Over the past 50 years the costs of American medical care have increased dramatically. While these high costs have been accompanied by substantial reductions in morbidity and mortality, Americans could derive significantly more value from health care expenditures.1 For many policymakers, the major focus of health care reform has centered on methods to improve economic efficiency–the outcomes achieved relative to per capita health care spending. A more recent emphasis on patient-centered care has added growing awareness of the importance of accommodating individual patients’ preferences, needs and beliefs into health care.2 Value-based insurance design (V-BID) describes a system of health insurance that varies patients’ cost-sharing in order to maximize use of high-value services while maintaining a focus on patient centeredness. This review addresses aspects of V-BID that are relevant to cardiovascular medicine: fundamental features, evidence for effectiveness, real-world applications, novel ways to build on strengths, relevance in future health policy landscapes, and known limitations.
V-BID Fundamentals
Patient Centeredness
The premise of V-BID is that patients should be placed at the center of value-based reform efforts by incentivizing their behavior through value-based modulation of out-of-pocket costs health care costs. V-BID is distinct from – yet complementary to– many other health policy constructs because it directs financial incentives toward patients rather than providers. At the same time, it promotes economic efficiency by allowing payers to subsidize care in a manner proportionate to its societal cost effectiveness. While patients must incorporate value-based financial incentives into their decision making process, financial considerations are neither the only factor nor a coercive factor. A wide range of services can be “covered”, with varying contributions from the patient and the payer based on how much relative value is provided for each party. This focus on non-coercive patient incentives respects and reinforces the reality that medical decisions should incorporate patients’ preferences as a central factor.
Cost-sharing incentives are designed to maximize use of high-value care, but patient autonomy is respected by permitting selection of lower-value care by patients who are willing to pay more of the cost. In a departure from the “covered/not-covered” dichotomy of conventional insurance designs with fixed copayments, partial coverage through selective use of higher patient cost sharing can be incorporated into V-BID. V-BID incentives are determined using the concept of clinical nuance, which supports value-based patient choice by recognizing that: 1) different medical services contribute variably to improving health; and 2) the clinical benefit and economic efficiency derived from a specific service depends on context (i.e. where it is used, when it is used and for which patients it is used).
Cost Sharing
Patient cost-sharing in the form of copayments and coinsurance strongly influences health care utilization,3–5 yet it is not overtly addressed in many other health policy constructs. Discretionary patterns of utilization are thought to be critical modifiable factors that can improve quality and control health care costs.6, 7 On the other hand, indiscriminate increases in cost-sharing can lead to reductions in the use of preventive and essential care, which may worsen health disparities.4, 8–10 V-BID employs clinical nuance to create a “carrot and stick” approach to mitigate concerns regarding cost-related non-adherence, as well as to reduce potentially harmful and wasteful health expenditures. Services across the entire spectrum of care that are deemed to be high value may be incentivized by lowering or eliminating cost sharing (“carrot”). Services without evidence of benefit can be discouraged through increases in cost-sharing (“stick”). V-BID can shift the focus of patients, doctors and payers away from a “one-size-ts-all” cost-sharing system that fails to acknowledge the differences in clinical value among medical interventions, and instead toward maximizing value in health care. It can steer stakeholder interactions away from the challenges of a reductionist, binary coverage decision model (“covered/not-covered’) or a cost-driven tiered model (“generic/branded/non-covered” drugs). Evidence-based services that are valued by patients and considered clinically indicated by physicians can be covered using V-BID principles as long as value-based incentives are appropriately aligned using carrots and sticks of variable cost sharing.
Evidence for V-BID’s Effectiveness
V-BID programs have thus far demonstrated moderate effectiveness for increasing patient demand for high-value care and for improving outcomes. Application of V-BID to medication benefits has been associated with an average 3% absolute increase in adherence (ranging up to 10% in individual studies)11 and moderate improvement in cardiovascular outcomes (Table 1)12–14 in an expected dose-response manner.15 There has been one, large randomized trial testing V-BID techniques for patients with high-risk cardiovascular disease. In the MI-FREEE study, commercially-insured patients experiencing acute myocardial infarction were randomly assigned to either usual prescription coverage or prescription coverage without cost-sharing for any generic or brand-name angiotensin-converting enzyme (ACE) inhibitor, angiotensin receptor blocker, beta-blocker, or statin.12 A V-BID coverage strategy that eliminated copayments for these medications led to improved medication adherence. The rate of full adherence with all three classes of evidence-based cardiovascular medications increased 3.2% (37% relative increase) in the V-BID group. Individual medication full adherence increased between 4.8% and 7.0% (relative increases of approximately 20%). Improved adherence was associated with lower rates of additional major vascular events and decreased patient spending, with no increase in overall health costs.
Table 1.
Studies evaluating effects of variable medication cost sharing on cardiovascular endpoints or health care utilization
| Study | Year | Design | Size | Patient characteristics | Observed effect |
|---|---|---|---|---|---|
| Keeler et al.14 | 1985 | RCT | 3,495 | Stable outpatient | ↓ Blood pressure |
| Pilote et al.37 | 2002 | ITS | 22,066 | >65 yo after AMI | None |
| Choudhry et al.12 | 2011 | RCT | 5,855 | <65 yo after AMI | ↓ First major vascular event (secondary endpoint) |
| Choudhry et al.13 | 2012 | CBA | 2,830 cases / 49,801 controls | Stable outpatient | ↓ Hospitalizations and emergency department admissions |
CBA indicates controlled before-after study; ITS, interrupted time series study; RCT, randomized controlled trial; and V-BID, value-based insurance design.
A secondary analysis was performed to examine the effect of the V-BID program on racial and ethnic disparities. 16 At baseline, nonwhite patients enrolled in the MI-FREEE study were less adherent with prescribed medication and had higher health care spending than their white counterparts. After cost-sharing was eliminated for the intervention group, adherence to beta-blockers and statins significantly improved for nonwhite enrollees. Compared to nonwhites with standard cost-sharing, those for whom copayments were eliminated experienced a 35% lower risk of readmission for a major vascular event or coronary revascularization, as well as a 70% reduction in total health care spending.
Existing Applications of V-BID
V-BID has been used to incentivize both drug and non-drug health services and adoption has increased over time. In a 2007 survey of large employers, 20% reported using V-BID and 80% reported being “interested” or “very interested” in incorporating it.17 With passage of the Affordable Care Act, V-BID incentives were extended to millions of Americans to promote preventive care. The Affordable Care Act mandated elimination of copayment and coinsurance for US Preventive Services Task Force level A and B recommendations, including screening for several cardiovascular risk factors and tobacco cessation interventions.18 V-BID has also been used to encourage a broader array of high-value care by directing patients toward high-quality clinicians or health systems. For example, the Oregon Public Employees Benefit Board has prioritized the use of high-quality primary care providers by lowering copayments for services at recognized primary care medical homes.19 Similarly, the home improvement retailer Lowes has prioritized high-value cardiovascular care at the Cleveland Clinic by eliminating deductibles and travel costs associated with treatment there.20
V-BID has garnered significant multi-stakeholder support, which has enabled its implementation at both the state and national levels.21 Several state employee programs such as those in Connecticut, Maine, Oregon and Virginia have implemented V-BID principles. Additionally the V-BID concept has been incorporated into state Medicaid programs, including those in Michigan, Oregon and New Mexico. Advanced V-BID designs that include both “carrots” and “sticks” for a variety of services (medications, office visits, imaging services, and procedures) are being offered and studied by innovators such as Group Health Cooperative and the Mayo Clinic.
Building on V-BID
A novel insurance design has been proposed that would expand V-BID reach and flexibility by shifting patient incentives from cost sharing at the episode-of-care level to value-based indexing of monthly insurance premiums. Relative value health insurance describes policies with premium levels set based on how closely coverage matches proven, cost-effective health care.22, 23 Policies covering primarily cost-effective drugs, devices and services would be offered at the lowest premium level. Policies covering health care that is unproven or not cost effective would be offered at higher premium levels. Again, patients could choose coverage that matches their personal preferences using principles analogous to V-BID. An advantage of the relative value health insurance construct is that it allows for general decisions about cost-sharing preferences at the time of policy selection. As a result, it distributes the costs (“sticks”) of low-value care preferred by some patients as well as the savings (“carrots”) from high-value preferred by others across the duration of the insurance policy, rather than concentrating them at the episode-of-care level.
Another alternative to conventional V-BID approaches could be created by bundling high-value services across episodes of care. Health care goods and services could be combined based on several different rubrics including clinical indication, patient diagnosis, and patient risk level.24 For example, a V-BID bundle could be constructed that pools post-MI medications, clinician visits, laboratory testing, cardiac rehabilitation sessions, cardiac imaging, and an implantable cardioverter-defibrillator (if indicated) into a single package that is well-defined and free for patients. Such an arrangement could simplify and make affordable what would otherwise be a daunting, unpredictable array of services and out-of-pocket costs for the average patient convalescing from an MI. In another setting, patients at high risk for hospital admission for heart failure could enjoy free medications, clinician encounters, home telemonitoring, and cardiac rehabilitation encounters to promote adherence and close follow-up. Finally, if desirable from a value standpoint or if other forms of bundling would be excessively complex, patients could be incentivized to receive care from select high-quality clinicians or health systems.
V-BID’s Future Roles
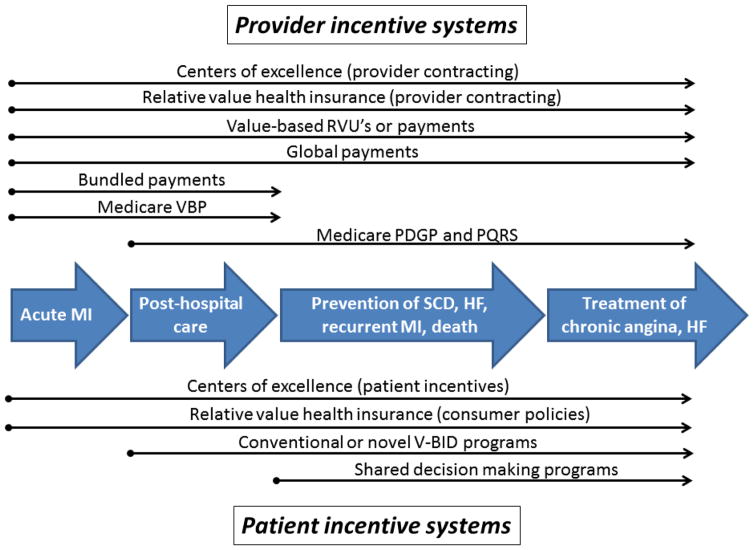
V-BID could be an important method for aligning incentives in the complex array programs that are available to policymakers (Figure 1, Table 2 and Table 3). Two features of V-BID make it a natural complement to existing health care reforms: 1) patient-focused incentives can be aligned with provider-focused incentives to better match supply and demand; 2) episode-of-care level incentives could be used to enhance the effects of global payments. These features could be employed in new ways to improve the value of cardiovascular care. While V-BID has historically been tested mostly as a motivating incentive (“carrot”), there is increasing interest in using its de-motivating features (“stick”) to discourage use of low-value/overutilized services.
Figure 1.
Example of the phases of care during which each patient-focused and provider-focused incentive system is most relevant, using the example of acute myocardial infarction. For more detailed descriptions see the text and Tables 2 and 3. PGDP indicates physician group demonstration project; PQRS, physician quality reporting system; RVUs, relative value units; V-BID, value-based insurance design; and VBP, value-based purchasing
Table 2.
Incentive programs that span multiple episodes of care
| Program | Primary targeted entity | Description |
|---|---|---|
| Relative value health insurance22 | Patients and providers | Theoretical system that shifts patient cost-sharing incentives from episodes of care to fixed monthly premiums. In the same manner as conventional V-BID programs, it uses lower pricing to incentive high-value care and higher pricing to disincentive low-value care. |
| Global payments38 | Health systems | Capitation or partial-capitation system with quality and efficiency incentives |
| Bundled payments39 | Health systems | Hybrid system that incorporates multiple episodes of care by multiple providers into a single episode. |
| Medicare value-based purchasing program40 | Health systems | Fee-for-service-based system that incentivizes efficient, quality care over multiple patients/encounters. |
| Medicare physician group demonstration projects41 | Physician groups | Fee-for-service-based system that incentives efficient, quality care over multiple patients/encounters. |
| Medicare physician quality reporting system42 | Individual physicians and physician groups | Fee-for-service-based system that incentivizes care based on self-selected quality measures to be assessed over multiple patients/encounters. |
Table 3.
Incentive programs that target individual episodes-of-care
| Program | Primary targeted entity | Description |
|---|---|---|
| V-BID43 | Patients | Variable patient cost-sharing system (usually at episode-of-care level) to incentivize high-value care |
| Shared decision making44 | Patients | Information system to insure medical decision making is consistent with patient preferences. Not value-targeted in a strict sense, but often leads to less costly care. |
| Value-based payments32 | Individual physicians and physician groups | Theoretical system for providers that is analogous to V-BID; providers receive greater remuneration for highly cost-effective care. Based in a fee-for-service environment. |
| Value-based RVUs45 | Individual physicians, physician groups and health systems | Theoretical system for providers that is analogous to both V-BID and value-based payments; clinician productivity metrics are weighted to favor high-value care. Could be used in either fee-for-service or capitated environments, and any form of health care organization. |
RVUs indicates relative value units; and V-BID, value-based insurance design
Aligning Supply and Demand
Maximizing the value of health care at a societal level requires that value-driven patient choices (demand) are well matched with available services (supply).25 Because multiple factors are at play, supply and demand for high-value services may become unbalanced. For example, supply distortions can arise from a shortage of primary care providers26 or geographic clustering of invasive cardiac services,27 while demand distortions can arise from poor patient participation in cardiac rehabilitation28 or excessive enthusiasm for routine ECG or echo in pre-participation athletic screening.29 V-BID can be used to help match supply and demand by functioning as a complement to provider-based value incentives.30 For example, the MI-FREEE study described above (“Evidence for V-BID’s Effectiveness” Section) showed that a V-BID program helped to move demand (patient medication adherence) closer to supply (provider medication prescription) for evidence-based cardiovascular therapy. It is unknown whether additional incentives, such as paying patients to take selected medications, would increase adherence further. Such a strategy has proven effective for smoking cessation pharamacotherapy.31 It is also unknown whether matching episode-of-care-based VBID incentives with episode-of-care-based clinician incentives32, 33 could have affected adherence.
Aligning Patient Behavior with Global Budgets
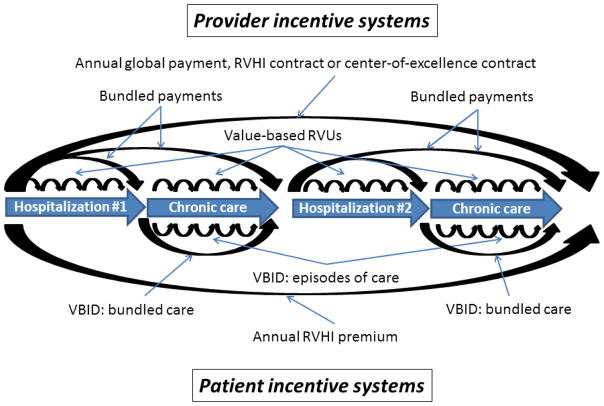
Even the broadest of health policies must ultimately affect decisions made by individual patients and clinicians at discrete moments in time, particularly outpatient episodes of care. Thus, explicitly addressing patient preferences and incentives at the episode-of-care level could complement global payment priorities directed at health systems (Figure 2). While many incentive systems attempt to influence providers using a variety of leverage points, few established programs aside from V-BID are available to influence patient behavior (Tables 2 and 3).
Figure 2.
Flow diagram of the alignment of patient and provider incentives using several health policy constructs, using a hypothetical patient experience of outpatient care with recurrent hospitalizations. Provider-facing programs such as annual global payment, bundled payments, and value-based relative value units (RVUs) are paired with patient-facing programs such as value-based insurance design (V-BID) strategies and relative value health insurance policies. Note, VBID bundled care, relative value health insurance and relative value RVU’s are all theoretical constructs. For more detailed descriptions each strategy see the text and Tables 2 and 3.
Accountable care organizations (ACOs) and even individual health systems could be motivated to utilize V-BID principles independent of payers if patient behavior is incorporated into global payment quality metrics. In such a scenario, the same rationale by which ACOs create disease management programs could drive them to create and fund their own V-BID programs. This issue could become relevant sooner than many realize. The Center for Medicare and Medicaid Services (CMS) recently proposed a quality measure for the National Quality Foundation’s (NQF) Cardiovascular Measures Project that would target an 80% adherence benchmark for statin use among patients with cardiovascular disease.34 V-BID could be an important tool to improve performance for this metric.
Increasing Appropriateness of Cardiovascular Care
Improving the appropriateness of cardiovascular care (reducing overutilization and underutilization) is an important focus. However, many interventions such as use of radiology benefits managers create administrative inefficiencies and focus one-sidedly on overutilization. In the future, V-BID approaches could be used to more efficiently align patient demand incentives for appropriate care with provider quality metrics and supply incentives at both the episode-of-care and global payment levels. For example, if guided by a marker of clinical value such as appropriateness criteria,35, 36 echocardiography could be completely subsidized in certain high-value contexts such as guiding treatment when new signs and symptoms of heart failure are present (high appropriateness; 0% patient / 100% payer). On the other hand, echocardiography in less valuable settings such as routine surveillance of established heart failure without a change in clinical status could be partially subsidized if done less often than yearly (moderate appropriateness; 50% patient/ 50% payer) or minimally subsidized if done more often than yearly (low appropriateness; 90% patient / 10% payer). In any of these scenarios, V-BID allows patients, providers and payers to partner in a manner that is more clinically nuanced than binary “coverage/no-coverage” decisions.
Limitations
Clinically nuanced payment models or benefit designs are not a panacea to substantial gaps in quality of care or variations costs. However, patient engagement initiatives that provide incentives based on efficiency and health benefits–not absolute cost or profit–can complement ongoing provider-facing programs with similar goals. Nonetheless, V-BID applications may be challenging in some domains. Clinical scenarios for which patient discretion is unrealistic, such as emergency care for acute myocardial infarction or cardiac arrest, may not be readily addressed with V-BID. Similarly, when high cost diagnostics or procedural treatments are imbedded in complex episodes of care such as prolonged hospitalizations or outpatient treatment protocols, isolating them for V-BID incentives can be difficult. In the most challenging scenarios, influencing provider behavior is likely to provide the maximum impact, and incentivizing patients to choose centers of excellence may be the only practical patient-directed approach.
Another limitation is that V-BID has generally proven cost-neutral rather than cost-saving. Reductions in event-related costs among V-BID medication adherence programs have been counterbalanced by associated increases in prescription drug costs. This is not surprising, given that the underlying clinical trials of these medications have generally demonstrated them to be cost-effective but not cost-reducing. It is also important to recognize that the overall goals of health reform are to reduce the rate of growth of health care spending while increasing the value derived from that spending. Thus many strategies included in health reform will improve cost efficiency without reducing absolute costs. Nonetheless, as the “stick” aspect of V-BID programs is tested to reduce overutilization of low-value services, cost may more often be targeted as the primary goal of interventions. One important exception, however, is for clinical services with simultaneous underutilization and overutilization. In such cases, reductions in use of overutilized services may subsidize use of underutilized services in a manner that is cost-neutral yet value-promoting.
Conclusion
V-BID is a multifaceted approach that aligns consumer cost sharing to promote high-value care and discourage low-value care. Cardiovascular medicine is an ideal setting for utilizing V-BID, given the breadth and depth of studies that evaluate the effect of medications, devices, procedures, imaging and clinician services on clinical outcomes. When aligned with provider-facing quality initiatives, a clinically nuanced approach such as V-BID could improve cardiovascular care by mitigating cost-related non-adherence to evidence-based services, reducing disparities, and minimizing potential conflicts between patients, physicians and payers.
Footnotes
Disclosures
All authors report no potential conflicts of interest that would affect the content of this manuscript.
References
- 1.Starfield B. Is US health really the best in the world? JAMA. 2000;284:483–5. doi: 10.1001/jama.284.4.483. [DOI] [PubMed] [Google Scholar]
- 2.Committee on Quality Health Care in America (Institute of Medicine) Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 3.Chernew ME, Newhouse JP. What does the RAND Health Insurance Experiment tell us about the impact of patient cost sharing on health outcomes? Am J Manag Care. 2008;14:412–4. [PubMed] [Google Scholar]
- 4.Gibson TB, Ozminkowski RJ, Goetzel RZ. The effects of prescription drug cost sharing: a review of the evidence. Am J Manag Care. 2005;11:730–40. [PubMed] [Google Scholar]
- 5.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. 2008;358:375–83. doi: 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]
- 6.Fox BJ, Yucel MK, Taylor JL. America’s health care problem: an economic perspective. Economic Review - Third Quarter. [accessed 10/7/14];Federal Reserve Bank of Dallas. 1993 https://www.dallasfed.org/assets/documents/research/er/1993/er9303b.pdf.
- 7.Virts JR, Wilson GW. Inflation and health care prices update. Health Aff (Millwood) 1984;3:135–6. doi: 10.1377/hlthaff.3.3.135. [DOI] [PubMed] [Google Scholar]
- 8.Chernew M, Gibson TB, Yu-Isenberg K, Sokol MC, Rosen AB, Fendrick AM. Effects of increased patient cost sharing on socioeconomic disparities in health care. J Gen Intern Med. 2008;23:1131–6. doi: 10.1007/s11606-008-0614-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei II, Lloyd JT, Shrank WH. The relationship between the low-income subsidy and cost-related nonadherence to drug therapies in Medicare Part D. J Am Geriatr Soc. 2013;61:1315–23. doi: 10.1111/jgs.12364. [DOI] [PubMed] [Google Scholar]
- 10.Kazerooni R, Bounthavong M, Watanabe JH. Association of copayment and statin adherence stratified by socioeconomic status. Ann Pharmacother. 2013;47:1463–70. doi: 10.1177/1060028013505743. [DOI] [PubMed] [Google Scholar]
- 11.Lee JL, Maciejewski M, Raju S, Shrank WH, Choudhry NK. Value-based insurance design: quality improvement but no cost savings. Health Aff (Millwood) 2013;32:1251–7. doi: 10.1377/hlthaff.2012.0902. [DOI] [PubMed] [Google Scholar]
- 12.Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, Reisman L, Fernandes J, Spettell C, Lee JL, Levin R, Brennan T, Shrank WH Post-Myocardial Infarction Free Rx E, Economic Evaluation T. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365:2088–97. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 13.Choudhry NK, Fischer MA, Avorn JL, Lee JL, Schneeweiss S, Solomon DH, Berman C, Jan S, Lii J, Mahoney JJ, Shrank WH. The impact of reducing cardiovascular medication copayments on health spending and resource utilization. J Am Coll Cardiol. 2012;60:1817–24. doi: 10.1016/j.jacc.2012.06.050. [DOI] [PubMed] [Google Scholar]
- 14.Keeler EB, Brook RH, Goldberg GA, Kamberg CJ, Newhouse JP. How free care reduced hypertension in the health insurance experiment. JAMA. 1985;254:1926–31. [PubMed] [Google Scholar]
- 15.Choudhry NK, Glynn RJ, Avorn J, Lee JL, Brennan TA, Reisman L, Toscano M, Levin R, Matlin OS, Antman EM, Shrank WH. Untangling the relationship between medication adherence and post-myocardial infarction outcomes: medication adherence and clinical outcomes. Am Heart J. 2014;167:51–58. e5. doi: 10.1016/j.ahj.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 16.Choudhry NK, Bykov K, Shrank WH, Toscano M, Rawlins WS, Reisman L, Brennan TA, Franklin JM. Eliminating medication copayments reduces disparities in cardiovascular care. Health Aff (Millwood) 2014;33:863–70. doi: 10.1377/hlthaff.2013.0654. [DOI] [PubMed] [Google Scholar]
- 17.Choudhry NK, Rosenthal MB, Milstein A. Assessing the evidence for value-based insurance design. Health Aff (Millwood) 2010;29:1988–94. doi: 10.1377/hlthaff.2009.0324. [DOI] [PubMed] [Google Scholar]
- 18. [accessed October 7, 2014]; https://www.healthcare.gov/what-are-my-preventive-care-benefits/
- 19. [accessed October 7, 2014]; http://www.oregon.gov/oha/pcpch/Pages/payment-incentives.aspx.
- 20.Chen C. Cheaper surgery sends Lowe’s flying to Cleveland Clinic. Bloomberg News. 2014 Mar 7; [Google Scholar]
- 21.Ndukwe EG, Fendrick AM, Udow-Phillips M. [accessed March 6, 2014];Value-Based Insurance Design: Shifting the Health Care Cost Discussion from How Much to How Well. http://www.ihpi.umich.edu/sites/default/files/downloads/IHPI-VBID_e-version_October_17_2014.pdf.
- 22.Korobkin R. Relative value health insurance. J Health Polit Policy Law. 2014;39:417–40. doi: 10.1215/03616878-2416310. [DOI] [PubMed] [Google Scholar]
- 23.Korobkin R. Comparative effectiveness research as choice architecture: the behavioral law and economics solution to the health care cost crisis. Mich Law Rev. 2014;112:523–74. [PubMed] [Google Scholar]
- 24.Fendrick AM, Sonnad SS. [accessed October 11, 2014];Value-based insurance design for diagnostics, devices, and procedures: a novel approach to better recognize the effectiveness and value of medical technology. 2012 http://www.sph.umich.edu/vbidcenter/publications/pdfs/V-BID%20and%20Devices%20InHealth.pdf.
- 25.Colla CH. Swimming against the current--what might work to reduce low-value care? N Engl J Med. 2014;371:1280–3. doi: 10.1056/NEJMp1404503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carrier ER, Yee T, Stark L. NIHCR Policy Analysis No. 7. National Institute for Health Care Reform; 2011. [accessed October 7, 2014]. Matching supply to demand: addressing the US primary care workforce shortage. http://www.nihcr.org/index.php?download=1tlcfl41. [Google Scholar]
- 27.Horwitz JR, Nichols A, Nallamothu BK, Sasson C, Iwashyna TJ. Expansion of invasive cardiac services in the United States. Circulation. 2013;128:803–10. doi: 10.1161/CIRCULATIONAHA.112.000836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–62. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 29.Leslie LK, Cohen JT, Newburger JW, Alexander ME, Wong JB, Sherwin ED, Rodday AM, Parsons SK, Triedman JK. Costs and benefits of targeted screening for causes of sudden cardiac death in children and adolescents. Circulation. 2012;125:2621–9. doi: 10.1161/CIRCULATIONAHA.111.087940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Antos J, Bertko J, Chernew ME, Cutler DM, Goldman D, McClellan M, McGlynn E, Pauly M, Schaeffer L, Shortell S. [accessed October 7, 2014];Bending the curve: effective steps to address long-term health care spending growth. 2009 http://www.brookings.edu/~/media/research/files/reports/2009/9/01%20btc/0826_btc_fullreport.pdf. [PubMed]
- 31.Volpp KG, Troxel AB, Pauly MV, Glick HA, Puig A, Asch DA, Galvin R, Zhu J, Wan F, DeGuzman J, Corbett E, Weiner J, Audrain-McGovern J. A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360:699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 32.McMahon LF, Jr, Chopra V. Health care cost and value: the way forward. JAMA. 2012;307:671–2. doi: 10.1001/jama.2012.136. [DOI] [PubMed] [Google Scholar]
- 33.Stecker EC. The Oregon ACO experiment--bold design, challenging execution. N Engl J Med. 2013;368:982–5. doi: 10.1056/NEJMp1214141. [DOI] [PubMed] [Google Scholar]
- 34. [accessed February 21, 2015]; http://www.qualityforum.org/ProjectMeasures.aspx?projectID=77924.
- 35.Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, van het Loo M, McDonnell J, Vader JP, Kahan JP. [accessed June 24, 2014];The RAND/UCLA Appropriateness Method User’s Manual. http://www.rand.org/content/dam/rand/pubs/monograph_reports/2011/MR1269.pdf.
- 36.American College of Cardiology Foundation Appropriate Use Criteria Task F, American Society of E, American Heart A, American Society of Nuclear C, Heart Failure Society of A, Heart Rhythm S, Society for Cardiovascular A Interventions, Society of Critical Care M, Society of Cardiovascular Computed T, Society for Cardiovascular Magnetic R. Douglas PS, Garcia MJ, Haines DE, Lai WW, Manning WJ, Patel AR, Picard MH, Polk DM, Ragosta M, Ward RP, Weiner RB. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011;57:1126–66. doi: 10.1016/j.jacc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 37.Pilote L, Beck C, Richard H, Eisenberg MJ. The effects of cost-sharing on essential drug prescriptions, utilization of medical care and outcomes after acute myocardial infarction in elderly patients. CMAJ. 2002;167:246–52. [PMC free article] [PubMed] [Google Scholar]
- 38.Landon BE. Keeping score under a global payment system. N Engl J Med. 2012;366:393–5. doi: 10.1056/NEJMp1112637. [DOI] [PubMed] [Google Scholar]
- 39.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012;366:1075–7. doi: 10.1056/NEJMp1113361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. [accessed October 11, 2015]; http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html?redirect=/hospital-value-based-purchasing.
- 41. [accessed October 7, 2015]; http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/Medicare-Demonstrations-Items/CMS1198992.html.
- 42. [accessed October 11, 2015]; http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html?redirect=/PQRS/
- 43.Fendrick AM, Chernew ME, Levi GW. Value-based insurance design: embracing value over cost alone. Am J Manag Care. 2009;15:S277–83. [PubMed] [Google Scholar]
- 44.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012;366:780–1. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 45.Stecker EC, Schroeder SA. Adding value to relative-value units. N Engl J Med. 2013;369:2176–9. doi: 10.1056/NEJMp1310583. [DOI] [PubMed] [Google Scholar]