Abstract
Background: Attention has recently focused on posttraumatic stress disorder (PTSD) among individuals with traumatic spinal cord injury (SCI). Purpose: To examine characteristics of individuals with and without symptoms of PTSD following acute SCI. Methods: Data were collected on 23 patients (age, 34.5 ± 14.4 years) at a Level I trauma center (14.35 ± 18.48 days following injury). Results: There were 52.2% (n = 12) who experienced symptoms of PTSD post injury, with a significant association in patients with a history of psychological disorders (p = .0094). Conclusion: Findings suggest that patients with SCI who present with PTSD symptoms in the acute trauma care settting should be provided with specific cognitive behavioral interventions.
Keywords: acute, injuries, psychological, rehabilitation, stress disorders
There are approximately 12,500 new cases of spinal cord injury (SCI) in the United States each year, with an estimated 276,000 Americans currently living with SCI.1 Etiology of traumatic SCI occurs most frequently from motor vehicle collisions (36.5%), but also results from falls and violence (eg, gunshot wounds); all of these incidents can be considered psychologically traumatic (eg, event causing the injury, realizing one's inability to move, witnessing another person's death or injury during the event).2 Severity and level of injury dictate the degree of functional impairment, but many people often experience psychological changes, with depression being the most studied.3,4 However, attention has begun to be directed to other psychological consequences of injury, including posttraumatic stress disorder (PTSD).
PTSD is classified as a “Trauma and Other Stress Related Disorder” in the DSM-55 and occurs when a person either witnesses or experiences a life-threatening event and characteristic symptom clusters develop, including arousal, avoidance, re-experiencing, and changes in cognition and mood. While it is recognized that PTSD is diagnosable 30 days or longer after the initial trauma, the American College of Surgeons Committee on Trauma (ACS-COT) recently recommended screening for PTSD symptoms during the acute phase of trauma because of the link to long-term psychological issues,6,7 inability to return to work,8 and increased health care and societal costs.9 PTSD is an issue for individuals following SCI who have been shown to have higher rates than other similar populations who experience trauma. Specifically, findings have indicated a high incidence of PTSD among individuals after injury in the United States (20%–40%)10,11 and Veterans undergoing inpatient rehabilitation (44% diagnosed within 2 days of admission).12
To our knowledge, no studies have examined PTSD symptoms in individuals with SCI while in an acute trauma care setting. Although the substantial economic impacts of SCI are well known,1 the psychological impact of acute SCI requires further examination,13 as it may further exacerbate the functional and emotional impairments and quality of life14 of individuals with SCI. Subsequently, identification of symptoms of PTSD in an acute trauma care setting may be important in reducing the future negative impact of symptom development. Therefore, the purpose of this brief report is to describe preliminary findings on rates and characteristics of PTSD in individuals with SCI with and without symptoms in an acute trauma care setting.
Methods
Procedure
Approval to complete the study was obtained from the hospital's institutional review board. Individuals were recruited from a large, urban Level I trauma center that admits approximately 2,500 patients annually. Patients were screened using trauma service admission lists and chart reviews and by attending bi-weekly trauma rounds. Patients who met inclusion criteria were approached more than 24 hours after admission.
Participants
Participants in the current analysis were part of a larger prospective observational cohort study (N = 469) including patients who had experienced acute traumatic injury (eg, motor vehicle collision, violent crime) between 2012 and 2014. There were 84 individuals who met inclusion criteria but declined to participate, accounting for an 85% acceptance rate. Of the 469 subjects enrolled, a subset of 23 had experienced a traumatic injury involving their spinal cord (ICD-9 code 806 and/or 952)15 and were included in the current analyses. Inclusion criteria consisted of age 18 years and older, admission to the Level I trauma center for at least 24 hours with acute SCI, medically stable, English-or Spanish-speaking, and meeting the trauma registry injury criteria determined by the ACS-COT Resources for Optimal Care of the Injured Patient.9 Cognitive deficits were assessed through chart review prior to approaching patients for participation. Patients with cognitive deficits that impaired their ability to provide informed consent and persisted throughout their length of stay were excluded from the study. Participants then completed standardized questionnaires with the research coordinator during their initial hospital admission.
Measures
Variables collected during hospitalization included (a) demographic characteristics (age, gender, ethnicity), (b) injury-related variables extracted from the trauma registry (cause of injury, Glasgow Coma Scale [GCS] score,16 Injury Severity Scale [ISS] score,17 and American Spinal Injury Association Impairment Scale [AIS] score),18 and (c) symptoms of PTSD.
Symptoms of PTSD were measured using the Primary Care PTSD (PC-PTSD) screen,19 which assesses the underlying characteristics specific to PTSD: re-experiencing, numbing, avoidance, and hyperarousal. The PC-PTSD is designed for use in medical settings and is the current screening instrument used in the Veterans Affairs (VA) centers; it is recommended as the most practical tool for screening PTSD.20 It has been used specifically in patients with SCI12 and has been shown to be comparable with longer assessments of PTSD in the trauma center setting, with a sensitivity of 72.4% and specificity of 93.4% when compared with the PTSD Checklist – Civilian Version 17-item screen.21 The PC-PTSD consists of 4 “yes or no” items, with scores ranging from 0 to 4. Because of the early time point of the first symptom assessment in the current study (acute hospital admission), a score of 3 or higher on the PC-PTSD was considered a positive screen for clinical levels of PTSD symptoms. With a cutoff score of 3 for diagnosis, the PC-PTSD has shown 85% diagnostic efficiency, 78% sensitivity, and 87% specificity among VA clinic patients.19 In the PC-PTSD screen, individuals are asked “in [their] life, have [they] ever had any experience that was so frightening, horrible or upsetting that in the past month” that they had trouble re-experiencing it (eg, nightmares, flashbacks), numbing feelings (eg, feeling detached), avoidance (eg, tried not to think about it, avoided situations), and hyperarousal (eg, constantly on guard).
Data analysis
Descriptive analysis was completed for all 23 participants including frequencies, means, standard deviations, and percentages. To compare differences in demographic and injury-related data between individuals with and without PTSD symptoms, Wilcoxon tests were calculated for continuous variables and Fisher's exact tests for categorical variables.
Results
Twenty-three participants with an SCI were included in the analysis. Demographic and injury-related information is reported in Table 1. There were an average of 14.35 days between date of injury and date of screening (SD = 18.48), with variance attributed to long intensive care unit length of stays before patients were medically stable and eligible to be enrolled into the study. Of the sample, 39% reported being diagnosed or treated for a premorbid psychological disorder (eg, depression, anxiety, PTSD, obsessive-compulsive disorder, phobia, schizophrenia) in the past. Further, PTSD symptoms were identified in 52.2% (n = 12) of the sample during acute hospitalization.
Table 1.
Summary of injury-related information (N=23)
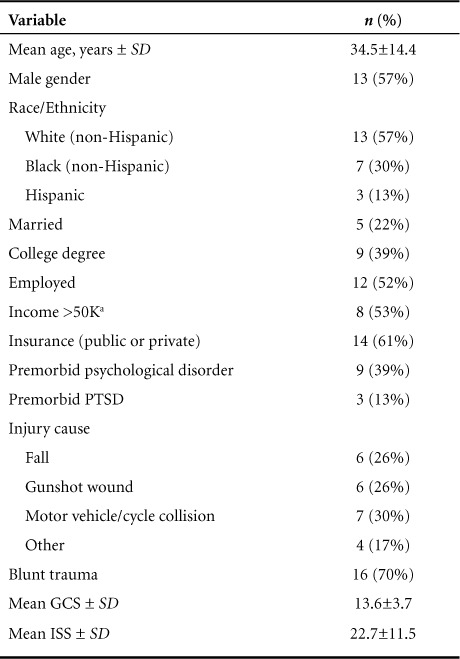
Table 1.
Summary of injury-related information (N=23) (CONT.)
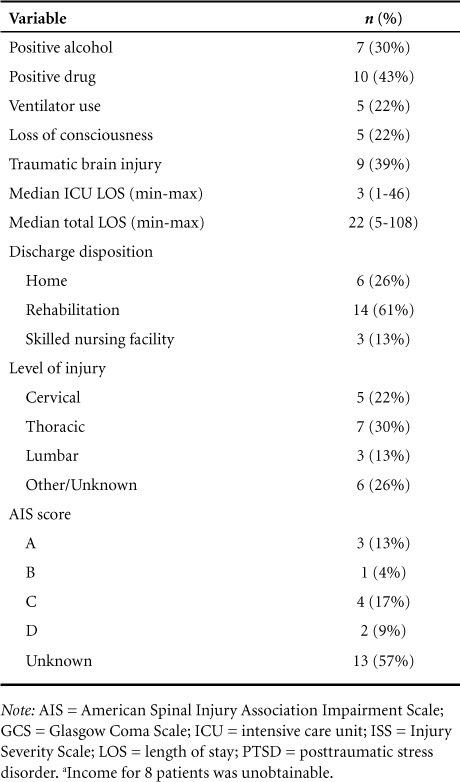
Analysis indicated that individuals with premorbid psychological disorders were significantly more likely to experience PTSD symptoms following SCI (n = 8; p < .01). Further, of the 12 individuals with PTSD symptoms, 6 of those also had a diagnosed traumatic brain injury. None of the remaining associations were significant.
Discussion
To our knowledge, this study is among the first to examine PTSD symptoms in individuals with SCI in an acute trauma care setting. Several findings warrant further discussion and investigation. First, 13% of the current sample reported premorbid PTSD, which is considerably higher than the 6.8% reported by the general population.22 Analysis was completed with and without these 3 individuals, with no difference determined. While this may be reflective of the small sample size, it warrants further investigation and possible recommendations of screening for premorbid PTSD in those with SCI. Second, the high incidence of PTSD symptoms following SCI (52.2%) suggests screening is important because individuals post SCI with PTSD have poorer health outcomes (eg, return to work) than individuals without PTSD.23 Although these symptoms can be normative to some degree after a trauma and may resolve on their own in some patients, it is not clear in the immediate post injury phase who will and will not benefit from intervention. Thus, early diagnosis of PTSD symptoms is imperative as there is evidence that PTSD has a better prognosis if clinical intervention is implemented early (within the first month).24 For example, evidence-based approaches to treatment including cognitive processing therapy and prolonged exposure24,25 can be modified to be applicable during the trauma center setting as early as in the emergency room26 and to continue through inpatient rehabilitation or into an outpatient setting.
As length of stay in the acute care unit for patients with SCI has declined from an average of 24 days to 11 days, early identification of PTSD symptoms is critical.1 This is emphasized by the fact that the ACS-COT23 now recommends that trauma centers have a psychologist/psychiatrist on staff to screen for mental health disorders, including PTSD, at the time of presentation to the acute trauma care setting.6
Due to the relationship between PTSD and chronic health conditions, it is important to identify and treat symptoms early in the rehabilitation process. The Chronic Care Model27 provides a framework to support the successful management of long-term conditions through (a) increasing patient activation through education, greater motivation, and improved skill-set during rehabilitation; (b) redesigning the health care system and continuum of care to enable proactive and productive patient-provider interactions; (c) supporting providers to maximize patient adherence to evidence-based practice; and (d) implementing information systems that provide timely data. In the context of the current results, this would be achieved by (a) screening, treating, and educating patients appropriately following admission to the acute trauma care setting and across the continuum of care; (b) having a team of psychologists that work collaboratively across the continuum; (c) using evidence-based approaches for the treatment of PTSD, and (d) ensuring that diagnosis and treatment plans are effectively communicated between settings and providers.
Limitations in the current pilot study analysis include a small sample size, however future efforts will continue within the Level I trauma center to target the 51 patients on average that are admitted annually with an SCI diagnosis. Another limitation is the use of a screener to identify symptoms of PTSD in an acute care setting rather than a full evaluation and diagnosis and that the PC-PTSD screen does not ask individuals if the experience they are referencing is the event that led to their injury. However the current analysis follows recommendations by the ACS-COT to screen for symptoms of PTSD in the acute care setting to address concerns early in the hospitalization to prevent issues in the long-term. Additionally, the strategy of identifying individuals with symptoms of PTSD within 30 days of traumatic injury is consistent with previous research.28 Future research should include another measure, such as the Life Events Checklist for DSM-5,29 in order to better examine and control for traumatic events in participants' lives other than their injuries. Lastly, prevalence of PTSD symptoms among patients who were ineligible for the pilot study (eg, cognitive deficits) is unknown.
These preliminary findings suggest that individuals with SCI may have a high incidence of PTSD symptoms in the acute trauma care setting, especially among those with a history of premorbid psychological disorders. While the link between PTSD symptoms in trauma and psychological disorders at different stages of the rehabilitation process should continue to be explored among a larger sample, current results suggest the importance of early screening for PTSD symptoms in an acute trauma care setting. Future implications include developing prevention strategies during acute hospitalization if results are replicated in larger studies.
Acknowledgments
Funding for this study was provided by the Stanley Seeger Fund of the Baylor Health Care System Foundation to the first author and principal investigator of the study (Warren). Support from this grant was also provided to Reynolds and Bennett. For the other authors, no conflicts were declared. The authors gratefully acknowledge the generosity of the Stanley Seeger Surgical Fund of the Baylor Health Care System Foundation for their full support to this study.
REFERENCES
- 1.Spinal Cord Injury Model Systems. Spinal cord injury (SCI) facts and figures at a glance. https://www.nscisc.uab.edu/reports.aspx. Updated August 2014. Accessed March 13, 2015.
- 2.Otis C, Marchand A, Courtois F. Risk factors for posttraumatic stress disorder in persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2012;18(3):253–263. doi: 10.1310/sci1803-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elliott TR, Frank RG. Depression following spinal cord injury. Arch Phys Med Rehabil. 1996;77(8):816–823. doi: 10.1016/s0003-9993(96)90263-4. [DOI] [PubMed] [Google Scholar]
- 4.Tate DG, Forchheimer M, Bombardier CH, Heinemann AW, Neumann HD, Fann JR. Differences in quality of life outcomes among depressed spinal cord injury trial participants. Arch Phys Med Rehabil. 2015;96(2):340–348. doi: 10.1016/j.apmr.2014.09.036. [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 6.Warren A, Marie, Stucky K, Sherman JJ. Rehabilitation psychology's role in the level I trauma center. J Trauma Nurs. 2014;21(3):139–145. doi: 10.1097/TA.0b013e3182858ab9. [DOI] [PubMed] [Google Scholar]
- 7.Osenbach JE, Lewis C, Rosenfeld B et al. Exploring the longitudinal trajectories of posttraumatic stress disorder in injured trauma survivors. Psychiatry Interpers Biol Process. 2014;77(4):386–397. doi: 10.1521/psyc.2014.77.4.386. [DOI] [PubMed] [Google Scholar]
- 8.Zatzick D, Jurkovich GJ, Rivara FP et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–437. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 9.American College of Surgeons. Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 10.Zatzick DF, Rivara FP, Nathens AB et al. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychol Med. 2007;37(10):1469–1480. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]
- 11.Shih R, Schell T, Hambarsoomian K, Marshall G, Belzberg H. Prevalence of PTSD and major depression following trauma-center hospitalization. J Trauma Acute Care Surg. 2010;69(6):1560. doi: 10.1097/TA.0b013e3181e59c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ullrich PM, Smith BM, Poggensee L et al. Pain and post-traumatic stress disorder symptoms during inpatient rehabilitation among operation enduring Freedom/Operation Iraqi Freedom veterans with spinal cord injury. Arch Phys Med Rehabil. 2013;94(1):80–85. doi: 10.1016/j.apmr.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Duff J, Kennedy P. Handbook of Clinical Health Psychology. Chichester, UK: Wiley; 2003. Spinal cord injury; pp. 251–275. [Google Scholar]
- 14.Davidson JRT. Trauma: The impact of post-traumatic stress disorder. J Psychopharmacol. 2000;14(2):S5–S12. doi: 10.1177/02698811000142S102. [DOI] [PubMed] [Google Scholar]
- 15.National Center for Health Statistics. Classifications of diseases and injuries. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Publications/ICD-9/ucod.txt. Updated 2002.
- 16.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 17.Baker SP, O'Neill B, Haddon WJ, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 18.Burns S, Biering-Sørensen F, Donovan W et al. International standards for neurological classification of spinal cord injury, revised 2011. Topics Spinal Cord Inj Rehabil. 2012;18(1):85–99. doi: 10.1310/sci1801-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prins A, Ouimette P, Kimerling R et al. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Prim Care Psychiatry. 2003;9(1):9–14. [Google Scholar]
- 20.Davis SM, Whitworth JD, Rickett K. Clinical inquiries. What are the most practical primary care screens for post-traumatic stress disorder? J Fam Pract. 2009;58(2):100–101. [PubMed] [Google Scholar]
- 21.Hanley J, deRoon-Cassini T, Brasel K. Efficiency of a four-item posttraumatic stress disorder screen in trauma patients. J Trauma Acute Care Surg. 2013;75(4):722–727. doi: 10.1097/TA.0b013e3182a53a5f. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 23.American College of Surgeons. Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2014. [Google Scholar]
- 24.Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. [Google Scholar]
- 25.Institute of Medicine. Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, DC: National Academies Press; 2008. [Google Scholar]
- 26.Rothbaum BO, Kearns MC, Price M et al. Early intervention may prevent the development of posttraumatic stress disorder: A randomized pilot civilian study with modified prolonged exposure. Biol Psychiatry. 2012;72(11):957–963. doi: 10.1016/j.biopsych.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wagner E. Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2–4. [PubMed] [Google Scholar]
- 28.Hanley J, deRoon-Cassini T, Brasel K. Efficiency of a four-item posttraumatic stress disorder screen in trauma patients. J Trauma Acute Care Surg. 2013;75(4):722–727. doi: 10.1097/TA.0b013e3182a53a5f. [DOI] [PubMed] [Google Scholar]
- 29.Weathers F, Blake D, Schnurr P, Kaloupek D, Marx B, Keane T. The Life Events Checklist for DSM-5 (LEC-5) Instrument available from the National Center for PTSD at www.ptsd.va.gov.


