Abstract
Background/Objective
The prevalence of type 2 diabetes is increasing rapidly around the world. Work-related stress is thought to be a major risk factor for type 2 diabetes; however, this association has not been widely studied, and the findings that have been reported are inconsistent. Therefore, we conducted a meta-analysis of prospective cohort studies to explore the association between work-related stress and risk for type 2 diabetes.
Methods
A systematic literature search and manual search limited to articles published in English were performed to select the prospective cohort studies evaluated the association between work-related stress and risk for type 2 diabetes up to September 2014 from four electronic databases including PubMed, EMBASE, the Cochrane Library and Web of Science. A random-effects model was used to estimate the overall risk.
Results
No significant association was found between work-related stress and risk for type 2 diabetes based on meta-analysis of seven prospective cohort studies involving 214,086 participants and 5,511 cases (job demands: relative risk 0.94 [95% confidence interval 0.72–1.23]; decision latitude: relative risk 1.16 [0.85–1.58]; job strain: relative risk 1.12 [.0.95–1.32]). However, an association between work-related stress and risk for type 2 diabetes was observed in women (job strain: relative risk 1.22 [1.01–1.46]) (P = 0.04). A sensitivity analysis conducted by excluding one study in each turn yielded similar results. No publication bias was detected with a funnel plot despite the limited number of studies included in the analysis.
Conclusions
The results of this meta-analysis did not confirm a direct association between work-related stress and risk for type 2 diabetes. In subgroup analyses we found job strain was a risk factor for type 2 diabetes in women.
Introduction
Type 2 diabetes is one of the most prevalent chronic diseases, ever-increasing worldwide, especially in developing countries. It is one of the major public health challenge of the 21st century. The 7th edition of the Diabetes Atlas, released by the International Diabetes Federation on World Diabetes Day, reports that the number of worldwide diabetes cases reached 415 million in 2015, and is expected to rise to 642 million by 2040. Researchers predict that annual health care expenditure may increase from the current figure of $673 billion to $802 billion by 2040 [1]. As early as the 17th century, Thomas Willis, the famous English physician, linked diabetes to emotional factors such as prolonged sorrow [2], which is now known as psychosocial stress. The American psychiatrist Dr. W. Menninger first tested Willis’s hypothesis and mentioned the existence of psychogenic diabetes in 1935 [3]. Almost 40 years later, psychosocial stress was attracting growing attention, and the famous psychiatrist George Engel noted the shift from a traditional biomedical to a biopsychosocial model [4].
Researchers have confirmed numerous risk factors for type 2 diabetes, including family history, low exercise levels [5,6], increased weight [7], heavy smoking [8] and alcohol consumption [9]. The etiology of type 2 diabetes is complex, and work-related stress may contribute to, or increase, the risk of its development. Some evidences have proved that psychosocial stress at work is an important risk factor for heart disease [10–13]. However, the results of the studies examining the association between work-related stress are inconsistent. Previous meta-analyses did not support the hypothesis that work-related stress increases the risk for type 2 diabetes [14,15].
The job strain model, proposed by Karasek and Theorell, provides a theoretical model for assessing the role of work stress in the onset of type 2 diabetes. The job strain model includes job demands (the summation of psychosocial work stressors), decision latitude/job control (the individual’s decision authority at work), and job strain (the combination of high levels of job demands and low levels of job control) [16].
Therefore, we performed a systematic review and meta-analysis of prospective cohort studies for the following purposes: 1) to review recent evidence on the relationship between work-related stress and incidence of type 2 diabetes; and 2) to examine whether this relationship differs according to the different kinds of work-related psychosocial factors and participant characteristics.
Materials and Methods
Data sources and searches
To identify observational epidemiological studies that investigated the association between work-related psychosocial stress and the incidence of type 2 diabetes, we followed guidelines for meta-analysis of observational studies in epidemiology [17]. Two investigators independently conducted a systematic literature search of English language articles published before September 2014 using the following bibliographic databases and time ranges: PubMed from 1948, EMBASE from 1974, the Cochrane Library from 1993, and Web of Science from 1900.
The main search strategy included medical subject heading terms or text words for “outcome” (diabetes mellitus, type 2 OR diabetes mellitus) and “exposure” (work stress OR occupational stress OR work-related psychosocial stress OR work-related psychosocial factors OR psychosocial work environment OR work characteristics OR work demand OR decision latitude OR job control OR job strain OR related terms) and “design type” (prospective studies OR cohort studies OR longitudinal studies OR incidence or follow-up studies). Furthermore, we examined the references of retrieved original articles and reviews to identify additional relevant studies. When necessary, we attempted to contact the authors for additional information. The supporting PRISMA checklist is available as supporting information (see S1 Checklist).
Study selection
The current systematic review and meta-analysis was restricted to prospective studies because case-control and cross-sectional studies are known to be subject to selection and recall bias, and cannot definitively determine the association between exposure and outcome. Published articles were included if they met the following criteria: (1) used a prospective cohort study design; (2) assessed the incidence of type 2 diabetes; (3) presented a measure of work-related stress (including job demands, decision latitude/job control, job strain); and (4) reported the odds ratios (OR) or relative risk (RR), or hazard ratio (HR) and its 95% confidence interval (CI), for highest versus lowest/non-level of work-related psychosocial stress. Studies were excluded for the following reasons: (1) the outcome measure was prediabetic state or metabolic syndrome rather than type 2 diabetes; (2) the study focused on control as opposed to incidence of type 2 diabetes; (3) or exposure was related to working hours or overtime work, night work or shift work, trauma, burnout, violence or accidents at work, social network outside the workplace, psychological distress such as anxiety and depression, personality, or coping style. If publications were duplicated, or if the same cohort was analyzed in more than one article, the study with the longer follow-up period, higher quality and more detailed information for both exposure and outcome was included.
Data extraction and quality assessment
We used a standard data extraction form to collect the following information: first author’s name, publication year, cohort designation, country, follow-up duration (years), participants’ sex and age, number of participants and cases, evaluation of exposure and outcome, most fully adjusted risk estimates with corresponding 95% CIs for the highest versus the lowest category of type 2 diabetes in relation to work-related stress category and sex, and the main confounding factors controlled for in the analysis. Study selection and data extraction were conducted by two experienced investigators independently. Any differences were resolved by consensus.
The Newcastle-Ottawa Quality Assessment Scale for cohort studies[18], in which a study is judged mainly according to the selection of study groups, comparability of the groups, and ascertainment of the exposure and outcome, was used to assess the quality of observational studies. The highest score possible is nine stars, we considered a study with six stars or above as a high-quality study.
Statistical Analysis
The RRs were used to examine associations across studies. To accomplish this, the HRs were regarded directly as RRs. The ORs were transformed into RRs using the following formula:
Where Po is the incidence of the outcome of interest in the unexposed group [19]. We found that outcomes across studies were relatively uncommon as the ORs mathematically approximated the RRs; therefore, we considered ORs as surrogates for RRs [20]. Statistical heterogeneity across studies was examined by Cochran’s Q statistics and quantified by I2 statistics. For the Q statistic, a P value < 0.10 was considered to indicate statistically significant heterogeneity. The I2 values vary from 0 to 100, with a level of 25% or less considered low heterogeneity, about 50% medium heterogeneity, and about 75% or greater high heterogeneity [21]. The fixed-effect model (inverse-variance method) [22] was used to compute summary RRs across studies. When statistically significant heterogeneity was detected, the pooled risk estimate was based on the random-effects model [23] because both within and between variations were present across the studies.
Meta-analyses generally include only one effect size per study. If more than one kind of work-related psychosocial factor was analyzed in a single article, we treated these factors as subjects of separate studies. Results that were presented separately by sex were entered into the meta-analyses as independent studies. To obtain more robust summary results, we calculated the pooled risk estimates and 95% CI of type 2 diabetes incidence for job demands, decision latitude, and job strain separately for highest versus lowest category [24] of work-related psychosocial factors.
Subgroup analyses were carried out to evaluate possible sources of statistical heterogeneity and to examine the potential impacts of participant characteristics (sex) on the relationship between work-related stress and incidence of type 2 diabetes. To assess the robustness of this relationship, we also conducted sensitivity analyses in which single studies were sequentially omitted and the remaining studies were synthesized to evaluate the influence of individual studies on the summary risk estimate.
Visual inspection of a funnel plot was used to detect publication or other types of bias. In the presence of publication bias, the funnel plot should be asymmetrical [25]. Meta-analysis was performed using Review Manager version 5.2 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). All statistical tests were two-sided and P<0.05 was considered statistically significant.
Results
Literature search
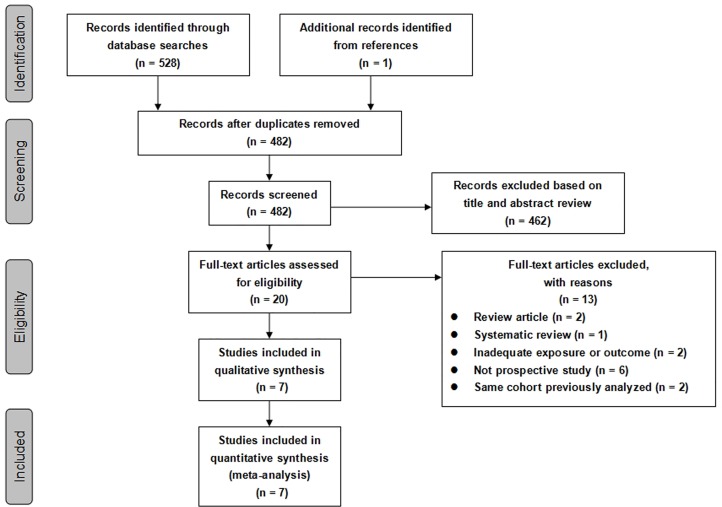
A flow diagram is shown in Fig 1. The literature search identified a total of 528 articles: 51 from PubMed, 40 from EMBASE, 0 from the Cochrane Library and 437 from Web of Science. Manual searching of the references yielded 1 additional record. A total of 47 duplicate articles were excluded, leaving 482 articles for screening. Among these, 462 articles were removed at the first screening on the basis of their titles or abstracts, leaving 20 studies for full-text review. In this review, 13 studies were excluded for various reasons (review, systematic review, inadequate exposures or outcomes, not prospective cohort studies, or data from the same cohort). There were seven prospective cohort studies [26–32] were included in this systematic review and meta-analysis. Additionally, three articles [28,33,34] were based on the same cohort as the Whitehall II study, but with different durations of follow-up. To avoid duplicate inclusion of study population, we selected the studies with a longer follow-up and more complete analysis [28].
Fig 1. Flow chart for selection of articles included in the meta-analysis.
Study characteristics
We identified seven prospective cohort studies involving 214,086 participants and 5,511 cases. Type 2 diabetes was reported as the main outcome in these articles, except for one study [29] that did not identify diabetes type (given the high prevalence of type 2 diabetes, in particular among older cohorts, this restriction was unlikely to impact the results [35]).The characteristics of the studies included in our analysis are presented in Table 1. The selected studies were published between 1999 and 2014. Regarding study location, four were performed in Europe [28,30–32], one in the United States [27], one in Canada [29], and one in Japan [26]. Four studies surveyed population-based cohorts [29–32] and three surveyed occupational cohorts [23–25]. The average follow-up duration ranged from 5.8 to 10.3 years. The number of subjects varied from 2,597 to 124,808, and the number of cases investigated in the studies ranged from 34 to 5,511. Five studies recruited both men and women [28–32], one consisted of men only [26], and one consisted of women only [27]. Mean age at baseline ranged from 18 to 66 years. Overall, six reported results on the relationship between job demands and type 2 diabetes [28–30], six on decision latitude [28–30], and eight on job strain [26–28,30–32]. All studies used the Karasek Job Content Questionnaire to assess work-related psychosocial factors. Although type 2 diabetes ascertainment was primarily based on self-reports from physician diagnoses, most of the cases were comfirmed in medical records. Most studies were adjusted for a wide range of confounders, including age, body mass index (BMI), education, physical activity, smoking, alcohol consumption and family history of diabetes. Additionally, the study quality score ranged from six to eight.
Table 1. Main characteristics of cohort studies included in the meta-analysis.
| Study | Country/Cohort Designation | Follow-up (y) | Participants (cases) | Age (y) | Psychosocial work characteristics | Adjusted RR (95%CI) | Exposure assessment | Case ascertainment | Adjustment for potential confounders | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|
| Kawakami, 1999 [26] | Japan/Electrical Co. | 8 | 2597 men (34) | 18–60 | Job strain | M:1.34 (0.50,3.55) | JCQ | OGTT, FPG | Age, education, BMI, alcohol consumption, smoking, leisure time physical activity, family history | 8 |
| Kroenke 2007 [27] | USA/NHS II | 5.8 | 62574 women (365) | 29–46 | Job strain | F:1.11 (0.80,1.52) | JCQ | Confirmed self-report | Age, BMI, family history of diabetes, work hours, rotating night-shift work, hours at work sitting, job support, hours per week of, work at home, leisure-time physical activity, smoking, alcohol intake, trans-unsaturated fat intake, glycemic load, caffeine intake, marital status, number of children, menopausal status, vitamin supplementation, aspirin use | 6 |
| Heraclides 2009 [28] | UK/Whitehall II | 11.6 | 4166 men and 1729 women (308) | 35–55 | Job demands, Decision latitude, Job strain | Job demands: T: 0.88(0.70–1.10) M: 0.82 (0.63–1.07) F: 1.06 (0.70–1.62) Decision latitude: T: 0.94(0.75–1.18) M: 0.86 (0.66–1.13) F: 1.09 (0.70–1.69) Job strain: T: 1.04 (0.80–1.34) M: 0.82 (0.59–1.15) F: 1.59 (1.03–2.45) | JCQ | Confirmed self-report, OGTT, use of diabetes medication | Age | 7 |
| Smith, 2012 [29] | Canada/CHS | 9 | 3691 men and 3752 women (639) | 35–60 | Job demands, Decision latitude | Job demands: T:–M: 1.30 (0.81–2.08) F: 1.32 (0.75–2.33) Decision latitude: T:–M: 0.92 (0.56–1.51) F: 2.04 (1.15–3.61) | JCQ | Physician reported | Age, immigration status, ethnicity, marital status, urban or rural living location, education, heart disease at baseline, hypertension at baseline, depression at baseline, activity limitations at work due to health problems, shift schedule, weeks worked, multiple jobs, physical activity at work, smoking, alcohol, leisure time physical activity, fruit and vegetable consumption, BMI | 8 |
| Eriksson, 2013 [30] | Sweden/SDPP | 8–10 | 2227 men and 3205 women (171) | 35–56 | Job demands, Decision latitude, Job strain | Job demands: T:0.70 (0.50–1.10) M: 0.50 (0.30–0.90) F: 1.00 (0.50–2.00) Decision latitude: T: 1.30 (0.80–2.10) M: 0.90 (0.50–1.70) F: 2.40 (1.10–5.20) Job strain: T: 0.80 (0.50–1.40) M: 0.50 (0.30–0.90) F: 2.10 (0.90–4.80) | Swedish version of the JCQ | OGTT | Age, Educational level, psychological distress, family history of diabetes, BMI, physical activity, smoking, civil status | 8 |
| Huth, 2014 [31] | Germany/ MONICA | 12.7 | 3350 men and 1987 women (291) | 29–66 | Job strain | Job strain: T: 1.45 (1.00–2.10) M:–F: – | JCQ | Self-report | Age, sex, baseline survey, BMI, low education, physical intensity of work, parental history of diabetes, physical inactivity, smoking, alcohol intake, living alone | 8 |
| Nyberg, 2014[32] | Finland, France, Denmark, Sweden, UK/ IPD-Work | 10.3 | 54006 men and 70802women (3703) | 35–53 | Job strain | Job strain: T: 1.15 (1.06–1.25) M: 1.19 (1.06–1.34) F: 1.13 (1.00–1.28) | JCQ, DCQ | OGTT, hospital records, mortality register, medication reimbursement, self-report | Age, sex, SES, working hours, BMI, leisure-time physical activity, smoking, alcohol consumption | 8 |
NHS II, Nurses Health Study; CHS, Community Health Survey; SDPP, Stockholm Diabetes Prevention Program; MONICA, Monitoring Trends and Determinants of Cardiovascular Disease; IPD-Work, Individual-Participant-Data meta-analysis of Work; JCQ, Job Content Questionnaire; DCQ, demand control questionnaire; OGTT, oral glucose tolerance test; FPG, fasting plasma glucose; BMI, body mass index; SES, socioeconomic status.
Main analysis
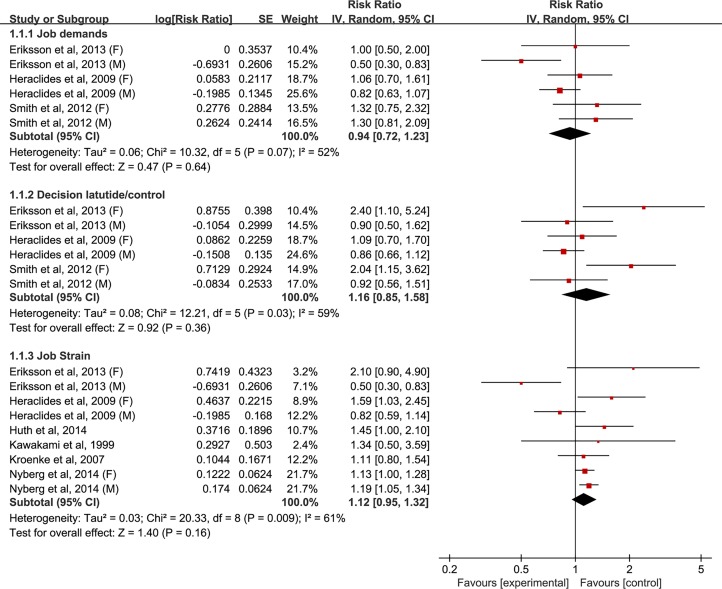
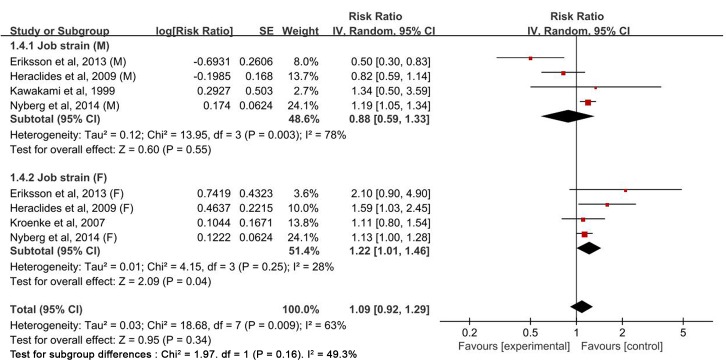
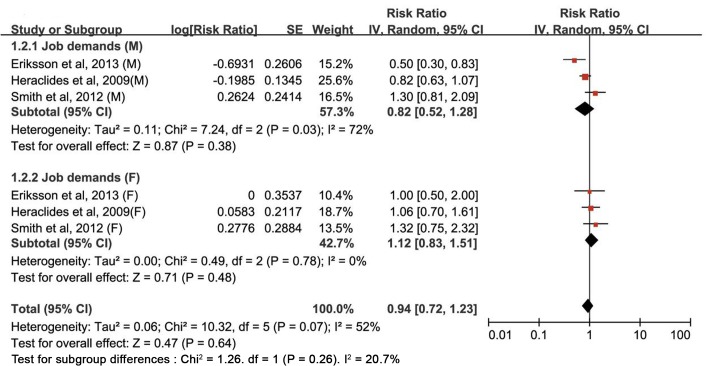
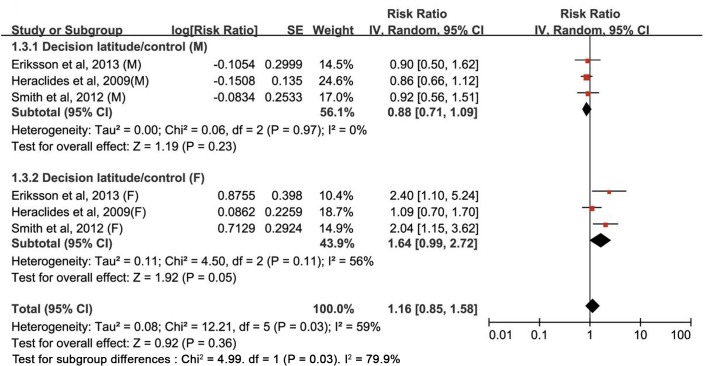
The multivariable-adjusted RRs of type 2 diabetes for each study and all studies combined for the highest versus the lowest category of four components of the job strain model are shown in Figs 2–5. The results of subgroup analyses stratified by sex are shown in Table 2.
Fig 2. Forest plot of the association between the job strain model and type 2 diabetes risk.
SE, standard error; CI, confidence interval; M, male; F, female.
Fig 5. Estimates of type 2 diabetes associated with job strain in men and women.
SE, standard error; CI, confidence interval; M, male; F, female.
Table 2. Subgroup analyses relating work stress to type 2 diabetes by sex.
| Type of work stress | Number of studies | RR | (95%CI) | P | Pheterogeneity | I2(%) | Pinteraction | References |
|---|---|---|---|---|---|---|---|---|
| Job demands | 0.26 | |||||||
| Total | 6 | 0.94 | (0.72–1.23) | 0.64 | 0.07 | 52.0 | 28–30 | |
| Male | 3 | 0.82 | (0.52–1.28) | 0.38 | 0.03 | 72.0 | 28–30 | |
| Female | 3 | 1.12 | (0.83–1.51) | 0.48 | 0.78 | 0 | 28–30 | |
| Decision latitude/control | 0.03 | |||||||
| Total | 6 | 1.16 | (0.85–1.58) | 0.36 | 0.03 | 59.0 | 28–30 | |
| Male | 3 | 0.88 | (0.71–1.09) | 0.23 | 0.97 | 0 | 28–30 | |
| Female | 3 | 1.64 | (0.99–2.72) | 0.05 | 0.11 | 56.0 | 28–30 | |
| Job strain | 0.16 | |||||||
| Total | 8 | 1.12 | (0.95–1.32) | 0.16 | 0.0009 | 61.0 | 26–28, 30, 31, 32 | |
| Male | 4 | 0.88 | (0.59–1.33) | 0.55 | 0.003 | 71.0 | 26, 28, 30, 32 | |
| Female | 4 | 1.22 | (1.01–1.46) | 0.04 | 0.25 | 28.0 | 27, 28, 30, 32 |
RR, relative risk; CI, confidence interval.
Job demands
In a pooled analysis of six studies, no significant relationship was observed between job demands and type 2 diabetes risk (RR: 0.94 [95% CI: 0.72–1.23]) (Fig 2). In subgroup analyses by sex, no significant association was in neither men (RR: 0.82 [0.52–1.28]) nor women (RR: 1.12 [0.83–1.51]). Substantial statistical heterogeneity was found among the studies (Pheterogeneity = 0.07, I2 = 52.0%); this heterogeneity remained significant for men (Pheterogeneity = 0.03, I2 = 72.0%), but not for women (Pheterogeneity = 0.78, I2 = 0.0%) (Fig 3 and Table 2). Sensitivity analyses evaluating the robustness of the association by sequentially omitting each study yielded a narrow range of RRs, from 0.93 (0.69–1.27) to 0.98 (0.82–1.18).
Fig 3. Estimates of type 2 diabetes associated with job demands in men and women.
SE, standard error; CI, confidence interval; M, male; F, female.
Decision latitude
The pooled results based on the six studies showed that the estimate of the association between decision latitude and the risk of type 2 diabetes was not significant (RR: 1.16 [0.85–1.58]) (Fig 2). In subgroup analyses by sex, no association was found between low decision latitude and high risk of type 2 diabetes both in women (RR: 1.64 [0.99–2.72]) (P = 0.05) and men (RR: 0.88 [0.71–1.09]) (P = 0.23). Statistically significant heterogeneity was observed across studies (Pheterogeneity = 0.03, I2 = 59.0%); this heterogeneity remained substantial for women (Pheterogeneity = 0.11, I2 = 56.0%), but not for men (Pheterogeneity = 0.97, I2 = 0.0%) (Fig 4 and Table 2). Sensitivity analyses assessing the robustness of the association by sequentially omitting each study yielded a narrow range of RRs, from 0.97 (0.80–1.17) to 1.05 (0.80–1.38).
Fig 4. Estimates of type 2 diabetes associated with decision latitude/control in men and women.
SE, standard error; CI, confidence interval; M, male; F, female.
Job strain
In a pooled analysis of nine studies, no association was found between job strain and risk of type 2 diabetes (RR: 1.12 [0.95–1.32]) (Fig 2). When stratified by sex, the studies for women showed job strain is the risk of type 2 diabetes (RR: 1.22 [1.01–1.46]) (P = 0.04), but not for men (RR: 0.88 [0.59–1.33]). Significant heterogeneity was evident among studies (Pheterogeneity = 0.0009, I2 = 61.0%); this heterogeneity showed a reduction for women (Pheterogeneity = 0.25, I2 = 28.0%), but remained significant for men (Pheterogeneity = 0.003, I2 = 78.0%) (Fig 5 and Table 2). Sensitivity analyses testing the robustness of our findings by sequentially excluding each study yielded a narrow range of RRs, from1.08(0.92–1.28)to 1.17(1.05–1.32)
Publication bias
Although the number of studies included in the analysis was limited, no publication bias was detected using a funnel plot.
Discussion
Main findings
Consistent with previous meta-analyses [14], our results did not confirm the association between work-related stress and risk for type 2 diabetes. We included prospective cohort studies to minimize the possibility of selection and recall biases. Furthermore, we conducted stratified analyses to explore sources of heterogeneity which improved the clinical value of this research [36]. More importantly, the association observed in women implied that sex may serve as an effect modifer of the association between work-related stress and type 2 diabetes. In our subgroup analyses, the effect of sex on the association between job strain and type 2 diabetes was obvious(P = 0.04). So job strain was a risk factor for type 2 diabetes in women.
At first we did not include the paper published by Nyberg et al. [32]. The results showed work-related stress was not a risk for type 2 diabetes (job demands: RR 0.94 [95% confidence interval 0.72–1.23]; decision latitude: RR 1.16 [0.85–1.58]; job strain: RR 1.11 [0.81–1.53]). When stratified by sex, the studies for women showed no effect of job strain on the development of type 2 diabetes (RR: 1.38 [0.99–1.91]) (P = 0.06). This study[32] is a multi center study, the researchers extracted individual-level data for 124,808 diabetes-free adults from 13 European cohort studies participating in the IPD-Work Consortium. Later, we included this article. Although the hypothesis that work-related psychosocial stress increases the risk for type 2 diabetes cannot be supported, in the subgroup analyses we found job strain was a risk factor for type 2 diabetes in women, (RR: 1.22 [1.01–1.46]) (P = 0.04).
Significant statistical heterogeneity was detected among these studies, further sensitivity analysis yielded similar results across studies. It was not surprising that significant heterogeneity was found due to the variations in ethnicity, method of case ascertainment, the components of the job strain model compared, and adjustment among studies. In the subgroup analyses by sex, heterogeneity showed a reduction. This suggests that sex may, at least partially, be responsible for heterogeneity.
Possible mechanism
A causal relationship between work-related stress and the incidence of type 2 diabetes is biologically credible. Type 2 diabetes is associated with work-related psychosocial stress via two key patterns including dysregulation of neuroendocrine and lifestyle-related factors. Dysregulation of neuroendocrine pathways maybe the most important mechanism. Work-related psychosocial stress may increase the risk for type 2 diabetes through chronic activation of the hypothalamus–pituitary–adrenal axis and the sympathetic nervous system, lead to the release of sympathetic hormones and glucocorticoids such as cortisol, resulting in increased hepatic glucose output, decreased insulin secretion, insulin resistance and visceral obesity. Chronic psychosocial work-related stress is associated with elevated cortisol levels [37]. Cortisol can influence the regulation of blood glucose by altering the body’s release of insulin and sensitivity to insulin, resulting in an increased risk of type 2 diabetes [38]. The indirect mechanism is the changes of lifestyle-related factors, such as poor eating behavior, physical inactivity, smoking and alcohol consumption [39–41], all of which have been shown to increase the risk for type 2 diabetes. However, the results regarding the association between work stress and type 2 diabetes are inconsistent. For example, one previous meta-analysis could not support the hypothesis that work-related stress increased the risk for type 2 diabetes [14]. Findings from a large pan-European dataset suggested that job strain is a risk factor for type 2 diabetes in men and women, independent of lifestyle-related factors [31]. Furthermore, long hours of overtime work may not be associated with increased prevalence of diabetes among Japanese [42].
In subgroup analyses we found job strain was related to risk of type 2 diabetes in female. Some previous researches have similar results [15,27,30]. Eriksson and colleagues [30] speculated that sex-based differences regarding the effects of work-related stress could be attributable to a divergence in gender roles outside work, as women tend to spend more time than men on household responsibilities and childcare, thereby not having the same opportunity to relax [43–47]. Additionally, some evidence suggest that women may be more prone to the health impact of chronic psychosocial stress due to gender-specific psychoneuroendocrine activation [43,48–50]. Among a subsample from the Whitehall II study, men and women had similar salivary cortisol levels during weekends, but women had significantly higher cortisol levels than men during working days [51]. Similar results have been observed in one Italian [52] and one German [53] study, which are regarding gender-specific cortisol responses to chronic work-related stress. The generation of job stress has a different pattern in men and women. Both quantitative and qualitative (intellectual and emotional) demands determine occupational stress in women, while only quantitative demands are stressors for men[54]. Support has a significantly stronger impact on levels of job stress in the workplace among women[15, 54].
Although we are unable to confirm that work-related stress increases the risk for type 2 diabetes, women in high demand and low-control occupations could be at a greater risk of negative health consequences [55].
Limitations
Several limitations should be acknowledged. First, observational studies cannot establish causal relationships between exposure factors and outcome events. Second, residual confounding remains a concern. A wide range of potential confounders were adjusted for in most studies, including age, BMI, physical activity, smoking, alcohol consumption and family history of diabetes. However, stress indices unrelated to work (such as depression, anxiety, life events, stress-prone personality, coping style and sleeping problems) and factors in other work-related stress models (such as work hours, rotating night-shift work, effort-reward imbalance and job insecurity) were not sufficiently adjusted. Therefore, we could not fully exclude the possibility that unadjusted confounders had effects on the association with risk for type 2 diabetes. Third, misclassification bias may have attenuated the association. Because work-related stress assessment was based on self-administered questionnaires, misclassification of work-related stress was inevitable. Case ascertainment in most studies was based on self-reports, so there could have been misclassification of type 2 diabetes cases. Additionally, one study [29] that did not distinguish between different types of diabetes might have weakened the relationships.We limited studies to publications in English. Multiple stress indicators across studies may have increased the risk of selective publication. Publication bias was thus conceivable, even though it was not detected using a funnel plot [56]. In addition, there are some other limitations. Sample sizes ranged from 2597 to 124808, thus the largest study [32] may have largely determined the results. A wide age range (18 to 66 years) and a wide range of follow-up time (5.8 to 12.7 years) limit the research. There is also only one Asian sample from Japan[26], limiting the study relevance for Asian populations.
Clinical implications
Until now, large scale and well-conducted randomized controlled trials, the gold standard for investigating a causal association [57], have not been conducted to directly assess the effect of work-related stress on risk for type 2 diabetes. With mounting observational studies of the diabetogenic effect of work-related stress, randomized controlled trials should focus on the reduction of work-related stress, either by improving the work environment or by improving individual coping strategies, especially for women [15].
In conclusion, the hypothesis that work-related psychosocial stress increases the risk for type 2 diabetes could not be supported from the meta-analysis. In a subgroup analysis we found job strain to increase the risk of type 2 diabetes in women. Although the more general hypothesis was not supported, our results suggest that it may depend on a number of factors, and thus further study is needed.
Supporting Information
(DOC)
Data Availability
All relevant data are within the paper.
Funding Statement
This work was financially supported by The Key Project of National Natural Science Foundation of China (No. 81230084), and by the Specialized Research Fund for the Doctoral Program of Higher Education of China (20132105130001). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.(2015) International Diabetes Federation. IDF Diabetes, 7 ed. Brussels, Belgium: International Diabetes Federation; Available: http://www.diabetesatlas.org. [Google Scholar]
- 2.Willis T (1674) Pharmaceutice rationalis sive diatriba demedicamentorum operationibus in humano corpore. E Theatro Sheldoniano. MDCLXXV. Oxford.
- 3.Menninger WC (1935) Psychological factors in etiology of diabetes. J Nerv Ment Dis 81: 1–13. [Google Scholar]
- 4.Engel GL (1977) The need for a new medical model: a challenge for biomedicine. Science 196: 129–136. [DOI] [PubMed] [Google Scholar]
- 5.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palermo A, Maggi D, Maurizi AR, Pozzilli P, Buzzetti R (2014) Prevention of type 2 diabetes mellitus: is it feasible? Diabetes Metab Res Rev 30 Suppl 1: 4–12. 10.1002/dmrr.2513 [DOI] [PubMed] [Google Scholar]
- 7.Anderson JW, Kendall CW, Jenkins DJ (2003) Importance of weight management in type 2 diabetes: review with meta-analysis of clinical studies. J Am Coll Nutr 22: 331–339. [DOI] [PubMed] [Google Scholar]
- 8.Pan A, Wang Y, Talaei M, Hu FB, Wu T (2015) Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 3: 958–967. 10.1016/S2213-8587(15)00316-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cullmann M, Hilding A, Ostenson CG (2012) Alcohol consumption and risk of pre-diabetes and type 2 diabetes development in a Swedish population. Diabet Med 29: 441–452. 10.1111/j.1464-5491.2011.03450.x [DOI] [PubMed] [Google Scholar]
- 10.Karasek R, Baker D, Marxer F, Ahlbom A, Theorell T (1981) Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Public Health 71: 694–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fishta A, Backe EM (2015) Psychosocial stress at work and cardiovascular diseases: an overview of systematic reviews. Int Arch Occup Environ Health 88: 997–1014. 10.1007/s00420-015-1019-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steptoe A, Kivimaki M (2012) Stress and cardiovascular disease. Nat Rev Cardiol 9: 360–370. 10.1038/nrcardio.2012.45 [DOI] [PubMed] [Google Scholar]
- 13.Kivimaki M, Nyberg ST, Fransson EI, Heikkila K, Alfredsson L, Casini A, et al. (2013) Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ 185: 763–769. 10.1503/cmaj.121735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cosgrove MP, Sargeant LA, Caleyachetty R, Griffin SJ (2012) Work-related stress and Type 2 diabetes: systematic review and meta-analysis. Occup Med (Lond) 62: 167–173. [DOI] [PubMed] [Google Scholar]
- 15.Norberg M, Stenlund H, Lindahl B, Andersson C, Eriksson JW, Weinehall L. (2007) Work stress and low emotional support is associated with increased risk of future type 2 diabetes in women. Diabetes Res Clin Pract 76: 368–377. [DOI] [PubMed] [Google Scholar]
- 16.Karasek R TT (1990) Healthy Work: Stress, productivity, and the reconstruction of the working life: New York, Basic Books. [Google Scholar]
- 17.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- 18.Wells GS, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. Available: www.ohri.ca/programs/clinical epidemiology/oxford.asp.: Ottawa Health Research Institute.
- 19.Zhang J, Yu KF (1998) What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280: 1690–1691. [DOI] [PubMed] [Google Scholar]
- 20.McNutt LA, Wu C, Xue X, Hafner JP (2003) Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol 157: 940–943. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woolf B (1955) On estimating the relation between blood group and disease. Ann Hum Genet 19: 251–253. [DOI] [PubMed] [Google Scholar]
- 23.DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 24.Danesh J, Collins R, Appleby P, Peto R (1998) Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA 279: 1477–1482. [DOI] [PubMed] [Google Scholar]
- 25.Sterne JA, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 54: 1046–1055. [DOI] [PubMed] [Google Scholar]
- 26.Kawakami N, Araki S, Takatsuka N, Shimizu H, Ishibashi H (1999) Overtime, psychosocial working conditions, and occurrence of non-insulin dependent diabetes mellitus in Japanese men. J Epidemiol Community Health 53: 359–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroenke CH, Spiegelman D, Manson J, Schernhammer ES, Colditz GA, Kawachi I. (2007) Work characteristics and incidence of type 2 diabetes in women. Am J Epidemiol 165: 175–183. [DOI] [PubMed] [Google Scholar]
- 28.Heraclides A, Chandola T, Witte DR, Brunner EJ (2009) Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: evidence from the Whitehall II study. Diabetes Care 32: 2230–2235. 10.2337/dc09-0132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith PM, Glazier RH, Lu H, Mustard CA (2012) The psychosocial work environment and incident diabetes in Ontario, Canada. Occup Med (Lond) 62: 413–419. [DOI] [PubMed] [Google Scholar]
- 30.Eriksson AK, van den Donk M, Hilding A, Ostenson CG (2013) Work stress, sense of coherence, and risk of type 2 diabetes in a prospective study of middle-aged Swedish men and women. Diabetes Care 36: 2683–2689. 10.2337/dc12-1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huth C, Thorand B, Baumert J, Kruse J, Emeny RT, Schneider A, et al. (2014) Job strain as a risk factor for the onset of type 2 diabetes mellitus: findings from the MONICA/KORA Augsburg cohort study. Psychosom Med 76: 562–568. 10.1097/PSY.0000000000000084 [DOI] [PubMed] [Google Scholar]
- 32.Nyberg ST, Fransson EI, Heikkila K, Ahola K, Alfredsson L, Bjorner JB, et al. (2014) Job strain as a risk factor for type 2 diabetes: a pooled analysis of 124,808 men and women. Diabetes Care 37: 2268–2275. 10.2337/dc13-2936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumari M, Head J, Marmot M (2004) Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II study. Arch Intern Med 164: 1873–1880. [DOI] [PubMed] [Google Scholar]
- 34.Heraclides AM, Chandola T, Witte DR, Brunner EJ (2012) Work stress, obesity and the risk of type 2 diabetes: gender-specific bidirectional effect in the Whitehall II study. Obesity (Silver Spring) 20: 428–433. [DOI] [PubMed] [Google Scholar]
- 35.American Diabetes Association (2005) Diagnosis and classification of diabetes mellitus. Diabetes Care 28: S37–S42. [DOI] [PubMed] [Google Scholar]
- 36.Thompson SG (1994) Why sources of heterogeneity in meta-analysis should be investigated. BMJ 309: 1351–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chida Y, Steptoe A (2009) Cortisol awakening response and psychosocial factors: a systematic review and meta-analysis. Biol Psychol 80: 265–278. 10.1016/j.biopsycho.2008.10.004 [DOI] [PubMed] [Google Scholar]
- 38.McEwen BS (1998) Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci 840: 33–44. [DOI] [PubMed] [Google Scholar]
- 39.Bonnet F, Irving K, Terra JL, Nony P, Berthezene F, Moulin P. (2005) Anxiety and depression are associated with unhealthy lifestyle in patients at risk of cardiovascular disease. Atherosclerosis 178: 339–344. [DOI] [PubMed] [Google Scholar]
- 40.McEwen BS (1998) Protective and damaging effects of stress mediators. N Engl J Med 338: 171–179. [DOI] [PubMed] [Google Scholar]
- 41.Rod NH, Gronbaek M, Schnohr P, Prescott E, Kristensen TS (2009) Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J Intern Med 266: 467–475. 10.1111/j.1365-2796.2009.02124.x [DOI] [PubMed] [Google Scholar]
- 42.Kuwahara K, Imai T, Nishihara A, Nakagawa T, Yamamoto S, Honda T (2014) Overtime work and prevalence of diabetes in Japanese employees: Japan epidemiology collaboration on occupational health study. PLoS One 9: e95732 10.1371/journal.pone.0095732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lundberg U (2005) Stress hormones in health and illness: the roles of work and gender. Psychoneuroendocrinology 30: 1017–1021. [DOI] [PubMed] [Google Scholar]
- 44.Frankenhaeuser M, Lundberg U, Fredrikson M, Melin B, Tuomisto M, Myrsten A, et al. (1989) Stress on and off the job as related to sex and occupational status in white-collar workers. J Organ Behav 10: 321–346. [Google Scholar]
- 45.Lundberg U, Frankenhaeuser M (1999) Stress and workload of men and women in high-ranking positions. J Occup Health Psychol 4: 142–151. [DOI] [PubMed] [Google Scholar]
- 46.Lundberg U, Mardberg B, Frankenhaeuser M (1994) The total workload of male and female white collar workers as related to age, occupational level, and number of children. Scand J Psychol 35: 315–327. [DOI] [PubMed] [Google Scholar]
- 47.Berntsson L, Lundberg U, Krantz G (2006) Gender differences in work-home interplay and symptom perception among Swedish white-collar employees. J Epidemiol Community Health 60: 1070–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rohleder N, Kudielka BM, Hellhammer DH, Wolf JM, Kirschbaum C (2002) Age and sex steroid-related changes in glucocorticoid sensitivity of pro-inflammatory cytokine production after psychosocial stress. J Neuroimmunol 126: 69–77. [DOI] [PubMed] [Google Scholar]
- 49.Kirschbaum C, Hellhammer DH (1999) Noise and Stress—Salivary Cortisol as a Non-Invasive Measure of Allostatic Load. Noise Health 1: 57–66. [PubMed] [Google Scholar]
- 50.Wust S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C. (2000) The cortisol awakening response—normal values and confounds. Noise Health 2: 79–88. [PubMed] [Google Scholar]
- 51.Kunz-Ebrecht SR, Mohamed-Ali V, Feldman PJ, Kirschbaum C, Steptoe A (2003) Cortisol responses to mild psychological stress are inversely associated with proinflammatory cytokines. Brain Behav Immun 17: 373–383. [DOI] [PubMed] [Google Scholar]
- 52.Maina G, Palmas A, Bovenzi M, Filon FL (2009) Salivary cortisol and psychosocial hazards at work. Am J Ind Med 52: 251–260. 10.1002/ajim.20659 [DOI] [PubMed] [Google Scholar]
- 53.Schulz P, Kirschbaum C, Prüßner J, Hellhammer D (1998) Increased free cortisol secretion after awakening in chronically stressed individuals due to work overload. Stress Med 14: 91–97. [Google Scholar]
- 54.Rivera-Torres P, Araque-Padilla RA, Montero-Simó MJ (2013) Job stress across gender: the importance of emotional and intellectual demands and social support in women. Int J Environ Res Public Health. 10:375–89. 10.3390/ijerph10010375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Krajnak KM (2014) Potential Contribution of Work-Related Psychosocial Stress to the Development of Cardiovascular Disease and Type II Diabetes: A Brief Review. Environ Health Insights 8: 41–45. 10.4137/EHI.S15263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Macaskill P, Walter SD, Irwig L (2001) A comparison of methods to detect publication bias in meta-analysis. Stat Med 20: 641–654. [DOI] [PubMed] [Google Scholar]
- 57.Concato J, Shah N, Horwitz RI (2000) Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med 342: 1887–1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the paper.