Abstract
Background:
Eccentric exercise is commonly used in the management of Achilles tendinopathy (AT) but its effectiveness for insertional AT has been questioned. Soft tissue treatment (Astym) combined with eccentric exercise could result in better outcomes than eccentric exercise alone.
Hypothesis:
Soft tissue treatment (Astym) plus eccentric exercise will be more effective than eccentric exercise alone for subjects with insertional AT.
Study Design:
Prospective randomized controlled trial.
Level of Evidence:
Level 2.
Methods:
Sixteen subjects were randomly assigned to either a soft tissue treatment (Astym) and eccentric exercise group or an eccentric exercise–only group. Intervention was completed over a 12-week period, with outcomes assessed at baseline, 4, 8, 12, 26, and 52 weeks. Outcomes included the Victorian Institute of Sport Assessment Achilles-Specific Questionnaire (VISA-A), the numeric pain rating scale (NPRS), and the global rating of change (GROC).
Results:
Significantly greater improvements on the VISA-A were noted in the soft tissue treatment (Astym) group over the 12-week intervention period, and these differences were maintained at the 26- and 52-week follow-ups. Both groups experienced a similar statistically significant improvement in pain over the short and long term. A significantly greater number of subjects in the soft tissue treatment (Astym) group achieved a successful outcome at 12 weeks.
Conclusion:
Soft tissue treatment (Astym) plus eccentric exercise was more effective than eccentric exercise only at improving function during both short- and long-term follow-up periods.
Clinical Relevance:
Soft tissue treatment (Astym) plus eccentric exercise appears to be a beneficial treatment program that clinicians should consider incorporating into the management of their patients with insertional AT.
Keywords: Achilles, tendinopathy, soft tissue treatment (Astym), eccentrics
Achilles tendinopathy (AT) is a clinical syndrome characterized by pain, swelling, and impaired function.41 It is the most common cause of posterior heel pain, and runners have the greatest risk of developing AT with a prevalence of 11% to 18%.16,23,36 Whereas runners represent the group most likely to develop AT, it can also occur in other athletes and sedentary individuals.21,22
Achilles tendinopathy is typically classified as either insertional or midportion based on the location of pain. Insertional AT causes pain at or near the point where the Achilles tendon attaches to the posterior calcaneus, while midportion AT causes pain 2 to 7 cm proximal to the calcaneal attachment.41 Insertional AT is responsible for between 20% and 25% of cases.8,13,19
Eccentric exercise is the most recommended conservative treatment in the management of AT.1,23,29,30,39,40 The outcomes after treatment with eccentric exercise have varied significantly between insertional and midportion AT. For midportion AT, success rates have ranged from 56% to 89%.9,33 For insertional AT, the results have been significantly less favorable with success rates between 28% and 32%.9,32 Because of the poor outcomes associated with insertional AT and eccentric exercise, a modified eccentric protocol that eliminated loading into dorsiflexion was developed.18 In 1 study with no control group, a 67% success rate was reported.18
Soft tissue mobilization is a recommended treatment in the management of tendinopathies, though there is limited evidence supporting this approach.11,20,28 Astym (Performance Dynamics) is a specialized soft tissue treatment that utilizes handheld instruments to transfer pressure and shear stress to underlying soft tissue.7 Astym treatment may induce regeneration and remodeling of soft tissue through activation of fibroblasts by means of the endogenous release of cellular mediators and growth factors.35 Increased fibroblast recruitment and activation as well as the production of fibronectin have followed Astym treatment in rat tendons, but this has not been studied in humans.6,12,34 As soft tissue treatment (Astym) and eccentric exercise both appear to effect tendon healing, it seems possible that the combination of the 2 treatments may result in better outcomes than eccentric exercise alone.24,25
A recent randomized controlled trial reported that Astym therapy, stretching, and eccentric exercise were more effective than stretching and eccentric exercise alone for subjects with lateral elbow tendinopathy.35 Therefore, the purpose of this study was to compare the outcomes between eccentric exercise only and eccentric exercise plus soft tissue treatment (Astym) for subjects with insertional AT.
Methods
This study was approved by the institutional review boards at Rocky Mountain University of Health Professions and Indiana University Health Ball Memorial Hospital. All subjects signed an informed consent form prior to participation, and the rights of all subjects were protected. The study was registered at clinicaltrials.gov (NCT01988155).
Subjects
Sixteen subjects older than 18 years with insertional AT participated in this study. The following were the inclusion criteria: diagnosis of insertional AT with a primary complaint of posterior heel pain, symptom duration of at least 6 weeks, and a VISA-A score of ≤78. Insertional AT was clinically determined by the primary investigator (J.R.M.) using the following criteria: pain at or within 2 cm of the posterior calcaneal insertion of the Achilles tendon along with localized tenderness and a subjective report of decreased activity levels secondary to Achilles pain.9,32 Exclusion criteria were: prior treatment with eccentric exercise or Astym for AT, anticoagulant medication, previous Achilles surgery on the involved side, bilateral symptoms, workers’ compensation or liability cases, peripheral neuropathy, pregnancy, lumbar radiculopathy, and inability to complete the required outcomes forms or comply with the recommended treatment regimen.
Prior to the start of subject recruitment, an individual not involved with the study used a random number generator to assign subjects to a treatment group. Group assignments were then placed in sequentially numbered and sealed opaque envelopes. An envelope was opened only once the corresponding subject agreed to enter the study.
Outcomes
The primary outcome was the Victorian Institute of Sport Assessment Achilles-Specific Questionnaire (VISA-A).31 The VISA-A is a self-administered questionnaire used to evaluate the severity of AT. It has previously been shown to be valid, reliable, and clinically relevant.14,31 VISA-A scores can range from 0 to 100, with higher scores considered better.
The secondary outcome was a self-administered 3-part numeric pain rating scale (NPRS). Subjects were asked to indicate their “worst pain” and “best pain” in the previous 24 hours in addition to their “current pain.” The average of all 3 was utilized as a subject’s score. The NPRS has been shown to be valid and reliable for individuals with musculoskeletal conditions.2,17,26,37
A 15-point Global Rating of Change scale (GROC)15 questionnaire was completed by subjects at the 12-week follow-up period. Subjects with scores of +5 or higher were considered to have experienced a successful outcome.3-5,27,38
Procedures
Baseline and demographic data including age, sex, duration of symptoms, height, weight, smoking status, presence of diabetes mellitus, and heel lift usage were collected. Initial scores on the NPRS and VISA-A were recorded at the first visit. Follow-up outcomes were obtained at 4, 8, and 12 weeks after initiation of treatment for the short-term portion of the study. Long-term outcomes were obtained at 26 and 52 weeks after the initiation of treatment. Subjects were given the option to complete and return their outcomes by mail or to come to the clinic to complete them in person.
Interventions
Subjects in both groups were instructed to perform the modified eccentric protocol (Figure 1).18 Subjects performed 3 sets of 15 repetitions per session and performed 2 sessions per day for a total of 12 weeks. In the event that a subject was unable to complete 3 sets of 15 repetitions, the subject was instructed to start with a lower number of repetitions and/or sets (a minimum of 2 sets of 10) and progress to the full amount as able. Subjects in both groups were instructed to avoid activities such as running for at least the first 4 weeks of treatment, but they could resume activities as tolerated after 4 weeks.
Figure 1.
Eccentric exercise as performed in current study for a subject with right side insertional Achilles tendinopathy. Step 1: Perform heel raise with unaffected leg; step 2: Transfer weight to affected leg; step 3: Slowly lower heel of affected leg to floor.
In addition to performing the eccentric protocol, subjects in the soft tissue treatment (Astym) group were seen in the clinic 2 times per week for 12 visits. Soft tissue treatment (Astym) was performed per the foot, ankle, and knee protocol.34 During each treatment session, a progression of instruments with decreasing areas of surface contact was used (Figures 2 and 3).10,34 Each treatment session lasted approximately 20 to 30 minutes.
Figure 2.

Astym instruments.
Figure 3.
Astym treatment.
To control for the effect of regular contact with a therapist, subjects in the control group were contacted by telephone once per week to discuss their progress with the program, encourage compliance, and address any questions.
Statistical Analysis
For the purpose of a power analysis, the smallest reported minimal clinically important difference (MCID) on the VISA-A of 12 points14 was selected to be the minimum between-group difference that would be considered significant. For subjects with insertional AT, the standard deviation in VISA-A scores after completion of an eccentric exercise program was 12 points.32 An a priori power calculation using an alpha of 0.05, an effect size index of 1.0, and power of 0.90 was performed, and a total sample size of 12 was recommended.
Statistical analyses were performed using SPSS Version 22.0 (IBM). Independent t tests (or chi-square tests for independence in the case of dichotomous data) were used to compare groups at baseline. Mixed-model (4 × 2) analyses of variance (ANOVAs) were used to analyze short-term VISA-A and NPRS scores. Correlation testing (Pearson for continuous variables and point-biserial for dichotomous variables) was performed to determine whether sex, body mass index, age, heel lift usage, or the presence of diabetes mellitus were significantly correlated with any of the dependent variables. The percentage of subjects in each group who achieved at least 1 MCID improvement on the VISA-A at 12 weeks and the percentage of subjects in each group who achieved a successful outcome at 12 weeks were compared using chi-square tests for independence. Additional mixed-model (3 × 2) ANOVAs, using 12 weeks as the baseline, were used to analyze long-term VISA-A and NPRS scores.
Results
Short-term Outcomes
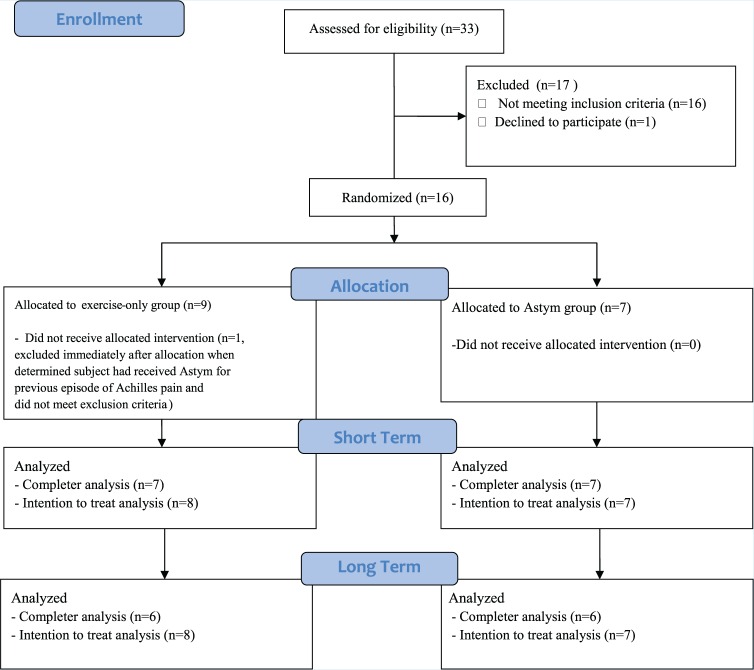
Both groups were considered similar at baseline (Table 1). A total of 16 subjects were enrolled, and 15 subjects completed the short-term portion of the study (Figure 4). One subject was excluded from the study immediately after enrollment because he had previously received Astym for an earlier episode of AT. Of the remaining 15 subjects, 14 completed their outcomes at all of the required time points and were included in the final analysis. One subject in the exercise group completed only the baseline and 12-week outcomes so his or her data could not be included in the final ANOVA. However, an intention to treat analysis (ITT) was performed using the multiple imputation method for missing data in a separate ANOVA. None of the baseline criteria were significantly correlated with baseline to 12-week change scores on the VISA-A or NPRS. No adverse effects were noted in either group.
Table 1.
Baseline demographics and clinical characteristics of subjects
| Exercise (n = 9) | Astym (n = 7) | P Value | |
|---|---|---|---|
| Sex, M/F | 3/6 | 2/5 | 0.84 |
| Age, y, mean (range) | 53.9 (42-69) | 53.3 (38-69) | 0.80 |
| Duration, wk | 20.8 | 21.9 | 0.87 |
| BMI, kg/m2, mean | 36.6 | 37.3 | 0.89 |
| Heel lift users, n | 2 | 2 | 0.77 |
| Smoker, n | 1 | 0 | 0.36 |
| Diabetes, n | 2 | 1 | 0.69 |
| VISA-A (SD) | 40.2 (17.3) | 36.6 (19.3) | 0.70 |
| NPRS (SD) | 5.4 (2.3) | 4.6 (1.9) | 0.47 |
BMI, body mass index; F, female; M, male; NPRS, numeric pain rating scale; VISA-A, Victorian Institute of Sport Assessment Achilles-Specific Questionnaire.
Figure 4.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram.
Victorian Institute of Sport Assessment Achilles-Specific Questionnaire
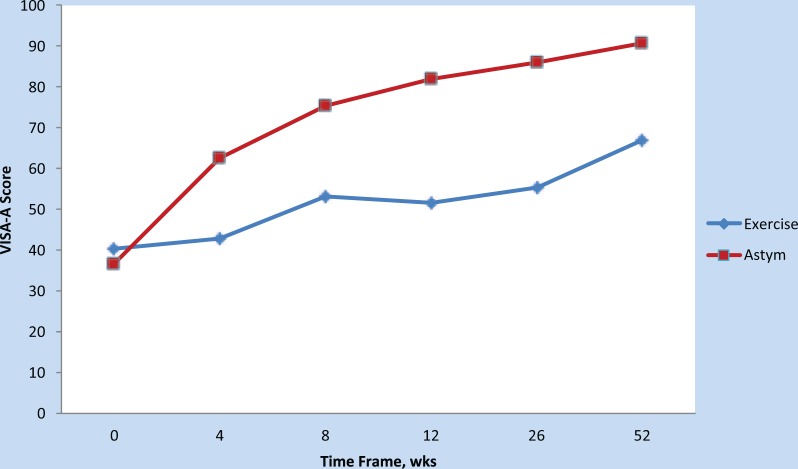
There was a significant interaction effect with greater improvements (P = 0.02) seen in the soft tissue treatment (Astym) group on the VISA-A (Figure 5). The ITT analysis yielded similar results.
Figure 5.
Mean Victorian Institute of Sport Assessment Achilles-Specific Questionnaire (VISA-A) scores at baseline and each follow-up period.
A significantly greater (P = 0.01) number of subjects in the soft tissue treatment (Astym) group (7/7, 100%) achieved at least 1 MCID improvement on the VISA-A at 12 weeks compared with the exercise group (3/8, 38%). For subjects receiving soft tissue treatment (Astym) and eccentric exercise, the number needed to treat (NNT) to prevent 1 subject from not achieving at least 1 MCID improvement was 2.
Numeric Pain Rating Scale
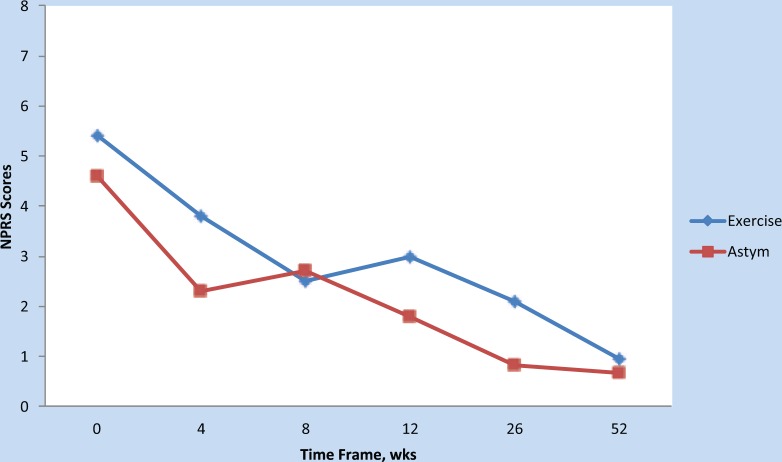
A significant main effect (P = 0.03) of time was found (Figure 6), but the between-group difference was not significant. The ITT analysis yielded similar results.
Figure 6.
Mean numeric pain rating scale (NPRS) scores at baseline and each follow-up period.
Global Rating of Change
A significantly greater (P = 0.03) number of subjects in the soft tissue treatment (Astym) group (7/7, 100%) achieved a successful outcome at 12 weeks compared with the exercise group (4/8, 50%). For subjects receiving soft tissue treatment (Astym) and eccentric exercise, the NNT to prevent 1 subject from not achieving a successful outcome was 2.
Long-term Outcomes
At the 26- and 52-week follow-up periods, 12 subjects completed all of the required outcomes and were included in the final analyses. All 15 subjects provided at least partial data for the long-term follow-up periods and were included in the ITT analyses.
Victorian Institute of Sport Assessment Achilles-Specific Questionnaire
A significant main effect for group was found (P < 0.01) in favor of the soft tissue treatment (Astym) group (Table 2). The ITT analysis yielded similar results.
Table 2.
VISA-A values at baseline and follow-upa
| Baseline | 4 wk | 8 wk | 12 wk | 26 wk | 52 wk | |
|---|---|---|---|---|---|---|
| Exercise | 40.2 (26.7-53.7) | 42.7 (22.1-63.3) | 53 (28.3-77.7) | 51.5 (33.2-69.8) | 55.3 (38.4-72.2) | 67 (52.8-81.2) |
| Astym | 36.6 (18.8-54.5) | 62.6 (49.2-76.0) | 75.3 (62.4-88.3) | 81.9 (69.9-94.0) | 86 (70.0-102.0) | 90.7 (79.2-102.1) |
| P value | 0.7 | 0.07 | 0.07 | <0.01 | <0.01 | <0.01 |
VISA-A, Victorian Institute of Sport Assessment Achilles-Specific Questionnaire.
Data presented as score (95% CI).
Numeric Pain Rating Scale
A significant main effect of time (P = 0.03) was found (Table 3), but the between-group difference was not significant. The ITT analysis yielded similar results.
Table 3.
NPRS values at baseline and follow-upa
| Baseline | 4 wk | 8 wk | 12 wk | 26 wk | 52 wk | |
|---|---|---|---|---|---|---|
| Exercise | 5.4 (3.6-7.2) | 3.8 (2.0-5.6) | 2.5 (1.0-3.9) | 3.0 (1.5-4.4) | 2.1 (1.4-2.8) | 1 (-0.6-2.6) |
| Astym | 4.6 (2.8-6.4) | 2.3 (1.1-3.5) | 2.7 (1.1-4.3) | 1.7 (0.8-2.8) | 0.8 (-0.2-1.9) | .67 (-0.6-1.9) |
NPRS, numeric pain rating scale.
Data presented as score (95% CI).
Additional Care
There was no significant difference (P = 0.53) in the number of subjects who sought additional care after completion of the 12-week study intervention phase. In the exercise group, 1 of 8 subjects sought additional care by the 52-week follow-up compared with 0 subjects in the soft tissue treatment (Astym).
Discussion
In the current study, soft tissue treatment (Astym) plus eccentric exercise was more effective than eccentric exercise at decreasing the severity of AT over a 12-week period, and these differences were maintained at 26- and 52-week follow-up periods. Additionally, a significantly greater number of subjects in the soft tissue treatment (Astym) group obtained a successful outcome. Both groups experienced a statistically significant decrease in pain over the course of the study, but the difference between groups was not statistically significant. These results seem to indicate that soft tissue treatment (Astym) plus eccentric exercise is an effective treatment in the management of insertional AT.
One possible explanation for the small difference in NPRS scores despite the large difference in VISA-A scores is that the subjects in the exercise-only group were generally less physically active at the study follow-up points. This is a reasonable assumption based on final VISA-A scores. With this in mind, it is plausible that subjects in the exercise-only group may have been avoiding aggravating activities, thus making their final NPRS scores artificially lower when compared with the more active soft tissue treatment (Astym) group.
There are some limitations to the current study that should be considered. First, the sample size was relatively small. While the study was adequately powered for the primary outcome, a larger sample size with multiple treatment sites could improve the generalizability of the results. A second limitation is the difference in contact with a therapist between the 2 groups. The soft tissue treatment (Astym) group was seen in the clinic for up to 12 sessions while subjects in the exercise-only group met with a therapist 1 to 4 times. The potential effect was minimized by contacting subjects in the exercise group 1 time per week by phone. It should also be considered that the eccentric exercise program is commonly performed as a home program only, and subjects in the exercise group actually received more contact than a typical patient receiving this intervention would.
Conclusion
Over a 12-week treatment period, soft tissue treatment (Astym) combined with eccentric exercise resulted in better outcomes than eccentric exercise alone for subjects with insertional AT. This difference was maintained at both 26- and 52-week follow-ups. Both groups experienced a statistically significant decrease in pain over the course of the study, but the difference between groups was not statistically significant.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article. This research was partially funded by Performance Dynamics, Muncie, Indiana. This funding was utilized to provide gift card incentives to research participants only. Performance Dynamics played no role in the study design, conduct, and reporting or in manuscript publication decisions.
References
- 1. Alfredson H, Pietila T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360-366. [DOI] [PubMed] [Google Scholar]
- 2. Cleland J, Childs J, Whitman J. Psychometric properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69-74. [DOI] [PubMed] [Google Scholar]
- 3. Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9-23. [DOI] [PubMed] [Google Scholar]
- 4. Cleland JA, Fritz JM, Whitman JM, Heath R. Predictors of short-term outcome in people with a clinical diagnosis of cervical radiculopathy. Phys Ther. 2007;87:1619-1632. [DOI] [PubMed] [Google Scholar]
- 5. Cleland JA, Mintken PE, Carpenter K, et al. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010;90:1239-1250. [DOI] [PubMed] [Google Scholar]
- 6. Davidson CJ, Ganion LR, Gehlsen GM, Verhoestra B, Roepke JE, Sevier TL. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc. 1997;29:313-319. [DOI] [PubMed] [Google Scholar]
- 7. Davies CC, Brockopp DY. Use of ASTYM treatment on scar tissue following surgical treatment for breast cancer: a pilot study. Rehabil Oncol. 2010;28:10. [Google Scholar]
- 8. Den Hartog BD. Insertional Achilles tendinosis: pathogenesis and treatment. Foot Ankle Clin. 2009;14:639-650. [DOI] [PubMed] [Google Scholar]
- 9. Fahlstrom M, Jonsson P, Lorentzon R, Alfredson H. Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc. 2003;11:327-333. [DOI] [PubMed] [Google Scholar]
- 10. Fowler S, Wilson JK, Sevier TL. Innovative approach for the treatment of cumulative trauma disorders. Work. 2000;15:9-14. [PubMed] [Google Scholar]
- 11. Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. Phys Sportsmed. 2005;33:32-43. [DOI] [PubMed] [Google Scholar]
- 12. Gehlsen GM, Ganion LR, Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999;31:531-535. [DOI] [PubMed] [Google Scholar]
- 13. Irwin TA. Current concepts review: insertional achilles tendinopathy. Foot Ankle Int. 2010;31:933-939. [DOI] [PubMed] [Google Scholar]
- 14. Iversen JV, Bartels EM, Langberg H. The Victorian Institute of Sports Assessment–Achilles Questionnaire (VISA-A)—a reliable tool for measuring Achilles tendinopathy. Int J Sports Phys Ther. 2012;7:76-84. [PMC free article] [PubMed] [Google Scholar]
- 15. Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407-415. [DOI] [PubMed] [Google Scholar]
- 16. James SL, Bates BT, Osternig LR. Injuries to runners. Am J Sports Med. 1978;6:40-50. [DOI] [PubMed] [Google Scholar]
- 17. Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83:157-162. [DOI] [PubMed] [Google Scholar]
- 18. Jonsson P, Alfredson H, Sunding K, Fahlstrom M, Cook J. New regimen for eccentric calf-muscle training in patients with chronic insertional Achilles tendinopathy: results of a pilot study. Br J Sports Med. 2008;42:746-749. [DOI] [PubMed] [Google Scholar]
- 19. Kvist M. Achilles tendon injuries in athletes. Sports Med. 1994;18:173-201. [DOI] [PubMed] [Google Scholar]
- 20. Lorenz D, Reiman M. The role and implementation of eccentric training in athletic rehabilitation: tendinopathy, hamstring strains, and ACL reconstruction. Int J Sports Phys Ther. 2011;6:27-44. [PMC free article] [PubMed] [Google Scholar]
- 21. Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med. 1998;26:266-270. [DOI] [PubMed] [Google Scholar]
- 22. Maffulli N, Binfield PM, King JB. Tendon problems in athletic individuals. J Bone Joint Surg Am. 1998;80:142-144. [PubMed] [Google Scholar]
- 23. Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med. 2009;19:54-64. [DOI] [PubMed] [Google Scholar]
- 24. McCormack JR. The management of bilateral high hamstring tendinopathy with ASTYM and eccentric exercise: a case report. J Man Manip Ther. 2012;20:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McCormack JR. The management of mid-portion Achilles tendinopathy with ASTYM® and eccentric exercise: a case report. Int J Sports Phys Ther. 2012;7:672-677. [PMC free article] [PubMed] [Google Scholar]
- 26. Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18:920-926. [DOI] [PubMed] [Google Scholar]
- 27. Puentedura EJ, Cleland JA, Landers MR, Mintken PE, Louw A, Fernandez-de-Las-Penas C. Development of a clinical prediction rule to identify patients with neck pain likely to benefit from thrust joint manipulation to the cervical spine. J Orthop Sports Phys Ther. 2012;42:577-592. [DOI] [PubMed] [Google Scholar]
- 28. Rees JD. Current concepts in the management of tendon disorders. J Rheumatol. 2006;45:508-521. [DOI] [PubMed] [Google Scholar]
- 29. Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology (Oxford). 2006;45:508-521. [DOI] [PubMed] [Google Scholar]
- 30. Rees JD, Wolman RL, Wilson A. Eccentric exercises; why do they work, what are the problems and how can we improve them? Br J Sports Med. 2009;43:242-246. [DOI] [PubMed] [Google Scholar]
- 31. Robinson JM, Cook JL, Purdam C, et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med. 2001;35:335-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rompe JD, Furia J, Maffulli N. Eccentric loading compared with shock wave treatment for chronic insertional Achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. 2008;90:52-61. [DOI] [PubMed] [Google Scholar]
- 33. Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport. 2007;10:52-58. [DOI] [PubMed] [Google Scholar]
- 34. Sevier T, Stover S, Helfst R, Zanas J. ASTYM Clinical Manual. 7th ed. Muncie, IN: Performance Dynamics; 2009. [Google Scholar]
- 35. Sevier TL, Stegink-Jansen CW. Astym treatment vs. eccentric exercise for lateral elbow tendinopathy: a randomized controlled clinical trial. PeerJ. 2015;3:e967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Solan M, Davies M. Management of insertional tendinopathy of the Achilles tendon. Foot Ankle Clin. 2007;12:597-615. [DOI] [PubMed] [Google Scholar]
- 37. Spadoni GF, Stratford PW, Solomon PE, Wishart LR. The evaluation of change in pain intensity: a comparison of the P4 and single-item numeric pain rating scales. J Orthop Sports Phys Ther. 2004;34:187-193. [DOI] [PubMed] [Google Scholar]
- 38. Stratford PW, Binkley J, Solomon P, Gill C, Finch E. Assessing change over time in patients with low back pain. Phys Ther. 1994;74:528-533. [DOI] [PubMed] [Google Scholar]
- 39. Sussmilch-Leitch SP, Collins NJ, Bialocerkowski AE, Warden SJ, Crossley KM. Physical therapies for Achilles tendinopathy: systematic review and meta-analysis. J Foot Ankle Res. 2012;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tan SC, Chan O. Achilles and patellar tendinopathy: current understanding of pathophysiology and management. Disabil Rehabil. 2008;30:1608-1615. [DOI] [PubMed] [Google Scholar]
- 41. van Dijk CN, van Sterkenburg MN, Wiegerinck JI, Karlsson J, Maffulli N. Terminology for Achilles tendon related disorders. Knee Surg Sports Traumatol Arthrosc. 2011;19:835-841. [DOI] [PMC free article] [PubMed] [Google Scholar]