Sir,
The Standing Parliamentary Committee that investigated the functioning of Central Drugs Standard Control Organization (CDSCO) noted that the regulatory body “had skewed priorities, according primacy to the propagation and facilitation of the drugs industry, due to which, the interest of the biggest stakeholder, i.e. the consumer has never been ensured.”[1] The report discussed CDSCO's inability to produce any information related to the regulatory process that led to the approval of Deanxit (fixed-dose combination [FDC] of flupenthixol and melitracen), which curiously is prohibited for sale and use in Denmark, its country of origin. The report remarked that the approval to import and market Deanxit was in clear violation of the existing laws.
Doctors also share the blame for being prolific prescribers of irrational combinations, due to lack of knowledge and/or in the lure of incentives offered by pharmaceutical companies. An evaluation of 100 resident doctors revealed that 81% lacked knowledge about the rationality of given FDCs and only 43% were able to mention a single banned FDC in India.[2] A study from Mumbai highlighted the nexus between pharmaceutical companies, medical representatives, chemists and doctors to make profits at the expense of consumers and the public's health.[3]
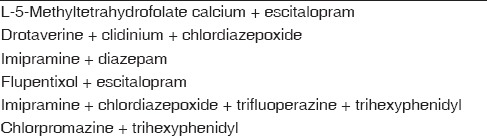
A gazette notification from the Government of India dated March 10, 2016 prohibiting manufacture, sale, and distribution of about 344 FDCs is a step in the right direction.[4] However, most of the irrational/unapproved antidepressant/benzodiazepine and antipsychotic/anticholinergic FDCs have been left out of the list. Table 1 displays the psychotropic FDCs included in the list of banned combinations.
Table 1.
Psychiatric formulations included in the list of banned fixed-dose combinations
A recent empirical research analyzing CDSCO approval status and sales volumes of oral FDCs came out with some dark findings.[5] Nearly, 81% of the marketed antidepressant/benzodiazepine FDCs and 70% of the antipsychotic formulations were unapproved. Proportions of sales volumes arising from unapproved formulations were 69% from antidepressants/benzodiazepines and 43% from antipsychotics; way ahead of parallel figures of 28% for NSAIDs and 0.4% for metformin-containing unapproved FDC formulations. Over 53% of antipsychotic FDC sales came from formulations including drugs banned/restricted internationally.
The promotion of antidepressant/benzodiazepine FDCs by pharmaceutical companies in India is often targeted at general/specialist physicians and neurologists to achieve greater sales. It is not uncommon to find patients turning up to psychiatrists being dependent on one of these FDCs being prescribed by non-psychiatrists, perpetuating iatrogenic benzodiazepine dependence, and abuse. A study investigating benzodiazepine prescription patterns in the United States reported that <10% of individuals using benzodiazepines have their prescriptions written by a psychiatrist.[6] Most guidelines restrict the use of benzodiazepines beyond 4 weeks for their dependence and abuse liability and potential to cause psychomotor and cognitive impairment. Long-term benzodiazepine use causes impairment in cognition across multiple domains,[7] with only partial recovery of cognitive function following withdrawal.[8]
Most available irrational antipsychotic FDCs (70%) contain a combination of trihexyphenidyl with risperidone, trifluoperazine, haloperidol, chlorpromazine, or thioridazine.[5] Apparently, the basis of this combination is to prevent the extrapyramidal side effects of antipsychotic medications. None of these FDCs has CDSCO approval, yet there are widely marketed and prescribed. Extrapyramidal side effects susceptibility differs from person to person, and all patients do not invariably require trihexyphenidyl as a preventive measure. The antipsychotic-anticholinergic combination does not allow a need-based dose titration of trihexyphenidyl, also incurring additional peripheral and central anticholinergic side effects for the patient. Long-term use may cause cognitive impairment and worsening of tardive dyskinesia.[9,10] The FDC containing chlorpromazine and trifluoperazine carries the risk of additive central nervous system toxicity and cardiac arrhythmia, without any logical reason or theoretical benefit of combing two drugs from the same class.
McGettigan et al. recommend policy level changes to deal with the menace.[5] Regulatory authorities should tender an immediate ban on the production and sales of unapproved FDCs, with a staged withdrawal from the market. Stringent measures need to be taken against pharmaceutical companies marketing and selling unapproved psychotropic FDCs. Accountability of regulatory decisions should be improved, and new drug approval processes need to be transparent and open to public access and scrutiny.
Psychiatric/nonpsychiatric doctors should use their clinical judgment and available evidence base for prescription decisions rather than falling trap to marketing gimmicks of pharmaceutical companies. Medical education and curriculum should sensitize doctors toward the practice of rational prescribing. Practitioners should totally refrain from prescribing antidepressant/benzodiazepine FDCs. There is no justifiable rationale for combining antidepressants with benzodiazepines. If the need to co-prescribe is deemed necessary by a clinician, both the drugs may be prescribed separately as antidepressant use may continue for a longer period while benzodiazepines may be tapered off completely in 4–6 weeks. Likewise, trihexyphenidyl may be separately prescribed in appropriate (rather than predetermined) doses alongside antipsychotics for persons that develop or have greater proneness for extrapyramidal side effects.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
- 1.New Delhi: Parliament of India; 2012. [Last accessed on 2016 Mar 15]. Department-Related Standing Committee on Health and Family Welfare (2012 May) 59th Report on the Functioning of the Central Drugs Standard Control Organization (CDSCO) Available from: http://www.164.100.475/newcommittee/reports/englishcommittees/committee%20on%20health%20and%20family%20welfare/59.pdf . [Google Scholar]
- 2.Goswami N, Gandhi A, Patel P, Dikshit R. An evaluation of knowledge, attitude and practices about prescribing fixed dose combinations among resident doctors. Perspect Clin Res. 2013;4:130–5. doi: 10.4103/2229-3485.111797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roy N, Madhiwalla N, Pai SA. Drug promotional practices in Mumbai: A qualitative study. Indian J Med Ethics. 2007;4:57–61. doi: 10.20529/IJME.2007.020. [DOI] [PubMed] [Google Scholar]
- 4.Ministry of Health and Family Welfare, Government of India Notification Dated 10 March, 2016, New Delhi. 2016. [Last accessed on 2016 Mar 18]. Available from: http://www.cdsco.nic.in/writereaddata/SO%20705(E)%20TO%201048(E)%20DATED%2010-03-2016.pdf .
- 5.McGettigan P, Roderick P, Mahajan R, Kadam A, Pollock AM. Use of fixed dose combination (FDC) drugs in India: Central regulatory approval and sales of FDCs containing non-steroidal anti-inflammatory drugs (NSAIDs), metformin, or psychotropic drugs. PLoS Med. 2015;12:e1001826. doi: 10.1371/journal.pmed.1001826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olfson M, King M, Schoenbaum M. Benzodiazepine use in the United States. JAMA Psychiatry. 2015;72:136–42. doi: 10.1001/jamapsychiatry.2014.1763. [DOI] [PubMed] [Google Scholar]
- 7.Barker MJ, Greenwood KM, Jackson M, Crowe SF. Cognitive effects of long-term benzodiazepine use: A meta-analysis. CNS Drugs. 2004;18:37–48. doi: 10.2165/00023210-200418010-00004. [DOI] [PubMed] [Google Scholar]
- 8.Barker MJ, Greenwood KM, Jackson M, Crowe SF. Persistence of cognitive effects after withdrawal from long-term benzodiazepine use: A meta-analysis. Arch Clin Neuropsychol. 2004;19:437–54. doi: 10.1016/S0887-6177(03)00096-9. [DOI] [PubMed] [Google Scholar]
- 9.Desmarais JE, Beauclair L, Margolese HC. Anticholinergics in the era of atypical antipsychotics: Short-term or long-term treatment? J Psychopharmacol. 2012;26:1167–74. doi: 10.1177/0269881112447988. [DOI] [PubMed] [Google Scholar]
- 10.Ogino S, Miyamoto S, Miyake N, Yamaguchi N. Benefits and limits of anticholinergic use in schizophrenia: Focusing on its effect on cognitive function. Psychiatry Clin Neurosci. 2014;68:37–49. doi: 10.1111/pcn.12088. [DOI] [PubMed] [Google Scholar]


