Abstract
Purpose
To validate computer software developed to assess digital corneal photographs of fungal keratitis in clinical research.
Methods
A cornea specialist and five medical students (after training) graded on two occasions 100 corneal photographs of patients with fungal keratitis using Optscore software. Variables assessed were lesion area, location, degree of opacity, percentage of the ulcer lying within a central 4mm circle of the cornea. Intraclass correlation coefficients (ICCs) were used to assess intragrader reliability, agreement of the students with the corneal specialist, and the reliability of the group mean of the student raters. The area determined using Optscore was compared to the area estimated from slit lamp and to visual acuity.
Results
As a group, medical students achieved an ICC greater than 0.9 for five out of the seven assessed variables. Similar levels of consistency were found after analyzing the graders’ individual results compared to the specialist. The area estimated using slit lamp examination was highly correlated with the mean area determined by Optscore, as was the logarithm of the minimum angle of resolution visual acuity at enrollment.
Conclusions
Non-expert graders using Optscore to assess digital photographs of fungal keratitis are self-consistent, agree with an expert grader both as a group and individually, and measurements of ulcer area obtained from Optscore are highly correlated with measurements of the same patients obtained on clinical examination. These observations support the validity of Optscore for assessing corneal pathology associated with fungal keratitis and make it a promising clinical research tool.
Keywords: Corneal ulcer grading, digital photography, Mycotic Ulcer Treatment Trial (MUTT), Optscore, Steroids for Corneal Ulcers Trial (SCUT)
INTRODUCTION
Digital photographs are commonly obtained in order to document corneal pathology and provide the opportunity to share images with colleagues for remote evaluation. Grading images in comparison to direct grading of pathology by treating physicians has several advantages. These include standardization of the grading process, the opportunity to re-examine images multiple times and the ability to focus the grader exclusively on the clinical pathology on the image, masked from other clinical data which might carry the potential to alter his or her interpretation of the clinical exam. Such methods have been used extensively in the study of retinal disorders, such as in the Early Treatment Diabetic Retinopathy Study (ETDRS; see for example1–3). Several methods have been designed to help the clinician evaluate the severity of a corneal infection but most help the physician on a case-by-case basis and do not allow for a study of many ulcers (including irregularly shaped ulcers), nor provide a user-friendly interface.4–7 We developed a software program, Optscore, as a platform for grading a large number of digital corneal photographs in a standardized fashion as part of the Steroids for Corneal Ulcers Trial (SCUT) and the Mycotic Ulcer Treatment Trial (MUTT).8,9 We present the results of our study to validate the use of this software in the evaluation of fungal corneal ulcers.
METHODS
Design of Optscore
Optscore was built using standard web application technologies, but all components of the software (including the server and the browser) run on a single machine. The server portion was built using the computer language Ruby on Rails (api.rubyonrails.org), and the browser-based portion was built using JavaScript and the HTML 5 canvas. This allowed rich, interactive graphics to be displayed and manipulated in the browser without plugins. Case series were prepared for grading by assembling the study images and creating a file describing the grading questions. Optscore then randomized the order of the images before presenting them to each grader. Optionally, the software allows the repetition of a random subset of the images at specified minimum separation from other occurrences of the same image, but this functionality was not used in the study presented here.
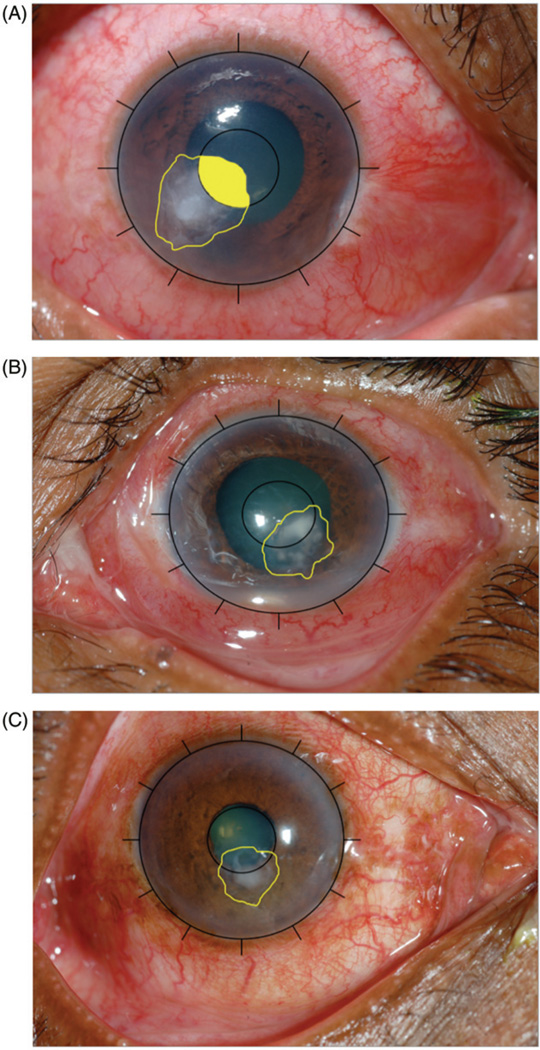
A multi-tiered strategy was followed for ensuring the correctness of Optscore and the calculations it performed. An extensive automated test suite was written which verified that Optscore produced the correct answers for selected problems. Finally, Optscore was used to trace simulated “ulcers” in a variety of geometric shapes and the results were verified by hand. In order to calculate the area of ulcers, standard techniques for calculating the area of a polygon were used.10 The polygon was broken into non-overlapping triangles, and the total area derived by summing the area of each triangle. We used Monte Carlo integration to calculate the fraction of an ulcer lying within the central 4mm circle of the cornea (see examples of overlapping ulcers in the central circle of the cornea in Figure 1).11
FIGURE 1.
Examples of ulcers outlined using Optscore software. The grid marking the 4mm central circle and the outer circle with marks for the 12 clock hours as seen in Optscore is presented. (A) The area of the ulcer within the central circle is colored. (B and C) Ulcers with variable opacities outlined using Optscore.
Source of Digital Corneal Images
The photographs used in this validation study were randomly selected using patient ID numbers and the Microsoft Excel RAND command from images obtained from South Indian patients with fungal keratitis in a study comparing topical voriconazole with topical natamycin.8 All patients consented to photography under a research protocol (following the guidelines of the declaration of Helsinki) approved by the Committee for the Protection of Human Subjects at Dartmouth College, University of California San Francisco and Aravind Eye Hospital (India), which included the current evaluation of Optscore. All pictures had a fixed size of 902 pixels in width and 600 pixels in height and had been taken using a Nikon (Tokyo, Japan) D series camera with a Telephoto AF micro Nikkor 105mm f/2.8 diopter (D) autofocus lens set up at 1:1 magnification. All photographers had been previously trained and certified for the study, and followed the established study protocol. Images were focused using the magnification on the lens set up at 1:1. Camera sensitivity was 200, the exposure F11, the shutter speed was 180, white balance was set on “auto,” and the flash was set up manually at 1/8 power. Image settings were .jpg, fine, large. Room lighting was always the same for each center, with only small variations from one study center to another. Once taken, photographs were not modified in any way.
Preparation of the Digital Corneal Images
Two sets of pictures were prepared. A training set containing 40 individual photographs picked from three time points: enrollment day, and 3 weeks and 3 months post-enrollment. A second set of 100 digital corneal photographs was used for analysis and evaluation. A total of 50 photographs were randomly chosen from the pool of 120 taken at enrollment as well as their corresponding ones from the 3-month follow-up visit. These 50 photographs provided approximately 80% power to detect a correlation of 0.4; 100 photographs provided power to detect a correlation of 0.3, thus the 100 photographs analyzed for this study were deemed sufficient to assess Optscore as a grading system. We chose to assess photographs of ulcers both at presentation and at 3 months in order to assess the ability of our system to accurately grade ulcers at different stages of healing. Ulcers or scars (of various sizes) were visible in 93 of the 100 pictures and involved the central area in 89% of cases. A hypopyon was visible in 10 pictures (all taken at enrollment) and 13 pictures showed some degree of neovascularization including eight enrollment pictures.
Outer and inner reference circles were superimposed on all photographs (Figure 1) within the Optscore program. The study coordinator marked the four cardinal points on the limbus. With these points defined, the Optscore software automatically superimposed the outer circle on each photograph outlining the outer limit of the cornea. An inner circle was then automatically applied with the same center for both circles. The diameter of the inner circle was one third of the diameter of the outer circle or an estimated 4mm, given an assumed average size of a cornea being approximately 12mm.12,13 These two circles served several purposes. The outer circle if assumed to have a diameter of 12mm allowed us to estimate the area, and compare this estimate to the area obtained during the clinical examination. Since corneal ulcers involving the visual axis are more likely to result in reduced visual acuity, it was important for our graders to be able to distinguish central from peripheral ulcers in a reproducible fashion with the help of the inner circle. The circumference of the outer circle was divided into 12 equal arcs and labeled from 1 to 12 as a clock face; these clock hours were counted to quantify an angular extent of corneal neovascularization and conjunctival inflammation (Figure 1). If by mistake the pictures were not taken at the same magnification, the computer automatically placed the correctly sized outer and inner reference circles.
Variables Analyzed
It should be noted that depending on the time point when the picture was taken if an ulcer or a scar was visible, we refer thereafter to both as ulcer. The following variables were assessed: area covered by the ulcer (calculated both in mm2 and as a percentage of the cornea); location and opacity of the ulcer; angular extent (clock hours) of corneal neovascularization (at all visible depths) and conjunctival inflammation (defined in this study as limbal inflammation) as well as presence or absence of a hypopyon (Table 1). To determine the area of the ulcer, graders used a computer mouse to outline the lesion with a digital cursor. The location of the ulcer was assessed in two ways. First, graders were given a standard choice by which they could describe the location of the ulcer (Table 1) with reference to whether or not the lesion involved the central circle, the periphery or both. Second, when graders outlined the lesion with a cursor to determine the area, Optscore automatically calculated the percent of the lesion within the central circle. Opacity was assessed by the ability of the graders to observe details of the anterior segment, iris, crystalline lens or intraocular lens, through the worst 50% of the opacity (Table 1).
TABLE 1.
Questions and possible answers for the variables evaluated in assessing Optscore software for fungal keratitis.
| Question | Possible answer | |
|---|---|---|
| Ulcer/scar visible? | Yes | No |
| Circle the area on picturea | Done | na |
| Location of the ulcer/scar |
|
na |
| Opacity of the ulcer/scar (worse 50%) |
|
na |
| Corneal neovascularization | From 0 to 12 clock hours | From 0 to 12 clock hours |
| Conjunctival inflammation | From 0 to 12 clock hours | From 0 to 12 clock hours |
| Hypopyon |
|
|
Once the area has been drawn on the picture, the software calculates automatically the percentage of the area that is within the inner circle.
na, not applicable
Steps of the Validation Study
Five second- and third-year Dartmouth medical students (graders A to E), in addition to a corneal specialist (gold standard), graded the photographs. The graders were all trained using a standard digital presentation, which contained information about the SCUT and MUTT studies, the variables to be assessed in Optscore, as well as the potential difficulties that could be encountered while grading pictures. This presentation remained available to the graders throughout the study. Upon completion of this training module, the graders graded the training set of 40 photographs during which time they could ask questions to the trainer (study coordinator) in order to make sure that they fully understood what was required of them. Having completed the training, the graders evaluated a set of 100 pictures twice between 2 and 7 weeks apart. All graders were masked to the clinical measurements of each of the patients whose photographs were used for this study.
A series of seven questions were asked for all evaluated photographs (Table 1). There was one screen per question. Answering one question would trigger the screen to change and show the next question. If the answer to the first question (“Is the ulcer/scar visible?”) was “yes”, the grader would be prompted to the next question which was to define the area of the ulcer/scar by drawing it, but if the answer was “no,” the next three questions directly related to the ulcer/scar were omitted and the grader was prompted directly to the question about corneal neovascularization.
Clinical Examination Data
We compared the results of photographic grading with the clinical examination of the patients. An estimated area was obtained during the clinical exam by measuring the longest dimension of the lesion and the length of the cord perpendicular to it. The area as determined by the clinical examination was approximated as the product of the longest diameter and the longest perpendicular to that diameter; the geometric mean is the square root of this pseudoarea and was used in the analysis.8 Best corrected visual acuity measurements were obtained after refraction using a protocol adapted from the Age Related Eye Disease Study using a tumbling E chart at 4- or 1m and logarithm of the minimum angle of resolution (logMAR) visual acuity.8
Statistical Analysis
We assessed intra- and intergrader agreement for the following variables: visibility of the ulcer, the square root of area (yielding a linear measure of the lesion size), the degree of neovascularization, the percent of the ulcer falling within the 4mm inner ring, the degree of opacity, the presence of hypopyon, and the ulcer location. We used one-way consistency intraclass correlation (ICC)14 to assess intragrader agreement, and two-way agreement ICC14 to assess intergrader agreement. In rare cases where no disagreements were observed between graders, confidence intervals (CIs) were constructed according to Nam.15 Thus, for each outcome variable, we computed (1) the intragrader consistency ICC for each of the six graders, (2) the intergrader agreement ICC comparing each student grader to the gold standard grader, and (3) the intergrader agreement ICC for all five student graders as a group (assuming random, rather than fixed, graders). Interpretation of intra- and intergrader agreement statistics was based on the table in Landis and Koch.16
Finally, validity was assessed by computing the Pearson correlation coefficient between the scar size as determined from photo ratings with the lesion dimensions as estimated from slit lamp examination (see8 for details). Note that the areas as estimated by slit lamp examination are determined by the longest diameter and longest perpendicular to it, an algorithm which is not expected to be in precise agreement with photographic ratings. The Pearson correlation was computed between the baseline logMAR visual acuity from the trial (see8 for details) and the photographically estimated area. Because of possible non-normality, we report bootstrap percentile CIs as well as the Spearman coefficient. We also determined whether the photographically determined area was a better predictor of visual acuity than the slit lamp-derived area using the Hotelling-Williams procedure.17 A Bland-Altman plot (with 95% limits) was also calculated to show agreement between the measurement of the size of the lesion by slit lamp and the graders (square root of the area determined by Optscore).
RESULTS
Intragrader Agreement
Intragrader agreements for each of the six graders were computed, and are shown in Table 2. For area, all graders achieved an ICC above 0.8, indicating “almost perfect” agreement,16 and the ICC was above 0.95 for four of the six graders. Similar results were obtained using the square root of area. All six graders achieved consistency ICCs in excess of 0.8 for hypopyon grading, percent in inner ring, degree of inflammation, and assessment of the visibility of the ulcer. For the case of location estimates, we found that five of the six graders (including the gold standard grader) achieved values above 0.8, while the remaining one was above 0.7. The lowest consistency occurred for assessments of the degree of neovascularization, where the gold standard grader ICC was 0.69, indicative of “substantial agreement”.16 All graders achieved ICCs above 0.6, except Grader D (0.59, indicating moderate agreement). No consistency ICC was estimated lower than 0.59 (Table 2).
TABLE 2.
Consistency intragrader intraclass correlation coefficients for grading of 100 randomly selected photos for fungal keratitis.
| Grader, ICC (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Variable | Gold standard | A | B | C | D | E |
| Opacity | 0.84 (0.77–0.89) | 0.67 (0.55–0.77) | 0.93 (0.90–0.96) | 0.79 (0.70–0.85) | 0.82 (0.74–0.88) | 0.93 (0.89–0.95) |
| Hypopyon | 0.89 (0.84–0.92) | 0.94 (0.91–0.96) | 0.89 (0.83–0.92) | 0.92 (0.88–0.94) | 0.86 (0.81–0.91) | 0.89 (0.84–0.92) |
| Location | 0.88 (0.83–0.92) | 0.82 (0.74–0.87) | 0.96 (0.94–0.97) | 0.75 (0.64–0.82) | 0.85 (0.79–0.90) | 0.82 (0.74–0.88) |
| Percent in inner circle | 0.95 (0.93–0.97) | 0.93 (0.90–0.95) | 0.96 (0.94–0.97) | 0.91 (0.87–0.94) | 0.92 (0.88–0.94) | 0.87 (0.82–0.91) |
| Inflammation | 0.90 (0.85–0.93) | 0.95 (0.93–0.97) | 0.96 (0.94–0.97) | 0.89 (0.85–0.93) | 0.91 (0.86–0.94) | 0.90 (0.86–0.93) |
| Neovascular-ization | 0.69 (0.57–0.78) | 0.70 (0.59–0.79) | 0.88 (0.82–0.92) | 0.73 (0.63–0.81) | 0.59 (0.45–0.71) | 0.77 (0.68–0.84) |
| Area | 0.96 (0.95–0.98) | 0.96 (0.94–0.98) | 0.90 (0.85–0.93) | 0.96 (0.93–0.97) | 0.81 (0.72–0.87) | 0.97 (0.96–0.98) |
| Area (transformed) | 0.96 (0.95–0.98) | 0.95 (0.93–0.97) | 0.95 (0.92–0.97) | 0.94 (0.91–0.96) | 0.85 (0.78–0.90) | 0.96 (0.93–0.97) |
| Ulcer visibility | 0.92 (0.88–0.94) | 0.90 (0.86–0.93) | 0.82 (0.75–0.88) | 1.0 (0.997–1.0)a | 1.0 (0.998–1.0)a | 0.88 (0.83–0.92) |
Both area and square root of the area are reported.
Conditional exact confidence interval.
CI, confidence interval; ICC, intraclass correlation coefficient
Agreement with Gold Standard
We computed the agreement ICC for each of the five student graders with the gold standard grader. Results are shown in Table 3. For area (transformed or not), each grader achieved an ICC above 0.8 in all cases, and all were above 0.95 except for grader D. For grading hypopyon and percent in inner circle, all five student graders achieved an ICC above 0.9, and for location and inflammation, all graders achieved an ICC above 0.8. This is indicative of “almost perfect” agreement. For the other outcome variables, all ICCs for agreement with the gold standard exceeded 0.6 for all graders, so that “substantial agreement” was achieved in all cases.
TABLE 3.
Agreement intraclass correlation coefficients for each grader compared to the gold standard for grading fungal keratitis.
| Grader, ICC (95% CI) | |||||
|---|---|---|---|---|---|
| Variable | A | B | C | D | E |
| Opacity | 0.86 (0.80–0.91) | 0.98 (0.97–0.98) | 0.77 (0.68–0.84) | 0.89 (0.84–0.93) | 0.85 (0.78–0.90) |
| Hypopyon | 0.92 (0.89–0.95) | 0.92 (0.88–0.94) | 0.95 (0.92–0.97) | 0.93 (0.90–0.96) | 0.97 (0.96–0.98) |
| Location | 0.91 (0.87–0.94) | 0.95 (0.92–0.96) | 0.86 (0.79–0.91) | 0.94 (0.92–0.96) | 0.87 (0.81–0.91) |
| Percent in inner circle | 0.94 (0.91–0.96) | 0.97 (0.95–0.98) | 0.91 (0.87–0.94) | 0.95 (0.93–0.97) | 0.92 (0.89–0.95) |
| Inflammation | 0.90 (0.85–0.94) | 0.85 (0.77–0.90) | 0.93 (0.89–0.95) | 0.86 (0.80–0.91) | 0.83 (0.72–0.89) |
| Neovascular-ization | 0.81 (0.73–0.87) | 0.81 (0.72–0.87) | 0.73 (0.63–0.81) | 0.63 (0.49–0.73) | 0.81 (0.73–0.87) |
| Area | 0.95 (0.92–0.96) | 0.96 (0.94–0.98) | 0.95 (0.86–0.98) | 0.85 (0.77–0.90) | 0.96 (0.94–0.97) |
| Area (transformed) | 0.94 (0.91–0.96) | 0.97 (0.95–0.98) | 0.92 (0.67–0.97) | 0.92 (0.87–0.95) | 0.96 (0.93–0.97) |
| Ulcer visibility | 0.86 (0.80–0.91) | 0.98 (0.97–0.98) | 0.77 (0.68–0.84) | 0.89 (0.84–0.93) | 0.85 (0.78–0.90) |
Both area and square root of the area are reported.
CI, confidence interval; ICC, intraclass correlation coefficient
Reliability of Student Graders as a Group
We assessed the reliability of the mean of the student graders by computing the agreement ICC for the collection of five graders, shown in Table 4. For all variables except for neovascularization, ICC values exceeded 0.9. For neovascularization, the agreement ICC was 0.76, indicating substantial agreement.
TABLE 4.
Agreement intraclass correlation coefficient to assess reliability of the trained graders as a group for grading of fungal keratitis.
| Variable | Mean of 5 student graders, ICC (95% CI) |
|---|---|
| Opacity | 0.86 (0.81–0.90) |
| Hypopyon | 0.92 (0.89–0.94) |
| Location | 0.90 (0.87–0.93) |
| Percent in inner circle | 0.93 (0.91–0.95) |
| Inflammation | 0.90 (0.87–0.93) |
| Neovascularization | 0.76 (0.69–0.81) |
| Area | 0.92 (0.89–0.94) |
| Area (transformed) | 0.93 (0.89–0.95) |
| Ulcer visibility | 0.87 (0.83–0.90) |
Both area and square root of the area are reported.
CI, confidence interval; ICC, intraclass correlation coefficient
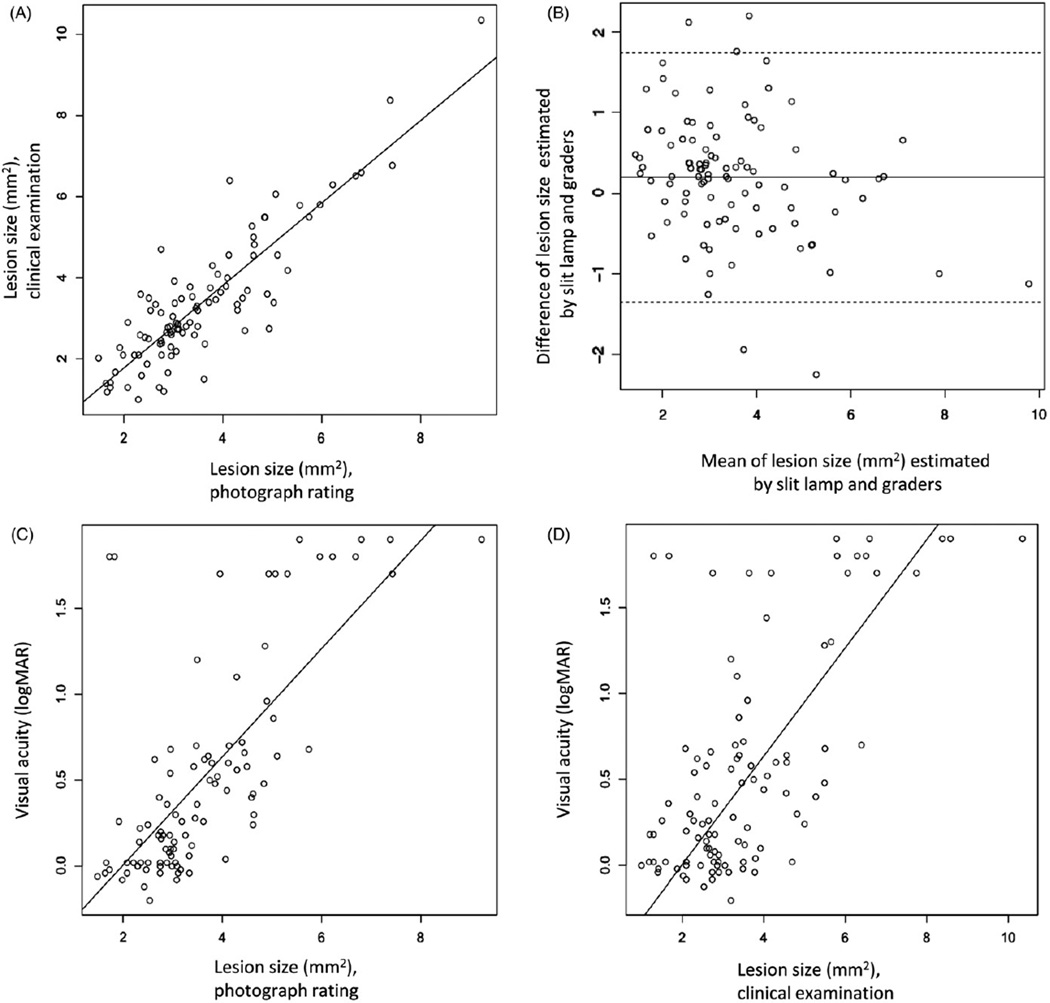
Comparison with Clinical Examination
The infiltrate/scar sizes estimated using slit lamp examination were highly correlated with the mean area determined by photograph grading, with a Pearson r of 0.88 (95% CI 0.79–0.93; Spearman r = 0.80, 95% CI 0.69–0.88; Figure 2A). The 95% limits of agreement using a Bland-Altman plot confirmed this correlation (Figure 2B). LogMAR visual acuity exhibited a correlation of 0.73 (Pearson) with the mean area determined by the graders (95% CI 0.57–0.85; Spearman r = 0.70, 95% CI 0.54–0.83; Figure 2C). By comparison, the correlation between logMAR visual acuity and slit lamp-derived area was smaller, with a Pearson correlation of 0.65 (95% CI 0.47–0.79, Spearman r = 0.54, 95% CI 0.36–0.69), a difference that was statistically significant (p = 0.03, Hotelling-Williams test; Figure 2D). Finally, the lesion size mean as measured at the slit lamp, by the gold standard and the five graders shows that all measurements are within the same limits (Table 5).
FIGURE 2.
(A) Scatterplot showing the relationship between areas of fungal keratitis determined by slit lamp and Optscore photographic grading (mean of five trained graders). The regression line is shown (Pearson r = 0.88, p < 0.0001). (B) Bland-Altman plot (with 95% limits) showing agreement between the measurement of the size of the lesion by slit lamp and the graders. (C) Visual acuity vs lesion size as determined by Optscore photographic grading (mean of five trained graders). The line shows the best fit linear regression (R2 = 0.52, p < 0.0001). (D) Visual acuity vs lesion size as determined by clinical examination. The line shows the best fit linear regression (R2 = 0.42, p < 0.0001). The regression line predicting visual acuity from Optscore-graded areas was significantly better than from areas determined by slit lamp (p = 0.03, Hotelling-Williams). 95% confidence (dotted line) is shown on all panels.
TABLE 5.
Comparison mean fungal keratitis scar size between graders.
| Grader/method | Mean scar size, mm (SD) |
|---|---|
| Slit lamp | 3.52 (1.74) |
| Gold standard | 3.61 (1.68) |
| Grader A | 3.52 (1.48) |
| Grader B | 3.49 (1.52) |
| Grader C | 4.01 (1.43) |
| Grader D | 3.50 (1.33) |
| Grader E | 3.68 (1.53) |
SD, standard deviation
DISCUSSION
We have presented data regarding the use of the Optscore computer program for grading digital corneal images for the MUTT and SCUT studies. Assessment of digital corneal photos at a reading center allows for less biased evaluation of corneal pathology by graders masked from clinical data, such as visual acuity, treatment and clinical history, associated with the corneal findings they are reviewing. This also means that the grader cannot always know whether the picture shows an active ulcer or a scar. The present work was designed to assess the reliability of this photography grading method using a randomly chosen sample of pictures taken at enrollment and 3-month follow-up visits, thus allowing us to work with a range of disease severity. For the variables of area, location, percent in inner circle, inflammation and hypopyon, ICCs >0.90 were achieved for the pooled student group (Tables 2–4). Opacity and ulcer visibility also had ICCs >0.8. ICCs >0.80 are considered to have excellent agreement. Corneal neovascularization showed the least consistency both in terms of intra- and inter-observer variation (Tables 2–4).
These data indicate that Optscore, as used in this study, is a reproducible method to evaluate corneal pathology by analyzing corneal images and does not depend on particular experts. This has the practical benefit of increasing the pool of potential graders for clinical studies and allows the inclusion of graders without preconceived notions about the pathology being assessed. We provide evidence that non-expert medical student graders can effectively evaluate corneal pathology (Tables 2–5) and averaging this group of newly trained graders provides clinically useful measurements of high reliability (Table 4).
We studied the correlation between calculated area using Optscore with the same assessment done by a treating physician at the slit lamp. The relationship between the Optscore generated area and presenting visual acuity was also investigated. A high degree of correlation between digital assessment and independent clinical exam as well as presenting visual acuity was found (Figure 2). As expected, a patient with a large ulcer area as graded in Optscore was highly likely to have a large ulcer as seen at the slit lamp by a treating physician and to have poor visual acuity. Optscore area grades were in fact more highly associated with visual acuity than were areas derived from clinical examination providing further evidence of a strong connection between Optscore measurements and the severity of corneal pathology.
Optscore builds on the contributions of previous studies. Similar to Optscore grading, both Mah-Sadorra and colleagues and Vital and colleagues in their retrospective studies emphasized the importance of ulcer size and location as predictors of clinical outcome.6,7 The study by Mukerji and co-authors18 reported that there was very little difference between two commonly used techniques to measure epithelial defects (area estimation of the area of an equivalent rectangle and use of Image Pro Plus image analysis software). Dastjerdi and co-authors19 measured three primary metrics for corneal neovascularization with digital slit lamp pictures. While prospective in nature and making extensive use of computational analysis of digital corneal photographs, this study focused on corneal neovascularization rather than corneal ulceration and did not have a separate study to validate this methodology. VanRoekel and colleagues20 presented an exploratory study assessing the area of 69 epithelial defects from digital slit-lamp pictures using Adobe Photoshop. The assessment performed by two physicians led to an excellent ICC of 0.99. This report represents a valuable demonstration of the reliability that can be obtained using digital methods to assess the area of anterior segment lesions. However, to our knowledge, it has not been tested in a larger patient cohort and the process has not been automated to facilitate its use for large numbers of photographs. Wilhelmus and co-authors21 analyzed calibrated scanned photographs of stromal keratitis patients from the Herpetic Eye Disease Study for size, location and density of stromal keratitis and endothelitis. This technique was validated with a high correlation coefficient (0.83) obtained after comparing clinical and computerized measurements. Both the Wilhelmus and VanRoekel studies analyzed corneal lesions of irregular shape.
We believe that Optscore contributes to past efforts at systematic grading of corneal ulcers. Digital corneal images can be loaded into Optscore without additional manipulation. Images and repeated images are presented in a random fashion to graders in a user-friendly format. Optscore’s computer graphic capabilities allow determination of the area of irregularly shaped lesions as well as calculation of the percentage of the lesion in the central cornea. Finally, the data is downloaded directly to a Microsoft Excel file facilitating rapid statistical analysis, making it valuable for large scale studies.
In sum, we have demonstrated that non-expert graders using Optscore to assess multiple variables in digital photographs of fungal keratitis are self-consistent, agree with the corneal expert grader both as a group and individually and that grading obtained from Optscore agrees with clinical measurements of the same patients (slit lamp assessment of area and visual acuity) leading us to conclude that the Optscore program is a valid method for assessing corneal pathology associated with fungal and potentially other microbial keratitis. Its ability to quantitatively assess the area and location of irregular corneal lesions is a valuable feature compared with many previously described corneal grading schemes. Finally, its reliability suggests that Optscore would be a valuable tool in the study of other corneal disorders.
Acknowledgments
The authors thank the patients in the Mycotic Ulcer Therapeutic Exploratory Trial and the five medical student graders. They also gratefully acknowledge the assistance of S. Chandra in creating the teaching presentation.
Financial support was provided by The National Eye Institute of the National Institutes of Health (Steroids for Corneal Ulcers Trial, U10-EY015114).
Footnotes
DECLARATION OF INTEREST
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- 1.Gómez-Ulla F, Fernandez MI, Gonzalez F, et al. Digital retinal images and teleophthalmology for detecting and grading diabetic retinopathy. Diabetes Care. 2002;25:1384–1389. doi: 10.2337/diacare.25.8.1384. [DOI] [PubMed] [Google Scholar]
- 2.Harding S, Broadbent DM, Neoh C, et al. Sensitivity and specificity of photography and direct ophthalmoscopy in screening for sight threatening eye disease: the Liverpool Diabetic Eye Study. BMJ. 1995;311:1131–1135. doi: 10.1136/bmj.311.7013.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kinyoun J, Martin DC, Fujimoto WY, Leonetti DL. Ophthalmoscopy versus fundus photographs for detecting and grading diabetic retinopathy. Invest Ophthalmol Vis Sci. 1992;33:1888–1893. [PubMed] [Google Scholar]
- 4.Harrison SM. Grading corneal ulcers. Ann Ophthalmol. 1975;7:537–539. 541–542. [PubMed] [Google Scholar]
- 5.Keay L, Edwards K, Dart J, Stapleton F. Grading contact-lens related microbial keratitis: relevance to disease burden. Optometry Vis Sci. 2008;85:531–537. doi: 10.1097/OPX.0b013e31817dba2e. [DOI] [PubMed] [Google Scholar]
- 6.Mah-Sadorra J, Yavuz SG, Najjar DM, et al. Trends in contact lens-related corneal ulcers. Cornea. 2005;24:51–58. doi: 10.1097/01.ico.0000138839.29823.57. [DOI] [PubMed] [Google Scholar]
- 7.Vital M, Belloso M, Prager TC, Lanier JD. Classifying the severity of corneal ulcers by using the “1, 2, 3” rule. Cornea. 2007;26:16–20. doi: 10.1097/ICO.0b013e31802b2e47. [DOI] [PubMed] [Google Scholar]
- 8.Prajna N, Mascarenhas J, Krishnan T, et al. Comparison of natamycin and voriconazole for the treatment of fungal keratitis. Arch Ophthalmol. 2010;128:672–678. doi: 10.1001/archophthalmol.2010.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Srinivasan M, Lalitha P, Mahalakshmi R, et al. Corticosteroids for bacterial corneal ulcers. Br J Ophthalmol. 2009;93:198–202. doi: 10.1136/bjo.2008.147298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Press W, Teukolsky SA, Vetterling WT, Flannery BP. The art of scientific computing. Cambridge: Cambridge University Press; 1992. Numerical recipes in C; p. 304. [Google Scholar]
- 11.Metropolis N, Ulam S. The Monte Carlo Method. J Am Statist Assoc. 1949;44:335–341. doi: 10.1080/01621459.1949.10483310. [DOI] [PubMed] [Google Scholar]
- 12.Hashemi H, KhabazKhoob M, Yazdani K, et al. White-to-white corneal diameter in the Tehran Eye Study. Cornea. 2010;29:9–12. doi: 10.1097/ICO.0b013e3181a9d0a9. [DOI] [PubMed] [Google Scholar]
- 13.Rüfer F, Schröder A, Erb C. White-to-white corneal diameter: normal values in healthy humans obtained with the Orbscan II topography system. Cornea. 2005;24:259–261. doi: 10.1097/01.ico.0000148312.01805.53. [DOI] [PubMed] [Google Scholar]
- 14.McGraw KO, Wong SP. Forming inferences about some intraclass correlation coefficients. Psycholog Meth. 1996;1:30–46. [Google Scholar]
- 15.Nam J. Interval estimation of the kappa coefficient with binary classification and an equal marginal probability model. Biometrics. 2000;56:583–585. doi: 10.1111/j.0006-341x.2000.00583.x. [DOI] [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 17.Dunn OJ, Clark V. Comparison of tests of the equality of dependent correlation coefficients. J Am Statist Assoc. 1971;66:904–908. [Google Scholar]
- 18.Mukerji N, Vajpayee RB, Sharma N. Technique of area measurement of epithelial defects. Cornea. 2003;22:549–551. doi: 10.1097/00003226-200308000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Dastjerdi M, Al-Arfaj KM, Nallasamy N, et al. Topical bevacizumab in the treatment of corneal neovascularization: results of a prospective, open-label, noncomparative study. Arch Ophthalmol. 2009;127:381–389. doi: 10.1001/archophthalmol.2009.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.VanRoekel R, Bower KS, Burka JM, Howard RS. Anterior segment measurements using digital photography: a simple technique. Optom Vis Sci. 2006;83:391–395. doi: 10.1097/01.opx.0000221404.40296.ba. [DOI] [PubMed] [Google Scholar]
- 21.Wilhelmus K, Mitchell BM, Dawson CR, et al. Slitlamp biomicroscopy and photographic image analysis of herpes simplex virus stromal keratitis. Arch Ophthalmol. 2009;127:161–166. doi: 10.1001/archophthalmol.2008.577. [DOI] [PubMed] [Google Scholar]