Abstract
Primary angiitis of the central nervous system (PACNS) is a rare disorder affecting both medium- and small-sized vessels. Intracranial haemorrhages though less reported are in the form of parenchymal haemorrhage and subarachnoid haemorrhage. We report a case of PACNS with intraventricular haemorrhage due to aneurysms secondary to progression of vasculitis.
Keywords: Infarcts, intraventricular hemorrhage, primary angiitis of the central nervous system (PACNS)
Introduction
Primary angiitis of the central nervous system (PACNS) is a rare disorder affecting both medium- and small-sized vessels.[1] Here we report a case of PACNS who presented initially with ischemic stroke followed by aneurysmal intraventricular hemorrhage.
Case Report
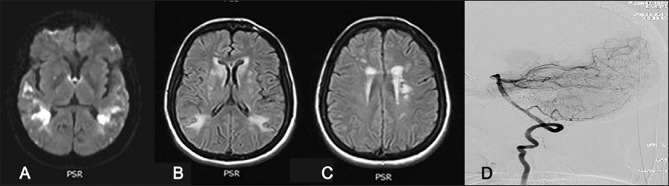
A 42-year-old female with no vascular risk factors presented with sudden onset of Wernicke's aphasia and right facial paresis. Her neuroimaging showed multiple acute and subacute infarcts involving cortical and subcortical regions of both the hemispheres [Figure 1].
Figure 1.
(a) DWI images showing diffusion restriction in bilateral peritrigonal region and patchy in bilateral posterior temporal and parietal lobes (b and c) FLAIR images showing hyperintense lesions in bilateral posterior parietal, bilateral caudate, and bilateral corona radiata (d) vertebro basilar system-conventional angiogram lateral view, showing normal appearance of vessels
Cardiac evaluation, systemic vasculitis workup, and cerebrospinal fluid analysis did not reveal any abnormality. Digital subtraction angiography showed mild luminal irregularities in bilateral internal carotid artery (ICA) origins and bilateral cavernous ICA. In view of cortical and subcortical infarcts in a patient with no risk factors, the possibility of PACNS was considered and she underwent meningocortical biopsy that was suggestive of small vessel vasculitis. Accordingly she was initiated on steroids and monthly cyclophosphamide. At 6 months follow-up, she had partial improvement in comprehension of speech with no fresh neurological events.
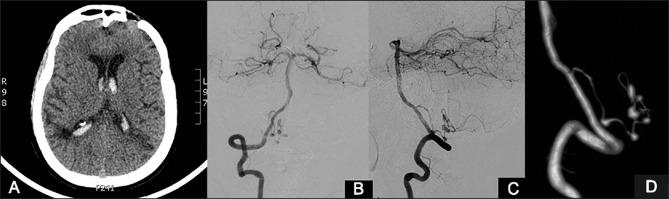
Nine months later, she presented with acute onset severe headache followed by alteration of sensorium. Computed tomography (CT) brain showed intraventricular hemorrhage. Conventional angiography showed multiple aneurysms in the left posterior inferior cerebellar artery (PICA) with luminal irregularities in multiple intracranial arteries [involving bilateral PCA, left middle cerebral artery (MCA) M2, and bilateral cavernous ICA], features consistent with a diagnosis of vasculitis [Figure 2]. She underwent clipping and wrapping of the PICA aneurysms. She was discharged on steroids and azathioprine.
Figure 2.
Vertebral angiograms AP (a) and lateral (b) views show multiple irregular aneurysms in the telovelomedullary and telovelotonsillar segments of right posterior inferior cerebellar artery. The findings are better appreciated in the 3D angiogram image (c) 3D reconstruction of vertebral angiogram showing multiple aneurysms in the left PICA (d)
Discussion
Primary angiitis of the CNS (PACNS) is a rare form of vasculitis confined to brain and spinal cord. Though the most common presentation is ischemic strokes, headache, seizures, and cognitive decline, while intracranial hemorrhage is a rare manifestation in 11-12% of cases.[2,3] Of the hemorrhagic strokes, intracerebral bleed and subarachnoid hemorrhage have been described, but intraventricular hemorrhage due to aneurysmal rupture has not been described in PACNS as was observed in our patient.
The diagnosis of an isolated CNS vasculitis can be challenging and it relies on a high index of suspicion, as the clinical presentation is usually diverse, and there are a number of causes and mimickers. Cerebrospinal fluid (CSF) analysis is abnormal in 80-90% of the patients and shows mildly increased leucocyte count and increase in total protein concentration.[4] Magnetic resonance imaging (MRI) findings are nonspecific and include cortical and subcortical infarcts, parenchymal and leptomeningeal enhancement, intracranial hemorrhage, and tumor-like mass lesions.[5,6,7]
On conventional angiography, smooth narrowing of affected vessels in multiple vascular distributions is found to be the most frequent abnormality. Other features include segmental arterial dilatations, vascular occlusions, collateral formation, and prolonged circulation time. Microaneurysms are rarely seen. However, many patients with histologically proven PACNS may have an entirely normal angiogram.[6]
Meningocortical biopsy is the gold standard for diagnosis of primary CNS vasculitis with a sensitivity of up to 60%.[5] Histopathology may show granulomatous, necrotizing, lymphocytic, or a mixed inflammatory response. Though granulomatous is the commonest pathology described in PACNS, in cases presenting with intracranial hemorrhage necrotizing vasculitis is the predominant histological pattern. In a study that analyzed the cases of PACNS presenting with intracranial hemorrhage, they observed that such patients were more frequently women, less frequently had altered cognition, a persistent neurologic deficit, or stroke at presentation and MRI evidence of cerebral infarctions, and less frequently needed immunosuppressive therapy at the last follow-up.[2]
Our patient presented initially with ischemic stroke, and the diagnosis of PACNS was proved by histopathology. But while on aggressive treatment with steroids and cyclophosphamide she presented with intraventricular bleeding 9 months later and digital subtraction angiography that was normal initially, showed significant progression of vasculitis with aneurysms that required surgical treatment and alternate immunosuppressive agent. To our knowledge, this is the first report of intraventricular bleeding with aneurysm in PACNS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Salvarani C, Brown RD, Jr, Hunder GG. Adult primary central nervous system vasculitis. Lancet. 2012;380:767–77. doi: 10.1016/S0140-6736(12)60069-5. [DOI] [PubMed] [Google Scholar]
- 2.Salvarani C, Brown RD, Jr, Calamia KT, Christianson TJH, Huston J, 3rd, Meschia JF, et al. Primary central nervous system vasculitis presenting with intracranial hemorrhage. Arthritis Rheum. 2011;63:3598–606. doi: 10.1002/art.30594. [DOI] [PubMed] [Google Scholar]
- 3.Calabrese LH, Duna GF, Lie JT. Vasculitis in the central nervous system. Arthritis Rheum. 1997;40:1189–201. doi: 10.1002/1529-0131(199707)40:7<1189::AID-ART2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 4.Calabrese LH, Furlan AJ, Gragg LA, Ropos TJ. Primary angiitis of the central nervous system: Diagnostic criteria and clinical approach. Cleve Clin J Med. 1992;59:293–306. doi: 10.3949/ccjm.59.3.293. [DOI] [PubMed] [Google Scholar]
- 5.Salvarani C, Brown RD, Jr, Calamia KT, Christianson TJ, Weigand SD, Miller DV, et al. Primary central nervous system vasculitis: Analysis of 101 patients. Ann Neurol. 2007;62:442–51. doi: 10.1002/ana.21226. [DOI] [PubMed] [Google Scholar]
- 6.Pomper MG, Miller TJ, Stone JH, Tidmore WC, Hellmann DB. CNS vasculitis in autoimmune disease: MR imaging findings and correlation with angiography. AJNR Am J Neuroradiol. 1999;20:75–85. [PubMed] [Google Scholar]
- 7.Greenan TJ, Grossman RI, Goldberg HI. Cerebral vasculitis: MR imaging and angiographic correlation. Radiology. 1992;182:65–72. doi: 10.1148/radiology.182.1.1727311. [DOI] [PubMed] [Google Scholar]