti-inflammatory drugs, and levothyroxine. She remained in the euthyroid state and then in the euthymic state for 3 years. Hashimoto's encephalopathy is steroid-responsive encephalopathy. Most researchers have observed a dramatic response to steroids with or without levothyroxine. A clinician may consider aspirin as an alternative to a steroid in long-term management to avoid steroid-related side effects and contraindications.
Key words: Aspirin, Hashimoto's encephalopathy, levothyroxine, steroid-responsive
INTRODUCTION
Thyroid gland dysfunctions are usually associated with cognitive and affective dysfunctions. A minor change in the thyroid hormone concentration has been reported with changes in cognitive and affective functions.[1] Hashimoto's encephalopathy was first reported in 1966 and was associated with Hashimoto's thyroiditis. Although it is a controversial disorder, Hashimoto's encephalopathy is considered an autoimmune disease because of its association with immunological disorders, such as myasthenia gravis, primary biliary cirrhosis, and pernicious anemia. Hashimoto's encephalopathy, an unusual neurological disorder with female preponderance, has its typical onset in the fifth decade of unclear etiology, pathogenesis, and management.[2]
Hashimoto's encephalopathy presents with neurological manifestations such as generalized/focal tonic-clonic seizures, status epileptics, myoclonus, stroke, hyperreflexia, and tremors. Neuropsychiatric manifestations such as psychosis, visual hallucination, paranoid delusion, mania, depression, dementia, and catatonia have been reported in 25-36% patients. These manifestations respond well to steroids rather than the conventional treatment, highlighting an autoimmune origin of the disorder.[2,3,4,5,6]
Although Hashimoto's encephalopathy is rare among the pediatric group, it is a diagnostic challenge in child psychiatry and neurology.[7] Managing the symptoms of this condition is often difficult because of the unpredictable nature of Hashimoto's thyroiditis.
In a recent review, only 50 cases aged <18 years were identified among 300 PubMed articles until July 2013.[8] Only a few Indian cases have been reported among the pediatric population. Most researchers have reported a dramatic response to steroids with or without levothyroxine. We report the first case of atypical presentation of Hashimoto's encephalopathy in an adolescent who recovered successfully with nonsteroid agents and levothyroxine.
CASE REPORT
A 16-year-old girl presented with acute onset of sadness of mood, decreased interest to work and pleasurable activities, irritability, aggressiveness and abusiveness, impulsivity, reduced appetite, easy fatigability, and sleep disturbance, and was unable to concentrate on work for more than a day.
On mental status examination, she was agitated, irritable, hostile, impulsive, emotionally labile, and unable to sustain attention. Her neurological examination was within the normal limit. She had no past history suggestive of any seizure, weakness, and tremors. She was premorbidly well-adjusted with an unremarkable developmental and familial history of mental and thyroid illness.
Five months back, she noticed a small swelling on her thyroid region along with menstrual irregularities called oligomenorrhea and menorrhagia. Her thyroid function tests were suggesting hypothyroidism, which was treated with homeopathic medicine [Table 1]. Her menstrual irregularities improved over 3-4 months. On admission, the patient's thyroid function test was indicative of the euthyroid state. Her brain magnetic resonance imaging (MRI) findings demonstrated infarcts in the bilateral gangliocapsular region and left frontal periventricular deep white matter lesion [Figure 1]. Her ultrasonography (USG) of the thyroid revealed a well-defined cystic lesion measuring 3.8 mm × 3.2 mm in the right thyroid lobe, followed by fine needle aspiration cytology of swelling, indicating lymphocytic thyroiditis. Anti-thyroid peroxidase antibody levels were elevated to 289 IU/mL. The erythrocyte sedimentation rate (ESR) increased to 50 mm/h with a slight increase in the leucocyte count. Her liver function test, renal function test, electrocardiogram, chest X-ray, USG of the abdomen and pelvis, and electroencephalogram were normal.
Table 1.
Laboratory findings in the index case

Figure 1.
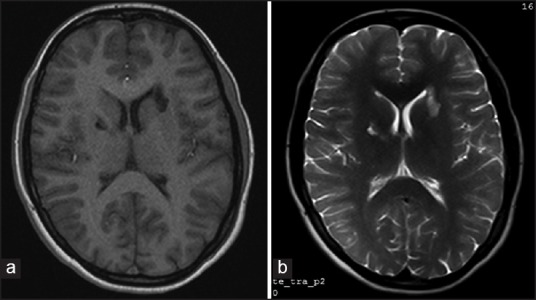
Axial magnetic resonance images of brain demonstrating infarcts in the bilateral gangliocapsular region and left frontal periventricular deep white matter. (a) T1-weighted magnetic resonance imaging. (b) T2-weighted magnetic resonance imaging
She was initially administered fluoxetine 20 mg/day, which was increased gradually to 40 mg/day. Addition of mood stabilizers was considered because of her extreme impulsivity and aggressiveness. Oxcarbazepine 200 mg/day was increased gradually to 600 mg/day. However, she showed no improvement in depressive symptoms and impulsivity. On the basis of laboratory findings and responses to drugs, we considered treatment-resistant depression secondary to Hashimoto's encephalopathy. The patient was administered levothyroxine for the thyroid state and aspirin as an anti-inflammatory agent. Adding levothyroxine (50 µg/day) with aspirin (150 mg/day) for a week resolved her symptoms completely. Her elevated ESR and antimicrosomal antibodies returned to normal, and she remained in the euthyroid state with a normal sensorium and behavior for approximately 3 years.
DISCUSSION
Hashimoto's encephalopathy is a rare neurological disorder that occurs primarily in the fifth decade with a male to female ratio of 1:4. It is mainly present in two subtypes: A sudden vasculitis type (up to 25% cases) and diffuse progressive type (up to 75% patients) characterized by cognitive decline, dementia, confusion, and psychiatric manifestation.[2] In the index case, the patient's clinical course was more consistent with the sudden vasculitis type because of the abrupt onset of depressive symptoms without a focal neurological deficit and MRI findings.
Most common presentations reported include a neurological presentation, the involvement of the pyramidal tract, seizure, and tremor in the descending order. The neuropsychiatric presentation that includes schizophrenia-like psychotic disorder, mania and depression was reported with lower incidence. Pathogenesis of neuropsychiatric manifestation in Hashimoto's encephalopathy remains unknown, and no correlation exists between the concentration of thyroid antibodies and severity of symptoms. The reaction of these autoantibodies with the brain tissue and endothelial cells remains unclear.[2] The formation of autoantibodies against the N-terminal of α-enolase (NAE) may cause infarcts in the bilateral gangliocapsular region and left frontal periventricular deep white matter lesion in our case.
Recent studies support the relationship between neuropsychiatric symptoms and α-enolase antibodies. The α-enolase antigen is found in both endothelial cells of the blood vessel and thyroid gland, indicating the possibility of an underlying autoimmune vasculitis mechanism. Therefore, autoantibodies against the NAE may be a potential biomarker of Hashimoto's encephalopathy, and this possibility is being supported by most recently published studies in Japan.[9,10]
Hashimoto's thyroiditis is characterized by bouts of hypothyroid, euthyroid, and hyperthyroid states. Thus, a single thyroid function test may not be useful for detecting thyroiditis. The longitudinal history of the thyroid status seems useful most cases.
Initially, our patient appeared nonresponsive to conventional antidepressants and mood stabilizers. Thus, one should highly suspect a possibility of Hashimoto's encephalopathy in a nonresponsive patient and a patient showing an initial response followed by unresponsiveness to conventional antidepressants. In most recently published reviews, the clinical response was observed in 98% patients treated with steroids, 92% with steroids and levothyroxine, and 67% with levothyroxine.[2] Most recent studies have well documented the effectiveness of steroids.[5,11,12,13] However, only a few have responded well with mood stabilizers, antidepressants, and antipsychotics.[4,14]
The role of steroids in the acute management of ischemic stroke remains controversial. The recently published Cochrane review recommends that steroids, considered magic drugs in neurology in the past, play no active role in the management of acute ischemic stroke. Moreover, they increase the risk of gastrointestinal bleed, infection, and hyperglycemia.[15,16] The long-term use of steroids, which is often required in Hashimoto's encephalopathy, predisposes to several side effects including hypertension, osteoporosis, cataract, cushing syndrome, and growth retardation.[17] The index case appears unique in this aspect because the patient responded well when levothyroxine and nonsteroidal anti-inflammatory drug (NSAID) (aspirin) along with fluoxetine was used to treat her depressive symptoms.
Although using NSAIDs has been attempted in the management of chronic thyroiditis, to the best of our knowledge, response is not documented for any other case report or study with the neuropsychiatric presentation. Most NSAIDs act through selective and nonselective cyclooxygenase-2 inhibition, reducing oxidative stress.[18,19] In addition to the anti-inflammatory properties of aspirin, it is an antiplatelet drug, which may be helpful in preventing further infarcts and procrastinating the relapsing and remitting nature of the illness.
CONCLUSION
Hashimoto's encephalopathy, a rare disorder, is unrelated to the thyroid status of a patient. Most patients present with variable neuropsychiatric manifestations and course, indicating pathogenesis through both autoimmune and vasculitis mechanisms. They may have treatment-resistant psychiatric and neurological illnesses and respond dramatically to steroids with serious and potential side effects; however, aspirin or other NSAIDs along with levothyroxine, mood stabilizers, and antipsychotics may be considered for treatment. A psychiatrist should be aware of this often unrecognized entity to ensure accurate diagnosis and timely treatment, particularly among the pediatric group.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zarkovic M. Autoimmune thyroid disease and brain. Srp Arh Celok Lek. 2005;133(Suppl 1):88–91. doi: 10.2298/sarh05s1088z. [DOI] [PubMed] [Google Scholar]
- 2.Chong JY, Rowland LP, Utiger RD. Hashimoto encephalopathy: Syndrome or myth? Arch Neurol. 2003;60:164–71. doi: 10.1001/archneur.60.2.164. [DOI] [PubMed] [Google Scholar]
- 3.Lin YT, Liao SC. Hashimoto encephalopathy presenting as schizophrenia-like disorder. Cogn Behav Neurol. 2009;22:197–201. doi: 10.1097/WNN.0b013e318197926e. [DOI] [PubMed] [Google Scholar]
- 4.Lin CL, Yang SN, Shiah IS. Acute mania in a patient with hypothyroidism resulting from Hashimoto's thyroiditis. Gen Hosp Psychiatry. 2013;35:683.e1–2. doi: 10.1016/j.genhosppsych.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Normann C, Frase L, Berger M, Nissen C. Steroid-responsive depression. BMJ Case Rep 2013. 2013:pii: Bcr2013009101. doi: 10.1136/bcr-2013-009101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chiba Y, Odawara T. Catatonia in the elderly. Nihon Rinsho. 2013;71:1804–9. [PubMed] [Google Scholar]
- 7.Voll R. Undetected Hashimoto encephalopathy — A diagnostic challenge in child psychiatry and child neurology. Z Kinder Jugendpsychiatr Psychother. 2010;38:21–7. doi: 10.1024/1422-4917.a000003. [DOI] [PubMed] [Google Scholar]
- 8.Patnaik SK, Upreti V, Dhull P. Steroid responsive encephalopathy associated with autoimmune thyroiditis (SREAT) in childhood. J Pediatr Endocrinol Metab. 2014;27:737–44. doi: 10.1515/jpem-2013-0435. [DOI] [PubMed] [Google Scholar]
- 9.Kishitani T, Matsunaga A, Yoneda M. The biomarker and treatment in Hashimoto's encephalopahty. Nihon Rinsho. 2013;71:893–7. [PubMed] [Google Scholar]
- 10.Takahashi Y. Diagnostic and therapeutic scheme of autoimmune mediated encephalitis/encephalopathy. Rinsho Shinkeigaku. 2012;52:836–9. doi: 10.5692/clinicalneurol.52.836. [DOI] [PubMed] [Google Scholar]
- 11.Olmez I, Moses H, Sriram S, Kirshner H, Lagrange AH, Pawate S. Diagnostic and therapeutic aspects of Hashimoto's encephalopathy. J Neurol Sci. 2013;331:67–71. doi: 10.1016/j.jns.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 12.Nayak HK, Daga MK, Kumar R, Garg SK, Kumar N, Mohanty PK. A series report of autoimmune hypothyroidism associated with Hashimoto's encephalopathy: An under diagnosed clinical entity with good prognosis. BMJ Case Rep 2010. 2010:pii: Bcr0120102630. doi: 10.1136/bcr.01.2010.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erol I, Saygi S, Alehan F. Hashimoto's encephalopathy in children and adolescents. Pediatr Neurol. 2011;45:420–2. doi: 10.1016/j.pediatrneurol.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Andreou C, Bozikas VP, Lagoudis A, Paspali D, Fokas K. Treatment of neuropsychiatric symptoms associated with euthyroid Hashimoto thyroiditis with antidepressants: A case report. Gen Hosp Psychiatry. 2009;31:199–200. doi: 10.1016/j.genhosppsych.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Sandercock PA, Soane T. Corticosteroids for acute ischaemic stroke. Cochrane Database Syst Rev. 2011;9:CD000064. doi: 10.1002/14651858.CD000064.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qizilbash N, Lewington SL, Lopez-Arrieta JM. Corticosteroids for acute ischaemic stroke. Cochrane Database Syst Rev. 2000;2:CD000064. doi: 10.1002/14651858.CD000064. [DOI] [PubMed] [Google Scholar]
- 17.Schäcke H, Döcke WD, Asadullah K. Mechanisms involved in the side effects of glucocorticoids. Pharmacol Ther. 2002;96:23–43. doi: 10.1016/s0163-7258(02)00297-8. [DOI] [PubMed] [Google Scholar]
- 18.Zenda T, Yokoyama K, Minato H, Masunaga T, Shinozaki K. A variant of thyrotoxicosis associated with chronic thyroiditis characterized by prolonged fever, absence of anti-thyroidal antibodies, and favorable response to naproxen. Am J Med Sci. 2007;333:305–8. doi: 10.1097/MAJ.0b013e318053d979. [DOI] [PubMed] [Google Scholar]
- 19.Taddei S, Caraccio N, Virdis A, Dardano A, Versari D, Ghiadoni L, et al. Low-grade systemic inflammation causes endothelial dysfunction in patients with Hashimoto's thyroiditis. J Clin Endocrinol Metab. 2006;91:5076–82. doi: 10.1210/jc.2006-1075. [DOI] [PubMed] [Google Scholar]


